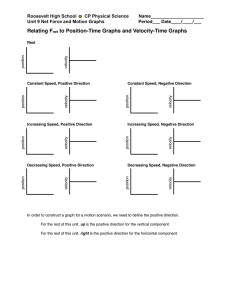
See discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/49814915 Left Atrial Volume Index Over Late Diastolic Mitral Annulus Velocity (LAVi/A′) Is a Useful Echo Index to Identify Advanced Diastolic Dysfunction and Predict Clinical Outcomes Article in Clinical Cardiology · February 2011 DOI: 10.1002/clc.20850 · Source: PubMed CITATIONS READS 8 196 10 authors, including: Hae-Ok Jung Jinsoo Min Seoul St. Mary's Hospital, Catholic University of Korea Catholic University of Korea 164 PUBLICATIONS 739 CITATIONS 41 PUBLICATIONS 253 CITATIONS SEE PROFILE Some of the authors of this publication are also working on these related projects: Cohort Study of Pulmonary Tuberculosis (COSMOTB) View project All content following this page was uploaded by Hae-Ok Jung on 18 December 2017. The user has requested enhancement of the downloaded file. SEE PROFILE Clinical Investigations Left Atrial Volume Index Over Late Diastolic Mitral Annulus Velocity (LAVi/A) Is a Useful Echo Index to Identify Advanced Diastolic Dysfunction and Predict Clinical Outcomes Address for correspondence: Hae-Ok Jung, MD Division of Cardiology, Department of Internal Medicine Seoul St. Mary’s Hospital, College of Medicine The Catholic University of Korea 505 Banpo-Dong, Seocho-Gu Seoul, South Korea [email protected] Hun-Jun Park, MD; Hae Ok Jung, MD; Jinsoo Min, MD; Mahn Won Park, MD; Chan Seok Park, MD; Dong Il Shin, MD; Woo-Seung Shin, MD; Pum Joon Kim, MD; Ho-Joong Youn, MD; Ki-Bae Seung, MD Division of Cardiology, Department of Internal Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, South Korea Background: Combined interpretation of late diastolic mitral annulus velocity (A ) with left atrial volume index (LAVi) may have additional benefits in the assessment of diastolic dysfunction. Hypothesis: The LAVi/A ratio may be useful in the identifying advanced diastolic dysfunction (ADD) and predicting clinical outcomes in patients with dyspnea. Methods: We enrolled 395 consecutive patients hospitalized with dyspnea (New York Heart Association class II–IV) and performed transthoracic Doppler echocardiography and B-type natriuretic peptide (BNP) measurement. LAVi/A values were evaluated in terms of diagnosing ADD and predicting clinical outcome. Results: On the receiver operation characteristic curve analysis for the determination of ADD, the area under the curves of LAVi/A in the entire population was comparable to those of BNP (0.94 vs 0.93, P = 0.845) and mitral E/E (0.94 vs 0.93, P = 0.614) and higher than that of LAVi (0.94 vs 0.87; P = 0.014). A LAVi/A of 4.0 was the best cut-off value to identify ADD. During a median follow-up of 31.9 months (range, 0.3 to 45.7 months), the group with LAVi/A ≥4.0 had a higher incidence of primary composite outcomes (cardiac death and/or rehospitalization for heart failure) than the group with LAVi/A <4.0 (25.0% vs 3.3%, P < 0.001). LAVi/A ≥4.0 was an independent predictor of clinical outcomes (odds ratio, 3.245; 95% confidence interval, 1.386–7.598; P = 0.007). Conclusions: As a new echo index, LAVi/A is a useful parameter to identify ADD and predict clinical outcomes in patients with dyspnea. Introduction The conventional diastolic dysfunction grading system using transmitral Doppler and mitral annular tissue Doppler data is useful in the assessment and prediction of a patient’s symptoms, diagnosis, treatment, and prognosis. Patients with pseudonormal and restrictive physiology have elevated left ventricular (LV) filling pressure, decreased LV compliance, and poorer prognosis compared to those with mild diastolic dysfunction.1 – 3 However, it is impossible to categorize all patients into only 4 categorical grades, and borderline zones exist. The early diastolic transmitral velocity/early diastolic mitral annular velocity ratio (E/E ) and left atrial volume index (LAVi) are well-validated echo indices. E/E correlates well with LV filling pressure and pulmonary capillary wedge pressure (PCWP).4 – 6 LAVi reflects chronic diastolic dysfunction caused by decreased LV compliance.7,8 The authors have no funding, financial relationships, or conflicts of interest to disclose. 