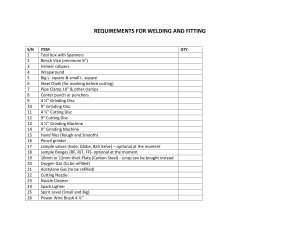
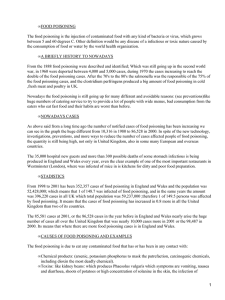
1040-5488/12/8902-0178/0 VOL. 89, NO. 2, PP. 178–182 OPTOMETRY AND VISION SCIENCE Copyright © 2012 American Academy of Optometry ORIGINAL ARTICLE Methanol Poisoning: Ocular and Neurological Manifestations Ranjana Sharma*, Sanjay Marasini†, Ananda Kumar Sharma*, Jeevan Kumar Shrestha‡, and Bhagvat Prasad Nepal‡ ABSTRACT Purpose. The purpose of this study was to examine the effectiveness of ethanol and high-dose intravenous steroid for preserving vision in acute methanol poisoning. Methods. Eight cases of acute methanol poisoning presented to the emergency department. Detailed physical examination including neurological assessment was performed. Detailed ocular examinations were performed including visually evoked potential and electroretinography in indicated cases. All patients had visual symptoms. Pupillary abnormality was observed in all. Edema of the optic disc and nerve fiber layer were common fundus findings. The majority of cases were treated with methylprednisolone intravenously. Ethanol was given intravenously in four cases who presented within 48 h. Hemodialysis was performed in two cases having neurological manifestations and metabolic acidosis. Sodium bicarbonate was given to four patients. Folinic acid and multivitamins were also given to all the patients based on neurological advice. Results. Most of the patients showed a good response to the treatment. In 87.5% of the cases, improvements in visual acuity of at least two lines were noted in follow-up visits. Conclusions. Early presentation with prompt treatment has a significant role in preserving and improving visual acuity. Ethanol and high-dose intravenous methylprednisolone can be an alternative treatment with better visual outcome where fomepizole is unavailable. (Optom Vis Sci 2012;89:178–182) Key Words: fomepizole, methanol poisoning, ocular toxicity, pupillary abnormality M ethyl alcohol is a colorless and odorless liquid, which is highly toxic. The pathological effects of methanol intoxication are attributed to the accumulation of the toxic metabolites formaldehyde and formic acid.1 They are toxic to the central nervous system, gastrointestinal tract, and the eyes causing metabolic acidosis and cellular dysfunction.2 After methanol intoxication, symptoms that have been described are blurred vision, double vision, photophobia, and changes in color perception.3 There may be constricted visual fields and occasionally a total loss of vision. Characteristic visual dysfunctions include pupillary dilation and loss of pupillary reflex.4,5 The ophthalmic diagnostic clues may include hyperemia of the optic disc, optic disc *MD † BOptom ‡ FRCS Department of Ophthalmology, Kathmandu University Hospital, Dhulikhel Hospital, Dhulikhel, Nepal (RS, SM, BPN), and BP Koirala Lions Center for Ophthalmic Studies, Institute of Medicine, Tribhuwan University, Maharajgunj, Nepal (AKS, JKS). edema, or disc pallor.6 The aim of this study was to examine the effectiveness of ethanol and high-dose intravenous steroid for preservation and restoration of visual acuity when fomipizole is not available as the treatment. MATERIALS AND METHODS The alcohol consumed by patients involved in this outbreak was manufactured illegally and transferred into mineral water bottles in the districts surrounding of Kathmandu. The alcohol was then sold in remote villages in Sindhupalchowk, Ramechhap, Dolakha, and Sindhuli districts where the outbreak occurred in July 2008. It claimed 31 lives. Eight of the victims presented to the emergency department of the hospital. Altered sensoria were observed in all cases during presentation at the hospital. Informed consent was taken for examination and publication of the