- Ninguna Categoria
Wood Smoke Pollution & Respiratory Health: A Questionnaire Study
Anuncio
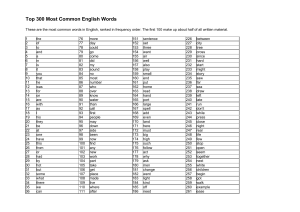
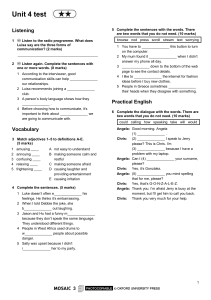
PEDIATRIC ASTHMA, ALLERGY & IMMUNOLOGY Volume 4, Number 3, 1990 Mary Ann Liebert, Inc., Publishers A Questionnaire Study of Respiratory Health in Areas of High and Low Ambient Wood Smoke Pollution KATHERINE G. BROWNING, M.S., JANE Q. KOENIG, Ph.D., HARVEY CHECKOWAY, Ph.D., TIMOTHY V. LARSON, Ph.D., and WILLIAM E. PIERSON, M.D. ABSTRACT A cross-sectional questionnaire study was conducted to determine whether there were differences in the prevalence of respiratory symptoms between residents of high and of low wood smoke pollution areas. Six hundred questionnaires were mailed to households in each area asking about respiratory symptoms, such as cold, cough, and congestion and wheezing. The response rate was 57% (325 households) in the high wood smoke area and 51% (257 households) in the low wood smoke area. There were no statistically significant differences between symptoms in the two areas when all age groups were combined for analysis. However, there was a trend toward more symptoms in children aged 1-5 years in the high wood smoke area both in an initial questionnaire, which asked about history of symptoms, and in the follow-up questionnaires, which asked about symptoms during the preceding 2 weeks. In particular, for congestion and wheezing, the percentage reported for the initial questionnaire in the high wood smoke area was 46.4 vs 28.6 in the low wood smoke area. This difference was 29.4 vs 0.0 during the second follow-up period. This pattern was not seen in the other age groups. It is concluded that this study supports the work of others who have suggested that wood smoke air pollution aggravates symptoms of respiratory disease in preschool children, despite an apparent absence of effect at older ages. INTRODUCTION energy costs, the number of Americans using woodburning devices for home has increased dramatically over the past few years. Intense particulate matter pollution has resulted in some communities where substantial amounts of residential wood combustion occur. Health concerns about wood smoke pollution have prompted citizens in several states to seek regulation of Because heating of increasing wood-burning devices/" on The use of wood stoves produces both indoor and outdoor pollution. Two recent studies'2·3' have focused the relationship between respiratory illness in children and the use of wood-burning stoves in the home. Departments of Environmental Health, Epidemiology, Pediatrics, and Civil Engineering, University of Washington, Seattle, Washington. 183 BROWNING ET AL. However, neither indoor nor outdoor air pollution from wood smoke was measured in these studies. To date, no studies have been published that have sought to evaluate the effect of community wood smoke pollution on the prevalence of respiratory illness. The object of this study was to evaluate the relationship between ambient wood smoke pollution and symptoms of respiratory illness. The approach used was a cross-sectional questionnaire study conducted during the 1987-1988 winter heating season in Seattle, Washington. Ambient air monitoring data exist for 1986-1987 and for the winter of the study. Prevalence of respiratory symptoms was compared between adults and children living in neighborhoods with high measured levels of ambient wood smoke pollution and adults and children living in neighborhoods with lower measured levels of such pollution. A pattern of increased respiratory symptoms was seen in young children who lived in the high wood smoke area. METHODS Initial and follow-up questionnaires were sent to 600 households in each of two study neighborhoods in a developed residential suburb of Seattle. Selection of neighborhoods was based on analysis of ambient air monitoring data obtained during the 1986-1987 heating season. One of the investigators (TVL) provided maps that correlated location with ambient wood smoke concentrations. The area selected as having high wood smoke levels was characterized by lower elevation and the presence of valleys and creek drainages. The area selected as having lower wood smoke levels was characterized by higher elevation and the presence of ridges and hills. Identification of households within the selected areas was accomplished by use of current year reverse directories.