Subido por
ALEJANDRA SOLANGE JORQUERA GALLARDO
Alexia, Aphasia, and Oral Reading: Classification & Treatment
Anuncio
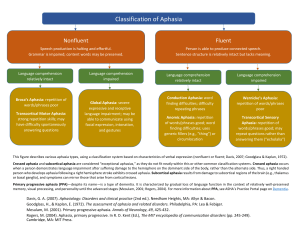
Aphasia, Alexia, and Oral Reading Leora Reiff Cherney Alexia is an acquired disturbance in reading. Alexias that occur after left hemisphere damage typically result from linguistic deficits and may occur as isolated symptoms or as part of an aphasia syndrome. This article presents an overview of the classification of the alexias, including both the traditional neuroanatomical perspective and the more recent psycholinguistic approach. Then, assessment procedures are reviewed, followed by a summary of treatment approaches for alexia. Finally, two case studies illustrate how oral reading of connected language (sentences and paragraphs rather than single words) has been used as a technique for treating alexia in patients with aphasia. Key words: alexia, aphasia, assessment, classification, reading, treatment A lexia, an acquired disturbance in reading, is a common consequence of brain damage. Both left and right hemisphere pathology may result in loss or impairment of the ability to comprehend written or printed language. Disturbances of reading that occur after right-brain damage are typically related to problems in visual processing such as spatial discrimination and unilateral visual neglect; these alexias have been referred to as neglect dyslexia or spatial or hemispatial alexia.1–7 Reading disturbances that occur after left-hemisphere damage typically result from linguistic deficits and may occur as isolated symptoms or as part of an aphasia syndrome.8 This article focuses on the alexias that result from left-hemisphere damage. First, an overview of the classification of the alexias is provided, including both the traditional neuroanatomical perspective and the more recent psycholinguistic approach. Then, assessment procedures are reviewed, followed by a summary of various treatment approaches for alexia. Finally, two case studies illustrate how oral reading of connected language (sentences and paragraphs rather than single words) has been used as a technique for treating alexia in patients with aphasia. Classification of the Alexias Traditionally, classification of the alexias has been based primarily on neuroanatomic distinctions. More than a century ago, Dejerine described two distinct alexia syndromes—alexia with 22 agraphia and alexia without agraphia.9,10 Alexia with agraphia occurred after left-hemisphere parietal damage; alexia without agraphia resulted from occipital damage together with damage to the splenium of the corpus callosum. Since then, several case reports have supported the clinical and neuropathological patterns of these two alexias. More recently, a third major alexia syndrome has been proposed, based on an anterior lesion in the left hemisphere; this has been called frontal alexia.8 Each of the alexias are described further in the following discussion. However, it should be noted that although the symptoms of each of these alexias are relatively clear-cut, associated clinical findings vary considerably depending on the extent of the lesions and involvement of other areas of the cerebrum.8 Alexia without agraphia (occipital alexia) Alexia without agraphia is easily recognized because it is characterized by a disturbance of reading contrasted with relatively preserved writLeora Reiff Cherney, PhD, CCC-SLP, BC-NCD, is Associate Professor, Physical Medicine and Rehabilitation, Northwestern University Feinberg School of Medicine, Chicago, Illinois, is Clinical Research Scientist, Rehabilitation Institute of Chicago, and is Associate Professor, Communication Sciences and Disorders, Northwestern University, Evanston, Illinois. Top Stroke Rehabil 2004;11(1):22–36 © 2004 Thomas Land Publishers, Inc. www.thomasland.com Aphasia, Alexia, & Oral Reading ing skills. Patients typically cannot read what they have just finished writing. The difficulty with letter and word recognition is specific to the visual modality, and patients can spell out aloud and recognize words spelled to them by the examiner. Therefore, alexia without agraphia is also called pure alexia, pure word blindness, or agnosic alexia. Letter naming, although initially slow, improves with practice, and the patients often learn to read the individual letters of the word aloud and then decipher the words from their oral spelling. Alexia with agraphia (parietal-temporal alexia) As its name implies, alexia with agraphia is characterized by impairments of both reading and writing, with the writing impairment usually equal in severity to the alexia. Patients display difficulty in comprehending written material that is read silently as well as in reading out loud. Reading of letters and words is impaired, and this difficulty extends to comprehension of numbers and musical notations.8 The problem with letter identification is not restricted to the visual modality; patients also have problems recognizing words when they are spelled aloud. Parietal-temporal alexia is often associated with a fluent paraphasic aphasia. Frontal alexia In patients with frontal alexia, reading comprehension is typically limited to a few single words, usually content words. Reading comprehension of function words such as prepositions and pronouns is impaired. In contrast to their ability to recognize some words, patients are unable to read the individual letters of the word. Spelling words out loud and comprehension of words that are spelled aloud is also poor. A severe agraphia accompanies the alexia, with writing characterized by poorly formed letters, omission of letters, and agrammatic sentences. Frontal alexia is typically associated with a nonfluent aphasia. Although these traditional neuroanatomically based distinctions have provided us with a better understanding of the alexias, they do not fully explain the degree of variability seen in patients 23 with alexia and do not permit subtypes of alexias to be distinguished. Interest has therefore shifted from the anatomical correlates of acquired reading disorders to the neurolinguistic and cognitive mechanisms underlying them. In this approach, various theoretical models of reading have been proposed to account for the performance of normal readers and to identify the components of the normal reading system that are disturbed in the alexia syndromes. Figure 1 shows a model of normal reading comprehension that was developed by analyzing the errors made by alexic patients while they read single words out loud.11–14 After the perceptual analysis and identification of letters, there are three distinct ways in which a phonological code (pronunciation of the word) is attained from the written word: 1. In the direct lexical-semantic route, the written word is matched to a corresponding word form in the visual word store or orthographic lexicon and is recognized. Meaning is then retrieved by activation of the semantic representation of the word by the semantic processor. Finally, if the word is to be read out loud, its pronunciation is activated by the phonological processor. This route accounts for “wholeword” reading of familiar real words. 2. In the indirect route, the written word is transformed into the spoken word via grapheme-tophoneme correspondence rules in the lettersound converter. This nonlexical or sublexical route accounts for oral reading of novel words that have no meaning or stored pronunciation or for regular words that can be pronounced correctly by sounding out the constituent letters. 