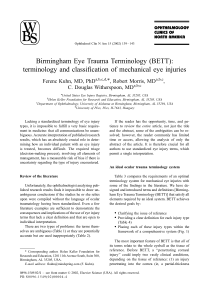
The Pediatric Traumatic Hyphema Danielle Trief, MD, MSc Olumuyiwa T. Adebona, MBChB, MPH Angela V. Turalba, MD Ankoor S. Shah, MD, PhD ’ Introduction The traumatic hyphema, defined as blood in the anterior chamber (AC) of the eye after trauma, occurs at a rate of approximately 17 per 100,000 per year.1 Between 70% and 75% of these patients are children, with a male-female ratio of at least 3:1.1,2 The complications of hyphema include corneal blood staining, elevated intraocular pressure (IOP), optic atrophy, and glaucoma. These complications can lead to visual impairment or even blindness. Children are an especially important population of hyphema patients, both because they comprise the majority of patients and because of important considerations in their treatment and management including amblyopia and compliance. This review broadly defines the traumatic hyphema: pathophysiology, classification, examination, complications, medical and surgical management, and long-term issues, with special attention toward the pediatric population. ’ Etiology and Pathophysiology In the United States, two thirds of traumatic hyphemas occur after blunt trauma and one third from a lacerating injury, with the majority of injuries occurring during sports.2,3 When a moving object hits the globe, it can distort the eye, leading to an equatorial stretching and posterior displacement of the lens-iris diaphragm.4 This stretching can produce tears in the anterior face of the ciliary body and iris vessels. Other causes INTERNATIONAL OPHTHALMOLOGY CLINICS Volume 53, Number 4, 43–57 r 2013, Lippincott Williams & Wilkins www.internat-ophthalmology.com | 43 44 ’ Trief et al of bleeding include iridodialysis or cyclodialysis.5 As bleeding ensues, the IOP increases and ultimately tamponades the vessels. A fibrin-platelet clot formation develops and bleeding stops.4,6 Maximal clot integrity is achieved approximately 4 to 7 days after the injury. Prior to this stabilization, rebleeding rates are highest. Clots are ultimately cleared by fibrinolytically active materials in the anterior chamber (AC).4 In addition to sports injuries, traumatic hyphemas are frequently seen after blunt trauma from airbag, paintball, or airsoft injuries.7–9 Hyphemas can also occur in the absence of trauma, and other etiologies should be considered in the proper setting. Hyphemas can result from iris neovascularization from diabetes, central retinal vein occlusion, carotid occlusive disease, or chronic retinal detachments.1 These conditions, however, are more common in adults. There have also been case reports of malignancy (retinoblastoma or iris melanoma) masquerading as hyphemas.10,11 The iris nodules that are seen in juvenile xanthogranuloma can bleed spontaneously as can iris vascular tufts.12,13 Hyphemas can be seen in some inflammatory conditions including keratouveitis, Fuchs heterochromic iridocyclitis, and uveitisglaucoma-hyphema syndrome.1 Rarer medical causes of hyphema include myotonic dystrophy, leukemia, and hemophilia. Hyphemas can also be secondary to surgical or laser procedures, like the laser iridotomy. ’ Classification Hyphemas are quantified as either microscopic or macroscopic (Table 1).17 Macroscopic hyphemas can be graded according to the percentage of space they occupy or their height in millimeters in the AC. Microscopic hyphemas are quantified between 1 and 4+ red blood cells in the AC. Immediately after trauma the red blood cells may still be suspended in the AC making classification difficult. If the patient remains erect or lies in a position in which the head of the bed is elevated 30 to 45 degrees, the blood will settle inferiorly, and grading of the hyphema can be achieved. Careful documentation of the grade ensures adequate monitoring of clearance of the blood over time. ’ History A careful history is essential in the diagnosis and management of hyphema. First, the mechanism of injury must be elicited because it can help a physician determine whether the hyphema is present in isolation or whether there may be other traumas. Head injuries, fractures, and open-globe injuries (OGI) must be considered and ruled out before documenting a closed-globe injury with hyphema. It is paramount to www.internat-ophthalmology.com Fills entirety of the anterior chamber 1/2 to nearly entire anterior chamber Between 1/3 and 1/2 of anterior chamber Less than 1/3 of anterior chamber 1+ cell = 6-15 cells/ HPF (1 1 mm slit beam) 2+ cell = 16-25 cells 3+ cell = 26-50 cells 4+ cell = >50 cells Grade 4 Grade 3 Grade 2 Grade 1 Microscopic (based on the SUN working group consensus for uveitis)16 Grade Percentage of Anterior Chamber Illustration 58 20 14 8 75-90 75-90 65-70 25-50 25-50 Frequency of Visual Prognosis Macroscopic of 20/50 or Hyphemas2 (%) Better14,15 (%) Table 1. Quantification of a Hyphema With its Frequency and Visual Prognosis. The