Patterns of death among patients treated at a Department of Medical
Anuncio
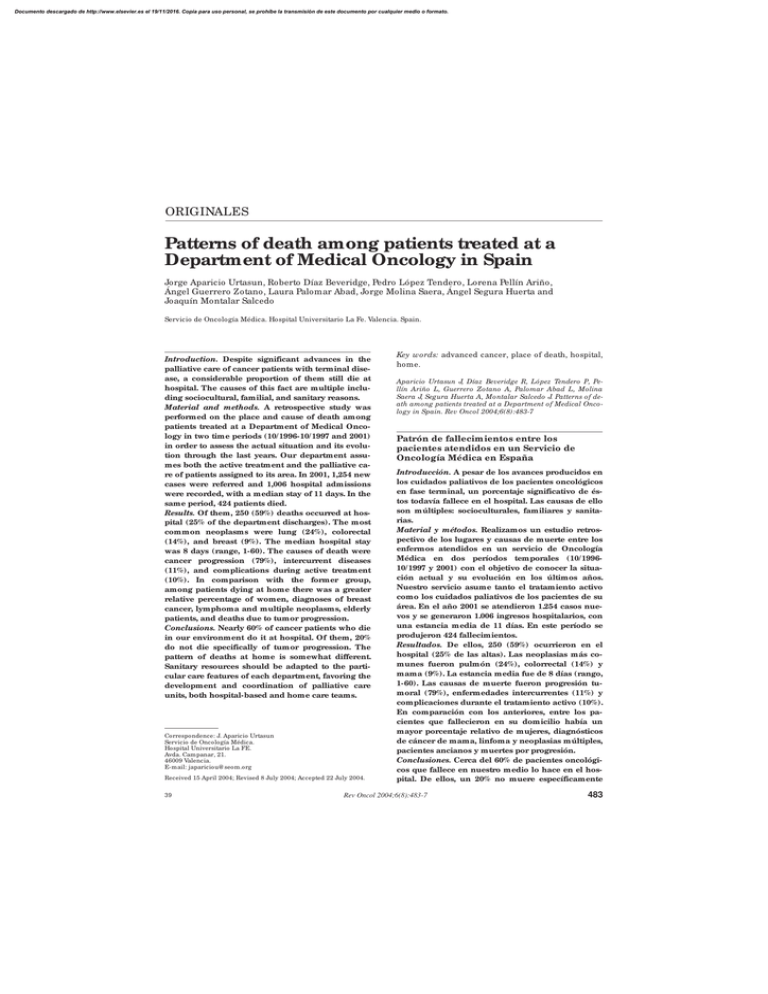
Documento descargado de http://www.elsevier.es el 19/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. ORIGINALES Patterns of death among patients treated at a Department of Medical Oncology in Spain Jorge Aparicio Urtasun, Roberto Díaz Beveridge, Pedro López Tendero, Lorena Pellín Ariño, Ángel Guerrero Zotano, Laura Palomar Abad, Jorge Molina Saera, Ángel Segura Huerta and Joaquín Montalar Salcedo Servicio de Oncología Médica. Hospital Universitario La Fe. Valencia. Spain. Introduction. Despite significant advances in the palliative care of cancer patients with terminal disease, a considerable proportion of them still die at hospital. The causes of this fact are multiple including sociocultural, familial, and sanitary reasons. Material and methods. A retrospective study was performed on the place and cause of death among patients treated at a Department of Medical Oncology in two time periods (10/ 1996-10/ 1997 and 2001) in order to assess the actual situation and its evolution through the last years. Our department assumes both the active treatment and the palliative care of patients assigned to its area. In 2001, 1,254 new cases were referred and 1,006 hospital admissions were recorded, with a median stay of 11 days. In the same period, 424 patients died. Results. Of them, 250 (59%) deaths occurred at hospital (25% of the department discharges). The most common neoplasms were lung (24%), colorectal (14%), and breast (9%). The median hospital stay was 8 days (range, 1-60). The causes of death were cancer progression (79%), intercurrent diseases (11%), and complications during active treatment (10%). In comparison with the former group, among patients dying at home there was a greater relative percentage of women, diagnoses of breast cancer, lymphoma and multiple neoplasms, elderly patients, and deaths due to tumor progression. Conclusions. Nearly 60% of cancer patients who die in our environment do it at hospital. Of them, 20% do not die specifically of tumor progression. The pattern of deaths at home is somewhat different. Sanitary resources should be adapted to the particular care features of each department, favoring the development and coordination of palliative care units, both hospital-based and home care teams. Correspondence: J. Aparicio Urtasun Servicio de Oncología Médica. Hospital Universitario La FE. Avda. Campanar, 21. 46009 Valencia. E-mail: japariciou@ seom.org Received 15 April 2004; Revised 8 July 2004; Accepted 22 July 2004. 39 Key words: advanced cancer, place of death, hospital, home. Aparicio Urtasun J, Díaz Beveridge R, López Tendero P, Pellín Ariño L, Guerrero Zotano A, Palomar Abad L, Molina Saera J, Segura Huerta A, Montalar Salcedo J. Patterns of death among patients treated at a Department of Medical Oncology in Spain. Rev Oncol 2004;6(8):483-7 Patrón de fallecimientos entre los pacientes atendidos en un Servicio de Oncología Médica en España Introducción. A pesar de los avances producidos en los cuidados paliativos de los pacientes oncológicos en fase terminal, un porcentaje significativo de éstos todavía fallece en el hospital. Las causas de ello son múltiples: socioculturales, familiares y sanitarias. Material y métodos. Realizamos un estudio retrospectivo de los lugares y causas de muerte entre los enfermos atendidos en un servicio de Oncología Médica en dos períodos temporales (10/ 199610/ 1997 y 2001) con el objetivo de conocer la situación actual y su evolución en los últimos años. Nuestro servicio asume tanto el tratamiento activo como los cuidados paliativos de los pacientes de su área. En el año 2001 se atendieron 1.254 casos nuevos y se generaron 1.006 ingresos hospitalarios, con una estancia media de 11 días. En este período se produjeron 424 fallecimientos. Resultados. De ellos, 250 (59%) ocurrieron en el hospital (25% de las altas). Las neoplasias más comunes fueron pulmón (24%), colorrectal (14%) y mama (9%). La estancia media fue de 8 días (rango, 1-60). Las causas de muerte fueron progresión tumoral (79%), enfermedades intercurrentes (11%) y complicaciones durante el tratamiento activo (10%). En comparación con los anteriores, entre los pacientes que