- Ninguna Categoria
High Flow Nasal Oxygen in Pregnant Women: Anesthesia
Anuncio
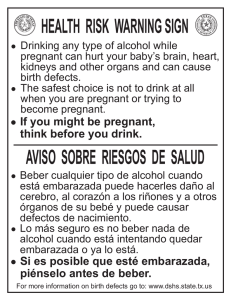
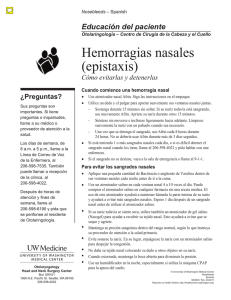
Anaesth Intensive Care 2018 | 46:1 P. C. F. Tan et al High flow humidified nasal oxygen in pregnant women P. C. F. Tan*, A. T. Dennis† Summary Failed airway management in the obstetric patient undergoing general anaesthesia is associated with major sequelae for the mother and/or fetus. Effective and adequate pre-oxygenation is an important safety strategy and a recommendation in all current major airway guidelines. Pre-oxygenation practice in the obstetric population may be suboptimal based on current literature. Recently, clinical applications for high flow nasal oxygen, also known as transnasal humidified rapid insufflation ventilatory exchange or THRIVE, are expanding in the non-obstetric population and may have theoretical benefits if used for pre-oxygenation and apnoeic oxygenation in the obstetric population. We review the current literature surrounding high flow nasal oxygen relevant to the pregnant woman. We also propose a basis for potential advantages and complications for its use in this context. Key Words: obstetric anaesthesia, airway management, pre-oxygenation, apnoeic oxygenation, intubation, desaturation, nasal high flow Difficulty in intubating the trachea or failure to oxygenate a pregnant woman during general anaesthesia is one of the most serious complications of obstetric anaesthesia. This complication may result in hypoxic brain injury and fetal and/or maternal death. Due to the known problem of the challenging obstetric airway, the Obstetric Anaesthetists’ Association (OAA) and Difficult Airway Society (DAS) of the United Kingdom published guidelines for management of difficult and failed tracheal intubation in obstetrics in November 20151. One of the key points discussed in the guidelines is the importance of pre-oxygenation in managing pregnant women undergoing general anaesthesia as it increases oxygen reserve in the lungs prior to anaesthesiainduced apnoea. Also discussed for the first time in an obstetric airway guideline was the possible use of high flow humidified nasal oxygen for pre-oxygenation and also for apnoeic oxygenation. High flow humidified nasal oxygen is gaining momentum in all fields of critical care as a tool to improve safety around airway management, especially during emergencies, with growing applications in anaesthesia, intensive care and emergency medicine. The objective of this literature review is to present an overview of the physiology underpinning high flow nasal pre-oxygenation, the changes in the obstetric airway and maternal physiology that may make high flow humidified nasal oxygen advantageous during induction of general anaesthesia, and to consider the application of this technology in the setting of term pregnant women undergoing general anaesthesia. * MBBS BMedSc, Anaesthetics Registrar, Royal Melbourne Hospital and Honorary Anaesthetics Research Fellow, Royal Women’s Hospital, Melbourne, Victoria † MBBS PhD MIPH PGDipEcho FANZCA, Staff Specialist Anaesthetist, Director of Anaesthesia Research, Department of Anaesthesia, The Royal Women’s Hospital and NHMRC Fellow, University of Melbourne, Departments of Pharmacology and Obstetrics and Gynaecology, Melbourne, Victoria Address for correspondence: Patrick Tan. Email: [email protected] Accepted for publication on September 21, 2017 36 Methods The literature reviewed included any systematic review, randomised controlled trial, observational study, case report or consensus statement pertaining to pre-oxygenation, apnoeic oxygenation and the use of high flow nasal oxygen in airway management in the pregnant and non-pregnant population. Obstetric airway issues were also explored in the same methodology. Electronic search strategies included the databases PUBMED (until May 2017), MEDLINE (until May 2017) and GOOGLE SCHOLAR (until May 2017) using the following key words: obstetric, parturient, pregnant, preoxygenation/preoxygenation, apnoeic/apneic oxygenation, difficult airway, high-flow nasal oxygen, transnasal humidified rapid insufflation ventilatory exchange. Current guidelines The latest airway management guidelines by the OAA and the DAS published in Anaesthesia November 2015 recommend that an end-tidal oxygen fraction (FetO2) of ≥0.9 should be achieved prior to induction of anaesthesia. This indicates effective lung denitrogenation. The traditional way anaesthetists pre-oxygenate pregnant women undergoing general anaesthesia is to use a tight-fitting facemask to deliver 100% inspired oxygen at a flow rate that