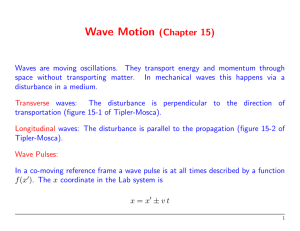
INTERNATIONAL JOURNAL OF BEHAVIORAL CONSULTATION AND THERAPY 2014, VOL. 9, NO. 2 ©2014, ALL RIGHTS RESERVED ISSN: 1555–7855 A comparison between dialectical behavior therapy, mode deactivation therapy, cognitive behavioral therapy, and acceptance and commitment therapy in the treatment of adolescents Christopher Bass1, Jolene van Nevel2, and Joan Swart2 Clark Atlanta University and 2Walden University 1 Abstract The recent rapid proliferation of “new wave” treatments, also loosely referred to as the third wave cognitive-behavioral therapies, has renewed interest in their comparative performance, scientific validity, and theoretical and methodological integrity. However, critics are also expressing concerns that these therapies are not well enough supported and “getting ahead of the data”. This article engages the literature on a small selection of modern therapy approaches, namely Mode Deactivation Therapy (MDT), Acceptance and Commitment Therapy (ACT), and Dialectical Behavior Therapy (DBT), and more specifically compared to Cognitive Behavioral Therapy (CBT). On the one hand, it challenges the assumption that third wave therapies in general, but more specifically in reference to MDT, ACT, and DBT, have little new to offer by way of superior performance, often in reference to populations that are usually deemed as difficult-to-treat in traditional approaches such as CBT. While, on the other hand, it investigates claims that third wave treatments are more part of a CBT family of approaches rather than distinct treatments. It draws from the conceptualizations, practices, and experiences of the respective developers themselves to argue for the distinct value and prospects that these third wave therapies offer in terms of scientifically established treatment outcomes. For example, it is difficult and unwise to dismiss the superior results that MDT has established in treating severe multi-problem adolescents, a population that has inarguably an extremely high human and economic impact in the long run. By an improved understanding and differentiation of the third wave therapies, their proliferation can be accelerated without compromise to harness their potential more effectively and focused. Keywords mode deactivation, acceptance and commitment, dialectic behavioral, cognitive behavioral, adolescent therapy, third wave therapy A s so-called third wave therapies, Dialectical Behavior Therapy (DBT) and Acceptance and Commitment Therapy (ACT), alongside with Mode Deactivation Therapy (MDT), are derivatives of Cognitive Behavioral Therapy (CBT). (Classical behavioral therapies are referred to as the first wave, and classical cognitive therapies as the second wave.) Currently these three types of therapy have been showing an increased amount of success with adolescent youth who have been suffering from disorders such as Conduct Disorder, post-traumatic stress symptomology, and other mood disorders (Apsche, DiMeo, & Kohlenberg, 2012; Apsche, Bass, & Backlund, 2012; Powers, Vörding, & Emmelkamp, 2009) . Dialectical Behavior Therapy DBT was developed in 1993 by Prof. Marsha Linehan, who wanted to adapt CBT when she recognized the shortcomings of the approach with her borderline personality disordered patients (Bayles, Blossom, & Apsche, 2014). The main objective was to accommodate those specific characteristics such as extreme emotional reactivity and high sensitivity to vulnerabilities like perceived rejection. DBT uses a variation of CBT that teaches the patient specific skills they will need to cope with stress, and to help in regulating their emotions (Apsche, 2010). Since then, it has been shown to be useful for treating a wide variety of presenting issues, including suicidal behaviors, substance abuse, eating disorders, and depression (Murphy & Siv, 2012; Dimeff & Koerner, 2007). The main goal of DBT is to teach the individual the skills that they will need to cope with stress (Apsche & DiMeo, 2012). This gives them tools that they will need to change their current negative coping (Arch, Eifert, Davies, Vilardaga, Rose, & Craske, 2012). DBT gives skills that are needed to become productive members of the outside community in which the individuals live in and helps them to gain a positive perspective on value and acceptance of their personal struggles, and enhances them for positive change (Apsche, Siv, & Matteson, 2005). A downfall to applying CBT elements in the DBT methodology is that since its nature is to constantly challenge the emotions of the individuals it is making it hard for them to accept their beliefs as real and reasonable. As such, they could perceive that others view their emotional pain as not real and an attempt to get attention, when, in fact, they are truly suffering and experiencing emotional pain. A positive of CBT elements in the DBT approach is that it provides a way of acknowledging the experience of their real pain (Apsche, Siv, & Matterson, 2005). It is also reassuring that their current maladaptive behavior actually makes sense and shows them that they should change this way of coping, while helping