![Continuum 2023 Vol 29.2[012-024]](http://s2.studylib.es/store/data/009457599_1-40e1052650b6faae8031b1dd64db9a92-768x994.png)
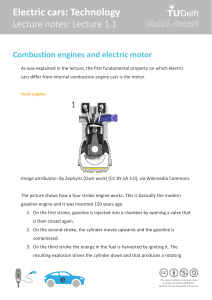
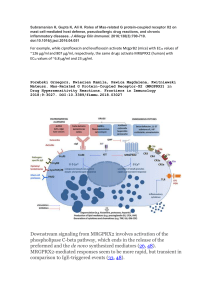
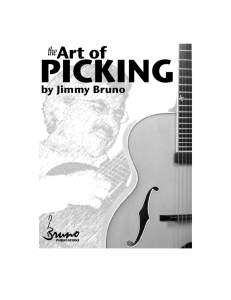
REVIEW ARTICLE C O N T I N UU M A UD I O I NT E R V I E W A V AI L A B L E ONLINE Diagnostic Evaluation of Stroke Etiology By James F. Meschia, MD, FAAN ABSTRACT OBJECTIVE: Precise therapies require precise diagnoses. This article provides an evidence-based approach to confirming the diagnosis of ischemic stroke, characterizing comorbidities that provide insights into the pathophysiologic mechanisms of stroke, and identifying targets for treatment to optimize the prevention of recurrent stroke. LATEST DEVELOPMENTS: Identifying the presence of patent foramen ovale, intermittent atrial fibrillation, and unstable plaque is now routinely included in an increasingly nuanced workup in patients with stroke, even as ongoing trials seek to clarify the best approaches for treating these and other comorbidities. Multicenter trials have demonstrated the therapeutic utility of patent foramen ovale closure in select patients younger than age 60 years. Insertable cardiac monitors detect atrial fibrillation lasting more than 30 seconds in about one in ten patients monitored for 12 months following a stroke. MRI of carotid plaque can detect unstable plaque at risk of being a source of cerebral embolism. ESSENTIAL POINTS: To optimize the prevention of recurrent stroke, it is CITE AS: CONTINUUM (MINNEAP MINN) 2023;29(2, CEREBROVASCULAR DISEASE):412–424. Address correspondence to Dr James F. Meschia, Division of Cerebrovascular Disease, Department of Neurology, Mayo Clinic, Jacksonville, FL 32224, [email protected]. RELATIONSHIP DISCLOSURE: The institution of Dr Meschia has received research support from the National Institute of Neurological Disorders and Stroke. UNLABELED USE OF PRODUCTS/INVESTIGATIONAL USE DISCLOSURE: Dr Meschia reports no disclosure. © 2023 American Academy of Neurology. important to consider pathologies of intracranial and extracranial blood vessels and of cardiac structure and rhythm as well as other inherited or systemic causes of stroke. Some aspects of the stroke workup should be done routinely, while other components will depend on the clinical circumstances and preliminary testing results. INTRODUCTION ith the advent of evidence-based mechanical thrombectomy, it is tempting to view all ischemic strokes as falling into two broad categories: strokes caused by an accessible clot (large vessel occlusion) and everything else. This perspective, while pragmatic when presented in the emergency department with a patient with acute stroke, is woefully inadequate when attempting to optimize prevention of recurrent stroke. To optimize prevention, a more nuanced characterization of stroke is required. While trying to identify stroke etiology is customary, usually etiology can only be inferred through identifying, or not identifying, various comorbidities. Often we cannot be certain that a specific comorbidity truly was on the causal pathway to the presenting stroke, in part because multiple comorbidities frequently coexist in the same patient. For some comorbidities, such as carotid atherosclerotic stenosis, whether a specific W 412 APRIL 2023 Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited. treatment (eg, endarterectomy) is indicated depends on whether the comorbidity is believed to be mechanistically related to stroke by perfusion zone (eg, symptomatic versus asymptomatic stenosis). For other comorbidities, such as atrial fibrillation, the indicated treatment is influenced by the increased risk associated with a history of stroke. For example, stroke increases the CHA2DS2-VASc risk estimation score (consisting of congestive heart failure, hypertension, age 75 years or older, diabetes mellitus, previous stroke, vascular disease, age 65 to 74 years, and sex category) by two points.1 Reference to a “stroke workup” (ie, a set of diagnostic tests performed because a patient has had a recent stroke) can be found in the medical literature since at least the early 1980s.2 The stroke workup has advanced in parallel with progress in diagnostic technologies and medical and interventional therapies. While some elements of the stroke workup should be done routinely in nearly all cases, other elements are contingent on clinical circumstances. Recently, the American Heart Association/ American Stroke Association (AHA/ASA) published evidence-based guidelines on stroke prevention in patients with recent stroke or transient ischemic attack (TIA).3 These guidelines have a section on the diagnostic evaluation of patients that includes an algorithm for ordering diagnostic tests annotated with class of recommendation and level of evidence for each decision (FIGURE 1-1). This article explains the AHA/ASA guidelines, puts them in clinical context, and highlights recent substantial advances. Hemorrhagic stroke will be addressed only insofar as it can mimic ischemic stroke at presentation. CLINICAL ASSESSMENT Before launching into a diagnostic workup, a focused but detailed clinical assessment of the patient experiencing stroke should be performed.4 The history of the present illness will include stroke symptoms and time last known to be at neurologic baseline. Patients should be questioned about recent prior transient neurologic deficits consistent with TIAs. Often these events will not be volunteered spontaneously because the patient is overwhelmed with concern over their presenting symptoms. If multiple TIAs have occurred, the physician should determine whether they all conform to dysfunction in the same area of perfusion (eg, left anterior circulation), which would suggest upstream atherosclerotic stenosis, and how many attacks