Frequency and Visual Prognosis are Based on Studies in Both Pediatric and Adult Populations. Modified From Brandt and Haug,15 with permission from Elsevier. Adaptations are themselves works protected by copyright. So in order to publish this adaptation, authorization must be obtained both from the owner of the copyright in the original work and from the owner of copyright in the translation or adaptation. Pediatric Traumatic Hyphema ’ 45 www.internat-ophthalmology.com 46 ’ Trief et al consider OGI in all hyphemas, especially when there are lacerating injuries or hyphemas secondary to small, high-velocity, and/or sharp objects (eg, BB guns, pellet or shot guns, metal from power tools, drills, or saws).14 The pediatric trauma examination can be challenging, and OGIs can be subtle. If there is suspicion for an OGI and an examination cannot be performed adequately, the physician should consider an examination under anesthesia. The child’s ocular history is also important. If a recent visual acuity is available, this should be documented so that it can be used to compare acuities in subsequent examinations. A history of amblyopia or strabismus should also be noted because this may limit the extent of the child’s visual recovery. The family should be questioned about a history of sickle-cell disease or blood dyscrasias as this will change the prognosis and management of the hyphema (see special populations below). Finally, a review of systems focusing on nausea and vomiting should be elicited, as valsava maneuvers can worsen bleeding. Somnolence is common, especially in children, and it may be difficult to obtain a full history from the child alone.2 When possible, additional history should be obtained from the family or from witnesses. One must always consider non-accidental trauma/abusive head trauma and involve social services as needed. African American, Afro-Caribbean, and Hispanic patients should be screened for sickle-cell disease through a sickle-cell preparation. If this is positive, a hemoglobin electrophoresis can distinguish sickle-cell anemia from trait.18 In patients with bleeding disorders, laboratory tests such as prothrombin/partial thromboplastin time, platelet count, liver function tests, and bleeding time should be ordered. ’ Examination The initial examination must rule out an OGI and must then carefully document the hyphema for comparison with subsequent examinations. Visual acuity should be measured and documented. Immediately after injury, acuity may be severely impaired because of the suspension of blood in the AC. As the blood settles inferiorly, the vision usually improves. The pupils and iris should be examined for an afferent pupillary defect, anisocoria (often secondary to torn iris sphincters), and iridodialysis. Once an OGI is ruled out, the IOP should be measured and documented. This may be difficult in an unhappy child, and special tonometers such as the Icare (Icare Finland Oy, Espoo, Finland) and Perkins tonometer can be useful. The anterior segment should be examined for eyelid abrasions or lacerations, orbital trauma, conjunctival lacerations or hemorrhages, corneal edema, corneal abrasions or foreign bodies, traumatic cataract, www.internat-ophthalmology.com Pediatric Traumatic Hyphema ’ 47 zonular dehiscence, and lens subluxation. A fundoscopic examination should be performed to look for vitreous hemorrhage, choroidal rupture, commotio retinae, retinal hemorrhages, and retinal breaks, tears, or retinal dialyses. It is recommended that both scleral depression and gonioscopy be deferred until at least 1 month after presentation to prevent worsening bleeding or secondary hemorrhage.6 The initial examination may be limited as blood may obscure the view of both the anterior and posterior segment. In these cases, B-scan ultrasonography, ultrasound biomicroscopy, and magnetic resonance and computed tomography imaging should be used judiciously to rule-out posterior pathologies such as retinal detachments, OGIs, or foreign bodies. There have been no studies investigating how frequently patients should be seen in outpatient follow-up. However, most authors recommend very frequent follow-ups (several times weekly or daily) while a layered hyphema is still present to monitor for the development of complications.2,19,20 ’ Complications Hyphema can lead to several complications including amblyopia, corneal blood staining, secondary hemorrhages, elevated IOP, inflammatory changes, optic nerve damage, and long-term issues. In children, there is a theoretical risk that the hyphema can cause vision deprivation, which can lead to amblyopia. However, in a retrospective review of 316 children, only 2 patients developed amblyopia. Both of these children had a traumatic cataract, which was felt to be the cause of the amblyopia.21 Corneal blood staining occurs in approximately 5% of patients with a hyphema and can also lead to