report. The case series was studied prospectively and follow-up examinations were performed at the time of discharge, on seventh day after discharge, after 1 month, 3 months, and 1 year later. Optometry and Vision Science, Vol. 89, No. 2, February 2012 Methanol Poisoning: Ocular and Neurological Manifestations—Sharma et al. Detailed histories about the amount of alcohol intake, local brand name, onset of visual symptoms, progression of vision loss, and associated neurological and gastrointestinal symptoms were taken. The diagnosis of methanol poisoning was based on the history, clinical presentation, ocular evaluation, elevated anion and osmolar gaps, the presence of methanol in the blood, and the absence of other toxins in a toxicology screen. Detailed ocular evaluation consisted of measurement of the presenting visual acuity, assessment of the pupillary size and reaction, anterior segment evaluation, and fundus evaluation under full mydriasis with binocular indirect ophthalmoscopy. Extraocular motility was assessed in six cardinal positions of gaze. Visually evoked potential and electroretinography (ERG) were performed in selected cases with normal looking fundi and abnormal pupillary reactions. Non-enhanced computerized tomography (CT) scan of the brain was conducted in all patients, and it was repeated in some with neurological manifestations. Conventional brain magnetic resolution imaging with a 1.5-T Gyroscan Interna scanner was also performed during follow-up visits on patients who had had no improvement in vision. Seven patients were treated with pulse methylprednisolone 500 mg in 200 ml of ringer lactate administered intravenously over 2 h twice a day for 3 days followed by oral prednisolone 1 mg/kg for 11 days. One patient who presented on the seventh day after methanol consumption was treated with oral steroid 1 mg/kg for 10 days which was then tapered over 2 weeks. Ethanol was given intravenously in four patients who presented within 48 h. Hemodialysis was performed in two patients having additional neurological 179 manifestations and metabolic acidosis. Sodium bicarbonate was given to four patients having bicarbonate concentrations ⬍15 mEq/L. Folinic acid and multivitamins were added to the treatment of all the patients based on neurological consultation. Patients were discharged once they were neurologically stable. They were followed up regularly in the neuro-ophthalmology clinic. This special clinic is run jointly by a neuro-ophthalmologist and a neurologist. The follow-up examination consisted of visual acuity measurement, pupillary assessment, and detailed fundus examination. No undesirable side effects of the treatment were observed. RESULTS There were eight cases (seven male and one female). The mean age was 48.75 (range, 45 to 60 years). The patient characteristics on the day of presentation, delay from methanol ingestion to onset of symptoms, systemic manifestations, assessments performed, and the treatment given are presented in Table 1. Six patients gave a history of intake of local brand “sofi” found to be contaminated with methanol; however, two cases could not name the brand consumed. The patients presented with a range of vision from severe impairment to complete blindness. The degree of visual impairment at presentation is shown in Table 2. Bilateral ocular involvement was noted in 67% of the cases. In all the cases, the pupil was involved. Pupil diameter was 3 to 4 mm with a sluggish reaction in 12 eyes (75%). Five eyes (31.25%) had relative afferent pupillary defect. Four eyes (25%) had pupil sizes of 5 to 6 mm, and pupils were fixed to both the direct and consensual TABLE 1. Summary of the investigation and the treatment Time of presentation Onset of symptoms (within) Other manifestations