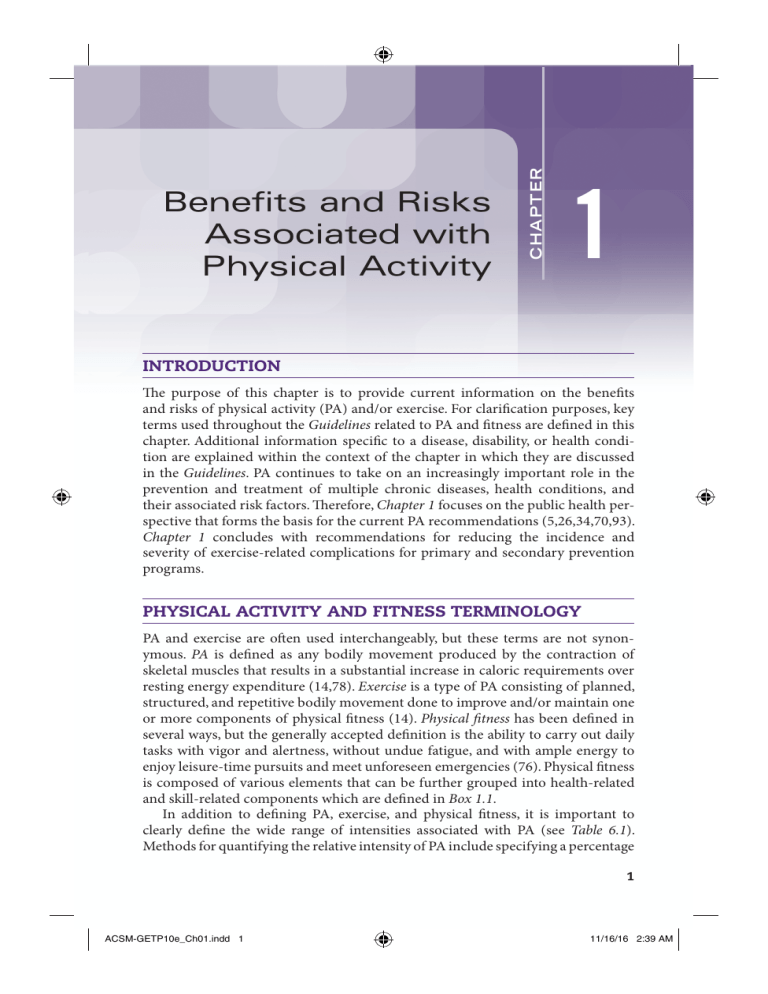
C H AP T E R Benefits and Risks Associated with Physical Activity 1 INTRODUCTION The purpose of this chapter is to provide current information on the benefits and risks of physical activity (PA) and/or exercise. For clarification purposes, key terms used throughout the Guidelines related to PA and fitness are defined in this chapter. Additional information specific to a disease, disability, or health condition are explained within the context of the chapter in which they are discussed in the Guidelines. PA continues to take on an increasingly important role in the prevention and treatment of multiple chronic diseases, health conditions, and their associated risk factors. Therefore, Chapter 1 focuses on the public health perspective that forms the basis for the current PA recommendations (5,26,34,70,93). Chapter 1 concludes with recommendations for reducing the incidence and severity of exercise-related complications for primary and secondary prevention programs. PHYSICAL ACTIVITY AND FITNESS TERMINOLOGY PA and exercise are often used interchangeably, but these terms are not synonymous. PA is defined as any bodily movement produced by the contraction of skeletal muscles that results in a substantial increase in caloric requirements over resting energy expenditure (14,78). Exercise is a type of PA consisting of planned, structured, and repetitive bodily movement done to improve and/or maintain one or more components of physical fitness (14). Physical fitness has been defined in several ways, but the generally accepted definition is the ability to carry out daily tasks with vigor and alertness, without undue fatigue, and with ample energy to enjoy leisure-time pursuits and meet unforeseen emergencies (76). Physical fitness is composed of various elements that can be further grouped into health-related and skill-related components which are defined in Box 1.1. In addition to defining PA, exercise, and physical fitness, it is important to clearly define the wide range of intensities associated with PA (see Table 6.1). Methods for quantifying the relative intensity of PA include specifying a percentage 1 ACSM-GETP10e_Ch01.indd 1 11/16/16 2:39 AM Guidelines for Exercise Testing • www.acsm.org 2 Box 1.1 Health-Related and Skill-Related Components of Physical Fitness Health-Related Physical Fitness Components ■ ■ ■ ■ ■ Cardiorespiratory endurance: the ability of the circulatory and respiratory system to supply oxygen during sustained physical activity Body composition: the relative amounts of muscle, fat, bone, and other vital parts of the body Muscular strength: the ability of muscle to exert force Muscular endurance: the ability of muscle to continue to perform without fatigue Flexibility: the range of motion available at a joint Skill-Related Physical Fitness Components ■ ■ ■ ■ ■ ■ Agility: the ability to change the position of the body in space with speed and accuracy Coordination: the ability to use the senses, such as sight and hearing, together with body parts in performing tasks smoothly and accurately Balance: the maintenance of equilibrium while stationary or moving Power: the ability or rate at which one can perform work Reaction time: the time elapsed between stimulation and the beginning of the reaction to it Speed: the ability to perform a movement within a short period of time Adapted from (96). Available from http://www.fitness.gov/digest_mar2000.htm · of oxygen uptake reserve (VO2R), heart rate reserve (HRR), oxygen consumption · (VO2), heart rate (HR), or metabolic equivalents (METs) (see Box 6.2). Each of these methods for describing the intensity of PA has strengths and limitations. Although determining the most appropriate method is left to the exercise professional, Chapter 6 provides the methodology and guidelines for selecting a suitable method. METs are a useful, convenient, and standardized way to describe the absolute intensity of a variety of physical activities. Light intensity PA is defined as requiring 2.0–2.9 METs, moderate as 3.0–5.9 METs, and vigorous as ⱖ6.0 METs (26). Table 1.1 gives specific examples of activities in METs for each of the intensity ranges. A complete list of physical activities and their associated estimates of energy expenditure can be found elsewhere (2). Maximal aerobic capacity usually declines with age (26). For this reason, when older and younger individuals work at the same MET level, the relative exercise in· tensity (e.g., %VO2max) will usually be different (see Chapter 6). In other words, the older individual will be working at a greater relative percentage of maximal oxygen · consumption (VO2max) than their younger counterparts. Nonetheless, physically active older adults may have aerobic capacities comparable to or greater than those of physically inactive younger adults. ACSM-GETP10e_Ch01.indd 2 11/3/16 1:38 AM Chapter 1 Benefits and Risks Associated with Physical Activity TABLE 3 1.1 Metabolic Equivalents (METs) Values of Common Physical Activities Classified as Light, Moderate, or Vigorous Intensity Very Light/Light (⬍3.0 METs) Moderate (3.0–5.9 METs) Walking Walking slowly around home, store, or office ⫽ 2.0a Walking Walking 3.0 mi ⴢ h⫺1 ⫽ 3.0a Walking at very brisk pace (4 mi ⴢ h⫺1) ⫽ 5.0a Household and occupation Standing performing light work, such as making bed, washing dishes, ironing, preparing food, or store clerk ⫽ 2.0–2.5 Leisure time and sports Arts and crafts, playing cards ⫽ 1.5 Billiards ⫽ 2.5 Boating — power ⫽ 2.5 Croquet ⫽ 2.5 Darts ⫽ 2.5 Fishing — sitting ⫽ 2.5 Playing most musical instruments ⫽ 2.0–2.5 Household and occupation Cleaning, heavy — washing windows, car, clean garage ⫽ 3.0 Sweeping floors or carpet, vacuuming, mopping ⫽ 3.0–3.5 Carpentry — general ⫽ 3.6 Carrying and stacking wood ⫽ 5.5 Mowing lawn — walk power mower ⫽ 5.5 Leisure time and sports Badminton — recreational ⫽ 4.5 Basketball — shooting around ⫽ 4.5 Dancing — ballroom slow ⫽ 3.0; ballroom fast ⫽ 4.5 Fishing from riverbank and walking ⫽ 4.0 Golf — walking, pulling clubs ⫽ 4.3 Sailing boat, wind surfing ⫽ 3.0 Table tennis ⫽ 4.0 Tennis doubles ⫽ 5.0 Volleyball — noncompetitive ⫽ 3.0–4.0 Vigorous (ⱖ6.0 METs) Walking, jogging, and running Walking at very, very brisk pace (4.5 mi ⴢ h⫺1) ⫽ 6.3a Walking/hiking at moderate pace and grade with no or light pack (⬍10 lb) ⫽ 7.0 Hiking at steep grades and pack 10–42 lb ⫽ 7.5–9.0 Jogging at 5 mi ⴢ h⫺1 ⫽ 8.0a Jogging at 6 mi ⴢ h⫺1 ⫽ 10.0a Running at 7 mi ⴢ h⫺1 ⫽ 11.5a Household and occupation Shoveling sand, coal, etc. ⫽ 7.0 Carrying heavy loads, such as bricks ⫽ 7.5 Heavy farming, such as bailing hay ⫽ 8.0 Shoveling, digging ditches ⫽ 8.5 Leisure time and sports Bicycling on flat — light effort (10–12 mi ⴢ h⫺1) ⫽ 6.0 Basketball game ⫽ 8.0 Bicycling on flat — moderate effort (12–14 mi ⴢ h⫺1) ⫽ 8.0; fast (14–16 mi ⴢ h⫺1) ⫽ 10.0 Skiing cross-country — slow (2.5 mi ⴢ h⫺1) ⫽ 7.0; fast (5.0–7.9 mi ⴢ h⫺1) ⫽ 9.0 Soccer — casual ⫽ 7.0; competitive ⫽ 10.0 Swimming leisurely ⫽ 6.0b; swimming — moderate/ hard ⫽ 8.0–11.0b Tennis singles ⫽ 8.0 Volleyball — competitive at gym or beach ⫽ 8.0 a On flat, hard surface. MET values can vary substantially from individual to individual during swimming as a result of different strokes and skill levels. b Adapted from (2). ACSM-GETP10e_Ch01.indd 3 11/3/16 1:38 AM Guidelines for Exercise Testing • www.acsm.org 4 PUBLIC HEALTH PERSPECTIVE FOR CURRENT RECOMMENDATIONS Over 20 yr ago, the American College of Sports Medicine (ACSM) in