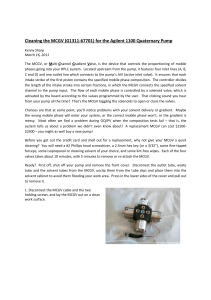
JACC: CARDIOVASCULAR INTERVENTIONS VOL. 14, NO. 5, 2021 ª 2021 BY THE AMERICAN COLLEGE OF CARDIOLOGY FOUNDATION PUBLISHED BY ELSEVIER NEW RESEARCH PAPERS STRUCTURAL Transfemoral Transcatheter Tricuspid Valve Replacement With the EVOQUE System A Multicenter, Observational, First-in-Human Experience Neil P. Fam, MD, MSC,a,* Ralph Stephan von Bardeleben, MD,b,* Mark Hensey, MB BCH, BAO,c Susheel K. Kodali, MD,d Robert L. Smith, MD,e Jörg Hausleiter, MD,f,g Geraldine Ong, MD,a Robert Boone, MD,c Tobias Ruf, MD,b Isaac George, MD,d Molly Szerlip, MD,e Michael Näbauer, MD,f,g Faeez M. Ali, MD,a Robert Moss, MD,c Vinayak Bapat, MD,d Katharina Schnitzler, MD,b Felix Kreidel, MD,b Jian Ye, MD,c Djeven P. Deva, MD,a Michael J. Mack, MD,e Paul A. Grayburn, MD,e Mark D. Peterson, MD,a Martin B. Leon, MD,d Rebecca T. Hahn, MD,d John G. Webb, MDc ABSTRACT OBJECTIVES The purpose of this observational first-in-human experience was to investigate the feasibility and safety of the EVOQUE tricuspid valve replacement system and its impact on short-term clinical outcomes. BACKGROUND Transcatheter tricuspid intervention is a promising option for selected patients with severe tricuspid regurgitation (TR). Although transcatheter leaflet repair is an option for some, transcatheter tricuspid valve replacement (TTVR) may be applicable to a broader population. METHODS Twenty-five patients with severe TR underwent EVOQUE TTVR in a compassionate-use experience. The primary outcome was technical success, with NYHA (NYHA) functional class, TR grade, and major adverse cardiac and cerebrovascular events assessed at 30-day follow-up. RESULTS All patients (mean age 76 3 years, 88% women) were at high surgical risk (mean Society of Thoracic Surgeons risk score 9.1 2.3%), with 96% in NYHA functional class III or IV. TR etiology was predominantly functional, with mean tricuspid annular diameter of 44.8 7.8 mm and mean tricuspid annular plane systolic excursion of 16 2 mm. Technical success was 92%, with no intraprocedural mortality or conversion to surgery. At 30-day follow-up, mortality was 0%, 76% of patients were in NYHA functional class I or II, and TR grade was #2þ in 96%. Major bleeding occurred in 3 patients (12%), 2 patients (8%) required pacemaker implantation, and 1 patient (4%) required dialysis. CONCLUSIONS This first-in-human experience evaluating EVOQUE TTVR demonstrated high technical success, acceptable safety, and significant clinical improvement. Larger prospective studies are needed to confirm durability and safety and the impact on long-term clinical outcomes. (J Am Coll Cardiol Intv 2021;14:501–11) © 2021 by the American College of Cardiology Foundation. From aSt. Michael’s Hospital, University of Toronto, Toronto, Ontario, Canada; bZentrum für Kardiologie, Universitätsmedizin Mainz, Johannes Gutenberg Universität, Mainz, Germany; cSt. Paul’s Hospital, Centre for Heart Valve Innovation, University of British Columbia, Vancouver, British Columbia, Canada; dNewYork-Presbyterian Hospital, Columbia University Medical Center, New York, New York, USA; eBaylor Scott & White Heart and Vascular Hospital, Dallas, Texas, USA; fMedizinische Klinik und Poliklinik I, Klinikum der Universität München, Munich, Germany; and gDZHK (German Center for Cardiovascular Research), Partner Site Munich Heart Alliance, Munich, Germany. *Drs. Fam and von Bardeleben are joint first authors and contributed equally to this paper. ISSN 1936-8798/$36.00 https://doi.org/10.1016/j.jcin.2020.11.045 502 Fam et al. JACC: CARDIOVASCULAR INTERVENTIONS VOL. 14, NO. 5, 2021 MARCH 8, 2021:501–11 EVOQUE Transfemoral TTVR for Severe TR S ABBREVIATIONS evere tricuspid regurgitation (TR) is a observational, nonrandomized, single-arm study. All common valvular disease with signifi- patients had right-sided HF (New York Heart Associ- cant morbidity and mortality (1–4). ation [NYHA] functional class II to IV) despite medical Most patients have functional TR, which is therapy and were deemed at high surgical risk or usually treated conservatively with diuretic inoperable by the local heart team. Eligible patients agents given the burden of comorbidities provided IVC = inferior vena cava and high risk of surgery in this patient cohort included after acceptance from the corresponding NYHA = New York Heart (5,6). Given this unmet clinical need, trans- national regulatory board on the basis of individual catheter tricuspid intervention has emerged patient characteristics. The study was approved by as a promising treatment option for patients the St. Michael’s Hospital research ethics board. RV = right ventricular with TR and right-sided heart failure (HF). Given that this was a compassionate-use experience, TAPSE = tricuspid annular The most commonly used technique is trans- there was no study protocol, and thus no formal pre- AND ACRONYMS CT = computed tomographic FAC = fractional area change HF = heart failure Association RA = right atrial plane systolic excursion TR = tricuspid regurgitation TTVr = transcatheter tricuspid valve repair TTVR = transcatheter