exceeds the patient’s estimated minute ventilation. The new guideline also states that a supplementary method, ‘nasal oxygenation’ to facilitate bulk flow of oxygen to the alveoli, could be considered as part of: 1. Pre-oxygenation—a pre-oxygenation method and 2. apnoeic oxygenation—a technique to increase apnoeic time. The guidelines suggest the anaesthetist should consider attaching nasal cannulae with 5 litres per minute oxygen flow before starting routine pre-oxygenation to maintain bulk flow of oxygen during intubation attempts or attach Anaesth Intensive Care 2018 | 46:1 High flow humidified nasal oxygen in pregnant women Figure 1: The Optiflow™ (Fisher & Paykel Healthcare, Auckland, New Zealand) high flow humidified oxygen delivery system consisting of nasal cannulae, humidifier/heating system and circuit. The system can be used without any disruption to laryngoscopy and intubation. nasal oxygenation after pre-oxygenation during the apnoeic period1. There is also mention of humidified high flow nasal oxygen, however, no data exist in pregnant women as to its safety, efficacy or acceptability by pregnant women. It is possible that a new pre-oxygenation technique, using high flow humidified nasal oxygen, may have an application in pregnant women. However, before this new pre-oxygenation technique is considered, it should be equivalent (at least) to the current available technique in terms of safety and efficacy, i.e. be able to obtain an FetO2 of ≥0.9 after three minutes of pre-oxygenation. Currently there are no studies reporting FetO2 values in pregnant women after pre-oxygenation with high flow humidified nasal oxygen delivery systems and no studies reporting the use of nasal high flow oxygen to increase apnoea times. Therefore, it is unclear whether humidified high flow nasal oxygen is safe and beneficial in pregnant women. Physiology underpinning high flow humidified nasal oxygen High flow humidified nasal cannula oxygen therapy is a method of providing oxygen and continuous positive airway pressure (CPAP) to patients whilst facilitating carbon dioxide clearance. It consists of an oxygen inlet, an active humidifier, a single heated circuit and nasal cannulae. The system delivers up to 70 litres per minute flow of heated, humidified oxygen. Due to its mechanism of action, high flow humidified nasal cannula oxygen therapy results in washout of anatomical dead space, a constant fraction of inspired oxygen, good humidification and the provision of a low level of CPAP. Work of breathing is also decreased. There is also emerging work utilising fluid dynamic modelling which explains the mechanism of carbon dioxide clearance during apnoea, which was demonstrably superior to previous lowflow oxygen delivery systems2. High flow humidified nasal oxygen in the non-pregnant population Concurrent development of systems such as the Optiflow™ by Fisher & Paykel Healthcare (Auckland, New Zealand) is beginning to find utility in the non-obstetric population. Patel et al’s THRIVE study showed a prolonged median (range) apnoea time of 14 (5–65) minutes in 25 patients with difficult airways2. These patients had a median (interquartile range [IQR]) Mallampati score of 3 (2–3) and laryngoscopy grade of 3 (3–3) and none experienced peripheral oxygen saturations (SpO2) of <90% or any clinically apparent complications of hypercapnia2. Following that study, Mir and Patel et al demonstrated that pre-oxygenation with high flow nasal oxygen was not inferior to pre-oxygenation with a facemask in patients undergoing rapid sequence induction. They showed no significant difference in maintenance of SpO2 and arterial blood gas profiles despite longer apnoea times in the high flow nasal oxygen group in their randomised controlled trial of 40 patients3. Doyle et al’s observational study targeted patients at high risk of hypoxia during intubation. They reported a 7% incidence of significant desaturation (drop of SpO2 >10%) when high flow nasal pre-oxygenation and apnoeic oxygenation was used. Participants included patients 37 P. C. F. Tan et al Anaesth Intensive Care 2018 | 46:1 Figure 2: Participant in ramped and left lateral tilted position using TroopTM (Goal Medical, LLC, Eugene, OR, USA) pillow and wedge during pre-oxygenation study protocol. Picture reproduced with permission of the patient. requiring intubation in the emergency department or critical care unit and those with risk factors for hypoxia being intubated in the operating theatre. The impact of the THRIVE protocol was unable to be quantified however as this study did not compare this technique to established practice or to a pre-study incidence