fallecieron en su domicilio había un mayor porcentaje relativo de mujeres, diagnósticos de cáncer de mama, linfoma y neoplasias múltiples, pacientes ancianos y muertes por progresión. Conclusiones. Cerca del 60% de pacientes oncológicos que fallece en nuestro medio lo hace en el hospital. De ellos, un 20% no muere específicamente Rev Oncol 2004;6(8):483-7 483 Documento descargado de http://www.elsevier.es el 19/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. APARICIO URTASUN J, DÍAZ BEVERIDGE R, LÓPEZ TENDERO P, ET AL. PATTERNS OF DEATH AMONG PATIENTS TREATED AT A DEPARTMENT OF MEDICAL ONCOLOGY IN SPAIN por progresión neoplásica. El patrón de fallecimientos en el domicilio es algo diferente. Los recursos sanitarios deberían adaptarse a las peculiaridades asistenciales de cada servicio, potenciándose el desarrollo y coordinación de las unidades de cuidados paliativos tanto hospitalarias como domiciliarias. Palabras clave: cáncer avanzado, lugar de fallecimiento, hospital, domicilio. INTRODUCTION Cancer represents one of the main causes of death in the Western world, accounting for 20% of the overall mortality. In fact, only approximately 50% of patients with this diagnosis will become long-term survivors of their malignant disease 1. Moreover, a significant number of cancer patients die of causes different from the neoplasm itself, such as intercurrent infections, concomitant diseases, and treatment-related toxicity. Depending on the sociocultural context, especially in North Europe, North America and Australia, a trend has been noted to move the place of death towards the familial environment and the patient’s home, with the support of palliative home care teams2,3. In contrast, many patient families in Spain still consider dying at hospital as a sign of quality of care. The practice of palliative care in cancer patients with terminal disease is differently distributed, as a function of territorial resources, among departments of Medical Oncology, Palliative Care Units, hospices, and palliative home care teams4. In order to investigate the actual situation and its evolution through the last years, a retrospective study was performed on the causes of death among patients treated at a Department of Medical Oncology in Spain. Two one-year periods were analysed with a time interval of 5 years. The objective was to know the prevalence of the underlying neoplasms, the main causes of death, and the place and context of these deaths in order to adequate the sanitary resources accordingly. PATIENTS AND M ETHODS Two one-year periods were retrospectively analysed: period 1 (between October 1996 and October 1997), and period 2 (between January and December 2001). In both of them, all deaths occurred among cancer patients admitted at the Department of Medical Oncology were recorded. Deaths occurring either at hospices or at other general hospitals were scant and so excluded from this analysis. The following parameters were coded in the data base: patient age and gender, underlying neoplasm, situation at hospital ad- 484 mission (no prior diagnosis of malignancy, diseasefree or complete remission, active disease with specific treatment, or active disease with supportive therapy), cause of admission (initial study, complication secondary to treatment, symptom control, or terminal status), duration of hospitalisation before death, and final cause of death (tumor progression, treatmentrelated toxicity, intercurrent disease, other causes). Results were grouped and compared between the two time periods analysed. Furthermore, in the second period, a comparison was made between patients dying at hospital and patients dying at home during the same time. For patients dying at home, circumstances and causes of death were directly collected by the investigators from family caregivers or palliative home care personnel. Comparisons between groups were performed by means of the Chi-squared test or the Fisher exact test, when appropriate, and statistical significance was defined as p<0.05. Our department assumes both the active medical treatment and the palliative care of the majority of patients of its geographical area. There is no a specific Palliative Care Unit, but we collaborate with a specialised home care team, and two hospitals