Medicaid Buy-In Program for Working People With Disabilities (MBI
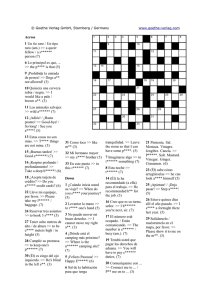
Anuncio
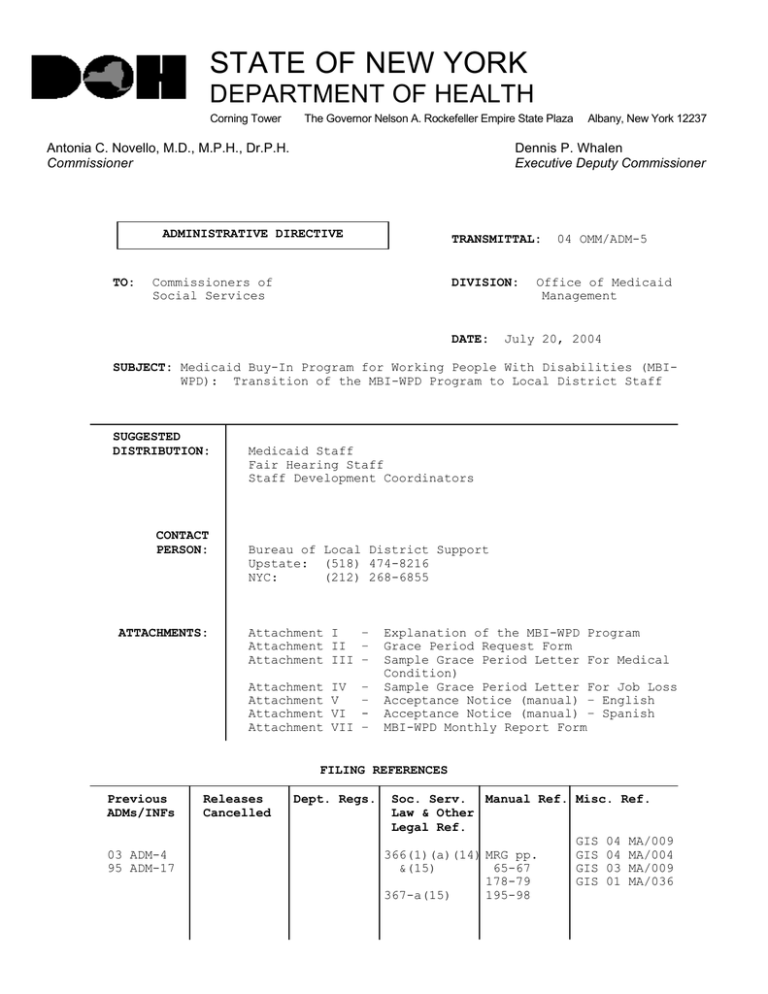
STATE OF NEW YORK DEPARTMENT OF HEALTH Corning Tower The Governor Nelson A. Rockefeller Empire State Plaza Antonia C. Novello, M.D., M.P.H., Dr.P.H. Commissioner Dennis P. Whalen Executive Deputy Commissioner ADMINISTRATIVE DIRECTIVE TO: Albany, New York 12237 TRANSMITTAL: Commissioners of Social Services DIVISION: DATE: 04 OMM/ADM-5 Office of Medicaid Management July 20, 2004 SUBJECT: Medicaid Buy-In Program for Working People With Disabilities (MBIWPD): Transition of the MBI-WPD Program to Local District Staff SUGGESTED DISTRIBUTION: CONTACT PERSON: ATTACHMENTS: Medicaid Staff Fair Hearing Staff Staff Development Coordinators Bureau of Local District Support Upstate: (518) 474-8216 NYC: (212) 268-6855 Attachment I – Attachment II – Attachment III – Attachment Attachment Attachment Attachment IV V VI VII – – – Explanation of the MBI-WPD Program Grace Period Request Form Sample Grace Period Letter For Medical Condition) Sample Grace Period Letter For Job Loss Acceptance Notice (manual) – English Acceptance Notice (manual) – Spanish MBI-WPD Monthly Report Form FILING REFERENCES Previous ADMs/INFs 03 ADM-4 95 ADM-17 Releases Cancelled Dept. Regs. Soc. Serv. Manual Ref. Misc. Ref. Law & Other Legal Ref. GIS 04 MA/009 366(1)(a)(14) MRG pp. GIS 04 MA/004 &(15) 65-67 GIS 03 MA/009 178-79 GIS 01 MA/036 367-a(15) 195-98 Date: July 20, 2004 Trans. No. 04 OMM/ADM-5 Page No. 2 320 Date: July 20, 2004 Trans. No. 04 OMM/ADM-5 Page No. 3 I. PURPOSE The purpose of this Administrative Directive is to provide Local Departments of Social Services (LDSS) with the plan for transition of eligibility determinations and full data entry for the MBI-WPD program to LDSS staff effective July 1, 2004. Sections 62-69 of Part A of Chapter 1 of the Laws of 2002 established the Medicaid Buy-In program for Working People with Disabilities (MBI-WPD) that extends Medicaid coverage to working applicants/recipients (A/Rs) with disabilities who have net incomes at or below 250% of the Federal Poverty Level (FPL) and non-exempt resources at or below $10,000. Administrative Directive (ADM) 03 OMM/ADM-4, issued on June 9, 2003, advised LDSS of the interim implementation plan for the MBI-WPD program that began July 1, 2003. Under the interim plan, eligibility determinations have been made by staff at the New York State Department of Health. There has been no systems support for automated premium collection and tracking; therefore, a moratorium on premium payment has been in effect. Because the automated Premium Payment Collection and Tracking (PPCT) system is not yet operational, the moratorium on premium collection continues. Once the PPCT system is operational, further instructions will be forthcoming. II.BACKGROUND Chapter 1 of the Laws of 2002 enacted two new categorically needy Medicaid groups under the MBI-WPD program in New York State, by adding two new subparagraphs (12) and (13) to Section 366.1(a) of the Social Services Law (SSL). A new subdivision (12) to Section 367-a of SSL provides for the payment of premiums for certain participants based on net available income. The MBI-WPD program is intended as a work incentive for persons with disabilities (including blindness). Since July 1, 2003, LDSS staff and the Inter-Agency Team (IAT) at the Office of Medicaid Management (OMM) Albany Central Office (ACO) have shared responsibility for implementation of the MBI-WPD program (see 03 OMM/ ADM-4). LDSS staff accepts applications and performs undercare and recertification functions and ACO staff performs eligibility determinations and full data entry. On July 1, 2004 the responsibility for implementation of the MBI-WPD program, including eligibility determinations and full data entry for new cases and spenddown conversion cases, will transition to the LDSS. Negotiations with a vendor are underway to provide premium collection and tracking for the MBI-WPD program but the contract will not be complete at the time the transition takes place. Therefore, the moratorium on premium payment and tracking continues. III.PROGRAM IMPLICATIONS A. Eligibility Requirements for the Medicaid Buy-In Program for Working People with Disabilities: Two Groups As stated in 03 OMM/ADM-4, effective July 1, 2003, two new eligibility groups were established for the MBI-WPD program: the Date: July 20, 2004 Trans. No. 04 OMM/ADM-5 Page No. 4 Basic Coverage group and the Medical Improvement group. To be eligible for either group, an A/R must have a disability that meets Date: July 20, 2004 Trans. No. 04 OMM/ADM-5 Page No. 5 the medical criteria for Supplemental Security Income (SSI) established by the Social Security Administration (SSA) but have too much income to qualify for SSI. Basic Coverage Group In addition to the usual Medicaid rules, the requirements that apply to the Basic Coverage group are: • • • • • • Age - The A/R must be at least 16 years of age, but under the age of 65. Work – The A/R must be engaged in a work activity for which they receive financial compensation and pay all applicable state and federal income and payroll taxes (see Required Action section for verification of Sheltered Workshop employees work). Disability – The A/R must have certification of disability. Income – The A/R must have total net income at or below 250% of the FPL. If net income is at or above 150% of the FPL but does not exceed 250% of the FPL, a premium payment will be required. Note: SSI-related budgeting, including allocation and deeming, is used for determining net available income and resources. Resources – Non-exempt resources cannot exceed $10,000. Premium Payment - The premium is 3% of net earned income plus 7.5% of net unearned income (after SSI-related budgeting methodology is applied). Individuals with net income below 150% of the FPL pay no premium. Note: A moratorium on premium payments is effective until such time as systems support for an automated premium collection and tracking become available. Medical Improvement Coverage Group In addition to the usual Medicaid rules, the requirements that apply to the Medical Improvement group are: • • • • A new applicant is NEVER placed in the Medical Improvement Group. The individual must first be in receipt of coverage through the Basic Group and lose eligibility for that group as a direct and specific result of medical improvement (see Disability requirement below). Age - The A/R must be at least 16 years of age but under the age of 65. Work – The A/R must be engaged in a work activity for which financial compensation is received and all applicable state and federal income and payroll taxes are paid (see Required Action section for verification of Sheltered Workshop employees work). A recipient in the Medical Improvement Group must be employed at least 40 hours per month and earn at least the federally required minimum wage. Disability – The recipient’s disability determination (performed by the State Disability Review Team in Albany as a Continuing Disability Review) indicates that the individual is no longer disabled but retains a severe medically determined impairment. Date: July 20, 2004 Trans. No. 04 OMM/ADM-5 • • • Page No. 6 Income – The A/R must have a total net income that is at or below 250% of the FPL. If net income is at or above 150% of the FPL but does not exceed 250% of the FPL, a premium payment will be required. Note: SSI-related budgeting, including allocation and deeming, is used for determining net available income and resources. Resources – The A/R’s non-exempt resources cannot exceed $10,000. Premium Payment - The premium is 3% of the net earned income plus 7.5% of net unearned income (after SSI-related budgeting methodology is applied). Individuals with net income below 150% of the FPL pay no premium. Note: A moratorium on premium payments is effective until such time as systems support for an automated premium collection and tracking is available. B. Managed Care MBI-WPD applicants who wish to participate in Managed Care may opt to enroll if their net income is less than 150% FPL. MBI-WPD participants with income between 150% and 250% FPL are excluded from Managed Care even in districts with mandatory Managed Care programs. C. Cost Shares Cost shares for MBI-WPD participants will be at the regular cost share rate of 50% federal, 25% State and 25% local, and 50% federal, 40% State and 10% local for Long Term Care costs, with no local administrative costs. Local districts must use the revised schedule D-4 to claim administrative costs for the MBI-WPD program. D. Premium Payment Collection and Tracking (PPCT) System: Subsystem A New WMS A new Welfare Management System (WMS) subsystem is under development to hold data specific to premium collection and tracking for the MBI-WPD program. A systems interface is also under development to supply necessary information to the selected Premium Payment Collection