3. In the lexical-nonsemantic route, the written word is matched to a visual word form in the orthographic lexicon and is recognized. Then its pronunciation is retrieved by the phonological processor. The word is read aloud, but without comprehension because the semantic processor is bypassed. It should be noted that Figure 1 represents only the major routes of the normal reading process. More complex models with other components have been postulated. For example, a phonologic buffer or short-term memory is thought to main- 24 TOPICS IN STROKE REHABILITATION/WINTER 2004 Vision Perceptual Analysis Letter-Sound Convertor Visual Word Store Semantic Processor Phonological Processor Speech Figure 1. Model of the normal reading process (after Marshall & Newcombe13 and Morton & Patterson14). tain individual phonemes during speech output and is active during oral reading regardless of the reading route that is used. As further investigations of oral reading in alexic patients continue, the model and its component processes will be more specifically defined. The direct and indirect routes are both available to the normal reader. The direct route enables patients to read real words, particularly high frequency words that are in their reading vocabulary and visual word store. The indirect route is used for reading low frequency, unfamiliar words; these are sounded out using grapheme-to-phoneme correspondence rules. In the proficient reader, the indirect route is used only when the reader is confronted with an unfamiliar word for which neither a phonological code nor a meaning code is activated quickly. Grapheme-phoneme decoding is usually achieved rapidly and automatically, so that most attention can be focused on comprehension of meaning. In contrast, the nonproficient reader has fewer words in the visual word store and must utilize the indirect route more frequently. Therefore attention is given primarily to the grapheme-to-phoneme conversion process, a complex process that is thought to involve three stages: graphemic parsing (segmentation of the written graphemes into individual units), grapheme-to-phoneme conversion (translation of the grapheme segments into corresponding sounds), and blending (assembling of the individual sounds into a whole word). As a result, the ability to comprehend meaning is compromised.15 Within the psycholinguistic approach, four different alexic syndromes have been described, each Aphasia, Alexia, & Oral Reading of which may occur in association with an aphasia. They have been labeled phonological, deep, surface, and semantic alexia and occur because of differential breakdowns in the normal reading process.16–24 Figures 2–5 illustrate these reading disorders as they relate to the model of reading described previously. In phonological alexia (Figure 2), the graphemeto-phoneme correspondence rules of language are no longer available, so reading is accomplished by the direct route. Often the reading disturbance is not readily apparent. The patient can read aloud real words, particularly high frequency words; these words have an orthographic address and are in the individual’s reading vocabulary and visual word store. However, there is difficulty with nonwords (e.g., bome), or with low frequency words. The patient is not able to sound out the letters to get the word, because the letter sound converter is not functioning. Typically, there are visual errors, such as mild for slid, in which the target word is read as another word that has similar letters in it. Patients with phonological alexia often complain of difficulty reading high level material such as books and newspapers. Deep alexia (Figure 3) is characterized by both an unavailability of the grapheme-to-phoneme correspondence rules and a disturbance of the lexical-semantic operations. Like phonological alexia, patients are unable to read nonwords with visual errors evident. In addition, patients with deep alexia make many semantic errors such as producing synonyms, antonyms, or subordinates for a target word. Reading is limited to a vocabulary of known words and is restricted by imageability and part of speech. Concrete nouns are read better than abstract nouns, and nouns are generally read better than verbs or adjectives. Patients with deep alexia also exhibit difficulty with function words. Deep alexia is often present in Broca’s aphasia. In semantic alexia (Figure 4), the semantic processor is not available. Thus, patients are able to read aloud fluently, but without meaning. They do not comprehend what they are reading aloud. This is the type of alexia that accompanies a dementia or some of the fluent aphasias such as transcortical sensory aphasia. Vision Perceptual Analysis Visual-Word Store Semantic Processor Phonological Processor Speech Figure 2. Phonological alexia. Vision Perceptual Analysis Semantic Processor Phonological Processor Speech Figure 3. Deep alexia. 25 26 TOPICS IN STROKE REHABILITATION/WINTER 2004 Vision Perceptual Analysis Letter-Sound Convertor Visual-Word Store Phonological Processor Speech Figure 4. Semantic alexia. Vision Perceptual Analysis Letter-Sound Convertor Phonological Processor Speech Figure 5. Surface alexia. In surface alexia (Figure 5), the direct route of reading aloud is not available, so the patient relies on the indirect route. However, the grapheme-tophoneme rules are applied inadequately. Although the patient can read nonwords and regular words with unambiguous orthographies, he or she has difficulty with irregular words that cannot be sounded out. The patient tends to make phonological (i.e., the error word sounds similar to the target word) and visual errors. Comprehension is tied to success at pronunciation; if a word is mispronounced as another real word, meaning will be assigned in accordance with the incorrect pronunciation. Reading problems that are associated with aphasia may conform to the distinct alexia syndromes described previously, but a predictable relationship between aphasia type and alexia syndrome has not been identified.25 In many cases, alexia associated with aphasia reflects multiple levels of impairment and has been called a mixed alexia or aphasic alexia.26,27 In other cases, like the nonproficient reader described previously, patients with aphasia may have difficulty, in varying degrees, with the grapheme-to-phoneme conversion system.28 The aphasic patient may have lost the ability to rapidly decode the phonological and visual information of the word, which interferes with the ability to read for meaning. This would explain why many aphasic patients who successfully read at the word and sentence level continue to show delays and comprehension problems when reading texts. In contrast to patients with aphasia, patients with pure alexia do not have direct visual access to the normal reading system. Several plausible hypotheses have been suggested to explain why the written word is not recognized overtly. Some investigators have suggested that visual perception of letters is adequate, but the word form that is needed to match the string of perceived letters is not available.29 Others have suggested that the word-form system is intact, but input from the letter recognition system is limited to a single letter at a time, so that the problem is primarily a deficit in the speed of letter identification.30 In either case, the patient with pure alexia cannot activate either the direct lexical-semantic or indirect sub- Aphasia, Alexia, & Oral Reading lexical reading routes when the input is visual. Assessment of Reading Although a brief screening is usually sufficient for identifying the presence of an acquired alexia, detailed assessment is necessary to delineate the precise areas of breakdown so that an effective treatment program can be developed. A thorough evaluation includes assessment of reading comprehension to determine the level at which breakdown occurs, an analysis of single word oral reading, and consideration of associated areas of strengths and deficits including visual skills, writing, naming, and spelling. 