conjunction with the Centers for Disease Control and Prevention (CDC) (73), the U.S. Surgeon General (93), and the National Institutes of Health (75) issued landmark publications on PA and health. An important goal of these reports was to clarify for exercise professionals and the public the amount and intensity of PA needed to improve health, lower susceptibility to disease (morbidity), and decrease premature mortality (73,75,93). In addition, these reports documented the dose-response relationship between PA and health (i.e., some activity is better than none, and more activity, up to a point, is better than less). In 1995, the CDC and ACSM recommended that “every U.S. adult should accumulate 30 min or more of moderate PA on most, preferably all, days of the week” (73). The intent of this statement was to increase public awareness of the importance of the health-related benefits of moderate intensity PA. As a result of an increasing awareness of the adverse health effects of physical inactivity and because of some confusion and misinterpretation of the original PA recommendations, the ACSM and American Heart Association (AHA) issued updated recommendations for PA and health in 2007 (Box 1.2) (34). More recently, the federal government convened an expert panel, the 2008 Physical Activity Guidelines Advisory Committee, to review the scientific evidence on PA and health published since the 1996 U.S. Surgeon General’s Report (76). This committee found compelling evidence regarding the benefits of PA for health as well as the presence of a dose-response relationship for many diseases and health conditions. Two important conclusions from the Physical Activity Box 1.2 ■ ■ ■ ■ ■ The ACSM-AHA Primary Physical Activity (PA) Recommendations (33) All healthy adults aged 18–65 yr should participate in moderate intensity aerobic PA for a minimum of 30 min on 5 d ⴢ wk⫺1 or vigorous intensity aerobic activity for a minimum of 20 min on 3 d ⴢ wk⫺1. Combinations of moderate and vigorous intensity exercise can be performed to meet this recommendation. Moderate intensity aerobic activity can be accumulated to total the 30 min minimum by performing bouts each lasting ⱖ10 min. Every adult should perform activities that maintain or increase muscular strength and endurance for a minimum of 2 d ⴢ wk⫺1. Because of the dose-response relationship between PA and health, individuals who wish to further improve their fitness, reduce their risk for chronic diseases and disabilities, and/or prevent unhealthy weight gain may benefit by exceeding the minimum recommended amounts of PA. ACSM, American College of Sports Medicine; AHA, American Heart Association. ACSM-GETP10e_Ch01.indd 4 11/3/16 1:38 AM Chapter 1 Benefits and Risks Associated with Physical Activity 5 Guidelines Advisory Committee Report that influenced the development of the PA recommendations are the following: ■ ■ Important health benefits can be obtained by performing a moderate amount of PA on most, if not all, days of the week. Additional health benefits result from greater amounts of PA. Individuals who maintain a regular program of PA that is longer in duration, of greater intensity, or both are likely to derive greater benefit than those who engage in lesser amounts. Similar recommendations have been made in the 2008 federal PA guidelines (http://www.health.gov/PAguidelines) (93) based on the 2008 Physical Activity Guidelines Advisory Committee Report (76) (Box 1.3). Since the release of the U.S. Surgeon General’s Report in 1996 (93), several reports have advocated PA levels above the minimum CDC-ACSM PA recommendations (22,26,80,92). These guidelines and recommendations primarily refer to the volume of PA required to prevent weight gain and/or obesity and should not be viewed as contradictory. In other words, PA that is sufficient to reduce the risk of developing chronic diseases and delaying mortality may be insufficient to prevent or reverse weight gain and/or obesity given the typical American lifestyle. PA beyond the minimum recommendations combined with proper nutrition is likely needed in many individuals to manage and/or prevent weight gain and obesity (22,42). Several large-scale epidemiology studies have been performed that document the dose-response relationship between PA and cardiovascular disease (CVD) and premature mortality (52,57,72,79,88,107). Williams (104) performed a meta-analysis of 23 sex-specific cohorts reporting varying levels of PA or cardiorespiratory fitness (CRF) representing 1,325,004 individual-years of follow-up and showed a dose-response relationship between PA or CRF and the risks of coronary artery disease (CAD) and CVD (Figure 1.1). It is clear that greater amounts of PA or increased CRF levels provide additional health benefits. Table 1.2 provides the Box 1.3 ■ ■ ■ The Primary Physical Activity Recommendations from the 2008 Physical Activity Guidelines Advisory Committee Report (93) All Americans should participate in an amount of energy expenditure equivalent to 150 min ⴢ wk⫺1 of moderate intensity aerobic activity, 75 min ⴢ wk⫺1 of vigorous intensity aerobic activity, or a combination of both that generates energy equivalency to either regimen for substantial health benefits. These guidelines further specify a dose-response relationship, indicating additional health benefits are obtained with 300 min ⴢ wk⫺1 or more of moderate intensity aerobic activity, 150 min ⴢ wk⫺1 or more of vigorous intensity aerobic activity, or an equivalent combination of moderate and vigorous intensity aerobic activity. Adults should do muscle strengthening activities that are moderate or high intensity and involve all major muscle groups in ⱖ2 d ⴢ wk⫺1 because these activities provide additional health benefits. ACSM-GETP10e_Ch01.indd 5 11/3/16 1:38 AM Guidelines for Exercise Testing • www.acsm.org 6 Relative risk 1 0.8 Physical activity 0.6 0.4 Physical fitness 0.2 0 25 50 75 100 Percentage Figure 1.1 Estimated dose-response curve for the relative risk of atherosclerotic cardiovascular disease by sample percentages of fitness and physical activity. Studies weighted by individual-years of experience. Used with permission from (104). strength of evidence for the dose-response relationships among PA and numerous health outcomes. The ACSM and AHA have also released two publications examining the relationship between PA and public health in older adults (5,70). In general, these publications offered some recommendations that are similar to the updated guidelines for adults (26,34), but the recommended intensity of aerobic activity reflected in these guidelines is related to the older adult’s CRF level. In addition, age-specific recommendations are made concerning the importance of flexibility, neuromotor, and muscle strengthening activities. The 2008 Physical Activity Guidelines for Americans made age-specific recommendations targeted at adults (18–64 yr) and older adults (ⱖ65 yr) as well as children and adolescents (6–17 yr) (http://www.health.gov/ PAguidelines) (93) that are similar to recommendations by the ACSM and AHA. Despite the well-known health benefits, physical inactivity is a global pandemic that has been identified as one of the four leading contributors to premature mortality (30,50). Globally, 31.1% of adults are physically inactive (30). In the United States, 51.6% of adults meet aerobic activity guidelines, 29.3% meet muscle strengthening guidelines, and 20.6% meet both the aerobic and muscle strengthening