of significant desaturation4. MiguelMontanes et al’s prospective before–after study in 101 intensive care unit patients compared pre-oxygenation via a non-rebreathing bag reservoir facemask versus high flow nasal cannulae. Their results showed a significant difference in SpO2 during intubation, improvement in pre-oxygenation quality and reduced episodes of severe hypoxaemia in the high flow nasal oxygen group5. The study population comprised intensive care unit (ICU) patients requiring intubation with a median (IQR) Simplified Acute Physiology Score II of 44 (35–61.5) and a corresponding mortality risk of 25% to 50%5. Another study highlights the application of positive end-expiratory pressure (PEEP) during induction of general anaesthesia and showed that it prolonged safe apnoea time6. The Optiflow system purportedly maintains 3 to 7 cmH2O of PEEP. There has also been opinion from airway experts who believe that high flow nasal oxygen will become part of routine practice for all adult tracheal intubations in the near future7. High flow humidified nasal oxygen in the pregnant population There is an absence of evidence surrounding the use of high flow nasal oxygen in pregnant women. Computational 38 modelling using the Nottingham Physiology Simulator, which models the respiratory and cardiovascular systems accounting for the changes of pregnancy, predicts that apnoeic oxygenation using an inspired fraction of oxygen (FiO2) of 1.0 should prolong time to desaturation (SpO2 less than 90%) to more than 50 minutes in the average parturient and to more than 40 minutes in the morbidly obese parturient (body mass index 50 kg/m2)8. In order to assess the feasibility of undertaking a proposed larger study we have published a small pilot study of the use of this equipment in pregnant women9. Four pregnant women at term were recruited with written informed consent. Participants were placed on a hospital bed in a ramped position using a TroopTM elevation pillow (Goal Medical, LLC, Eugene, OR, USA) with left lateral tilt using a wedge. High flow humidified nasal oxygen was then administered at 30 litres per minute for 30 seconds then 50 litres per minute for a further 150 seconds and end-tidal gas sampling was performed via a facemask at the end of the three minute period. Each woman achieved 100% SpO2 at the end of the pre-oxygenation period and remained as such during the washout period. However, only one woman achieved the recommended pre-oxygenation induction of anaesthesia trigger threshold of an FetO2 ≥0.9. All women preferred the nasal pre-oxygenation system to the tightly fitting facemask. We anticipate that pregnant women with elevated body mass indices may require longer pre-oxygenation times or higher flows or both to achieve adequate denitrogenation. Larger prospective studies are required to delineate this relationship and so to explore these Anaesth Intensive Care 2018 | 46:1 hypotheses, we are undertaking a larger prospective study (ACTRN12616000531415p) to characterise the safety and efficacy of high flow nasal oxygen as a pre-oxygenation and apnoeic oxygenation strategy in pregnant women. The obstetric airway and maternal physiology The difficult obstetric airway is well described in the anaesthesia literature. Some sources report the incidence of difficult or failed airway to be approximately ten times that in the general surgical population10-12. Airway management in the parturient at term can be challenging as a result of anatomical changes (airway oedema) and physiological changes (decreased functional residual capacity coupled with higher risk of aspiration) of pregnancy. Studies have shown that airway changes can also happen acutely as women go into labour leading to decreased upper airway volume and increasing Mallampati scores in more than 60% of parturients13,14. Additionally, in the instance that a term pregnant woman requires a general anaesthetic, airway instrumentation typically occurs in emergency situations, requiring rapid sequence induction with the added metabolic burden of the feto-placental unit. The combination of these factors confers a high risk of peri-intubation hypoxia in this population. The more widespread use of regional anaesthesia for obstetric procedures has had a two-pronged effect, that is, the reduction in number of general anaesthetics (GA) performed15-18 but also the subsequent diminishing of training opportunities19. This becomes a major problem when the anaesthetist is faced with the high-risk situation of an emergency GA caesarean section. There are known major complications of the failed airway including hypoxic brain injury and fetal