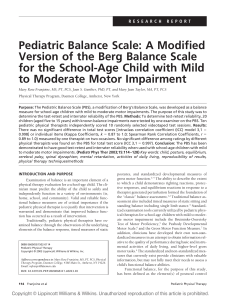
See discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/12649950 Flow Cytometric Immunophenotypic Characterization of Pediatric and Adult Minimally Differentiated Acute Myeloid Leukemia (AML-M0) Article in American Journal of Clinical Pathology · March 2000 DOI: 10.1309/2FYJ-00BE-R8N0-HMPQ · Source: PubMed CITATIONS READS 36 171 9 authors, including: Pauline M. Chou Md Northwestern University 146 PUBLICATIONS 4,142 CITATIONS SEE PROFILE Some of the authors of this publication are also working on these related projects: Midline NUT Carcinoma View project All content following this page was uploaded by Pauline M. Chou Md on 05 April 2016. The user has requested enhancement of the downloaded file. Hematopathology / PEDIATRIC AND ADULT AML-M0 Flow Cytometric Immunophenotypic Characterization of Pediatric and Adult Minimally Differentiated Acute Myeloid Leukemia (AML-M0) Patricia K. Kotylo, MD,1 In-Sook Seo, MD,1 Franklin O. Smith, MD,1 Nyla A. Heerema, PhD,1 Naomi S. Fineberg, PhD,1 Kathy Miller, MD,1 Marianne E. Greene, MD,2 Pauline Chou, MD,2 and Attilio Orazi, MD3 Key Words: Minimally differentiated acute myeloid leukemia; Pediatric; Adult; Immunophenotyping Abstract We reviewed the clinicopathologic and immunophenotypic profiles of 7 pediatric and 11 adult minimally differentiated acute myelogenous leukemias (AML-M0). We also compared and evaluated myeloperoxidase in leukemic blasts using standard cytochemical and polyclonal antibody immunohistochemical stains. No distinctive clinical findings were noted in either patient group; however, thrombocytopenia typically was more prominent in adults. Adult AML-M0 also was associated with an immature myeloid profile (CD34+, terminal deoxynucleotidyl transferase positive, CD13+, and CD33+), in contrast with pediatric AML-M0, which usually lacked terminal deoxynucleotidyl transferase or CD34 but expressed bright CD33 with weak or negative CD13. Coexpression of the T-cell–associated antigen CD7 was observed in both groups. Antibody immunohistochemical stains were more sensitive than cytochemical stains for detection of myeloperoxidase activity and a useful adjunct for establishing a diagnosis of myeloid leukemia in paraffin-embedded marrow tissues. Minimally differentiated acute myeloid leukemia (AMLM0) is a rare form of acute myeloid leukemia constituting approximately 2% to 3% of acute myelogenous leukemias. The 1991 French-American-British (FAB) group criteria for AML-M0 include1 less than 3% blasts that are positive for Sudan black B (SBB), myeloperoxidase, or both and expression of myeloid associated markers, such as CD13 or CD33, with absence of lymphoid antigens. AML-M0 blasts have been described as immature and agranular and frequently lack morphologic features of a specific cell lineage.2 Confirmation of the myeloid origin of AML-M0 may be accomplished with immunophenotyping and immunologic or ultrastructural peroxidase studies. The FAB study group acknowledged that some lymphoid associated antigens, such as CD2 or CD7, may be expressed in a proportion of AML-M0.1 However, no study to date has evaluated and compared complete immunophenotypic profiles in pediatric and adult AML-M0. Previous studies also lack correlation of routine cytochemical and immunoperoxidase stains for myeloperoxidase with flow cytometric immunophenotyping in well-characterized AML-M0. We reviewed and compared the immunophenotypic and cytogenetic profiles of 7 pediatric and 11 adult cases of AML-M0. We also evaluated standard cytochemical myeloperoxidase stains of marrow aspirate smears and an immunohistochemical stain for myeloperoxidase (aMPX) applied to the bone marrow samples in these same cases. Materials and Methods We reviewed 243 cases of adult AML at University Hospital (Indianapolis, IN) during a 5-year period and found © American Society of Clinical Pathologists Am J Clin Pathol 2000;113:193-200 193 Kotylo et al / PEDIATRIC AND ADULT AML-M0 ❚Table 1❚ Clinicopathologic Findings at Diagnosis for Patients With Acute Myeloid Leukemia (M-0)* Case No./ Sex/Age Adult 1/M/80 2/M/84 3/M/58 4/M/55 5/F/58 6/F/31 7/M/60 8/M/71 9/M/60 10/M/63 11/M/79 Pediatric 1/M/14 2/M/12 3/M/6 mo 4/F/6 mo 5/F/8 mo 6/F/2 mo 7/M/15 WBC Count × 109/L/ (× Hemoglobin % Blasts) (g/L) Platelet Count × 109/L) (× Bone Marrow/ % Blasts Cytochemical Stains aMPX (%) Cytogenetics 7.9/60 6.7/14 35.6/75 19.3/70 1.0/2 9.5/54 9.4/42 1.8/1 18.6/50 100 74 95 86 102 92 96 90 83 19 48 52 16.7 157 72 20 52 65 50 95 100 100 60 90 95 80 90 – – – – – – 2% MPX+ – 2% SBB+ 2 – 3 ND 7 10 3 ND 15 –Y,del(6) Normal chromosomes Normal chromosomes Normal chromosomes +8 Multiple anomalies Dicentric (7;20)(p11;p11) +8 +13 38.3/79 1.2/24 66 95 58 59 95 71 PAS+ PAS+ 10 – +13 +13 19.6/43 105 476 65 – 10 +13 1.9/2 19.9/30 6.5/1 10.0/3 40.0/40 28.6/87 62 103 74 62 82 54 155 204 211 364 50 53 94 92 62 32 60 85 PAS+ 3% MPX+ – – – PAS+ ND ND – 2 – – Normal Multiple anomalies t(10;11)(p11.2;q23) No metaphases present† inv(X);(p11.4q24) t(11,19)(q23;p13.3) Previous Disease No No No No No No No No Hodgkin disease, stage IA No Prostate cancer Selective IgA deficiency No No No No No No aMPX, antibody immunohistochemical stains; AWOD, alive without disease; AWD, alive with disease; CNS, central nervous system; DOD, died of disease; MPX, myeloperoxidase; ND, not done; PAS, periodic acid–Schiff; SBB, Sudan black B; +, positive; –, negative. * Age is given in years unless otherwise stated. For all patients, bone marrow examination revealed hypercellularity. Conversions to traditional units of measure are as follows: × 103/µL). WBC count, divide by 0.001 (/µL); hemoglobin, divide by 10 (g/dL); platelet count, divide by 1.0 (× † Relapse at 6 months, t(10;11)(p15;q23). 11 cases (4.5%) that fulfilled the FAB criteria for AML-M0; 90 cases of pediatric AML were reviewed for a similar period at Riley Hospital for Children (Indianapolis) and Children’s Memorial Hospital (Chicago, IL). Seven pediatric cases (8%) also fulfilled the FAB criteria for AML-M0. May-Grünwald-Giemsa–stained bone marrow smears were reviewed for all cases to confirm the original diagnosis. A minimum of 30% marrow blasts was required for inclusion in the study. Cytochemical stains of bone marrow aspirates were reviewed and included myeloperoxidase (cMPX), Sudan black B (SBB), alpha-naphthyl acetate esterase, alpha-naphthyl butyrate esterase, and periodic acid–Schiff stains (Sigma, St Louis, MO). Bone marrow trephine biopsy specimens were fixed in B-5 for up to 6 hours, decalcified using 10% nitric acid for 2 hours, and embedded in paraffin. Four-mm-thick sections were dried on polylysine-coated glass slides at 37°C overnight, deparaffinized by serial passages in xylene and graded alcohol series, and rehydrated in distilled water. H&E and Gomori reticulin silver stains were performed routinely on all samples. Immunohistochemical staining of the bone marrow biopsy specimens for myeloperoxidase was performed as previously reported.3 Briefly, deparaffinized slides were covered with goat serum for 20 minutes, blotted, 194 Am J Clin Pathol 2000;113:193-200 and incubated overnight at 4°C with negative control serum and the primary antibody, an antihuman myeloperoxidase polyclonal antibody that reacts with neutrophil precursor cells and granulocytes 4 (Dako, Carpinteria, CA). The primary antibody was stained with biotin-conjugated goat antimouse antibody (30 minutes; Kirkegaard and Perry Laboratories, Gaithersburg, MD) and then with a peroxidaseconjugated streptavidin (30 minutes; Kirkegaard and Perry). The enzyme was developed with 3,3´-diaminobenzidine (Sigma). Immunohistochemical results were expressed as a percentage of positively stained cells of the total number of blast cells evaluated on a bone marrow biopsy section with an artifact-free area of at least 10 mm 2 , as previously described.3 Immunophenotypic analyses were performed on fresh bone marrow aspirates with Profile, Elite (Coulter, Miami, FL) or FACS-Scan (Becton Dickinson, San Jose, CA) flow cytometers. Seven milliliters of lysing reagent (NH4Cl, pH = 7.3) was added to 500 µL of bone marrow. All samples were then stained