occurred within 2 weeks of presentation (three or more attacks suggests unstable plaque).5 The physician should ask about head or neck trauma or high-velocity chiropractic neck manipulation, as these may cause arterial dissection.6 The physician should also inquire about the use of drugs that can precipitate stroke such as amphetamines and cocaine.7 Although understudied, routine use of cannabis appears to significantly increase risk of stroke.8 Head or neck external beam radiotherapy should also be queried, as this can cause a vasculopathy. Vascular risk factors need to be surveyed, including the status of atrial fibrillation and all the components of CHA2DS2-VASc. A history of migraine should also be discussed, as migraine can be a stroke mimic or chameleon9 as well as a risk factor or cause of stroke.10 Migraine with or without aura is also an important component of the cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) phenotype. Head, neck, and chest pain can point to various stroke-relevant conditions, such as cervicocephalic arterial dissection, aortic dissection, or myocardial infarction.11 A family history of dementia, migraines, venous thrombosis, and premature atherosclerosis, not KEY POINTS ● The stroke workup is the set of diagnostic tests performed to gain insight into modifiable risk factors and stroke mechanism. The stroke workup has fixed and variable components, the latter being contingent on clinical circumstances, initial testing, and therapeutic objectives. ● Recent American Heart Association guidelines on secondary stroke prevention include an algorithm for performing an evidence-based diagnostic evaluation. ● Three or more transient ischemic attacks in a 2-week period in the same arterial distribution suggest an unstable atherosclerotic plaque as a mechanism. ● A stroke evaluation should include examining the patient for preceding strokes or transient ischemic attacks, atherosclerotic risk factors, head or neck trauma or radiation therapy, migraines, and a family history of stroke or dementia. CONTINUUMJOURNAL.COM Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited. 413 DIAGNOSTIC EVALUATION OF STROKE ETIOLOGY FIGURE 1-1 Algorithm for evaluating patients with a clinical diagnosis of stroke to optimize prevention of recurrent stroke. CT = computed tomography; CTA = computed tomography angiography; ECG = electrocardiography; MRA = magnetic resonance angiography; MRI = magnetic resonance imaging; SOE = source of embolism; TEE = transesophageal echocardiography. a When a patient has a transient neurologic deficit clinically characteristic of transient ischemic attack, the patient should be evaluated in the same manner as a patient who has an ischemic stroke with a corresponding cerebral infarct on imaging. b Basic laboratory tests include complete blood count, troponin, prothrombin time, partial thromboplastin time, glucose, hemoglobin A1c, creatinine, and fasting or nonfasting lipid profile. Reprinted with permission from Kleindorfer DO, et al, Stroke.3 merely stroke, must be obtained to properly assess potential heritable risk factors. Cursory screening examinations miss strokes. Emergency medical services miss about one-fourth of strokes using screening examinations like FAST (facial drooping, arm weakness, speech difficulties, and time of onset).12 The most common symptoms among false-negative stroke cases are speech disturbance, nausea and vomiting, dizziness, changes in mental status, and visual complaints. 414 APRIL 2023 Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited. Every patient should have a National Institutes of Health Stroke Scale (NIHSS) assessment performed by a certified examiner. The acute NIHSS score, which is an excellent predictor of outcomes, also moderately correlates with acute diffusion-weighted imaging (DWI) and perfusion-weighted imaging lesion volumes.13 However, an NIHSS score of 0 does not mean that the patient has not had a stroke. Nearly 5% of strokes, most of which are lacunar and infratentorial, will score a 0 on the NIHSS.14 These 0-point strokes are not benign and have similar stroke recurrence rates as other stroke types. All potential acute stroke patients deserve a thorough neurologic examination; however, given the time constraints of decision making in the emergency department, a thorough neurologic examination may not be appropriate at the time. Nonetheless, after performing an NIHSS assessment, if uncertainty about whether the patient had a stroke remains, a few quick bedside tests can enhance the NIHSS examination to bring out focal deficits often poorly characterized or missed entirely by the scale. Dysarthria testing in the NIHSS is not very sensitive. The patient can be asked to repeat “PA-TA-KA” three or four times to elicit scanning dysarthria or other impairment in forming labial, lingual, or fricative sounds. The physician can also perform “H” testing for external ophthalmoparesis and test for clumsy hands or distal weakness by having the patient tap the thumb and index finger as fast as possible (test each side separately to avoid mirror movements) and look for left-right asymmetry. Head CT, CT angiography, and, where appropriate, CT perfusion should be obtained as soon as possible to provide information about vessel occlusion, infarct core, ischemic penumbra, and degrees of collaterals (the so-called “imaging is brain” paradigm).15 Because of this time pressure, performing a thorough neurovascular clinical assessment prior to imaging is neither realistic nor even appropriate, but after the go/no-go decisions to proceed with thrombolysis or mechanical thrombectomy have been made, one should return to the patient’s bedside and explore the clinical case in greater detail. KEY POINTS ● Nearly 5% of strokes, most of which are lacunar and infratentorial, have a National Institutes