27 that correspond to a written sentence. One subtest assesses specifically morphosyntactic reading and another subtest assesses short paragraph comprehension. Longer paragraph comprehension is evaluated with factual and inferential questions. Functional reading of labels and signs is also included. This second edition of the RCBA also includes a lexical decision task in which patients choose a real word from a triad of one real word and two pseudowords. Several tests of reading comprehension provide grade levels and age equivalencies and may be appropriate for individuals with acquired alexia. Such tests include the Gates-MacGinitie Reading Tests,35 the Woodcock Reading Mastery Tests,36 and the Nelson-Denny Reading Test.37 Reading comprehension and level of breakdown Oral reading Reading comprehension tasks provide information about the ability to access semantic meaning from print. All general tests of aphasia have a variety of subtests that assess reading comprehension. These subtests are typically hierarchically organized, beginning with recognition of letters, matching letters written in different forms (e.g., uppercase, lower case, script), and letter naming. Testing then progresses to the single word level (e.g., recognizing highly familiar words such as name, name of town, country; matching single words to pictures), the sentence level (e.g., following written commands ), and finally to more complex paragraphs (e.g., answering questions about a paragraph that has just been read). However, reading subtests on aphasia batteries such as the Western Aphasia Battery31 and the Boston Diagnostic Aphasia Examination32 may have too few items on some tasks and may be insufficient to detect milder problems.33 A specific test of reading comprehension that has been developed for individuals with aphasia is the Reading Comprehension Battery for Aphasia (2nd ed.) (RCBA-2).34 The test includes single word comprehension tasks in which a single picture must be matched to one of three words that are orthographically, phonologically, or semantically similar. Sentence comprehension is assessed by having the patient select one of three pictures Oral reading of single words provides insight into the specific patterns of reading breakdown consistent with the neuropsychological models and the integrity of the semantic versus phonologic reading routes. A variety of word lists have been developed. Typically, these word lists include pronounceable nonwords, regular words, and irregular words. They also include words of different lengths, different frequencies, different degrees of imageability/concreteness, and different grammatical class (function words vs. content words). Accuracy of oral reading is compared across stimulus types (e.g., word vs. nonword), and careful analysis of errors (semantic, phonologic, visual, morphosyntactic) permits a determination of the type of alexia. The Psycholinguistic Assessments of Language Processing in Aphasia (PALPA)38 is a commercially available test with tasks that allow in-depth assessment of single word oral reading, as well as various tasks that assess semantic processing. Other word lists include the Johns Hopkins University Dyslexia Battery39,40 and the Battery of Adult Reading Functions.41 Oral reading of single words has also been added to the revised edition of the RCBA-2, but the stimuli are only nouns. Oral reading of sentences and paragraphs should also be evaluated. In addition to providing a measure of oral reading rate, attentional or con- 28 TOPICS IN STROKE REHABILITATION/WINTER 2004 textual factors that affect performance may be identified. The Grey Oral Reading Test–4 (GORT4)42 consists of 13 increasingly difficult passages of text. From the assessment of oral reading rate (time to read each passage), accuracy (number of oral reading errors), and comprehension (accuracy answering five multiple choice questions at the end of each passage), grade levels for reading fluency and comprehension are derived as well as an overall Oral Reading Quotient. Associated skills The assessment of reading is best conducted in the context of a general language evaluation that compares performance given a variety of input and output modalities. In particular, spelling skills should be assessed, including both the ability to spell words aloud as well as the ability to recognize words spelled aloud by the examiner. Both oral and written naming should always be assessed to determine whether there is an associated anomia or agraphia or whether the reading problem is a pure alexia. Assessment of visualperceptual processes, visual spatial attention, and working memory also should be included. Treatment Traditional approaches to the treatment of acquired reading problems typically begin at the level of breakdown, that is, at the grapheme, word, phrase, sentence, or paragraph level, and patients practice tasks that are arranged hierarchically. Some commonly used treatment tasks include: letter matching; word–picture matching; word–word matching in which the target may be the category name, an antonym, or a synonym; word–definition matching; phrase or sentence completion; following written commands; and answering yes/no or “wh” questions about a sentence or paragraph. Difficulty is modified by a change in various parameters such as the degree of similarity between the target and distractors; the number of distractors in the field; the frequency, grammatical class, concreteness of the words; or the complexity of the grammatical structure. Most commercially available workbooks for aphasia have numerous pages of pencil and paper exercises, and more recently a number of computer programs also have been developed that provide practice on these types of reading activities. However, despite their clinical widespread use, these reading tasks and programs for aphasia have not been carefully evaluated and there is little evidence supporting their efficacy. One randomized clinical trial evaluated the efficacy of computerized treatment in general by using hierarchically organized reading activities consistent with the traditional approach.43 Fifty-five patients with chronic aphasia were randomly assigned to one of three conditions: computer reading treatment that consisted of visual matching and reading comprehension tasks, computer stimulation such as nonverbal games and cognitive rehabilitation tasks, or no treatment. Patients in the computer groups used the computers 3 hours a week for 26 weeks. The results suggested that computerized reading treatment was efficacious with improvements generalizing to noncomputer language performance. It was also shown that these improvements resulted from the language content