Physician Adoption of New Technologies: A Qualitative Study
Anuncio

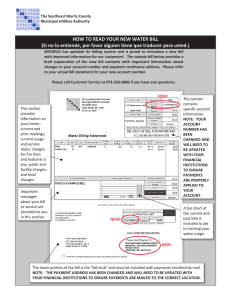
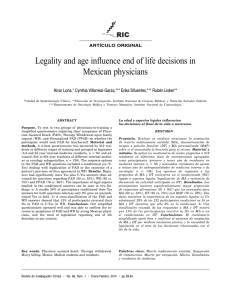
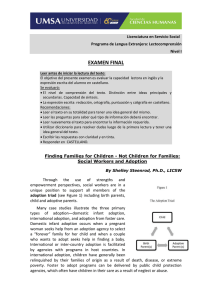
VALUE IN HEALTH 21 (2018) 1069–1076 Available online at www.sciencedirect.com journal homepage: www.elsevier.com/locate/jval Comparative-Effectiveness Research/HTA Physicians’ Decision Making on Adoption of New Technologies and Role of Coverage with Evidence Development: A Qualitative Study Susanne Felgner, MSc*, Patricia Ex, Dr. P.H., Cornelia Henschke, Dr. rer. oec. Department of Health Care Management, Technische Universität Berlin, Berlin, Germany AB STR A CT Objectives: To foster value-based pricing and coverage with evidence development in Germany, certain new diagnostic and treatment methods have been subject to a benefit assessment since 2016 to determine their reimbursement. Although this is a paradigm shift, the German approach is limited to some few specific technologies for which reimbursement is requested. As physicians encounter this regulatory instrument, the aim of the study was to understand physicians’ decision making regarding the adoption of new medical technologies and to identify their perspectives on the evidence base and financing with additional reimbursement systems. Methods: From April to August 2017, semistructured interviews with chief and senior physicians of vascular surgery and cardiology in inpatient care in Germany were conducted (N ¼ 23). The interviews were carried out by one researcher in one-to-one appointments or via telephone. Data were analyzed inductively to identify factors and generate thematic categories using qualitative content analysis. Results: We identified 52 factors in eight categories influencing physicians’ adoption of new technologies. The evidence base for new technologies was criticized (e.g., lack of available studies). Physicians’ knowledge of the regulation of market approval and innovation payments varied. They recommended the utilization of new technologies in certain specialist centers and the facilitation of observational studies. Conclusions: Physicians saw the need for the new approach and supported its aim. However, its design and implementation appeared to be questionable from their medical perspective. The provision of summarized information on the benefit of technologies might be a possibility to assist physicians’ decision making. Keywords: adoption of technologies, coverage with evidence development, evidence, innovation, inpatient care, physician. Introduction and decide, sometimes within teams, whether to adopt a new technology or to use established alternatives. A variety of studies have investigated factors influencing physicians’ decision making. Several quantitative studies have evaluated the influence of hospital characteristics [6,7], external factors (e.g., financing systems and reimbursement) [8,9], and technology-related factors of particular technologies [10,11]. Qualitative studies have highlighted that adoption decisions are based on financial and social pressures, while evidence is often limited [12,13]. Different dimensions to categorize factors influencing decision making have been developed, broadly differentiating among adopterspecific, technology-related, and external factors [14–18]. However, most of these studies used previously developed categories and fill the existing ones, which may undermine relevant aspects that do not fit into the model used. In particular, the trade-off between time of adoption and evidence base is highly relevant for physicians with regard to When new medical technologies enter the market, their time of adoption is a key point in patient care, as evidence and experience regarding their utilization often differ in their extent [1]. With the aim of maximizing patient benefit and reducing risks [2], many new technologies can lead to better outcomes in patients’ treatment and diagnosis; however, there might be uncertainty regarding their effectiveness and risks because at the time of market approval only little or no evidence may be available [3,4]. Thus, the adoption and utilization of new technologies is necessary to gather knowledge and real-world evidence. This is the case for medical devices, especially in the European Union, where requirements to obtain market approval are generally lower than, for instance, in the United States [5]. Regarding new technologies used in inpatient care, the primary adopters are physicians, as they assess treatment options Copyright & 2018, ISPOR–The Professional Society for Health Economics and Outcomes Research. Published by Elsevier Inc. The study was realized by using a 1st shared authorship of Susanne Felgner and Patricia Ex. * Address correspondence to: Susanne Felgner, Department of Health Care Management, Technische Universität Berlin, Straße des 17. Juni 135, H80, 10623 Berlin, Germany. E-mail: [email protected] 1098-3015$36.00 – see front matter Copyright & 2018, ISPOR–The Professional Society for Health Economics and Outcomes Research. Published by Elsevier Inc. https://doi.org/10.1016/j.jval.2018.03.006 1070 VALUE IN HEALTH 21 (2018) 1069–1076 technology adoption decisions but also for health care systems. In light of limited resources and high health expenditures, a large share of which is spent on technologies, health care systems and payers are under pressure to control their expenditures [19]. Many countries therefore have introduced schemes to reimburse only those new technologies that have shown benefit. The main idea is to link the coverage decision and price setting for a technology to its value [4]. Owing to the often low level of available evidence on the effectiveness of new technologies, the approach of coverage with evidence development (CED) has been developed, in which a technology is covered by health insurers while further post-market evidence is obligatorily generated. This approach was originally implemented for Medicare in the United States [20] and has been adapted in France [21], Germany [22], Sweden, and the Netherlands [23], among other countries. Although these CED approaches exhibit common elements (e.g., clear legal foundation and preference for high-quality study designs), their specific features depend on the underlying health system in each