Clinical Laboratory Haematology - 2008 - Sokol - Cold haemagglutinin disease clinical significance of serum haemolysins
Anuncio

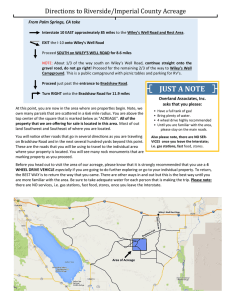
Clin. Lab. Haem. 2000, 22, 337±344 R.J. SOKOL*, D.J. BOOKER*, R. STAMPS*, R. WALEWSKA Cold haemagglutinin disease: clinical signi®cance of serum haemolysins *National Blood Service, Trent Centre, Shef®eld, Department of Haematology, Leicester Royal In®rmary, Leicester, UK Summary Two hundred and twenty-one patients with cold haemagglutinins of thermal amplitude ³ 30 °C (considered to be a reasonable indicator of clinical signi®cance) were classi®ed by in vitro haemolysin activity into three groups. Group 1 contained 116 individuals in whom haemolysins were never detected; the 74 patients in Group 2 had monophasic haemolysins alone; whereas both monophasic and biphasic haemolysins were detected in the 31 Group 3 patients. There was a signi®cantly higher proportion of patients in Groups 2 and 3 with haptoglobin levels < 0.1 g/l compared with Groups 1 and 2, respectively (P < 0.005 and P < 0.001). Direct antiglobulin test results showed that the autoimmune response became more complex and IgM predominant through Groups 1±3, resulting in an increasing ability to activate complement which was re¯ected in increasing haemolysin activity and number of patients with active haemolysis. The 31 patients in Group 3 were mostly elderly (median age 71 years at presentation) and the majority had chronic cold haemagglutinin disease (CHAD), several in association with lymphoid neoplasms or carcinomas; only four had acute CHAD. The natural history of idiopathic chronic CHAD was of mild, well compensated haemolysis, punctuated by severe acute episodes necessitating intensive therapy. The condition often remained active for long periods and did not appear to affect natural lifespan. In some cases, no treatment (or just warmth) was needed; in others continuous or intermittent prednisolone and/or chlorambucil were effective; yet others required a greater variety and more intense therapy, or treatment of associated conditions. Blood transfusion support was frequently required when haemolysis was severe. Keywords Anaemia, haemolytic, autoimmune, cold agglutinin disease, serum haemolysins Introduction Cold red cell autoantibody syndromes are usually divided into two groups, cold haemagglutinin disease (CHAD) and paroxysmal cold haemoglobinuria (PCH), based on their clinical and serological features, including different patterns of in vitro complement mediated haemolysis. The IgM class autoantibodies causing CHAD usually bind to red cells and activate complement to produce haemolysis in vitro at the same temperature, and as such are referred Accepted for publication 3 July 2000 Correspondence: Dr R.J. Sokol, National Blood Service, Trent Centre, Longley Lane, Shef®eld S5 7JN, UK. Fax: 0114 2034910; E-mail: [email protected] Ó 2000 Blackwell Science Limited to as monophasic haemolysins. On the other hand, the IgG class Donath-Landsteiner autoantibodies, considered pathognomonic of PCH, are usually described as biphasic haemolysins since they bind to red cells at low temperatures but activate complement to produce in vitro haemolysis at 37 °C (Sokol et al., 1999). However, whether a haemolytic autoantibody behaves biphasically or monophasically depends on its thermal range; for example, true IgG Donath-Landsteiner antibodies occasionally have a suf®ciently high thermal amplitude to cause haemolysis monophasically (Ries et al., 1971; Boccardi et al., 1977; Wolach et al., 1981; Lindgren et al., 1985) and conversely, the cold IgM autoantibodies of CHAD can cause biphasic haemolysis if they have a relatively low thermal 337 Serum haemolysins in CHAD range but a high complement ®xing ability (Dacie 1992). Such cases are more common than PCH and it is important that the two conditions are not confused, though this is not usually a problem if full and proper investigations are carried out. Likewise, they must not be confused with individuals having both CHAD and PCH; such mixed cases are exceedingly rare, but do exist (Sokol et al., 1999). Nowadays, serology reference laboratories rarely test for the presence of serum haemolysins in patients with suspected CHAD. In order to assess the signi®cance of haemolysin test results and to evaluate