
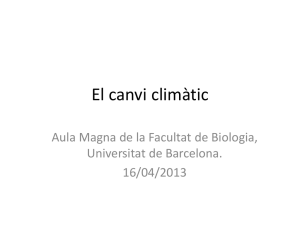
Original Investigation | Public Health Associations Between Procrastination and Subsequent Health Outcomes Among University Students in Sweden Fred Johansson, MA; Alexander Rozental, PhD; Klara Edlund, PhD; Pierre Côté, PhD; Tobias Sundberg, PhD; Clara Onell, MSc; Ann Rudman, PhD; Eva Skillgate, PhD Abstract Key Points IMPORTANCE Procrastination is prevalent among university students and is hypothesized to lead to adverse health outcomes. Previous cross-sectional research suggests that procrastination is associated with mental and physical health outcomes, but longitudinal evidence is currently scarce. Question Is procrastination associated with subsequent health outcomes among university students? Findings In this cohort study of 3525 OBJECTIVE To evaluate the association between procrastination and subsequent health outcomes Swedish university students, among university students in Sweden. procrastination was associated with worse subsequent mental health DESIGN, SETTING, AND PARTICIPANTS This cohort study was based on the Sustainable University (depression, anxiety, and stress Life study, conducted between August 19, 2019, and December 15, 2021, in which university students symptom levels), having disabling pain recruited from 8 universities in the greater Stockholm area and Örebro were followed up at 5 time in the upper extremities, unhealthy points over 1 year. The present study used data on 3525 students from 3 time points to assess lifestyle behaviors (poor sleep quality whether procrastination was associated with worse health outcomes 9 months later. and physical inactivity), and worse levels of psychosocial health factors (higher EXPOSURE Self-reported procrastination, measured using 5 items from the Swedish version of the loneliness and more economic Pure Procrastination Scale rated on a Likert scale from 1 (“very rarely or does not represent me”) to difficulties). 5 (“very often or always represents me”) and summed to give a total procrastination score ranging from 5 to 25. Meaning This study suggests that procrastination may be associated with a range of health outcomes. MAIN OUTCOMES AND MEASURES Sixteen self-reported health outcomes were assessed at the 9-month follow-up. These included mental health problems (symptoms of depression, anxiety, and stress), disabling pain (neck and/or upper back, lower back, upper extremities, and lower extremities), unhealthy lifestyle behaviors (poor sleep quality, physical inactivity, tobacco use, cannabis use, alcohol use, and breakfast skipping), psychosocial health factors (loneliness and + Supplemental content Author affiliations and article information are listed at the end of this article. economic difficulties), and general health. RESULTS The study included 3525 participants (2229 women [63%]; mean [SD] age, 24.8 [6.2] years), with a follow-up rate of 73% (n = 2587) 9 months later. The mean (SD) procrastination score at baseline was 12.9 (5.4). An increase of 1 SD in procrastination was associated with higher mean symptom levels of depression (β, 0.13; 95% CI, 0.09-0.17), anxiety (β, 0.08; 95% CI, 0.04-0.12), and stress (β, 0.11; 95% CI, 0.08-0.15), and having disabling pain in the upper extremities (risk ratio [RR], 1.27; 95% CI, 1.14-1.42), poor sleep quality (RR, 1.09, 95% CI, 1.05-1.14), physical inactivity (RR, 1.07; 95% CI, 1.04-1.11), loneliness (RR, 1.07; 95% CI, 1.02-1.12), and economic difficulties (RR, 1.15, 95% CI, 1.02-1.30) at the 9-month follow-up, after controlling for a large set of potential confounders. CONCLUSIONS AND RELEVANCE This cohort study of Swedish university students suggests that procrastination is associated with subsequent mental health problems, disabling pain, unhealthy lifestyle behaviors, and worse psychosocial health factors. Considering that procrastination is (continued) Open Access. This is an open access article distributed under the terms of the CC-BY License. JAMA Network Open. 2023;6(1):e2249346. doi:10.1001/jamanetworkopen.2022.49346 (Reprinted) Downloaded From: https://jamanetwork.com/ by a Mexico | Access Provided by JAMA User on 01/05/2023 January 4, 2023 1/11 JAMA Network Open | Public Health Associations Between Procrastination and Health Outcomes Among University Students Abstract (continued) prevalent among university students, these findings may be of importance to enhance the understanding of students’ health. JAMA Network Open. 2023;6(1):e2249346. doi:10.1001/jamanetworkopen.2022.49346 Introduction Procrastination is defined as voluntarily delaying an intended course of action despite expecting to be worse off because of the delay1 and is common, especially among younger people.2,3 It is estimated that at least half of university students engage in consistent and problematic procrastination, such as postponing studying for examinations or writing papers.1,4 Procrastination is described as a form of self-regulatory failure linked to personality traits such as impulsiveness,5,6 distractibility, and low conscientiousness.1,7 An individual’s tendency to procrastinate is relatively stable over time, but specific procrastination behaviors are influenced by contextual factors such as task aversiveness.1 For some students, procrastination is occasional and related to specific academic tasks, while for others it is more of a general disposition, potentially affecting academic achievements8 and health. Cross-sectional studies suggest that procrastination is associated with symptoms of