(4) Streets selected were classified by the directories as high or medium-high income areas. Multiple family dwellings (apartment houses and addresses with letter or unit number suffixes) and businesses were excluded. An initial mailed questionnaire containing 38 questions and a follow-up questionnaire with 6 questions were developed from the standardized respiratory questionnaire of the American Thoracic Society's Epidemiology Standardization Project.(5) The initial questionnaire included questions on personal character¬ istics, such as age, gender, and occupation. Other information collected included primary and secondary heat sources, frequency of wood stove use, cigarette smoking history, and history of asthma, hay fever, bronchitis, and emphysema. Questions regarding respiratory symptoms included questions about symptoms of a mild, moderate, or severe nature. Questions about mild symptoms asked about the presence of cough or congestion with colds. Questions about moderate symptoms asked about attacks of respiratory illness each year, occasional wheezing with colds, or other episodes of wheezing. Questions about severe symptoms asked about coughing on most days or nights, congestion apart from colds, and wheezing most days or nights. Questions also were asked about school or work absences due to respiratory illness and doctor visits or medication use due to respiratory illness. The follow-up questionnaire, which was sent at two different periods, included questions pertaining only to respiratory symptoms: presence of cough, cold, congestion and wheezing, absence from school or work due to respiratory illness, and doctor visits or medication use for respiratory illness. The respondents were asked if these symptoms or events had occurred during the preceding 2 weeks. Instructions specified that the person filling out the questionnaire provide information about himself or herself (adult) and one child closest to the age of 10 if there were children in the household. The initial questionnaire was mailed early in December 1987. Those households that returned the initial questionnaires and signed approved consent forms were sent the first follow-up questionnaire during the first week of January 1988. The second follow-up questionnaire was sent to the same households during the first week of February. Symptom prevalence was compared between high and low wood smoke areas by means of calculations of prevalence ratios and associated 95% confidence intervals.(6) Ambient air measurements were taken in both areas during the study period, using Harvard samplers for particulate matter less than 10 µ concentration (PM10) and 1590 series nephelometers for light scattering. Light scattering values are highly correlated (r 0.97) with PM10 at these sites during the heating season. = 184 RESPIRATORY HEALTH AND WOOD SMOKE AIR POLLUTION RESULTS Study subjects Response rates for the initial questionnaire were 57% (325 households, including 455 individuals) in the high wood smoke area and 51 % (257 households, including 368 individuals) in the low wood smoke area. The percent of households that responded to the initial and both follow-up questionnaires was 37% in the high wood smoke group and 34% in the low wood smoke group. Not all households responded to both the first and second follow-up questionnaires, however. The response rate for the first follow-up questionnaire was 64% in the high wood smoke group and 38% in the low wood smoke group. For the second follow-up, the rates were 54% and 69%, respectively. The age distributions were similar in both areas. Approximately 18% more females than males participated in the study. The job classifications were similar for both groups. Forced