- Ninguna Categoria
Butorphanol & Isoflurane Anesthesia in Horses: A Clinical Study
Anuncio
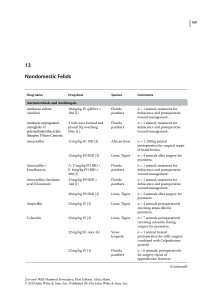
Veterinary Anaesthesia and Analgesia, 2011, 38, 186–194 doi:10.1111/j.1467-2995.2011.00600.x RESEARCH PAPER A clinical study on the effect in horses during medetomidine–isoflurane anaesthesia, of butorphanol constant rate infusion on isoflurane requirements, on cardiopulmonary function and on recovery characteristics Regula Bettschart-Wolfensberger*, Sidonia Dicht*, Cecilia Vullo , Angela Frotzlerà, Jan M Kuemmerle§ & Simone K Ringer* *Section of Anaesthesiology, Equine Department, Vetsuisse Faculty University of Zurich, Zurich, Switzerland Ospedale Veterinario Didattico, Università degli Studi di Camerino, Camerino, Italy àParaplegikerzentrum Nottwil, Switzerland §Section of Surgery, Equine Department, Vetsuisse Faculty University of Zurich, Zurich, Switzerland Correspondence: Regula Bettschart-Wolfensberger, Equine Department, Section of Anaesthesiology, Vetsuisse Faculty University of Zurich, Winterthurerstr, 260, 8057 Zurich, Switzerland. E-mail: [email protected] Abstract Objective To test if the addition of butorphanol by constant rate infusion (CRI) to medetomidine– isoflurane anaesthesia reduced isoflurane requirements, and influenced cardiopulmonary function and/or recovery characteristics. Study design Prospective blinded randomised clinical trial. Animals 61 horses undergoing elective surgery. Methods Horses were sedated with intravenous (IV) medetomidine (7 lg kg)1); anaesthesia was induced with IV ketamine (2.2 mg kg)1) and diazepam (0.02 mg kg)1) and maintained with isoflurane and a CRI of medetomidine (3.5 lg kg)1 hour)1). Group MB (n = 31) received butorphanol CRI (25 lg kg)1 IV bolus then 25 lg kg)1 hour)1); Group M (n = 30) an equal volume of saline. Artificial ventilation maintained end-tidal CO2 in the normal range. Horses received lactated Ringer’s solution 5 mL kg)1 hour)1, dobutamine <1.25 lg kg)1 minute)1 and colloids if required. Inspired and exhaled gases, heart rate and mean arterial blood pressure (MAP) 186 were monitored continuously; pH and arterial blood gases were measured every 30 minutes. Recovery was timed and scored. Data were analyzed using two way repeated measures ANOVA, independent t-tests or Mann–Whitney Rank Sum test (p < 0.05). Results There was no difference between groups with respect to anaesthesia duration, end-tidal isoflurane (MB: mean 1.06 ± SD 0.11, M: 1.05 ± 0.1%), MAP (MB: 88 ± 9, M: 87 ± 7 mmHg), heart rate (MB: 33 ± 6, M: 35 ± 8 beats minute)1), pH, PaO2 (MB: 19.2 ± 6.6, M: 18.2 ± 6.6 kPa) or PaCO2. Recovery times and quality did not differ between groups, but the time to extubation was significantly longer in group MB (26.9 ± 10.9 minutes) than in group M (20.4 ± 9.4 minutes). Conclusion and clinical relevance Butorphanol CRI at the dose used does not decrease isoflurane requirements in horses anaesthetised with medetomidine–isoflurane and has no influence on cardiopulmonary function or recovery. Keywords anaesthesia, butorphanol, horse, isoflurane, medetomidine. Butorphanol CRI during medetomidine–isoflurane anaesthesia R Bettschart-Wolfensberger et al. Introduction Complicated surgeries of >1.5 hours in horses are performed most usually using inhalation anaesthesia (Mee et al. 1998; Bidwell et al. 2007). All inhalant anaesthetics impair cardiopulmonary function in a dose dependent fashion (Steffey & Howland 1980) and under many clinical circumstances do not provide sufficient analgesia to prevent nociception during surgery. Therefore the use of combination anaesthesia has gained widespread popularity, the aim being to reduce the concentration of the inhalant used (Bettschart-Wolfensberger et al. 2001; Ringer et al. 2007) and to improve cardiopulmonary function. Furthermore combination anaesthesia often reduces nociception and provides better analgesia. As a result, horses recovering from such ‘balanced’ anaesthesia might experience less pain and have smoother and more coordinated recoveries. Drugs commonly used in horses for combination anaesthesia are lidocaine (Dzikiti et al. 2003; Valverde et al. 2005), ketamine (Yamashita et al. 2002; Larenza et al. 2009), alpha-2 adrenoceptor agonists (Bettschart-Wolfensberger et al. 2001; Bennett et al. 2004; Kalchofner et al. 2006), and opioids (Hofmeister et al. 2008; Larenza et al. 2009). All these drugs except the opioids reduce minimum alveolar concentration (MAC) dose dependently. Under experimental circumstances both morphine and butorphanol have failed consistently to reduce the MAC of inhalation agents (Matthews & Lindsay 1990; Steffey et