and/or maternal death. Despite the advocacy for early use of supraglottic airway devices to facilitate oxygenation in the failed intubation scenario, anaesthesiarelated maternal death still accounts for 1.6% of maternal deaths in the USA, with failed intubation being a leading cause20. Pre-oxygenation In Australia, recommended pre-oxygenation practice prior to caesarean section is three minutes of tidal breathing via a circle circuit delivering 100% oxygen or until the patient’s FetO2 reaches 0.9. FetO2 is widely accepted as the surrogate marker for lung denitrogenation21 and is the current accepted standard according to obstetric airway management guidelines1. A study of 20 pregnant women at term, using the traditional method of pre-oxygenation, showed that the mean time required to achieve an FetO2 of 0.9 was 107 +/-37 seconds but this was only achieved in 75% of the participants after three minutes of tidal volume breathing of 100% oxygen22. Porter et al reported retrospective data showing frequent inadequate pre-oxygenation of patients High flow humidified nasal oxygen in pregnant women anaesthetised in their obstetric emergency theatre23. It would seem that there is room for improvement in pre-oxygenation practice and better prospective data in the obstetric population to prevent undue risk to these patients. However, any change in practice needs to be supported by safety and efficacy data. In this area, any new pre-oxygenation technique needs to obtain the threshold value for FetO2 of 0.9 in at least the same percentage of the population compared with current routine practice. Apnoeic oxygenation The physiological phenomenon of apnoeic oxygenation has been known for more than a century with Volhard describing it in 190824. The nomenclature for it has evolved over time from ‘diffusion respiration’25 to ‘aventilatory mass flow’26 to ‘apnoeic oxygenation’27. They all refer to the physiological generation of mass flow of gas from the pharynx to alveoli as a consequence of the subatmospheric net pressure in the alveoli. This pressure gradient develops from the different rates by which oxygen in the alveoli moves into the bloodstream (~200 to 250 ml/minute) and carbon dioxide in the bloodstream moves into the alveoli (~8 to 20 ml/minute). The remaining carbon dioxide is buffered in the bloodstream, given its high water solubility. Alveoli will continue to take up oxygen even without diaphragmatic movements or lung expansion. In the clinical anaesthetic context, this process could theoretically be useful in extending the ‘safe apnoea time’ beyond which can be achieved by adequate preoxygenation alone. This time, which can be defined as the duration between apnoea and critical oxygen desaturation is typically six to eight minutes in a healthy, well preoxygenated non-pregnant adult. Apnoeic oxygenation can be achieved via various routes with potentially different levels of effectiveness and utility. For example, buccal oxygen administration of 10 litres per minute via a modified Ring– Adair–Elwyn (RAE) tube has been shown to increase apnoea time 2.5-fold in obese patients whilst maintaining safe endtidal carbon dioxide levels. This oral technique allows normal use of typical oral and nasal airway management adjuncts and manoeuvres28. Currently apnoeic oxygenation is not part of established practice in obstetric anaesthesia. The current practice is to pre-oxygenate the pregnant woman undergoing general anaesthesia and once the FetO2 is 0.9, to induce general anaesthesia. Tracheal intubation is performed without additional oxygenation or ventilation. The new guidelines advocate gentle bag–mask ventilation during the time between ceasing pre-oxygenation and attempting to intubate the trachea (the time it takes for the muscle relaxant to work). This has been suggested so as to prevent the desaturation that sometimes occurs in the setting of tracheal intubation in pregnant women. Based on the work of Patel in non-pregnant adults2 and Pillai’s computational modelling8, the use of high flow humidified nasal oxygen during this time (apnoeic 39 Anaesth Intensive Care 2018 | 46:1 P. C. F. Tan et al oxygenation) in pregnant women is likely to increase the time it takes for desaturation to occur as the woman will be receiving continuous oxygen. There are no clinical studies examining this. Potential advantages of this technology in pregnant women undergoing general anaesthesia The application of high flow nasal oxygen in obstetric anaesthesia seems relevant and logical. The technology may improve safety in a population that has a higher incidence of difficult airway, a higher metabolic rate and