and Tracking System vendor, who will be responsible for mailing premium bills/coupons, some notices and letters and for the necessary tracking functions for the MBI-WPD program. Once the automated PPCT system is operational, the contracted PPCT system vendor will report to the OMM and LDSS according to a prearranged schedule. Information regarding this system will follow at a later date. E. Application Process This section addresses application forms, the face-to-face interview and coverage codes for the MBI-WPD program. Application Forms The following application forms are accepted for the MBI-WPD program: • LDSS-2921 “Application for Public Assistance/Medical Assistance/Food Stamps/Services” • Medicaid Renewal (Recertification) Form • Access New York Health Care Form DOH-4220 Date: July 20, 2004 Trans. No. 04 OMM/ADM-5 Page No. 7 Local district staff is reminded that an MBI-WPD application form, whether the applicant is new or currently on spenddown, must be accompanied by current documentation of items subject to change, such as employment. If an applicant is currently on spenddown, the client’s most recent application or renewal form will be accepted as long as it was filed within the last six months. If it has been more than six months since the application was completed, a new form must be submitted. Face-to-Face Interview The LDSS must schedule and conduct the face-to-face interview with the applicant or his/her representative and during the interview: • • • • Discuss the availability of Impairment Related Work Expenses (IRWEs) deductions and Plan for Achieving Self-Support (PASS) accounts with the A/R. Provide the applicant with a copy of the “Explanation of the MBIWPD Program” (see Attachment I of this ADM). Verify age, work and disability status (see Required Actions for each of these requirements). Determine if disability certification is needed. If a disability determination is needed, local district staff must request medical documentation from the applicant’s medical providers (see Required Actions for disability determinations process). Coverage Codes That Apply Based on Resource Documentation The August 2004 systems migration for Attestation of Resources will include new coverage codes that will apply to the MBI-WPD program based on resource documentation provided. These coverage codes will appear in a separate ADM that will be released in the near future. See the Systems Implications section of this ADM for coverage codes that apply until attestation of resources is implemented. IV.REQUIRED ACTION As of July 1, 2004, the LDSS will be responsible for implementation of the MBI-WPD program. The application process will continue as directed in the Interim Implementation plan; however, as stated in GIS MA/004, the Access New York Health Care form DOH-4220 or the CNS generated Medicaid Renewal (Recertification) Form, if completed within six months of the request for participation in the MBI-WPD program, may now be used in addition to the LDSS-2921 “Application for Public Assistance/Medical Assistance/Food Stamps/Services” form. The face-to-face interview continues to be a requirement of application as does verification of the specific eligibility requirements. A. Age Requirement An applicant for the but under the age of age or older, she/he Documentation of age MBI-WPD program must be at least 16 years of age, 65. If the applicant is under 16 or 65 years of is not eligible for the MBI-WPD program. is necessary at the time of application or renewal. Date: July 20, 2004 Trans. No. 04 OMM/ADM-5 Page No. 8 If the A/R’s 65th birthday occurs within 12 months of the date of application or renewal, coverage under the MBI-WPD program must end on the last day of the month of the individual’s 65th birthday. The worker Date: July 20, 2004 Trans. No. 04 OMM/ADM-5 Page No. 9 must discuss this with the individual at the time of application or renewal and shorten the authorization period accordingly. B. Work Requirement If an applicant is not currently working, LDSS staff should offer a referral to VESID or to a Benefits Planner. Until the applicant is working, he/she cannot participate in the MBI-WPD program and must instead be evaluated for Medicaid under other programs, such as spenddown. Acceptable proof of work includes an A/R’s: current pay stub(s), pay check(s) or a written statement from the employer. When these are not available the A/R’s income tax return, W-2 form, or records of bank deposits may be used. Sheltered Workshop 03 OMM/ADM-4 states that, “the A/R must be engaged in a work activity for which they receive financial compensation and pay all applicable state and federal income and payroll taxes.” However, some sheltered workshop employees are tax blocked and for these individuals, although they may have pay stubs or a detailed statement of earnings from their employer, taxes are not deducted from their pay. In this case the tax requirement is not applicable and the pay stubs or employer’s detailed statement of work may be used to verify work. In these instances the detailed statement of earnings from the employer or current pay stubs is considered acceptable proof of work. Self-Employment The Medicaid Reference Guide (MRG) may be used for guidance regarding self-employment verification. The MRG contains information on verification of small business, farm income, partnerships and corporations, as well as instructions for estimating net earnings from self-employment and determining net profits. Applicants for the MBI-WPD program who are self-employed in their own business are not required to show a profit but must submit documentation as detailed in the MRG. Grace Periods A grace period is a time period during which a MBI-WPD program participant is not working but remains eligible for the program. Grace periods are a way of recognizing the fact that persons with disabilities may have periods of increased or decreased ability to work for medically verifiable or other reasons that require special consideration. Recipients may be granted multiple grace periods during a 12-month period; however, in no event may the sum of the grace periods exceed six months in the 12-month period. Two types of grace periods may be granted: 1. Change in Medical Condition: A grace period of up to six months will be allowed if, for medical reasons, the MBI-WPD participant is unable to continue working. Medical verification will be required. When an applicant requests this type of grace period, LDSS must request medical verification. 2. Job Loss (through no fault of participant): A grace period of up to six months will be allowed if, through no fault of the participant, job loss is suffered i.e., due to layoff, etc. Verification is required. Districts must verify that the Date: July 20, 2004 Trans. No. 04 OMM/ADM-5 Page No. 10 recipient is reasonably expected to return to employment, for example, a temporary layoff, or that the recipient is actively Date: July 20, 2004 Trans. No. 04 OMM/ADM-5 Page No. 11 seeking new employment. An individual who is in receipt of unemployment insurance, who was let go from a job related to behavior resulting from the individual’s disability, is considered eligible for a job loss grace period as the individual lost employment through no fault of their own. Receipt of unemployment insurance implies that the individual is actively seeking new employment. Note: MBI-WPD participants reporting job loss due to non-medical reasons should be referred to One-Stop Centers, Vocational and Educational Services for Individuals with Disabilities (VESID) and Benefits Planning Assistance & Outreach (BPA&O) services as applicable, so that assistance with employment may be sought prior to loss of eligibility in the program. If an individual loses eligibility for the MBI-WPD program due to job loss or medical condition that exceeds the six-month allowable grace period, the individual may reapply for the program without completing a new application form for up to 30 days following discontinuance. However, verification of return to work is needed. The current process for grace periods, which will carry over for the transition, is as follows: • • • • • A recipient must complete a MBI Grace Period Request form (see Attachment II to this ADM). The recipient must return the form with the required documentation to the LDSS. The required documentation must support the request for a grace period by detailing why the recipient is out of work and how long they will be out. o Change in medical condition supporting documentation must detail the current health problem, treatment and the time period that the recipient will be out of work. It must be provided by a Medical Doctor or primary care practitioner. o Job Loss documentation includes a layoff notice or a statement from the Department of Labor, VESID, etc. Each grace period request is reviewed along with the supporting documentation. o The grace period is approved by the LDSS for the time period requested by the