guidelines (15). SEDENTARY BEHAVIOR AND HEALTH Prolonged periods of sitting or sedentary behavior are associated with deleterious health consequences (see Chapter 6) (35,36,44,47) independent of PA levels (8,51, 63,82). This is concerning from a public health perspective because population-based studies have demonstrated that more than 50% of an average person’s waking day involves activities associated with prolonged sitting such as television viewing and computer use (62). A recent meta-analysis demonstrated that after statistical adjustment ACSM-GETP10e_Ch01.indd 6 11/3/16 1:38 AM Chapter 1 Benefits and Risks Associated with Physical Activity TABLE 7 1.2 Evidence for Dose-Response Relationship between Physical Activity and Health Outcome Variable All-cause mortality Cardiorespiratory health Metabolic health Energy balance: Weight maintenance Weight loss Weight maintenance following weight loss Abdominal obesity Musculoskeletal health: Bone Joint Muscular Functional health Colon and breast cancers Mental health: Depression and distress Well-being: Anxiety, cognitive health, and sleep Evidence for a DoseResponse Relationship Strength of Evidencea Yes Yes Yes Strong Strong Moderate Insufficient data Yes Yes Weak Strong Moderate Yes Moderate Yes Yes Yes Yes Yes Moderate Strong Strong Moderate Moderate Yes Moderate Insufficient data Weak a Strength of the evidence was classified as follows: “Strong” — Strong, consistent across studies and populations “Moderate” — Moderate or reasonable, reasonably consistent “Weak” — Weak or limited, inconsistent across studies and populations Adapted from (76). for PA, sedentary time was independently associated with a greater risk for all-cause mortality, CVD incidence or mortality, cancer incidence or mortality (breast, colon, colorectal, endometrial, and epithelial ovarian), and Type 2 diabetes mellitus (T2DM) in adults (8). However, sedentary time was associated with a 30% lower relative risk for all-cause mortality among those with high levels of PA as compared with those with low levels of PA, suggesting that the adverse outcomes associated with sedentary time decrease in magnitude among persons who are more physically active (8). HEALTH BENEFITS OF REGULAR PHYSICAL ACTIVITY AND EXERCISE Evidence to support the inverse relationship between regular PA and/or exercise and premature mortality, CVD/CAD, hypertension, stroke, osteoporosis, T2DM, ACSM-GETP10e_Ch01.indd 7 10/5/17 4:47 AM 8 Guidelines for Exercise Testing • www.acsm.org metabolic syndrome (Metsyn), obesity, 13 cancers (breast, bladder, rectal, head and neck, colon, myeloma, myeloid leukemia, endometrial, gastric cardia, kidney, lung, liver, esophageal adenocarcinoma), depression, functional health, falls, and cognitive function continues to accumulate (26,67,76). For many of these diseases and health conditions, there is also strong evidence of a dose-response relationship with PA (see Table 1.2). This evidence has resulted from clinical intervention studies as well as large-scale, population-based, observational studies (26,34,37,45,54,69,94,100,103). Several large-scale epidemiology studies have clearly documented a doseresponse relationship between PA and risk of CVD and premature mortality in men and women and in ethnically diverse participants (52,57,69,71,76,88,107). It is also important to note that aerobic capacity (i.e., CRF) has an inverse relationship with risk of premature death from all causes and specifically from CVD, and higher levels of CRF are associated with higher levels of habitual PA, which in turn are associated with many health benefits (10,11,26,49,84,99,103). Box 1.4 summarizes the benefits of regular PA and/or exercise. HEALTH BENEFITS OF IMPROVING MUSCULAR FITNESS The health benefits of enhancing muscular fitness (i.e., the functional parameters of muscle strength, endurance, and power) are well established (26,93,102). Higher levels of muscular strength are associated with a significantly better cardiometabolic risk factor profile, lower risk of all-cause mortality, fewer CVD events, lower risk of developing physical function limitations, and lower risk for nonfatal disease (26). There is an impressive array of changes in health-related biomarkers that can be derived from regular participation in resistance training including improvements in body composition, blood glucose levels, insulin sensitivity, and blood pressure in individuals with mild or moderate hypertension (17,26,74). Recent evidence suggests that resistance training is as effective as aerobic training in the management and treatment of T2DM (106) and in improving the blood lipid profiles of individuals who are overweight/obese (83). Resistance training positively affects walking distance and velocity in those with peripheral artery disease (PAD) (6,106). Further health benefits attributed to resistance training were confirmed by a recent meta-analysis of published reports which revealed that regimens featuring mild-to-moderate intensity isometric muscle actions were more effective in reducing blood pressure in both normotensive and hypertensive people than aerobic training or dynamic resistance training (13). Accordingly, resistance training may be effective for preventing and treating the dangerous constellation of conditions referred to as Metsyn (26) (see Chapter 10). Exercise that enhances muscle strength and mass also increases bone mass (i.e., bone mineral density and content) and bone strength of the specific bones stressed and may serve as a valuable measure to prevent, slow, or reverse the loss of bone mass in individuals with osteoporosis (5,26,93) (see Chapter 11). Resistance training can reduce pain and disability in individuals with osteoarthritis (26,65) and has been shown to be effective in the treatment of chronic back pain (57,97). ACSM-GETP10e_Ch01.indd 8 11/3/16 1:38 AM Chapter 1 Benefits and Risks Associated with Physical Activity Box 1.4 9 Benefits of Regular Physical Activity and/or Exercise Improvement in Cardiovascular and Respiratory Function ■ ■ ■ ■ ■ ■ ■ Increased maximal oxygen uptake resulting from both central and peripheral adaptations Decreased minute ventilation at a given absolute submaximal intensity Decreased myocardial oxygen cost for a given absolute submaximal intensity Decreased heart rate and blood pressure at a given submaximal intensity Increased capillary density in skeletal muscle Increased exercise threshold for the accumulation of lactate in the blood Increased exercise threshold for the onset of disease signs or symptoms (e.g., angina pectoris, ischemic ST-segment depression, claudication) Reduction in Cardiovascular Disease Risk Factors ■ ■ ■ ■ ■ ■ Reduced resting systolic/diastolic pressure Increased serum high-density lipoprotein cholesterol and decreased serum triglycerides Reduced total body fat, reduced intra-abdominal fat Reduced insulin needs, improved glucose tolerance Reduced blood platelet adhesiveness and aggregation Reduced inflammation Decreased Morbidity and Mortality ■ ■ Primary prevention (i.e., interventions to prevent the initial occurrence) ■ Higher activity and/or fitness levels are associated with lower death rates from CAD ■ Higher activity and/or fitness levels are associated with lower incidence rates for CVD, CAD, stroke, Type 2 diabetes mellitus, metabolic syndrome, osteoporotic fractures, cancer of the colon and breast, and gallbladder disease Secondary prevention (i.e., interventions after a cardiac event to