124 Clin. Cardiol. 34, 2, 124–130 (2011) Published online in Wiley Online Library (wileyonlinelibrary.com) DOI:10.1002/clc.20850 2011 Wiley Periodicals, Inc. However, there is no echo index that accurately reflects LV compliance and filling pressure simultaneously. We have invented a new echo index, left atrial volume index to late diastolic mitral annular tissue velocity ratio (LAVi/A ). A refers to late diastolic myocardial velocity of passive distension due to left atrial (LA) contraction. As LV compliance is decreased, A is decreased, and LAVi progressively increases.9 The information provided by the A and LAVi parameters may have an additional benefit in the assessment of diastolic dysfunction. In this study, we assessed the clinical usefulness of the LAVi/A ratio to identify advanced diastolic dysfunction (ADD) and predict clinical outcomes in patients with dyspnea. Methods Subjects We enrolled 395 consecutive patients hospitalized with dyspnea (New York Heart Association class II-IV) and performed transthoracic Doppler echocardiography for the evaluation Received: August 7, 2010 Accepted with revision: September 22, 2010 of dyspnea at Seoul St. Mary’s Hospital, Catholic University of Korea, between November 2005 and December 2006. Patients who had significant mitral valve diseases, atrial arrhythmia, congenital heart disease, or a history of cardiac surgery or permanent pacemaker implantation were excluded. Significant mitral valve disease was defined as more than moderate mitral valve stenosis or regurgitation on transthoracic echocardiography. Atrial arrhythmia was defined as atrial fibrillation, atrial flutter, or other documented and/or treated atrial rhythm abnormalities. Patients with renal insufficiency (serum creatinine ≥ 2.5 mg/dL) were also excluded due to potential confounding of plasma B-type natriuretic peptide (BNP) levels. Clinical data were obtained from a comprehensive review of the medical records using established criteria for hypertension, diabetes mellitus, hyperlipidemia, congestive heart failure (CHF), and myocardial infarction. All subjects gave written informed consent to participate in the study. The institutional review board of Seoul St. Mary’s Hospital, Catholic University of Korea, approved the study protocol. Doppler and 2-Dimensional Echocardiography Comprehensive echocardiography was performed using commercially available ultrasound systems (Vivid 7, GE; Vingmed Ultrasound, Horton, Norway; Sequoia 512, Acuson, Mountain View, CA). Standard M-mode and 2-dimensional measurements were taken according to the guidelines of the American Society of Echocardiography.10 LV ejection fraction was measured by the quantitative 2-dimensional biplane modified Simpson method from a 4- and 2-chamber view. LV end-diastolic and LV end-systolic dimensions were measured by M-mode and indexed to body surface area. The following pulsed-wave Doppler measurements were obtained in the apical view with the sample volume at the tip of the mitral valve and pulmonary vein: maximal early (E) and late (A) transmitral velocities, E wave deceleration time, A wave time duration, systolic peak of pulmonary venous flow, diastolic peak of pulmonary venous flow, and peak of atrial reverse flow and its duration. Tissue Doppler measurements were also performed at the septal mitral annulus, and systolic peak velocity (S ), early diastolic tissue velocity (E ), and late diastolic tissue velocity (A ) were obtained. The diastolic functional profile of each patient was categorized into normal, impaired relaxation, pseudonormal, or restrictive physiology (reversible and irreversible) using a previously published and validated method.11 Pseudonormal and restrictive physiologies (reversible and irreversible) were considered as ADD.3 The 2-dimensional maximal LA volume was determined based on the apical 2- and 4-chamber views at end-systole