whether they give worthwhile information on the likely clinical signi®cance of cold autoantibodies, the present study examines a series of patients with wide thermal range cold autoagglutinins who were classi®ed according to the pattern of in vitro haemolysin activity, and discusses the clinico-pathological features of the 31 individuals in whom the serum haemolysins showed biphasic properties. Materials and methods The records of all patients referred to the Trent Centre Immunohaematology Department between 13 December 1984 and 12 January 1996 were reviewed; cases with cold red cell autoagglutinins having a thermal amplitude of at least 30 °C by an albumin technique (Garratty et al., 1977) were examined and those with a complete set of haemolysin tests, but where full investigation had excluded a primary or concomitant diagnosis of PCH, were selected for detailed study. The investigations performed at this Centre have previously been reported in full (Sokol, Hewitt & Stamps 1981; Sokol et al., 1988a, b, 1990a, b; Sokol et al., 1995). They included direct antiglobulin tests using monospeci®c anti-IgG, -IgM, -IgA, -C3c and -C3d by the standard agglutination method and employing anti-IgG, -IgM and -IgA in an enzyme-linked assay (ELISA). Serum collected and separated at 37 °C was tested for autoantibodies using saline, enzyme and indirect antiglobulin techniques; autoantibody speci®city and thermal amplitude were determined by titrating at 20 °C and 30 °C against adult and cord cells using saline, albumin and enzyme methods (Sokol et al., 1995). In addition, the warm separated serum was tested for monophasic haemolysins using acidi®ed serum (pH 6.8) at 20 °C and 37 °C (Sokol et al., 1995); biphasic haemolysins were detected by the indirect Donath-Landsteiner procedure (Sokol et al., 1995). Serum haptoglobin levels were measured by their haemoglobin binding capacity (Ratcliff & Hardwicke 1964), our normal range being 0.4±2.0 g/l. A method of population proportions was used to examine the effects of haemolysin pattern on the likely presence or absence of active haemolysis, de®ned by haptoglobin levels of < 0.1 g/l and ³ 0.4 g/l, respectively. The difference between proportions was tested for signi®cance by the Chisquare procedure (with Yates correction) at 1 degree of freedom, and the 99% con®dence intervals were calculated (Mack 1967; Gardner & Altman 1986). Because multiple statistical comparisons were being made, the signi®cance level for individual tests was set at P < 0.01, which required a Chi-square value of ³ 6.63 (Sokol et al., 1990b). Results Two hundred and twenty-one patients with cold autoagglutinins active at 30 °C (or above) were classi®ed into three groups on the pattern of in vitro haemolysin activity (Tables 1±3). There were 116 in whom haemolysins were never detected (Group 1); 74 patients had haemolysins but these never showed biphasic properties (Group 2); and in 31 patients, both monophasic and biphasic haemolysins (demonstrated by a positive Donath-Landsteiner test) were present (Group 3). Direct antiglobulin tests were positive in all patients (except one in Group 1) with increased amounts of red cell bound C3d; in addition, C3c was detected in 28, 45 and 55% in Groups 1±3, respectively. Increased amounts of red cell bound immunoglobulins were detected by ELISA in 68, 85 and 93% of patients in Groups 1±3, respectively. IgM predominated, either alone or in combination with IgG and/or IgA, and was found, respectively, in 80, 90 and 100% of patients in Groups 1±3 who had a positive ELISA result. There were signi®cantly higher proportions of patients with haptoglobin levels < 0.1 g/l in Group 2 compared with Group 1 (0.09 vs. 0.29; 99% con®dence interval for Table 1. Group 1: 116 patients in whom in vitro haemolysins were never detected Males/females 53 Age at testing (years) 19±99 (median 66) Speci®city of cold agglutinin (n) I i `not I, i or Pr' Pr I/HI 82 14 12 7 1 Haptoglobin (g/l) (n) < 0.1 0.1±0.3 ³ 0.4 9 10 97 63 Ó 2000 Blackwell Science Ltd., Clin. Lab. Haem., 22, 337±344 13652257, 2000, 6, Downloaded from https://onlinelibrary.wiley.com/doi/10.1046/j.1365-2257.2000.00320.x by Universidad De Chile, Wiley Online Library on [25/05/2024]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License 338 Table 2. Group 2: 74 patients in whom in vitro haemolysins