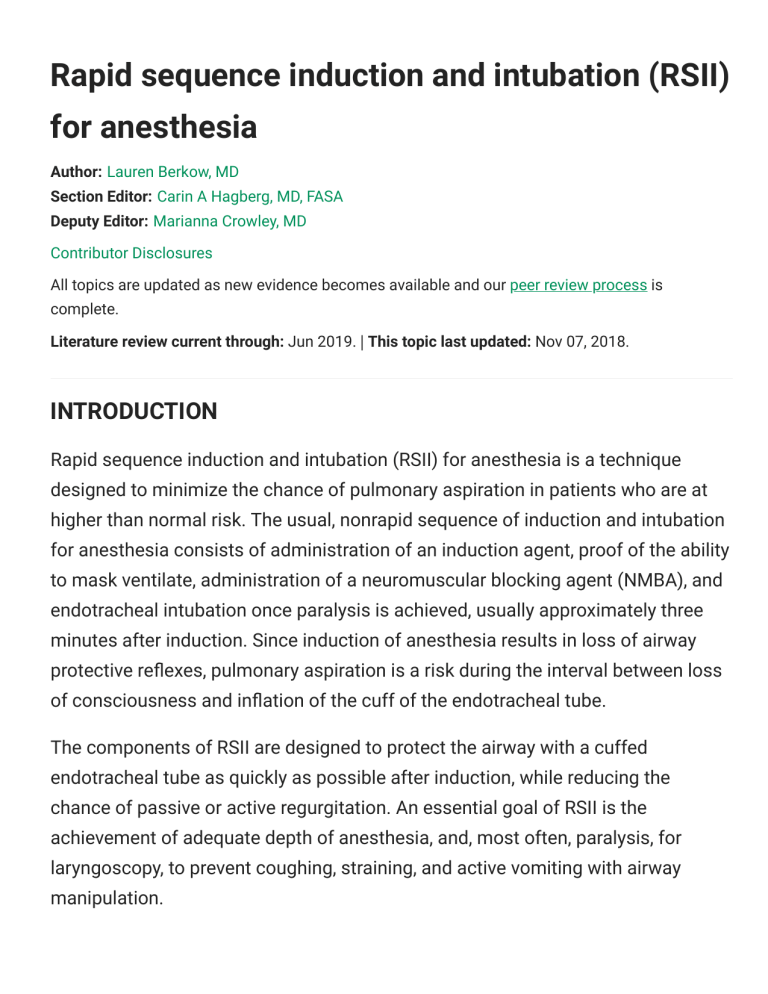
Rapid sequence induction and intubation (RSII) for anesthesia Author: Lauren Berkow, MD Section Editor: Carin A Hagberg, MD, FASA Deputy Editor: Marianna Crowley, MD Contributor Disclosures All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jun 2019. | This topic last updated: Nov 07, 2018. INTRODUCTION Rapid sequence induction and intubation (RSII) for anesthesia is a technique designed to minimize the chance of pulmonary aspiration in patients who are at higher than normal risk. The usual, nonrapid sequence of induction and intubation for anesthesia consists of administration of an induction agent, proof of the ability to mask ventilate, administration of a neuromuscular blocking agent (NMBA), and endotracheal intubation once paralysis is achieved, usually approximately three minutes after induction. Since induction of anesthesia results in loss of airway protective reflexes, pulmonary aspiration is a risk during the interval between loss of consciousness and inflation of the cuff of the endotracheal tube. The components of RSII are designed to protect the airway with a cuffed endotracheal tube as quickly as possible after induction, while reducing the chance of passive or active regurgitation. An essential goal of RSII is the achievement of adequate depth of anesthesia, and, most often, paralysis, for laryngoscopy, to prevent coughing, straining, and active vomiting with airway manipulation. While RSII is a departure from the usual practice of induction of anesthesia, the equivalent method of rapid airway control, often called "rapid sequence intubation" (RSI), is the most commonly used method of controlling the airway in the emergency room. This topic will discuss the components, techniques, and medications used for RSII for anesthesia. Preoperative fasting guidelines, airway management for induction of anesthesia, rapid sequence intubation in the emergency department, and medications used for induction of anesthesia are discussed more fully separately. (See "General anesthesia: Induction" and "Preoperative fasting guidelines" and "Airway management for induction of general anesthesia" and "Rapid sequence intubation for adults outside the operating room".) INDICATIONS General indications — RSII should be considered for the patient who is at increased risk of aspiration with induction of anesthesia. This includes the patient with a full stomach, gastrointestinal pathology, increased abdominal pressure, or pregnancy after 20 weeks gestation (table 1): ● Patients with a full stomach, which includes: • Patients undergoing emergency surgery • Patients who have sustained trauma, regardless of the interval since last oral intake • Patients who have not fasted according to preoperative fasting guidelines (see "Preoperative fasting guidelines") ● Patients with gastrointestinal pathology, which includes: • Gastroparesis • Small bowel obstruction • Gastric outlet obstruction • Esophageal stricture • Gastroesophageal reflux disease (see 'Gastroesophageal reflux disease (GERD)' below) ● Patients with increased intraabdominal pressure, which includes those with: • Morbid obesity • Ascites ● Pregnancy after 20 weeks gestation; earlier if symptoms of gastroesophageal reflux (controversial) (see "Management of the pregnant patient undergoing nonobstetric surgery", section on 'Aspiration mitigation') Gastroesophageal reflux disease (GERD) — GERD is a common condition that may put patients at risk for passive regurgitation and subsequent aspiration during induction of anesthesia. Patient selection — The decision to perform RSII for patients with GERD must be individualized based on the degree of symptoms and the potential risk of RSII. Patients should be questioned about symptoms of reflux during preoperative evaluation, including the presence of heartburn, regurgitation, dysphagia, reflux symptoms at night, and the need to sleep with the head of the bed elevated to avoid reflux. We consider RSII for the following patients: ● Patients with current symptoms of active reflux (ie, regurgitation, heartburn, or the need to sleep with the head of the bed elevated) ● Patients who had significant symptoms of active reflux prior to starting antacid medication, such as proton pump inhibitor (PPI), histamine-2 receptor antagonist (H2RA), or calcium carbonate ● Patients who believe that symptoms of reflux would recur if antacid therapy was discontinued ● Patients with hiatal hernia or endoscopic evidence of GERD We do not routinely perform RSII for patients who report heartburn only with spicy or acidic foods. Clinical manifestations, diagnosis, and management of GERD are discussed more fully separately. (See "Clinical manifestations and diagnosis of gastroesophageal reflux disease in