amblyopia.2 With rare exceptions, these patients have near-total or total hyphemas. Corneal blood staining is also associated with secondary hemorrhage, prolonged clot, elevated IOP, and preexisting endothelial dysfunction.1 On pathologic specimens, hemoglobin and hemosiderin deposits have been found in the central corneal stroma.22,23 There is also evidence that protoporphyrin, a blood product, can photosensitize the endothelium, leading to its decompensation in ambient light.24 Because of this, some clinicians have recommended patching eyes with long-standing hyphemas.1,25 The first clinical signs of corneal blood staining are tiny, yellow granules that appear in the deep stroma. A lack of definition of the fibrillar structure of the corneal stroma can also be seen.2 This process usually starts centrally and moves peripherally; clearance typically occurs reciprocally, and it may take months or years to clear completely.1 In these cases, one must consider surgery to prevent corneal damage and eventual amblyopia, depending on the age of the child. www.internat-ophthalmology.com 48 ’ Trief et al A second hemorrhage or rebleed is another complication that many studies have shown to lead to a worse visual prognosis.26 Studies have found that about 80% of patients with hyphemas ultimately achieve visual acuities better than 20/50, whereas only 64% of patients who have secondary hemorrhages achieve this level of vision.2 Further, patients with secondary hemorrhages are more likely to need a surgical intervention.27 The need for intervention and the poor prognosis with rebleeds is one argument used for daily ophthalmological examinations. The examiner should look for evidence of fresh blood around a dark, central clot or an increase in the size of the hyphema. However, one must distinguish fresh blood from clot degradation products, which change the color of the clot. The critical time for secondary hemorrhage is in the first 4 to 7 days after injury, when the clot is still stabilizing.14,26 The rate of secondary hemorrhage varies between 2% and 38%, depending on the population.1,4 Higher rates of secondary hemorrhage have been found among African Americans.3,28,29 Spoor et al3 reported a secondary hemorrhage rate of 24.2% for African Americans compared with 4.5% for whites. The etiology for this finding is not known, but one hypothesis is that melanin plays a role. Lai et al30 injected melanin into a rabbit eye and then induced a hyphema with a neodymium-doped yttrium aluminium garnet (ND:YAG) laser. The eyes with melanin had higher rates of secondary hemorrhage and prolonged absorption. Rates are also significantly higher for patients with sickle-cell disease or trait.18 Some studies have found that younger patients also have higher rates of secondary hemorrhage.2 This may be because pediatric patients have difficulty maintaining ‘‘limited activity’’ restrictions. Finally, some studies,31,32 but not all,33 have found that ingestion of aspirin leads to higher rates of secondary hemorrhage. It is generally recommended that patients avoid aspirin or nonsteroidal antiinflammatory drugs when being treated for hyphema. Fluctuations in IOP are another complication associated with acute hyphemas. In the first 24 hours, 32% of patients have IOPs>22.2 The mechanism is thought to be plugging of the trabecular meshwork by erythrocytes and fibrin.4 This is sometimes followed by a period of low IOP secondary to reduced aqueous production and uveitis. As the ciliary body recovers, the pressure can rise again. Rarely, an occult cyclodialysis cleft can cause low IOP in the setting of hyphema and should be considered. High pressures are more common with larger hyphemas.34 In total hyphemas, the incidence of elevated IOP is >95%.20 Large collar-button clots that involve both the anterior and posterior chamber can produce pupillary block. The inflammation associated with hyphema can lead to synechiae: posterior synechiae (adhesions between the iris and the lens) and peripheral anterior synechiae (PAS; adhesions between the iris and cornea). Both are seen more frequently in hyphemas that last for >1 www.internat-ophthalmology.com Pediatric Traumatic Hyphema ’ 49 week.1 Accommodation may also be impaired. This is seen in as many as 7% of patients after traumatic hyphema.35 Optic atrophy, which presents as pallor without glaucomatous cupping, is seen in approximately 6% of hyphema patients.1 It is most frequently seen with acute elevated pressures and in patients with sickle-cell disease. ’ Long-term Issues Damage to the iris through synechiae and iris sphincter tears can result in an abnormal pupil. Traumatic mydriasis is observed when the pupil is abnormally dilated. Physicians should describe these findings to patients and families and note if anisocoria is present. This knowledge can spare a patient a work up for anisocoria in the future. Glaucoma is a lifelong risk