were detected but did not show biphasic reactions Males/females 30 Age at testing (years) 16±95 (median 71) Speci®city of cold agglutinin (n) I i `not I, i or Pr' Pr I/HI 64 1 3 3 3 Monophasic haemolysin pattern (n) pH 6.8 (20 °C) pH 6.8 (20 °C + 37 °C) 62 12 Haptoglobin (g/l) (n) < 0.1 0.1±0.3 ³ 0.4 18 11 45 Table 3. Group 3: 31 patients in whom biphasic haemolysins were demonstrated Males/females 17 Age at testing (years) 19±90 (median 79) Speci®city of cold agglutinin (n) I i `not I, i or Pr' 14 29 1 1 Monophasic haemolysin pattern (n) pH 6.8 (20 °C) + biphasic haemolysins 19 pH 6.8 (20 °C + 37 °C) + 12 biphasic haemolysins Haptoglobin (g/l) (n)* < 0.1 0.1±0.3 ³ 0.4 19 9 2 *Out of 30 tested. difference 0.04±0.37; v2 10.42, P < 0.005) and in Group 3 compared with Group 2 (0.29 vs. 0.91, 99% con®dence interval for difference 0.48±0.92; v2 22.04, P < 0.001). The 31 patients in Group 3 were numbered according to age at presentation (Table 4). Severity of disease was a subjective attempt, after reviewing all available records, to indicate how the condition affected the individual's dayto-day life ± `mild' representing very few or no problems, `moderate' meaning that lifestyle had to be modi®ed to cope with the disease, whereas `severe' meant serious impairment and the patient required frequent hospital treatment. Minimum haemoglobin concentrations varied from 2.8/ 12.8 g/dl, with 21 patients having values below 8.5 g/dl. These data relate to a speci®c time during the course of a mainly chronic condition (which sometimes lasted for more Ó 2000 Blackwell Science Ltd., Clin. Lab. Haem., 22, 337±344 44 than 20 years) when, for various reasons full investigations were carried out and biphasic haemolysins detected. Discussion The whole patient group was selected on the basis that activity at ³ 30 °C (in albumin) was a reasonable indicator of a cold autoantibody being clinically signi®cant (Garratty et al., 1977; Garratty 1994). Our ®ndings showed that this was not always the case; and previous studies similarly demonstrated that although in vitro assessment of autoagglutination characteristics tended to correlate with the rate of haemolysis in vivo (Rosse & Adams 1980), there were many exceptions (Abramson 1977; Dacie 1992). Patients with low titre, high thermal amplitude cold agglutinins could be associated with severe 1 haemolysis (Schreiber et al., 1977) and conversely there were cases with high titre, high thermal amplitude cold agglutinins where there was never any evidence of haemolysis (as in many Group 1 patients), even over a period of years (Sniecinski et al., 1988). Our results showed that the pattern of haemolysin activity (Tables 1±3), taken in conjunction with thermal amplitude studies, was a better indicator of the severity of haemolysis than titration results alone. Less than 10% of Group 1 patients (serum haemolysins not detected) had haptoglobin levels of < 0.1 g/l, compared with approximately 30% of Group 2 patients (haemolysins present) and with over 90% of Group 3 patients (where the haemolysins showed biphasic properties). Although a normal haptoglobin level does not necessarily exclude haemolysis (Petz & Garratty 1980), it was felt that equating haptoglobin levels of < 0.1 and ³ 0.4 g/l with the presence and absence of active haemolysis was a reason- 339 13652257, 2000, 6, Downloaded from https://onlinelibrary.wiley.com/doi/10.1046/j.1365-2257.2000.00320.x by Universidad De Chile, Wiley Online Library on [25/05/2024]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License R. J. Sokol et al. M M M M F F 19 55 58 60 60 61 62 64 65 65 66 66 67 68 69 71 75 78 79 79 79 79 79 79 80 NK 83 84 86 90 90 01 02 03 04 05 06 07 08 09 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 2 months > 28 years > 14 years NK > 5 years > 11 years diabetes mellitus CLL NHL Ca lung NK Occasional blood transfusions Blood transfusion Nil Blood transfusion Prednisolone, cyclophosphamide, blood transfusion Prednisolone, cyclophosphamide, blood transfusion Chlorambucil (short course) Warmth, monthly blood transfusion, chlorambucil, prednisolone, splenectomy after 2 years (responded well) Prednisolone, cyclophosphamide, azathioprine, blood transfusion Antibiotics; oxygen; blood transfusion Blood transfusion, chlorambucil Nil Prednisolone; blood transfusion Chlorambucil (short