country. Differences exist with regard to the types of technologies being assessed (i.e., drugs, procedures, or medical devices) [22]. Compared to those in other countries, the German approach, introduced in 2016, is based on an early benefit assessment (§137h in combination with §137e Social Code Book V [SGB V]) of a particular group of medical devices. Furthermore, the approach has been linked to the concept of inpatient innovation payments (see Methods for detailed information), and is a further step in a paradigm shift for the medical device industry, patient care, and inpatient physicians adopting these technologies. As no international literature is available on the German health policy reform and its relevance for clinical practice, we aimed to fill this gap. Accordingly, the term “new technologies” in this article refers to medical devices as well as diagnostic and treatment methods, but excludes pharmaceuticals. The aim of this study was, first, to describe the German CED scheme to gain a more in-depth insight into the decision making of physicians adopting new technologies, and, second, to explore physicians’ perspectives on the trade-off between evidence base and reimbursement of new technologies. Our research has been led by two research questions: I. How do physicians describe their decision criteria for adopting a new technology in patient care? II. What experiences and constructive remarks do physicians have regarding the evidence base and financing of new technologies? Methods Brief Overview of 2016 German CED Reform The aim of this study and, consequently, the development of the interview questionnaire focused on the German health policy reform of the CED; thus, the approach will be introduced in this section, clarifying why the reform especially affects physicians (e.g., responsibility to provide further information on a medical device or its exclusion from reimbursement). Before 2016, approved new technologies could generally be used in German inpatient care without a prior external assessment (§137c SGB V). In 2012, the CED was first introduced for diagnostic and therapeutic methods (§137e SGB V), for which the German Federal Joint Committee (G-BA) had passed a directive for the conduction of clinical trials to gather additional data on effectiveness and safety [22]. The reform of 2016 focuses on new diagnostic and therapeutic methods whose technical application is based essentially on a medical device of high-risk class (i.e., “high-risk medical device”). According to the SGB V, “high-risk medical devices” are (1) medical devices of risk class IIb or III in line with the Directive 93/42/EEC or active implantable medical devices in line with the Directive 90/385/EEC,1 whose (2) application possesses a highly invasive character. “New diagnostic and therapeutic methods” are thereby defined as medical procedures using a new theoretical and scientific concept. The term “method” involves procedures in terms of a “physician-led treatment concept” characterized by a certain degree of complexity. These are thus different from other medical devices, such as medical instruments or appliances, that are used for one-step procedures [24]. The underlying new theoretical and scientific concept of the method has to differentiate it from others [24]; that is, according to §137h SGB V, the new method’s mode of action or its field of application needs to differ substantially from systematic approaches already used in inpatient care. An example of a method that was considered for assessment so far is coronary lithoplasty for the treatment of coronary heart disease (CHD). This is different from, for example, rotablation, which is utilized in the treatment of CHD using another mode of action for coronary plaque ablation [25]. Figure 1 provides a schematic overview of the new CED approach [26]. The starting point of an early benefit assessment is the hospitals’ first application on innovation payments for new technologies, so-called New Diagnostic and Treatment Methods. Innovation payments are separate from the system of diagnosisrelated groups (DRGs) in that they involve additional funding (i.e., are paid on a fee-for-service basis) and are negotiated locally [27,28]. The benefit assessment of a method leads to one of the following results: (1) sufficient proof of benefit, (2) no sufficient proof but potential of benefit, or (3) no sufficient proof of benefit. According to the Institute for Quality and Efficiency in Health Care (IQWiG), “benefit” is defined as valid positive effects of methods concerning patient-related end points (e.g., mortality, morbidity, or patient’s quality of life) compared to placebo or comparator interventions [29]. Study Design and Participants As the complexity of adoption processes is well known [17], we applied qualitative content analysis to adequately examine this organizational phenomenon [30]. This study was approved by the ethical committee of the Technische Universität Berlin via a fast track procedure. We collected data using in-depth semistructured interviews, enabling us to ask additional context-driven questions [31]. The questionnaire covered the following subject areas: (I) factors influencing physicians’ decisions to adopt new technologies, (IIa) physicians’ assessment of the evidence base, and (IIb) physicians’ assessment of the concept of innovation payments in clinical practice. With the aim of testing the comprehensibility and appropriateness of the questions, a pilot test was conducted with two physicians [32]. The interviews of the pilot study were not included in the analysis. To identify medical disciplines where a variety of new and higher priced technologies compared to standard technologies are used, the lists of requested innovation payments in Germany (2011–2015) were screened. As a result, we conducted all interviews in the disciplines of vascular surgery and cardiology or other designated areas, also carrying out interventions in those fields, for example, internal medicine. We identified all relevant inpatient hospitals in the city of Berlin and the federal state of Brandenburg, limiting the regional area for the following reasons: (1) keeping the area of investigation at a small size permits having all physicians interviewed by the same researcher, preventing bias resulting from different researchers [33]; (2) Berlin, as a populous city with a high hospital density, and Brandenburg, consisting of suburban and rural regions, offer a variety in hospital sizes and 1 As of May 25, 2017 the new Medical Device Regulation (MDR) came into force. Regulation (EU) 2017/745 will replace the directives concerning medical devices and active implantable devices after a transitional period of 3 years. 