tricuspid valve replacement written informed consent and were catheter leaflet repair, which has demon- specified inclusion or exclusion criteria were defined. strated reasonable All patients underwent informal external review by efficacy for TR reduction (7–9). However, a the sites and the sponsor to determine acceptable number of predictors of procedural failure anatomy for the procedure. In general, patients were for identified, considered if the heart team judged that trans- including baseline massive or torrential TR, catheter leaflet repair would not be feasible (i.e., large excellent leaflet repair safety have and been significant leaflet tethering, and coaptation gap [>10-mm] coaptation gaps, severe leaflet tethering, >7 mm, potentially limiting its broad application and/or pacemaker-induced TR), with suitable anat- (7,8,10). These predictors are similar to those for fail- omy ure of surgical tricuspid repair, and currently the ma- considered anatomically suitable for EVOQUE TTVR if jority of surgical candidates with advanced TR they had adequate screening transesophageal echo- undergo tricuspid valve replacement (5). cardiographic imaging of the tricuspid valve leaflets SEE PAGE 512 for EVOQUE implantation. Patients were for procedural guidance and computed tomography– derived tricuspid valve annular dimensions compat- Recently, the feasibility of transcatheter tricuspid ible with 44- or 48-mm valves. There were no specific valve replacement (TTVR) via thoracotomy or a anatomic exclusions. Patients with severe right ven- transjugular approach was reported but was associ- tricular (RV) dysfunction or significant pulmonary ated with significant risk for complications using a arterial hypertension (pulmonary artery systolic first-generation device (11–13). The EVOQUE valve pressure >60 mm Hg) were excluded. replacement system (Edwards Lifesciences, Irvine, The primary outcome was technical success, California) was first described for percutaneous, defined as absence of procedural mortality; success- transfemoral transcatheter mitral valve replacement ful access, delivery, and retrieval of the device de- (14) and recently for successful transfemoral TTVR livery system; successful deployment and correct (15). Our aim was to summarize the early experience, positioning of the first intended device; and freedom including feasibility, safety, short-term durability, from emergency surgery or reintervention related to and clinical outcome of patients with severe TR the device or access procedure. At 30-day follow-up, treated with the EVOQUE system for transfemoral NYHA functional class, and TR severity grade were TTVR. assessed as major outcome parameters along with major adverse cardiac and cerebrovascular events. METHODS Clinical endpoints were defined according to the Mitral Valve Academic Research Consortium criteria Twenty-five consecutive patients were treated for (16). Furthermore, echocardiographic parameters of symptomatic severe TR using the EVOQUE valve RV size and function were determined. replacement system between May 2019 and February STUDY 2020 at 6 centers as part of a compassionate-use, Procedures were performed under general anesthesia DEVICE AND PROCEDURAL The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center. Manuscript received September 29, 2020; revised manuscript received November 20, 2020, accepted November 24, 2020. TECHNIQUE. Fam et al. JACC: CARDIOVASCULAR INTERVENTIONS VOL. 14, NO. 5, 2021 MARCH 8, 2021:501–11 EVOQUE Transfemoral TTVR for Severe TR F I G U R E 1 EVOQUE Transcatheter Tricuspid Valve Replacement System (A) EVOQUE transcatheter heart valve: self-expanding Nitinol frame with bovine pericardial leaflets, intra-annular sealing skirt, and ventricular anchors. (B) The 28-F EVOQUE tricuspid delivery system. with transesophageal echocardiographic and fluoro- are positioned beneath the leaflet segments as well as scopic guidance. After percutaneous right femoral final depth and trajectory adjustment, the atrial venous access, a 12-F deflectable sheath (Oscor, Palm inflow portion of the valve with its sealing skirt is Harbor, Florida) is placed in the right atrium, and subsequently expanded at the annular level, followed subsequently a Safari Extra Small guidewire (Boston by release of the valve. The delivery system is then Scientific, Marlborough, Massachusetts) is advanced removed and the femoral puncture site is closed with through the tricuspid valve into the RV apex. To previously placed percutaneous or subcutaneous su- confirm that the wire path is free of the subvalvular ture. Patients were treated with intravenous heparin apparatus, a balloon is passed across the tricuspid during the procedure, targeting an activated clotting valve to the RV apex (Reliant, Medtronic, Minneap- time of >300 s. After the procedure, all patients olis, Minnesota). Alternatively, free wire motion is received oral anticoagulation with or without aspirin confirmed in multiple echocardiographic views. The for a minimum of 6 months. 