course): blood transfusions iv antibiotics, prednisolone, blood transfusion Nil Blood transfusion Warmth, blood transfusions on three occasions Warmth Prednisolone, blood transfusion Blood transfusion Chlorambucil (short course ± no effect), blood transfusions near end of life Avoidance of cold; prednisolone NK For AML only; nil for CHAD Blood transfusion, prednisolone, chlorambucil, azathioprine, cyclophosphamide, plasma exchange, splenectomy Chlorambucil, prednisolone, blood transfusion Treatment course Blood transfusion, chlorambucil (no response to prednisolone) Nil rheumatoid arthritis Blood transfusion mild/moderate severe Pneumonia moderate/severe NHL mild CLL severe Pemphigoid moderate severe Pneumonia mild/moderate moderate/severe mild/moderate ± mild ± becoming moderate with time NK NK moderate mild NHL died 2 weeks after presentation > 4 years mild > 3 years mild > 2 years mild/moderate > 12 years mild/moderate > 7 years mild/moderate > 13 years severe > 4 years < 1 month > 10 years > 11 years < 2 months > 4 years < 4/12 > 11 years > 6 years > 3 years > 3 years thyrotoxicosis NK AML CLL CRF Associated conditions severe, gradually got worse with time severe carcinomatosis mild moderate mild±severe episodes NK mild moderate/severe Severity NK NK chronic > 3 years NK died 6 days after presentation NK died 2 months severe after presentation chronic died 10 months mild/moderate after presentation chronic died 6 months severe after presentation chronic acute chronic chronic acute chronic acute chronic chronic chronic chronic chronic chronic chronic chronic chronic chronic NK chronic > 20 years acute chronic chronic NK chronic chronic Acute/ Length of chronic time affected Serum haemolysins in CHAD Ó 2000 Blackwell Science Ltd., Clin. Lab. Haem., 22, 337±344 13652257, 2000, 6, Downloaded from https://onlinelibrary.wiley.com/doi/10.1046/j.1365-2257.2000.00320.x by Universidad De Chile, Wiley Online Library on [25/05/2024]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License NK, not known (data not available); CRF, chronic renal failure; AML, acute myeloid leukaemia; CLL, chronic lymphocytic leukaemia; NHL, non-Hodgkin's lymphoma; Ca, carcinoma. M M M F F M F M M M M M F F F F M F F M F M F M F Sex Patient Age at prenumber sentation Table 4. Clinical features of Group 3 patients with biphasic haemolysins 340 able assumption for the purposes of statistical analysis; if anything it made the tests more stringent by excluding patients with marginally reduced levels (0.1±0.3 g/l). The most common autoantibody speci®city in all patient Groups was anti-I, but whether the apparent increasing prevalence from Groups 1±3 (71%, 86% and 94%) was signi®cant cannot be assessed as the number of patients in Group 3 was too small. In other reports, the antibodies also most commonly showed anti-I speci®city; examples of anti-i were proportionally more frequent in CHAD occurring in children and secondary to lymphoproliferative disorders 2 (Pruzanski & Shumak 1977; Crisp & Pruzanski 1982; Nydegger et al., 1991; Englefriet et al., 1992; Garratty 1994). The ability to cause in vitro haemolysis was greater with anti-I than with anti-i (Kirsch®nk et al., 1992). As well as predicting the likelihood of active haemolysis, classi®cation according to the pattern of in vitro haemolysin activity provided an insight into the autoimmune response, with more complex and stronger reactions from Group 1 through to Group 3 patients. Acid (monophasic) haemolysins (pH 6.8) active at 20 °C were found in all patients in Groups 2 and 3 (Tables 2 and 3); but titres of ³ 1 : 16 were found in 47% of Group 2 patients and in 94% of Group 3 patients (data not shown). Furthermore, haemolysin activity at 37 °C (at pH 6.8) was detected in 16% of Group 2 patients compared with 39% in Group 3. The biphasic haemolysins (the criterion for inclusion in Group 3) were usually weakly reacting. The increasingly complex pattern of direct antiglobulin test results from Groups 1±3 showed that the immune response in patients with cold autoagglutinins was more varied (and complex) than commonly thought; as the immune response became IgM predominant, the cold autoantibodies had an increasing ability to activate complement through Groups 1±3, which was re¯ected in increasing haemolysin activity and proportion of patients with active