1071 VALUE IN HEALTH 21 (2018) 1069–1076 Deadline 31 October 2 weeks 4 weeks 12 weeks 1. Evidence provides sufficient proof of benefit G-BA All requirements for benefit assessment need to be fulfilled: Hospital request on innovation payments regarding the new method¹ to the InEK and transfer of information² to the G-BA. Public call for • Innovation payment is requested for the first time. • Method is largely based on the utilisation of a ‘high-risk MD‘ Risk class IIb or risk class III or active implantable and highly invasive character. Yes • hospitals intending to use the method and No • manufacturers Legend: Decision of the G-BA Optional involvement of the IQWiG Request/ decision Information ¹ first-time request of ‘high-risk MD‘ ² on the best available scientific knowledge and use Assessment of the method’s benefit, harm and potential. to deliver further information² on MD. Method is authorised for utilisation. • Agreement on innovation payments within 12 weeks. • Quality requirements necessary? 2. Evidence does not provide sufficient proof of benefit, but shows potential • Decision on coverage with evidence development (§137e Social Code Book V). • Hospitals intending to use the method are required to participate in the study. IQWiG • and has a new theoretical and scientific concept. Return to standard procedure of innovation payments: negotiate payment with sickness funds if InEK determines that it is not yet covered by DRGs (Status 1). G-BA • Notification of the InEK until 31 January which methods qualify for innovation payments. 3. Evidence does not provide sufficient proof of benefit • Method is excluded from the benefit basket. Acronyms: DRG – Diagnosis Related Group G-BA – Federal Joint Committee InEK – Institute for the Hospital Remuneration System IQWiG – Institute for Quality and Efficiency in Health Care MD – Medical device Fig. 1 – Benefit assessment of methods with ‘high-risk medical devices’ in German inpatient care [26]; IQWiG, Institute for Quality and Efficiency in Health Care; MD, medical device. provider types [34,35]. The recruitment process took place from March to July 2017, and 170 physicians were contacted. The overall response rate was about 20% (N ¼ 33). However, 10 physicians declined the invitation because of lack of time or interest. The semistructured interviews were conducted in one-to-one appointments or via telephone from April to August 2017 and were audiotaped. After the 23 interviews were conducted, no fundamentally new information or arguments emerged. This indicated that the point of saturation had been reached [36]; thus, no further physicians were recruited. Data Editing and Analysis The recordings were transcribed verbatim by an external office and the transcripts were anonymized by two researchers. With the aim to prevent information processing bias and ensure a systematic analysis of qualitative data, we used the analytical software tool Atlas.ti (version 8.0) for coding [37]. All relevant text passages were coded separately by two researchers who directly derived code titles from the text data [38]. Two rounds of analysis were conducted. A first set of codes was developed based on a discussion with the option of adding or amending codes for further analysis. To harmonize the analysis, the final results were compared after the second round to reach consensus [39]. In case of disagreement, a neutral researcher was consulted and the codes were discussed. To answer the first research question, all codes representing factors influencing physicians’ decision making were pooled in thematic categories using the bottom-up-approach [40]. To answer the second research question, codes were systematically ordered. Results The data set consisted of 23 in-depth semistructured interviews with chief and senior physicians of vascular surgery and cardiology in inpatient care that lasted between 11 and 33 minutes. The interviewed physicians had practiced for an average of 24.7 years and 8.6 years in their current position. Their departments had a mean of 50.5 beds. Table 1 provides an overview of physicians’ characteristics, departments, and hospitals. Factors Influencing Physicians’ Decisions to Adopt New Technologies In the interviews, we identified a total of 52 individual factors that physicians described as influencing their decision to adopt a new technology. We grouped these influencing factors into eight thematic categories: 1) technology, 2) evidence base, 3) state of medical care, 4) manufacturer, 5) regulation, 6) hospital (including its institutional characteristics and strategy), 7) individual, and 8) patient. Figure 2 displays these categories including the influencing factors. Technology-related factors included the handling of a medical device by physicians, its durability and extent of improvement, and whether it reduced the invasiveness of a treatment. Owing to the diversity of technologies, the comparison of a single characteristic was not possible, forcing physicians to make an overall assessment considering a variety of aspects. Physicians also assessed the evidence base when deciding whether or not to adopt a technology. They were aware of a limited evidence base for medical devices after their market authorization, in particular in the European Union. However, physicians viewed this as an opportunity to carefully adopt a technology in a hospital setting. They also reported that this might nevertheless lead to an excessive proliferation of new technologies. Physicians criticized that available studies were often based on a very small patient cohort and were biased by manufacturer interests. Furthermore, physicians’ decision to use new technologies was influenced by the state of medical care. Interviewees assessed the level of care in their discipline as excellent with regard to the quality and availability of options. Thus, they set high standards for