for chronic patients (hospices). Although there are no Medical Oncology duties, our medical staff is available for consulting about cancer patients’ admissions in the Emergency Room every morning form Monday to Friday, and approximately for 40% of the days in the rest of time. RESULTS In 2001, 1,254 new cases of cancer were referred to our department. A total of 1,006 hospital admissions were generated, with a median hospital stay of 11 days. In the same time period, 424 patient deaths occurred, of which 250 (59%) took place at hospital, thus representing 25% of our hospital discharges. Table 1 shows the comparison of the features of these patients (period 2) with that of 193 patients who died during hospital admission at our department in period 1 (with 1,000 new cases registered). This 29% increase in the number of deaths is related to the 25% increase in the number of new cases per year achieved in this interval. The spectrum of diseases shows a (statistically non significant) trend to an increase in the percentage of deaths secondary to colorectal, breast, and esophagogastric cancers, whereas the relative percentage of deaths from lung cancer, head and neck tumors, and lymphoma have decreased. This could reflect their different prevalence, patient referral, prognosis, and pattern of place of death. In period 1, more patients were admitted in terminal status, whereas in period 2 there were more admissions for staging studies (initial diagnosis or at relapse) or due to treatment complications. These differences did Rev Oncol 2004;6(8):483-7 40 Documento descargado de http://www.elsevier.es el 19/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. APARICIO URTASUN J, DÍAZ BEVERIDGE R, LÓPEZ TENDERO P, ET AL. PATTERNS OF DEATH AMONG PATIENTS TREATED AT A DEPARTMENT OF MEDICAL ONCOLOGY IN SPAIN TABLE 1. Comparison of characteristics among patients dying at hospital in the two periods analysed Number Age (years) Median Range Gender Male Female Cancer type (percent) Lung Colorectal Breast Head and neck Esophago-gastric Lymphoma Unknown primary Bladder Sarcoma Multiple primary site Other tumors Cause of admission Symptom control Terminal status Study (initial, relapse) Treatment complications Other, unknown Cause of death Tumor progression Intercurrent causes Died in 2001 Died between 10/96-10/97 250 193 64 24-48 57 18-83 159 (64%) 91 (36%) 116 (60%) 77 (40%) 24% 14% 9% 6% 8% 3% 5% 4% 3% 1% 23% 32% 8% 6% 11% 5% 8% 4% 3% 5% 2% 16% 42% 21% 18% 13% 6% 45% 29% 11% 10% 5% 79% 11% 81% 8% not reach statistical significance. The other features (age, gender, cause of death, and median stay) did not differ among the periods of study. Table 2 depicts the comparison of characteristics among patients dying in 2001, either at hospital (250 cases) or at home (174 cases). In the former group, the percentage of patients dying because of treatment-related toxicity was greater (p=0.002), whereas in the latter patients tended to be more frequently older than 70 years (p=0.09) and women (p=0.049). Table 3 shows the relative percentage of patients dying at hospital as a function of the tumor type. Patients with neoplasms of the esophagus, bladder or stomach were more likely to die at hospital. In contrast, patients with lymphoma, multiple neoplasms, and cancers of the breast, pancreas, cervix and central nervous system tended to die more frequently at home. Comparisons between these groups of neoplasms were statistically significant. For patients dying during hospitalisation in period 2, further data were available that were not recorded for period 1. Twenty-two percent of them died in the first 48 hours after admission. Although the terminal situation was formally addressed in the medical records for the majority of patients ("terminally ill patient" or "do not resuscitate" orders), only in 30% of 41 TABLE 2. Comparison of characteristics between patients dying at hospital and patients dying at home (period 2001) Number (percent) Age (years) Median Range > 70 Gender Male Female Cancer type (percent) Lung Colorectal Breast Head and neck Esophago-gastric Lymphoma Unknown primary Bladder Sarcoma Multiple primary site Other tumors Cause of death Tumor progression Intercurrent causes Treatment-related toxicity Died at hospital Died at home 