depression, anxiety, and stress as well as loneliness and reduced life satisfaction.2,9-11 Procrastination is also associated with prevalent general physical health problems,12 cardiovascular disease,13 and unhealthy lifestyle behaviors.12,14,15 Students engaged in university studies have high levels of freedom and low structure, which places high demands on their capacity to self-regulate.16 These high demands on self-regulation may explain the high prevalence of procrastination among university students and make persons who are prone to procrastinate more vulnerable to the negative consequences of procrastination while at the university.16 The procrastination health model12,17 suggests that a general tendency to procrastinate is associated with negative health outcomes by increasing levels of stress, reducing healthy behaviors, and delaying treatment.12,17,18 However, the causal direction between procrastination and health outcomes is not well understood and could be bidirectional, with poor physical or mental health reducing energy levels and motivation, potentially leading to more procrastination. Some of the strongest support for the causal claims of the procrastination health model comes from studies on the effects of treating procrastination. Results from randomized clinical trials suggest that intervening on procrastination with psychological treatments can reduce subsequent levels of depression and anxiety and improve quality of life.19 However, the evidence is limited as there are only a few studies, with a focus solely on mental health outcomes.19 The procrastination health model provides a useful theoretical foundation for how procrastination could affect different health outcomes.12,17 However, longitudinal evidence from studies of procrastination and subsequent health outcomes is scant and focuses on only 1 or a few health outcomes.20-23 Furthermore, most studies have limited control for important confounders, including other health problems, age, and sociodemographic factors. Also, no study has, to our knowledge, controlled for the potential reverse causation that may arise if health problems increase procrastination. In this study, we investigated the associations between procrastination and a range of subsequent health outcomes while controlling for a large set of potential confounders, including prior levels of the outcomes. This method allows for stronger conclusions regarding the causal direction24 between procrastination and health outcomes and can provide a broader picture of the potential associations between procrastination and health. We aimed to evaluate the associations between procrastination and 16 health outcomes at the end of a 9-month period. The outcomes include mental health, disabling pain, and several unhealthy JAMA Network Open. 2023;6(1):e2249346. doi:10.1001/jamanetworkopen.2022.49346 (Reprinted) Downloaded From: https://jamanetwork.com/ by a Mexico | Access Provided by JAMA User on 01/05/2023 January 4, 2023 2/11 JAMA Network Open | Public Health Associations Between Procrastination and Health Outcomes Among University Students lifestyle behaviors and psychosocial health factors. Following the procrastination health model,12,17 we hypothesized that higher levels of procrastination would be associated with worse health outcomes at follow-up. Methods Design and Study Population The cohort for this study came from the Sustainable University Life study,25 which followed up Swedish university students for 1 year using web-based surveys. Undergraduate or graduate students (up to and including masters’ level) at full-time educational programs, with at least 1 year left of their education were eligible to participate. Students were recruited from 8 universities in the greater Stockholm area and Örebro. Data collection was ongoing from August 19, 2019, to December 15, 2021. The targeted universities represent a convenience sample and were selected to provide a variety of different types of disciplines, such as medicine, technology, social sciences, and economics and were restricted to universities in a limited geographical area to enable physical presence by study staff. The study was approved by the Swedish Ethical Review Authority and all participants provided informed consent electronically. More information about the study methods and data collection is available in the study protocol.25 This study is reported following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline for cohort studies. Eligible students were informed about the study during an in-class presentation and/or by an email with a link to the survey. Students who agreed to participate were followed up every 3 months for 1 year at 5 time points. In the present data analysis, the first time point was defined as prebaseline and was used for measures of the covariates. The second time point was defined as the baseline and was used for the procrastination measure and the fifth time point was defined as the 9-month follow-up and used for measurement of the health outcomes (Figure 1). The follow-up period of 9 months represents the length of an academic year, which we believe is adequate for procrastination to manifest its potential associations with different health outcomes. The sample was restricted to those responding at baseline and included 3525 participants; the follow-up rate was 73% (n = 2587) at the 9-month follow-up (Figure 2). Measures Exposure: Procrastination Procrastination was measured using 5 items from the Swedish version of the