factor for patients with hyphema. Children and their parents should be educated on this and instructed to have at least yearly eye examinations. Angle recession, defined as a separation of the longitudinal fibers from the circular fibers of the ciliary body, occurs in up to 85% of patients with hyphema.21,36 Glaucoma is more frequently seen when >180 degrees of the iris is involved.37 The risk of angle recession glaucoma ranges from 0% to 20%.2 In a cohort study using the United States Eye Injury Registry, the risk of developing posttraumatic glaucoma after an ocular contusion (blunt injury) was 3.39% within 6 months of follow-up. Longer follow-up was not evaluated. Glaucoma was independently associated with both hyphema (relative risk = 2.23) and angle recession (relative risk = 1.71).38 Gonioscopy should be performed at 1 month to document the presence and extent of angle recession. The patient’s IOP should then be monitored regularly. Further studies are needed to investigate the long-term risk of glaucoma after hyphema. In addition to angle recession, glaucoma can result from destruction and fibrosis of the trabecular meshwork, siderosis of the trabecular endothelium, PAS, and secondary angle-closure glaucoma or ghost-cell glaucoma. Ghostcell glaucoma occurs when there is an associated vitreous hemorrhage and can be seen 2 weeks to 3 months after the onset of bleeding.39 ’ Prevention As the majority of hyphemas occur in children and in sports injuries, children should be encouraged to wear safety goggles.40 ’ Treatment In the acute setting, the goals of treatment are to triage associated injuries, provide comfort, prevent secondary hemorrhage, and treat www.internat-ophthalmology.com 50 ’ Trief et al elevated IOP. Whether treatment should occur in the outpatient or inpatient setting is a source of long-standing debate. The advantages of the inpatient setting are that activities can be monitored and restricted, medication administration can be ensured, and patients can be assisted should they receive bilateral patching. A major disadvantage of hospitalization is the cost. Further, several studies have found no significant benefit of treating hyphemas at home as compared with those being treated on an inpatient basis.2,26,36,41,42 In 1 retrospective review, the secondary hemorrhage rate for outpatients was 4.5% compared with 5.0% for inpatients.19 Historically, children have been admitted, as they are more likely to be active and rebleed. In fidgety children, sedation with benzodiazepines has even been utilized.43 However, studies have again found no difference in secondary hemorrhage rates or final visual outcome in patients admitted versus those discharged home, and children have done quite well when discharged with strict instructions for medication and activity.34 It is now more common to discharge patients with daily follow-up. Hospital admission may be beneficial for higher-risk patients (Table 2). Regardless of whether or not the patient is admitted, most clinicians recommend ‘‘limited activity’’ to prevent secondary hemorrhage. This is usually enforced until the hyphema clears. Patients are also encouraged to elevate the head of the bed to at least 30 to 45 degrees, which allows the blood to settle inferiorly, facilitating the examination and preventing PAS. Most physicians also recommend a protective shield. This can be worn either at night only or for the entire day. In young patients, a clear plastic shield is preferable to an opaque one as it minimizes the risk of occlusive amblyopia. In the past, physicians would use bilateral patches to limit eye movement. A Cochrane review, however, found no difference in single versus bilateral patching or ambulation versus complete bed rest on the risk of secondary hemorrhage or on the visual acuity outcome.26 Some authors have recommended refraining from reading, as accommodation can theoretically stress injured vessels,14 although this has not been formerly studied. As mentioned above, most authors recommend against aspirin or nonsteroidal anti-inflammatory drugs, although studies have found mixed results in terms of rates of rebleeding.32,33 For pain management, acetominophen and, if necessary, opiates can be used instead. Table 2. Patients for Whom Hospitalization Should be Considered.2 Secondary hemorrhages (rebleed) Penetrating ocular trauma Hyphemas >50% Noncompliant patients or parents Suspected abuse Patients with sickle-cell anemia/trait www.internat-ophthalmology.com Pediatric Traumatic Hyphema ’ ’ 51 Medical Management Elevated IOP is seen in one third of hyphema patients at presentation and should be treated as necessary. The first-line treatment is a topical aqueous suppressant—for example, b-blockers.4 Carbonic anhydrase inhibitors are sometimes used, but care must be taken in sickle-cell patients (see below). Prostaglandins and miotics are typically avoided as they can lead