al. 2003). In contrast, the use of butorphanol in clinical cases resulted in a reduced sympathetic response to noxious stimuli and was therefore considered a beneficial combination with inhalation anaesthesia (Hofmeister et al. 2008). Medetomidine, an alpha-2 adrenoceptor agonist, has been compared to lidocaine and S-ketamine combination anaesthesia regimes in clinical cases (Larenza et al. 2007; Ringer et al. 2007). In both reports, the use of medetomidine resulted in recoveries from anaesthesia of better quality. As medetomidine is an alpha-2 adrenoceptor agonist, bradycardia, reduced cardiac output and changes in vascular tone might be of concern. When used in standing ponies a bolus of medetomidine was followed by a constant rate infusion (CRI) of medetomidine, only the bolus decreased cardiac output and heart rate (Bettschart-Wolfensberger et al. 1999a,b). At steady state, which is reached within 30 minutes following bolus application, cardiac output did not differ from presedation values (Betts- chart-Wolfensberger et al. 1999a). In an experimental group of horses, no difference in cardiac output was found when lidocaine-isoflurane was compared to lidocaine-medetomidine–isoflurane, but recovery was of better quality in the group receiving medetomidine (Valverde et al. 2010). In contrast, lidocaine-isoflurane anaesthesia was associated with better mean cardiopulmonary function than medetomidine–isoflurane anaesthesia (Ringer et al. 2007). However, the lowest individual heart rates, arterial blood pressures, cardiac indices and arterial oxygen tensions recorded in all groups were identical. It was speculated that the higher mean arterial blood pressures and cardiac output values were related to insufficient depth of anaesthesia rather than to a pure result of differences in drug regimens. Medetomidine–isoflurane was successfully used in a further 300 equine anaesthetic procedures with a mean duration of 149 minutes (Kalchofner et al. 2006) and in horses for fracture repair prior to pool recovery (Bettschart-Wolfensberger et al. 2008). Although it has been questioned whether administration of opioids to horses is useful (Bennett & Steffey 2002) there is no doubt that their combination with alpha-2 adrenoceptor agonists is beneficial (Clarke & Paton 1988; Schatzman et al. 2001; Kohler et al. 2004). The combination results in more reliable sedation and analgesia whilst using lower dose rates of alpha-2 adrenoceptor agonists (Taylor et al. 1988). When butorphanol was added to an intravenous (IV) anaesthetic protocol with alpha-2 adrenoceptor agonists and ketamine, duration of anaesthesia was prolonged (Matthews et al. 1991) and quality of anaesthesia was better (Corletto et al. 2005; Marntell et al. 2006). The aim of the present study was to investigate the effect of butorphanol in horses undergoing elective surgery and anaesthetized with a combination of medetomidine and isoflurane. The hypothesis was that with butorphanol, the dose of isoflurane required for maintenance of anaesthesia would be reduced and that cardiopulmonary function during anaesthesia and recovery from anaesthesia would be improved. Material and methods The study was performed according to the ethics and animal experimentation by-law of the Vetsuisse Faculty of the University of Zurich. Sixty-one client-owned horses (>200 kg), ASA (American Society of Anesthesiologists) category I 2011 The Authors. Veterinary Anaesthesia and Analgesia 2011 Association of Veterinary Anaesthetists and the American College of Veterinary Anesthesiologists, 38, 186–194 187 Butorphanol CRI during medetomidine–isoflurane anaesthesia R Bettschart-Wolfensberger et al. or II, which were to undergo elective surgical procedures in which the eye was not covered, were included in the study. Food but not water was withheld for 10–16 hours prior to anaesthesia. The horses were assigned randomly to one of the two treatment groups, group MB (medetomidine and butorphanol infusions) or group M (medetomidine and saline control). All anaesthetic procedures were performed always by the same experienced anaesthetist (RB) who was unaware of the treatment group of any specific case. At least 60 minutes before induction of anaesthesia a 14 gauge · 160 mm jugular catheter (Secalon T with flowswitch; Becton Dickinson AG, Switzerland) was inserted using local anaesthesia with mepivacaine 2% (Mepivacain HCL 2%; Kantonsapotheke Zurich, Switzerland). The horses were premedicated 60 minutes prior to anaesthesia with cefquinom (Cobactan 4.5% ad us. vet.; Veterinaria AG, Switzerland), 1 mg kg)1 IV, flunixin (Flunixin ad us. vet.; Biokema SA, Switzerland), 