with the following panel of dual-color monoclonal antibodies directly conjugated to fluorescein isothiocyanate (FITC), phycoerythrin (PE), and peridinin chlorophyll alpha protein: CD45-FITC/CD14-PE, CD7-FITC/HLADRPE, CD33-FITC/CD34-PE, CD15-FITC/CD13-PE, CD3© American Society of Clinical Pathologists Hematopathology / ORIGINAL ARTICLE ❚Table 1❚ (Continued) Extramedullary Leukemia Remission Length of Follow-Up (mo) Outcome Adult No No No No No No No No No No No No Yes Yes Yes Yes Yes Yes 1 2 2 14 42 4 4 8 6 Unknown DOD DOD DOD AWD AWOD AWOD AWD AWOD No No Yes Yes 11 7 AWD AWOD No 7 DOD Yes Yes Yes Yes Yes Yes 10 6 14 9 13 9 AWOD AWD DOD AWOD AWOD AWD Pediatric No No Yes (CNS, skin) Yes (chloroma of iris) No No No FITC/CD16+56-PE, CD2-FITC/CD13-PE, CD11bFITC/CD11c-PE, CD10-FITC/CD19-PE, CD41-PE, CD61FITC, glycophorin-PE (Coulter Immunology, Hialeah, FL), CD19-PE/kappa-FITC, CD19-PE/lambda-FITC (Kallestad, Austin, TX), and terminal deoxynucleotidyl transferase (TdTFITC, Caltag Laboratories, Burlingame, CA). Monoclonal antibodies were dispensed according to the manufacturer’s recommendations or determined with titration for 5 × 105 cells. Leukemic blasts were evaluated for antigen expression using 2 different gating strategies, including forward-angle light scatter vs side scatter in 13 of 18 cases and multiparameter analysis (CD45 vs side scatter) in the remaining cases. Peridinin chlorophyll alpha protein–conjugated CD45 was used with dual-color antibodies for multiparameter analysis.5 A marker was considered positive when 20% or more of the gated blast population stained with an antibody relative to an appropriate isotype control.6 The intensity of antigen brightness also was assessed in all cases by review of the histogram data. Cytogenetic analysis was performed on direct and 24hour unstimulated bone marrow cultures using a trypsinGiemsa banding procedure. Results were reported using the International System for Human Cytogenetic Nomenclature.7 A minimum of 20 analyzed cells was required for a © American Society of Clinical Pathologists diagnosis of normal chromosomes. Clinical outcome and follow-up data were obtained through chart reviews and physician interviews. Comparisons between immunophenotypic profiles were analyzed by using the Fisher exact test. Comparisons between continuous variables, such as WBC counts and platelets, used the Mann-Whitney U test since the data were not distributed normally.8 Results Of 333 cases reviewed, 11 adult and 7 pediatric acute myeloid leukemias fulfilled the FAB criteria for AML-M0. Clinicopathologic findings for both groups are summarized in ❚Table 1❚. The adults were 9 men and 2 women ranging from 31 to 84 years of age (median, 60 years). Two adults had secondary AML after previous therapy for malignant neoplasms. One patient was treated successfully for stage IA Hodgkin disease with chemotherapy and radiation therapy 10 years before the current diagnosis; the second was treated surgically for prostatic carcinoma without chemotherapy 1 year before the diagnosis of leukemia. The remaining 9 adults had de novo AML. There were 4 boys and 3 girls in the pediatric group; 4 of 7 were infants younger than 8 months of age. All children had de novo AML. WBC counts at diagnosis for adults varied from 1,000 to 38,800/µL (1.0-38.8 × 10 9 /L; median, 9,400/µL [9.4 × 109/L]), in contrast with higher WBC counts observed in the pediatric group (median, 19,600/µL [19.6 × 109/L]). Blasts were observed in the peripheral blood specimens of all patients at the time of diagnosis. All patients demonstrated mild to moderate anemia; thrombocytopenia was variable and more prominent in adults (median, 52 × 103/µL [52 × 109/L]) than in children (median, 204 × 103 /µL [204 × 109/L]; P = .020). Leukemic blasts in pediatric and adult cases of AML-M0 usually were medium to large with scant agranular cytoplasm. Nuclei were round to oval with fine chromatin and prominent nucleoli ❚Image 1❚. Routine cytochemical stains for myeloperoxidase and SBB demonstrated less than 3% positivity in leukemic blasts in all