of Health Stroke Scale (NIHSS) score of 0. Although these strokes are usually not treated with thrombolytics, they are nonetheless important to recognize because the stroke recurrence rates for NIHSS 0 and non-0 strokes are very similar. ● Nearly 7% of acute ischemic strokes do not have a focal area of restricted diffusion on initial diffusion-weighted imaging. Patients with posterior circulation stroke are 5 times as likely to have diffusionweighted imaging–negative stroke as patients with anterior circulation stroke. BRAIN IMAGING The first diagnostic step after clinical assessment is to determine with CT or MRI of the head whether a patient who presents with signs and symptoms of an acute stroke has had an acute ischemic stroke (AHA/ASA class 1 recommendation).3 National guidelines recommend initial imaging within 25 minutes of arrival at a stroke center to screen patients for thrombolysis with or without thrombectomy.16 Patients routinely receive a head CT combined with CT angiography, with or without CT perfusion, to rule out intracranial hemorrhage and assess for large vessel occlusion and ischemic penumbra. In many instances, this imaging is sufficient to confirm the diagnosis of acute ischemic stroke, although small strokes are often missed. If the patient remains symptomatic and multimodal CT imaging does not confirm the diagnosis, then MRI with DWI will often suffice. DWI is so sensitive and specific for acute cerebral infarcts, even for punctate lesions of only a few millimeters, that it is sometimes forgotten that a negative scan does not completely rule out a stroke (CASE 1-1). Nearly 7% of patients with acute ischemic stroke will have DWI-negative stroke.17 Patients with posterior circulation stroke are 5 times as likely to have DWI-negative stroke as patients with anterior circulation stroke.17 A head CT can reasonably be avoided in favor of MRI in neurologically stable patients who present late or with minor, nondisabling deficits. For patients who CONTINUUMJOURNAL.COM Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited. 415 DIAGNOSTIC EVALUATION OF STROKE ETIOLOGY present late, the brain MRI should include DWI sequences. In a consecutive series of 300 patients presenting 3 or more days after TIA or minor stroke, DWI showed a high-signal lesion in 70% of cases of stroke and 13% of cases of TIA and provided clinically meaningful information (eg, confirming the diagnosis or vascular territory of the lesion) in 36% of cases.18 Patients with minor (NIHSS score ≤3), nondisabling (modified Rankin scale, 0 or 1) stroke do not clearly benefit from thrombolytic therapy and rarely have a large vessel occlusion that requires immediate thrombectomy, so the timeliness of multimodal CT can be traded for the diagnostic yield of MRI. The diagnostic yield of DWI falls with lower NIHSS scores17 but remains clinically meaningful, even for patients with resolved deficits (TIAs).19 MRI with DWI can detect acute ischemic stroke in about 20% of patients presenting with acute dizziness and vertigo, whereas the sensitivity of CT for diagnosing acute ischemic stroke (typically posterior inferior cerebellar artery infarcts) in this patient population is under 10%.20 CASE 1-1 A 93-year-old man with hypertension presented to the emergency department with sudden generalized weakness, which had begun the previous day. The morning of presentation he could barely get out of bed and fell while trying to get to the bathroom. His son had to help him get off the floor. He did not hit his head, and the patient denied trouble with balance, vision, facial droop, speech, or language. On repeated questioning, he endorsed that his weakness may have been worse on his left side. He denied prior strokes, other neurologic illnesses, cancer, fevers, chills, shortness of breath, angina pectoris, or recent change in medications. He was taking lisinopril and hydrochlorothiazide. His temperature was 36.6°C (97.8°F), and his blood pressure was 162/95 mm Hg. His general physical examination was unremarkable. His National Institutes of Health Stroke Scale score was 6 (his left arm had some effort against gravity; right arm and both legs drifted; and there was ataxia on left-sided finger-to-nose testing). Complete blood count, basic metabolic panel, and thyroid-stimulating hormone (TSH) were normal, and chest x-ray showed clear lungs. Urinalysis showed no signs of infection. Head CT showed no acute intracranial abnormality. Brain MRI revealed an acute subcortical infarction in the right paracentral lobule and old small infarcts in the right frontal corona radiata and right thalamus as well as extensive small vessel ischemic disease seen on T2 fluid-attenuated inversion recovery (FLAIR). (FIGURE 1-2) CT angiography revealed highly calcified stenosis (<50%) of the right internal carotid artery. Transthoracic echocardiogram detected concentric left ventricular hypertrophy and a left ventricular ejection fraction of 71%. In-patient cardiac monitoring showed no atrial fibrillation. 