new technologies to compete against established methods. On the contrary, if few or no alternatives existed for an indication, such as rare diseases, physicians were willing to utilize certain new technologies despite lacking evidence. Nonetheless, overall, they mentioned guidelines as an important point of reference. Manufacturer-related aspects were identified as a further factor influencing physicians’ decisions to adopt new technologies. They described the influence of manufacturers’ sales activities, ranging from no interaction to using interactions as basically the only source of information, and criticized the focus on marketing activities. Furthermore, physicians considered the service provided by manufacturers in their decision making. Another factor mentioned was 1072 VALUE IN HEALTH 21 (2018) 1069–1076 Table 1 – Characteristics of 23 interviewed physicians (n=21 hospitals). Variable Physician level Position Years in practice Years in position Sex Department level Medical discipline Number of beds in department Patients’ financial situation* Hospital level Number of hospitals† From which University hospitals‡ Specialist centers‡ Specification N % Chief physician Senior physician ≤20 21–30 430 ≤5 6–10 410 Not specified Female Male Cardiology Vascular surgery ≤30 31–60 460 Not specified Rather poor Average Well off — 15 8 7 11 5 10 4 8 1 0 23 13 10 6 8 8 1 6 13 4 21 65 35 30 48 22 43 17 35 4 0 100 57 43 26 35 35 4 26 57 17 100 1 2 5 10 — — * Description of patients by physicians. † There were two physicians interviewed from the same hospital but different departments. ‡ One physician was interviewed from each of the institutions. the manufacturer price and cost–benefit ratio, that is, the manufacturer’s pricing strategy for a technology in relation to the expected benefits. They observed that prices decreased after the initial market launch, and some reported waiting until prices declined. In the context of regulation, relationships between different factors of adoption played a significant role: reimbursement decisions and price developments were relevant in physicians’ decisions to adopt new technologies. Some physicians mentioned the possibility of using a technology even if they had to cross-finance it from other DRGs. Technology Durability, Extent of improvement, Handling, Invasiveness, Overall assessment, Product generations, Product type State of medical care Guidelines, Pre-/ post care, Status quo, Treatment alternatives Regulation Liability, Possibility of reimbursement, Reimbursement requests at health insurance, Utilization without reimbursement Regarding hospital-related factors influencing the adoption decision of new technologies, physicians distinguished between characteristics of the institution, such as size and type of provider, and strategic decision making of hospitals. Interviewed physicians of non-university hospitals mentioned that university hospitals and specialist centers might have more possibilities of refinancing and thus should adopt new technologies first. They also reported not having sufficient patient numbers in a certain indication to utilize new technologies. Strategic aspects of hospitals included internal processes regarding central purchasing, logistical efforts, and coor- Evidence base Benefit and harm, Biased data, Plausibility, Quality of data, Study requirements Physicians’ decision Patient Expectations, Medical compatibility, Overall health and age Hospital: Institutional aspects Experienced staff, General vs. specialist care, Hospital size, Number of patients in indication, Provider, Structural conditions, University status Strategic aspects Central purchasing, Debate with CEO/ controlling, Division of locations, Freedom of choice, Hospital competition, Increase patient numbers, Instructions of supervisor, Logistical efforts, Pressure to be the first, Product portfolio, Reputation Manufacturer Market mechanisms, Price, Sales activities, Services Individual Familiarity with other technologies, Medical experiences, Medical school of thought, Peer group, Personality and interest, Product type, Research and career Note: Size and order of circles as of factors and determinants do not imply a weighting. Fig. 2 – Factors influencing technologies adoption decision of physicians. 1073 VALUE IN HEALTH 21 (2018) 1069–1076 Table 2 – Physicians’ statements on factors influencing technologies’ adoption decision (selection of factors and statements). Category Physician decision Factor Evidence base Quality of data Hospital Structural conditions (institutional aspects) Individual Increasing patient numbers (strategic aspects) Personality and interest Manufacturer Price Patient Overall health and age Regulation Possibility of reimbursement State of medical care Treatment alternatives Technology Handling Statement “The experience teaches that many medical devices in the first generation obviously sound great, include a basic innovation, but the benefit of this new system is eaten up, not only by the exorbitant costs, but also by complications, which then question the benefit again.” (no. 2) “…the larger the hospital, the more responsive the hospital is with regard to new technologies. However, there are hospitals of public ownership exhibiting a dormant status. Not that much happens there…” (no. 14) “…With this product, we will acquire new patients and improve the physicians’ work. This is of course a good argument…” (no. 17) “…Well, a positive consequence for me is that I receive more patients and more interesting patients. Because I have a service mission for about 90 percent, these are the basic care treatments, I always call it the ‘breadand-butter-business’. But 10 percent are issues that are interesting, they are fun, they bring color into life. And I want more of these…” (no. 18) “…If an existing technology has the same therapeutic effect and the new technology is considerably more expensive, then you have to weigh in how far the new technology really has an added value justifying the price…” (no. 23) “…If I can spare someone a surgery with a certain new device, then this is something I would not do with a 30-year old person, but I would do it with a really old patient, whose life expectancy is by far more limited and whose risks for surgery are much higher…” (no. 3) “…DRGs are