recipient, unless the approval would result in the recipient exceeding the six-month maximum grace period. Remember, the 12 month tracking period for grace periods starts with the first day of the first awarded grace period. At the end of the 12 months, a new 12 month tracking period starts. The 12 month tracking period is independent of the authorization period and is not tied to the authorization period. The signed notice of decision is sent to the recipient. The LDSS must return the completed request form to the recipient within 10 working days. Two model notices, one for each type of grace period, are included as Attachments III and IV of this ADM. One of these letters should be sent to a recipient when the district sends the signed grace period decision to the recipient. The letters inform the recipient of the necessary steps that will be required of them as the grace period draws to a close. Date: July 20, 2004 Trans. No. 04 OMM/ADM-5 Page No. 12 Beginning July 1, 2004 local districts will need to keep track of grace periods by either using a “tickler file” or database to make sure the recipient doesn’t exceed the six month grace period limit. The Office of Medicaid Management has a database that may be used for this purpose. If your district would like a copy of this database, you may e-mail a request to: [email protected] C. Disability Requirement Proof of Disability Applicants must provide proof of disability. Acceptable proof of disability for initial application in the MBI-WPD program include: • • An award letter from the Social Security Administration for Social Security Disability Insurance (SSDI) benefits or other proof of receipt of SSDI benefits, such as a check or bank deposits listing the benefit. A Medicare card is also considered acceptable proof. An existing State or Local Disability Review Team certification at initial application for the MBI-WPD program. Note: If the individual does not have existing certification of disability at the time of initial application, a disability determination must be performed by the State Disability Review Team in Albany. New Disability Determinations Local districts are reminded of their continuing responsibility to assist an A/R in establishing proof of disability or continuing disability. Medicaid applicants with an alleged disability, who are working and earning Substantial Gainful Activity (SGA) must be considered for a disability determination and informed of the MBI-WPD program. It is not appropriate to exclude these individuals from the first step of the sequential evaluation for disability. If an individual is working and alleges a disability but does not have acceptable proof of disability, the LDSS must: • • Discuss the MBI-WPD program with the individual and give them the written explanation of the program. Have the individual sign the appropriate release of medical documentation forms. Note: During the interim implementation period, counties requested that medical providers send evidence directly to the Albany Central Office. Beginning July 1, 2004, medical evidence is to be sent to the local district. The letter requesting medical evidence from treating sources should be modified to include the appropriate local district address to insure that medical evidence is sent to the local district and not to the Albany Central Office. Only a complete disability package will be sent to the State Disability Review Team in Albany. In the case of No Actions, the LDSS will be sent the completed DSS-639 with details of medical documentation needed. The district must make every effort to assist in obtaining the requested information and Date: July 20, 2004 Trans. No. 04 OMM/ADM-5 Page No. 13 carefully document the efforts in the applicant’s file. If the medical provider is unwilling or unable to provide the requested Date: July 20, 2004 Trans. No. • • • • • 04 OMM/ADM-5 Page No. 14 documentation, a consultative exam will be required (see Consultative Exam section below). If the requested documentation is not received after several attempts or if the applicant fails to comply with two consultative examination dates, the local district will deny the MBI-WPD application for failure to provide documentation. Note: It is important that attempts to obtain medical documentation and contacts with the applicant regarding consultative examination dates be carefully documented by local district staff. Complete the DSS-1151 interview form during the face-to-face interview and create a list of all treating sources (physicians, psychologists, hospitals, therapists, counselors, etc.). Utilize the DSS-486T forms and a copy of the release of medical evidence form to obtain medical evidence from all treating sources for a period up to 12 months prior to the date of application and cover the timeframe for which the disability determination is being sought. Be sure to send the treating physician a Functional Capacity Assessment form (page 2 of the DSS-486T). As medical evidence is received, a disability package is created consisting of: o The completed DSS-1151 o Applicable portions of the DSS-486T, signed by a Medical Doctor or qualified Psychologist (as applicable) o All requested medical evidence Complete a MBI-WPD Transmittal sheet with 2 copies placed on the front of the disability packet. Mail the complete disability packet to: MBI-WPD Coordinator Division of Consumer and Local District Relations NYS Department of Health Office of Medicaid Management One Commerce Plaza, Room 728 Albany, New York 12260 When the disability determination is complete, the State Disability Review Team in Albany will send a copy of the Disability Review Team Certificate (DSS-639), along with a copy of the submitted disability packet, to the local district. A DSS-4141 “Notice of Medical Assistance Disability Determination” will be included with the completed disability determination package that is returned to the LDSS. The State Disability Review Team will complete the determination portion of the form. Local district staff is responsible for filling in districtspecific information, including county name, address telephone number. Note: The local district must fill in a telephone number that the applicant may call to request a copy of the DSS-639 disability determination decision. The local district must send a copy of the completed DSS-4141 form to the applicant and retain a copy of the completed notice in the client’s record. Consultative Exams If an applicant does not have a medical treating source or the treating source is unwilling or unable to provide necessary medical information for a disability determination, the local district must arrange a consultative exam. Regulations at 18NYCRR 360-5.5 provide that the local district must pay for the cost of such examinations, consultations Date: July 20, 2004 Trans. No. 04 OMM/ADM-5 Page No. 15 and tests required by the disability review team when they indicate that more information is needed. These costs are subject to reimbursement as an administrative expense, whether or not the applicant is subsequently determined disabled. Federal financial participation shall be claimed for such expenditure even if the client is subsequently determined not disabled. However, as previously stated, there are no local administrative costs for the MBI-WPD program. Continuing Disability Review All Continuing Disability Reviews (CDR) for all working individuals, regardless of their participation in the MBI-WPD program, must now be performed by the State Disability Review Team, even if the local district performs its own disability determinations. This applies to all such individuals, even those not currently participating in the MBIWPD program. The local district prepares the CDR packet by contacting all known medical providers for current medical evidence. District workers will use the existing Disability Review Team Certificate (DSS-639) and the Disability Interview (DSS-1151) form as a guide in preparing the continuing disability review packet. Once the new medical evidence is received, the CDR packet is sent to the State Disability Review Team in Albany, MBI-WPD Coordinator (see instructions and address under “New Disability Determinations” section above). Upon completion of the continuing disability review, the State Disability Review Team will send the district a copy of the Disability Review Team Certificate (DSS-639), the medical evidence package and the DSS-4141. The DSS-4141 will be completed by the LDSS and sent to the recipient. The LDSS retains a copy of the DSS-4141 in the client record. Note: New disability determinations for A/Rs who are not working and/or not applying for the MBI-WPD program and Continuing Disability Reviews for recipients who are not working will continue to be performed by the responsible (State or local) review team. Assignment of Applicant to Basic or Medical Improvement MBI Group The only instance in which the local district may assign an individual to the MBI-WPD Basic Group