1 mg kg)1 for soft tissue surgery or phenylbutazone (Butadion ad us. vet.; Streuli AG, Switzerland), 4 mg kg)1 for orthopaedic surgeries IV. Thirty minutes before anaesthesia induction acepromazine (Prequillan; Arovet AG, Switzerland), 0.03 mg kg)1 was administered intramuscularly (IM). All horses were sedated in their stall with 3 lg kg)1 medetomidine (Dorbene; Dr. Graeub AG, Switzerland) IV. Their mouth was flushed and they were walked to the anaesthesia induction area. Five minutes after the initial medetomidine bolus the horses of group MB were given 25 lg kg)1 butorphanol (Alvegesic 1% forte ad us. vet.; Virbac AG, Switzerland) IV, whereas horses of group M received an equal volume of saline. This was followed 2 minutes later by an infusion of medetomidine at a dose rate of 1 lg kg)1 minute)1. When sedation was considered adequate (judged by the ‘blinded’ anaesthetist, RB) anaesthesia was induced with ketamine (Narketan 10 ad us. vet.; Chassot AG, Switzerland), 2.2 mg kg)1 IV in combination with diazepam (Valium 10 mg; Roche Pharma Schweiz AG, Switzerland), 0.02 mg kg)1 IV. Once the horses were recumbent and the trachea intubated, they were hoisted onto a surgical table and immediately attached to a large animal circle system (LAVC2000; JD Medical distributing Co., Inc, AZ, USA). Intermittent positive pressure ventilation (IPPV) was commenced (Bird Mark 8; Medical solution, Switzerland) to maintain an end-tidal partial pressure of CO2 (PE¢CO2) of 6–7.3 kPa (45–55 mmHg). The initial 188 fraction of inspired oxygen (FiO2) was 0.45–0.55. When arterial oxygen tension (PaO2) dropped below 10.7 kPa (80 mmHg) FiO2 was increased to 0.9–1. Anaesthesia was maintained with isoflurane (Isoflo ad us. vet.; Dr. Graeub AG, Switzerland) in oxygen and air to maintain a light but adequate plane of anaesthesia, as judged by the experienced anaesthetist (RB). A brisk palpebral reflex and/or sporadic spontaneous blinking was considered normal. If the horses developed nystagmus or were breathing against the ventilator, ketamine was administered at a dose of 0.05–0.1 mg kg)1 IV. If the horses moved, thiopental (Pentothal; Abbott AG, Switzerland) was administered at a dose of 0.5–1 mg kg)1 IV. Isoflurane concentration was increased following ketamine or thiopental administration. Immediately following anaesthesia induction all horses were given a CRI of medetomidine 3.5 lg kg)1 hour)1. Additionally, Group MB received a CRI of butorphanol at 25 lg kg)1 hour)1 and group M an equal volume of saline. Drug and saline placebo infusions were administered by an automatic syringe driver (Phoenix D; Schoch Electronics AG, Switzerland) and other fluids by an infusion pump (Volumed; Arcomed AG, Switzerland). Lactated Ringer’s solution (Ringer-Lactat-Lösung; Fresenius Kabi AG, Switzerland) was administered IV for the duration of anaesthesia at an infusion rate of 5 mL kg)1 hour)1. Dobutamine (Dobutrex; Eli Lilly S.A., Switzerland) infusion was started after anaesthesia induction at a rate of 0.63 lg kg)1 minute)1, and consequently, infusion rates were adjusted to maintain mean arterial blood pressure (MAP) between 70 and 90 mmHg. Maximal infusion rate of dobutamine was 1.25 lg kg)1 minute)1. If MAP remained <70 mmHg after 1.25 lg kg)1 minute)1 dobutamine had been infused for 10 minutes, the infusion rate of lactated Ringer’s solution was increased to 10 mL kg)1 hour)1. If MAP remained <70 mmHg for a further 20 minutes, an infusion of hetastarch (HAES-steril 10%; Fresenius Pharma Schweiz AG, Switzerland), 2–10 mL kg)1 hour)1 was commenced. A urinary catheter was placed in all horses immediately following anaesthesia induction and was left in place until the horse had recovered from anaesthesia. Cardiopulmonary function was measured using a multiparameter monitor (Datex-Ohmeda Cardiocap/ 5; Anandic AVL, Switzerland). Electrocardiogram (ECG), systolic (SAP), diastolic (SAP) and mean intra-arterial blood pressures were measured and 2011 The Authors. Veterinary Anaesthesia and Analgesia 2011 Association of Veterinary Anaesthetists and the American College of Veterinary Anesthesiologists, 38, 186–194 Butorphanol CRI during medetomidine–isoflurane anaesthesia R Bettschart-Wolfensberger et al. pulse-oximetry was performed continuously. Arterial blood pressures were measured via a 22-gauge catheter (Suflo IV Catheter 22G · 1¢¢; Terumo, Medical Solution Gmbh, Switzerland) inserted into the facial artery. The zero reference point was determined from the level of the manubrium sternae. Respiratory frequency (fR) and inspiratory and expiratory concentrations of isoflurane (Fi¢Iso, FE¢Iso), carbon dioxide and O2 were