Case no. Age/ sex 1 45/M Second day 24 h Gastrointestinal ⫹ neurological 2 53/M Second day 24 h Gastrointestinal ⫹ neurological 3 45/M Second day 24 h Gastrointestinal ⫹ neurological 4 46/M Second day 24–48 h Gastrointestinal 5 47/M Third day 24–48 h Gastrointestinal ⫹ neurological 6 60/F 24–48 h Gastrointestinal 7 48/M Fourth day 24–48 h Gastrointestinal 8 46/M Seventh day Third day After 48 h None Treatment given IV Methylprednisolone ⫹ oral prednisolone ⫹ IV ethanol ⫹ hemodialysis ⫹ folinic acid and multivitamins IV Methylprednisolone ⫹ oral prednisolone ⫹ IV ethanol ⫹ hemodialysis ⫹ folinic acid and multivitamins IV Methylprednisolone ⫹ oral prednisolone ⫹ IV ethanol ⫹ sodium bicarbonate ⫹ folinic acid and multivitamins IV Methylprednisolone ⫹ oral prednisolone ⫹ IV ethanol ⫹ sodium bicarbonate folinic acid and multivitamins IV Methylprednisolone ⫹ oral prednisolone ⫹ sodium bicarbonate ⫹ folinic acid and multivitamins IV Methylprednisolone ⫹ oral prednisolone ⫹ folinic acid and multivitamins IV Methylprednisolone ⫹ oral prednisolone ⫹ sodium bicarbonate ⫹ folinic acid and multivitamins Oral prednisolone ⫹ folinic acid and multivitamins VEP, visually evoked potential. Optometry and Vision Science, Vol. 89, No. 2, February 2012 Other special tests done CT scan ⫹ arterial pH, VEP, ERG CT scan ⫹ arterial pH CT scan ⫹ arterial pH, VEP, ERG CT scan (abnormal findings) ⫹ arterial pH CT scan ⫹ arterial pH, VEP, ERG CT scan ⫹ arterial pH CT scan (abnormal findings) ⫹ MRI CT scan 180 Methanol Poisoning: Ocular and Neurological Manifestations—Sharma et al. TABLE 2. Summary of the ocular findings PVA VA at 1 yr Pupil OD Fundus S. N. OD OS OD OS OS 1 NLP ⬍20/200 3/60 6/24 3 mma 3 mm 2 NLP NLP LFU LFU 4 mma,b 4 mma,b 3 4 5 6 20/400 NLP HM NLP HM 20/400 ⬍20/200 NLP 6/24 LFU 6/36 HM 6/60 LFU 6/60 HM 3 mm 4 mma,b 3 mma 3 mma,b Mid dilateda,b 4 mma 3 mma 3 mma 7 8 NLP LP NLP LP LFU LFU LFU LFU 5 mm fixed 3 mma 5 mm fixed 3 mma OD Hyperemic disc edema Hyperemic disc edema Normal Disc edema Normal Hyperemic disc edema Disc edema Hyperemic disc edema OS with NFL Normal with NFL Hyperemic disc with NFL edema Normal Normal Normal Hyperemic disc with NFL edema Disc edema Disc edema with NFL with NFL a Sluggish pupillary reaction. Relative afferent pupillary defect (RAPD). VA, visual acuity; PVA, presenting visual acuity; NPL, no light perception; LP, light perception; NFL, nerve fibre layer; LFU, lost to follow-up. b light reflexes. Fundoscopy revealed normal appearance in six eyes (37.5%), hyperemic optic disc with nerve fiber layer edema in six eyes (37.5%), and disc edema in four eyes (25%). Three eyes with disc edema progressed to optic atrophy after the 1-month follow-up. Visually evoked potentials were recorded in three patients of which two had abnormal b-wave amplitudes and increased peak III latencies whereas results were inconclusive in one patient. Similarly, scotopic ERGs were recorded in three cases. The scotopic ERG was subnormal with diminished a- and b-waves. Six patients underwent arterial blood pH testing of whom four had metabolic acidosis at presentation. Arterial blood pH was not assessed in two cases who presented after 4 days with only ocular complaints. All patients showed the presence of methanol in their blood. The blood methanol level was ⬎40 mg/dl in two cases. Six patients had normal CT scans. One patient showed a B/L hypodense area in the lenticular nucleus and another patient had dilated ventricles. Magnetic resolution imaging was performed in one patient at 1-month follow-up. The imaging was normal. Gastrointestinal symptoms such as nausea, abdominal pain, and vomiting were present in seven patients. However, neurological manifestations, which included headache, ataxia, and drowsiness, were seen in only