416 APRIL 2023 Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited. Patients with nonlacunar stroke can present with a classic lacunar syndrome: ataxic hemiparesis, dysarthria–clumsy hand syndrome, pure hemiparesis, pure hemisensory loss, or sensorimotor stroke. Almost one in six patients presenting with a classic lacunar syndrome has multiple infarctions demonstrated on DWI.21 MRI is usually required to detect acute infarcts in multiple cerebral circulations. This pattern of lesions can be found in about 10% of patients with acute infarction and is attributable to cardioembolism half of the time and less frequently to a hematologic or vasculitic mechanism.22 CERVICOCEPHALIC ARTERIAL IMAGING The AHA/ASA regards noninvasive imaging by ultrasonography, CT angiography, or magnetic resonance angiography (MRA) of the cervical anterior circulation (both carotid arteries) as a class 1 recommendation in patients with symptomatic infarction in the zone perfused by the anterior circulation.3 The FIGURE 1-2 Imaging of the patient in CASE 1-1. Axial diffusion-weighted (A) and T2 fluid-attenuated inversion recovery (FLAIR) (B) sequences of brain MRI showing an acute ischemic stroke and severe cerebral small-vessel ischemic disease. If the patient’s MRI had been delayed it might have been impossible to appreciate that there had been an acute focal area of ischemia given the preexisting severe white matter ischemic changes. This patient presented with vague symptoms of generalized weakness, but the abrupt onset and slight asymmetry to the motor examination favored diagnosis of an acute stroke. The head CT was only helpful in excluding an intraparenchymal or subdural hemorrhage that could present similarly. Although suspicion was high for an acute ischemic stroke after the CT, the brain MRI was helpful in securing a positive diagnosis. Knowing the size and location of the acute infarct and the presence of comorbid small vessel disease also helps with prognostication and planning of rehabilitation. CONTINUUMJOURNAL.COM Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited. COMMENT 417 DIAGNOSTIC EVALUATION OF STROKE ETIOLOGY CASE 1-2 A 75-year-old right-handed man noted the sudden onset of numbness and clumsiness in his left hand. He chose to go to bed and see if his symptoms would pass; when they did not, he presented for medical attention at the emergency department. He had a history of hyperlipidemia, but no prior neurologic history. He quit cigarette smoking more than two decades prior. He denied chest pain or palpitations. Vital signs were unremarkable. His National Institutes of Health Stroke Scale score was 7 (aphasia and left-sided numbness and weakness). Initial head CT showed an old right frontal infarction, but no acute changes. CT angiography showed no large vessel occlusion but did show an estimated 50% to 70% stenosis of the cervical right internal carotid artery. The next day a brain MRI showed scattered infarcts in the right frontal parietal lobes on DWI and a right frontal gliotic infarct on T2 fluid-attenuated inversion recovery (FLAIR). MR angiography estimated the right internal carotid artery stenosis to be 50%. MR plaque imaging (FIGURE 1-3) showed hemorrhagic plaque with a lipid core in the right carotid bifurcation extending 18 mm into the internal carotid artery. The patient was referred for revascularization. FIGURE 1-3 Imaging of the patient in CASE 1-2. Two-dimensional spin echo T1-weighted double inversion recovery images in two consecutive axial sections (A, B) of the neck at the C3 to C4 levels of the cervical spine show hemorrhagic plaque in the right internal carotid artery. Arrows indicate hyperintensities in the carotid plaque corresponding to plaque hemorrhage. MRI can be protocoled to highlight several features of plaque composition that indicate a so-called unstable or vulnerable plaque. There is an increased risk of stroke recurrence in the territory of brain supplied by an artery with vulnerable plaque. COMMENT This patient presented outside of a time window to allow for safe thrombolysis and did not have a large vessel occlusion to treat with mechanical thrombectomy. However, MRI was useful in ensuring that his stroke involved the right anterior circulation. CT angiography and MR angiography supported a moderate-to-severe carotid stenosis of the right internal carotid artery. Plaque characteristics were those seen in so-called vulnerable or unstable plaque and represented high-risk features. Most studies support early revascularization (within 2 weeks, and preferably within 2 days). 418 APRIL 2023 Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited. AHA/ASA regards noninvasive imaging using CT angiography or MRA of the posterior circulation (vertebrobasilar arteries) and intracranial arteries as a class 2a recommendation.3 The difference in recommendation level can be explained by the proven effectiveness of revascularization of a highly stenotic symptomatic cervical carotid artery, whereas there is no compelling evidence for angioplasty, stenting, or surgery of symptomatic vertebrobasilar or intracranial arteries. The distinction between imaging anterior versus posterior and intracranial arteries is moot for most patients as those with suspected ischemic stroke are now routinely submitted to emergent CT angiography of head and neck to screen for large vessel occlusion warranting attempted mechanical thrombectomy. CT angiography is particularly good for detecting carotid webs, which appear as a thin intraluminal filling defect along the posterior wall of the carotid bulb just distal to the bifurcation on oblique sections and as a septum on axial sections.23 If protocoled appropriately, vessel-wall imaging using MRI technology can identify several features associated with plaque vulnerability: intraplaque hemorrhage, a lipid-rich necrotic core, and thinning of the fibrous cap (CASE 1-2).24 KEY POINTS ● CT angiography in the oblique and axial planes is the imaging modality of choice for identifying carotid webs. ● Long-term cardiac rhythm monitoring detects severalfold more cases of atrial fibrillation than routine inpatient monitoring following a stroke (12.1% versus 1.8%), although the minimum burden of intermittent atrial fibrillation to justify anticoagulation remains uncertain. CARDIAC RHYTHM ASSESSMENT Every patient with stroke should have an ECG to screen for atrial fibrillation or flutter and, even if there is a well-documented history of atrial fibrillation, to screen for cardiac comorbidities like acute or chronic myocardial infarction and left ventricular hypertrophy (AHA/ASA class 1 recommendation).3 Long-term rhythm monitoring