Pure Procrastination Scale (PPS).26 The items were rated on a Likert scale from 1 (“very rarely or does not represent me”) to 5 (“very often or always represents me”) and summed to give a total procrastination score ranging from 5 to 25. The short version of the PPS includes items 4 through 8 from the full PPS and has shown adequate psychometric properties in nonclinical samples.26,27 In this sample, the scale had a Cronbach α of 0.92 at baseline and a test-retest reliability (Pearson r) of 0.79 over 3 months and of 0.75 over 9 months. Figure 1. Timeline of Data Collection in the Sustainable University Life (SUN) Cohort and How Data Were Organized for the Present Study Time point in the SUN cohort (time since enrollment) Definition in present study Measures in the present study T1 (0) T2 (3 mo) Prebaseline Baseline Covariates Procrastination T3 (6 mo) T4 (9 mo) T5 (12 mo) 9-mo Follow-up (9 mo since baseline) Health outcomes JAMA Network Open. 2023;6(1):e2249346. doi:10.1001/jamanetworkopen.2022.49346 (Reprinted) Downloaded From: https://jamanetwork.com/ by a Mexico | Access Provided by JAMA User on 01/05/2023 T indicates time point. January 4, 2023 3/11 JAMA Network Open | Public Health Associations Between Procrastination and Health Outcomes Among University Students Outcomes We assessed a range of health outcomes at the 9-month follow-up, including mental health problems (symptoms of depression, anxiety, and stress), disabling pain (neck and/or upper back, lower back, upper extremities, and lower extremities), unhealthy lifestyle behaviors (poor sleep quality, physical inactivity, weekly tobacco use, monthly cannabis use, daily alcohol use, and breakfast skipping), psychosocial health factors (loneliness and economic difficulties), and general health. For more information on the outcome measures, see eMethods 1 in Supplement 1. Confounders Potential confounders were selected using the modified disjunctive cause criterion.28 This approach is a feasible alternative to directed acyclic graphs when the causal knowledge needed to produce a reliable directed acyclic graph is unavailable.28 We used the same set of covariates in all the outcome models, as has been suggested for outcome-wide studies.29 The covariate set included all outcome variables at prebaseline to limit the risk of reverse causation,30 as well as age, gender, highest parental level of education, previous physical and psychiatric diagnoses, civil status, place of birth, and university education type. All covariates were measured at prebaseline to ensure that none were mediators between procrastination and the outcomes. Information on covariate measurement and coding is provided in eMethods 1 in Supplement 1. Statistical Analysis The characteristics of the sample are presented in Table 1, both for the full sample and across quartiles of procrastination (procrastination score range, 5-25; first quartile, 5-9; second quartile, 10-12; third quartile, 13-17; and fourth quartile, 18-25). To assess whether procrastination was associated with the health outcomes at follow-up, we used the outcome-wide approach,29 a newly developed analytic approach to study associations between an exposure and multiple outcomes. We built separate multivariable regression models for each of the outcomes to assess the association between baseline procrastination and the different outcomes at the 9-month follow-up. For continuous outcomes, linear regression models were used. For binary outcomes, modified Poisson regressions31 were used (rather than logistic regression models because some outcomes were relatively common). Procrastination and all continuous outcome measures were standardized (mean = 0, SD = 1). Estimates for continuous outcomes are thus interpreted as the difference in the outcome as measured in SDs associated with a 1-SD increase in procrastination, and estimates for the binary outcomes are interpreted as the risk ratio (RR) of the outcome associated with a 1-SD increase in procrastination. All models were adjusted for the set of prebaseline confounders described. For Figure 2. Flowchart of the Inclusion of Participants 18 973 Invited to participate 14 711 Did not respond Included in the SUN cohort 4262 Prebaseline (T1) 96 Withdrew from study 641 Did not respond Study base 3525 Baseline (T2) 85 Withdrew from study 853 Did not respond Analytic sample 2587 9-mo Follow-up (T5) JAMA Network Open. 2023;6(1):e2249346. doi:10.1001/jamanetworkopen.2022.49346 (Reprinted) Downloaded From: https://jamanetwork.com/ by a Mexico | Access Provided by JAMA User on 01/05/2023 The definition of each time point (T) in the present study (T1, T2, and T5) refers to the time point in the Sustainable University Life (SUN) Cohort (Figure 1). Note that T3 and T4 are not shown here, because data from these time points were not used for the main analyses. January 4, 2023 4/11 JAMA Network Open | Public Health Associations Between Procrastination and Health Outcomes Among University Students unadjusted estimates, see eTable 1 in Supplement 1. Visual inspection of the residuals from all models indicated fairly linear associations between procrastination and the outcomes. The homoscedasticity and distribution of the residuals were not assessed because they typically have minor impact on the regression estimates,32 but the modified Poisson models still applies robust SEs. This analytic Table 1. Characteristics of Participants Prebaseline for the Full Sample and by Quartiles of Procrastination Levelsa