of the software and not from the stimulation provided by the computer. In contrast to the lack of evidence supporting the traditional approach to acquired reading disorders, a variety of treatment approaches consistent with the neuropsychological approach have been developed for specific alexia syndromes. These treatments are implemented only after a detailed evaluation of the acquired alexia and target the impaired reading processes. Table 1 presents a brief summary of these studies. Taken together, these studies provide evidence that reading can be improved in cases of relatively wellspecified alexia syndromes44–68 and in cases of unspecified alexia associated with aphasia.43,69 The changes affected by treatment stand in contrast to the reports of relatively stable alexia profiles in patients who are untreated.2,70 Several issues arise from a review of the literature on treatment of alexia, as illustrated in Table 1. Although positive results have been reported for each type of alexia, the treatment approaches have been evaluated on only a limited number of patients. Furthermore, each approach has met with varying degrees of success, and often a treat- Aphasia, Alexia, & Oral Reading 29 Table 1. Treatment of acquired alexia: summary of studies Authors Lott et al.44 Alexia type Pure alexia Maher et al.45 Pure alexia Greenwald & Gonzalez-Rothi46 Pure alexia Behrmann & McCleod47 Lott & Friedman48 Pure alexia Rothi & Moss49 Rothi et al.73 Pure alexia Pure alexia Friedman & Lott50 Pure alexia Moyer51 Moody52 Toumainen & Laine53 Beeson54 Pure alexia Pure alexia Pure alexia Pure alexia Pure alexia No. of participants studied Treatment rationale and procedures 1 Tactile-kinesthetic letter identification: trained patient to trace letters onto the palm of his hand during oral letter naming 1 Motor cross-cuing strategy: patient used finger to pretend to copy letters in words and sentences 1 Trained letter-by-letter reading using letter naming 1 Speeded stimulus presentation so first and last letters of a word are apprehended together 1 Three-stage approach: (1) single-letter naming using tactile-kinesthetic feedback and feedback about speed of letter naming, (2) naming of letters in a letter string, (3) single word reading aloud with feedback about reading speed 1 Encouraged reliance on residual whole-word reading by presenting words too 1 rapidly to allow for letter-by-letter reading. Required patient to make a semantic category decision about each word. 1 Trained whole-word recognition as above; however, patient did not need to make a semantic judgment about each word. Patient was only required to read aloud each word as it was rapidly presented at a rate of 50 ms per word. 1 Multiple oral rereading (MOR), i.e., patient repeatedly read aloud a given text 1 over several days or weeks (see case study 2 for details) 3 1 Coltheart & Byng55 Surface alexia Weekes & Coltheart56 Surface alexia 1 1 Scott & Byng57 Surface alexia 1 Hillis58 Surface alexia 1 Designed to facilitate reading of irregularly spelled words. Irregular words were paired with a mnemonic picture/semantic cue (e.g., the word through was presented with an arrow through it). Patient practiced at home with sets of cards. Computer presentation of a sentence with a homophone deleted and six word choices, including the correct word, its homophone, and pseudohomophone of the correct word. Feedback provided regarding accuracy of patient selection. Homophone training. Patient read each homophone presented, its definition, and then wrote the word in a sentence. Friedman & Robinson59 Surface alexia 1 Direct training of a set of words with ambiguous pronunciation of specific letter clusters Moss et al.60 Surface alexia 1 Increased reading rate by having patient name the semantic category of target words presented at a speed too rapid to allow reading aloud De Partz61 Laine & Niemi71 Mitchum & Berndt72 Deep alexia 1 Nickels62 Deep alexia Friedman & Lott63 Deep alexia 1 Trained grapheme-phoneme conversion: (1) patient trained to associate each written letter with a code word that began with that letter; (2) each letter was 1 associated with the first sound of the code word; (3) reading of short words and nonwords. Note: In later two studies, patients had difficulty blending the phonemes into syllables. 1 Auto-cue strategy, i.e., patient instructed to produce the first phoneme of a word, think about its meaning, and then attempt to say the word 2 Bigraph training to access phonology from orthography: (1) a set of bigraphs (CV and VC) were associated with their corresponding sounds; (2) patient trained to produce a word that began with the two letters; (3) then trained to cut it short so only the bigraph was produced; (4) practiced combining CV and VC bigraphs into CVC words. 1 Direct teaching of phonics and blending using a phonics-based commercial reading program, the Wilson Reading System, to read aloud real words. Involved multisensory presentation, and systematic hierarchical, step-by-step instruction. 1 Phonological awareness training using the Auditory Discrimination in Depth program that trains motor-articulatory awareness during phoneme production 1 Taught rule-based sound conversion of whole-word orthography. Systematically exposed patient to words containing the “c” and “g” rules (e.g., cent, gem) until correct responses were given. 2 Paired associate learning: words that were low in semantic value were paired with words that sounded similar but were high in semantic content, e.g., be/bee, me/meat. Patient read target word printed on a card. If patient’s response was incorrect, he or she turned the card over and read/named the homophone/near homophone. Yampolsky & Waters64 Deep alexia Conway et al.65 Phonological alexia Kendall et al.66 Phonological alexia Friedman et al.67 Phonological alexia 30 TOPICS IN STROKE REHABILITATION/WINTER 2004 Table 1. (continued) No. of participants studied Treatment rationale and procedures 2 MOR, i.e., repeated reading aloud of a given text over several days or weeks (see case study 2 for details) Authors Moody68 Alexia type Phonological alexia Beeson & Insalaco25 Mayer & Murray78 Phonological alexia Mild alexia with decreased lexicalsemantic abilities and associated deficits in attention and working memory Alexia due to deficits with the phonological output lexicon and grapheme-to- phoneme conversion 2 1 Cherney et al.69 Varied 10 Katz & Wertz43 Varied 21 Kiran et al.79 2 Used MOR and oral reading of phrase-formatted text Used two treatment approaches: (1) text-level oral reading treatment (MOR) modified to include five comprehension questions that assessed comprehension of main ideas, details, and inferences; and (2) a working memory treatment that involved judging the grammaticality of a set of sentences as well as holding and processing the last word of each sentence in the set. The number of sentences in each set and the length of each sentence increased progressively. Trained grapheme-phoneme conversion for single words via oral reading of words. If the patients could not orally read a word, then they (1) repeated the word, (2) spelled the word out loud, (3) selected the letters of the target word from distractor letters, (4) identified the target word letters presented randomly, (5) read letters of target word. Finally, the patient attempted to read the word aloud again with feedback given. Oral reading for language in aphasia (ORLA), i.e., repeated