prevent another) ■ Based on meta-analyses (i.e., pooled data across studies), cardiovascular and all-cause mortality are reduced in patients with post-myocardial infarction (MI) who participate in cardiac rehabilitation exercise training, especially as a component of multifactorial risk factor reduction (Note: randomized controlled trials of cardiac rehabilitation exercise training involving patients with post-MI do not support a reduction in the rate of nonfatal reinfarction). Other Benefits ■ ■ ■ ■ ■ ■ ■ ■ Decreased anxiety and depression Improved cognitive function Enhanced physical function and independent living in older individuals Enhanced feelings of well-being Enhanced performance of work, recreational, and sport activities Reduced risk of falls and injuries from falls in older individuals Prevention or mitigation of functional limitations in older adults Effective therapy for many chronic diseases in older adults CAD, coronary artery disease; CVD, cardiovascular disease. Adapted from (45,70,94). ACSM-GETP10e_Ch01.indd 9 11/3/16 1:38 AM 10 Guidelines for Exercise Testing • www.acsm.org Preliminary work suggests that resistance exercise may prevent and improve depression and anxiety, increase vigor, and reduce fatigue (26,86). RISKS ASSOCIATED WITH PHYSICAL ACTIVITY AND EXERCISE Although the benefits of regular PA are well established, participation in exercise is associated with an increased risk for musculoskeletal injury (MSI) and cardiovascular complications (26). MSI is the most common exercise-related complication and is often associated with exercise intensity, the nature of the activity, preexisting conditions, and musculoskeletal anomalies. Adverse cardiovascular events such as sudden cardiac death (SCD) and acute myocardial infarction (AMI) are usually associated with vigorous intensity exercise (3,66,93). SCD and AMI are much less common than MSI but may lead to long-term morbidity and mortality (4). Exercise-Related Musculoskeletal Injury Participation in exercise and PA increases the risk of MSI (68,76). The intensity and type of exercise may be the most important factors related to the incidence of injury (26). Walking and moderate intensity physical activities are associated with a very low risk of MSI, whereas jogging, running, and competitive sports are associated with an increased risk of injury (26,39,40). The risk of MSI is higher in activities where there is direct contact between participants or with the ground (e.g., football, wrestling) versus activities where the contact between participants or with the ground is minimal or nonexistent (i.e., baseball, running, walking) (38,76). In 2012, over 6 million Americans received medical attention for sport-related injuries, with the highest rates found in children between the ages of 12 and 17 yr (91.34 injury episodes per 1,000 population) and children younger than the age of 12 yr (20.03 injury episodes per 1,000 population) (1). The most common anatomical sites for MSI are the lower extremities with higher rates in the knees followed by the foot and ankle (39,40). The literature on injury consequences of PA participation often focuses on men from nonrepresentative populations (e.g., military personnel, athletes) (43). A prospective study of community-dwelling women found that meeting the national guidelines of ⱖ150 min ⴢ wk⫺1 of moderate-to-vigorous intensity PA resulted in a modest increase in PA-related MSI compared to women not meeting the PA guidelines (68). However, the risk for developing MSI is inversely related to physical fitness level (76). For any given dose of PA, individuals who are physically inactive are more likely to experience MSI when compared to their more active counterparts (76). Commonly used methods to reduce MSI (e.g., stretching, warm-up, cool-down, and gradual progression of exercise intensity and volume) may be helpful in some situations; however, there is a lack of controlled studies confirming the effectiveness of these methods (26). A comprehensive list of strategies that may prevent MSI can be found elsewhere (12,28). ACSM-GETP10e_Ch01.indd 10 11/3/16 1:38 AM Chapter 1 Benefits and Risks Associated with Physical Activity 11 SUDDEN CARDIAC DEATH AMONG YOUNG INDIVIDUALS The cardiovascular causes of exercise-related sudden death in young athletes are shown in Table 1.3 (4). It is clear from these data that the most common causes of SCD in young individuals are congenital and hereditary abnormalities including TABLE 1.3 Cardiovascular Causes of Exercise-Related Sudden Death in Young Athletesa Van Camp et al. (n ⫽ 100)b (95) Hypertrophic CM Probable hypertrophic CM Coronary anomalies Valvular and subvalvular aortic stenosis Possible myocarditis Dilated and nonspecific CM Atherosclerotic CVD Aortic dissection/rupture Arrhythmogenic right ventricular CM Myocardial scarring Mitral valve prolapse Other congenital abnormalities Long QT syndrome Wolff-Parkinson-White syndrome Cardiac conduction disease Cardiac sarcoidosis Coronary artery aneurysm Normal heart at necropsy Pulmonary thromboembolism Maron et al. (n ⫽ 134) (60) Corrado et al. (n ⫽ 55)c (18) 51 5 18 8 36 10 23 4 1 0 9 0 7 7 3 3 5 1 3 2 1 2 5 3 10 1 11 0 1 0 3 2 1.5 0 6 0 0 1 0.5 0 0 1 0 0 3 0 1 7 0 0.5 0 2 0 0 0 1 1 a Ages ranged from 13 to 24 yr (95), 12 to 40 yr (60), and 12 to 35 yr (18). References (95) and (60) used the same database and include many of the same athletes. All (95), 90% (60), and 89% (18) had symptom onset during or within an hour of training or competition. b Total exceeds 100% because several athletes had multiple abnormalities. c Includes some athletes whose deaths were not associated with recent exertion. Includes aberrant artery origin and course, tunneled arteries, and other abnormalities. CM, cardiomyopathy; CVD, cardiovascular disease. Used with permission from (4). ACSM-GETP10e_Ch01.indd 11 11/3/16 1:38 AM 12 Guidelines for Exercise Testing • www.acsm.org hypertrophic cardiomyopathy, coronary artery abnormalities, and aortic stenosis. The absolute annual risk of exercise-related death among high school and college athletes is 1 per 133,000 men and 769,000 women (95). It should be noted that these rates, although low, include all sports-related nontraumatic deaths. Of the 136 total identifiable causes of death, 100 were caused by CVD. A more recent estimate places the annual incidence of cardiovascular deaths among young competitive athletes in the United States as 1 death per 185,000 men and 1.5 million women. (58). Some experts, however, believe the incidence of exercise-related sudden death in young sports participants is higher, ranging between 1 per 40,000 and 1 per 80,000 athletes per year (32). Furthermore, death rates seem to be higher in African American male athletes and basketball players (32,59). Experts debate on why estimates of the incidence of exercise-related sudden deaths vary among studies. These variances are likely due to differences in (a) the populations studied, (b) estimation of the number of sport participants, and (c) subject and/or incident case assignment. In an effort to reduce the risk of SCD incidence in young individuals, well-recognized organizations such as the International Olympic Committee and AHA have endorsed the practice of preparticipation cardiovascular screening (19,53,61). The recent position stand by the American Medical Society for Sports Medicine presents the latest evidence based research on cardiovascular preparticipation screening in