air heating systems predominated, with more oil than gas users in the high wood smoke area (35 vs 18%) and more gas than oil users (49 vs 26%) in the low wood smoke area. Households using wood stoves were very similar, 14% in the high and 13% in the low wood smoke area. There was a similar prevalence of cigarette smoking in each area, 9.3% in the high and 13% in the low wood smoke area. No association was seen between smoking and symptoms in either area (probably due to the low prevalence rate of smoking). History of chronic respiratory disease The prevalence of individuals in each area reporting a history of respiratory disease was similar in the two except among children aged 1-5 years. Among children 1-5 years old, the most notable difference between groups was for history of bronchitis; 14.3% of children in the high wood smoke area were reported to have bronchitis compared to 0.0% in the low wood smoke area. Among children 6-14 years old, more children in the low wood smoke area had histories of asthma (15.5%) and bronchitis (5.2%) than did children in the high wood smoke area (8.2% and 1.6%, respectively). Adults in the age 15-64 years category were very similar in their history of respiratory disease. Adults in the age 65 and older category in the low wood smoke area had a higher prevalence of emphysema (6.1%) and bronchitis (14.6%) than did adults in the high wood smoke area (1.6% and 11.1%, respectively). areas 24 hr average Light Scattering Values (October, 1987 March, 1988) - - E 2 w » 10 8 6 4 2 0 High Wood S noke An a Wood S noke Art a ^ * to · - S· io 6 4 0 - 'QjJ/vMJ/^U^^_ o to · M m evj cm w DATE FIG. 1. Light scattering values (24 hour means) vs time in high and low wood smoke areas. Light scattering in this study is a surrogate for PM10 185 BROWNING ET AL. Atmospheric monitoring Figure 1 shows light scattering (bsp) data for the high and low wood smoke areas from October 1987 through March 13, 1988. The high wood smoke area had higher bsp levels in all study periods, for both 24 hour average and peak values, than did the low wood smoke area. The equivalent 24 hour average PM10 concentration on a given day followed a similar pattern in both areas but was consistently lower in the low wood smoke area (p < 0.001). In the low wood smoke area for November and December 1987 and January 1988 the monthly PM10 averages were 36,41, and 22 µg/m3, respectively. For the high wood smoke area, the monthly average PM10 values were 72, 53, and 41 µg/m3, respectively. The highest 24-hour PM10 values by month in the low wood smoke area were 56, 59, and 29 µg/m3; in the high wood smoke area, the highest 24-hour values by month were 100, 53, and 127 µg/m3. Chemical analysis of selected filter samples at the high wood smoke site indicated that on average 70% of the PM10 was wood smoke, and the remainder was primarily due to diesel exhaust.7 Prevalence of symptoms The initial questionnaire was completed from 11/20/87 to 12/15/87, the first follow-up period was from 12/20/87 to 1/10/88, and the second follow-up was from 1/15/88 to 2/7/88. The age-stratified prevalence of respiratory symptoms reported and the ratios of the prevalence in the high vs low wood smoke areas during the initial study period are given in Table 1. The most notable differences between areas were seen in the children ages 1-5. The differences remained consistent in the mild, moderate, and severe symptom category. None of the differences was statistically significant at the 0.05 level, since the confidence intervals overlapped the null value of 1.0. However, because of the exploratory nature of this study and the relatively small sample size, the intent was to look for patterns of response. As shown in Table 1, in the age 1-5 years category, the largest differences between groups were reported for usually having congestion with cold (46.4% in the high wood smoke area and 28.6% in the low wood smoke area, ratio 1.62), having occasional wheezing without a cold (14.3% in the high wood smoke area and 7.1% in the low wood smoke area, ratio 2.01), and