without foreshortening, using a biplane modified Simpson’s method excluding the LA appendage and pulmonary vein confluences. Each LA volume was indexed by body surface area. Digital echocardiographic data containing a minimum of 3 consecutive beats were acquired and transferred to a server for storage and were interpreted by 2 independent cardiologists blinded to each other’s reading. In all patients, LAVi/A was measured as shown in Figure 1 and compared with E/E and LAVi. Figure 1. Representative samples of LA volume index over A (LAVi/A ) in patients with mild diastolic dysfunction (A) and moderate diastolic dysfunction (B). The 2-dimensional maximal left atrial (LA) volume was determined by a biplane modified Simpson’s method based on the apical 2- and 4-chamber views, and each LA volume was indexed by body surface area. Late diastolic tissue velocity (A ) was obtained by tissue Doppler measurements at the septal mitral annulus. LAVi/A was finally calculated in all subjects. Clin. Cardiol. 34, 2, 124–130 (2011) H.- J. Park et al: LAVi/A as a new echo index to predict clinical outcomes Published online in Wiley Online Library (wileyonlinelibrary.com) DOI:10.1002/clc.20850 2011 Wiley Periodicals, Inc. 125 BNP Assay Blood samples were collected in sterile tubes (EDTA) on the same day of echocardiography. In all patients, plasma BNP levels were measured by chemiluminescence immunoassay (Bayer Diagnostics, Tarrytown, NY).12 Clinical Outcomes Participants were followed for a median of 31.9 months (range, 0.3 to 45.7 months) and were monitored on a regular basis. The primary outcome in our study was the composite of cardiac death and/or rehospitalization for CHF, which was defined according to the Framingham critera.13 Statistical Analysis All data are presented as mean ± standard deviation for continuous variables and as frequency percentages for categorical variables. Group comparisons were performed using Student t and analysis of variance tests for continuous variables and χ2 for frequency variables. Using receiveroperator characteristic curve analysis, we acquired the areas under the curves (AUC) of BNP, E/E , LAVi, and LAVi/A for the detection of ADD and then compared them by the method of Hanley and McNeil.14 We divided all patients into 2 groups according to the best cutoff value of LAVi/A and then compared the incidence of clinical outcomes between them using the KaplanMeier survival curve. We also performed Cox proportional hazards uni- and multivariate analyses to acquire the odds ratios of prespecified risk factors, including BNP ≥ 200 pg/mL, E/E ≥15, LAVi ≥34 mL/m2 , and the best cutoff value of LAVi/A for the detection of ADD. Statistical analyses were performed with SPSS version 15.0 (SPSS Inc., Chicago, IL). For all analyses, P < 0.05 was considered significant in identifying independent predictors of clinical outcomes. Results Baseline Characteristics Table 1 reports the baseline characteristics of 395 enrolled patients. Among them, 174 (44.1%) patients had heart failure symptom with NYHA class III or IV. During the admission periods, 93 (23.5%) patients received intravenous diuretics, 33 (8.4%) patients received intravenous inotropes, and 15 (3.8%) patients received mechanical ventilation. Based on conventional diastolic function grading system, the patients were divided into the following groups: normal (n = 21, 5.3%), impaired relaxation (n = 291, 73.7%), pseudonormal (n = 53, 13.4%), and restrictive physiology (reversible and irreversible) (n = 30, 7.6%). As diastolic function grade worsened, LV ejection fraction (LVEF) gradually decreased, and LV mass, E/E , and LAVi gradually increased. LAVi/A was similar between the normal and impaired relaxation group, but it gradually increased in patients with pseudonormal and restrictive physiology. Plasma level of BNP also increased gradually according to the diastolic function grade (Table 2). 126 Clin. Cardiol. 34, 2, 124–130 (2011) H.