is if a new applicant is in an existing approval period for disability certification at the time of application. If, at the time of new application, the individual is in receipt of SSDI or if the individual is in a disability approval period that was determined by the State or Local Disability Review Team, the individual may be placed in the MBI-WPD Basic Group by the local district if otherwise eligible for the program and working. In all other instances, the State Disability Review Team assigns the MBI group for which the A/R is eligible. If an applicant is not in receipt of SSDI benefits or is not currently determined disabled or is in the MBI-WPD program and a CDR is indicated, the disability determination must be made by the State Disability Review Team in Albany. The State Disability Review Team will notify the local district if the applicant is to be considered for eligibility in the Medical Improvement Group. Date: July 20, 2004 Trans. No. 04 OMM/ADM-5 D. Financial Requirements: Page No. 16 Income and Resources Regular SSI-related budgeting rules will be used to determine an individual’s net available monthly income and countable resources. This includes applying all SSI-related income and resource disregards and allocation and deeming, when applicable. Local district staff is reminded that as for all SSI-related cases, the individual’s non-medical Impairment Related Work Expenses (IRWEs) may be disregarded (see Medicaid Reference Guide pages 195 –198 and the December 10, 2003 videoteleconference on IRWEs and PASS). We anticipate that some of the applicants will be seeking Plans to Achieve Self Support (PASS) accounts, which are disregarded for purposes of determining SSI-related A/R’s Medicaid eligibility (see Medicaid Reference Guide pages 178-179, 200-201 and 320 and the December 10, 2003 video-teleconference on IRWEs and PASS). Procedures for establishing household size for MBI-WPD will be the same as for regular SSI-related budgeting. The individual’s net available income, after applying all disregards and exemptions, will be compared to 150% or 250% of the FPL for a household of one or two. If an A/R’s income exceeds 250% of the FPL, the A/R is determined ineligible for the MBI-WPD program. If an A/R’s net available monthly income is at or below 250% of the FPL and countable resources are at or below the $10,000 resource standard (regardless of household size), the A/R will be financially eligible for Medicaid coverage under the MBI-WPD program. A/Rs cannot spenddown income to 250% of the FPL and qualify for coverage under the MBI-WPD program. Additionally, countable resources must be at or below the $10,000 resource standard as of the first of the month in which coverage is sought. E. Social Security Administration Programs: (SSI) 1619(a) and 1619(b) Programs Supplemental Security Income The LDSS is reminded that if an individual is active on a Supplemental Security Income (SSI) case, the individual receives automatic Medicaid and is not eligible for the MBI-WPD program. If the individual is notified by the Social Security Administration that their SSI case will terminate, that individual must have a separate Medicaid eligibility determination, including a determination of eligibility under the MBIWPD program. Medicaid coverage must continue until a separate eligibility determination for Medicaid is made. All criteria must be met for the MBI-WPD program in order for an individual to be found eligible for the program. The most likely scenario will be that the individual has been participating in SSA’s 1619(b) program and has reached the income threshold for participation in that program. Another likely scenario would be one in which the individual exceeds the resources amount allowed by SSI. The LDSS is reminded that the resources level for the MBI-WPD program is $10,000 for an individual or a couple. F. Medicaid Managed Care Medicaid Managed Care is a voluntary option only for those MBI-WPD recipients who are income eligible under 150% of the FPL. Pursuant to statute, all other MBI-WPD recipients are excluded from managed care. In districts where enrollment in a managed care plan is mandatory, individuals in the MBI-WPD program cannot be required to enroll. It Date: July 20, 2004 Trans. No. 04 OMM/ADM-5 Page No. 17 should be noted that individuals in receipt of Medicare, regardless of income level, are excluded from enrollment in managed care at this time. Date: July 20, 2004 Trans. No. 04 OMM/ADM-5 Page No. 18 G. Premium Payments MBI-WPD participants with net (earned and unearned) income between 150% and 250% of the FPL shall be required to pay a monthly premium for Medicaid coverage based on a percentage of their earned and unearned income. However, due to the unavailability of an automated premium collection and tracking system for the MBI-WPD program, a moratorium exists on premium collection until the automated system is completed. H. Co-Pays All applicable Medicaid co-pays continue to apply for MBI-WPD program participants. Co-pays apply in addition to any premium payment the participant makes. I. Notices The LDSS is to provide the individual with a copy of the “Explanation of the MBI-WPD Program” (see Attachment I of this ADM). CNS and manual notices have been developed. Manual Acceptance notices in English and Spanish are Attachments V and VI of this ADM. These manual notices must be used until further instructions are issued. CNS notices are in development and instructions for use will be forthcoming. J. Reimbursement of Spenddown Individuals transitioned from spenddown to the MBI-WPD program are eligible for reimbursement of any spenddown amount paid in the three months prior to the MBI-WPD application if the eligibility determination indicates that the individual was eligible for the MBI-WPD program during that retroactive period. The usual procedures for retroactive coverage apply. K. Third Party Health Insurance All Third Party Health Insurance rules that are used for Medicaid apply for the MBI-WPD program. L. MBI-WPD Recertification/Renewal MBI-WPD recertifications/renewals must be carefully screened to insure that all MBI-WPD eligibility requirements are met. Current employment must be verified. District workers must see current pay stubs or other acceptable verification of work (per the MRG) or the case cannot be recertified for the MBI-WPD program. The district worker must also attend to the applicant’s current age and remember to discuss the age requirement if the individual’s 65th birthday will be attained within 12 months from recertification. The authorization period must be adjusted accordingly. Disability certification must also be verified. If the expiration date on the certification falls within 12 months of the date of recertification, a Continuing Disability Review (CDR) is necessary and a disability packet must be initiated for review by the State Disability Review Team in Albany. Individuals recertifying/renewing for the MBI-WPD program must continue to be income and resource eligible. Date: July 20, 2004 Trans. No. 04 OMM/ADM-5 Page No. 19 M. Co-Op Cases There is no longer a need for separation of an MBI-WPD individual from other members of the household on a co-op case. Use of the appropriate Individual Category Code (see Systems Implications) when performing data entry for an MBI-WPD individual allows identification of MBI-WPD participants for DOH OMM federal reporting purposes. Therefore, it is no longer imperative that the SSI-related budget be stored separately from any other budget(s) for the household. N. LDSS Reporting Requirements Due to federal reporting requirements, select MBI-WPD data must be reported monthly by all local districts. Local district staff must use the MBI-WPD Monthly Report form (see Attachment VII) to report necessary data. The report form must be received in the Albany Central Office by the fifth day of every month and cover data for the previous month. The form may be submitted via U.S. mail to the MBI-WPD Coordinator or by email to: [email protected] V. SYSTEMS IMPLICATIONS A. New York City New York City systems instructions will follow under separate cover. B. Upstate Systems codes and edits which were modified to support the interim implementation of the MBI-WPD program are available to LDSS. A description of the items below can be found in the WMS/CNS Coordinator Letter and the MBL transmittal that we issued that describes the July 21, 2003 WMS migration of the MBI-WPD program. Note: In the near future, Resource Attestation codes will apply for the MBI-WPD program. A separate Administrative Directive will be issued to address resource attestation. 