measured continuously using side-stream spirometry (Cardiocap). The following parameters were recorded at five minute intervals: heart rate (HR), fR, arterial blood pressures, haemoglobin saturation, FiO2, PE¢CO2, FE¢Iso, eye reflexes, infusion rate of dobutamine, administered drugs and infusion rates. Arterial blood gases and pH were measured 10 minutes following induction of anaesthesia and every 30 minutes thereafter. For blood gas analyses, blood was withdrawn anaerobically from the arterial catheter and analysed immediately by a portable analyser (i-STAT Analyser; Axon Lab AG, Switzerland). Fifteen to 20 minutes before the end of anaesthesia morphine (Morphin HCl 10 mg; Sintetica SA, Switzerland), 0.1 mg kg)1 was administered IM. At the end of surgery the horses were disconnected from the rebreathing circuit and, at the same time, CRIs were stopped. For recovery all horses were sedated with medetomidine, 2 lg kg)1 IV. During the recovery phase inspired air was supplemented with O2 (15 L minute)1), which was administered via the endotracheal tube or, following extubation, via a small tube in the nasal cavity. Horses’ tracheas were extubated when the return of the swallowing reflex was noted or if the horse tried to get up before this point was reached. Before extubation each horse received 10 mL phenylephrine 0.15% (Phenylephrini hydrochloridum 1.5 mg mL)1; G.Streuli & Co. AG, Switzerland) into the nares. The horse’s nose was manually raised from the floor and the phenylephrineinstilledintotheventralmeatusofthenasalcavity. Horses were allowed to recover from anaesthesia without assistance. Horses that were not standing 60 minutes after disconnection were stimulated by voice. The recoveries from anaesthesia were scored and timed by the same investigating anaesthetist (RB). The quality of recovery was graded on a scale of five points (Table 1) with a score of 1 representing the best recovery. Recovery timing consisted of recording time from disconnection of the anaesthetic to extubation, duration of lateral recumbency, time to sternal recumbency, duration of sternal recumbency and the time to standing. Table 1 Scoring system used to assess recovery from anaesthesia Score awarded 1 2 3 4 5 Description of recovery Horse capable to stand at the first attempt, minimal ataxia Two attempts needed before standing More than 2 attempts needed before standing, horse remains calm, minimal ataxia when standing Horse becomes excited during recovery, danger of injury Recovery resulting in injury of the horse Statistical analyses These were performed using the software package SigmaStat 3.5 (Systat Software GmbH, Germany). Normality was checked by plotting data as histograms and by using a Kolomogrov–Smirnov test. Differences between groups were tested using an independent t-test (normally distributed data) or a Mann–Whitney Rank Sum test (non-normally distributed data). Repeatedly measured parameters were analysed using a two-way repeated-measures analysis of variance (ANOVA) for differences over time and between treatments. All pairwise multiple comparison procedures were performed by the Tukey post hoc test. Data from the first two hours of anaesthesia were included in the 2-way ANOVA. Significance was considered when p < 0.05. Results Data are presented as mean ± SD or median and range. Group MB consisted of 31 horses and group M of 30 horses. There were no differences between the groups concerning weight (MB: 509 ± 88 kg, M: 493 ± 101 kg), age (MB: 7.8 ± 5.01 years, M: 7.7 ± 5.09 years), and duration of anaesthesia (MB: 115, 55–230 minutes, M: 104, 66–204 minutes). Types of surgery in both groups were: three and six minor orthopaedic surgeries (arthroscopy of one joint, splint bone removal), 16 and 17 major orthopaedic surgeries (arthroscopy of several joints, bilateral neurectomy, arthroscopy including tourniquet) and 12 and 7 soft tissue surgeries in MB and M, respectively. Median dose of medetomidine necessary for sedation prior to anaesthesia induction was 7 lg kg)1 in 2011 The Authors. Veterinary Anaesthesia and Analgesia 2011 Association of Veterinary Anaesthetists and the American College of Veterinary Anesthesiologists, 38, 186–194 189 Butorphanol CRI during medetomidine–isoflurane anaesthesia R Bettschart-Wolfensberger et al. 160 Group M Group MB 140 MAP (mmHg) 120 * * 100 80 60 40 20 0 30 40 50 60 70 80 90 100 110 120 Time (minutes) Figure 1 Mean arterial blood pressures (MAP) (mean ± SD) in horses during medetomidine–butorphanol–isoflurane (MB) or medetomidine–isoflurane (M) anaesthesia. Both groups received a constant rate infusion (CRI) of medetomidine (3.5 lg kg)1 hour)1). Group