haemolysis, Group 3 patients, with biphasic haemolysins, representing the severest form of CHAD. The ®ndings of increased amounts of IgG and IgA in many patients were thought to re¯ect a more generalized autoimmune response (Sokol et al., 1990a), multiple immunoglobulin coating of red cells per se being known to have an important effect on the degree of haemolysis (Sokol et al., 1990a). These ®ndings were in contrast to those of previous studies in patients with CHAD which stressed the presence of large amounts of complement on the red cells with only rare cases additionally showing small amounts of immunoglobulin (Garratty et al., 1977; 3 Pruzanski & Shumak 1977; Schreiber et al., 1977; Crisp & Pruzanski 1982; Nydegger et al., 1991; Garratty 1994; Gilliland 1996; Berentsen et al., 1997). Ó 2000 Blackwell Science Ltd., Clin. Lab. Haem., 22, 337±344 Patients in Group 3 were predominantly elderly and, apart from one individual aged 19 years, all the others were 55 or over, with a median age of 71 years at presentation (Table 4). Similarly, in other published series, the majority of patients with CHAD (irrespective of their haemolysin status) were over 60 (Crisp & Pruzanski 1982; Hadnagy1993; Nydegger et al., 1991; Dacie 1992; Berentsen et al., 1997); and one report noted that only 8% of patients were under 40 years (Crisp & Pruzanski 1982). CHAD does occur in children, albeit rarely, and our own studies (Sokol et al., 1992) showed that it was at least as common as warm type autoimmune haemolytic anaemia. The slight male bias (ratio 1 : 0.8) was of interest, and an excess of males with CHAD was also noted previously (Nydegger et al., 1991). The majority of patients in this and in other studies; (Rosse & Adams 1980; Crisp & Pruzanski 1982; Nydegger et al., 1991; Berentsen et al., 1997) had the chronic condition; we could not classify a few cases as death occurred within a short time of diagnosis. Only four patients had acute CHAD (Table 4). In one (number 1), this was a brief episode at the time when he was rejecting a renal transplant and was possibly secondary to a viral infection; haemolysis was mild. In two of the three others (numbers 16 and 21), severe haemolysis was associated with pneumonia (though not due to Mycoplasma pneumoniae (Nydegger et al., 1991; Dacie 1992; Rordorf et al., 1994)); in the remaining patient (number 19 ± who also had pemphigoid), there was no obvious precipitating incident; all three individuals were very ill, but eventually made good recoveries without recurrence. In view of the known associations between autoimmune haemolytic anaemia and malignancy (Sokol et al., 1992; Sokol et al., 1994) and between malignancy and age, it was not surprising that several of the patients were also suffering from lymphoid neoplasms or carcinoma (Table 4). The relationship between cold autoagglutinins and lymphoproliferative disorders is complex. Some authorities regard idiopathic CHAD as nonmalignant (although with a slight but de®nite increase in marrow lymphoid cells) (Nydegger et al., 1991); others feel it is a premalignant or low grade lymphoproliferative disease 4 (Berentsen et al., 1997); while yet others think of conditions with persistent cold agglutinins as a spectrum that varies from benign autoimmune chronic CHAD to malignant lymphoma (Crisp & Pruzanski 1982). The natural history of our Group 3 patients with idiopathic chronic CHAD was commonly of mild, well compensated haemolysis that required no treatment for long periods, punctuated with acute episodes of severe haemolysis (67% of patients had haemoglobin levels of less 341 13652257, 2000, 6, Downloaded from https://onlinelibrary.wiley.com/doi/10.1046/j.1365-2257.2000.00320.x by Universidad De Chile, Wiley Online Library on [25/05/2024]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License R. J. Sokol et al. Serum haemolysins in CHAD than 8.5 g/dl and values below 6.0 g/dl were not uncommon) necessitating intensive therapy. This was very much an individual picture and in some patients the treatment requirements became more frequent or greater as time went by; in others they did not. The severity of disease column (Table 4) attempts to show this variation. The condition could remain active for long periods (Table 4), over 28 years in patient 2, which taken with the high age at presentation, suggests