oxygen consumption coupled with a lower respiratory reserve, by minimising hypoxaemia and its consequences on mother and fetus. As the relevant physiological changes in pregnancy have their peak effects near term, it would seem most pertinent to assess safety and efficacy of the use of this equipment in this population. If the physiology and physics of high flow humidified nasal oxygenation as described can translate to clinical outcomes (as it has in the non-obstetric population), then there may be specific benefits for the obstetric population. As an adjunct to current airway management practice, we propose that these systems may provide a safety net in the higher-risk and time-critical situation of a Category 1 (urgent threat to the life or health of a woman or fetus) GA caesarean section and alleviate some operator stress in this scenario by prolonging safe apnoea time. As an alternative to current practice, it has the added benefit of ‘hands-free’ pre-oxygenation allowing anaesthetic staff to attend to other tasks in a timecritical situation. Once safety and clinical benefit can be demonstrated, anaesthetists will have an evidence base for its use across all gestations and indications. Applications may expand from there. Potential complications As there is paucity of evidence, practitioners may be understandably cautious in the use of high flow humidified nasal oxygen in the obstetric population due to the theoretical risks of epistaxis and gastric insufflation. Epistaxis is a known but uncommon risk associated with this technique29,30 but could theoretically be lessened by the efficient humidification of gases through the Optiflow system. The incidence of epistaxis may be more common in the obstetric population due to increased nasopharyngeal mucosal oedema and vascularity. Further study is needed. Stolady et al in the United Kingdom have shown using a manikin study that oesophageal pressures remain low with the use of high flow nasal oxygen which suggests that it may be safe to use despite the increased incidence of aspiration in the obstetric population31. Conclusion This review discusses the known issue of the difficult obstetric airway, current practice and shortcomings of pre- 40 oxygenation in the obstetric population and a potential role for an alternative method of pre-oxygenation with the added benefit of apnoeic oxygenation. Furthermore, in the obstetric population, there is a risk that this technique may be incorporated into current practice without appropriate scientific testing for efficacy and safety. Therefore it is important to perform an ethically approved, prospective safety and efficacy study prior to the possibility of widespread and uncontrolled adoption of the technique. Acknowledgements Dr Patrick Tan was awarded the Kevin McCaul Prize at the 2016 ASA National Scientific Congress for this review article. We would like to acknowledge Mr Adrian Vendy from Fisher & Paykel Healthcare for his assistance in obtaining the images for this article. Fisher & Paykel Healthcare provides equipment for the purposes of ongoing research in our department. References 1. Mushambi MC, Kinsella SM, Popat M, Swales H, Ramaswamy KK, Winton AL, Quinn AC. Obstetric Anaesthetists’ Association and Difficult Airway Society guidelines for the management of difficult and failed tracheal intubation in obstetrics. Anaesthesia 2015; 70:1286-1306. 2. Patel A, Nouraei SAR. Transnasal Humidified Rapid-Insufflation Ventilatory Exchange (THRIVE): a physiological method of increasing apnoea time in patients with difficult airways. Anaesthesia 2015; 70:323-329. 3. Mir F, Patel A, Iqbal R, Cecconi M, Nouraei SAR. A randomised controlled trial comparing transnasal humidified rapid insufflation ventilatory exchange (THRIVE) pre-oxygenation with facemask pre-oxygenation in patients undergoing rapid sequence induction of anaesthesia. Anaesthesia 2017; 72: 439-443. 4. Doyle AJ, Stolady D, Mariyaselvam M, Wijewardena G, Gent E, Blunt M, Young P. Preoxygenation and apneic oxygenation using Transnasal Humidified Rapid-Insufflation Ventilatory Exchange for emergency intubation. J Crit Care 2016; 36:8-12. 5. Miguel-Montanes R, Hajage D, Messika J, Bertrand F, Gaudry S, Rafat C et al. Use of high flow nasal cannula oxygen therapy to prevent desaturation during tracheal intubation of intensive care patients with mild-to-moderate hypoxemia. Crit Care Med 2015; 43:574-583. 6. Gander S, Frascarolo P, Suter M, Spahn DR, Magnusson L. Positive end-expiratory pressure during induction of general anesthesia increases duration of nonhypoxic apnea in morbidly obese patients. Anesth Analg 2005; 100:580-584. 