MB also received a CRI of butorphanol (25 lg kg)1 hour)1); group M an equal volume of saline. Timepoints with identical symbols (*) differ significantly (p < 0.05) within groups for both groups. both groups (ranges MB: 5–11.8 lg kg)1, M: 5– 8 lg kg)1). Four horses of group MB and two horses of group M needed a bolus of thiopental following induction of anaesthesia as they were swallowing, thus preventing endotracheal intubation. There were no differences between the groups in mean FE¢Iso concentrations (MB: 1.06 ± 0.11%, M: 1.05 ± 0.1%) or any of the measured cardiopulmonary parameters: MAP (MB: 88 ± 9, M: 87 ± 7 mmHg), HR (MB: 33 ± 6, M: 35 ± 8 beats minute)1), pH (MB: 7.37 ± 0.03, M: 7.38 ± 0.03), PaO2 (MB: 19.2 ± 6.6, M: 18.2 ± 6.6 kPa), PaCO2 (MB: 6.9 ± 0.6, M: 6.7 ± 0.7 kPa). In Figs 1–4 HR, MAP, PaO2 and PaCO2 over time are presented graphically. Within groups, there were significant changes in HR, MAP, PaCO2 and PaO2 over time, but no differences between the groups. From minutes 30 to 70 and minutes 70 to 100 HR rose significantly in both groups. MAPs were significantly lower 110 minutes following anaesthesia induction compared to MAPs at 30 minutes. PaO2 was significantly lower 60 minutes following anaesthesia induction in comparison to values at 30 minutes. There was no difference between the groups in the median (range) dobutamine infusion rate [MB: 0.55 (0.28–1.17) lg kg)1 minute)1, M: 0.55 (0.3–1.36) lg kg)1 minute)1] or the amount of lactated Ringer’s solution [MB: 8.8 (3.7–15.1) mL kg)1 hour)1, M: 8.7 (5.8–24.2) mL kg)1 hour)1] infused. A total of 11 horses, all in dorsal recumbency 190 (four in MB and seven in M) were given hetastarch (MB 1.5 ± 0.9 mL kg)1 hour)1, M: 1.5 ± 0.6 mL kg)1 hour)1). In group MB, seven horses were given ketamine on 11 occasions and in group M nine horses on 16 occasions. In group MB one horse received thiopental during anaesthesia. Recovery times are listed in Table 2. Time to extubation was significantly longer in group MB. All other times relating to recovery did not differ between groups. Recovery scores are represented graphically in Fig. 5. There was no difference in recovery scores between the groups. Discussion The present study tested whether the addition of butorphanol to medetomidine–isoflurane anaesthesia in horses reduced isoflurane requirements and influenced cardiopulmonary function and recovery characteristics. Butorphanol did not cause any differences in cardiopulmonary function, requirement of isoflurane to maintain anaesthesia or recovery times and quality. However, the time to swallowing and extubation during the recovery phase was significantly longer in the butorphanol group. It is commonly agreed that in conscious horses the use of butorphanol improves the reliability of alpha-2 adrenoceptor agonist induced sedation at dose rates lower than those originally recommended 2011 The Authors. Veterinary Anaesthesia and Analgesia 2011 Association of Veterinary Anaesthetists and the American College of Veterinary Anesthesiologists, 38, 186–194 Butorphanol CRI during medetomidine–isoflurane anaesthesia R Bettschart-Wolfensberger et al. 80 Group M Group MB 70 Beats minute–1 60 50 * * 40 30 20 10 0 30 40 50 60 70 80 90 100 110 120 Time (minutes) Figure 2 Heart rates (mean ± SD) in horses during medetomidine–butorphanol–isoflurane (MB) or medetomidine– isoflurane (M) anaesthesia. Timepoints with identical symbols (* and ) differ significantly (p < 0.05) within groups for both groups. For dose regimens see Fig. 1. 30 * Group M * Group MB PaO2 (kPa) 25 20 15 10 5 30 60 90 120 Time (minutes) Figure 3 Arterial PO2 tensions (mean ± SD) in horses during medetomidine–butorphanol–isoflurane (MB) or medetomidine–isoflurane (M) anaesthesia. Timepoints with identical symbols (*) differ significantly (p < 0.05) within groups for both groups. For dose regimens see Fig. 1. for sole use (Clarke & Paton 1988; Clarke et al. 1991). In the present study the use of butorphanol did not reduce the dose of medetomidine necessary to achieve sedation considered profound enough for anaesthesia induction with ketamine. The horses were not stimulated and sedation was not scored in detail before anaesthesia induction in order not to unnecessarily prolong this phase. Two recent stud- ies (Ringer et al. 2009; Ringer et al. 2011) investigated, whether butorphanol reduces the dose of xylazine or romifidine necessary to maintain sedation in unstimulated horses (judged only by the position of the head) and came to the same conclusion. The use of butorphanol in combination with alpha-2 adrenoceptor agonists might alter reliability of but not apparent depth of sedation. 