cases. Alpha-naphthyl butyrate esterase and alpha-naphthyl acetate esterase stains also were negative; 2 pediatric and 2 adult cases demonstrated focal globular periodic acid–Schiff positivity (Table 1). Immunohistochemical aMPX stains were performed on fixed bone marrow particle sections or biopsy specimens in 9 adults and 5 children (Table 1). The aMPX staining was more sensitive than cMPX in both patient groups. Seven of 9 adult cases demonstrated positive aMPX staining in leukemic blasts varying from 2% to 15%; aMPX staining in 2 of 5 pediatric cases was 2% and 10%, respectively. In 5 Am J Clin Pathol 2000;113:193-200 195 Kotylo et al / PEDIATRIC AND ADULT AML-M0 ❚Table 2❚ Immunophenotypic Findings for Patients With Acute Myeloid Leukemia (M0)* Case No. ❚Image 1❚ (Case 11) Bone marrow aspirate of adult with acute myeloid leukemia (M-0). Leukemic blasts with prominent nucleoli and scant cytoplasm with minimal granulation (Wright-Giemsa, ×1,000). adults and 2 children in whom cMPX stains were entirely negative, aMPX staining was observed. Immunophenotypic profiles are summarized in ❚Table 2❚. Statistically significant differences were observed in CD34 (P = .003) and TdT (P = .011) expression in pediatric vs adult AML-M0. Adult AML-M0 was characterized by an immature myeloid profile and frequently expressed CD34 and TdT in combination with the myeloid antigens CD33, CD13, or both. Blasts in adult cases demonstrated bright expression of CD34 (11/11), CD13 (10/11), CD33 (8/11), and HLA-DR (10/11); CD33 and CD13 were expressed in 7 cases. Nuclear TdT was positive in 6 of 10 cases and was weak in contrast with prominent expression of CD34 and myeloid antigens. Four of 11 adult AML-M0 samples also were positive for CD7. The CD7 activity observed in 3 of these cases was less prominent than myeloid antigen expression; the fourth case displayed equal intensity of CD7 and myeloid antigens on leukemic blasts. The latter case (case 6), a CD7+ adult case of AML-M0, which was cMPX negative but aMPX positive, was evaluated with multiparameter analysis to exclude lymphocytes from the analysis. CD15 (5/9) and CD11b or CD11c (6) were expressed in adult cases of AML-M0 and were of variable intensity. In contrast with the adult group, leukemic blasts of pediatric cases of AML-M0 typically displayed a more mature myeloid phenotypic profile ❚ Figure 1❚. TdT studies were negative in all 6 pediatric cases of AML-M0 evaluated for 196 Am J Clin Pathol 2000;113:193-200 Adult 1 2 3 4 5 6 7 8 9 10 11 Pediatric 1 2 3 4 5 6 7 Gate† CD45 HLA-DR TdT CD34 CD13 1 1 1 1 1 2 1 2 1 1 2 98 80 74 93 95 99 98 73 94 93 73 86 81 81 91 12 30 54 87 82 37 96 6 63 47 7 87 4 52 2 ND 15 56 84 88 71 43 69 98 89 92 92 92 95 68 65 62 38 32 81 13 81 82 24 65 1 1 1 2 2 1 1 95 82 98 98 72 96 97 62 82 97 88 90 6 91 4 1 ND 2 8 2 2 81 1 1 86 2 2 1 50 6 1 25 48 45 37 Cyto µ, cytoplasmic mu heavy chain; ND, not done; SIg, surface immunoglobulin; TdT, terminal deoxynucleotidyl transferase. * Data are given as percentage of positivity. † 1 indicates forward angle light scatter vs side scatter; 2, CD45 vs side scatter. this marker; CD34 activity was present in only 2 cases. Bright CD33 positivity was observed in all pediatric AMLM0 samples and was associated with negative or relatively dim CD13 in 5 of 7 cases. Weak CD7 coexpression was observed in 4 pediatric cases of AML-M0, 1 of which also was aMPX positive. CD15 was positive in 5 of 6 cases; CD11b and CD11c were positive in 2 of 3 cases tested for these antigens. All pediatric and adult cases of AML-M0 tested were negative for CD3, CD14, CD19, CD20, CD10, CD41/CD61 and surface immunoglobulin expression. One pediatric and 1 adult case of AML-M0 displayed CD16/56 activity. Cytogenetic findings are summarized in Table 1. Three adult and 1 pediatric case demonstrated trisomy 13 as the sole abnormality. Trisomy 8 was present in 2 adults. An 11q23 breakpoint was present in 2 children at diagnosis. A third infant (case 5), whose cytogenetic testing was unsuccessful at diagnosis, had an 11q23 breakpoint at relapse 6 months later. Only 2 of all