that CHAD does not seriously affect the natural lifespan. Those patients who died within a year of presentation either had disseminated malignancy (numbers 8 and 28), or congestive cardiac failure (number 29), or had already reached their 90th birthday (numbers 30 and 31). These ®ndings are in keeping with those in the literature, where most patients with idiopathic CHAD had chronic low grade haemolysis, with occasional acute exacerbations and with very much an individual course to the disease, the patients usually remaining in good general condition (Petz & Garratty 1980; Rosse & Adams 1980; Nydegger et al., 1991; Dacie 1992; Hillen & Bakker 1994; Berentsen et al., 1997). In some patients, there was a progressive worsening of symptoms over the years throughout autumn and winter (Hillen & Bakker 1994). Survival times of greater than 5 years were quoted for idiopathic CHAD and for CHAD associated with chronic lymphocytic leukaemia, but of less than 3 years for patients where the disease was secondary to other lymphoproliferative disorders (Crisp & Pruzanski 1982). Not surprisingly, in view of their high median age, at least 18 of our patients are now known to be deceased, but as far as could be seen from the available hospital case notes, not one died of intractable haemolysis. Fulminating haemolysis causing death is rare in CHAD and only a few individual cases have been reported (Seldon et al., 1980; Rousey & Smith 1990; Mandigers et al., 1996). Treatment varied (Table 4) and was tailored to an individual; in some cases none was needed, or avoidance of cold and/or keeping warm were suf®cient. In other patients, either continuous or intermittent treatment with prednisolone and/or chlorambucil were used with good effect. Yet others (e.g. number 6) required a greater variety and more intense therapy. Antibiotics (and oxygen in one case) were important in the patients with pneumonia. Blood transfusion support was frequently required at times when haemolysis was severe. Splenectomy was carried out in two individuals and was particularly successful in one (number 14). The treatment of associated conditions (Table 4), for example lymphoproliferative malignancies, was often also effective against the CHAD. These treatment modalities were similar to those in the published literature, which also recognized that many cases required no active intervention; otherwise, warmth (or avoidance of cold) supported by blood transfusion on occasions formed the basis of management (Ulvestad 1998; Petz & Garratty 1980; Rosse & Adams 1980; Rosse 5 1990; Nydegger et al., 1991; Englefriet et al., 1992; Rordorf et al., 1994; Berentsen et al., 1997). Chlorambucil was probably ®rst choice if drug treatment was needed (Ulvestad 1998; Chaplin 1982; Englefriet et al., 1992; Rordorf et al., 1994; Berentsen et al., 1997) (though there was a suggestion in two cases that it might have induced the development of lymphoma (Chaplin 1982)). Cyclophosphamide, vincristine, azathioprine, ¯udarabine and monoclonal antibody directed against CD20, with or without plasma exchange and steroids, were also prescribed in various combinations in more severe (or desperate) cases, with varying degrees of success (Seldon et al., 1980; Rousey & Smith 1990; Nydegger et al., 1991; Jacobs 1996; Mandigers et al., 1996; Berentsen et al., 1997; Lee & Kueck 1998). Although steroids (prednisolone) were generally disappointing, exceptions have been reported, particularly in the subgroup of CHAD characterized by low titre, high thermal amplitude cold agglutinins (Lahav et al., 1989; Schreiber et al., 1977; Englefriet et al., 1992; Gilliland 1996); also, the synthetic steroid danazol was successful in 4 patients (Geffray & Najman 1992). There were several reports of the use of a-interferon-2b, some successful (O'Connor et al., 1989; Fest et al., 1994; Rordorf et al., 1994), others not (Hillen & Bakker 1994). Similarly, splenectomy was thought to be of limited value, though exceptions (as our patient 14 exempli®es) were reported (Rordorf et al., 1994; Gilliland 1996). Some authorities have concluded that there is no really satisfactory treatment for CHAD, a view with which we would concur, and it is fortunate that active intervention is not often needed (Rosse 1990; Petz & Garratty 1980). Until the present work, CHAD had never been