28-F EVOQUE valve replacement system for TR (Figure 1), which is identical to the system for mitral regurgitation (14), is then introduced over the wire and advanced to the tricuspid valve. The available EVOQUE valve sizes were 44 and 48 mm, and the device consists of a self-expanding Nitinol frame, ECHOCARDIOGRAPHY. The severity of TR was graded using transthoracic echocardiography according to current guidelines at baseline, before discharge, and at 30-day follow-up. We reported the grade of TR using a 5-grade scheme (17). bovine pericardial leaflets, and a fabric skirt to mini- STATISTICAL ANALYSIS. Continuous variables are mize paravalvular leak. The valve has a unique presented as mean SD. We used the Fisher exact anchoring mechanism that uses the annulus, leaflets, test to compare categorical variables and the Wil- and chords for stable implantation. The EVOQUE de- coxon signed rank test for the comparison of contin- livery system allows 3 planes of motion: primary uous variables. A 2-tailed p value <0.05 was flexion is first used to move perpendicular to the considered to indicate statistical significance. All tricuspid annulus, and secondary flexion is then used patients to ensure coaxial alignment within the tricuspid treat analysis. were included using an intention-to- valve. Depth of implantation is adjusted with a depth knob while maintaining coaxial alignment. The sys- RESULTS tem is secured in a stabilizer to allow ease of use BASELINE CHARACTERISTICS. Baseline patient charac- during the procedure. Once the system has been advanced across the teristics are summarized in Table 1. A total of 25 tricuspid valve annulus to an appropriate depth with consecutive patients (88% women) with a mean age confirmation of device position and trajectory, the of 76 3 years were at high surgical risk as expressed ventricular anchors are exposed by slowly with- by an Society of Thoracic Surgeons risk score of 9.1 drawing the outer restraining capsule (Figure 2). 2.3% and a European System for Cardiac Operative Further expansion results in positioning of the U- Risk Evaluation II score of 7.7 3.8%. All patients had shaped anchors on the ventricular side of the right-sided HF due to severe TR (TR $3þ), 96% were tricuspid in NYHA functional class III or IV, 84% were in atrial leaflets, dimensional and which is confirmed 3-dimensional by 2- transesophageal echocardiography. After confirming that all 9 anchors fibrillation or flutter, 44% had previous left-sided valve intervention, and 36% had permanent 503 504 Fam et al. JACC: CARDIOVASCULAR INTERVENTIONS VOL. 14, NO. 5, 2021 EVOQUE Transfemoral TTVR for Severe TR MARCH 8, 2021:501–11 F I G U R E 2 Case Example of EVOQUE Tricuspid Replacement Continued on the next page Fam et al. JACC: CARDIOVASCULAR INTERVENTIONS VOL. 14, NO. 5, 2021 MARCH 8, 2021:501–11 EVOQUE Transfemoral TTVR for Severe TR pacemaker leads. The majority of patients (71%) had T A B L E 1 Baseline Characteristics (n ¼ 25) chronic kidney disease, 28% had coronary artery Age (yrs) 76 3 disease, with elevated N-terminal brain natriuretic Female 22 (88) peptide (mean 3,106 2,028 pg/ml). Baseline medical EuroSCORE II (%) 7.7 2.2 therapy included loop diuretic agents in 100%, aldo- STS score (%) 9.1 2.3 sterone antagonists in 68%, and anticoagulant agents NYHA functional class II III IV 3 (12) 19 (76) 3 (12) Coronary artery disease 7 (28) The etiology of TR was functional in 19 patients 1 (4) (76%), degenerative in 1 patient (4%) (carcinoid), and 5 (20) mixed in 5 patients (20%) (annular dilatation with 2 (8) tricuspid valve prolapse in 3 patients, annular dila- Previous valve intervention AVR (5.6 3.9 yrs) MVR (13.1 3.4 yrs) TV DeVega annuloplasty (11 yrs) 11 (44) 7 (28) 6 (24) 1 (4) tation with rheumatic disease in 2 patients). TR was Transtricuspid PM/ICD lead 9 (36) Renal impairment 15 (60) Previous myocardial infarction Previous CABG Previous PCI COPD 3 (12) Atrial fibrillation 21 (84) Previous TIA/stroke 6 (24) Hypertension 17 (68) Diabetes 8 (32) Peripheral edema 18 (72) Ascites 14 (56) in 92% of patients. Baseline echocardiographic and computed tomographic (CT) parameters are summarized in Table 2. graded as torrential in 56%, massive in 28%, and severe in 16% of patients. The mean left ventricular ejection fraction was 58.3 8.6%, mean RV basal diameter was 50.8 7.2 mm, and mean RV/right atrial (RA) gradient was 35 4 mm Hg. Overall, RV function was mildly to moderately reduced, with mean tricuspid annular plane systolic excursion (TAPSE) of 16 2 mm (64% with TAPSE <17 mm), RV fractional area change (FAC) of 37 11% (36% with FAC <35%), and RV dP/dt of 423 240 ms. CT analysis demonstrated mean tricuspid annular diameter of 45.2 2.7 mm, inferior vena cava (IVC)–tricuspid annulus Loop diuretic agent 25 (100) Aldosterone antagonist agent 19 (68) Anticoagulant Warfarin (AVR or MVR) DOAC (AF) 23 (92) 11 (44) 12 (48) diastole was 3.0 4.1%. Figure 3 shows CT analysis of GFR (ml/min/1.73 m2) 52 8 jectory of the delivery system in a patient with NT-BNP (pg/ml) 3,106 2,028 AST (U/l) 30 4 ALT (U/l) 25 10 GGT (U/l) 137 7 Bilirubin (mg/dl) 1.9 1.7 distance of 5.8 1.8 mm, and IVC–tricuspid