them find a more positive way of coping with their problems that in the end will be healthier for their well-being and mind set (Bayles, Blossom, & Apsche, 2014). Furthermore, DBT uses CBT principles to form a bond between the patient and the therapist so that they can work together to resolve the problems and provide the patient new ways of accepting what is causing them stress and to help them change in a positive manner. Acceptance and commitment Therapy mechanisms into positive ones that will help them to regulate their emotions and improve relationships with others around them (Apsche, 2010). It will then teach the individual the skills that are needed to cope in a positive manner to stress, regulate their emotions, and to help them improve relationships with other such as for adolescents their parents and other family members. There are four key components that make DBT successful; (a) cognitive behavioral theoretical framework, (b) validation, (c) dialectics, and (d) radical acceptance (Bayles, Blossom, & Apsche, 2014). DBT uses dialectics which applies the concept that everything is made up of opposites and the change that happens is when one opposing force is stronger than the other. This has three basic assumptions, first being; all things are interconnected. Second, change is constant and inevitable. Third, the opposites can be integrated to form a closer approximation (Apsche, 2010; Murphy & Siv; 2012, Apsche, DiMeo, & Kohlenberg, 2012). Today DBT is mainly used with individuals who present strong urges to harm themselves and or who have self-destructive behavior (Apsche, DiMeo, & Kohlenberg, 2012). This is one reason why this has been successful in adolescents, particularly young males. DBT also encourages acceptance and change. The acceptance is unconditional and change is brought about through the direct change of thoughts in a positive manner (Apsche, DiMeo, & Kohlenberg, 2012). DBT has been shown to improve behavior in three strong areas that disordered adolescents typically need help in improving: (a) lack of the needed behavioral coping skills, (b) accepting reality as it is, and (c) maintaining strong commitment to change 4 Acceptance and Commitment Therapy (ACT), alongside Mode Deactivation Therapy (MDT), Cognitive Behavioral Therapy (CBT), and Dialectical Behavior Therapy (DBT), are all considered to belong to the third wave of cognitive-behavioral therapies (Apsche, 2010; Zettle, 2012). The main goal of ACT is to help the patient to stay aware of their private memories, thoughts, and feelings without the need to change or avoid them (Apsche, 2010; Ruiz, 2010; Jennings, Apsche, Blossom, & Bayles, 2013). Alike MDT and DBT, ACT also uses mindfulness techniques to gain acceptance, commitment and positive behavioral change. ACT therefore uses parts of CBT that focus on cognition, and then allows the adolescent to change the focus from challenging or controlling to accepting the negative thoughts or emotions instead of rejecting them (Jennings, Apsche, Blossom, & Bayles, 2013). ACT then guides the adolescent in separating the negative thoughts and behaviors in order to change them into positive ones with the use of mindfulness principles. Mindfulness in ACT is the building bridge between the collaborative relationship between the patient and therapist (Jennings, Apsche, Blossom, & Bayles, 2013). Mindfulness in ACT is used to defuse language, increase awareness, and to understand the self as the observer of thoughts, feelings and experiences (Romanoff, 2012). Mindfulness also helps the adolescent in this therapy approach to commit to taking action in change. ACT uses defusion to separate words from emotions (Ruiz, 2010). In ACT, cognitive defusion techniques are applied in an attempt to alter undesirable functions of thoughts and other private events instead of denying their existence. A COMPARISON BETWEEN DBT, MDT, CBT, AND ACT Table 1. Comparison between CBT, ACT, DBT, and MDT Principle CBT ACT DBT MDT Basic philosophies Faulty thinking lead to disturbances which is corrected by learning Mixed acceptance, mindfulness, commitment & behavior change strategies Combines CBT with Buddhist meditative practices Childhood experiences lead to core beliefs, which may lead to dysfunctional behavior Key concepts Problems rooted in childhood but reinforced by present thinking and core beliefs Problems rooted in experiential avoidance & cognitive entanglement Emphasize psychosocial aspects to manage arousal levels by support-oriented, cognitive-based & collaborative therapy Focus on processes between experiences, beliefs, modes/schemas, thoughts, and behavior Goals of therapy Confront faulty beliefs and change automatic thinking Guides to contact with self-as-context; Accept & choose alternative Stabilizing, achieve behavioral control & non-traumatic experiencing To realign beliefs via modes to promote healthier thoughts and behavior Teacher-student and directive Empowering & accepting Ally with uncon-ditional acceptance Collaboration as team is key Techniques Structured cognitive, behavioral & emotive techniques Teaches to notice, accept & embrace