a quasi-downward spiral as they are constantly revised. There is only one direction, namely the downward direction. This makes it more difficult for all involved actors […] leading to enormous cost pressures for hospitals. […] This is far away from medical treatment, medical ethos, and patient care. It leads to the fact that the provision of patient treatment is only a secondary product of earning money…” (no. 9) “Well, in the field of cardiology, treatment alternatives that we can use these days are good, in any way. And we do not have the need, from my perspective, to urgently take a risk because standard therapy would not be satisfying. There is no thought about that at any point.” (no. 5) “…when the handling is impractical. That is one factor, when you would not want to use the product…” (no. 6) Note: Number of interviewee is added at the end of each quotation in brackets. dination with administrative colleagues. In addition, strategic hospital decisions such as increasing patient numbers and quality in patient care played a role in physicians’ decisions to adopt new technologies, as well as reputation and patient satisfaction. Physicians also mentioned that they did not feel under pressure to be the first to adopt a new technology. Instead, they would wait for other clinicians to utilize the technology first, so as to adopt it at a later stage when more experience had been acquired. Regarding individual-related factors, physicians reported their interest in something new and extraordinary as a driver to utilize new technologies, which was closely related to their personalities. Their careers and urge to publish articles, however, also constituted motivations that physicians assessed as a dominating incentive at times. On the other hand, being familiar with a certain product could set a barrier to using new technologies. Regarding patient-related factors affecting the decision to adopt new technologies, physicians mentioned patients’ overall health and the compatibility of the new technology with individual patients. Whereas some physicians stated that they utilized new technologies primarily with young patients, others reported the opposite. Besides, some physicians were also willing to consider patient preferences for a certain technology, even in the context of implantable devices, while others were not willing to do so. A selection of physicians’ statements on the determinants of the decision to adopt new technologies is listed in Table 2. Physicians’ Experiences and Remarks Regarding Evidence Base and Financing of New Technologies With regard to the second research question, physicians overall mentioned a trade-off between early adoption and the possibility to utilize innovative technologies, in particular in the case of new technologies without treatment alternatives. They criticized the fact that the evidence base at the point of market entry was scarce. Therefore, they sometimes preferred to wait for additional evidence. Physicians complained that some new technologies were financed too early through innovation payments. Moreover, they reported that the process of requesting and receiving an innovation payment was too complicated and inflexible. Table 3 provides an overview of physicians’ experiences and remarks. Statements about the evidence base at the time of adoption were divided into comments regarding market authorization, utilization, and study situation. Physicians’ experiences and expectations about innovation payments were divided into issues regarding the new technology, process of requesting and negotiating additional payments, and effects of this financing system. Discussion This study provides detailed information on factors determining the adoption of new technologies from clinicians’ point of view. 1074 VALUE IN HEALTH 21 (2018) 1069–1076 Table 3 – Overview of physicians’ experiences and remarks. Variable Remark/ criticism Evidence base at the time of adoption Market Ensuring product variety authorization Suggestion of diversified approval Requirements for approval Adoption and utilisation Broad diffusion despite lack of evidence No treatment alternatives Long-term effects Study situation Study availability Study design Generating further evidence Risk information letter Innovation payments Technology Insufficient evidence and outdated technologies Process of applying and negotiating Effects of financing Complicated and inflexible Nontransparent reimbursement criteria Negotiations differ regionally No sufficient coverage of additional expenses Wrong economic incentives Statement “I experienced many developments and saw the USA at the same time. I saw that due to the faster implementation of evolutionary steps, we always had much nicer and better designed products, while the Americans, even worse the Japanese, had to use those old things, which we had not used in the last eight, nine years.” (no. 3) “What I think is missing in the field of innovative medical devices in Germany is a tiered system of the approval. The initial barrier of new devices that do not have market approval is too high. That is why we lose these companies and therefore benefits for the German market.” (no. 14) “It’s different here than for example the regulation in the United States through the FDA. There, you first have to show that your new product is better than existing alternatives, before being allowed to use it.” (no. 13) “The [procedure] was a sensation [...] but the results were based on small pilot studies only, so the evidence was limited. Several colleagues used the procedure that was easy to perform and, without a doubt, might have had a certain placebo effect on people. But finally, the long-term study could not show any proven benefit.” (no. 2) “Regarding technologies for rare indications, where no evidence exists due to the low number of diagnoses or illnesses… This probably exists more often than we would like. But I still believe that this technology is the best we have, even if I cannot prove it.” (no. 18) “It usually takes a long time until you know for sure what a specific medical device is able to accomplish.” (no. 14) “We experience that a manufacturer publishes three main results, e.g. “somewhat superior regarding mortality”, and it can take a long time until the entire study is available […] I think