reading aloud of sentences in unison with the clinician (see case study 1 for details) Computer treatment that consisted of 10 visual matching activities (e.g., matching letters, matching numbers, matching words) and 22 reading comprehension tasks involving words, phrases, "wh" questions, and sentences. Activities and tasks arranged sequentially in a hierarchy of difficulty determined by the activity, the task, and the number and type of response foils. ment that was initially successful turned out to be less successful with replication. For example, the success achieved by de Partz61 on a treatment involving grapheme-to-phoneme conversion training for a patient with deep alexia was not demonstrated in the subsequent studies,71,72 because the patients had particular difficulty blending phonemes into syllables. Rothi and colleagues73 were not able to replicate the successful outcome of the speeded whole-word training for a patient with pure alexia that they accomplished in an earlier study.49 Another factor that requires consideration but is not included in Table 1 is the number of treatment sessions provided to accomplish a positive outcome. In some studies, fewer than 10 sessions were needed, whereas in other studies, as many as 9 months of treatment were administered. For further details of each study, the reader is referred to the original articles. Many of the treatment studies reported in Table 1 are primarily directed toward improved reading accuracy of a corpus of single words, with little information about the impact of these treatments on reading performance for connected texts, which often is the ultimate treatment goal.25 Treatment protocols that have targeted connected text are rare. One such technique that focuses on connected discourse has been called multiple oral rereading (MOR).51 Unlike other methods of treatment that usually involve repeated practice on isolated words to increase speed of word identification, MOR involves repeated reading aloud of the same text over a period of days or weeks. MOR was initially applied to a 30-year-old alexic patient with a transitory mild aphasia and resulted in a substantial gain in reading speed over a relatively short period of time.51 MOR has been used in later studies to improve letter-by-letter reading, and results have consistently indicated improved reading rate for practiced materials as well as for new material.25,52–54 In the following section, a case study is presented to illustrate how MOR was used successfully in a patient with phonological alexia. A second case study illustrates a different oral reading approach for acquired alexia, called oral reading for language in aphasia (ORLA).69 With this technique, the person with aphasia repeatedly reads aloud sentences and short paragraphs, first in unison with the clinician and then independently. The box titled “Oral Reading for Language in Aphasia (ORLA)” delineates the specific steps of ORLA. The treatment is based on a stimulation approach in which repetitive multimodality stimulation is presented to elicit a response. Responses are not forced Aphasia, Alexia, & Oral Reading Oral Reading for Language in Aphasia (ORLA) 1. The speech-language pathologist reads aloud to the patient, pointing to each word as he or she reads along. The length of the material may vary from 3 to 100 words, depending on the auditory comprehension skills of the patient. 2. The speech-language pathologist reads aloud to the patient again, pointing to each word as he or she reads along and encouraging the patient to also point to each word. 3. The speech-language pathologist reads the para- graph aloud together with the patient, while continuing to point to each word as he or she reads along. The patient also points to each word. The clinician adjusts the rate and volume of the oral reading according to the specific patient (e.g., reading a little ahead of the patient so he or she is able to hear the initial phonemes of the words; decreasing volume as he or she requires fewer cues). 4. For each line or sentence of the paragraph, the speech-language pathologist states a word that the patient must then identify. Words may be content words (e.g., nouns, verbs) or function words (e.g., pronouns, prepositions, conjunctions). 5. For each line or sentence of the paragraph, the speech-language pathologist points to a word for the patient to read aloud. Both content and function words are selected. 6. The patient reads the whole sentence aloud again in unison with the speech-language pathologist. or corrected; rather, correct responses are modeled while error responses are followed by further stimulation. The design of the ORLA technique is consistent with learning theory and adheres to principles such as active participation by the learner, repetitive practice in the over-learning of skills, use of meaningful materials, and successful experiences. ORLA is unique for several reasons. Like MOR, it focuses on connected discourse rather than single words, therefore it permits the modeling of more natural intonations and speech. Furthermore, it allows practice on a variety of grammatical structures, rather than just one specific grammatical form. Finally, the technique is quickly learned by patients because of its simplicity and ease of administration. In a study of 10 patients with different types of reading problems, ORLA was shown to be effec- 31 tive for all groups of patients regardless of the type, severity, and acuity of the associated aphasia.69 An important observation from this study indicated that improved oral reading preceded changes in reading comprehension. This finding lends support to the idea that as the patients learn to decode words more rapidly, they are able to direct their attention to comprehension of meaning, which results in improved comprehension scores. This study remains the largest published study of an oral reading treatment for patients with acquired reading problems. The ORLA technique was developed to target reading comprehension, but an interesting outcome of the study was that the patients’ language performance improved in all modalities, not only reading.69 Beeson and Insalaco noted similar findings; both their patients improved their aphasia quotients over the course of the oral reading treatment.25 The reasons for the occurrence of crossmodal generalization are not clear. Cherney and colleagues have suggested that the choral reading in their study provided repeated stimulation to the auditory comprehension modality as well as repeated practice in oral expression.69 Therefore, improvements in these modalities could be expected. Indeed, the ORLA treatment program was found to be an effective approach for treating apraxia of speech in two patients with Broca’s aphasia.74 ORLA may be effective because it incorporates three elements — rhythm, pacing, and linguistic templates — that have been identified as important to help establish an underlying oscillatory rhythm, melody, and rate for speech production.75 The patient’s paced pointing to each word of the sentence, together with the linguistic template provided by the clinician, may help facilitate the patient’s temporal flow and articulatory rate of speech. Although oral reading appears to give the patient practice with the grapheme-to-phoneme conversion process, Beeson and Insalaco explain the cross-modal generalization by suggesting that the interactive processing during oral reading