annulus angle of 83 13 . The degree of valve oversizing in tricuspid annular dimensions, device sizing, and trapacemaker leads. PROCEDURAL OUTCOMES. Sixteen patients (64%) received 48-mm valves and 8 (32%) received 44-mm valves (Table 3). Technical success was achieved in 23 of 25 patients (92%). One patient had an unsuc- Values are mean SD or n (%). cessful procedure with no valve implanted because of AF ¼ atrial fibrillation; ALT ¼ alanine aminotransferase; AST ¼ aspartate aminotransferase; AVR ¼ aortic valve replacement; CABG ¼ coronary artery bypass graft; COPD ¼ chronic obstructive pulmonary disease; DOAC ¼ direct oral anticoagulant agent; EuroSCORE ¼ European System for Cardiac Operative Risk Evaluation; GFR ¼ glomerular filtration rate; GGT ¼ gamma-glutamyl transferase; ICD ¼ implantable cardioverter-defibrillator; MVR ¼ mitral valve replacement; NTBNP ¼ N-terminal B type natriuretic peptide; NYHA ¼ New York Heart Association; PCI ¼ percutaneous coronary intervention; PM ¼ pacemaker; STS ¼ Society of Thoracic Surgeons; TIA ¼ transient ischemic attack; TV ¼ tricuspid valve. a noncoaxial approach, and the delivery system was removed without complications. One patient had a low implantation (too ventricular) with severe residual central TR secondary to native leaflet interference, successfully SAPIEN 3 treated (Edwards acutely Lifesciences) with 29-mm valve-in-valve F I G U R E 2 Continued (A) Baseline echocardiogram demonstrating lead adherent to posterior tricuspid leaflet. (B) Baseline echocardiogram with color Doppler showing massive tricuspid regurgitation (TR). (C) Fluoroscopy of initial position of EVOQUE delivery system across the tricuspid annulus. (D) Corresponding 3-dimensional (3D) transesophageal echocardiographic (TEE) imaging of delivery system position and trajectory. (E) Fluoroscopy showing ventricular anchors deployed. (F) Corresponding 3D TEE imaging of tricuspid leaflet capture. (G) Fluoroscopy after atrial expansion and valve release. (H) Transthoracic echocardiography at follow-up showing trace TR. (I) Three-dimensional TEE imaging showing pacemaker lead in posteroseptal commissure. 505 506 Fam et al. JACC: CARDIOVASCULAR INTERVENTIONS VOL. 14, NO. 5, 2021 MARCH 8, 2021:501–11 EVOQUE Transfemoral TTVR for Severe TR pacemaker implantation through the EVOQUE valve. T A B L E 2 Baseline Echocardiographic Parameters There were 3 patients (12%) with major bleeding TR etiology Functional Degenerative Mixed 19 (76) 1 (4) 5 (20) TR severity Grade 5þ Grade 4þ Grade 3þ 14 (56) 7 (28) 4 (16) complications: 1 gastrointestinal bleed, 1 spontaneous thigh intramuscular hematoma, and 1 retroperitoneal bleed from the nonaccess site, all in the context of combination LVEF (%) 58.3 3.6 RV diameter base (mm) 50.7 3.1 RV diameter mid (mm) 40.1 3.2 Tricuspid annular S-L (mm) 44.7 7.1 RVEF (%) 49.2 3.4 TAPSE (mm) 15.6 2.5 423.5 109.2 RV dP/dt (mm Hg/s) 15.4 4.2 RV free wall strain 37.6 5.1 RV FAC (%) 12.2 2.1 TR vena contracta (mm) 85.7 20.7 2 TR EROA (mm ) TR regurgitant volume (ml) 60.2 8 TV mean gradient (mm Hg) 1.5 0.4 RVSP (mm Hg) 34.6 4.3 IVC (mm) 28.4 2.1 therapy with anticoagulation and aspirin. Two patients (8%) with baseline moderate to severe RV dysfunction developed afterload mismatch with worsening RV function and required short-term inotropic support. One patient (4%) developed asymptomatic leaflet thickening with increased valve gradient in the context of subtherapeutic anticoagulation, which completely resolved once therapeutic anticoagulation was achieved. No other major adverse cardiac and cerebrovascular events were observed. There was a significant improvement in NYHA functional class in 76% of patients (19 of 25) (Central Illustration). In addition, the incidence of patients in NYHA functional class $III was reduced from 96% (24 of 25 patients) at baseline to 24% (6 of 25 patients) at 30-day follow-up (p < 0.001) (Central Illustration). Moreover, clinical signs of right-sided HF including peripheral edema (72% vs. 24%; p < 0.001) and ascites (56% vs. 8%; p < 0.001) Values are n (%) or mean SD. significantly improved, and diuretic agent doses dP/dt ¼ change in pressure/change in time; EROA ¼ effective regurgitant orifice area; FAC ¼ fractional area change; IVC ¼ inferior vena cava; LVEF ¼ left ventricular ejection fraction; RV ¼ right ventricular; RVEF ¼ right ventricular ejection fraction; RVSP ¼ right ventricular systolic pressure; S-L ¼ septal-lateral; TAPSE ¼ tricuspid annular plane systolic excursion; TR ¼ tricuspid regurgitation; TV ¼ tricuspid valve. could be reduced in 28% of patients at follow-up. There was no significant change in renal function from baseline to follow-up (glomerular filtration rate 52 8 ml/min vs. 58 9 ml/min; p ¼ 0.14), but biochemical measures of hepatic congestion improved, including bilirubin (1.9 1.7 mg/dl vs. 0.9 0.2 mg/dl; p ¼ 0.01) and gamma-glutamyl transimplantation. No patient experienced peri-procedural ferase (137 77 U/l vs. 99 58 U/l; p ¼ 0.08). All myocardial infarction, stroke, or device embolization. patients were anticoagulated with either warfarin After valve