considered from the perspective of the autoantibodies' ability to cause in vitro haemolysis. Our study showed that haemolysin test results provided valuable information on the complexity of the cold autoimmune response, were signi®cantly related to the likelihood of an autoantibody causing haemolysis in vivo and identi®ed a group of patients, characterized by the presence of biphasic haemolysins, with the severest form of CHAD. Acknowledgements We thank our clinical colleagues for allowing access to case records of patients under their care and Mrs Carol Mitchell for secretarial assistance. Ó 2000 Blackwell Science Ltd., Clin. Lab. Haem., 22, 337±344 13652257, 2000, 6, Downloaded from https://onlinelibrary.wiley.com/doi/10.1046/j.1365-2257.2000.00320.x by Universidad De Chile, Wiley Online Library on [25/05/2024]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License 342 References Abramson N. (1977) Cold agglutinins. New England Journal of Medicine 297, 727±728. Berentsen S., Bù K., Shammas F.V., Myking A.O. & Ulvestad E. (1997) Chronic cold agglutinin disease of the `idiopathic' type is a premalignant or low-grade malignant lymphoproliferative disease. APMIS 105, 354±362. Boccardi V., D'Annibali S., Di Natale G., Girelli G. & Summonti D. (1977) Mycoplasma pneumoniae infection complicated by paroxysmal cold hemoglobinuria with anti-P speci®city of biphasic hemolysin. Blut 34, 211±214. Chaplin H. (1982) Lymphoma in primary cold hemagglutinin disease treated with chlorambucil. Archives of Internal Medicine 142, 2119±2123. Crisp D. & Pruzanski W. (1982) B-cell neoplasms with homogeneous cold-reacting antibodies (cold agglutinins). American Journal of Medicine 72, 915±922. Dacie J. (1992) The Haemolytic Anaemias, Vol. 3, the AutoImmune Haemolytic Anaemias. 3rd edn. Churchill Livingstone. Edinburgh. Englefriet C.P., von Overbeeke M.A.M., dem Borne A.E.G. & Kr. (1992) Autoimmune hemolytic anemia. Seminars in Hematology 29, 3±12. Fest T., de WazieÁres B., Lamy B., Maskani M., Vuitton D. & Dupond J.L. (1994) Successful response to alpha-interferon 2b in a refractory IgM autoagglutinin-mediated hemolytic anemia. Annals of Hematology 69, 147±149. Gardner M.J. & Altman D.G. (1986) Con®dence intervals rather than P values: estimation rather than hypothesis testing. British Medical Journal 292, 746±750. Garratty G. (1994) Autoimmune hemolytic anemia. In: Immunobiology of Transfusion Medicine. (Ed. Garratty G.). Marcel Dekker, New York, 493±521. Garratty G., Petz L.D. & Hoops J.K. (1977) The correlation of cold agglutinin titrations in saline and albumin with haemolytic anaemia. British Journal of Haematology 35, 587±595. Geffray E. & Najman A. (1992) Ef®cacite du danazol dans l'aneÂmie heÂmolytique auto-immune avec agglutinines froides: 4 observations. Presse Medicale 21, 1472±1475. Gilliland B.C. (1996) Autoimmune hemolytic anemia. In: Principles of Transfusion Medicine, 2nd edn. (Ed. Rossi E.C., Simon T.L., Moss G.S. & Gould S.A.) Williams & Wilkins, Baltimore, 101±120. Hadnagy C. (1993) Agewise distribution of idiopathic cold agglutinin disease. Zeitschrift Fur Gerontologie 26, 199±201. Hillen H.F.P. & Bakker S.J.L. (1994) Failure of interferon-a-2b therapy in chronic cold agglutinin disease. European Journal of Haematology 53, 242±243. Jacobs A. (1996) Cold agglutinin hemolysis responding to ¯udarabine therapy. American Journal of Hematology 53, 279±280. Kirsch®nk M., Fritze H. & Roelcke D. (1992) Complement activation by cold agglutinins. Vox Sanguinis 63, 220±226. Lahav M., Rosenberg I. & Wysenbeek A.J. (1989) Steroidresponsive idiopathic cold agglutinin disease: a case report. Acta Haematologica 81, 166±168. Lee E.J. & Kueck B. (1998) Rituxan in the treatment of cold agglutinin disease. Blood 92, 3490±3491. Ó 2000 Blackwell Science Ltd., Clin. Lab. Haem., 22, 337±344 Lindgren S., Zimmerman S., Gibbs F. & Garratty G. (1985) An unusual Donath-Landsteiner antibody detectable at 37°C by the antiglobulin test. Transfusion 25, 142±144. Mack C. (1967) Essentials for Statistics for Scientists and Technologists. Plenum Press. New York. Mandigers C.M.P.W., Keuning J.J. & Booij A.C. (1996) A patient with fatal cold haemagglutinins. Netherlands Journal of Medicine 49, 209±211. Nydegger U.E., Kazatchkine M.D. & Miescher P.A. (1991) Immunopathologic and clinical features of hemolytic