is an AHA/ASA class 2a recommendation for patients with cryptogenic stroke and no contraindication to anticoagulation.3 This monitoring can be done in various ways, including mobile cardiac outpatient telemetry or an insertable loop recorder. The longer the rhythm is monitored the more likely atrial fibrillation is to be detected. For example, in the STROKE-AF (Rate of Atrial Fibrillation Through 12 Months in Patients With Recent Ischemic Stroke of Presumed Known Origin) trial, 12 months of insertable cardiac monitoring detected severalfold more cases of atrial fibrillation than routine care in patients with recent ischemic stroke (12.1% versus 1.8%).25 Currently, oral anticoagulation is an AHA/ASA class 1 (level of evidence B-R) recommendation for atrial fibrillation, whether paroxysmal, persistent, or permanent.3 However, uncertainty remains around the optimal duration of monitoring and the minimum burden of atrial fibrillation detection necessary to justify long-term oral anticoagulation. As noted in a recent editorial,26 trials have shown that many patients have subclinical atrial fibrillation after non–atrial-fibrillation-related ischemic stroke; the longer the monitoring, the more subclinical atrial fibrillation will be detected. Furthermore, there appears to be a dose relationship between duration of atrial fibrillation and stroke risk.27 Future trials are underway to clarify the threshold of subclinical atrial fibrillation that justifies long-term anticoagulation. STRUCTURAL CARDIAC IMAGING Echocardiography with or without contrast is an AHA/ASA class 2a recommendation for patients with cryptogenic stroke. Transesophageal echocardiography (TEE), cardiac CT, or cardiac MRI of patients with embolic stroke of undetermined significance is an AHA/ASA class 2b recommendation.3 Echocardiography can detect a host of pathologies that predispose a patient to cardioembolism; some are common, such as patent foramen ovale, and many are CONTINUUMJOURNAL.COM Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited. 419 DIAGNOSTIC EVALUATION OF STROKE ETIOLOGY rare, such as atrial myxoma, papillary fibroelastoma, and valvular vegetations. Many echocardiographically detected abnormalities are likely etiologically related but are not likely to change management. For example, patients with known atrial fibrillation and a moderate to high CHA2DS2-VASc score need long-term oral anticoagulation regardless of whether a thrombus is identified by echocardiography in the left atrium, left atrial appendage, or aorta. TEE is generally considered more sensitive and specific than transthoracic echocardiogram (TTE) for detecting sources of cardioembolism, but the discovery of pathologies that should alter management occurs in less than 5% of cases.28 TEE, the more invasive test, may be less effective in detecting patent foramen ovale than TTE with contrast and the Valsalva maneuver.29 EMBOLIC STROKE OF UNDETERMINED SOURCE Embolic stroke of undetermined source (ESUS) is a diagnostic subset of ischemic stroke. ESUS is a diagnosis made by negation (ie, that the stroke is not lacunar in size and is not associated with large vessel high-grade stenosis or obvious cardiac source of embolism).30 ESUS is a subset of cryptogenic stroke. A stroke may be cryptogenic because a cursory workup failed to identify an etiology. However, ESUS requires a certain diagnostic intensity, with a proposed workup including brain imaging, ECG, transthoracic echocardiography, cardiac monitoring for at least 24 hours, and imaging of both intracranial and extracranial arteries.30 Only when and if clinical trials clearly establish that patients with ESUS require treatment different from patients without ESUS will the concept truly be proven useful. TESTING FOR INHERITED STROKE SYNDROMES Testing for single-gene disorders that cause stroke is of vanishingly low yield in most stroke patients and should not be done routinely. However, certain clinical scenarios should push the neurologist to perform targeted testing. This author has found the yield to be much higher when patients have a positive family history or a plethora of recurrent strokes and a paucity of conventional risk factors, particularly if the strokes appear to be related to small vessel disease (<15-mm infarcts with unremarkable MRA or CT angiography). There are many well-characterized monogenic cerebral small vessel diseases: CADASIL; cerebral autosomal recessive arteriopathy with subcortical infarcts and leukoencephalopathy (CARASIL); pontine autosomal dominant microangiopathy and leukoencephalopathy (PADMAL); Fabry disease; mitochondrial encephalopathy, lactic acidosis, and strokelike episodes (MELAS); and type IV collagen–related diseases (COL4A1/COL4A2 mutations).31,32 At present, none of these conditions are curable, but that should not dissuade the neurologist from securing a definitive diagnosis with gene testing. A definitive diagnosis can avoid mistreatment for conditions that the patient does not have (eg, multiple sclerosis or central nervous system [CNS] vasculitis). Family history taking has evolved in the postgenomic era; some patients may present as at-risk because they were contacted by a relative about the results of a direct-to-consumer genomic test that found a mutation in NOTCH3. Ultimately, if a patient is diagnosed with a monogenic stroke syndrome, the physician should refer the patient to genetic counseling to properly review who may or may not be at risk in a family and what the medical, occupational, and social implications are for presymptomatic testing. 