implantation, TR was reduced to #1þ in 23 (80%) or direct oral anticoagulant agents (20%) of 25 patients (92%), with a mean tricuspid valve indefinitely; 68% of patients also received aspirin. gradient of 2.1 1.1 mm Hg (Central Illustration). In patients with residual mild TR, the location was paravalvular in 44% and intravalvular in 56%. One patient had moderate paravalvular TR due to device canting within the annulus, with stable position. Mean RA pressure was reduced from 15.0 3.3 to 12.8 5.1 mm Hg (p ¼ 0.03) and mean RA V-wave pressure from 24.6 9.0 to 15.4 6.9 mm Hg (p ¼ 0.005). Total procedure time was 140 79 min, device time was 68 47 min, and contrast volume was 25 36 ml. 30-DAY ECHOCARDIOGRAPHIC RESULTS. Echocardio- graphy demonstrated sustained TR reduction, with TR grade #2þ in 96% and #1þ in 88% at 30-day follow-up (Central Illustration). Overall, the mean TR grade was reduced from 4.4 0.3 to 0.8 0.5 (p < 0.001). The mean tricuspid valve gradient was 3.2 0.6 mm Hg. We observed a slight worsening of RV function (TAPSE 16 2 mm vs. 14 3 mm [p ¼ 0.11] and FAC 37 11% vs. 30 8% [p ¼ 0.01]), as expected given significant reduction of TR. IVC diameter 30-DAY CLINICAL OUTCOMES. At follow-up, mor- decreased from 28 2 mm to 20 3 mm (p < 0.001), tality was 0%. There was no myocardial infarction, while RV systolic pressure remained similar (34.6 stroke, valve reintervention, or HF hospitalization 4.3 mm Hg vs. 42 5.5 mm Hg; p ¼ 0.21). Further- (Table 4). One patient (4%) with baseline stage IV more, there was evidence of favorable RV remodel- renal impairment developed progressive renal failure ing: RV basal diastolic diameter decreased from 50.8 requiring dialysis. Two patients (8%) developed 7.2 mm at baseline to 46.4 6.3 mm at 30-day conduction follow-up disturbances requiring permanent (p ¼ 0.009). Selected patients also Fam et al. JACC: CARDIOVASCULAR INTERVENTIONS VOL. 14, NO. 5, 2021 MARCH 8, 2021:501–11 EVOQUE Transfemoral TTVR for Severe TR F I G U R E 3 Computed Tomography for Procedural Planning (A) Cross-sectional dimensions of the tricuspid annulus in systole. (B) Cross-sectional dimensions of the tricuspid annulus in diastole. (C) Valve sizing and spatial relationship to pacemaker leads. (D) Projected trajectory of delivery system. underwent follow-up CT assessment, which demon- (7–9). However, in the recently reported prospective strated reductions in RV volume with RV reverse TRILUMINATE study of the TriClip system, TR remodeling and no instances of hypoattenuating grade #2þ was achieved in only 57% of patients by leaflet thickening (Figure 4). echocardiography core laboratory assessment at 30day DISCUSSION follow-up (21). The presence of baseline massive or torrential TR, significant leaflet tethering, and large coaptation gaps are predictors of proce- Here, we demonstrate for the first time in a dural failure with transcatheter leaflet repair, which compassionate-use cohort the feasibility and safety of percutaneous, transfemoral TTVR with the EVOQUE system in patients with severe TR. In this early experience, we observed a high rate of technical success of valve implantation (92%), with no mortality, myocardial infarction, stroke, or HF hospitalization. Furthermore, the results seem to be durable and associated with significant improvement in functional status at short-term follow-up. Given the high risk of tricuspid surgery (5,6,18) and poor (19,20), outcomes transcatheter with conservative tricuspid therapy intervention has recently emerged as a viable alternative. Transcatheter leaflet repair is the most common strategy, with excellent safety and site-reported procedural success (TR grade #2þ) ranging from 72% to 86% T A B L E 3 Procedural Outcomes (n ¼ 25) Technical success Mortality 23 (92) 0 (0) Myocardial infarction 0 (0) Stroke 0 (0) Device embolization 0 (0) Major bleeding 0 (0) Conversion to surgery 0 (0) Reintervention Tricuspid regurgitation #1þ Procedure time (min) Values are n (%) or mean SD. 1 (4) 23 (92) 140 79 507 508 Fam et al. JACC: CARDIOVASCULAR INTERVENTIONS VOL. 14, NO. 5, 2021 MARCH 8, 2021:501–11 EVOQUE Transfemoral TTVR for Severe TR C E N T R A L IL L U ST R A T I O N Outcomes After EVOQUE Transfemoral Transcatheter Tricuspid Valve Replacement for Severe Tricuspid Regurgitation EVOQUE Transfemoral TTVR Impact on Clinical Outcomes N = 25 A NYHA Functional Class 100% 90% NYHA IV NYHA IV NYHA III 80% B Tricuspid Regurgitation 100% 70% 60% 60% NYHA III 40% 20% 20% 0% Baseline TR 1+ TR 1+ TR 4+ TR 0+ TR 0+ Procedural 1 Month 40% 30% NYHA II TR 5+ 50% NYHA II 30% 10% TR 5+ TR 2+ 80% 70% 50% TR 5+ TR 2+ 90% NYHA I 1 Month 10% 0% TR 3+ Baseline Fam, N.P. et al. J Am Coll Cardiol Intv. 2021;14(5):501–11. (A) New York Heart Association (NYHA) functional class at baseline and 1-month follow-up showing significant improvement (p < 0.001). (B) Tricuspid regurgitation (TR) grade at baseline, post-procedure, and 1-month follow-up demonstrated significant TR reduction (p < 0.001). is associated with increased risk for mortality and patients with severe RV dysfunction and/or pulmo- HF hospitalization