that’s really bad.” (no. 5) “Some of the conducted studies really leave much to be desired. Sometimes it is just not acceptable. There are medical devices with participants of 20, 30, 50, 60 people. How can you possibly assess whether it really makes sense or not. That’s challenging.” (no. 10) “University hospitals should utilise more technologies within trials, to clarify whether that’s really suitable for the patient. […] And these hurdles of post-market control. […] It should be designed in a way that if an innovative product comes to the market, one would have to do a respective observational study in the next phase.” (no. 10) “Something important such a ‘red hand letter’ does not exist from my knowledge for medical devices. There have been a few safety alerts, but a comprehensive system, as it is the case for pharmaceuticals, does not exist.” (no. 2) “Funny system. It’s outdated and once something is reimbursed, even if it’s nonsense, they just continue paying it. In cardiology, I still see innovation payments for technologies where everyone knows that they are worthless. But, no one is doing anything.” (no. 3) “You can only request innovation payments until 31st of October, but you cannot say ‘well, I apply for it in January for the running year.’ […] I think that’s impractical.” (no. 6) “The procedure, in particular the selection criteria, which diagnostic and treatment procedures might be reimbursed and which not, is not-transparently I have to say.” (no. 7) “There are different forms of negotiating an innovation payment. Here in province 1, it is completely different from my previous experiences in province 2.” (no. 9) “The approved requests for innovation payments are in few cases really revenuerelevant. The procedure is overall good, but its implementation is deficient.” (no. 13) “One should really control that it is impossible for hospitals with an urgent need for financial means that they take this chance to improve their financial situation.” (no. 7) Note: Number of interviewee is added at the end of each quotation in brackets. The lack of evidence of individual values and attitudes of local innovators was previously highlighted by Varabyova [18]. In addition, Hatz et al. [17] concluded in their analysis of adoption decisions that the behavior of physicians differed according to the length of time that a cardiovascular medical device had been on the market; they thus differentiated between “new” and “old” medical technologies. We contributed to the research on adoption of new technologies by addressing these differences and the research gap, and in addition investigated the role of innovation payments in combination with the introduction of a new regulatory approach for high-risk medical devices in Germany. Our in-depth analysis of physicians’ decision making in relation to the adoption of new technologies generated eight thematic categories. These categories are similar to the categories of influencing factors in German inpatient care identified in previous studies [14–18]. The category regulation can be seen to refer to VALUE IN HEALTH 21 (2018) 1069–1076 previously defined structural, contextual, and environmental factors [14–18]. Organizational factors described in the literature [14,16–18] are presented in our study as hospital-related factors, split into institutional and strategic factors. A particularity in health care is the structure of demand, as physicians use technologies in patient care but the patient is actually the end user. Thus, we decided to split adopter-specific factors into (1) the individual category, including factors of the physicians themselves, and (2) the patient category, covering patient-relevant adoption factors. Lastly, our results comprise typical technology-related factors. Moreover, new thematic categories were identified. Further categories need to be defined supplementing the existing dimensions based on previous research. First, for the physicians in our study, the state of medical care played an important role in adopting decisions, that is, availability of alternative treatments, existence of different technology generations, availability of a follow-up treatment for certain technologies, and so forth. Most previous studies did not consider these factors. The same holds true for activities of the manufacturer, which have been described in the present study, but rarely in previous studies examining physicians’ adoption behavior. Hatz et al. [17] showed that perceived support from the manufacturer was associated with a higher probability of adoption for the group of “new” technologies [17]. Our results show that physicians expected a high service availability, while taking a critical view on studies because of possible influences of manufacturers. High service availability might improve device–operator interactions, as it generates learning curve effects by increasing operators’ experience in the utilization of technologies. Learning curve effects might affect the technologies’ effectiveness [41], as shown by Varabyova et al. [42] for endovascular aneurysm repair (EVAR), a minimally invasive treatment method for abdominal aortic aneurysms. This emphasizes the need for training in the use of medical devices. In addition, physicians discussed the available evidence extensively. Hatz et al. [17] did not identify perceived medical evidence as a major driver of adoption. However, our results showed that the evidence base, depending on the availability of treatment alternatives, was a factor influencing adoption decisions. The interviewed physicians assessed studies and its evidence independently. However, they also stated that the manufacturer served as the basis for decision making. As evidence base did not fit properly into any of the defined categories, we established it as an extra category. Indeed, physicians considered available evidence as an important issue influencing their decision. Our results indicated that physicians perceived the evidence base at the time of market entry to be scarce. In this context, the interviewed physicians criticized the overall lack of studies, the small number of patients in approval studies, and the supposed influence of manufacturers on studies. Furthermore, they noted a lack of studies investigating the effectiveness of new technologies