also serves to strengthen partial or degraded lexical information.25 Therefore, the benefit is not purely at the level of the orthographic input lexicon but extends to language processing by other modalities as well. 32 TOPICS IN STROKE REHABILITATION/WINTER 2004 Oral Reading Treatment: Case Studies Multiple oral rereading (MOR) G.B., a 23-year-old male, initially presented with a moderately severe Wernicke’s aphasia after resection for an arteriovenous malformation in December 1998. He participated in approximately 6 months of intensive interdisciplinary rehabilitation, first as an inpatient at an acute rehabilitation facility and then as an outpatient in a day rehabilitation program. At the time of evaluation by this investigator at the end of May 2000, G.B. was no longer receiving any rehabilitation. His goal was to return to school, but he reported that his difficulty in reading prevented him from doing this. Testing indicated that G.B. presented with a mild anomic aphasia and an associated phonological alexia. The alexia was characterized by difficulty reading aloud nonwords and low frequency words. He was slow in sounding out letters to get to words, although this was a strategy that he attempted when presented with less familiar words. He could read aloud real words, particularly high frequency words. Errors were typically visual errors, in which the target word was read as another word with similar letters in it. G.B. completed the reading comprehension subtest of the Boston Diagnostic Aphasia Examination32 and achieved a score of 6/10. Oral reading rate of novel text was 34.6 words per minute. A reading comprehension test, the Gates-MacGinitie Reading Tests, Level D,76 geared for 4th–6th graders was attempted; however, G.B. was unable to proceed with the test because of slow reading and subsequent complaints of fatigue during reading. Because the patient lived geographically far from the investigator and insurance would no longer provide reimbursement for services, there was a need to provide a reading program that could be independently practiced by the patient. Therefore MOR was selected in which a family member chose an item from the newspaper and the patient would practice reading it aloud for 30 min each day for an entire week. All practice sessions were tape recorded; at the end of the week, tapes were sent to the investigator for review. Then a new item was selected by a family member for practice during the following week. Table 2 shows the initial reading rate of each item at the beginning of the week and the final reading rate that was accomplished at the end of each week. The patient was seen again in August 2000 after 6 weeks of practice, at which time the reading rate of novel material had not yet improved. However, G.B. was able to achieve reading rates of up to 100 words per minute at the end of a week of practicing and reported improved reading comprehension of the items. It was decided to continue with the MOR program. Because G.B. was compliant with all aspects of the treatment, he was only required to tape record the first and last reading of the week for submission to the investigator. After an additional 10 weeks, G.B. was re-evaluated in December 2000. He reported that his understanding of each new reading item had improved; he understood more of it the first time he read it. He also reported that he was able to achieve a faster reading rate much sooner, after just 2 or 3 days of practice. Reading rate of practiced text had increased to a maximum of 156 words per minute (normal oral reading rate is approximately 150–200 words per minute). During the assessment, reading rate of novel text had improved to 44 words per minute. The readTable 2. Initial and final weekly reading rates obtained by G.B. during independent MOR practice Week no. Evaluation 1 2 3 4 5 6 7 – Reevaluation 8 9 10 11 12 13 14 15 16 17 18 – Reevaluation Initial reading rate Final reading rate (words/minute) (words/minute) 34.6 43.2 67 38.3 95 31.5 68.6 35.6 100 37.6 87.3 33.9 87 34.7 37.7 97.2 29.6 128.5 49.8 155 26 105 No tape submitted 44 123 42 135 52 156 No tape submitted (Thanksgiving) 41 147 44 Aphasia, Alexia, & Oral Reading ing comprehension test (Gates-MacGinitie, Level D, 1978)76 was readministered and G.B. achieved a grade equivalent of 5.0. It should be noted that this is a timed test, and G.B. completed only 25 items of the total 43 items. For the items that he did complete, comprehension was high (96% accuracy). This test also offers a multiple-choice vocabulary test. For the vocabulary items, G.B. scored at a grade equivalency of 11.9. It was suggested that G.B. continue with the oral reading program on his own, but no further follow-up was scheduled because G.B. had moved out of state. Oral reading for language in aphasia (ORLA) V.P., a 39-year-old female, was evaluated in May 2003, more than 13 years after suffering a stroke during emergency surgery for a chronic gastrointestinal disorder. At the time of this evaluation, she presented with a moderate Broca’s aphasia and achieved an Aphasia Quotient of 62.8 on the Western Aphasia Battery.32 Additional testing included the reading and writing subtests of the Western Aphasia Battery and selected subtests of the Reading Comprehension Battery for Aphasia–2.34 Spontaneous language samples were obtained using two composite pictures and two picture sequences, and these were scored for Correct Information Units.77 These assessment results are included in Table 3. Oral reading of word lists from the Battery of Adult Reading Function was also completed.41 V.P. was unable to read aloud any nonwords. She read regular words, rule-governed words, and irregular words with 46%, 40%, and 36% accuracy, respectively. Errors were primarily semantic and morphological. She achieved 88% on a homonym–picture matching task, but only 38% on pseudohomonym–picture matching. Finally, she read a list of content words with 73% accuracy and a list of function words with 30% accuracy. These results are consistent with the presence of a deep alexia. The ORLA treatment was initiated, with V.P. attending a total of 24 one-hour treatment sessions over 7 weeks. Three groups of sentences, each with 30 sentences, were used. During the first 10 sessions, V.P. practiced Group 1 sentences that were three to five words in length. From sessions 11–24, 33 Table 3. Pre- and posttreatment test scores of V.P. WAB: AQ WAB: Reading WAB: Writing RCBA-2: Functional reading RCBA-2: Paragraph-picture RCBA-2: Paragraph factual RCBA-2: Paragraph inferential % CIU – Composite picture 1 % CIU – Composite picture 2 % CIU – Sequenced picture 1 % CIU – Sequenced picture 2 Pretreatment (5/21/03) Posttreatment (8/13/03) 62.8 51 48.5 6/10 5/10 1/10 0/10 59 74 66 48 67.7 61 51.5 7/10 8/10 7/10 6/10 50 81 73 74 Note: WAB = Western Aphasia Battery; AQ = Aphasia Quotient; RCBA = Reading Comprehension Battery for Aphasia; CIU = Correct Information Units. Group 2 sentences (i.e., stimuli that were 8 to10 words in length) were trained. Group 3 sentences were an untrained set with three- to five-word sentences. Daily oral reading probes of 10 randomly selected sentences from each of the groups were taken at the beginning of each treatment session. Figure 6 displays oral reading accuracy achieved on the probes during baseline and throughout treatment. It can be seen that accuracy on Group 1 sentences increased from a baseline score of about 60% to 