- J. Park et al: LAVi/A as a new echo index to predict clinical outcomes Published online in Wiley Online Library (wileyonlinelibrary.com) DOI:10.1002/clc.20850 2011 Wiley Periodicals, Inc. Table 1. Baseline Patient Characteristics (N = 395) Clinical Variables Age, y 63.0 ± 13.2 Male gender, n (%) 219 (55.4) Body mass index, Kg/m2 24.4 ± 4.2 Body surface area, m2 1.67 ± 0.19 Hypertension, n (%) 180 (45.6) Diabetes mellitus, n (%) 101 (25.6) Hyperlipidemia, n (%) 74 (18.7) Smoking, n (%) 70 (17.7) Prior congestive heart failure (%) 42 (10.6) Prior myocardial infarction, n (%) 56 (14.2) Prior percutaneous coronary intervention, n (%) 107 (27.1) Functional status of dyspnea NYHA class II 221 (55.9) III 81 (20.5) IV 93 (23.5) SBP <90 mm Hg, n (%) 14 (3.5) Heart rate ≥100 bpm, n (%) 38 (9.6) Pulmonary edema or pleural effusion 59 (14.9) Use of intravenous diuretics, n (%) 93 (23.5) Use of intravenous inotropics, n (%) 33 (8.4) Use of mechanical ventilator, n (%) 15 (3.8) Laboratory findings Hemoglobin, g/L 13.0 ± 2.0 Creatinine, mg/dL 1.02 ± 0.33 eGFR, mL/min 68.8 ± 27.7 Medication ACE/ARB 193 (48.9) Beta blocker 185 (46.8) Calcium channel blocker 133 (33.7) Diuretics 138 (34.9) Abbreviations: ACE/ARB, angiotensin converting enzyme inhibitor/ angiotensin receptor blocker; bpm, beats per minute; eGFR, estimated glomerular filtration rate by Cockcroft-Gault equation; NYHA, New York Heart Association; SBP, systolic blood pressure. LAVi/A As a New Echo Index to Identify Advanced Diastolic Dysfunction The AUC of LAVi/A for the entire study population was comparable to that of BNP (0.94 vs 0.93, P = 0.845) and Table 2. Comparison of Echocardiographic Variables and Plasma BNP Level According to Diastolic Dysfunction Grade Diastolic Dysfunction Grade Grade 0 Grade I Grade II Grade III–IV Normal (n = 21) Impaired Relaxation (n = 291) Pseudonormal (n = 53) Restrictive (n = 30) LVEF (%) 63 ± 6 60 ± 10 LVMi (g/m2 ) 90 ± 19 LAVi (mL/m2 ) 14a 33 ± 13b 106 ± 30 134 ± 32c 155 ± 60d 22 ± 7 27 ± 12 50 ± 21c 50 ± 17c Mitral E (cm/s) 73 ± 16 60 ± 17a 94 ± 28c 106 ± 23d Mitral A (cm/s) 54 ± 15 79 ± 19c 60 ± 21 43 ± 16a 188 ± 32 240 ± 78c 154 ± 40a 118 ± 39b PV, S (cm/s) 51 ± 13 58 ± 16 40 ± 15a 36 ± 15a PV, D (cm/s) 45 ± 13 40 ± 10 57 ± 22c 68 ± 21d PV, AR (cm/s) 25 ± 4 31 ± 21c 26 ± 11 26 ± 11 (cm/s) 8.7 ± 1.3 E (cm/s) A (cm/s) DT (msec) S PASP, (mm Hg) 43 ± 8.3 ± 1.8 6.1 ± 2.0a 4.9 ± 1.2b 11.3 ± 2.6 6.8 ± 1.9a 5.5 ± 1.9b 5.1 ± 1.7b 9.4 ± 1.6 10.7 ± 2.1c 7.7 ± 2.6a 5.1 ± 1.3b 25.9 ± 6.8 30.1 ± 8.7 44.1 ± 14.6c 50.3 ± 28.1c Mitral E/E 6.7 ± 1.9 9.4 ± 4.2c 19.3 ± 9.3d 23.3 ± 10.5e LAVi/A 2.4 ± 0.8 2.7 ± 1.6 7.2 ± 3.5c 10.6 ± 5.0d BNP, pg/mL 57 ± 82 123 ± 336 1050 ± 1135c 1217 ± 1168c Abbreviations: A, transmitral late diastolic velocity; A , late diastolic mitral annular velocity; AR, pulmonary venous atrial reversal flow; BNP, B type natriuretic peptide; DT, deceleration time; E, transmitral early diastolic velocity; E , early diastolic mitral annular velocity; E/E , early diastolic transmitral velocity to early diastolic mitral annular velocity; LAVi, left atrial volume index; LAVi/A , left atrial volume index over late diastolic mitral annular velocity; LVEF, left ventricular ejection fraction; LVMi, left ventricular mass index; PV, D, pulmonary venous diastolic forward flow; PV, S, pulmonary venous peak systolic forward flow; PV, S , peak systolic mitral annular velocity; PASP, pulmonary artery systolic pressure. a, b Post-hoc analysis between the groups (P < 0.05, decreased values in comparison with Grade O) c,d,e Post-hoc analysis between the groups (P < 0.05, increased values in comparison with Grade O). mitral E/E (0.94 vs 0.93, P = 0.614) and higher than that of LAVi (0.94 vs 0.87; P = 0.014). These findings were largely attributed to the difference of AUCs between LAVi/A and LAVi in patients with LVEF <50% (0.89 vs 0.80; P = 0.017). A LAVi/A of 4.0 was the best optimal cut-off value for the determination of ADD, with a sensitivity of 89% and specificity of 86%. In subgroup analysis of patients presenting with 8 ≤ E/E <15, the AUC of LAVi/A to identify ADD was