compared to their alternatives, highlighting that such studies are not required for medical devices in the European Union. They viewed additional benefits as a relevant indicator, as in their experience, many technologies provided some minor improvements while generating several complications and overall uncertainty. Regarding the financing of new technologies, the interviewed physicians had the power within the hospital to choose the product and manufacturer they preferred, even if it was more expensive than the calculated costs in the reimbursed rates. Nonetheless, physicians felt a personal responsibility to support the economic well-being of the hospital or the goal of breaking even. Therefore, clinicians tried to act within the scope of the DRGs. This supports the notion that the diffusion of new technologies is steered by their reimbursement. Owing to scarce evidence and the requirement of additional reimbursement, the physicians supported the aim and objectives of the health policy reform. However, the design of the approach 1075 and its implementation were criticized. With regard to medical decision making based on effectiveness evidence, this regulatory instrument will fall short. Additional evidence may be gathered only for a small group of technologies with the following prerequisites: (1) hospitals’ first request for innovation payment, (2) defined as “high-risk medical device”, (3) with an underlying “new theoretical and scientific concept,” and (4) status of “potential.” Many technologies do not fall under this approach as it is currently designed (e.g., high-risk technologies without requests for innovation payments). Although this study allowed a unique insight into physicians’ perspectives using a qualitative approach, some limitations need to be acknowledged [43]. Besides the researchers’ individual conclusions of the analysis, our study results might not be representative of all physicians [44,45]. In addition, conducting telephone interviews has disadvantages compared to an appointment in person (e.g., lack of interaction between interviewer and participant) [46]. Carrying out telephone interviews, however, has also shown some advantages (e.g., high response rate, low costs) [47]. Furthermore, we interviewed chief and senior physicians only, who were professionals with a certain hierarchical and thus experience level. As years of medical practice were found to be negatively associated with the adoption of new technologies [48,49], clinicians in other positions should also be considered in further research. Overall, as the present analysis was based on 23 interviews to identify a wide range of factors influencing physicians’ adoption decisions, further quantitative studies are necessary to investigate factors according to their relevance in adoption decisions and their relations. Conclusions This study provides an in-depth understanding of factors influencing the decision of clinicians to adopt new technologies. We identified 52 factors grouped in eight thematic categories, depicting the overall trade-off that physicians have to manage in adoption decisions. The interviewed physicians supported the general notion of conducting benefit assessments and, if necessary, generating additional evidence. However, they criticized the design and implementation of the German CED approach. They appreciated improvements in receiving summarized information. Therefore, a further step and challenge for policymakers and payers could be to bring together country-specific evidence on the effectiveness of new technologies at the European level to build a transnational overarching database. The central provision of summarized evidence might assist physicians in their decision to use new technologies. Overall, the results of the 23 interviews based on qualitative content analysis should be verified via quantitative studies in future research to investigate factors according to their relevance in adoption decisions and their relations in more detail. Acknowledgments We are grateful to the clinicians who took part in the interviews free at charge. We appreciate their time and valuable answers. This study was funded through the Berlin Centre for Health Economics Research by the German Federal Ministry of Education and Research (grant no. 01EH1604A). P Ex holds a Cusanuswerk scholarship to conduct research for her doctorate. Supplemental Materials Supplementary data associated with this article can be found in the online version at https://doi.org/10.1016/j.jval.2018.03.006. 1076 VALUE IN HEALTH 21 (2018) 1069–1076 R EF E R EN CE S [25] [1] Rothery C, Claxton K, Palmer S, et al. Characterising uncertainty in the assessment of medical devices and determining future research needs. Health Econ 2017;26(Suppl.1):109–23. [2] Greer AL. Adoption of medical technology: the hospital's three decision systems. IJTAHC 1985;1:669–80. [3] van de Wetering EJ, van Exel J, Brouwer WBF. The challenge of conditional reimbursement: stopping reimbursement can be more difficult than not starting in the first place! Value Health 2017;20:118–25. [4] Walker S, Sculpher M, Claxton K, et al. Coverage with evidence development, only in research, risk sharing, or patient access scheme? A framework for coverage decisions. Value Health 2012;15:570–9. [5] van Norman GA. Drugs and devices: comparison of European and U.S. approval processes. JACC Basic Transl Sci 2016;1:399–412. [6] Blank JLT, Valdmanis VG. Technology diffusion in hospitals: a log odds random effects regression model. Int J Health Plann Manage 2015;30:246–59. [7] Bech M, Christiansen T, Dunham K, et al. The influence of economic incentives and regulatory factors on the adoption of treatment technologies: a case study of technologies used to treat heart attacks. Health Econ 2009;18:1114–32. [8] Sorenson C, Drummond M, Torbica A, et al. The role of hospital payments in the adoption of new medical technologies: an international survey of current practice. Health Econ Policy Law 2015;10:133–59. [9] Cappellaro G, Ghislandi S, Anessi-Pessina E. Diffusion of medical technology: the role of financing. Health Policy 2011;100:51–9. [10] Cutler DM, Huckman RS. Technological development and medical productivity: the diffusion of angioplasty in New York State. J Health Econ 2003;22:187–217. [11] Sloan