to increased inflammation.1 a-Adrenergic agonists are used in adults but should be avoided in very young children as they can cause central nervous system and respiratory depression.44 When topical therapy is insufficient, oral therapy with acetazolamide or methazolamide can be used. Again, these therapies are typically avoided in sicklecell patients because they can produce metabolic acidosis and volume depletion, which worsens sickling.6 Cycloplegics are used both for comfort and also for iris muscle paralysis, which can theoretically prevent secondary hemorrhage. Dilation of the iris may also prevent the formation of posterior synechiae. Topical atropine, cyclopentolate, or scopolamine is commonly used for this. In children, atropine has the advantage of less frequent drop administration. There is little evidence for this practice. As mentioned above, miotics are typically avoided. One study reported a longer time to resolution of a hyphema among patients treated with pilocarpine compared with atropine.45 Both topical and systemic steroids have been used to treat hyphemas. The mechanism of action is thought to be 3-fold: (1) stabilization of the blood ocular barrier; (2) inhibition of fibrinolysis to prevent secondary hemorrhage; and (3) reduced inflammation.14,46 Several studies have shown significantly decreased rates of secondary hemorrhage among patients treated with topical steroids compared with those without.1,47,48 However, a recent Cochrane review concluded that there are no significance differences in terms of the resolution of primary hemorrhage, risk of secondary hemorrhage, or risk of increased IOP in patients treated with topical steroids compared with controls.26 In any case, topical steroids are also beneficial in that they reduce inflammation and can therefore provide comfort and prevent PAS formation, although this has not formerly been studied. However, caution should be exercised in the long-term use of steroids in children because of the risk for cataracts and glaucoma.49,50 There has been a wealth of literature on the use of antifibrinolytic agents in the prevention of secondary hemorrhage.43,51–53 In the United States, E-aminocaproic acid (Amicar; Xanodyne Pharmaceuticals, Newport, KY) is most commonly used. Plasmin usually binds to lysine molecules in a clot. h-Aminocaproic acid resembles lysine and competitively occupies the binding site on plasmin thus inhibiting fibrin clot digestion.1 Multiple studies including a Cochrane meta-analysis have found decreased rates of secondary hemorrhage in patients who have www.internat-ophthalmology.com 52 ’ Trief et al been treated with Amicar compared with controls.26 Historically, h-aminocaproic acid was administered intravenously, but more recently topical preparations have been created and have been found to have similar efficacy to the intravenous preparations.54 h-Aminocaproic acid has been used safely in children,53 although h-aminocaproic acid does carry a risk of clotting and is contraindicated in patients with active intravascular thrombosis. Relative contraindications include pregnancy and renal, hepatic, or cardiac disease.1 It has a high side-effect profile including nausea, vomiting, and postural hypotension. Discontinuation of h-aminocaproic acid can lead to secondary hemorrhage.51 Systemic and local side effects can also be seen for the topical preparation.54 Patients using h-aminocaproic acid take a significantly longer time to clear the clot compared with those without it.51,52 As a large clot can obstruct vision, authors have recommended against the use of haminocaproic acid for clots >50% of the AC.2 Another antifibrinolytic agent, tranexamic acid, also a lysine analog, is more commonly used outside the United States. Tranexamic acid has also has been shown to prevent secondary hemorrhage.26,55–57 Tranexamic acid has been studied in children and found to be safe.58,59 In vitro, it is 5 to 10 more potent than Amicar, and there are less gastric side effects.26 Several other experimental treatments have been used. Conjugated estrogen (Premarin) was hypothesized to decrease secondary hemorrhages by increasing prothrombin concentration and decreasing antithrombin activity. A case series showed promising results, but the rates of secondary hemorrhage were not significant in a prospective randomized control trial.60,61 Intracameral tissue plasminogen activator (t-PA) has been used to break up persistent clots; however, use of t-PA does carry the risk for hemorrhage. In a case series of 3 eyes with persistent total hyphemas, t-PA led to the resolution of all 3 hyphemas; however, 1 patient developed a vitreous hemorrhage.62 ’ Surgical Management Hyphemas are largely treated medically, but approximately 5% of patients ultimately require surgical intervention.1 The indications for surgery are outlined in Table 3. Table 3. Patients for Whom Surgery Should be Considered.4,14 