children and adolescents" and "Medical management of gastroesophageal reflux disease in adults".) Preoperative antacids — Patients presenting for elective surgery who take antacid medication, including PPIs and H2RAs, on a regular or as-needed basis should be instructed to take their usual medication before surgery. PPIs are more effective at reducing gastric volume and pH if given in two doses, one the evening prior to surgery, and another on the morning of surgery [1,2]. A single dose of oral ranitidine three hours prior to induction of anesthesia has been shown to significantly reduce gastric volume and increase pH of stomach contents. PREPARATION FOR ANESTHESIA In addition to the preparation for routine induction of anesthesia, an assistant should be present who understands RSII and is capable of correctly applying cricoid pressure to assist in airway management. Airway evaluation — Airway evaluation is an important step in making the decision to perform an RSII. If a difficult airway is predicted, the risk of aspiration must be weighed against the risk of difficult or failed airway management. This is because RSII usually includes the administration of a neuromuscular blocking agent (NMBA) without proof that mask ventilation will be possible once the patient is paralyzed. In all but the most emergent situations, a quick airway examination and query about previous airway problems should be possible. If difficult airway management is expected, a modified RSII, awake intubation, or even an inhalation induction may be chosen as alternatives. (See "Airway management for induction of general anesthesia", section on 'Prediction of the difficult airway' and 'Potential complications of RSII' below.) Equipment — Preparation of equipment for RSII should be similar to that for routine induction. An assortment of standard and alternative airway devices should be immediately available, including small, medium, and large facemasks; several sizes and types of laryngoscopes; oral and nasal airways; several sizes of supraglottic airway, and a bougie. Alternative devices for laryngoscopy, including a video laryngoscope and flexible intubating scope, as well as other emergency airway equipment, should be accessible quickly and present in the operating room or anesthetizing location if difficult airway is suspected. Working suction must always be close by during induction of anesthesia; for RSII, we usually place the suction directly under the headrest for immediate access. Premedication — Premedication may be administered prior to RSII to relieve anxiety, to blunt or eliminate the physiologic response to airway management, and to reduce the volume or increase the pH of stomach contents. ● Anxiolytics – For patients who are hemodynamically stable, a benzodiazepine (eg, midazolam up to 1 to 2 mg IV) may be administered to reduce anxiety. This dose should be titrated cautiously in older adults and when given simultaneously with narcotic premedication, to avoid hypotension and loss of protective airway reflexes [3]. ● Atropine – The administration of succinylcholine and airway manipulation can trigger a vagal response, especially in children and neonates. We therefore suggest the use of atropine with RSII for all children younger than one year and for children less than five years of age who receive succinylcholine, though succinylcholine is rarely administered to children in the operating room. (See "Rapid sequence intubation (RSI) outside the operating room in children: Approach", section on 'Pretreatment'.) A vagal response to straightforward endotracheal intubation is much less common in adults; as such, atropine is not routinely administered as a premedication before RSII for adults. However, anticholinergic treatment may be required if bradycardia occurs with difficult laryngoscopy and intubation, or as a result of intubation in patients with preexisting bradycardia caused by medication or conduction system disease [4-6]. ● Opioids – Opioids may be administered as part of premedication for analgesia and sedation. They should be titrated to avoid respiratory depression and loss of protective airway reflexes in patients at risk for aspiration, especially in older patients, and when administered with benzodiazepines. ● Antacids – We suggest premedication with antacids prior to induction of anesthesia for patients at high risk of aspiration to increase the pH of gastric contents so that, if aspiration does occur, it will result in less pulmonary damage. Several classes of antacid medication are routinely used: • Clear, nonparticulate oral antacid (eg, sodium citrate-citric acid, 30 mL orally immediately prior to induction) increases pH of stomach contents [7]. • Histamine-2 receptor antagonist (H2RA) (eg, ranitidine 50 mg