420 APRIL 2023 Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited. HEMATOLOGIC DISORDERS AND HYPERCOAGULABLE STATES It is vital to diagnose sickle cell disease or be aware of the diagnosis in patients who present with stroke because proven, highly effective therapies exist, including hydroxycarbamide, blood transfusions, and hematopoietic stem cell transplantation.33 Sickle cell disease causes ischemic stroke, hemorrhagic stroke, and moyamoya vasculopathy. In children and adolescents, transcranial Doppler screening for elevated blood flow velocities in the middle cerebral artery can detect signs of an emerging vasculopathy for which exchange transfusions dramatically reduce the risk of stroke. Indiscriminate screening for thrombophilia is low yield in patients with ischemic stroke. Testing patterns vary greatly, and testing results in a treatment change only about 1% to 8% of the time.34 Among young patients with ischemic stroke, rates of positive thrombophilia screening are higher but management changes in only 8% of patients.35 Screening for hypercoagulable states like protein C, protein S, and antithrombin III deficiencies, and factor V Leiden and prothrombin 20210 mutations seems justifiable in patients with cerebral venous thrombosis.36 Antiphospholipid antibody syndrome is an acquired hypercoagulable state in which the main manifestations are recurrent thromboses (thrombotic antiphospholipid syndrome) and pregnancy complications (obstetric antiphospholipid syndrome). Current diagnostic criteria require persistently (12 or more weeks) positive lupus anticoagulant, anti–β2 glycoprotein I, or anticardiolipin antibodies.37 Routine screening for antiphospholipid antibodies is hard to justify. APASS (Antiphospholipid Antibody and Stroke Study) was a prospective, observational study nested within a multicenter randomized trial of warfarin versus aspirin for the prevention of stroke recurrence. This study of more than 1700 patients did not find the presence of antiphospholipid antibodies to predict increased stroke risk or a differential response to treatment.38 Diagnostic nihilism is not appropriate either. Some patients can have a severe variant of the syndrome known as catastrophic antiphospholipid syndrome, a life-threatening syndrome requiring immediate treatment.39 INFECTIOUS CAUSES OF STROKE Being vigilant for an infectious etiology is crucial, not because it is common, but because delay in diagnosis can have devastating consequences. Embolism from infective endocarditis occurs in less than 2% of all patients hospitalized with stroke.40 Both native and prosthetic valves can become infected. Although transcatheter aortic valve replacement generally has lower overall risk than open surgical aortic valve replacement, the risk of subsequent endocarditis appears to be comparable with both valve procedures.41 In an administrative data review of nonfederal acute care hospitals in California, the absolute increase in risk of stroke was 9.1% in the month after diagnosis of infectious endocarditis.42 Interestingly, the risk of stroke was significantly elevated in the 4 months preceding the diagnosis of infectious endocarditis. While this increased risk might be the result of a systemic inflammatory state, some of the increase might be due to delayed diagnosis of infective endocarditis. Suspicion for infective endocarditis should be raised if C-reactive protein levels are higher than 10 mg/L.40 In most patients with known or suspected infective endocarditis, acute ischemic lesions and cerebral microbleeds are seen on brain MRI, with other hemorrhagic lesions seen in about KEY POINTS ● Transesophageal echocardiography may be less sensitive in detecting patent foramen ovale than contrasted transthoracic echocardiography. ● To diagnose embolic stroke of undetermined source, patients should have a stroke workup that includes, at a minimum, brain imaging, ECG, transthoracic echocardiography, cardiac monitoring for at least 24 hours, and imaging of both intracranial and extracranial arteries. ● The yield of testing for genetic stroke syndromes is much higher when patients have a positive family history or a plethora of recurrent strokes and a paucity of conventional risk factors, particularly if the strokes are due to small vessel disease. ● Patients with aseptic cerebral venous thrombosis should be screened for thrombophilia. ● A C-reactive protein level higher than 10 mg/L should raise suspicion for stroke caused by endocarditis. CONTINUUMJOURNAL.COM Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited. 421 DIAGNOSTIC EVALUATION OF STROKE ETIOLOGY one-fourth of patients and intracranial mycotic aneurysms occurring in less than 10% of patients.43 DWI may help differentiate acute cardioembolism from infective endocarditis from nonbacterial thrombotic endocarditis. One large, single-center study found that all patients (14/14) with nonbacterial thrombotic endocarditis had numerous <10 mm, 10 mm to 30 mm, and >30 mm lesions in multiple territories, whereas patients with infective endocarditis showed different patterns, including having a single lesion, a territorial infarction, or disseminated punctate lesions.44 When clinical suspicion for infective endocarditis is high, it may be necessary to repeat echocardiography, optimally TEE, to secure a diagnosis.45 In addition to infections causing endocarditis and, secondarily, cardioembolism, infections can cause stroke through cerebral vasculitis.46 The microbiological differential diagnosis is quite different; common conditions and organisms associated with infectious cerebral vasculitis include syphilis, Lyme disease, invasive fungi, and herpes zoster. Headache, seizures, and encephalopathy are commonly associated with stroke due to infectious cerebral vasculitis. Diagnosis of an infectious cerebral vasculitis typically requires angiography (CT angiography, MRA, or digital-subtraction catheter angiography) as well as appropriate microbiological studies of blood and CSF. Sometimes brain biopsy is required. AUTOINFLAMMATORY CENTRAL NERVOUS SYSTEM VASCULITIS Stroke is rarely caused by