Participants, No. (%) Procrastination quartileb Characteristic Full sample (N = 3525) First (n = 1052) Second (n = 713) Third (n = 1003) Fouth (n = 757) Age, mean (SD), y 24.8 (6.2) 25.3 (6.7) 24.8 (6.3) 24.7 (6.2) 24.0 (5.5) Female 2229 (63) 674 (64) 458 (64) 640 (64) 457 (60) Male 1274 (36) NRc NRc NRc NRc Other 22 (1) NRc NRc NRc NRc Gender Education type Medical or health 1688 (48) 556 (53) 343 (48) 471 (47) 318 (42) Technical 1407 (40) 354 (34) 274 (38) 413 (41) 366 (48) Social science or humanities 294 (8) 100 (10) 68 (10) 79 (8) 47 (6) Economic 85 (2) 28 (3) 16 (2) 28 (3) 13 (2) Other 51 (1) 14 (1) 12 (2) 12 (1) 13 (2) Civil status Single 1975 (56) 494 (47) 395 (55) 594 (59) 492 (65) Cohabiting partner 1133 (32) 435 (41) 227 (32) 294 (29) 177 (23) Noncohabiting partner 417 (12) 123 (12) 91 (13) 115 (11) 88 (12) Sweden 2826 (80) 859 (82) 579 (81) 797 (79) 591 (78) Other Nordic countries 118 (3) 38 (4) 23 (3) 31 (3) 26 (3) Other Europe 192 (5) 57 (5) 41 (6) 61 (6) 33 (4) Outside Europe 389 (11) 98 (9) 70 (10) 114 (11) 107 (14) Place of birth Highest parental educational level University 2553 (72) 747 (71) 513 (72) 737 (73) 556 (73) Abbreviation: NR, not reported. Less than university 972 (28) 305 (29) 200 (28) 266 (27) 201 (27) a 1.0 (1.3) 0.9 (1.2) 1.0 (1.3) 1.1 (1.2) 1.2 (1.4) Procrastination was measured at baseline, while all covariates and outcomes were measured prebaseline. Percentages of some categorical variables do not add up to 100% due to rounding. Depression symptoms 4.7 (4.7) 2.9 (3.6) 4.1 (4.2) 5.0 (4.4) 7.3 (5.4) b Anxiety symptoms 3.0 (3.3) 2.1 (2.9) 2.7 (3.1) 3.2 (3.2) 4.2 (4) Stress symptoms 6.3 (4.6) 5.0 (4.3) 6.0 (4.3) 6.7 (4.4) 7.9 (4.8) Neck and/or upper back 405 (11) 90 (9) 84 (12) 117 (12) 114 (15) Lower back 364 (10) 86 (8) 62 (9) 117 (12) 99 (13) Upper extremities 436 (12) 90 (9) 98 (14) 137 (14) 111 (15) The procrastination score ranged from 5 to 25, with the quartiles 9 (25th percentile), 12 (50th percentile), and 17 (75th percentile). Participants were categorized based on their procrastination score as follows: 5 to 9, first quartile; 10 to 12, second quartile; 13 to 17, third quartile; and 18 to 25, fourth quartile. c Lower extremities 545 (15) 123 (12) 106 (15) 162 (16) 154 (20) Poor sleep quality 1893 (54) 380 (36) 351 (49) 605 (60) 557 (74) Physically inactive 1831 (52) 438 (42) 364 (51) 548 (55) 481 (64) Daily alcohol use 51 (1) 7 (1) 17 (2) 12 (1) 15 (2) The gender categories “male” and “other” are not presented for procrastination quartiles because the “other” category had low cell counts (<5). The gender category “other” included participants responding “Other” or “Do not want to identify with either of these identities.” d Weekly tobacco use 542 (15) 136 (13) 130 (18) 141 (14) 135 (18) Monthly cannabis use 72 (2) 12 (1) 17 (2) 16 (2) 27 (4) Breakfast skipping 878 (25) 188 (18) 160 (22) 246 (25) 284 (38) Loneliness 1485 (42) 273 (26) 275 (39) 477 (48) 460 (61) Economic difficulties 555 (16) 110 (10) 110 (15) 172 (17) 163 (22) Poor general health 113 (3) 14 (1) 11 (2) 34 (3) 54 (7) The previous diagnoses variable is a count indicating how many of the following diagnoses the participants had received: rheumatic diseases; allergies; respiratory diseases; cardiovascular diseases; gastrointestinal diseases; diabetes; diseases in urinary tracts or internal or external genitals; diseases in the nervous system, eyes, or ears; mental disorders; tumors or cancers; and attention deficits or learning disabilities. Previous diagnoses, mean (SD), No.d Mental health score, mean (SD) Disabling pain Lifestyle behaviors Psychosocial health factors JAMA Network Open. 2023;6(1):e2249346. doi:10.1001/jamanetworkopen.2022.49346 (Reprinted) Downloaded From: https://jamanetwork.com/ by a Mexico | Access Provided by JAMA User on 01/05/2023 January 4, 2023 5/11 JAMA Network Open | Public Health Associations Between Procrastination and Health Outcomes Among University Students strategy deviates from the ones prespecified in our study protocol25 but was selected as it was deemed most appropriate for the research questions. Analyses were conducted using R, version 4.1.2 (R Group for Statistical Computing). Missing Data Outcome data were missing for 938 participants not responding at the 9-month follow-up, and the main analyses were performed as complete-case analyses (n = 2587). Prebaseline characteristics stratified by missingness at the 9-month follow-up are presented in eTable 2 in Supplement 1. We had complete data on the exposure and all covariates, except for the sleep quality variable. The Pittsburgh Sleep Quality Index (PSQI) had missing data on 3 items for sleep disturbances for 9% (n = 225) of the respondents in the analytic sample due to a technical error at the beginning of data collection. These missing data were handled by imputing the person-mean of the items for sleep disturbances. Sensitivity Analyses First, we computed the E-value33,34 that assesses how strongly unmeasured and residual confounding would need to be associated with the exposure and the outcomes on the RR scale to reduce the point estimates to the null. When the 95% CIs did not include the null, we also computed the E-value of the 95% CI bound closest to the null, to assess the strength of unmeasured and residual confounding needed to shift the 95% CI to include the null. Second, we calculated the pointbiserial correlation between procrastination at baseline and missingness at follow-up to investigate the possibility of selection bias in relation to the internal