usually without cold in the wood smoke and 0.0% in the low wood smoke area). a area having a cough (7.1% high Exclusion of children with asthma did not alter these differences materially. In adults age 65 and older, contrary to our expectation, the trend was in the opposite direction. Respondents in the low wood smoke area reported a higher prevalence of symptoms in each category. It was noted earlier that the prevalence rates of history of bronchitis and emphysema were higher in the low wood smoke area. Eliminating the emphysema cases from the analysis decreased the difference between areas but did not alter the trend. There were no consistent patterns in the other two age groups, 6-14 and 15-65 years of age (Ta¬ ble 2). None of the differences reported for the follow-up periods for children was statistically significant at the 0.05 level (Table 3). There was a trend among children ages 1-5 years in the high wood smoke area to have higher prevalences of colds (66.7 vs 50%) and congestion and wheezing (23.8 vs 16.7%) in the first follow-up period. The percentages for the second follow-up period were 41.2 vs 20.0% for cold, 41.2 vs 22.2% for cough, and 29.4 vs 0.0% for congestion and wheezing and absence due to respiratory disease (29.4 = = = = vs 10.0). Although this study focused on outdoor air pollution from wood stoves, data regarding indoor use of wood stoves also were collected. In the high wood smoke area, households with children ages 1-5 years reported that 28.8% used the wood stove from 3 days a week to daily. In the low wood smoke area, only 7.1% of the households with children ages 1-5 years reported wood stove use of that frequency. However, except for coughing without a cold, there was no tendency toward more symptoms in children from homes using wood stoves, as shown in Table 4. DISCUSSION This study has investigated the occurrence of symptoms of respiratory illness in residents of areas with relatively high and low measured levels of ambient wood smoke pollution. The findings suggest that young 186 RESPIRATORY HEALTH AND WOOD SMOKE AIR POLLUTION Table 1. Prevalence of Symptoms (%) (n Mild symptoms 1. Usually coughs with cold High WS Low WS Ratioa = = (n (n = = 15-44 (n (n 63) 59) = 109) 70) 45-64 (n (n = = 86) 55) >65 (n (n = = 60) 45) 49.7 45.5 1.09 49.2 40.0 46.2 46.2 0.87 (0.41,2.46) (0.59, 1.60) (0.78, 1.53) (0.73, 1.55) (0.53, 1.43) Low WS Ratio 46.4 28.6 1.62 39.7 37.3 1.06 47.8 51.6 0.93 52.9 47.2 1.12 31.6 41.5 0.76 (95% CI) (0.53, 4.96) (0.60, 1.89) (0.66, 1.29) (0.77, 1.62) (0.44, 1.31) Low WS Ratio 42.9 42.9 1.00 33.3 39.7 0.84 36.6 38.5 0.95 28.3 31.1 0.91 17.5 33.3 0.53 (95% CI) (0.38, 2.65) (0.47, 1.52) (0.65, 1.40) (0.56, 1.47) (0.27, 1.31) 10.0 18.5 0.54 14.8 11.0 1.35 13.6 14.0 0.98 10.3 14.3 0.72 (0.20, 1.48) (0.67, 2.71) (0.46, 2.05) (0.26, 1.99) 40.7 28.6 1.42 31.7 33.9 0.94 30.7 27.3 1.12 29.4 23.8 19.5 22.2 0.88 (0.46, 4.46) (0.50, 1.74) (0.72, 1.75) (0.74, 2.06) (0.42, 1.82) 14.1 11.7 1.21 11.8 14.3 0.83 15.3 17.5 0.87 (0.62, 2.35) (0.40, 1.71) (0.38, 2.02) 10.6 13.8 0.77 9.2 18.1 0.51 11.4 20.0 0.57 (0.16,3.19) (0.39, 1.51) (0.24, 1.06) (0.24, 1.33) 12.7 11.9 1.06 12.3 8.9 1.38 10.8 19.0 0.57 11.5 28.8 0.40 (0.39, 2.95) (0.66, 2.86) (0.28, 1.14) (0.18,0.89) Moderate symptoms 1. History of asthma High WS Low WS Ratio 7.1 0 (95% CI) — 2. Occasional wheeze with cold High WS Low WS Ratio (95% CI) Severe symptoms 1. Occasional wheeze without cold High WS Low WS Ratio (95% CD Low WS Ratio 14.3 7.1 2.01 9.5 8.5 1.12 — without cold (95% CI) — — Ratio of prevalence in high 1.24 - 7.1 0 Low WS Ratio (0.34, 3.68) 4.8 6.8 0.71 3.6 0 (95% CI) Usually coughs High WS 1.06 - (0.22,17.85) Usually congested without cold High WS a = 49.2 50.8 0.97 Yearly coughs and congestion High WS 3. 28) 14) 50.0 50.0 1.00 (95% CI)b Usually congested with cold High WS 2. 6-14 1-5 (n Low 3. Questionnaire Age group (years) Symptom severity and exposure classification High 2. Respiratory Illness During Initial Study Period of wood smoke to low wood smoke b95% confidence interval for prevalence ratio. 