IV or famotidine 20 mg IV, given 40 to 60 minutes prior to induction) reduces the volume and increases the pH of stomach contents. For pregnant patients and for those at high risk of aspiration, we routinely administer clear, nonparticulate antacid prior to induction. For nonpregnant patients at high risk of aspiration who have not received a proton pump inhibitor (PPI) or H2RA on the morning of surgery, we also administer an H2RA 40 to 60 minutes prior to induction. ● Prokinetic agent – Intravenous (IV) metoclopramide increases lower esophageal sphincter tone [8], induces peristalsis, and enhances stomach emptying, thereby reducing gastric volume and the risk of regurgitation. Metoclopramide is particularly useful in patients with gastroparesis undergoing general anesthesia. It is also antiemetic and may help prevent postoperative nausea and vomiting. Rare adverse effects of metoclopramide include extrapyramidal effects and tardive dyskinesia, which are more common if administered quickly. We reserve metoclopramide for patients with uncontrolled reflux and pregnant patients who are symptomatic with reflux. In this setting, we administer metoclopramide 10 mg IV over one to two minutes. Positioning — The patient's head should be positioned in the sniffing position to facilitate intubation (atlanto-occipital extension with head elevation of 3 to 7 cm). Obese patients may require a ramped position (figure 1). (See "Airway management for induction of general anesthesia", section on 'Patient positioning'.) When RSII is planned, we prefer to position the operating table with the head up because passive regurgitation and aspiration may be less likely if the larynx is above the level of the lower esophageal sphincter. We flex the hips to elevate the back of the operating table, or tilt the table 20 degrees head up, making sure that once that is done, the height of the patient's head is optimal for intubation. Should the patient regurgitate prior to or during induction, the table should be quickly tipped head down, the patient's head turned to the side, and the mouth suctioned to avoid aspiration. Preoxygenation — All patients presenting for general anesthesia should be preoxygenated with 100 percent oxygen to increase oxygen reserve and provide additional time to secure the airway. This is particularly important prior to RSII, since with this technique, mask ventilation is not usually performed between induction and intubation. Preoxygenation is administered for three minutes of normal tidal volume breathing, for eight deep breaths over one minute, or until the fraction of expired oxygen is over 90 percent [9]. (See 'Mask ventilation' below.) The use of nasal cannula for passive apneic oxygenation during laryngoscopy can prolong the time to desaturation in high-risk patients during airway management [10-12]. We suggest the administration of oxygen by nasal cannula at 10 L in addition to facemask oxygen for those patients who are at high risk for rapid oxygen desaturation during the apneic period between induction and intubation, and for those at higher risk of difficult intubation. Methods for apneic oxygenation have become available that may be useful for preoxygenation as well as passive oxygenation during RSII. The transnasal humidified rapid insufflation ventilatory exchange (THRIVE) technique uses a device that provides humidified high-flow nasal oxygen with continuous positive airway pressure (CPAP). THRIVE may maintain a blood gas profile equivalent to face mask preoxygenation in spite of longer apnea time [13,14]. (See "Preoxygenation and apneic oxygenation for intubation".) A number of studies have shown either more rapid or effective preoxygenation or increased time to desaturation after apnea with the use of CPAP during preoxygenation [15-17]. CPAP can be provided using a tight-fitting anesthesia face mask, and pressure support ventilation provided with positive end-expiratory pressure (PEEP). Morbidly obese patients in particular may benefit from CPAP preoxygenation. Low levels of inspiratory pressure should be used to avoid gastric insufflation. CRICOID PRESSURE DURING RSII Although controversial, we routinely apply cricoid pressure (also known as Sellick's maneuver) prior to and during RSII until confirmation of correct endotracheal tube placement. Despite conflicting evidence regarding the effectiveness of cricoid pressure for preventing regurgitation, clinical experience suggests that, in most situations, it is not harmful and may be beneficial. The most significant downside to the use of cricoid pressure is the possibility that it may make laryngoscopy, supraglottic airway placement, or mask ventilation more difficult. We routinely have an assistant apply cricoid pressure during RSII, but we