validity. No association between the exposure and loss to follow-up indicates that selection bias cannot affect the internal validity, but only the external validity.35 Third, we conducted analyses controlling for prior levels of procrastination, as has been suggested for outcome-wide studies.29 These analyses had to be performed with a 6-month follow-up because we did not have data on procrastination at prebaseline (eMethods 2 and eTable 3 in Supplement 1). Fourth, the robustness of our results to the personmean imputation of values on the PSQI was assessed by performing multiple imputation for the 3 missing items (eMethods 3 in Supplement 1). Results At prebaseline, the study included 3525 participants (2229 women [63%] and 1274 men (36%); mean [SD] age, 24.8 [6.2] years) (Table 1). The mean (SD) procrastination score at baseline was 12.9 (5.4). Gender and age were similar across levels of procrastination, but participants with higher levels of procrastination tended to be more likely to study technical sciences, be single, and have been born outside of Europe. All outcome variables showed higher prevalence or mean levels at prebaseline among participants with higher procrastination levels at baseline. Table 2 presents the results from the outcome regression models. At the 9-month follow-up, a 1-SD increase in procrastination was associated with higher mean symptom levels of depression (β, 0.13; 95% CI, 0.09-0.17), anxiety (β, 0.08; 95% CI, 0.04-0.12), and stress (β, 0.11; 95% CI, 0.08-0.15) as well as having disabling pain in the upper extremities (RR, 1.27; 95% CI, 1.14-1.42), poor sleep quality (RR, 1.09, 95% CI, 1.05-1.14), physical inactivity (RR, 1.07; 95% CI, 1.04-1.11), loneliness (RR, 1.07; 95% CI, 1.02-1.12), and economic difficulties (RR, 1.15, 95% CI, 1.02-1.30). The results showed no clear evidence of associations between procrastination and subsequent disabling pain in other body regions; use of tobacco, alcohol, or cannabis, breakfast skipping; or general health afer adjustment for the prebaseline covariates. For estimates with a 95% CI that excluded the null, the E-values suggested that unmeasured confounders would need to increase the risk of both procrastination and the outcomes by 35% to 86%, depending on the outcome, to move the point estimates to the null (Table 2). The point-biserial correlation between procrastination at baseline and missingness at the follow-up was 0.05. Outcome JAMA Network Open. 2023;6(1):e2249346. doi:10.1001/jamanetworkopen.2022.49346 (Reprinted) Downloaded From: https://jamanetwork.com/ by a Mexico | Access Provided by JAMA User on 01/05/2023 January 4, 2023 6/11 JAMA Network Open | Public Health Associations Between Procrastination and Health Outcomes Among University Students levels at prebaseline were generally somewhat higher in the group that was missing at the 9-month follow-up (eTable 2 in Supplement 1). The associations between procrastination and health outcomes 6 months later, while controlling for prior procrastination levels, were similar to the results in the main analysis (eMethods 2 and eTable 3 in Supplement 1). Using multiple imputation for the 3 missing items on the PSQI gave results identical to the main analysis when rounded to the second decimal place (eMethods 3 in Supplement 1). Discussion In this cohort of Swedish university students, higher levels of procrastination were associated with worse subsequent mental health (depression, anxiety, and stress symptom levels), having disabling pain in the upper extremities, unhealthy lifestyle behaviors (poor sleep quality and physical inactivity), and worse levels of psychosocial health factors (higher loneliness and more economic difficulties) 9 months later. We found no clear associations between procrastination and subsequent disabling pain in other body regions (neck and/or upper back, lower back, or lower extremities), other unhealthy lifestyle behaviors (alcohol, tobacco, or cannabis use and breakfast skipping), or general health. The identified associations are in the same direction, but to a lesser magnitude, than those reported in most previous studies on procrastination and health outcomes.1,2,9,10,12 There are several potential reasons for this difference in magnitude, such as the use of different scales to measure procrastination and the health outcomes. However, the arguably largest difference between this study and most previous studies is that we controlled for an extensive set of potential confounders. To our knowledge, this is the first study of procrastination and health outcomes to adjust for prior levels of the outcomes. As shown in eTable 1 in Supplement 1, when controlling for prior levels of the outcome variables, the unadjusted estimates of associations between procrastination and the health outcomes corresponded more closely to those of some previous studies.2,9,10 By adjusting for prebaseline levels of the outcome variables, we reduced the risk of reverse causality.30 Still, interpreting these association as causal effects requires the assumptions of no unmeasured or Table 2. Procrastination and Subsequent Health Outcomesa E-value Outcome β or RR (95% CI) PE LCL Depression symptoms 0.13 (0.09-0.17) 1.57 1.45 Anxiety symptoms 0.08 (0.04-0.12) 1.41 1.27 Stress symptoms 0.11 (0.08-0.15) 1.53 1.41 Neck and/or upper back 1.09 (0.96-1.24) 1.41 NA Lower back 1.03 (0.90-1.18) 1.22 NA Upper extremities 1.27 (1.14-1.42) 1.86 1.53 Lower extremities 1.10 (0.99 to 1.23) 1.44 NA Poor sleep quality 1.09 (1.05-1.14) 