problem events Learn skills of mindfulness, interpersonal effectiveness, emotional regulation & distress tolerance Identify beliefs and associated fears, and functional alternatives. Reinforce by anticipation. Applications Wide range of Axis I disorders Wide range of Axis I disorders, addictions, compulsive behaviors, pain BPD, mood disorders, sexual trauma, chem. dependency CD & complex comorbidity of male youths 14-17 Limitations Client dependency, not confrontational, structured, little focus on past Does not address underlying cognitive processes and origin of core beliefs Treatment stability, client expectations & differential effectiveness is questioned (Scheel, 2000) May be seen as confrontational; limited independent validation; limited target population Empirical support Extensive (137k ref. on Google Scholar) Limited (219 ref.) Low-Modest (669 ref.) Limited (130 ref.) Modest to good depending on application Low-Modest (d range 0-0.6) Low-Moderate (avg d 0.2) (Kriem, Kroger, & Kosfelder, 2010) Good with target populations (avg d 0.97) Therapeutic relationship Efficacy Thereby, the unpleasant thoughts and feelings are placed in their proper context where their impact is diminished. Patients are encouraged to observe their thoughts and emotions dispassionately and objectively, without attaching them as reified parts of their self. In essence, ACT helps patients “connect with a transcendent, compassionate sense of self that is bigger than our constructed identity or self-made concepts (Romanoff, 2012, p. 134). By using the philosophy of functional contextualism in ACT it helps to analyze the specific behaviors that are causing the maladaptive behavior in terms of their specific function in a very discrete context (Arch, Eifert, Davies, Vilardaga, Rose, & Craske, 2012). In functional contextualism, psychological events—thoughts, feelings, and behaviors—are emphasized by focusing on manipulable variables in their particular context at the time. As such, functional contextualism has been developed to help in clarifying psychological issues that continually remain foggy or unclear but are at the root of the individual’s problematic behavior (Romanoff, 2012). This is used through the means of prediction and influence. In the ACT paradigm, the patient’s thoughts and feelings are not seen as being correct or incorrect but rather as useful in understanding and changing life to in order to experience more value and satisfaction (Ruiz, 2010). Mode deactivation therapy Mode Deactivation Therapy (MDT) is one of the most recent types of therapy in treating aggression and conduct disorder among juvenile adolescent males. This therapy was developed by Dr. Jack Apsche in the late 1990’s to overcome the limitations of CBT with disturbed multi-problem adolescents who were diagnosed with conduct disorders and aggressive behavior (Apsche, 2010). Adolescents with similar psychopathology are unable to override the automatic responses that come along with their emotional regulation. Therefore, at the center of the MDT methodology is assessing and reconstructing the core beliefs by way of Aaron Beck’s (1996) theoretical constructs of modes (Apsche, 2010), where modes are powerful sub-organizations of one’s personality. According to Beck the modes are constructed of four interconnected networks, consisting of (a) cognitive (b) affective (c) motivational and (d) behavioral components (Apsche, 2010; Beck, 1996). This was originally developed to be a proactive strategy in the response to trauma and abuse (Beck, 1996). The main goal of this therapy approach is to work together with the youth in collaboration to help in discovering how to change their current maladaptive behavior from being socially unacceptable to being acceptable with normal healthy responses to trauma and stress (Bayles, Blossom, & Apsche, 2014). As such, MDT has then shown to be very effective in the reduction of physical and sexual aggression among aggressive male adolescents (Apsche, 2010). To understand MDT it is important to know what a mode is and how it is used in the MDT methodology. As briefly mentioned before, the modes in MDT consist of four integrated networks that work together to provide a proactive response to traumatic and abusive experiences, with (a) cognitive, (b) affective, (c) motivational and (d) behavioral components (Apsche, 2010, Apsche, Ward, & Evile, 2003). The youth who best benefit from this therapy are those who are to be considered to be emotionally charged, have maladaptive behaviors, and “fly off the handle” (gets enraged, angry) too quickly in reaction to perceived threats. MDT utilizes mindfulness techniques to help improve self-regulation. Mindfulness is described in MDT by one being fully aware and accepting oneself as you are in the moment without judgment (Apsche, 2010, Bayles, Blossom, & Apsche, 2014). MDT helps patients to notice that the influx of emotions can be better used in other positive ways, just like in DBT. This therapy concentrates on these strong emotions of fear, rage, and anxiety and teaches adolescents how to overcome their negative urges and attachments (Apsche, Ward, & Evile, 2003). The use of MDT with this population is viewed as a positive therapy. Dr. Apsche has found that traditional CBT can be too judgmental and intrusive on the adolescent’s emotions. When working with these adolescents with severe and aggressive behavior problems, he has found that CBT caused them to regress from the progress that was made with MDT, and increased their resistance to therapy (Apsche, 2010). But, through the application of MDT, the adolescents are gaining trust with the therapist and have opened up to different and positive pathways of coping. This can be solidified by the use of the concept unique to the MDT methodology known as “validation, clarification and redirection” (VCR) (Apsche, 2010). VCR is used to provide the adolescent with tools and guidance to find their own unconditional acceptance and validate their learning experience (Apsche, 2010). Therefore, unlike CBT, MDT accepts the adolescent’s beliefs as a truth no matter how irrational it may seem to others (Bayles, Blossom, & Apsche, 2014). This helps in forming the strong bond that is needed between the therapist and the adolescent. It also helps in the validation of what the adolescent believes to be the truth and what is the actual truth, and helps them to see the difference between what they have made up to be true and what is true. In a way it lifts the dark cloud and provides a clean window in to the truth of their current reality (Jennings, Apsche, Blossom, & Bayles, 2013). By doing this over all MDT helps the adolescent to discover who they really are and how to accept it in the context of their current environment. 5 6 BASS, VAN NEVEL, & SWART Comparison between MDT, DBT, and CBT On the surface, it may seem that there is not that much of a difference between MDT and DBT. Both of these therapies have been proven as effective ways to increase positive social change in these multi-problem adolescents. However, one difference is that MDT does not utilize CBT principles to the same extent, because the inherent disputation of their beliefs, thoughts, and feelings in the CBT approach causes the youth to regress from the progress what was made with MDT and DBT therapy (Murphy & Siv, 2012). On comparison of the treatment outcomes of MDT versus CBT, MDT has been shown to provide superior results in dealing with aggressive and multi-problem adolescents, and is significantly more effective in achieving treatment goals. As such, MDT has been developed as an derivative of CBT in order to help find a reliable method that is better suited for treating adolescents with multiple issues while managing their typical resistance to treatment (Apsche, 2010; Apsche, Bass, & DiMeo, 2011). Furthermore, when MDT is compared to CBT, it is also more effective in decreasing severe and life-interfering behaviors such as physical aggression and self-harm (Apsche, 2010; Swart & Apsche, 2014). Both ACT and DBT utilizes mindfulness as a core concept to facilitate change. Although the initial conceptualization of MDT did not include explicit mindfulness techniques, it was added in the early 2000s in an adapted form that was suitable for MDT’s adolescent target population. As such, the exercises were shortened, simplified, and focused on breathing, visual concentration, mindful walking, and guided imagery that was brief, effective, and within the adolescent’s ability (Apsche & Jennings, 2013), whereas traditional adult programs for mindfulness training have prohibitive time demands (Carmody & Baer, 2009). Furthermore, DBT incorporates some of the training skills aspects of CBT in order to teach the adolescents how to change their behaviors and learn new and more efficient ones. Using these therapies together has given adolescent youth the opportunity to change their maladaptive behaviors and poor coping mechanisms while still accepting the truth and not discouraging or completely changing their belief system (Apsche, Bass, & Backlund, 2012; Swart & Apsche, 2014). Also, ACT and MDT both address the adolescent’s avoidance of difficult and painful thoughts and emotions (Apsche, 2010). This is achieved by using both cognitive and emotional defusion, mainly through a process where adolescents teach themselves how to anticipate and avoid painful stimuli or triggers. ACT and MDT both have deep roots in the aspect of using mindfulness. As briefly mentioned before, MDT’s mindfulness techniques are specifically designed for use with adolescents. MDT and ACT also use the acceptance of one’s self as they are in the moment, and progressing or moving forward with these particular emotions and accepting them as they are without judgment or attachment (Apsche, 2010; Bayles, Blossom, & Apsche, 2014). Throughout ACT, MDT, and DBT the principle of validation is used to encourage positive behavior changes by allowing the individuals to accept being non-judgmental of their emotions. These three therapies have been proven to show increasing positive change in adolescents. Although each of these therapies use selected aspects of CBT, each applies a distinct focus to cause this change, encourage a strong therapist-patient