communicate the need to shift or release the pressure as necessary to facilitate endotracheal intubation. Cricoid pressure may have to be released if intubation proves difficult and/or mask ventilation, supraglottic airway placement, or flexible fiberoptic bronchoscopy become necessary. Indeed, the 2015 Difficult Airway Society guidelines from the United Kingdom recommend that cricoid pressure be released if initial attempts at laryngoscopy are difficult [18]. Should active vomiting occur, cricoid pressure should be released to avoid esophageal rupture. We do not routinely use cricoid pressure during RSII for patients with acute cervical spinal cord injury because it can move unstable cervical spine fractures. In trauma patients with possible but unevaluated cervical spine injury, cricoid pressure should only be used along with manual in line stabilization to stabilize the posterior cervical spine. (See "Anesthesia for adults with acute spinal cord injury", section on 'Airway management strategy'.) As originally described by Sellick in 1961, the cricoid cartilage ring is pressed backward by an assistant against the underlying cervical vertebrae, occluding the lumen of the esophagus to prevent regurgitation of stomach contents into the pharynx (figure 2) [19]. Based on cadaver and patient studies, pressure should be applied at 10 Newtons (approximately 2.5 lbs) while the patient is awake and increased to 30 Newtons after loss of consciousness. Despite these recommendations, clinicians and assistants are not routinely trained to standardize application of pressure [20-22]. While optimal external laryngeal manipulation (OELM) of the thyroid cartilage is often used to improve the view of the vocal cords during laryngoscopy, cricoid pressure should not be applied in an attempt to improve laryngeal view, as it may in fact make the view worse. Cricoid pressure controversies — The need for, efficacy, anatomical basis, and optimal technique for application of cricoid pressure have all been questioned, and literature is inconclusive. Some guidelines, including the American Heart Association Guidelines for Cardiopulmonary Resuscitation, no longer recommend the routine use of cricoid pressure [23]. Only two randomized controlled trials have evaluated cricoid pressure for RSII with direct laryngoscopy [24]. In one of these trials, the primary outcome was the pressor response to endotracheal intubation; there was no difference between patients who had cricoid pressure applied and those who did not [25]. The other trial, which evaluated aspiration and intubating conditions with and without cricoid pressure, was a prospective, randomized, multicenter study of 3472 patients who required RSII for increased risk of aspiration [26]. There was no difference in the incidence of aspiration (0.6 percent with cricoid pressure versus 0.5 percent without). Median intubation time was longer in patients who had cricoid pressure applied (27 versus 23 seconds), and there was higher incidence of Cormack Lehane grade 3 or 4 laryngeal views with cricoid pressure (10 versus 5 percent) (figure 3). (See "Direct laryngoscopy and endotracheal intubation in adults", section on 'Glottic view scores'.) ● Evidence that cricoid pressure may reduce the incidence of aspiration of gastric contents is scant and consists primarily of observational clinical studies and experimental data from cadaver studies [27], including the following: • Cadaver studies have shown that cricoid pressure prevents reflux of saline into the pharynx at esophageal pressures up to 50 cmH2O [20,2830]. • Several studies have shown that cricoid pressure prevents gastric insufflation during mask ventilation in children and adults [31-33]. • An observational study performed in patients undergoing elective surgery reported that cricoid pressure applied at 30 Newtons effectively occluded the upper esophagus, as determined by the inability to pass gastric tubes of two different sizes [34]. • There are case reports of regurgitation when cricoid pressure was released [19,35]. ● Lack of efficacy of cricoid pressure and possible harm are suggested by several studies and observations, as follows: • The anatomical basis for the use of cricoid pressure has been questioned by imaging studies. Both computed tomography (CT) and magnetic resonance imaging (MRI) studies have shown that the esophagus is located lateral to the midline in approximately 50 percent of patients [36,37]. The application of cricoid pressure displaced the esophagus laterally in 90 percent of subjects [37], suggesting that the esophagus would not be occluded by pressing the cartilage against cervical vertebrae. In contrast, an MRI study showed that application of 2 to 4 kg of cricoid pressure moved the cricoid cartilage and the