90% after 10 sessions. Performance on Group 2 sentences varied from 58% to 68% during the first 10 sessions when she was not treated, and then improved to 84% during treatment. Some improvement in the accuracy of the untreated Group 3 sentences was evident but performance was variable between 68% and 78%. These results indicate that ORLA treatment is effective in improving oral reading of trained sentences. A reevaluation was conducted at the end of treatment and results are shown in Table 3. It can be seen that improvements were made in reading comprehension, as measured by the RCBA-2 and the reading subtests of the WAB. Cross-modal generalization was also evident. The WAB AQ, which measures auditory comprehension and oral expression, improved almost 5 points; CIU analysis indicated improvements in V.P.’s ability to describe pictures; and some improvements on the writing subtest of the WAB were also noted. These results indicate that, for V.P., an individual with chronic aphasia and deep alexia, ORLA was 34 TOPICS IN STROKE REHABILITATION/WINTER 2004 Percent Accuracy 100 80 Group 1 Treated 60 Group 2 Treated 40 Group 3 Untreated 20 0 1 4 7 10 13 16 19 22 25 Session Figure 6. Daily oral reading probes for V. P. Arrows indicate the beginning of treatment of each group of sentences. Sessions 1-3: baseline; Sessions 4-12: treatment – Group 1 (3- to 5-word sentences); Sessions 13-24: treatment – Group 2 (8- to 10-word sentences). effective in improving not only oral reading of sentences but also reading comprehension. In addition, generalized improvement to other language modalities resulted from the ORLA treatment. Conclusion This article has presented an overview of the acquired alexias, including classification, assessment, and treatment. The alexia therapies are idiosyncratic and are frequently highly individualized by the treating clinician to conform to a particular patient’s unique combination of deficits and residual capabilities. As a result, few therapy approaches have been sufficiently defined and critically evaluated with large numbers of patients. Yet, several studies have suggested that oral reading, particularly oral reading of connected text, may be an effective treatment mode. Two examples of how oral reading of connected text has been successfully used to treat acquired alexia have been provided. The rationale for using such an approach is derived from the neuropsychological models of normal reading and acquired alexias. Repeated reading aloud, particularly when done in unison with another individual, seems to provide practice primarily in grapheme-phoneme decoding. In addition, oral reading may strengthen partial or degraded lexical information, thereby positively impacting other language modalities. Additional studies with larger numbers of participants, detailed description of the specific reading problems, careful administration of the selected treatment, and frequent measurement of the patients’ response to treatment will help elucidate our understanding of the acquired alexias. Acknowledgments The preparation of this manuscript was supported by grant H133G010098 from the National Institute on Disability and Rehabilitation Research, US Department of Education. The author gratefully acknowledges the participation of G.B. and V.P. and extends thanks to Edna Babbitt and Jodi Oldani for their assessment and treatment of V.P. REFERENCES 1. Ardila A, Rosselli M. Spatial alexia. Int J Neurosci. 1994;76:49–59. 2. Behrmann M., Black SE, Bub D. The evolution of pure alexia: a longitudinal study of recovery. Brain Lang. 1990;39:405–427. 3. Hillis AE, Caramazzo A. The effects of attentional deficits on reading and spelling. In: Caramazzo A, ed. Cognitive Neuropsychology and Neurolinguistics. Hillsdale NJ: Lawrence Erlbaum; 1990:211–275. 4. Kinsbourne M, Warrington EK. A variety of reading Aphasia, Alexia, & Oral Reading 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. disability associated with right hemisphere lesions. J Neurol Neurosurg Psychiatry. 1962;25:339–344. Riddoch MJ, Humphreys GW, Cleton P, Fery P. Interaction of attentional and lexical processes in neglect dyslexia. Cogn Neuropsychol. 1990;7: 479–517. Warrington EK. Right neglect dyslexia: a single case study. Cogn Neuropsychol. 1991;8:193–212. Young AW, Newcombe F, Ellis AW. Different impairments contribute to neglect dyslexia. Cogn Neuropsychol. 1991;8:177–193. Benson DF, Ardila A. Aphasia: A Clinical Perspective. New York: Oxford University Press; 1996. Dejerine J. Sur un cas de cécité verbal avec agraphie, suivi d’autopsie. Mémoires de la Société de Biologie. 1891;3:197–201. Dejerine J. Contribution à l'etude anatomopathologique et clinique des differentes variétés de cécité verbale. Mémoires de la Société de Biologie 1892;4:61–90. Ellis AW. Reading, Writing and Dyslexia: A Cognitive Analysis. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum; 1993. Hillis AE, Caramazzo A. The reading process and its disorders. In: Margolin DI, ed. Cognitive Neuropsychology in Clinical Practice. New York: Oxford University Press; 1992:229–262. Marshall JC, Newcombe F. Patterns of paralexia: a psycholinguistic approach. J Psycholinguist Res. 1973;2:175–199. Morton J, Patterson KE. A new attempt at an interpretation, or an attempt at a new interpretation. In: Coltheart M, Patterson K, Marshall JC, eds. Deep Dyslexia. London: Routledge & Kegan Publishers; 1980:91–108. La Berge P, Samuals SJ. Towards a theory of automatic information processing in reading. Cogn Psychol. 1974:6;293–339. Barry C, Richardson JTE. Accounts of oral reading in deep dyslexia. In: Whitaker HA, ed. Phonological Processes and Brain Mechanisms. New York: Springer Verlag; 1988:119–171. Coltheart M, Patterson K, Marshall JC. Deep Dyslexia. London: Routledge & Kegan Paul; 1980. Coltheart M, Masterson J, Byng S, Prior M, Riddoch J. Surface dyslexia. Q J Exp Psychol. 1983;35A:469–495. Henderson L. Information processing approaches to acquired dyslexia. Q J Exp Psychol. 1981;33A: 507–522. Newcombe F, Marshall JC. On psycholinguistic classification of the acquired dyslexias. Bull Orton Society. 1981;31:29–46. Patterson KE. Phonemic dyslexia: errors of meaning and the meaning of errors. Q J Exp Psychol. 1978; 30:587–601. Patterson KE. Neuropsychological approaches to the study of reading. Br J Psychol. 1981;72:151–174. Patterson KE, Marshall JC, Coltheart M. Surface Dyslexia. London: Lawrence Erlbaum; 1985. Shallice T, Warrington E. Word recognition in a phonemic dyslexia patient. Q J Exp Psychol. 1975;27: 35 187–199. 25. Beeson PM, Insalaco D. Acquired alexia: lessons from successful treatment. J Int Neuropsychol Soc. 1998;4:621–635. 26. Friedman RB, Ween JE, Albert ML. Alexia. In: Heilman KM, Valenstein E. eds. Clinical Neuropsychology. 3rd ed. New York: Oxford University Press; 1993:37–62. 27. Goodglass H. Understanding Aphasia. San Diego: Academic Press; 1993. 28. Webb WG, Love RJ. Reading problems in chronic aphasia. J Speech Hearing Disord. 1983;48: 164–170. 29. Shallice T, Saffran EM. Lexical processing in the absence of explicit word-identification: evidence from a letter-by-letter reader. Cogn Neuropsychol. 1986;3:429–458. 30. Patterson KE, Kay J. Letter-by-letter reading: psychological descriptions of a neurological syndrome. Q J Exp Psychol. 1982:34A;411–441. 31. Kertesz A. Western Aphasia Battery. New York: Harcourt Brace Jovanovich; 1982. 32. Goodglass H, Kaplan E. The Assessment of Aphasia and Related Disorders. 