four cases. Four eyes (25%) were lost to follow-up 1 week after discharge. Six eyes (38%) were lost to follow-up at 1 month. Only eight eyes (50%) were followed up for 1 year. At the time of discharge, a total of 13 eyes improved (81.25%) among which five eyes improved from no light perception to light perception and hand movement (HM). Eyes with light perception and HM also improved to HM and 20/400, respectively. At 1-week follow-up, there was a significant improvement in visual acuity. Eyes with HM and 20/400 further improved to 20/200. Patients with visual acuities of 20/200 and 20/400 improved to 20/120 and 20/80, respectively. However, vision in two eyes deteriorated at 1 month, and one remained unchanged. Excluding those lost to follow-up, 87.5% of patients showed at least two lines of improvement of visual acuity at 1-year follow-up. DISCUSSION Even small amounts of ingested methanol can cause severe visual dysfunction and death through acute destruction of parts of the central nervous system or may lead to permanent neurological dysfunction and irreversible blindness. Without treatment, ingestion of 30 ml (0.5 mg/kg body weight) of pure methanol usually results in death and as little as 4 ml can result in blindness.1 As methanol metabolism proceeds, the serum bicarbonate falls concomitantly with a rise in the anion gap and a fall in the serum osmolality. Formic acid, the primary toxin, accounts for the majority of anion gap metabolic acidosis and ocular toxicity.2 The ocular changes are reported to correlate with the degree of acidosis. Retinal damage is believed to be due to the inhibition of retinal hexokinase by formaldehyde, an intermediate metabolite of methanol.7 After entering into the retinal circulation, formic acid inhibits cytochrome oxidase in the retina. It then impairs mitochondrial function resulting in decreased ATP production and finally leads to disruption of axoplasnic flow and swelling of axons in the optic disc and subsequently retinal nerve fiber layer edema. These events cause marked visual impairment.8 The diagnosis of methanol poisoning is based on a positive history of methanol ingestion or a ingestion of a methanolcontaining product. The early non-specific symptoms of methanol consumption are nausea, headache, abdominal discomfort, generalized weakness, and deterioration of the level of consciousness. This picture can then proceed to blindness, coma, and death because of profound metabolic acidosis.9 The serum methanol concentration, anion gap metabolic acidosis, and an osmolal gap confirm the diagnosis. The electrophysiological tests support the diagnosis. In our case series, we measured the scotopic ERG and found that a- and b-waves were diminished, as was reported by Optometry and Vision Science, Vol. 89, No. 2, February 2012 Methanol Poisoning: Ocular and Neurological Manifestations—Sharma et al. McKellar et al.10 It has been emphasized that pupillary status provides the best prognostic information for both morbidity and mortality.11 In our patients, pupillary involvement was 100% of whom 87.5% had some amount of improvement in vision over a time period of 1 year. Fixed, dilated pupils, and optic atrophy, with or without excavation, are the most common findings reported.12 We observed sluggish to fixed pupillary reactions. Different studies have reported varying fundus changes. Patel and Narang12 report neuroretinitis with peripapillary retinal edema in 34% of cases. We found hyperemic optic discs with nerve fiber layer edema in six eyes (37.5%) and disc edema in four eyes (25%) at presentation. Cases with disc edema and fixed pupillary reaction progressed to disc pallor and narrowed vessels within 4 weeks. Roe13 observed that the fundus is usually normal with occasional blurring