cases of AML-M0 had multiple cytogenetic abnormalities. Clinical outcomes are summarized in Table 1. None of the adult cases demonstrated extramedullary leukemic infiltrates during the course of disease. One adult refused treatment and was lost to follow-up 1 month after diagnosis. The remaining 10 patients were treated with different multiagent chemotherapy protocols. Two adults did not achieve remission and died of disease 2 months after diagnosis; a third achieved remission but experienced relapse 6 months later © American Society of Clinical Pathologists Hematopathology / ORIGINAL ARTICLE ❚Table 2❚ (Continued) CD2 CD3 CD14 CD15 13 5 10 50 15 68 96 6 18 10 53 18 6 10 12 17 ND 35 1 15 9 2 12 3 8 5 12 ND 6 1 4 5 3 7 6 1 4 2 1 2 1 6 4 2 7 54 32 64 16 17 40 25 ND ND 3 7 14 15 47 4 77 86 37 9 ND ND 14 34 22 80 15 41 29 50 ND ND ND ND 1 2 2 ND ND 3 1 ND 60 5 2 1 5 1 1 2 2 1 3 1 1 ND ND ND ND ND 1 1 1 ND ND 2 3 5 8 1 1 ND 1 1 ND 3 ND ND ND ND 1 ND 1 1 1 1 ND 1 2 2 5 4 3 1 7 1 4 2 1 4/2 9/1 6/ND 7/ND 3/ND 11/ND 1/2 1/1 ND/1 ND 19/ND 25 14 60 3 19 37 42 27 1 ND ND 1 13 38 5 1 1 ND 1 6 4 5 4 1 1 2 4 1 ND 5 65 83 38 73 77 ND ND ND ND 57 8 50 ND ND ND ND 79 3 74 2 77 1 ND 1 2 1 1 1 1 1 1 2 1 15 1 1 3 6 2 2 3 1 1 ND 1 5 2 1 1 ND 1 1 1 1 5 1 11 5 2 5 15 3/5 1/1 1/1 7/ND 1/1 2/3 1/1 A 64 50 A Cyto µ CD20 SIg CD19 CD41/61 D 50 C 50 Count B 90 LS CD11b CD11c CD16/56 CD10 Count Adult 6 72 23 93 10 98 83 45 53 60 7 Pediatric 77 85 93 84 78 94 58 CD7 Count CD33 B 0 .1 1,000 CD45 B 0 .1 1,000 CD45 .1 CD34 1,000 CD33 1,000 0 0 0 .1 H 24 G 50 Count A CD13 1,000 Count F 50 90 LS .1 CD34 E 64 0 0 1,000 Count 0 .1 .1 CD13 1,000 .1 1,000 CD33 ❚Figure 1❚ Multiparameter histogram flow cytometric analysis. A-D, Adult acute myeloid leukemia (AML M-0). E-H, Pediatric AML M-0. Note leukemic blasts (gate A) lack CD34 in the pediatric case, in contrast to CD34+ in the adult case. LS, light scatter. and died of disease 14 months after diagnosis. Seven other patients achieved remission and are alive with (n = 3) or without (n = 4) recurrent disease at follow-up times ranging from 4 to 42 months. Limited follow-up for pediatric cases of AML-M0 ranged from 6 to 14 months. Two patients had extramedullary disease at diagnosis. All were treated with multiagent chemotherapy protocols; 1 received a cord blood transplant (case 6). One patient did not achieve an initial complete remission and died of disease 7 months after diagnosis. The remaining 6 pediatric patients achieved an initial © American Society of Clinical Pathologists complete remission, 5 of whom are alive with or without recurrent disease. Both patient groups included males and females; no specific gender-associated clinicopathologic features were observed in the present study. Discussion Flow cytometric immunophenotyping and/or electron microscopic demonstration of the presence of myeloperoxidase Am J Clin Pathol 2000;113:193-200 197 Kotylo et al / PEDIATRIC AND ADULT AML-M0 often are necessary to confirm the true myeloid nature of AML-M0 and distinguish it from a primitive leukemia of lymphoid origin. Unfortunately, electron microscopic or other ultrastructural studies frequently are labor intensive, cumbersome, and not readily available at many institutions. Immunophenotyping and cytochemical or immunocytochemical stains are used more frequently for determination of cell lineage.9,10 The present study is the first to include evaluation and comparison of the clinicopathologic features of pediatric and adult cases of AML-M0 in males and females. It also is the first report, to the best of our knowledge, to compare standard cytochemical with polyclonal antibody immunocytochemical myeloperoxidase stains in a series of well-characterized cases of AML-M0. The first report of a series of AML-M01 consisted of 8 adults and 2 children. All cases were positive for at least 1 of the myeloid antigens, CD13 or CD33. Five cases coexpressed CD7, while nuclear TdT was positive in 1 of 4 tested for this antigen. Ultrastructural myeloperoxidase studies were helpful for confirming myeloid lineage in selected