similar to that of BNP (0.87 vs 0.88, P = 0.758) and numerically higher than that of E/E (0.87 vs 0.80; P = 0.258) and LAVi (0.87 vs 0.83; P = 0.512), although this difference was statistically insignificant (Figure 2). LAVi/A As a Predictor of Clinical Outcomes During a median follow-up of 31.9 months (range, 0.3 to 45.7 months), 39/395 (9.9%) patients experienced cardiac death (n = 10) or rehospitalization for CHF (n = 29). The event rates of each cardiac death and rehospitalization of CHF were higher in the group with LAVi/A ≥4.0 than the group with LAVi/A <4.0 (6/120 [5.0%] vs 4/275 [1.5%], P < 0.001; 24/120 [20.0%] vs 5/275 [1.8%], P < 0.001, respectively). Event-free survival curves also showed a greater risk of adverse outcomes in the group of LAVi/A ≥4.0 (log-rank test; P < 0.001, Figure 3). In Cox proportional hazards multivariate analysis, LAVi/A ≥4.0 was an independent predictor of primary composite outcome (odds ratio, 3.245; 95% confidence interval, 1.386–7.598; P = 0.007) (Table 3). Discussion The current study shows that LAVi/A is a useful new echo index to discriminate ADD in dyspneic patients with a wide range of LVEF. LAVi/A has the additional benefit in the assessment of the gray zone diastolic dysfunction with 8 ≤ E/E <15. LAVi/A ≥4.0 is an independent echocardiographic predictor of clinical outcomes. E/E is a noninvasive surrogate index to estimate LV filling pressure. Nagueh et al4 first demonstrated that E/E correlated well (r = 0.87, P < 0.001) with PCWP using the lateral mitral annulus for the measurement of E . Ommen et al5 demonstrated that E/E (using the mitral septal annulus) had a reasonable correlation (r = 0.64, P < 0.001) with mean LV diastolic pressure in patients referred for left heart catheterization. Some authors showed Clin. Cardiol. 34, 2, 124–130 (2011) H.- J. Park et al: LAVi/A as a new echo index to predict clinical outcomes Published online in Wiley Online Library (wileyonlinelibrary.com) DOI:10.1002/clc.20850 2011 Wiley Periodicals, Inc. 127 Figure 2. Receiver-operator characteristic curves for B-type natriuretic peptide (BNP), E/E , LAVi, and LAVi/A for the prediction of advanced diastolic dysfunction. ∗ Statistically significant difference of area under the curve (AUC) compared to LAVi (P < 0.05). its ability to predict future cardiovascular event and mortality. Liang et al15 demonstrated that E/E and LAVi were the best independent predictors of future heart failure and provide prognostic information incremental to the clinical history and LVEF. With increasing acceptance of mitral E/E ratio as a surrogate measure of diastolic function and a reliable estimate of intracardiac filling pressure, LAVi/A provides an important refinement to the clinical interpretation of mitral E/E from a different view point of LV compliance. LV compliance is an important factor affecting the contribution of LA to diastolic performance, which maximizes LV filling and protects the lungs from elevated LV end-diastolic pressure.16,17 In patients with decreased LV compliance, LA contribution to diastolic performance may decrease and LA volume may increase due to elevated LV filling pressure.9 128 Clin. Cardiol. 34, 2, 124–130 (2011) H.- J. Park et al: LAVi/A as a new echo index to predict clinical outcomes Published online in Wiley Online Library (wileyonlinelibrary.com) DOI:10.1002/clc.20850 2011 Wiley Periodicals, Inc. In the current study, LAVi/A , as a new echo index, has several advantages over E/E and LAVi for the assessment of diastolic dysfunction. First, LAVi/A may be potentially useful in the diagnosis of chronic diastolic dysfunction compared with E/E , which represents an acute stage of elevated LV filling pressure.18 Our study demonstrate that a LAVi/A value ≥ 4.0 is an independent predictor of primary composite outcome (cardiac death and rehospitalization for CHF), but E/E do not perform as well in predicting these outcomes. Second, LAVi/A is a better index to identify ADD among patients with 8 ≤ E/E <15. The patient population with 