250 (59%) 174 (41%) 64 24-84 65 (26%) 64 21-92 59 (34%) 159 (64%) 91 (36%) 94 (54%) 80 (46%) 24% 14% 9% 6% 8% 3% 5% 4% 3% 1% 23% 18% 11% 13% 5% 4% 7% 6% 2% 2% 4% 28% 79% 11% 10% 88% 10% 2% TABLE 3. Number (percentage) of dying patients according to the place of death by cancer type (period 2001) Cancer type Lung Colorectal Breast Head and neck Stomach Esophagus Lymphoma Bladder Unknown primary Ovary Multiple primary sites Pancreas Cervix Central nervous system Sarcoma Prostate Multiple myeloma Place of death (mean) Hospital Home 250 (59%) 174 (41%) 60 36 22 15 13 07 08 11 13 09 03 04 05 03 07 06 05 (66%) (65%) (50%) (65%) (68%) (87%) (40%) (73%) (54%) (64%) (30%) (50%) (45%) (27%) (64%) (67%) (56%) 31 19 22 08 06 01 12 04 11 05 07 04 06 08 04 03 04 (34%) (35%) (50%) (35%) (32%) (13%) (60%) (27%) (46%) (36%) (70%) (50%) (55%) (73%) (36%) (33%) (44%) them an express mention of specific pharmacological treatment of this condition was evident. Finally, only 19% of patients dying of potential treatment-related toxicity were admitted in the Intensive Care Unit. DISCUSSION For many centuries, most human beings have died in the place they lived. However, in the 20th century, so- Rev Oncol 2004;6(8):483-7 485 Documento descargado de http://www.elsevier.es el 19/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. APARICIO URTASUN J, DÍAZ BEVERIDGE R, LÓPEZ TENDERO P, ET AL. PATTERNS OF DEATH AMONG PATIENTS TREATED AT A DEPARTMENT OF MEDICAL ONCOLOGY IN SPAIN ciocultural changes in perception of the concepts of life and death and significant advances in the practice of medicine have moved the place of death from home to hospitals. Patient death is now more often seen as a medical failure than as a natural outcome. In fact, nearly 60% of terminal patients had active treatment in progress at the time of death in one study, thus reflecting the treatment imperative to prolong life in western societies5. The percentage of cancer patients dying at the acute care hospital setting (in contrast with those dying at home) varies significantly from 40% to 70% as a function of the period of study, the geographical area, and the sanitary resources2-7. Our data are in concordance with previous studies. Nearly 60% of our cancer patients who die do it at hospital. Their median hospital stay is short, reflecting a high percentage of admissions in terminal status. Some 20% of patients die from intercurrent causes or treatment-related complications, although admission to the Intensive Care Unit is infrequently asked. Main limitations and potential biases of the present study are its retrospective nature and the fact that it is a hospital-based population, thus making difficult to generalize its conclusions. With a median of 21 deaths per month, personal and sanitary resources should be adapted accordingly. However, further collaboration with non hospital palliative care units is evidently needed. Approximately two-thirds of cancer patients, when asked about the preferred place of death, wish to die in their own homes. During the last decade it is becoming increasingly more common for dying patients to be offered home care by their relatives with the support of an advanced palliative home care team 8. In fact, a recent trend has been noted to rise the proportion of people who die out of the hospital9. A number of individual patient factors are known to be predictive of the place of death among terminal cancer patients7, 9-16: female gender, children, elderly people, residency in rural areas, longer survival after diagnosis of cancer, functionally dependent patient status, family support (more than one caregiver), patient’s and caregiver’s desires, support of their family physician, and availability of advanced palliative home care are associated with an increased frequency of death at home, whereas haematological malignancies, short survival after diagnosis of cancer, black ethnicity, low income, low social class, low educational level, residency in deprived areas, family exhaustion, rehospitalisation, and prolonged home nursing care are predictors of dying at hospital. For elderly patients, factors predicting death in the general hospital for men were digestive comorbidities, vomiting, and weakness, whereas for women were functional dependency