3rd ed. Philadelphia: Lea & Febiger; 2000. 33. Friedman RB. Clinical diagnosis and treatment of reading disorders. In: Hillis AE, ed. The Handbook of Adult Language Disorders. New York: Psychology Press; 2002:27–43. 34. La Pointe LL, Horner J. Reading Comprehension Battery for Aphasia. 2nd ed. Austin, TX: Pro-Ed; 1998. 35. MacGinitie WH, MacGinitie RK, Maria K, Dreyer LG. Gates-MacGinitie Reading Tests. 4th ed. Itasca, IL: Riverside Publishing; 2000. 36. Woodcock RW. Woodcock Reading Mastery TestsRevised-Normative Update. Circle Pines, MN: American Guidance Service; 1998. 37. Brown JI, Fishco VV, Hanna GS. Nelson-Denny Reading Test. Itasca, IL: Riverside Publishing; 1993. 38. Kay J, Lesser R, Coltheart M. PALPA: Psycholinguistic Assessments of Language Processing in Aphasia. Hillsdale, NJ: Lawrence Erlbaum; 1992. 39. Goodman RA, Caramazza A. The Johns Hopkins Dyslexia Battery. Baltimore: Johns Hopkins University Press; 1986. 40. Beeson PM, Hillis AE. Comprehension and production of written words. In: Chapey R, ed. Language Intervention Strategies in Adult Aphasia. 4th ed. Baltimore, MD: Lippincott, Williams, & Williams; 2001:572–595. 41. Rothi LJG. Battery of adult reading function. Unpublished manuscript. 1985. 42. Wiederholt JL, Bryant BR. Gray Oral Reading Tests 4. Austin TX: Pro-Ed; 2001. 43. Katz RC, Wertz RT. The efficacy of computer-provided reading treatment for chronic aphasic adults. J Speech Lang Hearing Res. 1997;40:493–507. 44. Lott SN, Friedman RB, Linebaugh CW. Rationale and efficacy of a tactile-kinaesthetic treatment for alexia. Aphasiology. 1994;8:181–195. 45. Maher LM, Clayton MC, Barrett AM, Schober- 36 46. 47. 48. 49. 50. 51. 52. 53. 54. 55. 56. 57. 58. 59. 60. 61. 62. 63. TOPICS IN STROKE REHABILITATION/WINTER 2004 Peterson D, Gonzalez-Rothi LJ. Rehabilitation of a case of pure alexia: exploiting residual abilities. J Int Neuropsychol Soc. 1998;4:636–647. Greenwald ML, Gonzalez-Rothi LJ. Lexical access via letter naming in a profoundly alexic and anomic patient: a treatment study. J Int Neuropsychol Soc. 1998;4:595–607. Behrmann M, McCleod J. Rehabilitation for pure alexia: efficacy of therapy and implications for models of normal word recognition. In: Berndt RS, Mitchum CC, eds. Cognitive Neuropsychologcal Approaches to the Treatment of Language Disorders. Hillsdale NJ: Lawrence Erlbaum; 1995:149–180. Lott SN, Friedman RB. Can treatment for pure alexia improve letter-by-letter reading speed without sacrificing accuracy? Brain Lang. 1999;67:188–201. Rothi LJG, Moss S. Alexia without agraphia: potential for model assisted therapy. Clin Commun Disord. 1992;2:11–18. Friedman RB, Lott SN. Rapid word identification in pure alexia is lexical but not semantic. Brain Lang. 2000;72:219–237. Moyer S. Rehabilitation of alexia: A case study. Cortex. 1979;15:139–144. Moody S. The Moyer reading technique re-evaluated. Cortex. 1988;24:473–476. Tuomainen J, Laine M. Multiple oral rereading technique in rehabilitation of pure alexia. Aphasiology. 1991;5:401–409. Beeson PM. Treatment for letter-by-letter reading: a case study. In: Helm-Estabrooks N, Holland AL. eds. Approaches to the Treatment of Aphasia. San Diego, CA: Singular Press; 1998:153–177. Coltheart M, Byng S. A treatment for surface dyslexia. In: Seron X, Deloche G, eds. Cognitive Approaches to Neuropsychological Rehabilitation. Hillsdale, NJ: Lawrence Erlbaum; 1989:159–174. Weekes B, Coltheart M. Surface dyslexia and surface dysgraphia: treatment studies and their theoretical implications. Cogn Neuropsychol. 1996;13: 277–315. Scott C, Byng S. Computer assisted remediation of a homophone comprehension disorder in surface dyslexia. Aphasiology. 1989;3:301–320. Hillis AE. The role of models of language processing in rehabilitation of language impairments. Aphasiology. 1993;7:5–26. Friedman RB, Robinson SR. Whole-word training therapy in a stable surface alexic patient: it works. Aphasiology. 1991;5:521–528. Moss S, Rothi LJG, Funnell EB. Treating a case of surface dyslexia after closed head injury. J Clin Neuropsychol. 1991;6:35–47. DePartz MP. Re-education of a deep dyslexic patient: rationale of the method and results. Cogn Neuropsychol. 1986;3:149–177. Nickels L. The autocue? Self-generated phonemic cues in the treatment of a disorder of reading and naming. Cogn Neuropsychol. 1992;9:155–182. Friedman RB, Lott SN. Phonological treatment for deep dyslexia using bigraphs instead of graphemes. Brain Lang. 1996;55:116–118. 64. Yampolsky S, Waters G. Treatment of single word oral reading in an individual with deep dyslexia. Aphasiology. 2002;16:455–471. 65. Conway T, Heilman P, Rothi L, Alexander A, Adair J, Crosson B, Heilman K. Treatment of a case of phonological alexia with agraphia using the Auditory Discrimination in Depth (ADD) program. J Int Neuropsychol Soc. 1998;4:608–620. 66. Kendall DL, McNeil MR, Small SL. Rule-based treatment for acquired phonological dyslexia. Aphasiology. 1998;12:587–600. 67. Friedman RB, Sample DM, Lott SN. The role of level of representation in the use of paired associate learning for rehabilitation of alexia. Neuropsychologia. 2000;40:223–234. 68. Moody S. Remediation of acquired alexia. Clin Rehabil. 1988;2:291–298. 69. Cherney LR, Merbitz C, Grip J. Efficacy of oral reading in aphasia therapy outcome. Rehabil Lit. 1986;47:112–118. 70. Wilson BA. Syndromes of acquired dyslexia and patterns of recovery: a 6-10 year follow-up study of seven brain-injured people. J Clin Exp Neuropsychol. 1994;16:354–371. 71. Laine M, Niemi J. Can the oral reading skills be rehabilitated in deep dyslexia? In: Hietanen M, Vilkki J, Niemi ML, Korkman M, eds. Clinical Neuropsychology: Excursions into the Field in Finland. Rauma Finland: Acta Psychologica Fennica; 1990:80–85. 72. Mitchum CC, Berndt RS. Diagnosis and treatment of the non-lexical route in acquired dyslexia: an illustration of the cognitive neuropsychological approach. J Neurolinguistics. 1991;6:103–137. 73. Rothi LJG, Greenwald ML, Maher LM, Ochipa C. Alexia without agraphia: lesssons from a treatment failure. In: Helm-Estabrooks N, Holland AL, eds. Approaches to the Treatment of Aphasia. San Diego, CA: Singular Press; 1998:179–201. 74. Cherney LR. Efficacy of oral reading in the treatment of two patients with chronic Broca’s aphasia. Top Stroke Rehabil. 1995;2:57–67. 75. Square PA, Martin RE. The nature and treatment of neuromotor speech disorders in adults. In: Chapey R, ed. Language Intervention Strategies in Adult Aphasia. 3rd ed. Baltimore, MD: Williams & Wilkins; 1994:467–499. 76. MacGinitie WH. Gates-MacGinitie Reading Tests. 2nd ed. Boston, MA: Houghton Mifflin Company; 1978. 77. Nicholas LE, Brookshire RH. A system for quantifying the informativeness and efficiency of the connected speech of adults with aphasia. J Speech Hearing Res. 1993;36:338–350. 78. Mayer JF, Murray LL. Approaches to the treatment of alexia in chronic aphasia. Aphasiology. 2002;16:727–743. 79. Kiran S, Thompson CK, Hashimoto N. Training grapheme to phoneme conversion in patients with oral reading and naming deficits: a model-based approach. Aphasiology. 2001;15:855–876.
Anuncio
Documentos relacionados
Descargar
Anuncio
Añadir este documento a la recogida (s)
Puede agregar este documento a su colección de estudio (s)
Iniciar sesión Disponible sólo para usuarios autorizadosAñadir a este documento guardado
Puede agregar este documento a su lista guardada
Iniciar sesión Disponible sólo para usuarios autorizados