Uncontrolled IOP >50 mm Hg for 5 d or 35 mm Hg for 7 d In sickle-cell patients >25 mm Hg for >24 h Corneal blood staining Total hyphemas that persist for >5 d Large clots that persist for >10 d to avoid posterior synechiae IOP indicates intraocular pressure. www.internat-ophthalmology.com Pediatric Traumatic Hyphema ’ 53 The purpose of surgery is to clear blood from the AC to prevent corneal blood staining and/or elevated IOP. This can be performed by irrigationaspiration through a single incision, ‘‘hyphemectomy’’ using a microvitrectomy cutting-aspiration system, limbal clot delivery (most effective after clot consolidation, which occurs 4 to 7 days after injury), or trabeculectomy with AC wash out.1,4,6 One risk of surgical evacuation of the clot is rebleeding. ’ Special Populations Patients with sickle-cell anemia or sickle-cell trait who have hyphemas are at higher risk for elevated IOP, optic atrophy, secondary hemorrhage, and visual impairment.1,63,64 The irregular, ‘‘sickled’’ erythrocytes are more likely to clog the trabecular meshwork thereby decreasing outflow and leading to higher IOP. As IOP rises, hypoxia, acidosis, and hypercapnea in the AC produce further sickling. Patients with sickle-cell anemia and trait are also predisposed to optic nerve damage and central retinal artery occlusion. Even at IOP measurements in the mid 20s to 30s, these patients can experience permanent optic nerve damage.2 Rebleeding rates are also higher for sickle-cell patients. In 1 retrospective study of 99 children, 9 experienced secondary hemorrhage, all of whom were sickle-cell trait positive.63 In addition, as mentioned above, care must be taken with medical therapies as medications such as topical and oral carbonic anhydrase inhibitors can lead to hemo-concentration and systemic acidosis, thereby worsening sickling. Surgery should be considered earlier and at a lower IOP in patients with sickle-cell anemia (Table 3). Approximately 10% of African Americans carry the sickle-cell trait, and all African American patients who present with a hyphema without a known history of sickle-cell anemia should be screened by laboratory tests. Patients with bleeding dyscrasias like hemophilia can have spontaneous hyphemas or may develop hyphema after minor trauma, and they are also more prone to rebleed.65 Blood factors (eg, factor VIII in hemophilia A) should be maintained at normal levels, or antifibrinolytics should be used to prevent secondary hemorrhage.66 Patients and parents should be asked about a history of bleeding problems, and if there is concern, a compete blood count and coagulation tests should be performed. ’ Conclusions Although the majority of patients with traumatic hyphemas ultimately regain excellent visual acuity, complications such as secondary hemorrhage, corneal blood staining, and glaucoma can be sight threatening. Thus, these complications need to be monitored and detected early. In addition, the majority of hyphema patients are children, and www.internat-ophthalmology.com 54 ’ Trief et al Ocular trauma + hyphema History or family history of blood dyscrasias? yes no Follow up q3 months for 2 visits than q6 months for 1 year, then yearly if IOP is normal. yes yes no History of sickle cell? Open-globe injury? no unsure Open-globe injury? Sedated exam unsure yes Sickle cell preparation and if positive hemoglobin electrophoresis. Sickle cell or trait? Check PT, PTT, CBC, and depending on history, blood factors, replete factors as necessary, consider starting antifibrinolytics Repair open globe yes yes Consider admission to yes hospital if IOP > 25 Start topical beta blocker; avoid carbonic anhydrase inhibitors IOP > 25 at 24 hours? yes no Yearly follow up no Angle recession? 1 month follow up: gonioscopy and scleral depression Start atropine, topical prednisolone, head of bed elevated 30 -45 degrees, clear fox shield, Tylenol for pain (avoid ASA and NSAIDS) If sickle cell Consider antifibrinolytics Start topical beta blocker, carbonic anhydrase inhibitors (if not sickle cell), avoid alpha adrenergic agonist in young children yes IOP > 25? Surgery IOP > 50 for 5 days or > 35 for 7 days? yes Rebleed? no yes Consider admission, start anti -fibrinolytics no Daily follow up until gross hyphema clears Large clot persists greater than 10 days OR Total hyphema persists greater than 5 days OR Corneal blood staining Hyphema resolves Figure 1. Algorithm for the management of pediatric traumatic hyphema. The purple boxes represent a standard course without complications. The orange boxes represent complications or predisposing conditions to complications. therefore special care must be taken by a good history taking, tailored treatment, and long-term follow-up. Patients should be asked about blood dyscrasias, and African American patients should be screened for sickle-cell disease as these conditions may alter management. Treatment should be