of the disc margins and vessel tortuosity. He reported that the disc pallor and narrowing of the blood vessels start within 6 to 12 weeks and pallor proceeds to narrowing of the vessels. Of the four cases (50%) with neurological symptoms at presentation, only one had ataxia at 1-month follow-up. One study noted that severe poisoning causes necrosis of the basal ganglion, particularly the putamen.14 We observed one patient with a hypodense area in the lenticular nucleus on the CT scan. The essential therapy of methanol poisoning is adequate alkalinization and ethanol administration. Ethanol competes with methanol for the enzyme alcohol dehydrogenase (ADH) in the liver thereby inhibiting the accumulation of toxic metabolites of methanol in the body. The three primary goals of therapy are treatment of metabolic acidosis, inhibition of the methanol metabolism, and enhanced elimination of the unmetabolized compound and existing toxic metabolites.15 Currently recommended management aims to delay methanol metabolism by using intravenous ethanol infusion, gastric lavage, ADH enzyme blockade by means of fomepizole, hemodialysis, alkalinization, and use of cofactors such as folic acid.9,16,17 Folic acid enhances the metabolism of formic acid.18 Ethanol and fomepizole are specific antidotes. These agents block the conversion of methanol to formic acid. Bicarbonate and hemodialysis are used to correct the systemic acidosis. Fomepizole (4-methylpyrazole) has ⬃500 to 1000 times greater affinity for ADH than ethanol and can completely inhibit ADH at a much lower serum concentration.19 Intravenous high doses of steroids are reported to benefit the visual status provided that the interval between the consumption of methanol and start of treatment is short.20,21 We treated most of the cases with intravenous high-dose steroids and attained good results (87.5% showed improvement) that depended on the severity of the acidosis, pupillary involvement, and stage at presentation. We could not treat our patients with fomepizole because it was unavailable. Fifty percent of our cases presented after more than 24 h. This may be attributable to the lack of awareness about the potentially dangerous effect of the alcohol ingested. Patients who presented within 48 h and were treated with ethanol and steroids had a better outcome, an observation also noted by Hassanian-Moghaddam et al.22 Our cases who presented later had severe metabolic acidosis, had fixed and dilated pupils, who required hemodialysis and bicar- 181 bonate, and those with severe visual impairment did not have as good an outcome. Fifty percent of our cases were lost to follow-up within the 1-year study duration. Among those who followed up, 87.5% had some visual acuity improvement. This reflects the gradual improvement of visual acuity as observed by other authors.23 We could not trace those cases that were lost to follow-up because they were from remote districts. Seven of the eyes (43.75%) had visual acuity of ⬍20/400. CONCLUSIONS All patients in our case series presented with visual symptoms. Pupillary abnormality was observed in all cases. Edema of the optic disc and nerve fiber layer were common fundus findings. Most patients showed an improvement of vision with the use of methylprednisolone. Early presentation with prompt treatment has a significant role in preservation and improvement of visual acuity in acute methanol poisoning. Where fomepizole is unavailable, ethanol, which serves as an antidote, and high-dose intravenous methyprednisolone can be used as alternative treatments that improve visual outcome. ACKNOWLEDGMENTS The authors have received no outside financial support and declare no conflict of interest with any of the products or devices mentioned in the manuscript. The paper has been presented orally at the “26th Asia Pacific Academy of Ophthalmology Congress” at Sydney, Australia on 20 –24th March, 2011. Received March 3, 2011; accepted September 28, 2011. REFERENCES 1. Agency for Toxic Substances and Disease Registry (ATSDR), U.S. Department for Health and Human Services. Methanol Toxicity. Am Fam Physician 1993;47:163–71. 