cases. Pediatric phenotypic profiles were not distinguished separately and described in that report.1 Sempere et al11 studied antigen expression by using fluorescent microscopy in 11 adult cases of AML-M0 (9 men, 2 women). All cases expressed CD13 or CD33; CD34 was noted in 3 of 4 cases tested and TdT in 1 of 7. Coexpression of the lymphoid markers, including CD4 and CD7, also was observed in several cases. These authors concluded that these T-cell antigens were not lineage restricted and could be observed on early myeloid cells. Another study12 characterized 25 cases of adult AMLM0 in 13 women and 12 men. These authors also compared standard cMPX stains with monoclonal aMPX tissue stains. They reported all aspirates as cMPX and SBB negative (<3% positivity), but the corresponding methanol-fixed cytospin aspirate materials were aMPX positive in all cases. Five cases also were reported as “faintly” butyrate positive at diagnosis. Flow cytometric immunophenotyping of AML-M0 samples demonstrated a “stem cell” pattern, with TdT and CD34 positivity frequently observed in combination with CD13 or CD33. aMPX positivity was useful for confirming myeloid lineage in 4 cases that were entirely negative for myeloid antigens. Eighty percent of the cases of AML-M0 in that study12 coexpressed at least 1 of the lymphoid-lineage associated antigens, including TdT, CD7, CD4, CD2, CD5, CD10, and CD19. Cytogenetic studies revealed complex karyotypes in 53% of patients with AML-M0, with frequent abnormalities of chromosomes 5, 7, 8, and 13. A poor outcome was reported in these cases of AML-M0 compared with other FAB myeloid subtypes. A recent report13 of AML-M0 consisted of 17 adults, including 10 men and 7 women. These investigators noted a 198 Am J Clin Pathol 2000;113:193-200 similar primitive phenotypic profile and observed TdT and CD34 expression in all cases tested. Positivity for CD13, CD33, or both also was observed in all 17 samples, frequently in association with lymphoid markers, such as CD7, CD19, CD20, and CD22. These lymphoid-associated markers were relatively dim or weak in contrast with bright myeloid antigen activity. Abnormal clonal karyotypes were found in 6 of 14 cases; abnormalities of chromosomes 7 and 13 were the most common finding. The aMPX stains of 12 bone marrow aspirates or biopsy specimens demonstrated a lower incidence of peroxidase activity than in previously described reports, with significant staining observed in only 2 of 12 samples tested. An isolated study14 including 3 pediatric cases of AMLM0 described weak or negative TdT and CD34 antigen activity. However, most AML-M0 studies15-18 consist of limited numbers of adults with few or no pediatric patients. The morphologic features of AML-M0 were similar in both of our patient groups. Bone marrow specimens typically were hypercellular and replaced with primitive agranular blasts. Significant cytologic dysplasia was not observed in peripheral blood or bone marrow samples in the present series. The phenotypic profiles observed in adults were similar to those noted in previous reports and consisted predominantly of an “immature” myeloid pattern with frequent expression of HLA-DR, CD34, and nuclear TdT in combination with myeloid antigens CD33, CD13, or both. Weaker coexpression of the T-cell antigens CD7 or CD2 was observed in 4 of 11 cases (36%). In contrast, the pediatric cases demonstrated a more mature myeloid profile. All cases lacked TdT and only 2 expressed CD34; all were CD33+, while CD13 expression was relatively less prominent or negative. Weaker coexpression of CD7 and or CD2 also was observed in 4 of 7 cases (57%). No coexpression of other lymphoid antigens, including CD3, CD10, CD19, CD20, or surface immunoglobulin, was detected in any patient in our study. Standard cytochemical stains were performed on all cases and revealed negative or weak (<3%) myeloperoxidase or SBB reactivity. The aMPX staining performed with a polyclonal rabbit antihuman antibody on paraffin-embedded bone marrow particle preparation or biopsy specimen was more sensitive than cMPX