bond, and decrease treatment resistance and drop-out. Mostly, with the exception of traditional CBT, third wave therapies share the principles of mindfulness and acceptance, and although the basic philosophies, principles, and goals may overlap, there are subtle differences that arose from their respective theoretical underpinnings and focus on a specific target population (see Table 1). Also evident from Table 1 is that these subtle—but sometimes more pronounced—differences are mostly in the manner that dysfunctional cognitions are approached (disputation versus acceptance), orientation to the past or present, emphasis on experiential avoidance, philosophy of emotion regulation (antecedent-focused versus response-focused), goal-orientation (behavioral or cognitive), and focus on function compared to content of psychological events (i.e., thoughts, feelings, and emotions). The applications in terms of target population and/or presenting problems are also varied, as are the availability of an evidence base, and reports of efficacy. Although there is a rapidly growing evidence base to support third wave therapies empirically, there is no conclusive support for a general and unconditional assumption that any or all third wave therapies are superior to classical Cognitive Behavioral Therapies. However, specific therapeutic outcomes and attrition rates are distinctive in particular patient populations (Kahl, Winter, & Schweiger, 2012). Research of third wave therapies have not yet reached the point of maturity where component or mediation analyses have been able to define—quantitatively or qualitatively—the effect that different therapeutic elements have in mediating or moderating the outcome. Nevertheless, there are subtle, and sometimes more definitive, differences between traditional CBT and therapies such as ACT, DBT, and MDT. The most prominent and meaningful of these are briefly discussed in an attempt to delineate the particular therapies in more detail. It is important to reemphasize that some approaches that are often included with the third wave, are not deemed as such by their developers. One such a therapy is Dialectical Behavior Therapy (DBT). The developer, Marsha Linehan considers DBT to be an extension of CBT that integrates acceptance strategies instead of an authentic theoretical deviation thereof (Hofmann, Sawyer, & Fang, 2010). In fact, CBT and other third wave therapies can be considered as a family of interventions that are based on the notion that “modifying maladaptive behaviors can lead to a decrease in emotional distress and problematic behaviors” (p. 702). However there are important philosophical and procedural differences among them. 1. Theoretical roots: Both CBT and DBT are based on the basic premise of the causal interaction between cognitions, behaviors, and emotions. According to developer Dr. Stephen C. Hayes, ACT is not an extension of the CBT model, but a reformulation of Skinnerian radical behaviorism that links responding with reinforcement according to operant conditioning principles, which are incorporated with acceptance and mindfulness. The developer of MDT, Dr. Jack Apsche, has purposefully taken a step back by adopting elements of psychoanalytic object relations and Piagetian schema development into the frame of Beck’s cognitive theory together with acceptance and mindfulness. 2. Resistance to treatment, dropout, and attrition: Despite claims that the newer third wave therapies outperform CBT, several factors have to be taken into account. Firstly, the evidence base for ACT, DBT, and MDT are much smaller, although expanding rapidly. Secondly, the development of third wave therapies were based on specific target populations and the cognitive content specific to their issues where CBT has been deemed ineffective. Nevertheless, third wave therapies are reporting great success with their target populations in terms of resistance to treatment—a common problem in many difficult-to-treat groups and countered by the acceptance approach common to third wave therapies—dropout, and attrition (Kahl, Winter, & Schweiger, 2012; Jennings, Apsche, Blossom, & Bayles, 2013). 3. Durability and relapse: The same limitations relating to a smaller evidence base apply that were previously discussed. Here, the third limitation is the relative recentness of the third wave therapy conceptualizations and practice, which only started in the late 1980s and 1990s. However, indications are that these approaches also outperform CBT for their respective target groups with respect to durability of treatment effect and relapse rate (Bach & Hayes, 2002; Linehan, Comtois, Murray, Brown, Gallop, Heard,…Lindenboim, 2009), although some results to the contrary were also reported (Forman, Shaw, Goetter, Herbert, Park, & Yuen, 2012). Specifically pertaining to adolescents with severe multi-problem behaviors, MDT research found a significant improvement in behavioral treatment effects that markedly outperformed the CBT-based TAU control groups, and was sustained to a follow-up period of at least 18 months (Apsche, Bass, & Siv, 2006a; Apsche, Bass, & Siv, 2006b). 