hypopharynx as one unit, effectively obliterating the lumen of the alimentary tract, even with lateral displacement [38]. • Cricoid pressure at 20 Newtons has been shown to reduce lower esophageal pressure in awake, un-anesthetized volunteers (presumably by reflex), with restoration to baseline after release of pressure [39]. If applicable to anesthetized patients, this effect could theoretically increase the chance of gastroesophageal reflux, though it isn't clear whether this would increase the chance of reflux into the pharynx. Another study of awake volunteers reported that application of cricoid pressure did not promote gastroesophageal reflux [40]. • Several studies have reported a worsened Cormack Lehane grade view during laryngoscopy, prolonged time to intubation, and/or airway obstruction with the use of cricoid pressure [27,41-45]. NASOGASTRIC TUBE For patients with bowel obstruction, ileus, and other gastrointestinal pathology, some clinicians place a nasogastric tube to decompress the stomach prior to induction of anesthesia. Nasogastric drainage or suction does not guarantee an empty stomach and may not remove particulate matter. Such patients often present for anesthesia and surgery with a nasogastric tube already in place. We generally leave the nasogastric tube in place during RSII, connect it to suction to drain the stomach prior to induction, and then leave it open to air as a vent for the stomach. The stomach is suctioned again prior to emergence. While presence of a nasogastric tube may impair the function of the lower and upper esophageal sphincters [46], two cadaver studies have shown that cricoid pressure effectively prevents regurgitation of stomach contents with a nasogastric tube in place [21,28]. In addition, the nasogastric tube can help identify the esophagus during laryngoscopy and therefore make esophageal intubation less likely. CHOICE OF MEDICATIONS Since the aim of RSII is to place an endotracheal tube as quickly as possible after loss of consciousness, all medications used should be rapid in onset, without significant hemodynamic effects when given at the required doses, and should achieve optimal intubating conditions. Depending on the planned surgical procedure, a short duration of action or reversibility may be desirable as well. An important goal of RSII is the achievement of an adequate depth of anesthesia and, in most cases, paralysis to prevent coughing, gagging, straining, or vomiting during airway manipulation. Induction agents Dose and timing of induction agent — We typically titrate the anesthesia induction agent to loss of consciousness prior to the administration of neuromuscular blocking agent (NMBA). As RSII was originally described, a precalculated dose of an induction drug was administered, immediately followed by an NMBA. This timing can result in either underdosing, with the possibility of awareness or an undesirable sympathetic response to intubation, or to overdosing, with the possibility of hypotension. An alternative method of administration is to titrate the induction medication to loss of consciousness, recognizing that total induction time may be slightly longer with a titration technique. There are no data comparing the risk of aspiration, awareness, or hemodynamic consequence of RSII using the titration versus bolus technique. Choice of agent — Propofol is the induction agent we use most commonly for RSII, but the choice, dose, and speed of administration of the induction agent should be individualized. Patients presenting for emergency surgery may be hypovolemic or have other comorbidities that increase the risk of hemodynamic instability with induction. Ketamine and etomidate are alternatives to propofol for patients at increased risk of hypotension with induction. Propofol — Propofol is the most commonly used medication for induction of anesthesia and for RSII. Advantages for RSII include its rapid onset (30 to 45 seconds) and its ability to suppress airway reflexes and produce apnea [47]. Duration of action of propofol is short (5 to 10 minutes), which is an advantage if airway management is difficult and the patient must be awakened. However, the short duration of action means that repeat doses of propofol may be required if airway management is prolonged. (See "General anesthesia: Intravenous induction agents", section on 'Propofol'.) Propofol can cause hypotension because of dose-dependent venodilation, arterial dilation, and decrease in cardiac contractility [48]. The usual induction dose for RSII is 2 mg/kg, with reduced doses for patients at increased risk of hypotension [47]. Etomidate — Etomidate is an imidazole drug that inhibits GABA receptors, with a fast onset and short duration of action. Unlike propofol, etomidate does not