1. WMS Changes A. Effective with the July 21, 2003 Migration Individual Categorical Codes Two new Individual Categorical Codes have been added for identification and Federal/State/Local claiming purposes: 70 Medicaid Buy-In – Disabled Basic Group 71 Medicaid Buy-In – Medically Improved Codes 70 and 71 are allowed in Case Type 20 only. If the Individual Categorical Code is 70 or 71, the Medicaid Coverage Code must be 01, 10 or 30. Date: July 20, 2004 Trans. No. 04 OMM/ADM-5 Page No. 20 If the Individual Categorical Code is 70 or 71, the individual must be between 16 and 64 years of age. Restriction/Exception Codes Two Restriction/Exemption codes for Managed Care will apply: 90 Managed Care Excluded will be used for those individuals with a net income between 150% and 250% FPL. 91 Managed Care Exempt will be used for those individuals with a net income that is below 150% FPL who choose not to be in managed care. Corresponding AID Categories Two AID category codes apply: 82 Medicaid Buy-In Disabled Basic Group 83 Medicaid Buy-In Medically Improved Group These AID Categories have been added for reporting purposes. 2. MBL Implications Effective for MBL budgets with a From Date of July 1, 2003 or after, two new EEC Codes are available for the MBI-WPD program: “V” – MBI-WPD(SSI–related budgeting prior to MBI-WPD) “W” – MBI-WPD(MBI budget only) The new EEC codes are valid for Budget Types 04, 05 and 06. In addition, a new field entitled “PASS” is available to enter income that is to be disregarded in accordance with an approved Plan for Achieving Self-Support. When an EEC Code of V or W is entered, the SSI-Related Total Net Income minus PASS amount is used to calculate eligibility for the MBI-WPD program. The FPL table used is based on the Living Arrangement Codes of 1 or 2 (not number in case) and whether a non SSI-related spouse has sufficient income remaining after allocation to any non-disabled children in the household. MBI-WPD total net income after applying all SSI-related income disregards is compared to 150% of the FPL and 250% of the FPL. The second EEC screen will display the Net Income and a Medicaid Buy-In section with one of the following messages: Eligible Eligible Ineligible Income Ineligible Resources Ineligible Income/Resources For an EEC of 150% 250% 250% 250% $ $ $ $ $ Amount Amount Amount 10,000 Amount/$10,000 “V” or “W”, the Resource test is $10,000. Date: July 20, 2004 Trans. No. 04 OMM/ADM-5 Page No. 21 3. CNS Changes Numerous additions to the CNS Denial, Closing and Undercare codes were implemented to accommodate the MBI-WPD program. The notices are available and may be found in the WMS/CNS Coordinator Letter and the MBL transmittal that were issued to describe the July 2003 WMS migration of the MBI-WPD program. VI. EFFECTIVE DATE July 1, 2004 ______________________________________ Kathryn Kuhmerker, Deputy Commissioner Office of Medicaid Management Attachment I Explanation of the Medicaid Buy-In Program For Working People with Disabilities (MBI-WPD) The MBI-WPD program offers people with disabilities who are working the chance to buy Medicaid health care coverage. The Medicaid Buy-In program works much like any insurance program. Currently, no premium will be charged for this coverage, however, in the future you may be asked to pay a monthly premium. The amount of your premium will be based on your income. To qualify for the Medicaid Buy-In program, you must: • Be certified disabled by either the Social Security Administration (SSA) or State or County Medical Review Team • Live in New York State • Be at least 16 but under 65 years of age, and be a U.S. Citizen, a National, a Native American or an Immigrant with satisfactory immigration status • Work in a paid position for which all applicable State and Federal income and payroll taxes are paid • Meet the income and resource limits (see below) • Pay a premium, if required If you have applied for Medical Assistance, the local department of social services worker will tell you if you meet the eligibility requirements for full Medicaid coverage under the MBI-WPD program. Participation in this program is voluntary. Budgeting Special budgeting rules (called methodology) are used to figure the amount of your income and resources that will be counted to decide if you are eligible for the MBI-WPD program. We will not count all of your income and resources. See the Income and Resources sections below for an explanation. Income Because of the special budgeting rules that are used, the amount of your income that is counted may be considerably less than your gross income. Income is defined as anything a person receives that can be used to buy food, clothing or shelter. All of your income (earned and unearned) will be considered. If your spouse is not disabled, his/her income may also be considered. Examples of earned income are wages, salary, and compensation for work for which financial compensation is received and all applicable State and Federal income and payroll taxes are paid. Examples of unearned income are Social Security disability or retirement benefits, interest, or dividends. The income that is counted after the special budgeting rules are applied is called your net income. Under the MBI-WPD program, if your net income is less than 150% of the FPL, you will receive full Medicaid coverage without paying a premium. If your net income is equal to or above 150% of the Federal Poverty Level (FPL), you will have to pay a premium for the coverage. If your net income is above 250% of the FPL, you will be determined ineligible for Medicaid under this program. A premium payment will not be required at this time. However, in the future New York State Medicaid may implement a premium payment if your net income is between 150% and 250% of the Federal Poverty Level. You will be notified when the premium payment requirement becomes effective. If you already get Medicaid at no cost because you qualify through another program (such as persons receiving SSI, or those in the 1619 (a) or (b) program) you will not be considered for Medicaid under the MBIWPD program. If you are receiving Medicaid coverage with a spenddown, you will have the choice of staying on the spenddown program or switching to the MBI-WPD program. Resource Limits The amount of resources a person has is also used to decide if a person is eligible for the MBI-WPD program. A resource is anything a person owns that can be converted to cash to purchase food, clothing or shelter. Examples of resources include checking or savings accounts, real estate, cars, boats, or other vehicles, stocks, and bonds. To be eligible for the Medicaid Buy-In program, a person may have countable resources up to $10,000. However, because a special budget is used, certain resources are not counted. See the next section for items that might not be counted. Exemptions, Exclusions, Deductions, and Disregards The words: exemptions, exclusions, deductions, and disregards may all be used to describe amounts of money or values of items that are subtracted from a person’s total income to figure the person’s countable income and resources. Some examples of these include $20.00 deducted from unearned income, $65.00 deducted from earned income (plus ½ the remainder deducted from earned income), one automobile not counted as a resource, etc. NOTE: • Co-pays: Some Medicaid services have a small co-payment. These services may be provided using your Medicaid card or through your managed care plan if you are enrolled in managed care. You will not have a co-pay if you are in a managed care plan. • Managed Care: Only applicants with an income that is below 150% of the Federal Poverty Level are eligible to participate in a managed care plan through the MBI-WPD program. • You are required to tell us if your income changes. You may call your local department of social services. ATTACHMENT II MEDICAID BUY-IN FOR WORKING PEOPLE WITH DISABILITIES (MBI-WPD) GRACE PERIOD REQUEST FORM NAME: _________________________________________________________________ ADDRESS: _________________________________________________________________ _________________________________________________________________ PHONE NUMBER: __________________ DATE OF BIRTH: ________________ COUNTY: __________________ SOCIAL SECURITY #: _________________ I AM REQUESTING A GRACE PERIOD FOR CONTINUED PARTICIPATION IN THE MBI-WPD FOR THE FOLLOWING REASON: CHANGE IN MEDICAL CONDITION: (medical verification needed) Verification Attached (physician’s statement) Date of Last Day Worked: ___________ JOB LOSS (through no fault of the participant) _____ This is a temporary layoff. My anticipated return date is ______________. _____ I am actively seeking new employment. Verification Attached (e.g., layoff notice, statement from Department of Labor, VESID, etc.) Please Explain: _________________________________________________________________________ ______________________________________________________________________________________ ______________________________________________________________________________________ Date of Last Day Worked: ____________ I certify, under penalty of perjury, that the information I have provided on this request form is true and complete to the best of my knowledge. ________________________________________ Print Full Name ________________________________________ Signature of Application ______________________ Date -------------------------------------------------------------------------------------------------------------------------------------------To be Completed by the Local District Social Services Office LDSS Contact: ____________________________________ REQUEST APPROVED Date: _____________ REQUEST DENIED Date: _____________ Phone #: ___________________________ Grace Period: __________ to ___________ Reason for Denial: ___________________________________________________________________________ ___________________________________________________________________________________________ _________________________________ Signature of LDSS Contact ____________________ Date MBI-WPD GRACE PERIOD INSTRUCTIONS What Are Grace Periods? A grace period is a time period during which MBI-WPD program participant is not working but remains eligible for the program. Two types of grace periods may be granted: • Medical Reasons: a grace period of up to six months will be allowed if, for medical reasons, the MBI-WPD participant is unable to continue working. Medical verification will be required. When an applicant requests this type of grace period, LDSS must request medical verification. • Grace Period for Job Loss: a grace period of up to six months will be allowed if, no fault of the participant, job loss is suffered, i.e., due to layoff, etc. Verification is required. Districts must verify that the recipient is reasonably expected to return to employment, for example, a temporary layoff, or that the recipient is actively seeking new employment. Note: MBI-WPD participants reporting job loss due to non-medical reasons should be referred to One-Stop Centers, Vocational and Educational Services for Individuals with Disabilities (VESID) and Benefits Planning Assistance and Outreach (BPA&O) services as applicable, so that assistance with employment may be sought prior to loss of eligibility in the program. ` How Do I Go About Getting a Grace Period? A MBI-WPD participant must complete a grace period request on the opposite side of this form. The completed form, along with the required documentation must be submitted to your Local District Social Services (LDSS) office. How Often Can I Have a Grace Period? Recipients may be granted multiple grace periods during a 12-month period. However, in no event may the sum of the grace periods exceed six months in the 12-month period. What Kind of Documentation Do I Need? When applying for a Change in Medical Condition Grace Period, a physician’s statement is required which contains the current health problem, treatment and the anticipated amount of time you will be out of work. When applying for a Job Loss Grace Period, verification is also required. Acceptable forms of verification include layoff notice, statement from Department of Labor, VESID, etc. How Will I Know if My Grace Period is Approved? Your LDSS office will send you a letter informing you of your approval and the period of time authorized. Remember, the sum of your grace periods cannot exceed six months in a 12-month period. What Happens When I Return to Work? You should immediately notify your LDSS office of your return to work. Unless you inform the LDSS office of your return to work, your grace period continues throughout the approved period. This is important because the sum of the grace periods cannot exceed six months in a 12-month period. Will My Grace Period Affect My Premium Payments? Premium payments are calculated on the applicant’s net (earned and unearned) income between 150% and 250% of the FPL. You must notify your LDSS office immediately of any change in income. The LDSS office will use this information to re-calculate your premium payments. Attachment III MBI-WPD Sample Grace Period Letter For Medical Condition Address/Letterhead Date Dear ________: This letter will confirm the approval of your request for a grace period in the Medicaid Buy-In program for Working People with Disabilities (MBI-WPD) due to a change in your medical condition. This grace period is effective ______ through ______. Your participation in the MBI-WPD program means that your Medicaid coverage will not be interrupted during this grace period. When there is again a change in your medical condition such that you can return to work, you must notify the local Department of Social Services in writing and submit verification of employment, i.e. a copy of your first pay stub. At that time, you will no longer be in a grace period as you will, once again, be considered an actively employed participant in the MBI-WPD program. If you are unable to return to work by ______, and require an extension of this grace period, you will be required to request the extension in writing and document your medical condition with a letter from your physician. Remember that for the MBI-WPD program, no more than six months grace period may be allowed in a twelve month period. Please contact me if you have any further questions. Sincerely, Signature Attachment IV MBI-WPD Sample Grace Period Letter For Job Loss Address/letterhead Dear ________: This letter will confirm the approval of your request for a grace period in the Medicaid Buy-In program for Working People with Disabilities (MBI-WPD) due to job loss. This grace period is effective ______ through ______. Your participation in the MBI-WPD program means that your Medicaid coverage will not be interrupted during this grace period. Once you have a new job, you must notify the local Department of Social Services in writing and submit verification of employment, i.e. a copy of your first pay stub. At that time, you will no longer be in a grace period as you will, once again, be considered an actively employed participant in the MBI-WPD program. If you do not obtain a job by ______, and require an extension of this grace period, you will be required to request the extension in writing and document your efforts to actively seek employment during the time of the current grace period. Documentation of employment-seeking means you must keep a job interview record containing the following: 1. The date of each job interview that you have attended. 2. The name and title of the individual who conducted the interview and the address and phone number of the business or agency where the interviews took place. 3. The outcome of each interview (offered a job, or were not offered a job). 4. If you declined a job offer, the reason you declined. 5. If a VESID counselor is assisting you in your job-seeking efforts, written verification from the VESID counselor will be accepted as supportive documentation, as long as it contains the information in your job interview record. We wish you luck in your efforts to obtain employment. Sincerely, Signature Attachment V NOTICE OF ACCEPTANCE OF YOUR MEDICAL ASSISTANCE APPLICATION (MEDICAID BUY-IN PROGRAM FOR WORKING PEOPLE WITH DISABILITIES) Notice Date Name and Address of Agency/Center or District Office _________________ Case Number CIN Number Case Name and Address GENERAL TELEPHONE NO. FOR QUESTIONS OR HELP: _______________ OR Agency Conference Fair Hearing Information and Assistance Worker No. Office No. OCP Unit No. MBI-WPD _________________ (800) 342-3334 Record Access _________________ Legal Assistance _________________ Worker Name Telephone No. We will ACCEPT the Medical Assistance Application dated _________________ for the Medicaid Buy-In Program for Working People with Disabilities (MBI-WPD) effective _________________, for _________________. Please review the Medical Assistance Utilization Threshold Fact Sheet, found in the Medical Assistance section of the booklet “LDSS-4148B: “What You Should Know About Social Services Programs”. The Fact Sheet explains any services limitations. The LDSS-4148B was given to you when you applied for assistance. This is because your net income (gross income less Medical Assistance deductions) of _________________ is at or below the Medicaid Buy-In Program for Working People with Disabilities (MBI-WPD) income limit of $ _________________ (250% of the Federal Poverty Level) and your countable resources of _________________ are at or below the resource limit of $10,000. This means that you will be enrolled in the New York State MBI-WPD program, which will provide you with Medical Assistance coverage as long as you are: • certified disabled; and • are working; and • are at least 16 but less than 65 years of age; and • have net income at or below 250% of the Federal Poverty Level (FPL); and • have resources at or below $10,000; and • are meeting your premium payment obligations (if required). NOTE: A PREMIUM PAYMENT WILL NOT BE REQUIRED AT THIS TIME. HOWEVER, IN 2005 NEW YORK STATE MEDICAID WILL IMPLEMENT A PREMIUM PAYMENT COLLECTION SYSTEM. IF YOUR NET INCOME IS BETWEEN 150% AND 250% OF THE FEDERAL POVERTY LEVEL YOU WILL BE REQUIRED TO PAY A PREMIUM. WHEN THE PREMIUM PAYMENT REQUIREMENT BECOMES EFFECTIVE YOU WILL BE NOTIFIED OF THE