4. Evidence base: As mentioned before, the evidence base of ACT, DBT, and MDT are much smaller compared to CBT. Where CBT is explored in hundred-thousands of peer reviewed publications, ACT, DBT, and MDT continue to lag significantly in this regard (see Table 1). However, the research pool of these newer third wave therapies are increasing at an exponential pace. 5. Past orientation: With the exception of MDT, CBT and third wave therapies focus exclusively in the present moment and attempt to modify behavior by disputing or otherwise addressing related thoughts and feelings in real time. MDT has adopted a different focus by exploring past experiences in conjunction with problematic psychological events in the present. The premise is that by incorporating a psychoanalytic component in context with the present situation, the improved insight will bring about a more effective and durable change effect. A COMPARISON BETWEEN DBT, MDT, CBT, AND ACT 6. Disputation and acceptance: In CBT, dysfunctional thoughts, feelings, and behavior are disputed as “bad” and attempts are made to change their contents or deny their existence altogether. Newer therapies, including ACT, DBT, and MDT, have instead incorporated the concept of radical acceptance, where psychological events are accepted and not judged while attachment and identification with it are discouraged. Instead a decentered perspective of thoughts and feelings are fostered, which are “de-linked” from the concept of self or reality. 7. Mindfulness: Mindfulness has been defined as “the awareness that emerges through paying attention on purpose, in the present moment, and nonjudgmentally to the unfolding of experience moment by moment” (Hofmann, Sawyer, & Fang, 2010, p. 703). CBT in the traditional sense does not utilize mindfulness techniques and—other than mindfulness-based interventions—focus on a reflexive rather than reflective response to stressful situations and negative emotions. The presumption is that active awareness suppresses the default mode network of the brain at wakeful rest, thereby avoiding rumination of negative thinking that tends to become a self-perpetuating cycle. ACT and DBT tend to base mindfulness techniques on traditional Buddhist meditative practices, while MDT favors basic mindfulness exercises that are easy and quick for adolescents to learn, and find non-threatening—as “multiple paths to mindfulness” (Jennings & Apsche, in press). 8. Procedural: There are various procedural differences evident between and among CBT and third wave therapies. In general, CBT tend to be more structured versus the eclectic largely procedural approach of most third wave therapies. It is interesting to note that this has also been raised as a concern in terms of theoretical and therapist “drift” from established frameworks and protocols that tend to reduce cost effectiveness and integrity of the intended methodology. Of these, with a structured and sequential assessment and treatment process, MDT is considered to be the most procedurally strict (Swart & Apsche, 2014). 9. Behavioral strategies: Where traditional CBT focuses on changing or modifying psychological events that people experience in order to achieve desired behavioral outcomes, third wave therapies instead focus on changing the function of these events. Furthermore, CBT emphasizes experiential avoidance strategies instead of acceptance as ACT and MDT does. As such, CBT attempts to “identify and refute maladaptive cognitions with the goal to change the emotional response associated with them” (Hofmann, Sawyer, & Fang, 2010, p. 706), whereas ACT and MDT creates and awareness an acceptance of problematic thoughts, feelings, and behavior as they occur. ACT is therefore response-focused compared to CBT that is antecedent-focused. MDT seems to be somewhere between these two, with a primary focus on present events, but a secondary focus on underlying past experiences to identify and anticipate triggers that can assist with emotion regulation. 10. Techniques: Although there does not seem to be major differences in the principles and goals of CBT, DBT, MDT, and ACT, Brown, Gaudiano, and Miller (2011) contend that differences are mostly evident in the actual strategies and techniques that are applied. We have already mentioned that third wave therapies utilize more mindfulness and acceptance techniques, but Brown and her colleagues also reported a greater reported use of existential-humanistic techniques to address the challenges of everyday life in a balanced and holistic way, although the experiences and influences of the past are given much less emphasis than those in the present. Functional contextualism has special importance; techniques are functionally defined rather than topographically distinguished as from where it originates. Exposure techniques are more commonly used in third wave therapies, which illustrates the emphasis on traditional behavior strategies in lieu of cognitive restructuring techniques, although the latter is prominently employed in the “Validation, Clarification, and Redirection” (VCR) step that is a unique process