187 areas. BROWNING ET AL. II II <u -* oo in o\ r> ?5ïSf -S r- tí- es oo o ^D es r~ oo —« ö ö co ö ö *-e — es On" ö '-' -h O 00 ·* vD o m es ^o co — p no cn Ö Ö Ö es es no o O w <* es — -h es* es en es oo —¡ — co On es — es <n oo no es no r* ö Ö ^ Ö es es * es in in in Ö co oo -w -h -- Ö O m "î ©S Q O 2 u Tt en iri su —- en ^- —- Ö oo es es es w en en — ö O o Tt r- no co co » vq es Tt Tf co -H O Vi r^ Tf —î r-" co ON ON on so es w s H C« 3 •<J- > —I es 00 ej\*¬ es m es ejv ^h o r> ri oo oo -h ö Ö B 3 oo \o o *n ejv os C f- -g I (N p r> en v-i ö Ö — Ö «ri ö Ö *—' CO t'odd es co — es Tf w Tf CO Tf ö —; ö es OO (S ^ ej\ t vo r— en en es" VO Ö *-* p O in r- es r*— eo ~h" co es no es on co m co co oo (N Tr m -^ es 6 Ò w -h t'^odd ¿1 S \o o B Mil Is- ^û *0 rN tN d d d s-"' —' (N E* O g co » On es — O es es © ö 5 »® d u u-, * —> —, —, Il 9> w NO cO II «S J= - r^ ; d d —; —; ON NO p no in >n m MM ¬ oo -rt —< r^ O iri ò Ò ^ oo es es o o o eu S > ^> «i i^ o *o ~*< 00 H < ~^ · trî ( *-< ( * ·* MM — \¿ O es ejv o Ö —¡ —' Ö —i ^ O I Cu e o o g. "S t/5 r/J I int IIs·3 j= > ß Er2 « .9 s£ j= > g U e .9 * S ? -S S -S * I 3= J 188 u j= cd .-h „» u P « io ¡ -a· * > O — .9 î£ rai.' H*H ^_- RESPIRATORY HEALTH AND WOOD SMOKE AIR POLLUTION Table 3. Prevalence of Acute Respiratory Symptoms (During Previous Week) Study Period in Children by Study period First follow-up Initial questionnaire Symptoms and Age 1High (n 28) exposure = classification Low (n = 14) Age 6-14 High (n 63) Age 1-5 High (n 21) = Low (n = Age 6-14 High (n 35) = Low (n 59) = Second follow-up = 5) Low (n = 20) Age 1-5 High (n 17) = Low (n = 9) Age 6-14 29) Low (n = 34) High (n = Cold High WS Low WS Ratio3 32.1 (95%CI)b Cough High WS 42.9 0.75 24.2 32.2 0.75 66.7 50.0 1.33 36.1 47.6 0.76 41.2 20.0 2.06 58.6 47.2 1.24 (0.27,2.10) (0.38, .48) (0.39, 4.58) (0.33, 1.72) (0.43, 9.84) (0.64, 2.42) 25.0 Low WS Ratio 35.7 0.70 17.5 39.0 0.45 57.1 60.0 0.95 (95% CI) 25.0 33.3 0.75 41.2 22.2 1.85 (0.22, 2.20) 27.6 41.7 0.66 (0.22, 0.92) (0.27, 3.33) (0.28, 2.01) (0.39, 8.85) (0.28, .56) 23.8 16.7 1.43 8.3 14.3 0.58 29.4 0 17.2 13.9 1.24 (0.17, 12.14) (0.12, 2.89) 4.8 14.6 0.32 33.3 33.3 1.00 19.4 40.0 0.49 29.4 10.0 2.94 20.7 33.3 .62 (0.06, 1.57) (0.27, 4.77) (0.18, 1.34) (0.35, 25.04) (0.23, 1.65) Congestion wheezing High WS Low WS Ratio — — (95% CI) Absence due High WS Low WS Ratio — to respiratory disease 0 0 (95% CI) — aRatio of prevalence in high wood smoke to low wood smoke 95% confidence interval for prevalence ratio. Table 4. Moderate symptoms with cold 44.4 Frequent use" Infrequent/no useb 50.0 Ratio0 95% CId 0.89 0.40-2.00 Usually congested with cold 55.6 Frequent use Infrequent/no use 37.5 Ratio 1.48 95% CI 0.71-3.09 Yearly coughs and congestion 33.3 Frequent use Infrequent/no use 43.8 Ratio 0.76 95% CI 0.28-2.08 a Frequent use = 3 bInfrequent/no use History of asthma Frequent use Infrequent/no use Ratio 95% CI 0 3.1 — Severe symptoms Occasional wheeze without cold 0 Frequent use Infrequent/no use 15.6 Ratio 95% CI Usually congested without cold 0 Frequent use Infrequent/no use 3.1 Ratio 95% CI Usually coughs without cold 11.1 Frequent use Infrequent/no use 3.1 Ratio 3.56 95% CI 0.25-51.41 — Occasional wheeze with cold 33.3 Frequent use Infrequent/no use 34.4 Ratio 95% CI 0.97 0.34-2.75 - — — times/ week or more, 10. less than 3 times/week, = = Ratio of prevalence by frequent to infrequent d95% confidence interval for prevalence ratio. c areas. Prevalence of Symptoms of Respiratory Illness m in Children Aged 1-5 Years Comparing Frequency of Wood Stove Usage Mild symptoms Usually coughs (0.36, 4.28) = 31. use. 189 BROWNING ET AL. children (ages 1-5) develop more symptoms of respiratory illness if they live in an area with larger amounts of wood smoke pollution. For adults over age 65, the trends were generally in the opposite direction, although increased history of chronic respiratory disease in the low wood smoke area may explain these comparisons. Ambient wood smoke pollution levels (measured as PM10 concentration and light scattering, which serves as a surrogate for PM10 in these