at follow-up (7,8). In the present nary hypertension. All patients underwent compre- study of EVOQUE transfemoral TTVR, TR grade #2þ hensive assessment prior to intervention with both was achieved in 96% and #1þ in 88% of patients at right and left heart catheterization in addition to 30-day follow-up, even though massive or torrential echocardiography, which may underestimate pulmo- TR was present in 84% of patients at baseline. nary artery pressure in the setting of severe TR (22). Similar to surgical tricuspid valve replacement, Further studies are needed to define optimal thresh- TTVR potentially allows treatment of a broader olds of RV function and pulmonary vascular resis- TR patient population, particularly those with pre- tance in patients being considered for TTVR. dictors of tricuspid repair failure and advanced tricuspid disease. In this early experience with EVOQUE transfemoral T A B L E 4 Clinical Outcomes at 30-Day Follow-Up (n ¼ 25) TTVR, we observed significant improvements in Mortality NYHA functional class, signs of right-sided HF, and Myocardial infarction 0 (0) biochemical indexes of hepatic congestion, with a Stroke 0 (0) subset of patients requiring fewer diuretic agents at Conversion to surgery 0 (0) 30-day follow-up. As expected, RV function was Reintervention 0 (0) slightly reduced at follow-up, but this was offset by Heart failure hospitalization 0 (0) significant reductions in pre-load and RV volumes Major bleeding 3 (12) with evidence of reverse remodeling by echocardio- Conduction abnormality requiring pacemaker 2 (8) graphic and CT assessment. Importantly, clinically Dialysis 1 (4) significant afterload mismatch was uncommon in this patient cohort, likely because of avoidance of TTVR in Values are n (%). 0 (0) Fam et al. JACC: CARDIOVASCULAR INTERVENTIONS VOL. 14, NO. 5, 2021 MARCH 8, 2021:501–11 EVOQUE Transfemoral TTVR for Severe TR F I G U R E 4 CT Analysis of RV Volumes (A) Baseline computed tomographic (CT) volumetric analysis indicating right ventricular (RV) diastolic volume of 228 cm3. (B) Follow-up CT imaging at 3 months indicating reduction in RV diastolic volume to 168 cm3. Our results are notable for an absence of mortality and other major adverse outcomes acutely and at 30- timing of valve intervention, and the relative roles of TTVr and TTVR. day follow-up, particularly given the compassionate- The main complications of EVOQUE transfemoral use cohort treated. In comparison, the TriValve TTVR in the present series were valve reintervention registry reported 30-day mortality of 3.6% in patients in 4%, new conduction abnormalities requiring per- predominantly treated with transcatheter tricuspid manent pacemaker implantation in 8%, and major valve repair (TTVr) devices, with 2.8% mortality in bleeding in 12%. The patient who required acute SA- those treated with tricuspid leaflet repair (7,8). The PIEN 3 valve-in-valve reintervention had a low valve early compassionate-use experience with TTVR using implantation in the setting of a small right ventricle the Navigate device with access mainly by mini- and entrapment of the EVOQUE anchors in the ven- thoracotomy reported in-hospital mortality of 10% tricular trabeculations and chordal arcades near the (13), similar to that reported in recent studies of sur- tips of the papillary muscles. The atrioventricular gical tricuspid valve replacement (5,6). We used a node is in close proximity to the anteroseptal percutaneous, transfemoral approach, which likely commissure of the tricuspid valve, and it is likely that contributed to the safety of the procedure compared the observed conduction abnormalities resulted from with other vascular or surgical access routes, as has either direct compression by the valve frame or ven- been transfemoral tricular anchors. Of note, 1 patient had right bundle transcatheter aortic valve replacement (23). Only a branch block at baseline, while the other had normal small fraction (<5%) of patients with TR are offered conduction. Future iterations in device design along surgery, and they represent a highly selected popu- with improved CT valve-sizing algorithms may lation (18). Compared with patients undergoing reduce the risk for atrioventricular block and subse- tricuspid surgery, patients considered for trans- quent pacemaker implantation. The observed major catheter tricuspid intervention are older, with a bleeding events all occurred in the setting of thera- greater burden of comorbidities and advanced HF peutic anticoagulation with warfarin in combination (7,8). Furthermore, such patients are often not can- with aspirin. Notably, 20% of patients instead didates for TTVr, because of advanced tricuspid dis- received direct oral anticoagulant agents (the major- ease, making TTVR potentially generalizable to a ity of these patients received apixaban) and had larger subset of patients. Analogous to surgical ap- normal valve function and stable gradients at short- proaches to TR, TTVr is likely preferred in earlier term follow-up. Avoidance of combination therapy stages of the disease, before large coaptation