athletes (23). EXERCISE-RELATED CARDIAC EVENTS IN ADULTS In general, exercise does not provoke cardiovascular events in healthy individuals with normal cardiovascular systems. The risk of SCD and AMI is very low in apparently healthy individuals performing moderate intensity PA (76,101). There is an acute and transient increase in the risk of SCD and AMI in individuals performing vigorous intensity exercise, particularly in sedentary men and women with diagnosed or occult CVD (3,4,29,66,85,90,105). However, this risk decreases with increasing volumes of regular exercise (89). Chapter 2 includes an exercise preparticipation health screening algorithm to help identify individuals who may be at risk for exercise-related cardiovascular events. It is well established that the transient risks of SCD and AMI are substantially higher during acute vigorous physical exertion as compared with rest (29,66,85,91,105). A recent meta-analysis reported a fivefold increased risk of SCD and 3.5-fold increased risk of AMI during or shortly after vigorous intensity PA (20). The risk of SCD or AMI is higher in middle-aged and older adults than in younger individuals due to the higher prevalence of CVD in the older population. The rates of SCD and AMI are disproportionately higher in the most sedentary individuals when they perform unaccustomed or infrequent exercise (4). For example, the Onset Study (65) showed that the risk of AMI during or immediately following vigorous intensity exercise was 50 times higher for the habitually sedentary compared to individuals who exercised vigorously for 1-h sessions ⱖ5 d ⴢ wk⫺1 (Figure 1.2). Although the relative risks of SCD and AMI are higher during sudden vigorous physical exertion versus rest, the absolute risk of these events is very low. ACSM-GETP10e_Ch01.indd 12 11/3/16 1:38 AM Chapter 1 Benefits and Risks Associated with Physical Activity 13 200 Active subject * 100 Sedentary subject Relative risk of AMI 50 *Vigorous exercise bout 30 * 10 8 * 4 * 2 1 0.5 0 Baseline risk 0 1-2 (Days/Week) 3-4 5+ Habitual frequency of vigorous physical activity Figure 1.2 The relationship between habitual frequency of vigorous physical activity and the relative risk of acute myocardial infarction (AMI). Used with permission from (24). Prospective evidence from the Physicians’ Health Study and Nurses’ Health Study suggests that SCD occurs every 1.5 million episodes of vigorous physical exertion in men (3) and every 36.5 million h of moderate-to-vigorous exertion in women (101). Retrospective analyses also support the rarity of these events. Thompson et al. (90) reported 1 death per 396,000 h of jogging. An analysis of exercise-related cardiovascular events among participants at YMCA sports centers found 1 death per 2,897,057 person-hours, although exercise intensity was not documented (55). Kim et al. (46) studied over 10 million marathon and half-marathon runners and identified an overall cardiac arrest incidence rate of 1 per 184,000 runners and an SCD incidence rate of 1 per 256,000 runners, which translates to 0.20 cardiac arrests and 0.14 SCDs per 100,000 estimated runner-hours. Although the risk is extremely low, vigorous intensity exercise has a small but measurable acute risk of CVD complications; therefore, mitigating this risk in susceptible individuals is important (see Chapter 2). The exact mechanism of SCD during vigorous intensity exercise with asymptomatic adults is not completely understood. However, evidence exists that the increased frequency of cardiac contraction and excursion of the coronary arteries produces bending and flexing of the coronary arteries may be the underlying cause. This response may cause cracking of the atherosclerotic plaque with resulting platelet aggregation and possible acute thrombosis and has been documented angiographically in individuals with exercise-induced cardiac events (9,16,31). ACSM-GETP10e_Ch01.indd 13 11/3/16 1:38 AM 14 Guidelines for Exercise Testing • www.acsm.org EXERCISE TESTING AND THE RISK OF CARDIAC EVENTS As with vigorous intensity exercise, the risk of cardiac events during exercise testing varies directly with the prevalence of diagnosed or occult CVD in the study population. Several studies have documented these risks during exercise testing (7,27,41,48,64,78,87). Table 1.4 summarizes the risks of various cardiac events including AMI, ventricular fibrillation, hospitalization, and death. These data indicate in a mixed population the risk of exercise testing is low with approximately six cardiac events per 10,000 tests. One of these studies includes data for which the exercise testing was supervised by nonphysicians (48). In addition, the majority of these studies used symptom-limited maximal exercise tests. Therefore, it would be expected that the risk of submaximal testing in a similar population would be lower. TABLE 1.4 Cardiac Complications during Exercise Testinga Reference Year Site Rochmis and 1971 73 U.S. Blackburn centers (78) No. of Tests MI VF Death Hospitalization Comment 170,000 NA NA 1 3 NA 4.67 0 NR 34% of tests were symptom limited; 50% of deaths in 8 h; 50% over the next 4 d Irving et al. (41) 1977 15 Seattle facilities 10,700 McHenry (64) 1977 Hospital 12,000 0 0 0 0 Atterhög et al. (7) 1979 20 Swedish centers 50,000 0.8 0.8 0.4 5.2 Stuart and Ellestad (87) 1980 1,375 U.S. centers 0.5 NR VF includes other dysrhythmias requiring treatment. Gibbons et al. (27) 1989 Cooper Clinic 71,914 0.56 0.29 0 NR Only 4% of men and 2% of women had CVD. Knight et al. (48) 1995 Geisinger Cardiology Service 28,133 1.42 1.77 NR 25% were inpatient tests supervised by non-MDs. 518,448 3.58 4.78 0 a Events are per 10,000 tests. CVD, cardiovascular disease; MD, medical doctor; MI, myocardial infarction; NA, not applicable; NR, not reported; VF, ventricular fibrillation. ACSM-GETP10e_Ch01.indd 14 10/5/17 4:47 AM Chapter 1 Benefits and Risks Associated with Physical Activity TABLE 15 1.5 Summary of Contemporary Exercise-Based Cardiac Rehabilitation Program Complication Rates Patient Exercise Cardiac Hours Arrest Myocardial Fatal Infarction Events Investigator Year Van Camp and Peterson (96) 1980–1984 2,351,916 1/111,996b 1/293,990 Digenio et al. (21) 1982–1988 480,000 1/120,000c Vongvanich et al. (98) 268,503 1/89,501d 1986–1995 Franklin et al. (25) 1982–1998 292,254 1/146,127 Average 1/116,906 1/783,972 1/81,101 1/160,000 1/120,000 1/268,503d d Major Complicationsa 0/268,503 1/67,126 d 1/97,418 0/292,254 1/58,451 1/219,970 1/752,365 1/81,670 a Myocardial infarction and cardiac arrest. Fatal 14%. Fatal 75%. d Fatal 0%. b c Used with permission from (4). RISKS OF CARDIAC EVENTS DURING CARDIAC REHABILITATION The highest risk of cardiovascular events occurs in those individuals with diagnosed CAD. In one survey, there was one nonfatal complication per 34,673 h and one fatal cardiovascular complication per 116,402 h of cardiac rehabilitation (33). Other studies have found a lower rate: one cardiac arrest per 116,906 patient-hours, one AMI per 219,970 patient-hours, one fatality per 752,365 patient-hours, and one major complication per 81,670 patient-hours (21,25,96,98). These studies are presented in Table 1.5 (4). A more recent study demonstrated an even lower rate of cardiovascular complications during cardiac rehabilitation with one cardiac arrest per 169,344 patient-hours, no AMI per 338,638 patient-hours, and one fatality per 338,638 patient-hours (81). Although these complication rates are low, it should be noted