locations) always were higher in high wood smoke areas. The monthly averages were highest in both areas during the initial and first follow-up study periods. The highest peak value for the low wood smoke area was in the first follow-up period (59 µg/m3). For the high wood smoke area, it was in the second follow-up period (127 µg/m3). Symptoms in the young children also were greatest during the second follow-up period. The results of this study are consistent with other reported research on the health effects of particulate matter. A study in Steuben ville, Ohio, found a positive correlation between decreased lung function in children and increased concentrations of total suspended particulate matter (TSP) and sulfur dioxide (S02).<8) The lung function decreases lasted for 1-2 weeks after exposure. A similar study in the Netherlands followed lung function measurements in 179 children aged 7-11 years while TSP and S02 were monitored.<9> The study found 3%-5% reductions in lung volume measurements during air pollution episodes when high concentra¬ tions of these pollutants were present. These authors reported that the lung function changes persisted for about 16 days after the period of elevated air pollution. In our study, the questionnaires reflect an exposure lag of about 2 weeks at most, but based on the other studies, the lag could have been greater in some cases. In both the Steuben ville and Netherlands studies, S02 concentrations as well as PM were elevated. Thus, determining the unique contribution of PM on the lung function decrements is difficult. In the Seattle airshed in the winter, S02 levels are very low (monthly arithmetic averages ranged from 0.004 to 0.016 ppm during 1986). Thus the only elevated air pollutant measured in our study was PM10. A recently published article also showed that rates of respiratory illness and symptoms were elevated among children living in cities with high particulate matter pollution/10' This study found, in children slightly older than in the present study (10—12 years of age), a significant association between both bronchitis and chronic cough (odds ratios 2.5 and 3.7, respectively) and particulate matter less than 15 µ in diameter. The contribution from wood smoke was not reported. The question of exposure effects resulting from ambient air pollution is a difficult one. Results obtained at fixed monitoring stations may not be truly representative of exposures throughout a geographical region/11' We sought to minimize this variability by having monitoring stations in each area, selecting areas that had overall geographical similarity and selecting households located in geographically similar subareas of each study area. Mobile monitoring also was used throughout the high wood smoke area. The relationship between ambient PM]0 concentrations and actual personal exposures has been studied by Spengler et al.( '2) They found that ambient concentrations were poorly correlated with personal exposures and that indoor concentrations of PM10 frequently were higher than outdoor concentrations. The indoor concentrations were highest in the homes of smokers. They did not specifically examine the relationships between wood stove use or ambient wood smoke pollution and indoor concentrations of PM,0. Larson et al./7) however, studied indoor-outdoor fine particle mass concentration relationships. In a building with an electric furnace, the indoor fine particle mass concentration was approximately 70% of the outdoor fine particle mass concentration. The conclusion was that particles and reactive gases penetrate buildings, and consequently even the indoor environment of homes not using wood stoves will be polluted by ambient wood smoke pollution/7' This supports our data that show no association between personal use of a wood stove and respiratory symptoms but did show a pattern of increased symptoms associated with high levels of community outdoor wood smoke that could pollute the indoor environment. A limitation of the present study is the relatively low questionnaire return rate. Mail