8 ≤ E/E <15 is a gray zone that is difficult to define and accurately determine clinical status.18 Based on our data, the AUC of LAVi/A is also higher than that of E/E and LAVi in the subgroup analysis. Third, LAVi/A is thought to be less influenced by age as compared to E/E and LAVi.19 – 21 This characteristic Table 3. Odd Ratios of Primary Composite Outcome (Cardiac Death and Re-Hospitalization for CHF) in 395 Patients With Dyspnea According to Cox Proportion Hazard Analysis (Forward Conditional Method) Univariate Analysis Multivariate Analysis Variables OR 95% CI P OR 95% CI P Age ≥65 y 4.203 1.932−9.145 <0.001 — — — Male gender 0.488 0.256−0.931 0.029 — — — BMI ≥25 g/m2 0.526 0.250−1.107 0.091 Hb <12 g/dL 6.400 3.287−12.459 <0.001 2.841 1.352−5.969 0.006 eGFR <60 ml/min 8.665 3.823−19.639 <0.001 2.842 1.146−7.045 0.024 BNP ≥200 pg/mL 10.487 4.969−23.681 <0.001 3.108 1.214−7.954 0.018 LVEF <50% 3.050 1.627−5.717 0.001 — — — PASP ≥40 mm Hg 5.603 2.972−10.562 <0.001 — — — LAVi ≥34 mL/m 6.693 3.176−14.105 0.001 — — — Mitral E/E ≥15 6.595 3.479−12.499 <0.001 — — — LAVi/A ≥4 8.965 4.253−18.899 <0.001 2.658 1.104−6.401 0.029 2 Abbreviations: BMI, body mass index; CI, confidence interval; E/E , early diastolic transmitral velocity to early diastolic mitral annular velocity; eGFR, estimated glomerular filtration rate by Cockcroft-Gault equation; Hb, hemoglobin; LAVi, left atrial volume index; LAVi/A , left atrial volume index over late diastolic mitral annular velocity; LVEF, left ventricular ejection fraction; OR, odds ratio; PASP, pulmonary artery systolic pressure. Unfortunately, we do not have invasive hemodynamic data, such as PCWP, to correlate with LAVi/A . As mentioned above, invasive measurement of LV filling pressure with the cardiac catheterization would be helpful to confirm the utility of LAVi/A for the prediction of elevated LV filling pressure, although BNP and E/E are well established as noninvasive methods of estimating LV filling pressures. Because A can be measured only in patients with normal sinus rhythm, it difficult to use this new index in patients with atrial fibrillation or flutter. Furthermore, our sample size and number of events are relatively small, increasing the possibility of error. Conclusion As a unique echo index, LAVi/A is a useful parameter to identify ADD and predict clinical outcomes in patients with dyspnea. The clinical significance of this index needs to be verified in a larger group of patients with longer follow-up. Figure 3. Kaplan-Meier and log-rank comparisons of the incidence of cardiac death and/or rehospitalization for congestive heart failure according to the LAVi/A cutoff value. may be due to the compensatory role of A to LA volume enlargement seen with the aging process, and may be helpful in assessing diastolic dysfunction, especially in elderly patients. Finally, LAVi/A is superior to LAVi in the identification of ADD, especially in patients with decreased LV systolic dysfunction. Our previous study showed that LAVi had no statistical difference between groups with mild and advanced diastolic dysfunction in patients with LVEF <50%.22 LAVi/A may overcome this limitation by virtue of adding LA contractile function to LA volume. References 1. 2. 3. 4. Oh JK, Appleton CP, Hatle LK, et al. The noninvasive assessment of left ventricular diastolic function with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr. 1997; 10:246–270. Oh JK, Hatle L, Tajik J, et al. Diastolic heart failure can be diagnosed by comprehensive two-dimensional and Doppler echocardiography. J Am Coll Cardiol. 2006;47:500–506. Redfield MM, Jacobsen SJ, Burnett JC Jr, et al. Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. JAMA. 2003;289:194–202. Nagueh SF, Middleton KJ, Kopelen HA, et al. Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressure. J Am Coll Cardiol. 1997;30:1527–1533. Clin. Cardiol. 34, 2, 124–130 (2011) H.- J. Park et al: LAVi/A as a new echo index to predict clinical outcomes Published online in Wiley Online Library (wileyonlinelibrary.com) DOI:10.1002/clc.20850 2011 Wiley Periodicals, Inc. 129 5. 