that patients were screened and exercised in medically supervised settings equipped to handle cardiac emergencies. The mortality rate appears to be six times higher when patients exercised in facilities without the ability to successfully manage cardiac arrest (4,21,25,96,98). Interestingly, however, a review of home-based cardiac rehabilitation programs found no increase in cardiovascular complications versus formal center-based exercise programs (100). PREVENTION OF EXERCISE-RELATED CARDIAC EVENTS Because of the low incidence of cardiac events related to vigorous intensity exercise, it is very difficult to test the effectiveness of strategies to reduce the occurrence of ACSM-GETP10e_Ch01.indd 15 11/3/16 1:38 AM 16 Guidelines for Exercise Testing • www.acsm.org these events. According to a recent statement by the ACSM and AHA (4), “Physicians should not overestimate the risks of exercise because the benefits of habitual physical activity substantially outweigh the risks.” This report also recommends several strategies to reduce these cardiac events during vigorous intensity exercise (4): ■ ■ ■ ■ ■ ■ Health care professionals should know the pathologic conditions associated with exercise-related events so that physically active children and adults can be appropriately evaluated. Physically active individuals should know the nature of cardiac prodromal symptoms (e.g., excessive, unusual fatigue and pain in the chest and/or upper back) and seek prompt medical care if such symptoms develop (see Table 2.1). High school and college athletes should undergo preparticipation screening by qualified professionals. Athletes with known cardiac conditions or a family history should be evaluated prior to competition using established guidelines. Health care facilities should ensure their staff is trained in managing cardiac emergencies and have a specified plan and appropriate resuscitation equipment (see Appendix B). Physically active individuals should modify their exercise program in response to variations in their exercise capacity, habitual activity level, and the environment (see Chapters 6 and 8). Although strategies for reducing the number of cardiovascular events during vigorous intensity exercise have not been systematically studied, it is incumbent on the exercise professional to take reasonable precautions when working with individuals who wish to become more physically active/fit and/or increase their PA/fitness levels. These precautions are particularly true when the exercise program will be of vigorous intensity. Although many sedentary individuals can safely begin a light-to-moderate intensity exercise program, all individuals should participate in the exercise preparticipation screening process to determine the need for medical clearance (see Chapter 2). Exercise professionals who supervise exercise and fitness programs should have current training in basic and/or advanced cardiac life support and emergency procedures. These emergency procedures should be reviewed and practiced at regular intervals (see Appendix B). Finally, individuals should be educated on the signs and symptoms of CVD and should be referred to a physician for further evaluation should these symptoms occur. ONLINE RESOURCES American College of Sports Medicine Position Stand on the Quantity and Quality of Exercise: http://www.acsm.org 2008 Physical Activity Guidelines for Americans: http://www.health.gov/PAguidelines ACSM-GETP10e_Ch01.indd 16 11/3/16 1:38 AM Chapter 1 Benefits and Risks Associated with Physical Activity 17 REFERENCES 1. Adams PF, Kirzinger WK, Martinez M. Summary health statistics for the U.S. population: National Health Interview Survey, 2012. Vital Health Stat. 2013;10(259):1–95. 2. Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(Suppl 9):S498–504. 3. Albert CM, Mittleman MA, Chae CU, Lee IM, Hennekens CH, Manson JE. Triggering of sudden death from cardiac causes by vigorous exertion. N Engl J Med. 2000;343(19):1355–61. 4. American College of Sports Medicine, American Heart Association. Exercise and acute cardiovascular events: placing the risks into perspective. Med Sci Sports Exerc. 2007;39(5):886–97. 5. American College of Sports Medicine, Chodzko-Zajko WJ, Proctor DN, et al. American College of Sports Medicine Position Stand. Exercise and physical activity for older adults. Med Sci Sports Exerc. 2009;41(7):1510–30. 6. Askew CD, Parmenter B, Leicht AS, Walker PJ, Golledge J. Exercise & Sports Science Australia (ESSA) position statement on exercise prescription for patients with peripheral arterial disease and intermittent claudication. J Sci Med Sport. 2014;17(6):623–9. 7. Atterhög JH, Jonsson B, Samuelsson R. Exercise testing: a prospective study of complication rates. Am Heart J. 1979;98(5):572–9. 8. Biswas A, Oh PI, Faulkner GE, et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med. 2015;162(2):123–32. 9. Black A, Black MM, Gensini G. Exertion and acute coronary artery injury. Angiology. 1975;26(11):759–83. 10. Blair SN, Kohl HW III, Barlow CE, Paffenbarger RS Jr, Gibbons LW, Macera CA. Changes in physical fitness and all-cause mortality. A prospective study of healthy and unhealthy men. JAMA. 1995;273(14):1093–8. 11. Blair SN, Kohl HW III, Paffenbarger RS Jr, Clark DG, Cooper KH, Gibbons LW. Physical fitness and all-cause mortality. A prospective study of healthy men and women. JAMA. 1989;262(17): 2395–401. 12. Bullock SH, Jones BH, Gilchrist J, Marshall SW. Prevention of physical training-related injuries recommendations for the military and other active populations based on expedited systematic reviews. Am J Prev Med. 2010;38:S156–181. 13. Carlson DJ, Dieberg G, Hess NC, Millar PJ, Smart NA. Isometric exercise training for blood pressure management: a systematic review and meta-analysis. Mayo Clin Proc. 2014;89(3):327–34. 14. Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100(2):126–31. 15. Centers for Disease Control and Prevention. Adult participation in aerobic and muscle-strengthening activities — United States, 2011. MMWR Morb Mortal Wkly Rep. 2013;62(17):326–30. 16. Ciampricotti R, Deckers JW, Taverne R, el Gamal M, Relik-van Wely L, Pool J. Characteristics of conditioned and sedentary men with acute coronary syndromes. Am J Cardiol. 1994;73(4):219–22. 17. Colberg SR, Sigal RJ, Fernhall B, et al. Exercise and type 2 diabetes: the American College of Sports Medicine and the American Diabetes Association: joint position statement. Diabetes Care. 2010;33(12):e147–67. 18. Corrado D, Basso C, Rizzoli G, Schiavon M, Thiene G. Does sports activity enhance the risk of sudden death in adolescents and young adults? J Am Coll Cardiol. 2003;42(11):1959–63. 19. Corrado D, Pelliccia A, Bjørnstad HH, et al. Cardiovascular pre-participation screening of young competitive athletes for prevention of sudden death: proposal for a common European protocol. Consensus Statement of the Study Group of Sport Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. Eur Heart J. 2005;26(5):516–24. 20. Dahabreh IJ, Paulus J. Association of episodic physical and sexual activity with triggering of acute cardiac events: systematic review and meta-analysis. JAMA. 2011;305(12):1225–33. 21. Digenio AG, Sim JG, Dowdeswell RJ, Morris R. Exercise-related cardiac arrest in cardiac rehabilitation. The Johannesburg experience. S Afr Med J. 1991;79(4):188–91. ACSM-GETP10e_Ch01.indd 17 11/3/16 1:38 AM 18 Guidelines for Exercise Testing • www.acsm.org 22. Donnelly JE, Blair SN, Jakicic JM, et al. American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009;41(2):459–71. 