questionnaire surveys in particular present concerns about response selectivity. Persons receiving the questionnaire have the chance to look at the entire questionnaire before making decisions about responding. People who are interested in the subject of the questionnaire may be more likely to respond/4' We did send a postcard to nonrespondents in an attempt to determine the reasons for not responding. Fifty percent of those who returned the postcard stated that they were "too busy." Demographically, the nonrespondents who returned the card were not different from respondents. The socioeconomic level in the communities involved in our study was well above average. People in upper socioeconomic strata are more likely to have better access to health care, to be able to afford 190 RESPIRATORY HEALTH AND WOOD SMOKE AIR POLLUTION housing, and may be healthier overall than those in lower socioeconomic strata. In addition, cigarette smoking is generally thought to be more prevalent among lower socioeconomic groups. In conclusion, the results of this study indicate that some differences existed in the prevalence of respiratory symptoms in high wood smoke pollution areas vs low wood smoke pollution areas. These patterns of response were most pronounced for children in the 1-5 years of age group. No such pattern of response was seen when in-home wood stove use was used as the surrogate exposure variable. Because of the small sample size and lack of personal monitoring data, the results of this study should be regarded cautiously. However, the patterns of response indicate that the health effects of wood smoke air pollution warrant further evaluation. better diet and ACKNOWLEDGMENT This study was supported by a grant from the American Lung Association of Washington. REFERENCES Covert DS, Larson TV, et al. Wood smoke: Health effects and legislation. Northwest Environ J !;4:41-45. 2. Honicky RE, Osorne JS, Akpom CA. Symptoms of respiratory illness in young children and the use of wood burning 1. Koenig JQ, for indoor heating. Pediatrics 1985;75:587-593. 3. Tuthill RW. Woodstoves, formaldehyde and respiratory disease. Am J Epidemiol 1984;120:952-955. 4. Dillman DA. Mail and telephone surveys: The total design method. New York: John Wiley & Sons, 1978. stoves 5. Ferris BG. Epidemiology 1978;118:36-47. standardization project, July 1978: Children's questionnaire. 6. Rothman KJ. Modern epidemiology. Boston: Litttle,Brown, 1986. 7. Larson TV, Kaiman D, Wang S, Nothstein G. Urban air toxics mitigation study: Phase I. Report submitted to Puget Sound Air Pollution Control Agency, September 1988. 8. 9. Am Rev Respir Dis University of Washington. Dockery DW, Ware JH, Ferris BG et al. Changes in pulmonary function in children associated with air pollution episodes. J Air Pollut Control Assoc 1982;32:937-942. Dassen W, Brunekreef B, Hoek G, et al. Decline in children's pulmonary function during an air pollution episode. J Air Pollut Control Assoc 1986;36:1223-1227. 10. Dockery DW, Speizer FÉ, Stram DO, et al. Effects of inhalable particles on respiratory health of children. Am Rev Respir Dis 1989;139:587-594. 11. Goldstein IF, Hartel D. Critical assessment of epidemiological studies in environmental factors in asthma. In: Goldsmith JR, ed. Environmental epidemiology: Epidemiological investigations of community environmental health problems. Boca Raton, FL: CRC Press, 1986, pp 101-113. 12. Spengler JD, Treitman RD, Tosteson TD, et al. Personal exposures to respirable particulates and implications for air pollution epidemiology. Environ Sci Technol 1985;19:700-707. Address reprint requests to: Jane Q. Koenig, Ph.D. Department of Environmental Health SC-34 University of Washington Seattle, WA 98195 191
Anuncio
Documentos relacionados
Descargar
Anuncio
Añadir este documento a la recogida (s)
Puede agregar este documento a su colección de estudio (s)
Iniciar sesión Disponible sólo para usuarios autorizadosAñadir a este documento guardado
Puede agregar este documento a su lista guardada
Iniciar sesión Disponible sólo para usuarios autorizados