2. Onder F, Ilker S, Kansu T, Tatar T, Kural G. Acute blindness and putaminal necrosis in methanol intoxication. Int Ophthalmol 1998; 22:81–4. 3. Hovda KE, Hunderi OH, Tafjord AB, Dunlop O, Rudberg N, Jacobsen D. Methanol outbreak in Norway 2002–2004: epidemiology, clinical features and prognostic signs. J Intern Med 2005;258: 181–90. 4. Bennett IL, Jr., Cary FH, Mitchell GL, Jr., Cooper MN. Acute methyl alcohol poisoning: a review based on experiences in an outbreak of 323 cases. Medicine (Baltimore) 1953;32:431–63. 5. Erlanson P, Fritz H, Hagstam KE, Liljenberg B, Tryding N, Voigt G. Severe methanol intoxication. Acta Med Scand 1965;177:393–408. 6. Jacobsen D, McMartin KE. Antidotes for methanol and ethylene glycol poisoning. J Toxicol Clin Toxicol 1997;35:127–43. 7. Martin-Amat G, McMartin KE, Hayreh SS, Hayreh MS, Tephly TR. Methanol poisoning: ocular toxicity produced by formate. Toxicol Appl Pharmacol 1978;45:201–8. 8. Kraut JA, Kurtz I. Toxic alcohol ingestions: clinical features, diagnosis, and management. Clin J Am Soc Nephrol 2008;3:208–25. 9. Lin ES, Buckley T, Li E, Lai KN, Oh TE. Case reports: a case of severe methanol intoxication. J Hong Kong Med Assoc 1989;41:273–4. 10. McKellar MJ, Hidajat RR, Elder MJ. Acute ocular methanol toxicity: clinical and electrophysiological features. Aust N Z J Ophthalmol 1997;25:225–30. Optometry and Vision Science, Vol. 89, No. 2, February 2012 182 Methanol Poisoning: Ocular and Neurological Manifestations—Sharma et al. 11. Sullivan-Mee M, Solis K. Methanol-induced vision loss. J Am Optom Assoc 1998;69:57–65. 12. Patel JK, Narang SK. Eye changes in methyl alcohol poisoning. J All India Ophthalmol Soc 1970;18:125–7. 13. Roe O. Clinical investigations of methyl alcohol poisoning. Acta Med Scand 1943;113:558–608. 14. Blanco M, Casado R, Vazquez F, Pumar JM. CT and MR imaging findings in methanol intoxication. AJNR Am J Neuroradiol 2006; 27:452–4. 15. Ravichandran R, Dudani RA, Almeida AF, Chawla KP, Acharya VN. Methyl alcohol poisoning. (Experience of an outbreak in Bombay). J Postgrad Med 1984;30:69–74. 16. Brent J, McMartin K, Phillips S, Aaron C, Kulig K. Fomepizole for the treatment of methanol poisoning. N Engl J Med 2001;344: 424–9. 17. Gonda A, Gault H, Churchill D, Hollomby D. Hemodialysis for methanol intoxication. Am J Med 1978;64:749–58. 18. Mégarbane B, Borron SW, Baud FJ. Current recommendations for treatment of severe toxic alcohol poisonings. Intensive Care Med 2005;31:189–95. 19. Barceloux DG, Bond GR, Krenzelok EP, Cooper H, Vale JA. Amer- 20. 21. 22. 23. ican Academy of Clinical Toxicology practice guidelines on the treatment of methanol poisoning. J Toxicol Clin Toxicol 2002;40: 415–46. Sodhi PK, Goyal JL, Mehta DK. Methyl alcohol induced optic neuropathy treated with intravenous high dose steroids. Int J Clin Prac 2001;9:599–602. Shukla M, Shikoh I, Saleem A. Intravenous methylprednisolone could salvage vision in methyl alcohol poisoning. Indian J Ophthalmol 2006;54:68–9. Hassanian-Moghaddam H, Pajoumand A, Dadgar SM, Shadnia S. Prognostic factors in methanol poisoning. Hum Exp Toxicol 2007; 26:583–6. Scrimgeour EM, Dethlefs RF, Kevau I. Delayed recovery of vision after blindness caused by methanol poisoning. Med J Aust 1982;2: 481–3. Optometry and Vision Science, Vol. 89, No. 2, February 2012 Ranjana Sharma Kathmandu University Hospital Dhulikhel Hospital Dhulikhel, Nepal e-mail: [email protected]