noninfectious vasculitis, so vigilance is required for early diagnosis. Several rheumatologic conditions can cause CNS vasculitis: giant cell arteritis, Takayasu disease, eosinophilic granulomatosis with polyangiitis, granulomatosis with polyangiitis, polyarteritis nodosa, and Buerger disease. Clues found during the neurologic evaluation that lead to the diagnosis of an underlying systemic vasculitis causing CNS vasculitis include mononeuritis multiplex, visual loss, seizures, muscle disease, and encephalopathy.47 Primary CNS vasculitis is particularly challenging to diagnose. Suspicion for the condition may be raised in an individual who is 40 to 60 years old who has headache, encephalopathy, and ischemic or hemorrhagic strokes. A normal brain MRI practically excludes the diagnosis, while an abnormal CSF is seen in 80% to 90% of affected individuals.48 Brain biopsy is the only way of securing a definitive premortem diagnosis, but sensitivity is poor. If the cerebral angiogram is consistent with CNS vasculitis, there may be reluctance to pursue a tissue diagnosis. However, brain biopsy may identify a lymphoproliferative disease or an infectious vasculitis in more than 30% of cases.49 CONCLUSION The stroke workup has evolved and expanded with advances in diagnostic testing and refinement in clinical trials of stroke prevention. Some tests are fundamental to nearly every patient, while others should be performed only in response to positive or negative results of first-round testing or in the context of specific clinical situations (eg, strongly positive family history of stroke). Because the stroke evaluation has fixed and variable elements, the workup may be at risk of cognitive biases like anchoring, premature closure, and availability of testing.50 It is important to revisit presumptions of etiology, particularly when patients have recurrent stroke despite good medical compliance. 422 APRIL 2023 Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited. REFERENCES 1 Lip GYH, Nieuwlaat R, Pisters R, et al. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest 2010;137(2): 263-272. doi:10.1378/chest.09-1584 13 Fink JN, Selim MH, Kumar S, et al. Is the association of National Institutes of Health Stroke Scale scores and acute magnetic resonance imaging stroke volume equal for patients with right- and lefthemisphere ischemic stroke? Stroke 2002;33(4): 954-958. doi:10.1161/01.str.0000013069.24300.1d 2 Barber F, Rosen P, Okin T. Atrial myxoma presenting as stroke. Ann Emerg Med 1982;11(6): 316-318. doi:10.1016/s0196-0644(82)80132-7 14 Eskioglou E, Huchmandzadeh Millotte M, Amiguet M, Michel P. National Institutes of Health Stroke Scale zero strokes. Stroke 2018;49(12):3057-3059. doi:10.1161/STROKEAHA.118.022517 3 Kleindorfer DO, Towfighi A, Chaturvedi S, et al. 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke 2021;52(7):e364-e467. doi:10.1161/STR. 0000000000000375 4 Southerland AM. Clinical evaluation of the patient with acute stroke. Continuum (Minneap Minn) 2017;23(1, Cerebrovascular Disease):40-61. doi:10.1212/CON.0000000000000437 5 Fereydooni A, Gorecka J, Xu J, et al. Carotid endarterectomy and carotid artery stenting for patients with crescendo transient ischemic attacks: a systematic review. JAMA Surg 2019; 154(11):1055-1063. doi:10.1001/jamasurg.2019.2952 6 Biller J, Sacco RL, Albuquerque FC, et al. Cervical arterial dissections and association with cervical manipulative therapy: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2014;45(10):3155-3174. doi:10.1161/STR. 0000000000000016 7 Middlekauff HR, Cooper ZD, Strauss SB. Drugs of misuse: focus on vascular dysfunction. Can J Cardiol 2022;38(9):1364-1377. doi: 10.1016/j. cjca.2022.04.011 8 Page RL, 2nd, Allen LA, Kloner RA, et al. Medical marijuana, recreational cannabis, and cardiovascular health: a scientific statement from the American Heart Association. Circulation 2020;142(10):e131-e152. doi:10.1161/ CIR.0000000000000883 9 Otlivanchik O, Liberman AL. Migraine as a stroke mimic and as a stroke chameleon. Curr Pain Headache Rep 2019;23(9):63. doi:10.1007/ s11916-019-0801-1 10 Øie LR, Kurth T, Gulati S, et al. Migraine and risk of stroke. J Neurol Neurosurg Psychiatry 2020;91: 593-604. doi:10.1136/jnnp-2018-318254 11 Cadena R. Cervical artery dissection: early recognition and stroke prevention. Emerg Med Pract 2016;18(7):1-24. 12 Jones SP, Bray JE, Gibson JM, et al. Characteristics of patients who had a stroke not initially identified during emergency prehospital assessment: a systematic review. Emerg Med J 2021;38(5):387-393. doi:10.1136/emermed-2020209607 15 Puig J, Shankar J, Liebeskind D, et al. From “time is brain” to “imaging is brain”: a paradigm shift in the management of acute ischemic stroke. J Neuroimaging 2020;30(5):562-571. doi:10.1111/ jon.12693 16 Kelly AG, Hellkamp AS, Olson D, et al. Stroke 2012; 43(5):1279-1284. doi:10.1161/STROKEAHA.111.626374 17 Edlow BL, Hurwitz S, Edlow JA. Diagnosis of DWI-negative acute ischemic stroke: a meta-analysis. Neurology 2017;89(3):256-262. doi:10.1212/WNL.0000000000004120 18 Schulz UG, Briley D, Meagher T, et al. Diffusionweighted MRI in 300 patients presenting late with subacute transient ischemic attack or minor stroke. Stroke 2004;35(11):2459-2465. doi:10.1161/ 01.STR.0000143455.55877.b9 19 Amarenco P. Transient ischemic attack. Reply. N Engl J Med 2020;383(16):-15961598. doi:10.1056/ NEJMc2022610 20 Kabra R, Robbie H, Connor SEJ. Diagnostic yield and impact of MRI for acute ischemic stroke in patients presenting with dizziness and vertigo. Clin Radiol 2015;70(7):736-742. doi:10.1016/j. crad.2015.01.016 21 Ay H, Oliveira-Filho J, Buonanno FS, et al. Diffusionweighted imaging identifies a subset of lacunar infarction associated with embolic source. Stroke 1999;30(12):2644-2650. doi:10.1161/01.str.30.12.2644 22 Depuydt S, Sarov M, Vandendries