2011 The Authors. Veterinary Anaesthesia and Analgesia 2011 Association of Veterinary Anaesthetists and the American College of Veterinary Anesthesiologists, 38, 186–194 191 Butorphanol CRI during medetomidine–isoflurane anaesthesia R Bettschart-Wolfensberger et al. 10 Group M Group MB PaCO2 (kPa) 9 8 7 6 5 4 30 60 90 120 Time (minutes) Figure 4 Arterial PCO2 (mean ± SD) tensions in horses during medetomidine–butorphanol–isoflurane (MB) or medetomidine–isoflurane (M) anaesthesia. The increase over time within both groups was significant (p < 0.05). For dose regimens, see Fig. 1. Time (minutes) to extubation (horse swallowing or trying to stand up) Duration of lateral recumbency (minutes) Duration of sternal recumbency (minutes) Time to standing, unassisted (minutes) Group MB Group M 26.9 ± 10.9 20.4 ± 9.4 Group MB Group M 15 10 5 0 1 2 3 4 5 Score 44.6 ± 11.0 6.0 (0.0–40.0) 54.6 ± 16.0 46.2 ± 12.9 1.8 (0.0–24.0) 51.2 ± 13.4 Sedation before induction of anaesthesia with ketamine has to be sufficiently profound in order to optimise the quality of this induction. All horses in the present study showed deep sedation before ketamine administration and therefore it is surprising that four horses in the MB and two in the M groups required thiopental after recumbency in order to enable endotracheal intubation. It is unlikely that butorphanol influenced this, although one study reported that the combination of romifidine with butorphanol resulted in very poor anaesthesia induction quality in two out of six horses 192 20 Number of horses Table 2 Mean (± SD) or median (range) recovery times (minutes) from disconnection of isoflurane recorded following combination anaesthesia with medetomidine– butorphanol–isoflurane (Group MB n = 31) or medetomidine–isoflurane (Group M, n = 30). For dose regimens, see Fig. 1 Figure 5 Recovery scores in horses following medetomidine–butorphanol–isoflurane (MB) or medetomidine– isoflurane (M) anaesthesia. For dose regimens, see Fig. 1. (Marntell & Nyman 1996). However, a larger field study in 54 ponies was not able to show any effect of butorphanol on the quality of anaesthesia induction (Corletto et al. 2005). Garcia Lascurain et al. (2006) demonstrated that different dose rates of butorphanol had the same effect on anaesthesia induction in horses so it is unlikely that a different dose of butorphanol in the present study would have influenced the results. In dogs, 0.4 mg kg)1 IV butorphanol decreased MAC by 20% (Ko et al. 2000) and 0.2 mg kg)1 IM butorphanol prevented a positive reaction to tail clamping during isoflurane anaesthesia for an average duration of 1.5 hours (Grimm et al. 2000). This effect was markedly prolonged to 2011 The Authors. Veterinary Anaesthesia and Analgesia 2011 Association of Veterinary Anaesthetists and the American College of Veterinary Anesthesiologists, 38, 186–194 Butorphanol CRI during medetomidine–isoflurane anaesthesia R Bettschart-Wolfensberger et al. 5.6 hours when butorphanol was combined with 5 lg kg)1 medetomidine (Grimm et al. 2000). Amongst equine anaesthesia experts there is no doubt that opioids act as analgesics in horses. Nevertheless their usefulness in combination with inhalation anaesthesia is under debate. Under experimental conditions MAC of inhalants is not reduced consistently (Matthews & Lindsay 1990; Steffey et al. 2003). In these studies some horses showed a decrease in MAC, others an increase and the remainders no effect at all. One study (Thomasy et al. 2006) showed that a relatively high dose of fentanyl did significantly reduce MAC of isoflurane, but when this study was repeated using the dose previously found effective, (Knych et al. 2009), reductions in MAC were no longer significant; nor were they consistent at even higher doses. Additionally, following these high doses of fentanyl, very poor quality recoveries were observed in some horses. Clinical studies that have investigated the use of opioids during inhalation anaesthesia are either of retrospective nature (Hofmeister et al. 2008) or were performed in a very small number of horses (Clark et al. 2005). Nevertheless, both studies provide some evidence that the intraoperative use of opioids during inhalation anaesthesia in horses is beneficial. Hofmeister et al. (2008) showed that following the administration of butorphanol to horses under isoflurane anaesthesia, the sympathetic response to surgical stimulation was reduced; he considered this to be a sign of a deeper plane of anaesthesia. In Clark et al.’s study (2005), the horses that received a morphine bolus followed by a morphine CRI during anaesthesia needed fewer