gaps and/or use of direct oral anticoagulant agents may and/or severe tethering develop, with TTVR reserved reduce bleeding risk in this comorbid cohort, but the for more advanced disease (5–7,24). Further studies optimal antithrombotic regimen has yet to be are needed to refine patient and device selection, established. previously demonstrated for 509 510 Fam et al. JACC: CARDIOVASCULAR INTERVENTIONS VOL. 14, NO. 5, 2021 MARCH 8, 2021:501–11 EVOQUE Transfemoral TTVR for Severe TR Pacemaker lead–induced TR has an estimated speaker honoraria from Abbott Vascular and Edwards Lifesciences. prevalence of 10% to 25% (25) and is associated with Dr. Ye is a consultant to Edwards Lifesciences, JC Medical, and Cry- the onset of right-sided HF and adverse prognosis oLife. Dr. Moss is a consultant to Edwards Lifesciences. Dr. Hausleiter has received speaker honoraria and research support from Abbott (26,27). In the present study, 36% of patients had Vascular and Edwards Lifesciences; and is a consultant to Abbott pacemaker leads, and all had successful TTVR with Vascular and Edwards Lifesciences. Dr. George is consultant to either no or mild paravalvular TR at the site of the VDyne, CardioMech, Atricure, MitreMedical, Neptune Medical, and lead, with no change in pacemaker function, W.L. Gore. Dr. Nabauer has received speaker honoraria from Abbott Vascular. Dr. Mack is co–principal investigator of the PARTNER including patients who were pacemaker dependent at (Placement of Aortic Transcatheter Valves) 3 trial for Edwards Life- baseline. sciences; is co–principal investigator of the COAPT (Cardiovascular Patients with lead-induced TR are frequently encountered in clinical practice and represent a therapeutic challenge, given the potential risks of lead extraction or tricuspid Outcomes Assessment of the MitraClip Percutaneous Therapy for Heart Failure Patients With Functional Mitral Regurgitation) trial for Abbott; and is study chair of the APOLLO (Transcatheter Mitral Valve surgery. Replacement With the Medtronic Intrepid TMVR System in Patients Furthermore, these patients are usually not candi- With Severe Symptomatic Mitral Regurgitation) trial for Medtronic dates for transcatheter leaflet repair or annuloplasty. (all uncompensated). Dr. Hahn has received speaker fees from Edwards Lifesciences; is a consultant for Abbott Vascular, Boston Thus, TTVR may represent an ideal solution for many Scientific, Gore & Associates, and Medtronic; holds equity with such patients, who often have no other therapeutic Navigate; and is the chief scientific officer for the Echocardiography options. Core Laboratory at the Cardiovascular Research Foundation for STUDY LIMITATIONS. The major limitations of our industry compensation. Dr. Webb is a consultant to and has received multiple industry-sponsored trials, for which she receives no direct report include small sample size, observational design, and a lack of standardized protocols for patient management. In addition, clinical and echocar- research funding from Edwards Lifesciences, Abbott Vascular, Boston Scientific, Becton Dickinson, and ViVitro Medical. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose. diographic results were site reported, without core laboratory adjudication. Furthermore, these out- ADDRESS FOR CORRESPONDENCE: Dr. Neil P. Fam, comes are from expert, high-volume centers familiar Division of Cardiology, St. Michael’s Hospital, 30 with transcatheter tricuspid intervention and thus Bond Street, Toronto, Ontario M5B 1W8, Canada. may not be generalizable to less experienced centers. E-mail: [email protected]. CONCLUSIONS PERSPECTIVES This first-in-human experience evaluating percutaneous, transfemoral TTVR with the EVOQUE system demonstrated high technical success, excellent WHAT IS KNOWN? TR is associated with significant morbidity and mortality, and many patients are not candidates for surgery or TTVr. safety, and significant clinical improvement in patients with severe TR and HF. Larger studies with WHAT IS NEW? In this compassionate-use experi- long-term follow-up are needed to confirm these ence, EVOQUE transcatheter tricuspid replacement initial promising results and further define patient demonstrated high technical success, acceptable selection criteria, timing of intervention, and the safety, and significant clinical improvement. impact of EVOQUE tricuspid valve replacement on WHAT IS NEXT? Large prospective studies are clinical outcomes. needed to determine the impact of EVOQUE trans- FUNDING SUPPORT AND AUTHOR DISCLOSURES catheter tricuspid replacement on long-term clinical outcomes. Dr. Fam has received speaker honoraria from Abbott Vascular; and is a consultant to Edwards Lifesciences. Dr. von Bardeleben received REFERENCES 1. Nath J, Foster E, Heidenreich PA. Impact of tricuspid regurgitation on long-term survival. J Am Coll Cardiol 2004;43:405–9. 2. Topilsky Y, Maltais S, Medina Inojosa J, et al. Burden of tricuspid regurgitation in patients diagnosed in the community setting. J Am Coll Cardiol Img 2019;12:433–42. 