23. Drezner JA, O’Connor FG, Harmon KG, et al. AMSSM position statement on cardiovascular preparticipation screening in athletes: current evidence, knowledge gaps, recommendations and future directions. Curr Sports Med Rep. 2016;15(5):359–75. 24. Franklin BA. Preventing exercise-related cardiovascular events: is a medical examination more urgent for physical activity or inactivity? Circulation. 2014;129(10):1081–4. 25. Franklin BA, Bonzheim K, Gordon S, Timmis GC. Safety of medically supervised outpatient cardiac rehabilitation exercise therapy: a 16-year follow-up. Chest. 1998;114(3):902–6. 26. Garber CE, Blissmer B, Deschenes MR, et al. American College of Sports Medicine position stand. The quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334–559. 27. Gibbons L, Blair SN, Kohl HW, Cooper K. The safety of maximal exercise testing. Circulation. 1989;80(4):846–52. 28. Gilchrist J, Jones BH, Sleet DA, Kimsey C. Exercise-related injuries among women: strategies for prevention from civilian and military studies. MMWR Recomm Rep. 2000;49(RR-2):15–33. 29. Giri S, Thompson PD, Kiernan FJ, et al. Clinical and angiographic characteristics of exertionrelated acute myocardial infarction. JAMA. 1999;282(18):1731–6. 30. Hallal PC, Andersen LB, Bull FC, et al. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380(9838):247–57. 31. Hammoudeh AJ, Haft J. Coronary-plaque rupture in acute coronary syndromes triggered by snow shoveling. N Engl J Med. 1996;335(26):2001. 32. Harmon KG, Drezner JA, Wilson MG, Sharma S. Incidence of sudden cardiac death in athletes: a state-of-the-art review. Heart. 2014;100(16):1227–34. 33. Haskell WL. Cardiovascular complications during exercise training of cardiac patients. Circulation. 1978;57(5):920–4. 34. Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39(8):1423–34. 35. Healy GN, Dunstan DW, Salmon J, et al. Breaks in sedentary time: beneficial associations with metabolic risk. Diabetes Care. 2008;31(4):661–6. 36. Healy GN, Matthews CE, Dunstan DW, Winkler EA, Owen N. Sedentary time and cardiometabolic biomarkers in US adults: NHANES 2003-06. Eur Heart J. 2011;32(5):590–7. 37. Hollingworth M, Harper A, Hamer M. Dose–response associations between cycling activity and risk of hypertension in regular cyclists: the UK Cycling for Health Study. J Hum Hypertens. 2015;29(4):219–23. 38. Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311–9. 39. Hootman JM, Macera CA, Ainsworth BE, Addy CL, Martin M, Blair SN. Epidemiology of musculoskeletal injuries among sedentary and physically active adults. Med Sci Sports Exerc. 2002;34(5):838–44. 40. Hootman JM, Macera CA, Ainsworth BE, Martin M, Addy CL, Blair SN. Association among physical activity level, cardiorespiratory fitness, and risk of musculoskeletal injury. Am J Epidemiol. 2001;154(3):251–8. 41. Irving JB, Bruce RA, DeRouen TA. Variations in and significance of systolic pressure during maximal exercise (treadmill) testing. Am J Cardiol. 1977;39(6):841–8. 42. Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63(25):2985–3023. 43. Kaplan RM, Hermann AK, Morrison JT, DeFina LF, Morrow JR Jr. Costs associated with women’s physical activity musculoskeletal injuries: the women’s injury study. J Phys Act Health. 2014;11(6):1149–55. ACSM-GETP10e_Ch01.indd 18 11/3/16 1:38 AM Chapter 1 Benefits and Risks Associated with Physical Activity 19 44. Katzmarzyk PT, Church TS, Craig CL, Bouchard C. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med Sci Sports Exerc. 2009;41(5):998–1005. 45. Kesaniemi YK, Danforth E Jr, Jensen MD, Kopelman PG, Lefèbvre P, Reeder BA. Dose-response issues concerning physical activity and health: an evidence-based symposium. Med Sci Sports Exerc. 2001;33(Suppl 6):S351–8. 46. Kim JH, Malhotra R, Chiampas G, et al. Cardiac arrest during long-distance running races. N Engl J Med. 2012;366(2):130–40. 47. Kim Y, Wilkens LR, Park SY, Goodman MT, Monroe KR, Kolonel LN. Association between various sedentary behaviours and all-cause, cardiovascular disease and cancer mortality: the Multiethnic Cohort Study. Int J Epidemiol. 2013;42(4):1040–56. 48. Knight JA, Laubach CA Jr, Butcher RJ, Menapace FJ. Supervision of clinical exercise testing by exercise physiologists. Am J Cardiol. 1995;75(5):390–1. 49. Kodama S, Saito K, Tanaka S, et al. Cardiorespiratory fitness as a quantitative predictor of allcause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA. 2009;301(19):2024–35. 50. Kohl HW III, Craig CL, Lambert EV, et al. The pandemic of physical inactivity: global action for public health. Lancet. 2012;380(9838):294–305. 51. Koster A, Caserotti P, Patel KV, et al. Association of sedentary time with mortality independent of moderate to vigorous physical activity. PLoS One. 2012;7(6):e37696. 52. Lee IM, Rexrode KM, Cook NR, Manson JE, Buring JE. Physical activity and coronary heart disease in women: is “no pain, no gain” passe? JAMA. 2001;285(11):1447–54. 53. Ljungqvist A, Jenoure P, Engebretsen L, et al. The International Olympic Committee (IOC) consensus statement on periodic health evaluation of elite athletes, March 2009. Br J Sports Med. 2009;43(9):631–43. 54. Loprinzi PD, Lee H, Cardinal BJ. Dose response association between physical activity and biological, demographic, and perceptions of health variables. Obes Facts. 2013;6(4):380–92. 55. Malinow M, McGarry D, Kuehl K. Is exercise testing indicated for asymptomatic active people? J Cardiac Rehab. 1984;4:376–9. 56. Manniche C, Lundberg E, Christensen I, Bentzen L, Hesselsøe G. Intensive dynamic back exercises for chronic low back pain: a clinical trial. Pain. 1997;47(1):53–63. 57. Manson JE, Greenland P, LaCroix AZ, et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. 2002;347(10):716–25. 58. Maron BJ, Doerer JJ, Haas TS, Tierney DM, Mueller FO. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980-2006. Circulation. 2009;119(8): 1085–92. 59. Maron BJ, Haas TS, Murphy CJ, Ahluwalia A, Rutten-Ramos S. Incidence and causes of sudden death in U.S. college athletes. J Am Coll Cardiol. 2014;63(16):1636–43. 60. Maron BJ, Shirani J, Poliac LC, Mathenge R, Roberts WC, Mueller FO. Sudden death in young competitive athletes. Clinical, demographic, and pathological profiles. JAMA. 1996;276(3):199–204. 61. Maron BJ, Thompson PD, Ackerman MJ, et al. Recommendations and considerations related to preparticipation screening for cardiovascular abnormalities in competitive athletes: 2007 update: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism: endorsed by the American College of Cardiology Foundation. Circulation. 2007;115(12):1643–455. 62. Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167(7):875–81. 63. Matthews CE, George SM, Moore SC, et al. Amount of time spent in sedentary behaviors and cause-specific mortality in US adults. Am J Clin Nutr. 2012;95(2):437–45. 64. McHenry PL. Risks of graded exercise testing. Am J Cardiol. 1977;39(6):935–7. 65. Messier SP. Obesity and osteoarthritis: disease genesis and nonpharmacologic weight management. Med Clin North Am. 2009;93(1):145–159. 