additional anaesthetic drugs to maintain a stable plane of anaesthesia and prevent horses from purposeful movements during surgery. The combination of alpha-2 adrenoceptor agonists and opioids during inhalation anaesthesia has been previously investigated under experimental conditions (Bennett et al. 2004). These authors demonstrated that a bolus dose of xylazine decreased the MAC of halothane but the addition of morphine did not result in a further reduction. In our current study the addition of butorphanol to medetomidine did not result in a further reduction of isoflurane requirements when compared to medetomidine alone. However, cardiopulmonary function was not depressed by adding butorphanol. Butorphanol is a very potent antitussive (Westermann et al. 2005) and it is possible that this property led to a later reoccurrence of swallowing reflexes. This might be advantageous in cases of laryngeal surgery or in cases where horses need to be recovered with the trachea intubated. In conclusion, the addition of butorphanol to medetomidine sedation and to a medetomidine CRI in isoflurane anaesthetized horses did not show any significant effects on isoflurane requirements, cardiopulmonary function, recovery times or recovery quality. The only parameter which was influenced was time to extubation following anaesthesia which was longer in the butorphanol group. References Bennett RC, Steffey EP (2002) Use of opioids for pain and anesthetic management in horses. Vet Clin North Am Equine Pract 18, 47–60. Bennett RC, Steffey EP, Kollias-Baker C et al. (2004) Influence of morphine sulfate on the halothane sparing effect of xylazine hydrochloride in horses. Am J Vet Res 65, 519–526. Bettschart-Wolfensberger R, Bettschart R, Vainio O et al. (1999a) Cardiopulmonary effects of a two hour infusion of medetomidine and its reversal by atipamezole in horses and ponies. Vet Anaesth Analg 26, 8–12. Bettschart-Wolfensberger R, Clarke KW, Vainio O et al. (1999b) Pharmacokinetics of medetomidine in ponies and elaboration of a medetomidine infusion regime which provides a constant level of sedation. Res Vet Sci 67, 41–46. Bettschart-Wolfensberger R, Jaggin-Schmucker N, Lendl C et al. (2001) Minimal alveolar concentration of desflurane in combination with an infusion of medetomidine for the anaesthesia of ponies. Vet Rec 148, 264–267. Bettschart-Wolfensberger R, Picek S, Ringer S et al. (2008) Retrospective Report of Anesthesia Management Before and During Hydropool Recovery in 50 Horses. 14th IVECCS, Phoenix, USA, pp. 858 (abstract). Bidwell LA, Bramlage LR, Rood WA (2007) Equine perioperative fatalities associated with general anaesthesia at a private practice-a retrospective case series. Vet Anaesth Analg 34, 23–30. Clark LR, Clutton E, Blissitt KJ et al. (2005) Effects of perioperative morphine administration during halothane anaesthesia in horses. Vet Anaesth Analg 32, 10–15. Clarke KW, Paton BS (1988) Combined use of detomidine with opiates in the horse. Equine Vet J 20, 231–234. Clarke CW, England GCW, Gossens L (1991) Sedative and cardiovascular effects of romifidine, alone and in combination with butorphanol, in the horse. Vet Anaesth Analg 18, 25–28. Corletto F, Raisis AA, Brearley JC (2005) Comparison of morphine and butorphanol as pre-anaesthetic agents in combination with romifidine for field castration in ponies. Vet Anaesth Analg 32, 16–22. 2011 The Authors. Veterinary Anaesthesia and Analgesia 2011 Association of Veterinary Anaesthetists and the American College of Veterinary Anesthesiologists, 38, 186–194 193 Butorphanol CRI during medetomidine–isoflurane anaesthesia R Bettschart-Wolfensberger et al. Dzikiti TB, Hellebrekers LJ, Dijk P (2003) Effects of intravenous lidocaine on isoflurane concentration, physiological parameters, metabolic parameters and stress-related hormones in horses undergoing surgery. J Vet Med A Physiol Pathol Clin Med 50, 190– 195. Garcia Lascurain AA, Sumano Lopez H, Steffey EP (2006) The influence of butorphanol dose on characteristics of xylazine-butorphanol-propofol anesthesia in horses at altitude. Vet Anaesth Analg 33, 104–110. Grimm KA, Tranquilli WJ, Thurmon JC et al. (2000) Duration of nonresponse to noxious stimulation after intramuscular administration of butorphanol, medetomidine, or a butorphanol-medetomidine combination during isoflurane administration in dogs. Am J Vet Res 61, 42–47. Hofmeister EH, Mackey EB, Trim CM (2008) Effect of butorphanol administration on cardiovascular parameters in isoflurane-anesthetized horses - a retrospective clinical evaluation. Vet Anaesth Analg 35, 38–44. Kalchofner KS, Ringer SK, Boller J et al. (2006) Clinical