anemia due to cold agglutinins. Seminars in Hematology 28, 66±77. O'Connor B.M., Clifford J.S., Lawrence W.D. & Logue G.L. (1989) Alpha-interferon for severe cold agglutinin disease. Annals of Internal Medicine 111, 255±256. Petz L.D. & Garratty G. (1980)Acquired Immune Hemolytic Anemias. Churchill Livingstone. New York. Pruzanski W. & Shumak K.H. (1977) Biologic activity of coldreacting autoantibodies (®rst of two parts). New England Journal of Medicine 297, 538±542. Ratcliff A.P. & Hardwicke J. (1964) Estimation of serum haemoglobin-binding capacity (haptoglobin) on Sephadex G.100. Journal of Clinical Pathology 17, 676±679. Ries C.A., Garratty G., Petz L.D. & Fudenberg H.H. (1971) Paroxysmal cold hemoglobinuria: report of a case with an exceptionally high thermal range Donath-Landsteiner antibody. Blood 38, 491±499. Rordorf R., Barth A., Nydegger U. & Tobler A. (1994) Behandlung einer schweren idiopathischen KaÈlteagglutinin-krankheit mit Interferon-a2b. Schweizerische Medizinische Wochenschrift 124, 56±61. Rosse W.F. (1990) Clinical Immunohematology: Basic Concepts and Clinical Applications. Blackwell Scienti®c Publications. Boston. Rosse W.F. & Adams J.P. (1980) The variability of hemolysis in the cold agglutinnin syndrome. Blood 56, 409±416. Rousey S.R. & Smith R.E. (1990) A fatal case of low titer anti-PR cold agglutinin disease. American Journal of Hematology 35, 286±287. Schreiber A.D., Herskovitz B.S. & Goldwein M. (1977) Low-titer cold-hemagglutinin disease: mechanism of hemolysis and response to corticosteroids. New England Journal of Medicine 296, 1490±1494. Seldon M., Isbister J.P., Raik E. & Biggs J.C. (1980) A fatal case of cold autoimmune hemolytic anemia. American Journal of Clinical Pathology 73, 716±717. Sniecinski I., Margolin K., Shulman I., Oien L., Meyer E. & Branch D.R. (1988) High-titer, high-thermal-amplitude cold autoagglutinin not associated with hemolytic anemia. Vox Sanguinis 55, 26±29. Sokol R.J., Booker D.J. & Stamps R. (1992) The Pathology of autoimmune haemolytic anaemia. Journal of Clinical Pathology 45, 1047±1052. Sokol R.J., Booker D.J. & Stamps R. (1994) Erythrocyte autoantibodies, autoimmune haemolysis, and carcinoma. Journal of Clinical Pathology 47, 340±343. Sokol R.J., Booker D.J. & Stamps R. (1995) Investigation of patients with autoimmune haemolytic anaemia and provision of blood for transfusion. Journal of Clinical Pathology 48, 602±610. 343 13652257, 2000, 6, Downloaded from https://onlinelibrary.wiley.com/doi/10.1046/j.1365-2257.2000.00320.x by Universidad De Chile, Wiley Online Library on [25/05/2024]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License R. J. Sokol et al. Serum haemolysins in CHAD Sokol R.J., Booker D.J. & Stamps R. (1999) Paroxysmal cold haemoglobinuria: a clinico-pathological study of patients with a positive Donath-Landsteiner test. Hematology 4, 137±164. Sokol R.J., Hewitt S., Booker D.J. & Bailey A. (1990a) Red cell autoantibodies, multiple immunoglobulin classes, and autoimmune hemolysis. Transfusion 30, 714±717. Sokol R.J., Hewitt S., Booker D.J. & Bailey A. (1990b) Erythrocyte autoantibodies, subclasses of IgG and autoimmune haemolysis. Autoimmunity 6, 99±104. Sokol R.J., Hewitt S., Booker D.J. & Morris B.M. (1988a) Patients with red cell autoantibodies: selection of blood for transfusion. Clinical and Laboratory Haematology 10, 257±264. Sokol R.J., Hewitt S., Booker D.J., Stamps R. & Booth J.R. (1988b) An enzyme-linked direct antiglobulin test for assessing erythrocyte bound immunoglobulins. Journal of Immunological Methods 106, 31±35. Sokol R.J., Hewitt S. & Stamps B.K. (1981) Autoimmune haemolysis: an 18-year study of 865 cases referred to a regional transfusion centre. British Medical Journal 282, 2023±2027. Ulvestad E. (1998) Paradoxical haemolysis in a patient with cold agglutinin disease. European Journal of Haematology 60, 93±100. Wolach B., Heddle N., Barr R.D., Zipursky A., Pai K.R.M. & Blajchman M.A. (1981) Transient Donath-Landsteiner haemolytic anaemia. British Journal of Haematology 48, 425±434. Ó 2000 Blackwell Science Ltd., Clin. Lab. Haem., 22, 337±344 13652257, 2000, 6, Downloaded from https://onlinelibrary.wiley.com/doi/10.1046/j.1365-2257.2000.00320.x by Universidad De Chile, Wiley Online Library on [25/05/2024]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License 344