6. 7. 8. 9. 10. 11. 12. Ommen S, Nishimura R, Appleton C, et al. Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures-a comparative simultaneous Doppler-catheterization study. Circulation. 2000;102:1788–1794. Dokainish H, Zoghbi WA, Lakkis NM, et al. Optimal noninvasive assessment of left ventricular filling pressures: a comparison of tissue Doppler echocardiography and B-type natriuretic peptide in patients with pulmonary artery catheters. Circulation. 2004;109:2432–2439. Tsang TS, Barnes ME, Gersh BJ, et al. Left atrial volume as a morphologic expression of left ventricular diastolic dysfunction and relation to cardiovascular risk burden. Am J Cardiol. 2002;90:1284–1289. Tsang TS, Barnes ME, Gersh BJ, et al. Prediction of risk for first age-related cardiovascular events in an elderly population: the incremental value of echocardiography. J Am Coll Cardiol. 2003;42:1199–1205. Khankirawatana B, Khankirawatana S, Peterson B, et al. Peak atrial systolic mitral annular velocity by Doppler tissue reliably predicts left atrial systolic function. J Am Soc Echocardiogr. 2004;17:353–360. Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–1463. Rakowski H, Appleton C, Chan KL, et al. Canadian consensus recommendations for the measurement and reporting of diastolic dysfunction by echocardiography. J Am Soc Echocardiogr. 1996;9:736–760. Wu AH, Packer M, Smith A, et al. Analytical and clinical evaluation of the Bayer ADVIA Centaur automated B-type natriuretic peptide 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. assay in patients with heart failure: a multisite study. Clin Chem. 2004;50:867–873. McKee PA, Castelli WP, McNamara PM, et al. The natural history of congestive heart failure: the Framingham study. N Engl J Med. 1971;285:1441–1446. Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology. 1983;148:839–843. Liang HY, Cauduro SA, Pellikka PA, et al. Comparison of usefulness of echocardiographic Doppler variables to left ventricular end-diastolic pressure in predicting future heart failure events. Am J Cardiol. 2006;97:866–871. Little WC, Downes TR. Clinical evaluation of left ventricular diastolic performance. Prog Cardiovasc Dis. 1990;32:273–290. Gibson DG, Francis DP. Clinical assessment of left ventricular diastolic function. Heart. 2003;89:231–238. Dokainish H. Combining tissue Doppler echocardiography and B-type natriuretic peptide in the evaluation of left ventricular filling pressures: review of the literature and clinical recommendations. Can J Cardiol. 2007;23:983–989. De Sutter J, De Backer J, Van de Veire N, et al. Effects of age, gender, and left ventricular mass on septal mitral annulus velocity (E ) and the ratio of transmittal early peak velocity to E (E/E ). Am J Cardiol. 2005;95:1020–1023. Prasad A, Okazaki K, Arbab-Zadeh A, et al. Abnormalities of Doppler measures of diastolic function in the healthy elderly are not related to alterations of left atrial pressure. Circulation. 2005;111:1499–1503. Nikitin NP, Witte KK, Thackray SD, et al. Effect of age and sex on left atrial morphology and function. Eur J Echocardiogr. 2003;4:36–42. Park HJ, Jung HO, Hwang HS, et al. Clinical implication of natriuretic peptides and left atrial volume for the screening methods of advanced diastolic dysfunction in the community. J Cardiovasc Ultrasound. 2006;14:98–104. INDEX TO ADVERTISERS Abbott Laboratories..............................................C2–A1 Accumetrics.............................................................C4 Effient....................................................................68–73 This index is provided as a service. Every effort to achieve accuracy is made. Publisher is not responsible for errors or omissions. 130 Clin. Cardiol. 34, 2, 124–130 (2011) H.- J. Park et al: LAVi/A as a new echo index to predict clinical outcomes Published online in Wiley Online Library (wileyonlinelibrary.com) DOI:10.1002/clc.20850 2011 Wiley Periodicals, Inc. View publication stats