assessment of anesthesia with isoflurane and medetomidine in 300 equidae. Pferdeheilkunde 22, 301–308. Knych HKD, Steffey EP, Mama KR et al. (2009) Effects of high plasma fentanyl concentrations on minimum alveolar concentration of isoflurane in horses. Am J Vet Res 70, 1193–1200. Ko JC, Lange DN, Mandsager RE et al. (2000) Effects of butorphanol and carprofen on the minimal alveolar concentration of isoflurane in dogs. J Am Vet Med Assoc 217, 1025–1028. Kohler I, Armbruster S, Lanz F et al. (2004) Analgesic effect of romifidine combined with butorphanol or levomethadone in the horse. A randomized, placebocontrolled experimental study. Tierarztl Prax Ausg Grosstiere Nutztiere 32, 345–349. Larenza MP, Ringer S, Kutter A et al. (2007) Recovery Quality Following Racemic Ketamine-Isoflurane in Comparison to S-Ketamine-Isoflurane Anaesthesia in Horses. BEVA (ed.). 46th BEVA conference, Edinburgh, UK, pp. 311 (abstract). Larenza MP, Ringer SK, Kutter AP et al. (2009) Evaluation of anesthesia recovery quality after low-dose racemic or S-ketamine infusions during anesthesia with isoflurane in horses. Am J Vet Res 70, 710–718. Marntell S, Nyman G (1996) Effects of additional premedication on romifidine and ketamine anaesthesia in horses. Acta Vet Scand 37, 315–325. Marntell S, Nyman G, Funkquist P (2006) Dissociative anaesthesia during field and hospital conditions for castration of colts. Acta Vet Scand 47, 1–11. Matthews NS, Lindsay SD (1990) Effect of low-dose butorphanol on halothane minimum alveolar concentration in ponies. Equine Vet J 22, 325–327. 194 Matthews NS, Hartsfield SM, Cornick JL et al. (1991) A comparison of injectable anesthetic combinations in horses. Vet Surg 20, 268–273. Mee AM, Cripps PJ, Jones RS (1998) A retrospective study of mortality associated with general anaesthesia in horses: elective procedures. Vet Rec 142, 275–276. Ringer SK, Kalchofner K, Boller J et al. (2007) A clinical comparison of two anaesthetic protocols using lidocaine or medetomidine in horses. Vet Anaesth Analg 34, 257– 268. Ringer S, Portier K, Hérbert P et al. (2009) Development of a Romifidine Constant Rate Infusion (With or Without Butorphanol) for Standing Sedation of Horses. AVA spring meeting, Helsinki, Finland, pp. 27 (abstract). Ringer S, Portier K, Gaudefroy T et al. (2011) Development of a xylazine constant rate infusion with or without butorphanol for standing sedation of horses. Vet Anaesth Analg, in press. Schatzman U, Armbruster S, Stucki F et al. (2001) Analgesic effect of butorphanol and levomethadone in detomidine sedated horses. J Vet Med A Physiol Pathol Clin Med 48, 337–342. Steffey EP, Howland D (1980) Comparison of circulatory and respiratory effects of isoflurane and halothane anesthesia in horses. Am J Vet Res 41, 821–825. Steffey EP, Eisele JH, Baggot JD (2003) Interactions of morphine and isoflurane in horses. Am J Vet Res 64, 166–175. Taylor PM, Browning AP, Harris CP (1988) Detomidinebutorphanol sedation in equine practice. Vet Rec 123, 388–390. Thomasy SM, Steffey EP, Mama KR et al. (2006) The effects of i.v. fentanyl administration on the minimum alveolar concentration of isoflurane in horses. Br J Anaesth 97, 232–237. Valverde A, Gunkelt C, Doherty TJ et al. (2005) Effect of a constant rate infusion of lidocaine on the quality of recovery from sevoflurane or isoflurane general anaesthesia in horses. Equine Vet J 37, 559–564. Valverde A, Rickey E, Sinclair M et al. (2010) Comparison of cardiovascular function and quality of recovery in isoflurane-anaesthetised horses administered a constant rate infusion of lidocaine or lidocaine and medetomidine during elective surgery. Equine Vet J 42, 192–199. Westermann CM, Laan TT, van Nieuwstadt RA et al. (2005) Effects of antitussive agents administered before bronchoalveolar lavage in horses. Am J Vet Res 66, 1420–1424. Yamashita K, Muir WW 3rd, Tsubakishita S et al. (2002) Infusion of guaifenesin, ketamine, and medetomidine in combination with inhalation of sevoflurane versus inhalation of sevoflurane alone for anesthesia of horses. J Am Vet Med Assoc 221, 1150–1155. Received 16 June 2010; accepted 2 August 2010. 2011 The Authors. Veterinary Anaesthesia and Analgesia 2011 Association of Veterinary Anaesthetists and the American College of Veterinary Anesthesiologists, 38, 186–194
Anuncio
Documentos relacionados
Descargar
Anuncio
Añadir este documento a la recogida (s)
Puede agregar este documento a su colección de estudio (s)
Iniciar sesión Disponible sólo para usuarios autorizadosAñadir a este documento guardado
Puede agregar este documento a su lista guardada
Iniciar sesión Disponible sólo para usuarios autorizados