1.41 1.27 Physical inactivity 1.07 (1.04-1.11) 1.35 1.24 Daily alcohol use 1.05 (0.71-1.56) 1.29 NA Weekly tobacco use 0.96 (0.89-1.04) 1.24 NA Monthly cannabis use 1.21 (0.91-1.62) 1.71 NA Breakfast skipping 1.03 (0.97-1.09) 1.19 NA Mental health, β (95% CI) Disabling pain, RR (95% CI) Lifestyle behaviors, RR (95% CI) Abbreviations: LCL, lower confidence limit; NA, not applicable; PE, point estimate; RR, relative risk. a Psychosocial health factors, RR (95% CI) Loneliness 1.07 (1.02-1.12) 1.35 1.17 Economic difficulties 1.15 (1.02-1.30) 1.57 1.17 Poor general health 1.14 (0.97-1.34) 1.54 NA JAMA Network Open. 2023;6(1):e2249346. doi:10.1001/jamanetworkopen.2022.49346 (Reprinted) Downloaded From: https://jamanetwork.com/ by a Mexico | Access Provided by JAMA User on 01/05/2023 All models were adjusted for the set of prebaseline covariates described, including all outcomes prebaseline. Procrastination and all continuous outcomes were standardized (mean = 0 and SD = 1), and β is the standardized effect size. January 4, 2023 7/11 JAMA Network Open | Public Health Associations Between Procrastination and Health Outcomes Among University Students residual confounding, selection bias, or other biases affecting the associations,36 assumptions that are unlikely to be fully met in the present study. We do believe, however, that our results may correspond more closely to the consequences that interventions targeting procrastination would have for different health outcomes, than those of earlier cross-sectional studies. Our estimates indicate that the associations between procrastination and subsequent health outcomes are weak. For instance, a 1-SD increase in procrastination was associated with a mean increase in subsequent depression symptoms of only 0.13 SDs, and many of the associations were weaker than this. The follow-up time of 9 months represents 1 academic year and was chosen because we believe this is sufficient induction time for procrastination to lead to health problems. It is possible, however, that these estimates would be stronger for a longer follow-up because the potential negative associations of procrastination with health outcomes could accumulate over time. Still, even though the associations are not very strong, it seems that procrastination could have associations with many different aspects of health, including mental health, physical pain, lifestyle behaviors, and psychosocial health factors. Thus, although it seems that intervening on procrastination is unlikely to produce large associations with any specific health outcome, it could possibly produce small associations with a diverse set of different health outcomes. Limitations This study has some limitations. The E-value analysis suggests that unmeasured and residual confounding (from, for instance, neuroticism, conscientiousness, or genetic factors) could potentially explain away the observed associations. This potential unmeasured or residual confounding would, however, need to be moderately associated with procrastination and the outcomes, independent of all measured covariates29 (ie, associated with procrastination and the outcomes even after adjusting for all covariates). Given the large number of confounders adjusted for in these analyses, it is likely that a substantial proportion of any unmeasured confounding is already accounted for in our analyses. Controlling for prior procrastination levels gave results similar to those in the main analysis, limiting the risk of reverse causality and unmeasured confounding29 (eMethods 2 and eTable 3 in Supplement 1). We also have the risk of misclassification of exposure and outcomes, which is probably not an issue for the procrastination measure given that the PPS showed excellent reliability. The outcomes, however, differ somewhat in their psychometric properties, and misclassification may have attenuated the observed associations for some of the outcomes. We found that procrastination at baseline had a near-null association with loss to follow-up, so it is unlikely that the internal validity of observed associations is subject to selection bias.35 There were, however, small differences in prebaseline characteristics, especially prior outcome levels, between responders and nonresponders, which could affect external validity (eTable 2 in Supplement 1). Furthermore, the sample is not fully representative of the overall Swedish student population (for instance, we have more medical and health and technical students than average). Thus, it is uncertain whether our estimates are generalizable to Swedish students overall or to other populations. Furthermore, our measures were collected during the COVID-19 pandemic, which could affect generalizability to other time periods. Conclusions This cohort study of Swedish university students suggests that procrastination is associated with subsequent mental health problems, disabling pain, unhealthy lifestyle behaviors, and worse psychosocial health factors. Considering that procrastination is prevalent among university students, these findings may be of importance to enhace the understanding of students’ health. JAMA Network Open. 2023;6(1):e2249346. doi:10.1001/jamanetworkopen.2022.49346 (Reprinted) Downloaded From: https://jamanetwork.com/ by a Mexico | Access Provided by JAMA User on 01/05/2023 January 4, 2023 8/11 JAMA Network Open | Public Health Associations Between Procrastination and Health Outcomes Among University Students ARTICLE INFORMATION Accepted for Publication: November 13, 2022. Published: January 4, 2023. doi:10.1001/jamanetworkopen.2022.49346 Open Access: This is an open access article distributed under the terms of the CC-BY License. © 2023 Johansson F et al. JAMA Network Open. Corresponding Author: Fred Johansson, MA, Sophiahemmet Högskola, PO Box 5605, 114 86 Stockholm, Sweden ([email protected]). Author Affiliations: Department of Health Promotion Science, Sophiahemmet University, Stockholm, Sweden (Johansson, Edlund, Sundberg, Onell, Skillgate); Department of Psychology, Uppsala University, Uppsala, Sweden (Rozental); Department of Clinical Neuroscience, Karolinska Institutet, Stockholm, Sweden (Rozental, Rudman); Unit of Intervention and Implementation Research for Worker Health, Institute of Environmental Medicine, Karolinska Institutet, Stockholm, Sweden (Edlund, Skillgate); Institute for Disability and Rehabilitation Research and Faculty of Health Sciences, Ontario Tech University, Oshawa, Ontario, Canada (Côté); Department of Caring Sciences, Dalarna University, Falun, Sweden (Rudman). Author Contributions: Mr Johansson had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: Johansson, Edlund, Côté, Rudman, Skillgate. Acquisition, analysis, or interpretation of data: Johansson, Rozental, Côté, Sundberg, Onell, Skillgate. Drafting of the manuscript: Johansson, Edlund, Côté, Sundberg, Skillgate. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: Johansson, Côté. Obtained funding: Rudman, Skillgate. Administrative, technical, or material support: Edlund, Sundberg, Onell. Supervision: Rozental, Edlund, Côté, Sundberg, Rudman, Skillgate. Conflict of Interest Disclosures: Mr Johansson and Drs Edlund, Sundberg, and Skillgate reported receiving grants from the Swedish Research Council for Health, Working Life and Welfare (FORTE) during the conduct of the study. No other disclosures were reported. Funding/Support: This research project was funded by grant number FORTE2018-00402 from the Swedish Research Council for Health, Working Life and Welfare (FORTE). The Sustainable University Life study also received financial support from the Public Health Agency of Sweden. Role of the Funder/Sponsor: The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. Data Sharing Statement: See Supplement 2. Additional Contributions: We would also like to express our appreciation to ACTIC (health club chain), the Tim Bergling Foundation, and all the participating students for their contribution to the Sustainable University Life study. REFERENCES 1. Steel P. The nature of procrastination: a meta-analytic and theoretical review of quintessential self-regulatory failure. Psychol Bull. 2007;133(1):65-94. doi:10.1037/0033-2909.133.1.65 2. Beutel ME, Klein EM, Aufenanger S, et al. Procrastination, distress and life satisfaction across the age range—a German representative community study. PLoS One. 2016;11(2):e0148054. doi:10.1371/journal.pone.0148054 3. Steel P, Ferrari J. Sex, education and procrastination: an epidemiological study of procrastinators’ characteristics from a global sample. Eur J Pers. 2013;27(1):51-58. doi:10.1002/per.1851 4. Day V, Mensink D, O’Sullivan M. Patterns of academic procrastination. J Coll Read Learn. 2000;30(2):120-134. doi:10.1080/10790195.2000.10850090 5. Gustavson DE, Miyake A, Hewitt JK, Friedman NP. Genetic relations among procrastination, impulsivity, and goal-management ability: implications for the evolutionary origin of procrastination. Psychol Sci. 2014;25(6): 1178-1188. doi:10.1177/0956797614526260 6. Loehlin JC, Martin NG. The genetic correlation between procrastination and impulsivity. Twin Res Hum Genet. 2014;17(6):512-515. doi:10.1017/thg.2014.60 7. Steel P, Svartdal F, Thundiyil T, Brothen T. Examining procrastination across multiple goal stages: a longitudinal study of temporal motivation theory. Front Psychol. 2018;9:327. doi:10.3389/fpsyg.2018.00327 JAMA Network Open. 2023;6(1):e2249346. doi:10.1001/jamanetworkopen.2022.49346 (Reprinted) Downloaded From: https://jamanetwork.com/ by a Mexico | Access Provided by JAMA User on 01/05/2023 January 4, 2023 9/11 JAMA Network Open | Public Health Associations Between Procrastination and Health Outcomes Among University Students 8. Kim KR, Seo EH. The relationship between procrastination and academic performance: a meta-analysis. Pers Individ Dif. 2015;82:26-33. doi:10.1016/j.paid.2015.02.038 9. Fernie BA, Bharucha Z, Nikčević AV, Marino C, Spada MM. A metacognitive model of procrastination. J Affect Disord. 2017;210:196-203. doi:10.1016/j.jad.2016.12.042 10. Sirois FM. Procrastination and stress: exploring the role of self-compassion. Self Ident. 2014;13(2):128-145. doi:10. 1080/15298868.2013.763404 11. Rozental A, Forsström D, Hussoon A, Klingsieck KB. Procrastination among university students: differentiating severe cases in need of support from less severe cases. Front Psychol. 2022;13:783570. doi:10.3389/fpsyg.2022. 783570 12. Sirois FM. “I’ll look after my health, later”: a replication and extension of the procrastination–health model with community-dwelling adults. Pers Individ Dif. 2007;43(1):15-26. doi:10.1016/j.paid.2006.11.003 13. Sirois FM. Is procrastination a vulnerability factor for hypertension and cardiovascular disease? testing an extension of the procrastination-health model. J Behav Med. 2015;38(3):578-589. doi:10.1007/s10865-0159629-2 14. Kroese FM, Evers C, Adriaanse MA, de Ridder DTD. Bedtime procrastination: a self-regulation perspective on sleep insufficiency in the general population. J Health Psychol. 