aimed at clearing the hyphema while maintaining good IOPs. If this is not possible through medical management, surgery is recommended. Given this information, we suggest the use of the algorithm shown in Figure 1. There are still many unanswered questions in the management of hyphemas: What is the ultimate rate of glaucoma? How frequently should patients be seen in the acute setting and in long-term follow-up? Should medical regiments be tailored for specific populations such as sickle-cell patients, pediatric patients, and adult patients? Future studies may address these unresolved issues. The authors declare that they have no conflicts of interest to disclose. www.internat-ophthalmology.com Pediatric Traumatic Hyphema ’ ’ 55 References 1. Walton W, Von Hagen S, Grigorian R, et al. Management of traumatic hyphema. Surv Ophthalmol. 2002;47:297–334. 2. Crouch ER Jr, Crouch ER. Management of traumatic hyphema: therapeutic options. J Pediatr Ophthalmol Strabismus. 1999;36:238–250. quiz 279-280. 3. Spoor TC, Kwitko GM, O’Grady JM, et al. Traumatic hyphema in an urban population. Am J Ophthalmol. 1990;109:23–27. 4. Zagelbaum BM, Hersh PS, Shingleton BJ, et al. Anterior Segment Trauma. In: Jakobiec FA, Albert DM, eds. Principles and Practice of Ophthalmology. 3rd ed. Vol 4: Philadelphia: Saunders; 2008:5093–5109. 5. Wilson FM. Traumatic hyphema. Pathogenesis and management. Ophthalmology. 1980;87:910–919. 6. Sankar PS, Chen TC, Grosskreutz CL, et al. Traumatic hyphema. Int Ophthalmol Clin. 2002;42:57–68. 7. Shazly TA, Al-Hussaini AK. Pediatric ocular injuries from airsoft toy guns. J Pediatr Ophthalmol Strabismus. 2012;49:54–57. 8. Motley WW III, Kaufman AH, West CE. Pediatric airbag-associated ocular trauma and endothelial cell loss. J AAPOS. 2003;7:380–383. 9. Lueder GT. Air bag-associated ocular trauma in children. Ophthalmology. 2000;107:1472–1475. 10. Shields JA, Shields CL, Materin M. Diffuse infiltrating retinoblastoma presenting as a spontaneous hyphema. J Pediatr Ophthalmol Strabismus. 2000;37:311–312. 11. Arentsen JJ, Green WR. Melanoma of the iris: report of 72 cases treated surgically. Ophthalmic Surg. 1975;6:23–37. 12. Blanksma LJ, Hooijmans JM. Vascular tufts of the pupillary border causing a spontaneous hyphaema. Ophthalmologica. 1979;178:297–302. 13. Bruner WE, Stark WJ, Green WR. Presumed juvenile xanthogranuloma of the iris and ciliary body in an adult. Arch Ophthalmol. 1982;100:457–459. 14. Andreoli CM, Gardiner MF. Traumatic hyphema: clinical features and management. In: Wiley JF, ed. Uptodate. Waltham: Wolters Kluwer; 2012. 15. Brandt MT, Haug RH. Traumatic hyphema: a comprehensive review. J Oral Maxillofac Surg. 2001;59:1462–1470. 16. Jabs DA, Nussenblatt RB, Rosenbaum JT. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005;140:509–516. 17. Edwards WC, Layden WE. Traumatic hyphema. A report of 184 consecutive cases. Am J Ophthalmol. 1973;75:110–116. 18. Lai JC, Fekrat S, Barron Y, et al. Traumatic hyphema in children: risk factors for complications. Arch Ophthalmol. 2001;119:64–70. 19. Shiuey Y, Lucarelli MJ. Traumatic hyphema: outcomes of outpatient management. Ophthalmology. 1998;105:851–855. 20. Sheppard JD, Crouch ER, Williams PB, et al. Hyphema. Medscape. 2011. Available at: http://emedicine.medscape.com/article/1190165-overview. Last accessed July 18, 2013. 21. Agapitos PJ, Noel LP, Clarke WN. Traumatic hyphema in children. Ophthalmology. 1987;94:1238–1241. 22. Pouliquen Y, Desvignes P. Ultrastructure of a hematocornea. Arch Ophtalmol Rev Gen Ophtalmol. 1967;27:45–52. 23. McDonnell PJ, Green WR, Stevens RE, et al. Blood staining of the cornea. Light microscopic and ultrastructural features. Ophthalmology. 1985;92:1668–1674. 24. Gottsch JD, Graham CR Jr, Hairston RJ, et al. Photoporphyrin IX photosensitization of corneal endothelium. Arch Ophthalmol. 1989;107:1497–1500. www.internat-ophthalmology.com 56 ’ Trief et al 25. Gottsch JD. Hyphema: diagnosis and management. Retina. 1990;10:(suppl 1): S65–S71. 26. Gharaibeh A, Savage HI, Scherer RW, et al. Medical interventions for traumatic hyphema. Cochrane Database Syst Rev. 2011;1:CD005431. 27. Thomas MA, Parrish RK II, Feuer WJ. Rebleeding after traumatic hyphema. Arch Ophthalmol. 1986;104:206–210. 28. Skalka HW. Recurrent hemorrhage in traumatic hyphema. Ann Ophthalmol. 1978;10: 1153–1157. 29. Palmer DJ, Goldberg MF, Frenkel M, et al. A comparison of two dose regimens of epsilon aminocaproic acid in the prevention and management of secondary traumatic hyphemas. Ophthalmology. 1986;93:102–108. 30. Lai WW, Bhavnani VD, Tessler HH, et al. Effect of melanin on traumatic hyphema in rabbits. Arch Ophthalmol. 1999;117:789–793. 31. Crawford JS, Lewandowski RL, Chan W. The effect of aspirin on rebleeding in traumatic hyphema. Am J Ophthalmol. 1975;80:(pt 2):543–545. 32. Gorn RA. The detrimental effect of aspirin on hyphema rebleed. Ann Ophthalmol. 1979;11:351–355. 