FA, Valvona J, Perrin JM, et al. Diffusion of surgical technology. An exploratory study. J Health Econ 1986;5:31–61. [12] Gold HT, Pitrelli K, Hayes MK, et al. Decision to adopt medical technology: case study of breast cancer radiotherapy techniques. Med Decis Making 2014;34:1006–15. [13] Ubel PA, Asch DA. Creating value in health by understanding and overcoming resistance to de-innovation. Health Aff (Millwood) 2015;34:239–44. [14] Kimberly JR, Evanisko MJ. Organizational innovation: the influence of individual, organizational, and contextual factors on hospital adoption of technological and administrative innovations. Acad Manage J 1981;24:689–713. [15] McCullough JS. The adoption of hospital information systems. Health Econ 2008;17:649–64. [16] Chaudoir SR, Dugan AG, Barr CHI. Measuring factors affecting implementation of health innovations: a systematic review of structural, organizational, provider, patient, and innovation level measures. Implement Sci 2013;8:22. [17] Hatz MHM, Schreyögg J, Torbica A, et al. Adoption decisions for medical devices in the field of cardiology: results from a European survey. Health Econ 2017;26(Suppl.1):124–44. [18] Varabyova Y, Blankart CR, Greer AL, et al. The determinants of medical technology adoption in different decisional systems: a systematic literature review. Health Policy 2017;121:230–42. [19] Banta HD, Russell LB. Policies toward medical technology: an international review. Int J Health Serv 1981;11:631–52. [20] Tunis SR, Pearson SD. Coverage options for promising technologies: Medicare's ‘coverage with evidence development. Health Aff (Millwood) 2006;25:1218–30. [21] Martelli N, van den Brink H, Borget I. New french coverage with evidence development for innovative medical devices: improvements and unresolved issues. Value Health 2016;19:17–9. [22] Olberg B, Perleth M, Busse R. The new regulation to investigate potentially beneficial diagnostic and therapeutic methods in Germany: up to international standard? Health Policy 2014;117:135–45. [23] Ferrario A, Kanavos P. Dealing with uncertainty and high prices of new medicines: a comparative analysis of the use of managed entry agreements in Belgium, England, the Netherlands and Sweden. Soc Sci Med 2015;124:39–47. [24] Olberg B, Fuchs S, Matthias K, et al. Evidence-based decision-making for diagnostic and therapeutic methods: the changing landscape of [26] [27] [28] [29] [30] [31] [32] [33] [34] [35] [36] [37] [38] [39] [40] [41] [42] [43] [44] [45] [46] [47] [48] [49] assessment approaches in Germany. Health Res Policy Syst 2017;15:1–11. Gemeinsamer Bundesausschuss, G-BA (Federal Joint Commitee). Tragende Gründe zum Beschluss des Gemeinsamen Bundesausschusses über die Einschlägigkeit des Verfahrens gemäß 2. Kapitel § 33 Absatz 1 Verfahrensordnung: Koronare Lithoplastie bei koronarer Herzkrankheit 2017. Available from: https://www.g-ba.de/ downloads/40-268-4664/2017-11-17_137h_BAh-17-004_Lithoplastie_ TrG.pdf. [Accessed January 22, 2018]. Ex P, Busse R, Henschke C. Die Nutzenbewertung von nichtmedikamentösen Untersuchungs- und Behandlungsmethoden. Welche Tragweite hat die Regelung nach § 137h SGB V? GuS 2016;70:48–55. Sorenson C, Drummond M, Wilkinson G. Use of innovation payments to encourage the adoption of new medical technologies in the English NHS. Health Policy Technol 2013;2:168–73. Scheller-Kreinsen D, Quentin W, Busse R. DRG-based hospital payment systems and technological innovation in 12 European countries. Value Health 2011;14:1166–72. Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen, IQWiG (Institute for Quality and Efficiency in Health Care). Allgemeine Methoden: Version 5.0 vom 10.07.2017. Köln, 2017. Denzin NK, Lincoln YS, editors. The Sage Handbook of Qualitative Research (3rd ed.). Thousand Oaks, CA: SAGE, 2009. Gill P, Stewart K, Treasure E, et al. Methods of data collection in qualitative research: interviews and focus groups. Br Dent J 2008;204:291–5. Turner DW. Qualitative interview design: a practical guide for novice investigators. Qual Rep 2010;15:754–60. Breakwell GM, ed. Research Methods in Psychology (3rd ed.). Los Angeles, CA: SAGE, 2007. Porter ME, Guth C. Redefining the German Healthcare System. Berlin, Heidelberg: Springer-Verlag, 2012. Bölt U. In: Klauber J, Friedrich J, Wasem J, eds. Statistische Krankenhausdaten: Grund- und Kostendaten der Krankenhäuser 2012. Schwerpunkt: Strukturwandel: Mit 98 Tabellen. Stuttgart: Schattauer Verlag, 2015. Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Method 2006; 18:59–82. Miles MB, Huberman AM, Saldana J. Qualitative Data Analysis: A Methods Sourcebook (3rd ed). Thousand Oaks, CA: SAGE, 2014. Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15:1277–88. Campbell JL, Quincy C, Osserman J, et al. Coding in-depth semistructured interviews: problems of unitization and intercoder reliability and agreement. Sociol Methods Res 2013;42: 294–320. Webb C. Analysing qualitative data: computerized and other approaches. J Adv Nurs 1999;29:323–30. Tarricone R, Torbica A, Drummond M. Challenges in the assessment of medical devices: the MedtecHTA project. Health Econ 2017;26 (Suppl.1):5–12. Varabyova Y, Blankart CR, Schreyögg J. The role of learning in health technology assessments: an empirical assessment of endovascular aneurysm repairs in German hospitals. Health Econ 2017;26 (Suppl.1):93–108. Stewart K, Gill P, Chadwick B, et al. Qualitative research in dentistry. Br Dent J 2008;204:235–9. Eysenbach G, Köhler C. How do consumers search for and appraise health information on the world wide web? Qualitative study using focus groups, usability tests, and in-depth interviews. BMJ 2002;324:573–7. Mays N, Pope C. Rigour and qualitative research. BMJ 1995;311:109–12. Trier-Bieniek A. Framing the telephone interview as a participantcentred tool for qualitative research: a methodological discussion. Qual Res 2012;12:630–44. Carr EC, Worth A. The use of the telephone interview for research. J Res Nurs 2001;6:511–24. Scott SD, Plotnikoff RC, Karunamuni N, et al. Factors influencing the adoption of an innovation: an examination of the uptake of the Canadian Heart Health Kit (HHK). Implement Sci 2008;3:1–8. Choudhry NK, Fletcher RH, Soumerai SB. Systematic review: the relationship between clinical experience and quality of health care. Ann Intern Med 2005;142:260–73.