C, et al. Significance of acute multiple infarcts in multiple cerebral circulations on initial diffusion weighted imaging in stroke patients. J Neurol Sci 2014; 337(1-2):151-155. doi:10.1016/j.jns.2013.11.039 23 Mac Grory B, Emmer BJ, Roosendaal SD, et al. Carotid web: an occult mechanism of embolic stroke. J Neurol Neurosurg Psychiatry 2020;91: 1283-1289. doi:10.1136/jnnp-2020-323938 24 Saba L, Moody AR, Saam T, et al. Vessel wall-imaging biomarkers of carotid plaque vulnerability in stroke prevention trials: a viewpoint from the carotid imaging consensus group. JACC Cardiovasc Imaging 2020;13(11): 2445-2456. doi:10.1016/j.jcmg.2020.07.046 CONTINUUMJOURNAL.COM Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited. 423 DIAGNOSTIC EVALUATION OF STROKE ETIOLOGY 25 Bernstein RA, Kamel H, Granger CB, et al. Effect of long-term continuous cardiac monitoring vs usual care on detection of atrial fibrillation in patients with stroke attributed to large- or small-vessel disease: the STROKE-AF randomized clinical trial. JAMA 2021;325(21): 2169-2177. doi:10.1001/jama.2021.6470 26 Tirschwell D, Akoum N. Detection of subclinical atrial fibrillation after stroke: is there enough evidence to treat? JAMA 2021;325(21):2157-2159. doi:10.1001/jama.2021.7429 27 Noseworthy PA, et al. Subclinical and device-detected atrial fibrillation: pondering the knowledge gap: a scientific statement from the American Heart Association. Circulation 2019; 140(25):e944-e963. doi:10.1161/CIR. 0000000000000740 28 Shah S, Malik P, Patel U, et al. Diagnostic yield of TEE in patients with cryptogenic stroke and TIA with normal TTE: a systematic review and meta-analysis. Neurol Int 2021;13(4):659-670. doi:10.3390/neurolint13040063 29 Rodrigues AC, Picard MH, Carbone A, et al. Importance of adequately performed Valsalva maneuver to detect patent foramen ovale during transesophageal echocardiography. J Am Soc Echocardiogr 2013;26(11):1337-1343. doi:10.1016/j. echo.2013.07.016 30 Hart RG, Diener HC, Connolly SJ. Embolic strokes of undetermined source: support for a new clinical construct–authors' reply. Lancet Neurol 2014;13(10):967. doi:10.1016/S1474-4422(14)70197-8 31 Mancuso M, Arnold M, Bersano A, et al. Monogenic cerebral small-vessel diseases: diagnosis and therapy. Consensus recommendations of the European Academy of Neurology. Eur J Neurol 2020;27(6):909-927. doi:10.1111/ene.14183 32 Bersano A, Kraemer M, Burlina A, et al. Heritable and non-heritable uncommon causes of stroke. J Neurol 2021;268(8):2780-2807. doi:10.1007/ s00415-020-09836-x 33 Kato GJ, Piel FB, Reid CD, et al. Sickle cell disease. Nat Rev Dis Primers 2018;4:18010. doi:10.1038/ nrdp.2018.10 34 May JE, Martin KD, Taylor LJ, et al. Current practice and clinical utility of thrombophilia testing in hospitalized patients with acute ischemic stroke. J Stroke Cerebrovasc Dis 2020; 29(11):105209. doi:10.1016/j.jstrokecerebrovasdis. 2020.105209 35 Omran SS, Lerario MP, Gialdini G, et al. Clinical impact of thrombophilia screening in young adults with ischemic stroke. J Stroke Cerebrovasc Dis 2019;28(4):882-889. doi:10.1016/ j.jstrokecerebrovasdis.2018.12.006 36 Green M, Styles T, Russell T, et al. Non-genetic and genetic risk factors for adult cerebral venous thrombosis. Thromb Res 2018;169:15-22. doi:10. 1016/j.thromres.2018.07.005 37 Linnemann B. Antiphospholipid syndrome - an update. Vasa 2018;47(6):451-464. doi:10.1024/ 0301-1526/a000723 38 Levine SR, Brey RL, Tilley BC, et al. Antiphospholipid antibodies and subsequent thrombo-occlusive events in patients with ischemic stroke. JAMA 2004;291(5):576-584. doi:10.1001/jama.291.5.576 39 Carmi O, Berla M, Shoenfeld Y, Levy Y. Diagnosis and management of catastrophic antiphospholipid syndrome. Expert Rev Hematol 2017;10(4):365-374. doi:10.1080/17474086. 2017.1300522 40 Hobohm C, Hagendorff A, Schulz S, et al. Clinical presentation and multi-parametric screening surrogates of ischemic stroke patients suffering from infective endocarditis. Cerebrovasc Dis 2016;41(1-2):60-67. doi:10.1159/000442005 41 Goldsweig AM, Baron SJ. Prosthetic valve endocarditis: literally a growing concern following transcatheter aortic valve replacement. Catheter Cardiovasc Interv 2022; 99(3):904-905. doi:10.1002/ccd.30126 42 Merkler AE, Chu SY, Lerario MP, et al. Temporal relationship between infective endocarditis and stroke. Neurology 2015;85(6):512-516. doi:10.1212/ WNL.0000000000001835 43 Ahn Y, Joo L, Suh CH, et al. Impact of brain MRI on the diagnosis of infective endocarditis and treatment decisions: systematic review and meta-analysis. AJR Am J Roentgenol 2022;218(6): 958-968. doi:10.2214/AJR.21.26896 44 Singhal AB, Topcuoglu MA, Buonanno FS. Acute ischemic stroke patterns in infective and nonbacterial thrombotic endocarditis: a diffusion-weighted magnetic resonance imaging study. Stroke 2002;33(5):1267-1273. doi:10.1161/ 01.str.0000015029.91577.36 45 Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation 2015;132(15):1435-1486. doi:10.1161/CIR. 0000000000000296 46 Carod Artal FJ. Clinical management of infectious cerebral vasculitides. Expert Rev Neurother 2016; 16(2):205-221. doi:10.1586/14737175.2015.1134321 47 Adams HP Jr. Cerebral vasculitis. Handb Clin Neurol 2014;119:475-494. doi:10.1016/B978-07020-4086-3.00031-X 48 Salvarani C, Brown RD Jr, Hunder GG. Adult primary central nervous system vasculitis. Lancet 2012;380(9843):767-777. doi:10.1016/S01406736(12)60069-5 49 Krawczyk M, Barra LJ, Sposato LA, Mandzia JL. Primary CNS vasculitis: a systematic review on clinical characteristics associated with abnormal biopsy and angiography. Autoimmun Rev 2021; 20(1):102714. doi:10.1016/j.autrev.2020.102714 50 Croskerry P. The rational diagnostician and achieving diagnostic excellence. JAMA 2022; 327(4):317-318. doi:10.1001/jama.2021.24988 424 APRIL 2023 Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.