and lack of social support17. Although some results are conflicting among studies, the type of primary tumor seems to be related with 486 the chance of dying at hospital16. The present study confirms previous data regarding the influence of gender and age in the place of death, but also shows how certain cancer types (breast, lymphoma, multiple primary site) are more commonly associated with death at home whereas others (esophagus, bladder, stomach) frequently predict for death at hospital. This trend could be related to other described factors such as the length of survival and specific tumor complications (bleeding, digestive tract obstruction, etc.). We have not specifically addressed other features such as family support, income, educational level, and social class. However, it is becoming evident that if advanced palliative home care is easily available, adequately offered, and caregivers instructed, an increasing percentage of terminally ill cancer patients would benefit of dying at home, thus increasing the congruence between patient’s preferred and actual place of death18. References 1. Brenner H. Long-term survival rates of cancer patients achieved by the end of the 20th century: a period analysis. Lancet 2002;360:1131-5. 2. Townsend J, Frank S, Fermont D, et al. Terminal cancer care and patients’ preferences for place of death: A prospective study. BMJ 1990;301:415-7. 3. Hunt R, Bonett A, Roder D. Trends in terminal care of cancer patients: South Australia, 1981-1990. Austr N Zeal J Med 1993;23:245-51. 4. Sánchez Sobrino M, Sastre Moyano P. Cuidados paliativos domiciliarios y hospitalarios. En: González Barón M, editor. Tratado de Medicina Paliativa y tratamiento de soporte en el enfermo con cáncer. Madrid: Panamericana, 1996; p.97-113. 5. Middlewood S, Gardner G, Gardner A. Dying in hospital: medical failure or natural outcome? J Pain Symptom Manage 2001;22:1035-41. 6. Constantini M. Palliative home care and place of death among cancer patients: a population-based study. Palliative Med 1993;7:323-31. 7. Carlsson ME, Rollison B. A comparison of patients dying at home and patients dying at a hospice: Sociodemographic factors and caregivers’ experiences. Palliative and Supportive Care 2003;1:33-9. 8. Beck-Friis B, Strang P. The organization of hospital-based home care for terminally ill cancer patients: The Motala model. Palliative Med 1993;7:93-100. 9. Burge F, Lawson B, Johnston G. Trends in the place of death of cancer patients, 1992-1997. Can Med Assoc J 2003;168:265-70. 10. Cantwell P, Turco S, Brenneis C, et al. Predictors of home care death in palliative care cancer patients. J Palliat Care 2000;16:23-8. 11. Higginson I, Thompson M. Children and young people who die from cancer: epidemiology and place of death in England (1995-9). BMJ 2003;327:178-9. 12. Bruera E, Russell N, Sweeney C, Fisch M, Palmer JL. Place of death and its predictors for local patients registered at a comprehensive cancer center. J Clin Oncol 2002;2127-33. Rev Oncol 2004;6(8):483-7 42 Documento descargado de http://www.elsevier.es el 19/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. APARICIO URTASUN J, DÍAZ BEVERIDGE R, LÓPEZ TENDERO P, ET AL. PATTERNS OF DEATH AMONG PATIENTS TREATED AT A DEPARTMENT OF MEDICAL ONCOLOGY IN SPAIN 13. Gatrell AC, Harman JC, Francis BJ, et al. Place of death: analysis of cancer deaths in part of North West England. J Public Health Med 2003;25:53-8. 14. Fukui S, Kawagoe H, Masako S, Noriko N, Hiroko N, Toshie M. Determinants of the place of death among terminally ill cancer patients under home hospice care in Japan. Palliat Med 2003;17:445-53. 15. Grande GE, McKerral A, Addington-Hall JM, Todd CJ. Place of death and use of health services in the last year of life. J Palliat Care 2003;19:263-70. 43 16. Tang ST, McCorkle R. Determinants of place of death for terminal cancer patients. Cancer Invest 2001;19: 165-80. 17. Izquierdo-Porrera AM, Trelis-Navarro J, Gomez-Batiste X. Predicting place of death of elderly cancer patients followed by a palliative care unit. J Pain Symptom Manage 2001;21:481-90. 18. Tang ST, McCorkle R. Determinants of congruence between the preferred and actual place of death for terminally ill cancer patients. J Palliat Care 2003;19:230-7. Rev Oncol 2004;6(8):483-7 487