AMOUNT OF THE PREMIUM REQUIRED. Since you requested that we determine your Medicaid eligibility for all covered care and services INCLUDING community-based long-term care BUT NOT nursing facility services, we did not review your resources for the past 36 months (60 months for trusts) and you will not be covered for the following nursing facility services: • Nursing home care that is expected to last at least 30 days; or • Nursing home care provided in a hospital; or • Home and community based waiver services; or • Hospice in a nursing home; or • Managed long-term care in a nursing home. If you need nursing facility services, notify your local Department of Social Services. They will then arrange to review your resources for the past 36 months (60 months for trusts) to find out if you are eligible for Medicaid coverage for these services. We have enclosed a budget worksheet(s) so that you can see how we determined your eligibility for benefits. The LAW(S) AND/OR REGULATION(S) which allows us to do this is Sections 366(1)(a)(12) and 367-a(12)of the Social Services Law. REGULATIONS REQUIRE THAT YOU IMMEDIATELY NOTIFY THIS DEPARTMENT OF ANY CHANGES IN NEEDS, RESOURCES, LIVING ARRANGEMENTS OR ADDRESS YOU HAVE THE RIGHT TO APPEAL THIS DECISION BE SURE TO READ THE BACK OF THIS NOTICE ON HOW TO APPEAL THIS DECISION RIGHT TO A CONFERENCE: You may have a conference to review these actions. If you want a conference, you should ask for one as soon as possible. At the conference, if we discover that we made the wrong decision or if, because of information you provide, we determine to change our decision, we will take corrective action and give you a new notice. You may ask for a conference by calling us at the number on the first page of this notice or by sending a written request to us at the address listed at the top of the first page of this notice. This number is used only for asking for a conference. It is not the way you request a fair hearing. If you ask for a conference you are still entitled to a fair hearing. If you want to have your benefits continue unchanged (aid continuing) until you get a fair hearing decision, you must request a fair hearing in the way described below. Read below for fair hearing information. RIGHT TO A FAIR HEARING: If you believe that the above action is wrong, you may request a State fair hearing by: (1) Telephone: (PLEASE HAVE THIS NOTICE WITH YOU WHEN YOU CALL) The new Statewide toll-free request number is (800) 342-3334 OR (2) Fax: Send a copy of this notice to fax no. (518) 473-6735. OR (3) On-Line: Complete and sending the online request form at: https://www.otda.state.ny.us/oah/oahforms/erequestform.asp OR http://www.otda.state.ny.us/oah/forms.asp OR (4) Write: Send a copy of this notice completed, to the Fair Hearing Section, New York State Office of Temporary and Disability Assistance, P.O. Box 1930, Albany, New York 12201. Please keep a copy for yourself. I want a fair hearing. The Agency’s action is wrong because:____________________________________________________ _______________________________________________________________________________________________________ _______________________________________________________________________________________________________ _______________________________________________________________________________________________________ Print Name: __________________________________________________________ Case Number_____________________ Address: _____________________________________________________________Telephone: ______________________ Signature of Client: ____________________________________________________ Date: ___________________________ YOU HAVE 60 DAYS FROM THE DATE OF THIS NOTICE TO REQUEST A FAIR HEARING If you request a fair hearing, the State will send you a notice informing you of the time and place of the hearing. You have the right to be represented by legal counsel, a relative, a friend or other person, or to represent yourself. At the hearing you, your attorney or other representative will have the opportunity to present written and oral evidence to demonstrate why the action should not be taken, as well as an opportunity to question any persons who appear at the hearing. Also, you have a right to bring witnesses to speak in your favor. You should bring to the hearing any documents such as this notice, paystubs, receipts, medical bills, heating bills, medical verification, letters, etc. that may be helpful in presenting your case. CONTINUING YOUR BENEFITS: If you request a fair hearing before the effective date stated in this notice, you will continue to receive your benefits unchanged until the fair hearing decision is issued. However, if you lose the fair hearing, we may recover the cost of any Medical Assistance benefits that you should not have received. If you want to avoid this possibility, check the box below to indicate that you do not want your aid continued, and send this page along with your hearing request. If you do check the box, the action described above will be taken on the effective date listed above. I agree to have the action taken on my Medical Assistance benefits, as described in this notice, prior to the issuance of the fair hearing decision. LEGAL ASSISTANCE: If you need free legal assistance, you may be able to obtain such assistance by contacting your local Legal Aid Society or other legal advocate group. You may locate the nearest Legal Aid Society or advocate group by checking your Yellow Pages under “Lawyers” or by calling the number indicated on the first page of this notice. ACCESS TO YOUR FILE AND COPIES OF DOCUMENTS: To help you get ready for the hearing, you have a right to look at your case file. If you call or write to us, we will provide you with free copies of the documents from your file, which we will give to the hearing officer at the fair hearing. Also, if you call or write to us, we will provide you with free copies of other documents from your file, which you think you may need to prepare for your fair hearing. To ask for documents or to find out how to look at your file, call us at the Record Access telephone number listed at the top of page 1 of this notice or write us at the address printed at the top of page 1 of this notice. If you want copies of documents from your case file, you should ask for them ahead of time. They will be provided to you within a reasonable time before the date of the hearing. Documents will be mailed to you only if you specifically ask that they be mailed. INFORMATION: If you want more information about your case, how to ask for a fair hearing, how to see your file, or how to get additional copies of documents, call us at the telephone numbers listed at the top of page 1 of this notice or write to us at the address printed at the top of page 1 of this notice. Attachment VI AVISO DE ACEPTACIÓN DE SU SOLICITUD PARA ASISTENCIA MÉDICA (PROGRAMA DE COMPRA DE BENEFICIOS DE MEDICAID PARA PERSONAS QUE TRABAJAN Y ESTÁN INCAPACITADAS) Nombre y dirección de la agencia/Centro u oficina de distrito Fecha del aviso Número de Caso Número CIN Nombre del Caso y Dirección No. DE TELÉFONO GENERAL PARA HACER PREGUNTAS O PEDIR AYUDA (518) 473-8887 O No. de oficina No. de unidad No. de trabajador(a) de casos Conferencia con la agencia Audiencias imparciales Información y asistencia (518) 473-8887 (800) 342-3334 Acceso a los archivos (518) 473-8887 Asistencia Legal ________________ Nombre del trabajador(a) No. de teléfono MBI-WPD ACEPTAREMOS su solicitud para Asistencia Médica de fecha _______________ para el Programa de Compra de Beneficios de Medicaid para Personas que Trabajan y están Incapacitadas(MBI-WPD) a partir del _______________, para la(s) siguiente(s) persona(s) (nombre/s) ________________________________________. Favor de revisar la hoja de datos del umbral de utilización del programa de Asistencia Médica que se encuentra en la sección de Asistencia Médica del folleto LDSS-4148B-SP titulado «Lo que usted debe saber sobre los programas de servicios sociales». Esta hoja le explica las limitaciones en los tipos de servicios. El folleto LDSS-4148B se le entregó cuando solicitó los servicios de asistencia. Esto de debe a que su ingreso neto (ingresos brutos menos las deducciones de Asistencia Médica) por la cantidad de _______________ es igual o menor que la cantidad límite permitida por el programa de Compra de Beneficios de Medicaid para Personas que Trabajan y están Incapacitadas (MBI-WPD) cuyo límite es de $______________ (250% del nivel de pobreza según lo establece el gobierno federal) y los recursos que se tomaron en cuenta por la cantidad de $_______________ sobrepasan o llegan al límite de recursos de $10,000. Esto significa que usted puede afiliarse al programa del Estado de Nueva York de MBI-WPD, el cual le proporcionará cobertura de Asistencia Médica siempre y cuando: • tenga un reconocimiento médico indicando su incapacidad; y • esté trabajando; y • tenga por lo menos 16 años de edad pero menos de 65; y • tenga ingresos netos menores o igual al 250% del nivel de pobreza según lo establece el gobierno federal (FPL); y • tenga recursos igual o menor a una cantidad de $10,000; y • cumpla con sus obligaciones en cuanto a los pagos de prima (de ser obligatorios). TOME NOTA: NO SE LE EXIGE UN PAGO DE PRIMA POR EL MOMENTO. SIN EMBARGO, EN EL 2005 EL ESTADO DE NUEVA YORK PONDRÁ EN MARCHA UN SISTEMA PARA LA RECOLECCIÓN DE LOS PAGOS DE PRIMA. SI SUS INGRESOS NETOS ESTÁN ENTRE EL 150% Y EL 250% DEL NIVEL DE POBREZA SEGÚN LO ESTABLECE EL GOBIERNO FEDERAL SE LE EXIGIRÁ PAGAR UNA PRIMA. CUANDO EL REQUISITO DEL PAGO DE PRIMA ENTRE EN VIGOR SE LE NOTIFICARÁ DE LA CANTIDAD DE LA PRIMA A PAGAR. Debido a que usted nos solicitó determinar si reúne las condiciones para recibir todos los cuidados y servicios que cubre Medicaid INCLUYENDO cuidados a largo plazo proveídos en la comunidad PERO NO los servicios de enfermería en centros de cuidados, no examinamos sus recursos de los últimos 36 meses (60 meses si se trata de un fideicomiso) y no tendrá cobertura por los siguientes servicios de enfermería: • Cuidados de enfermería que se crea tengan una duración de por lo menos 30 días; o • Cuidados de enfermería provistos en un hospital; o • Cuidados de hospicio en centro de cuidados de enfermería; o • Cuidados administrados de salud a largo plazo en un centro de cuidados de enfermería. Si necesita cuidados de enfermería en un centro, comuníquese con su departamento local de Servicios Sociales. El personal de ese departamento examinará los recursos de los que ha dispuesto en los últimos 36 meses (60 si se trata de un fideicomiso) para determinar si reúne las condiciones para que Medicaid cubra estos servicios. Hemos incluido una hoja(s) de cálculo de presupuesto de manera que usted pueda entender cómo hemos determinado los beneficios para los cuales usted reúne los requisitos. La LEGISLACIÓN Y/O REGLAMENTO que nos permite tomar esta decisión es la Sección 366(1)(a)(12) y 367-a(12) de las leyes de Servicios Sociales. ATENCIÓN: Las personas que reciben Asistencia Médica podrían reunir los requisitos para recibir un descuento en su servicio telefónico. Para más información sobre el servicio de Lifeline llame al 1-800-555-5000, la llamada es gratis. LEGISLACIÓN VIGENTE EXIGE QUE USTED NOTIFIQUE INMEDIATAMENTE A ESTE DEPARTAMENTO DE TODO CAMBIO EN SUS NECESIDADES, RECURSOS, SITUACIÓN DE VIVIENDA O DIRECCIÓN. USTED TIENE EL DERECHO DE APELAR ESTA DECISIÓN. LEA EL REVERSO DE ESTE AVISO PARA MÁS INFORMACIÓN SOBRE CÓMO APELAR ESTA DECISIÓN. LDSS-4374-S (Rev. 10/03) REVERSO DERECHO A UNA CONFERENCIA: Usted puede pedir una conferencia para revisar estas acciones. Si desea una conferencia, le sugerimos solicitarla lo más pronto posible. Si durante la conferencia nos percatamos que nuestra decisión fue errónea, o en base a la información que usted proporcione, decidimos cambiar nuestra decisión; tomaremos acción correctiva y le proporcionaremos una nueva notificación. Puede solicitar una conferencia llamándonos al número que aparece en la primera página de esta notificación o enviándonos una solicitud a la dirección que aparece en la parte superior de la misma página. Este número es solamente para solicitar conferencias y no es la manera de solicitar una audiencia imparcial. Aunque solicite una conferencia, también tiene el derecho a una audiencia imparcial. Si desea que sus beneficios continúen sin cambios (asistencia ininterrumpida) a la espera de la decisión de la audiencia imparcial; debe solicitar una audiencia imparcial de la manera que se describe abajo. Lea a continuación la información sobre audiencias imparciales. DERECHO A UNA AUDIENCIA IMPARCIAL: Si cree que la decisión antes mencionada es errónea, puede solicitar una audiencia estatal de la siguiente manera: (1) Por teléfono: (FAVOR DE TENER A MANO ÉSTA NOTIFICACIÓN CUANDO LLAME) (800) 342-3334 (2) Por facsímil: Envíe una copia de esta notificación al número de fax (518) 473-6735 ó (3) Por computadora: Complete y envíe el formulario electrónico de petición en la siguiente dirección de Internet: https://www.otda.state.ny.us/oah/oahforms/erequestform.asp ó http://www.otda.state.ny.us/oah/forms.asp ó (4) Por escrito: Envíe una copia de esta notificación completamente rellenada a: Fair Hearing Section, New York State Office of Temporary and Disability Assistance, P.O. Box 1930, Albany, New York 12201. Favor de quedarse con una copia. Solicito una audiencia imparcial. La decisión de la agencia es errónea porque: _________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ Nombre (en letra de molde): ________________________________________________No. de caso_________________ Dirección: _____________________________________________________________Teléfono: ______________________ Firma del cliente: ____________________________________________________ Fecha: ____________________________ USTED TIENE 60 DÍAS A PARTIR DE LA FECHA DE ESTE AVISO PARA SOLICITAR UNA AUDIENCIA IMPARCIAL Si usted solicita una audiencia imparcial, el Estado le enviará una notificación informándole acerca de la hora y el lugar de la audiencia. Usted tiene el derecho de ser representado(a) por un abogado, un familiar, un amigo(a) u otra persona, o puede representarse a sí mismo(a). Durante la audiencia, usted, su abogado u otro representante tendrá la oportunidad de presentar pruebas orales y escritas para demostrar la razón por la cual la acción no debe llevarse a cabo, así como también la oportunidad de interrogar a toda persona que compadezca en la audiencia. También, tiene el derecho de presentar testigos que testifiquen en su favor. Se le sugiere presentar en la audiencia documentos tales como: esta notificación, talonarios de pagos salariales, recibos, cuentas médicas, cuentas de calefacción, verificación médica, cartas, etc., que puedan ayudarle en la presentación de su caso. CONTINUACIÓN DE SUS BENEFICIOS: Si usted solicita una audiencia imparcial antes de la fecha de vigencia indicada en este aviso; continuará recibiendo sus beneficios como siempre hasta que se dé a conocer la decisión de la audiencia imparcial. No obstante, si no se decide a su favor en la decisión de la audiencia imparcial, nos podremos cobrar los beneficios de Asistencia Médica que usted recibió y a los cuales no tenía derecho. Si desea evitar esta situación, marque la casilla abajo indicando que usted no desea continuar recibiendo ayuda y envíe esta página junto con su petición de audiencia. Si usted marca la casilla, la acción descrita arriba será adoptada en la fecha de vigencia indicada arriba. Estoy de acuerdo que se tome la decisión con respecto a mis beneficios de Asistencia Médica, según se describe en esta notificación, antes de darse a conocer la decisión de la audiencia imparcial. ASISTENCIA LEGAL: Si usted necesita asistencia legal gratis, puede obtener tal ayuda comunicándose con la Sociedad de Ayuda Legal de su localidad (Legal Aid Society) u otro grupo legal de abogacía. Usted puede localizar la Sociedad de Ayuda Legal o el grupo de abogacía más cercano buscando en las Páginas Amarillas bajo “Abogados” (“Lawyers”) o llamando al número que se indica en la primera página de esta notificación. ACCESO A SU ARCHIVO Y COPIAS DE DOCUMENTOS: Para ayudarle a prepararse para la audiencia, se le otorga el derecho de examinar el archivo de su caso. Si nos llama por teléfono o nos manda una carta, le proporcionaremos copias gratis de los documentos de su archivo, los mismos que entregaremos al funcionario de audiencias en la audiencia imparcial. Así mismo, si usted nos llama por teléfono o nos manda una carta, le proporcionaremos copias gratis de otros documentos de su archivo que usted considere necesarios al prepararse para la audiencia imparcial. Para solicitar los documentos o para averiguar cómo examinar su archivo, llámenos al número de teléfono para Acceso a archivos que aparece en la parte superior de la página 1 de esta notificación o escríbanos a la dirección impresa en la parte superior de esa misma página. Si desea copias de los documentos en su archivo, debe pedirlas con anticipación. Se le entregarán en un plazo razonable antes de la fecha de la audiencia. Se le envirarán los documentos por correo solamente si usted específicamente lo solicita. INFORMACIÓN: Si desea más información sobre su caso, cómo solicitar una audiencia imparcial, cómo examinar su archivo o cómo conseguir copias adicionales de documentos, llámenos a los números de teléfono indicados al comienzo de la página 1 de esta notificación o escríbanos a la dirección impresa en esa misma página. Attachment VII MBI-WPD MONTHLY REPORT County Name: ____________________________________ County Contact: ____________________________________ Month of Report: ______________________ Phone #: _______________ Date: _______________ NEW APPLICANTS FOR MBI: CIN # Receipt of SSDI Disability Diagnosis Yes No Mental Physical Combination Job Title Grace Period Requested This Month # Days Available UNDERCARE: CIN # # Days Requested