7. Marshall SD, Pandit JJ. Radical evolution: the 2015 Difficult Airway Society guidelines for managing unanticipated difficult or failed tracheal intubation. Anaesthesia 2016; 71:131-137. 8. Pillai A, Chikhani M, Hardman JG. Apnoeic oxygenation in pregnancy: a modelling investigation. Anaesthesia 2016; 71:1077-1080. 9. Tan PCF, Dennis AT. High flow humidified nasal pre-oxygenation in pregnant women. Anaesthesia 2016; 71:851-852. Anaesth Intensive Care 2018 | 46:1 10. McDonnell NJ, Paech MJ, Clavisi OM, Scott KL. Difficult and failed intubation in obstetric anaesthesia: an observational study of airway management and complications associated with general anaesthesia for caesarean section. Int J Obstet Anesth 2008; 17:292-297. 11. Quinn AC, Milne D, Columb M, Gorton H, Knight M. Failed tracheal intubation in obstetric anaesthesia: 2 yr national casecontrol study in the UK. Br J Anaesth 2013; 110:74-80. 12. Tao W, Edwards JT, Tu F, Xie Y, Sharma SK. Incidence of unanticipated difficult airway in obstetric patients in a teaching institution. J Anesth 2012; n/a:n/a. 13. Boutonnet M, Faitot V, Katz A, Salomon L, Keita H. Mallampati class changes during pregnancy, labour, and after delivery: can these be predicted? Br J Anaesth 2010; 104:67-70. 14. Kodali B-S, Chandrasekhar S, Bulich LN, Topulos GP, Datta S. Airway changes during labor and delivery. Anesthesiology 2008; 108:357-362. 15. Hawthorne L, Wilson R, Lyons G, Dresner M. Failed intubation revisited: 17-yr experience in a teaching maternity unit. Br J Anaesth 1996; 76:680-684. 16. Johnson RV, Lyons GR, Wilson RC, Robinson AP. Training in obstetric general anaesthesia: a vanishing art? Anaesthesia 2000; 55:179-183. 17. Rahman K, Jenkins JG. Failed tracheal intubation in obstetrics: no more frequent but still managed badly. Anaesthesia 2005; 60:168-171. 18. Tsen LC, Pitner R, Camann WR. General anesthesia for cesarean section at a tertiary care hospital 1990-1995: indications and implications. Int J Obstet Anesth 1998; 7:147-152. 19. Smith NA, Tandel A, Morris RW. Changing patterns in endotracheal intubation for anaesthesia trainees: a retrospective analysis of 80,000 cases over 10 years. Anaesth Intensive Care 2011; 39:585-589. 20. Hawkins JL, Chang J, Palmer SK, Gibbs CP, Callaghan WM. Anesthesia-related maternal mortality in the United States: 1979-2002. Obstet Gynecol 2011; 117:69-74. 21. Machlin HA, Myles PS, Berry CB, Butler PJ, Story DA, Heath BJ. End-tidal oxygen measurement compared with patient factor assessment for determining preoxygenation time. Anaesth Intensive Care 1993; 21:409-413. 22. Chiron B, Laffon M, Ferrandiere M, Pittet JF, Marret H, Mercier C. Standard preoxygenation technique versus two rapid techniques in pregnant patients. Int J Obstet Anesth 2004; 13:11-14. 23. Porter R, Wrench IJ, Freeman R. Preoxygenation for general anaesthesia in pregnancy: is it adequate? Int J Obstet Anesth 2011; 20:363-365. 24. Volhard F. Uber kunstliche Atmung durch Ventilation der Trachea und eine einfache Vorrichtung zur hytmischen kunstlichen Atmung. München Medizinische Wochenschrift. 1908. pp. 209-211. 25. Draper WB, Whitehead RW. Diffusion respiration in the dog anesthetized with pentothal sodium. Anesthesiology 1944; 5:262-273. 26. Bartlett RG Jr, Brubach HF, Specht H. Demonstration of aventilatory mass flow during ventilation and apnea in man. J Appl Physiol 1959; 14:97-101. 27. Frumin M J, Epstein RM, Cohen G. Apneic oxygenation in man. Anesthesiology 1959; 20:789-798. High flow humidified nasal oxygen in pregnant women 28. Heard A, Toner AJ, Evans JR, Aranda Palacios AM, Lauer S. Apneic oxygenation during prolonged laryngoscopy in obese patients: a randomized, controlled trial of buccal RAE tube oxygen administration. Anesth Analg 2017; 124:1162-1167. 29. Baudin F, Gagnon S, Crulli B, Proulx F, Jouvet P, Emeriaud G. Modalities and complications associated with the use of high flow nasal cannula: experience in a pediatric ICU. Respir Care 2016; 61:1305-1310. 30. Sotello D, Rivas M, Mulkey Z, Nugent K. High flow nasal cannula oxygen in adult patients: a narrative review. Am J Med Sci 2015; 349:179-185. 31. Stolady D, Gavula L, Young E, Blunt M, Young P. The risk of gastric insufflation with THRIVE. World Airway Management Meeting, Poster Presentation; 12-14 November; Dublin, Ireland 2015. 41
Anuncio
Documentos relacionados
Descargar
Anuncio
Añadir este documento a la recogida (s)
Puede agregar este documento a su colección de estudio (s)
Iniciar sesión Disponible sólo para usuarios autorizadosAñadir a este documento guardado
Puede agregar este documento a su lista guardada
Iniciar sesión Disponible sólo para usuarios autorizados