component in MDT. Hereby the client becomes aware of dysfunctional cognitions and their underlying beliefs, while developing and trying out functional alternatives “one small step at a time”, on a continuum. Therefore, in general, there are perhaps more similarities than differences between and among CBT and third wave therapies than typically assumed, although the subtle differences are purposely directed at target populations and conditions, which amplify their functional effect. The concepts of mindfulness and acceptance are common to this wave therapies, while the past is for the most part discounted, with the exception of MDT, in which past experiences are explored in relation to the experience of their remnants in present psychological events. The future of third wave therapies, in particular MDT The concerns that we have briefly mentioned before need to be more thoroughly examined, with special emphasis on the effect that it has on treatment effectiveness, reliability, and generalizability. Of particular interest is the validity of the underlying scientific and theoretical framework, as well as how each therapy approach embody the principles conceptually and in actual practice. It would also be extremely worthwhile to understand and differentiate the mediating and moderating influence of each process component on the change effect and therapeutic outcomes. Thereby, we can come to quantitatively appreciate to what extent and how process elements such as mindfulness techniques contribute to change. Such studies have already been conducted for CBT, but are still lacking in the third wave therapies. It will also contribute to an understanding of how and why CBT reportedly fail for certain populations, while third wave therapies seem more effective to a lesser or greater extent. We presume, with good reason, that each emotional disorder are characterized by cognitive content that is specific to that disorder, but to what degree can protocols be tailored and/ or generalized to improve treatment for the same, other, and broader populations? The developers of ACT (Stephen Hayes), DBT (Marsha Linehan), and MDT (Jack Apsche) has already done a sterling job to promote and establish the evidence base of their respective approaches. Now, continued effort is required to better understand and appreciate the differences in mechanisms and applications of these respective therapies. We do not necessarily need more emerging themes, but maybe a unified and flexible application instead that remains in the realm of scientific principles and validity. As we have compared CBT, MDT, ACT, and DBT, it hopefully became evident that differences are for the most part not theoretically or procedurally irreconcilable, in fact many ideas and principles seem perfectly compatible. For example, Mode Deactivation Therapy (MDT) is a synthesis of elements from DBT, CBT, ACT, mindfulness, and psychoanalysis that was adapted for an adolescent population that was traditionally considered as difficult-to-treat. In various studies already it has shown remarkable results while holding up under stringent scientific scrutiny of its theory and practice. MDT, “the third wave movement”, and psychotherapy as a whole, can greatly benefit from statistically sound evidence of the influence that respective process components exert on the overall treatment effect. References Apsche, J. A. (2010). A literature review and analysis of Mode Deactivation Therapy. International Journal of Behavioral Consultation and Therapy, 6(4), 296-340. Apsche, J. A., Bass, C. K., & Backlund, B. (2012). Mediation analysis of Mode Deactivation Therapy (MDT). Behavior Analyst Today, 13(2), 2-10. Apsche, J. A., Bass, C. K., & DiMeo, L. (2011). Mode Deactivation Therapy (MDT) Comprehensive meta-analysis. International Journal of Behavioral Consultation and Therapy, 7(1), 47-54. Apsche, J. A., Bass, C. K., & Siv, A. M. (2006a). A treatment study of Mode Deactivation Therapy in an outpatient community setting. International Journal of Behavioral Consultation and Therapy, 2(2), 277-285. Apsche, J. A., Bass, C. K., & Siv, A. M. (2006b). Summary of Mode Deactivation Therapy: Cognitive Behavior Therapy and Social Skills Training with two year post treatment results. International Journal of Behavioral Consultation and Therapy, 2(1), 29-44. Apsche, J. A., Ward, S. R., & Evile, M. M. (2003). Mode deactivation: A functionally based treatment, theoretical constructs. Behavior Analyst Today, 3(4), 455-459. Apsche, J., & DiMeo, L. (2012). Mode Deactivation Therapy for aggression and oppositional behavior in adolescents: An integrative methodology using ACT, DBT, and CBT. Oakland, CA: New Harbinger. Apsche, J. A., & Jennings, J. (2013). The mindfulness toolkit for counselors, teachers, coaches and clinicians of youth. Holyoke, MA: NEARI Press. Apsche, J. A., Siv, A. M., & Matteson, S. (2005). A Comparison of MDT and DBT: A case study and analysis. International Journal of Behavioral Consultation and Therapy, 1(3), 204-215. Arch, J. J., Eifert, G. H., Davies, C., Vilardaga, J. C. P., Rose, R. D., & Craske, M. G. (2012). Randomized clinical trial of cognitive behavioral therapy (CBT) versus acceptance and commitment therapy (ACT) for mixed anxiety disorders. Journal of Consulting and Clinical Psychology, 80(5), 750-765. DOI: 10.1037/a0028310 Bach, P., & Hayes, S. C. (2002). The use of Acceptance and Commitment Therapy to prevent the re-hospitalization of psychotic patients: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 70(5), 1129-1139. DOI: 10.1037//0022-006X.70.5.1129 Bayles, C., Blossom, P., & Apsche, J. (2014). A brief review and update of mode deactivation therapy. International Journal of Behavioral Consultation and Therapy, 9(1), 46-48. 