33. Marcus M, Biedner B, Lifshitz T, et al. Aspirin and secondary bleeding after traumatic hyphema. Ann Ophthalmol. 1988;20:157–158. 34. Rocha KM, Martins EN, Melo LA Jr, et al. Outpatient management of traumatic hyphema in children: prospective evaluation. J Aapos. 2004;8:357–361. 35. Theriault FA, Pearce WG. Incidence of accommodative impairment following traumatic hyphema. Can J Ophthalmol. 1993;28:263–265. 36. Kennedy RH, Brubaker RF. Traumatic hyphema in a defined population. Am J Ophthalmol. 1988;106:123–130. 37. Sihota R, Kumar S, Gupta V, et al. Early predictors of traumatic glaucoma after closed globe injury: trabecular pigmentation, widened angle recess, and higher baseline intraocular pressure. Arch Ophthalmol. 2008;126:921–926. 38. Girkin CA, McGwin G Jr, Long C, et al. Glaucoma after ocular contusion: a cohort study of the United States Eye Injury Registry. J Glaucoma. 2005;14:470–473. 39. Campbell DG. Ghost cell glaucoma following trauma. Ophthalmology. 1981;88: 1151–1158. 40. Napier SM, Baker RS, Sanford DG, et al. Eye injuries in athletics and recreation. Surv Ophthalmol. 1996;41:229–244. 41. Clever VG. Home care of hyphemas. Ann Ophthalmol. 1982;14:25–27. 42. Wright KW, Sunalp M, Urrea P. Bed rest versus activity ad lib in the treatment of small hyphemas. Ann Ophthalmol. 1988;20:143–145. 43. Kraft SP, Christianson MD, Crawford JS, et al. Traumatic hyphema in children. Treatment with epsilon-aminocaproic acid. Ophthalmology. 1987;94:1232–1237. 44. Al-Shahwan S, Al-Torbak AA, Turkmani S, et al. Side-effect profile of brimonidine tartrate in children. Ophthalmology. 2005;112:2143. 45. Bedrossian RH. The management of traumatic hyphema. Ann Ophthalmol. 1974;6: 1016–1018. 1020-1011. 46. Yasuna E. Management of traumatic hyphema. Arch Ophthalmol. 1974;91:190–191. 47. Romano PE, Phillips PJ. Traumatic hyphema: a critical review of the scientifically catastrophic history of steroid treatment therefore; and A report of 24 additional cases with no rebleeding after treatment with the Yasuna systemic steroid, no touch PLUS protocol. Binocul Vis Strabismus Q. 2000;15:187–196. 48. Rynne MV, Romano PE. Systemic corticosteroids in the treatment of traumatic hyphema. J Pediatr Ophthalmol Strabismus. 1980;17:141–143. 49. Armaly MF. Effect of corticosteroids on intraocular pressure and fluid dynamics. I. The effect of dexamethasone in the normal eye. Arch Ophthalmol. 1963;70:482–491. 50. Goldmann H. Cortisone glaucoma. Arch Ophthalmol. 1962;68:621–626. www.internat-ophthalmology.com Pediatric Traumatic Hyphema ’ 57 51. Crouch ER Jr, Frenkel M. Aminocaproic acid in the treatment of traumatic hyphema. Am J Ophthalmol. 1976;81:355–360. 52. Kutner B, Fourman S, Brein K, et al. Aminocaproic acid reduces the risk of secondary hemorrhage in patients with traumatic hyphema. Arch Ophthalmol. 1987;105:206–208. 53. Teboul BK, Jacob JL, Barsoum-Homsy M, et al. Clinical evaluation of aminocaproic acid for managing traumatic hyphema in children. Ophthalmology. 1995;102:1646–1653. 54. Crouch ER Jr, Williams PB, Gray MK, et al. Topical aminocaproic acid in the treatment of traumatic hyphema. Arch Ophthalmol. 1997;115:1106–1112. 55. Rahmani B, Jahadi HR. Comparison of tranexamic acid and prednisolone in the treatment of traumatic hyphema. A randomized clinical trial. Ophthalmology. 1999; 106:375–379. 56. Sukumaran K. The role of tranexamic acid (Cyklokapron) in the treatment of traumatic hyphaema. Med J Malaysia. 1988;43:155–158. 57. Vangsted P, Nielsen PJ. Tranexamic acid and traumatic hyphaema. A prospective study. Acta Ophthalmol (Copenh). 1983;61:447–453. 58. Deans R, Noel LP, Clarke WN. Oral administration of tranexamic acid in the management of traumatic hyphema in children. Can J Ophthalmol. 1992;27:181–183. 59. Albiani DA, Hodge WG, Pan YI, et al. Tranexamic acid in the treatment of pediatric traumatic hyphema. Can J Ophthalmol. 2008;43:428–431. 60. Goldberg JL. Conjugated estrogens in the prevention of secondary hyphema after ocular trauma. Arch Ophthalmol. 1960;63:1001–1004. 61. Spaeth GL, Levy PM. Traumatic hyphema: its clinical characteristics and failure of estrogens to alter its course. A double-blind study. Am J Ophthalmol. 1966;62: 1098–1106. 62. Kim MH, Koo TH, Sah WJ, et al. Treatment of total hyphema with relatively low-dose tissue plasminogen activator. Ophthalmic Surg Lasers. 1998;29:762–766. 63. Nasrullah A, Kerr NC. Sickle cell trait as a risk factor for secondary hemorrhage in children with traumatic hyphema. Am J Ophthalmol. 1997;123:783–790. 64. Goldberg MF. The diagnosis and treatment of secondary glaucoma after hyphema in sickle cell patients. Am J Ophthalmol. 1979;87:43–49. 65. Wilker SC, Singh A, Ellis FJ. Recurrent bleeding following traumatic hyphema due to mild hemophilia B (Christmas disease). J Aapos. 2007;11:622–623. 66. Morsman CD, Holmes J. Traumatic hyphaema in a haemophiliac. Br J Ophthalmol. 1990;74:563. www.internat-ophthalmology.com