2016;21(5):853-862. doi:10.1177/ 1359105314540014 15. Kroese FM, de Ridder DT. Health behaviour procrastination: a novel reasoned route towards self-regulatory failure. Health Psychol Rev. 2016;10(3):313-325. doi:10.1080/17437199.2015.1116019 16. Svartdal F, Dahl TI, Gamst-Klaussen T, Koppenborg M, Klingsieck KB. How study environments foster academic procrastination: overview and recommendations. Front Psychol. 2020;11:540910. doi:10.3389/fpsyg.2020. 540910 17. Sirois F, Melia-Gordon M, Pychyl T. “I’ll look after my health, later”: an investigation of procrastination and health. Pers Individ Dif. 2003;35:1167-1184. doi:10.1016/S0191-8869(02)00326-4 18. Stead R, Shanahan MJ, Neufeld RWJ. “I’ll go to therapy, eventually”: procrastination, stress and mental health. Pers Individ Dif. 2010;49(3):175-180. doi:10.1016/j.paid.2010.03.028 19. Rozental A, Bennett S, Forsström D, et al. Targeting procrastination using psychological treatments: a systematic review and meta-analysis. Front Psychol. 2018;9:1588. doi:10.3389/fpsyg.2018.01588 20. Cui G, Yin Y, Li S, et al. Longitudinal relationships among problematic mobile phone use, bedtime procrastination, sleep quality and depressive symptoms in Chinese college students: a cross-lagged panel analysis. BMC Psychiatry. 2021;21(1):449. doi:10.1186/s12888-021-03451-4 21. Rice KG, Richardson CM, Clark D. Perfectionism, procrastination, and psychological distress. J Couns Psychol. 2012;59(2):288-302. doi:10.1037/a0026643 22. Sternberg N, Luria R, Chandhok S, Vickers B, Kross E, Sheppes G. When Facebook and finals collide— procrastinatory social media usage predicts enhanced anxiety. Comput Human Behav. 2020;109:106358. doi:10. 1016/j.chb.2020.106358 23. Tice DM, Baumeister RF. Longitudinal study of procrastination, performance, stress, and health: the costs and benefits of dawdling. Psychological Sci. 1997;8:454-458. doi:10.1111/j.1467-9280.1997.tb00460.x 24. VanderWeele TJ. Can sophisticated study designs with regression analyses of observational data provide causal inferences? JAMA Psychiatry. 2021;78(3):244-246. doi:10.1001/jamapsychiatry.2020.2588 25. Edlund K, Sundberg T, Johansson F, et al. Sustainable UNiversity Life (SUN) study: protocol for a prospective cohort study of modifiable risk and prognostic factors for mental health problems and musculoskeletal pain among university students. BMJ Open. 2022;12(4):e056489. doi:10.1136/bmjopen-2021-056489 26. Rozental A, Forsell E, Svensson A, Forsström D, Andersson G, Carlbring P. Psychometric evaluation of the Swedish version of the Pure Procrastination Scale, the Irrational Procrastination Scale, and the Susceptibility to Temptation Scale in a clinical population. BMC Psychol. 2014;2(1):54. doi:10.1186/s40359-014-0054-z 27. Svartdal F, Steel P. Irrational delay revisited: examining five procrastination scales in a global sample. Front Psychol. 2017;8:1927. doi:10.3389/fpsyg.2017.01927 28. VanderWeele TJ. Principles of confounder selection. Eur J Epidemiol. 2019;34(3):211-219. doi:10.1007/s10654019-00494-6 29. VanderWeele TJ, Mathur MB, Chen Y. Outcome-wide longitudinal designs for causal inference: a new template for empirical studies. Stat Sci. 2020;35(3):437-466, 430. doi:10.1214/19-STS728 30. VanderWeele TJ, Jackson JW, Li S. Causal inference and longitudinal data: a case study of religion and mental health. Soc Psychiatry Psychiatr Epidemiol. 2016;51(11):1457-1466. doi:10.1007/s00127-016-1281-9 JAMA Network Open. 2023;6(1):e2249346. doi:10.1001/jamanetworkopen.2022.49346 (Reprinted) Downloaded From: https://jamanetwork.com/ by a Mexico | Access Provided by JAMA User on 01/05/2023 January 4, 2023 10/11 JAMA Network Open | Public Health Associations Between Procrastination and Health Outcomes Among University Students 31. Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702-706. doi:10.1093/aje/kwh090 32. Gelman A, Hill J, Vehtari A. Regression and Other Stories. Cambridge University Press; 2020. doi:10.1017/ 9781139161879 33. VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167(4):268-274. doi:10.7326/M16-2607 34. Haneuse S, VanderWeele TJ, Arterburn D. Using the E-value to assess the potential effect of unmeasured confounding in observational studies. JAMA. 2019;321(6):602-603. doi:10.1001/jama.2018.21554 35. Hernán MA. Invited commentary: selection bias without colliders. Am J Epidemiol. 2017;185(11):1048-1050. doi:10.1093/aje/kwx077 36. Hernan MA, Robins JM. Causal Inference: What If. Chapman & Hall/CRC; 2020. SUPPLEMENT 1. eMethods 1. Assessment of the Outcome and Confounder Variables eTable 1. Comparisons of Estimates Under Different Adjustments eTable 2. Characteristics of Participants at Pre-baseline Stratified by Missingness at the Nine-Month Follow-up eMethods 2. Sensitivity Analysis Controlling for Prior Levels of Procrastination eTable 3. Procrastination (T3) and Subsequent Health Outcomes Six Months Later (T5), Adjusted for Prior Levels of Procrastination (T2) eMethods 3. Sensitivity Analysis for the Imputation of the Three Missing Items on the Pittsburgh Sleep Quality Inventory eReferences SUPPLEMENT 2. Data Sharing Statement JAMA Network Open. 2023;6(1):e2249346. doi:10.1001/jamanetworkopen.2022.49346 (Reprinted) Downloaded From: https://jamanetwork.com/ by a Mexico | Access Provided by JAMA User on 01/05/2023 January 4, 2023 11/11
![[William Knaus] End Procrastination Now! - Get it Done with a Proven Psychological Approach](http://s2.studylib.es/store/data/009318659_1-7cca290345eea50977cc7a53b1f40266-300x300.png)