7 8 BASS, VAN NEVEL, & SWART Beck, A. (1996). Beyond belief: A theory of modes, personality and psychopathology. In P. Salkovaskis (Ed.), Frontiers of cognitive therapy (pp. 1-25). New York, NY: Guilford Press. Hofmann, S. G., Sawyer, A. T., & Fang, A. (2010). The empirical status of the “new wave” of CBT. Psychiatric Clinics of North America, 33(3), 701-710. DOI: 10.1016/j.psc.2010.04.006 Brown, L. A., Gaudiano, B. A., & Miller, I. W. (2011). Investigating the similarities and differences between practitioners of second and third wave cognitive-behavioral therapies. Behavior Modification, 35(2), 187-200. DOI: 10.1177/0145445510393730 Jennings, J. L., & Apsche, J. A. (in press). The evolution of a fundamentally mindfulness-based methodology: From DBT and ACT to MDT and beyond. International Journal of Behavioral Consultation and Therapy. Carmody, J. & Baer, R. (2009). How long does a mindfulness-based stress reduction program need to be? A review of class contact hours and effect sizes for psychological distress. Journal of Clinical Psychology, 65, 627-638. Dimeff, L. A., & Koerner, K. (2007). Dialectical Behavior Therapy in clinical practice: Applications across disorders and settings. New York, NY: Guilford. Forman, E. M., Shaw, J. A., Goetter, E. M., Herbert, J. D., Park, J. A., & Yuen, E. K. (2012). Long-term follow-up of a randomized controlled trial comparing Acceptance and Commitment Therapy and standard Cognitive Behavior Therapy for anxiety and depression. Behavior Therapy, 43, 801-811. Jennings, J. L., Apsche, J. A., Blossom, P., & Bayles, C. (2013). Using mindfulness in the treatment of adolescent sexual abusers: Contributing common factor or a primary modality? International Journal of Behavioral Consultation and Therapy, 8(3-4), 17-22. Kahl, K. G., Winter, L., & Schweiger, U. (2012). The third wave of cognitive behavioral therapies. Current Opinion in Psychiatry, 25(6), 522-528. DOI: 10.1097/YCO.0b013e328358e531 Kriem, S., Kröger, C., & Kosfelder, J. (2010). Dialectic Behavior Therapy for Borderline Personality Disorder: A meta-analysis using mixed-effects modeling. Journal of Consulting and Clinical Psychology, 78(6), 938-951. DOI: 10.1037/a0021015 Gaudiano, B. A. (2008). Cognitive-behavioral therapies: Achievements and challenges. Evidence-Based Mental Health, 11(1), 5-7. DOI: 10.1136/cbmh.11.1.5 Linehan, M. M., Comtois, K. A., Murray, A. M., Brown, M. Z., Gallop, R. J., Heard, H. L.,…Lindenboim, N. (2009). Two-year randomized controlled trial and follow-up of Dialectical Behavior Therapy vs. therapy by experts for suicidal behaviors and Borderline Personality Disorder. Archives of General Psychiatry, 63, 757-766. Hofmann, S. G., & Asmundson, G. J. G. (2008). Acceptance and mindfulness-based therapy: New wave or old hat? Clinical Psychology Review, 28(1), 1-16. DOI: 10.1016/j.cpr.2007.09.003 Murphy, C. J., & Siv, A. M. (2012). A one year study of Mode Deactivation Therapy: Adolescent residential patients with conduct and personality disorders. International Journal of Behavioral Consultation and Therapy, 7(1), 33-40. Powers, M. B., Vörding, M. B., & Emmelkamp, P. M. G. (2009). Acceptance and Commitment Therapy: A meta-analytic review. Psychotherapy and Psychosomatics, 78(2), 73-80. DOI: 10.1159/000190790 Romanoff, B. D. (2012). Acceptance and Commitment Therapy (ACT). In R. A. Neimeyer, Techniques of Grief Therapy: Creative Practices for Counseling the Bereaved (pp. 133-135). New York, NY: Routledge. Ruiz, F. J. (2010). A Review of Acceptance and Commitment Therapy (ACT) empirical evidence: Correlational, experimental psychopathology, component and outcome studies. International Journal of Psychology & Psychological Therapy, 10(1), 125-162. Scheel, K. R. (2000). The empirical basis of Dialectic Behavioral Therapy: Summary, critique, and implications. Clinical Psychology: Science and Practice, 7, 68-86. Swart, J., Apsche, J. A. (2014). Family mode deactivation therapy (FMDT) as a contextual treatment. International Journal of Behavioral Consultation and Therapy, 9(1), 30-37. Swart, J., & Apsche, J. A. (2014). Family mode deactivation therapy (FMDT) mediation analysis. The International Journal of Behavioral Consultation and Therapy, 9(1), 1-13. Zettle, R. D. (2012). Acceptance and commitment therapy (ACT) vs. systematic desensitization in treatment of mathematics anxiety. The Psychological Record, 53(2), 197-215. All in-text references underlined in blue are linked to publications on ResearchGate, letting you access and read them immediately.