staining of bone marrow tissues. Seven cases in our series (5 adults, 2 children) that were negative with cMPX stains demonstrated positive staining using the aMPX technique. These results are similar to those noted in previous studies that have suggested immunologic stains may be a more sensitive method for myeloperoxidase detection than cMPX.4,19-22 The polyclonal aMPX used in the present retrospective study may be used on fixed bone marrow material rather than methanol-fixed cytospin material. Flow cytometric studies in the present series were performed using a whole-blood lysis technique and, in many instances, multiparameter analysis with selective gating on leukemic blasts. © American Society of Clinical Pathologists Hematopathology / ORIGINAL ARTICLE Leukemic cells were stained with a consistent panel of monoclonal antibodies conjugated with similar fluorochromes throughout the study. The combination of flow cytometric analysis, cytochemical stains, and immunohistochemical studies described herein was particularly useful for cases in which only fixed bone marrow–embedded tissue was available for study or for confirming myeloid lineage in leukemias that coexpressed various lymphoid antigens. Cytogenetic abnormalities were detected in 8 of 11 adult cases and 4 of 5 pediatric cases of AML-M0. One additional pediatric case for which the cytogenetic analysis was unsuccessful at diagnosis had an abnormal karyotype at relapse. In our series of patients with AML-M0, trisomy 13 was present in 3 older men and one 14-year-old boy; in all 4 cases, this was the sole abnormality, which is consistent with findings of previous reports.23,24 In contrast with previous studies that have reported frequent complex abnormalities in AML-M0, only 2 of the present cases (1 adult and 1 pediatric) had complex abnormalities.25 One adult and 3 pediatric cases demonstrated breakpoints at 11q23. This breakpoint frequently is observed in monoblastic leukemia, and its presence in these cases is consistent with previous observations that some cases of AML-M0 may, in fact, represent primitive monoblastic proliferations. The adult group consisted primarily of men, while the pediatric group consisted of both boys and girls. Statistically significant clinicopathologic gender differences were not observed in the present pilot study. Limited clinical follow-up and a small sample preclude analysis of overall survival in our patient groups. However, the different phenotypic profiles observed in children and adults in the present series suggest that AML-M0 may represent a different disease process in these patient populations. The present study also revealed that polyclonal aMPX staining of fixed bone marrow tissues may be useful for confirming myeloid lineage, especially in cases with negative cMPX or lymphoid antigen coexpression. Additional multicenter cooperative group studies26 are necessary to determine the clinical significance of AML-M0 in children and adults. From the 1Indiana University School of Medicine, Indianapolis, 2Children’s Memorial Hospital, Chicago, IL, and 3College of Physicians and Surgeons of Columbia University, New York, NY. Address reprint requests to Dr Kotylo: Riley Hospital for Children, Dept of Pathology and Laboratory Medicine, Room 0959, 702 N Barnhill Dr, Indianapolis, IN 46202-5200. References 1. Bennett JM, Catovsky D, Daniel MT, et al. Proposal for the recognition of minimally differentiated acute myeloid leukaemia (AML-M0). Br J Haematol. 1991;78:325-329. © American Society of Clinical Pathologists 2. Foucar K. Bone Marrow Pathology. Chicago, IL: ASCP Press; 1995:193-194. 3. Orazi A, Cattoretti G, Schiro R, et al. Recombinant human interleukin-3 and recombinant human granulocytemacrophage colony-stimulating factor administered in-vivo after high dose cyclophosphamide cancer-chemotherapy: effect on the hematopoiesis and micro environment in the human bone marrow. Blood. 1992;79:2610-2619. 4. Pinkus G, Pinkus J. Myeloperoxidase: a specific marker for myeloid cells in paraffin sections. Mod Pathol. 1991;4:733-741. 