66. Mittleman MA, Maclure M, Tofler GH, Sherwood JB, Goldberg RJ, Muller JE. Triggering of acute myocardial infarction by heavy physical exertion. Protection against triggering by regular exertion. Determinants of Myocardial Infarction Onset Study Investigators. N Engl J Med. 1993;329(23):1677–83. ACSM-GETP10e_Ch01.indd 19 11/3/16 1:38 AM 20 Guidelines for Exercise Testing • www.acsm.org 67. Moore SC, Lee I, Weiderpass E, et al. Association of leisure-time physical activity with risk of 26 types of cancer in 1.44 million adults. JAMA Intern Med. 2016;176(6):816–25. doi:10.1001 /jamainternmed.2016.1548 68. Morrow JR Jr, DeFina LF, Leonard D, Trudelle-Jackson E, Custodio MA. Meeting physical activity guidelines and musculoskeletal injury: the WIN study. Med Sci Sports Exerc. 2012;44(10): 1986–92. 69. Naci H, Ioannidis J. Comparative effectiveness of exercise and drug interventions on mortality outcomes: metaepidemiological study. BMJ. 2013;347:f5577. 70. Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39(8):1435–45. 71. Paffenbarger RS Jr, Hyde RT, Wing AL, Lee IM, Jung DL, Kampert JB. The association of changes in physical-activity level and other lifestyle characteristics with mortality among men. N Engl J Med. 1993;328(8):538–45. 72. Paffenbarger RS Jr, Lee IM. Smoking, physical activity, and active life expectancy. Clin J Sport Med. 1999;9(4):244. 73. Pate RR, Pratt M, Blair SN, et al. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273(5):402–7. 74. Pescatello LS, Franklin BA, Fagard R, et al. American College of Sports Medicine position stand. Exercise and hypertension. Med Sci Sports Exerc. 2004;36(3):533–53. 75. Physical activity and cardiovascular health. NIH Consensus Development Panel on Physical Activity and Cardiovascular Health. JAMA. 1996;276(3):241–6. 76. Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Report, 2008 [Internet]. Washington (DC): U.S. Department of Health and Human Services; 2008 [updated Sep 24]. 683 p. Available from: http://www.health.gov/paguidelines/Report/pdf /CommitteeReport.pdf 77. President’s Council on Physical Fitness and Sports. Definitions — Health, Fitness, and Physical Activity [Internet]. Washington (DC): President’s Council on Physical Fitness and Sports; 2000 [cited 2016 Jun 6]. Available from: http://purl.access.gpo.gov/GPO/LPS21074 78. Rochmis P, Blackburn H. Exercise tests. A survey of procedures, safety, and litigation experience in approximately 170,000 tests. JAMA. 1971;217(8):1061–6. 79. Rockhill B, Willett WC, Manson JE, et al. Physical activity and mortality: a prospective study among women. Am J Public Health. 2001;91(4):578–83. 80. Saris WH, Blair SN, van Baak MA, et al. How much physical activity is enough to prevent unhealthy weight gain? Outcome of the IASO 1st Stock Conference and consensus statement. Obes Rev. 2003;4(2):101–14. 81. Scheinowitz M, Harpaz D. Safety of cardiac rehabilitation in a medically supervised, communitybased program. Cardiology. 2005;103(3):113–7. 82. Schmid D, Ricci C, Leitzmann MF. Associations of objectively assessed physical activity and sedentary time with all-cause mortality in US adults: the NHANES study. PLoS One. 2015;10(3):e0119591. 83. Schwingshackl L, Missbach B, Dias S, König J, Hoffmann G. Impact of different training modalities on glycaemic control and blood lipids in patients with type 2 diabetes: a systematic review and network meta-analysis. Diabetologia. 2014;57(9):1789–97. 84. Sesso HD, Paffenbarger RS Jr, Lee IM. Physical activity and coronary heart disease in men: the Harvard Alumni Health Study. Circulation. 2000;102(9):975–80. 85. Siscovick DS, Weiss NS, Fletcher RH, Lasky T. The incidence of primary cardiac arrest during vigorous exercise. N Engl J Med. 1984;311(14):874–7. 86. Strickland JC, Smith M. The anxiolytic effects of resistance exercise. Front Psychol. 2014;5:753. 87. Stuart RJ Jr, Ellestad MH. National survey of exercise stress testing facilities. Chest. 1980;77(1):94–7. 88. Tanasescu M, Leitzmann MF, Rimm EB, Willett WC, Stampfer MJ, Hu FB. Exercise type and intensity in relation to coronary heart disease in men. JAMA. 2002;288(16):1994–2000. ACSM-GETP10e_Ch01.indd 20 11/3/16 1:38 AM Chapter 1 Benefits and Risks Associated with Physical Activity 21 89. Thompson PD, Franklin BA, Balady GJ, et al. Exercise and acute cardiovascular events placing the risks into perspective: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism and the Council on Clinical Cardiology. Circulation. 2007;115(17):2358–68. 90. Thompson PD, Funk EJ, Carleton RA, Sturner WQ. Incidence of death during jogging in Rhode Island from 1975 through 1980. JAMA. 1982;247(18):2535–8. 91. Thompson PD, Stern MP, Williams P, Duncan K, Haskell WL, Wood PD. Death during jogging or running. A study of 18 cases. JAMA. 1979;242(12):1265–7. 92. U.S. Department of Agriculture, U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2010. 7th ed. Washington (DC): U.S. Government Printing Office; 2010. 112 p. 93. U.S. Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans [Internet]. Washington (DC): U.S. Department of Health and Human Services; 2008 [cited 2016 Jun 6]. Available from: http://health.gov/paguidelines/pdf/paguide.pdf 94. U.S. Department of Health and Human Services. Physical Activity and Health: A Report of the Surgeon General. Atlanta (GA): U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; 1996. 278 p. 95. Van Camp SP, Bloor CM, Mueller FO, Cantu RC, Olson HG. Nontraumatic sports death in high school and college athletes. Med Sci Sports Exerc. 1995;27(5):641–7. 96. Van Camp SP, Peterson RA. Cardiovascular complications of outpatient cardiac rehabilitation programs. JAMA. 1986;256(9):1160–3. 97. Vincent HK, George SZ, Seay AN, Vincent KR, Hurley RW. Resistance exercise, disability, and pain catastrophizing in obese adults with back pain. Med Sci Sports Exerc. 2014;46(9):1693–701. 98. Vongvanich P, Paul-Labrador MJ, Merz CN. Safety of medically supervised exercise in a cardiac rehabilitation center. Am J Cardiol. 1996;77(15):1383–5. 99. Wang CY, Haskell WL, Farrell SW, et al. Cardiorespiratory fitness levels among US adults 20-49 years of age: findings from the 1999-2004 National Health and Nutrition Examination Survey. Am J Epidemiol. 2010;171(4):426–35. 100. Wenger NK, Froelicher ES, Smith LK, et al. Cardiac rehabilitation as secondary prevention. Agency for Health Care Policy and Research and National Heart, Lung, and Blood Institute. Clin Pract Guidel Quick Ref Guide Clin. 1995;(17):1–23. 101. Whang W, Manson JE, Hu FB, et al. Physical exertion, exercise, and sudden cardiac death in women. JAMA. 2006;295(12):1399–403. 102. Williams MA, Haskell WL, Ades PA, et al. Resistance exercise in individuals with and without cardiovascular disease: 2007 update: a scientific statement from the American Heart Association Council on Clinical Cardiology and Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2007;116(5):572–84. 103. Williams PT. Dose-response relationship of physical activity to premature and total all-cause and cardiovascular disease mortality in walkers. PLoS One. 2013;8(11):e78777. 104. Williams PT. Physical fitness and activity as separate heart disease risk factors: a meta-analysis. Med Sci Sports Exerc. 2001;33(5):754–61. 105. Willich SN, Lewis M, Löwel H, Arntz HR, Schubert F, Schröder R. Physical exertion as a trigger of acute myocardial infarction. Triggers and Mechanisms of Myocardial Infarction Study Group. N Engl J Med. 1993;329(23):1684–90. 106. Yang Z, Scott CA, Mao C, Tang J, Farmer AJ. Resistance exercise versus aerobic exercise for type 2 diabetes: a systematic review and meta-analysis. Sports Med. 2014;44(4):487–99. 107. Yu S, Yarnell JW, Sweetnam PM, Murray L. What level of physical activity protects against premature cardiovascular death? The Caerphilly study. Heart. 2003;89(5):502–6. ACSM-GETP10e_Ch01.indd 21 11/3/16 1:38 AM