3. Puls M, Lubos E, Boekstegers P, et al. One-year outcomes and predictors of mortality after MitraClip therapy in contemporary clinical practice: results from the German transcatheter mitral valve interventions registry. Eur Heart J 2016;37:703–12. 4. Wang N, Fulcher J, Abeysuriya N, et al. Tricuspid regurgitation is associated with increased mortality independent of pulmonary pressures and right heart failure: a systematic review and meta-analysis. Eur Heart J 2019;40: 476–84. 5. Alqahtani F, Berzingi CO, Aljohani S, Hijazi M, Al-Hallak A, Alkhouli M. Contemporary trends in the use and outcomes of surgical treatment of Fam et al. JACC: CARDIOVASCULAR INTERVENTIONS VOL. 14, NO. 5, 2021 MARCH 8, 2021:501–11 tricuspid regurgitation. J Am Heart Assoc 2017;6: e007597. 6. Zack CJ, Fender EA, Chandrashekar P, et al. National trends and outcomes in isolated tricuspid valve surgery. J Am Coll Cardiol 2017; 70:2953–60. 7. Taramasso M, Alessandrini H, Latib A, et al. Outcomes after current transcatheter tricuspid valve intervention: mid-term results from the international TriValve registry. J Am Coll Cardiol Intv 2019;12:155–65. 8. Mehr M, Taramasso M, Besler C, et al. 1-Year outcomes after edge-to-edge valve repair for symptomatic tricuspid regurgitation: results from the TriValve registry. J Am Coll Cardiol Intv 2019; 12:1451–61. 9. Fam NP, Braun D, von Bardeleben RS, et al. Compassionate use of the PASCAL transcatheter valve repair system for severe tricuspid regurgitation: a multicenter, observational, first-inhuman experience. J Am Coll Cardiol Intv 2019; 12:2488–95. 10. Besler C, Orban M, Rommel KP, et al. Predictors of procedural and clinical outcomes in patients with symptomatic tricuspid regurgitation undergoing transcatheter edge-to-edge repair. J Am Coll Cardiol Intv 2018;11:1119–28. 11. Navia JL, Kapadia S, Elgharably H, et al. Firstin-human implantations of the navigate bioprosthesis in a severely dilated tricuspid annulus and in a failed tricuspid annuloplasty ring. Circ Cardiovasc Interv 2017;10:e005840. 12. Hahn RT, George I, Kodali SK, et al. Early single-site experience with transcatheter tricuspid valve replacement. J Am Coll Cardiol Img 2019;12:416–29. EVOQUE Transfemoral TTVR for Severe TR 13. Hahn RT, Kodali S, Fam NP, et al. Initial multicenter experience of transcatheter tricuspid valve replacement for treating severe tricuspid regurgitation. J Am Coll Cardiol Intv 2020;13:2482–93. tricuspid regurgitation: 6-month outcomes of the TRILUMINATE single-arm study. Lancet 2019;394: 2002–11. 14. Webb J, Hensey M, Fam N, et al. Transcatheter mitral valve replacement with the transseptal 22. Karam N, Mehr M, Taramasso M, et al. Value of echocardiographic right ventricular and pulmonary pressure assessment in predicting transcatheter EVOQUE system. J Am Coll Cardiol Intv 2020;13: 2418–26. tricuspid repair outcome. J Am Coll Cardiol Intv 2020;13:1251–61. 15. Fam NP, Ong G, Deva DP, et al. Transfemoral transcatheter tricuspid valve replacement. J Am Coll Cardiol Intv 2020;13:e93–4. 23. Blackstone EH, Suri RM, Rajaswaran J, et al. Propensity-matched comparisons of clinical out- 16. Stone GW, Adams DH, Abraham WT, et al. Clinical trial design principles and endpoint definitions for transcatheter mitral valve repair and replacement: part 2: endpoint definitions: a consensus document from the Mitral Valve Academic Research Consortium. Eur Heart J 2015;36: 1878–91. 17. Hahn RT, Zamorano JL. The need for a new tricuspid regurgitation grading scheme. Eur Heart J Cardiovasc Imaging 2017;18:1342–3. 18. Axtell AL, Bhambhani V, Moonsamy P, et al. Surgery does not improve survival in patients with isolated severe tricuspid regurgitation. J Am Coll Cardiol 2019;74:715–25. 19. Taramasso M, Benfari G, van der Bijl P, et al. Transcatheter versus medical treatment of patients with symptomatic severe tricuspid regurgitation. J Am Coll Cardiol 2019;74:2998–3008. 20. Cai S, Bowers N, Dhoot A, et al. Natural history of severe tricuspid regurgitation: outcomes after transcatheter tricuspid valve intervention compared to medical therapy. Int J Cardiol 2020; 320:49–54. 21. Nickenig G, Weber M, Lurz P, et al. Transcatheter edge-to-edge repair for reduction of comes after transapical or TF transcatheter aortic valve replacement: a Placement of Aortic Transcatheter Valves (PARTNER)-1 trial substudy. Circulation 2015;131:1989–2000. 24. Ho EC, Ong G, Fam NP. Transcatheter tricuspid valve intervention: a practical algorithm for patient selection. Curr Opin Cardiol 2019;34: 164–72. 25. Al-Bawardy R, Krishnaswamy A, Bhargava M, et al. Tricuspid regurgitation in patients with pacemakers and implantable cardiac defibrillators: a comprehensive review. Clin Cardiol 2013;36: 249–54. 26. Delling FN, Hassan ZK, Piatkowski G, et al. Tricuspid regurgitation and mortality in patients with transvenous permanent pacemaker leads. Am J Cardiol 2016;117:988–92. 27. Hoke U, Auger D, Thijssen J, et al. Significant lead-induced tricuspid regurgitation is associated with poor prognosis at long-term follow-up. Heart 2014;100:960–8. KEY WORDS EVOQUE, transcatheter tricuspid valve replacement, tricuspid regurgitation 511