5. Borowitz MJ, Guenther KL, Shultz KE, et al. Immunophenotyping of acute leukemia by flow cytometric analysis: use of CD45 and right-angle light scatter to gate on leukemic blasts in three-color analysis. Am J Clin Pathol. 1993;100:534-540. 6. Carey JL, Hanson CA. Flow cytometric analysis of leukemia. In: Keren DF, Hanson CA, Hurtubise PE, eds. Flow Cytometry and Clinical Diagnosis. Chicago, IL: ASCP Press; 1994:197-203. 7. Mitelman F, ed. An International System for Human Cytogenetic Nomenclature. Basel, Switzerland: S. Karger; 1995. 8. Lee ET. Statistical Methods for Survival Data Analysis. Belmont, CA: Lifetime Learning Publications; 1980:129-130, 299-335. 9. Jennings CD, Foon KA. Recent advances in flow cytometry: application to the diagnosis of hematologic malignancy. Blood. 1997;90:2863-2892. 10. van’t Veer MB. The diagnosis of acute leukemia with undifferentiated or minimally differentiated blasts. Ann Hematol. 1992;64:161-165. 11. Sempere A, Jarque I, Guinot M, et al. Acute myeloblastic leukemia with minimal myeloid differentiation (FAB AML-M0): a study of eleven cases. Leuk Lymphoma. 1993;12:103-108. 12. Vendetti A, del Poeta G, Buccisano F, et al. Minimally differentiated acute myeloid leukemia (AML-M0): comparison of 25 cases with other French-American-British subtypes. Blood. 1997;89:621-629. 13. Cohen P, Hoyer J, Kurtin P, et al. Acute myeloid leukemia with minimal differentiation: a multiple parameter study. Am J Clin Pathol. 1998;109:32-38. 14. Praxedes MK, De Oliveira LZ, Pereira WD, et al. Monoclonal antibody anti-MPO is useful in recognizing minimally differentiated acute myeloid leukemia. Leuk Lymphoma. 1994;12:233-239. 15. Brito-Babapulle F, Pullon H, Layton DM, et al. Clinicopathologic features of acute undifferentiated leukaemia with a stem cell phenotype. Br J Haematol. 1990;76:210-214. 16. Campos L, Guyotat D, Archimbaud E, et al. Surface marker expression in adult acute myeloid leukaemia: correlations with initial characteristics, morphology and response to therapy. Br J Haematol. 1989;72:161-166. 17. Khalidi H, Medeiros J, Chang KL, et al. The immunophenotype of adult acute myeloid leukemia: high frequency of lymphoid antigen expression and comparison of immunophenotype, French-American-British classification, and karyotype abnormalities. Am J Clin Pathol. 1998;109:211-220. 18. Ball ED, Davis RB, Griffin JD, et al. Prognostic value of lymphocyte surface markers in acute myeloid leukemia. Blood. 1991;77:2242-2250. 19. Arber DA, Jenkins, KA. Paraffin section immunophenotyping of acute leukemias in bone marrow specimens. Am J Clin Pathol. 1996;106:462-468. Am J Clin Pathol 2000;113:193-200 199 Kotylo et al / PEDIATRIC AND ADULT AML-M0 20. Vander Schoot CE, Daams GM, Pinkster J, et al. Monoclonal antibodies against myeloperoxidase are valuable immunological reagents for the diagnosis of acute myeloid leukemia. Br J Haematol. 1990;74:173-178. 21. Wang JC, Beauregard P, Soamboonsrup P, et al. Monoclonal antibodies in management of acute leukemia. Am J Hematol. 1995;50:188-199. 22. Matutes E, de Oliveira MP, Foron L, et al. The role of ultrastructural cytochemistry and monoclonal antibodies in clarifying the nature of undifferentiated cells in acute leukemia. Br J Haematol. 1988;69:205-211. 23. Pedersen B, Jensen IM. Trisomy 13: a preferentially male chromosome aberration interfering specifically with myeloid proliferation and differentiation? report of a case and review of the literature. Cancer Genet Cytogenet. 1991;57:79-85. 200 Am J Clin Pathol 2000;113:193-200 View publication stats 24. Sreekantaiah C, Baer MR, Morgan S, et al. Trisomy/tetrasomy 13 in seven cases of acute leukemia. Leukemia. 1990;4:781-785. 25. Cuneo A, Ferrant A, Michaux JL, et al. Cytogenetic profile of minimally differentiated (FAB-M0) acute myeloid leukemia: correlation with clinicobiologic findings. Blood. 1995;85:3688-3694. 26. Stasi R, Del Poeta G, Vendetti A, et al. Analysis of treatment failure in patients with minimally differentiated acute myeloid leukemia (AML-M0). Blood. 1994;83:1619-1625. © American Society of Clinical Pathologists