cause vasodilation or myocardial depression, an advantage for patients who are at increased risk for hypotension [49]. For RSII, the induction dose of etomidate is 0.2 to 0.4 mg/kg IV, with rapid onset (30 to 45 seconds) and duration of action of 5 to 15 minutes [50]. (See "General anesthesia: Intravenous induction agents", section on 'Etomidate'.) Etomidate has been associated with adrenal suppression in the first 12 hours after a single dose and may prevent a rise in cortisol in response to a surgical stimulus [49]. However, a systematic review including six trials (772 patients) reported that a single induction dose of etomidate for endotracheal intubation in critically ill patients was not associated with increased mortality compared with other induction agents [51]. Ketamine — Ketamine is an NMDA receptor antagonist used for induction of anesthesia. It is a mild direct myocardial depressant [52], but in patients with an intact autonomic nervous system, it increases sympathetic tone, resulting in an increase in blood pressure, heart rate, and cardiac output [53]. Thus, ketamine is an alternative to etomidate for patients at risk for hypotension. However, sympathetic stimulation with administration of ketamine is dependent upon the presence of adequate sympathetic reserve. In the patient who has maximally activated the sympathetic response and depleted all reserve (eg, patients with profound hypovolemic shock), ketamine administration may result in hypotension as a result of myocardial depression. The RSII induction dose of ketamine is 1 to 2 mg/kg IV. (See "General anesthesia: Intravenous induction agents", section on 'Ketamine'.) Induction with ketamine for patients with traumatic brain injury is controversial. The concern is that ketamine may increase cerebral blood flow and intracranial pressure (ICP), thereby reducing cerebral perfusion. However, since it increases cardiac output and maintains mean arterial pressure, cerebral perfusion may actually increase. We believe that ketamine is an appropriate induction agent for RSII in patients with suspected ICP elevation and normal blood pressure or hypotension. In patients with hypertension and suspected ICP elevation, ketamine should be avoided because of its tendency to further elevate blood pressure. Barbiturates — Prior to the introduction of propofol, thiopental was the most commonly used agent for both routine induction of anesthesia and RSII. It is no longer available in the United States, though it is still used in other parts of the world. Methohexital is another barbiturate used for induction, with limited availability in the United States. With an induction dose of thiopental, 3 to 5 mg/kg IV, the time to effect is less than 30 seconds, and the duration of action is approximately 5 to 10 minutes. The induction dose of methohexital is 1 to 3 mg/kg IV, with similar time to effect and duration of action [54]. (See "General anesthesia: Intravenous induction agents", section on 'Methohexital'.) Both barbiturates are myocardial depressants and venodilators, and can cause hypotension. Doses should be reduced for older patients and for those at risk for hypotension. In addition, thiopental releases histamine and should be avoided in patients with asthma or reactive airway disease [55]. Opioids — Short-acting opioids (eg, fentanyl 1 to 3 mcg/kg IV three minutes prior to induction) is usually administered to reduce the sympathetic nervous system response to intubation. Remifentanil, an ultrashort-acting opioid, can be administered to profoundly suppress airway reflexes for intubation when the administration of NMBA is undesirable or contraindicated. (See 'Remifentanil intubation' below and "General anesthesia: Induction", section on 'Induction with endotracheal intubation'.) Lidocaine — Lidocaine (eg, 1 to 1.5 mg/kg IV given two minutes prior to intubation) is administered to blunt the sympathetic response to laryngoscopy and suppress the cough reflex [56-59]. Lidocaine pretreatment may prevent or decrease the transient rise in intracranial pressure with laryngoscopy and intubation, though studies of this effect have reached contradictory conclusions. Hypotension may occur with administration of higher doses of intravenous lidocaine [60]. (See "Pretreatment medications for rapid sequence intubation in adults outside the operating room", section on 'Lidocaine' and "General anesthesia: Induction", section on 'Induction with endotracheal intubation'.) Neuromuscular blocking agents (NMBAs) — NMBAs are administered for RSII to achieve optimal intubating conditions and to prevent coughing, gagging, straining, and vomiting as a result of airway manipulation. Succinylcholine — Unless contraindicated, for most cases we suggest the use of succinylcholine (1 to 1.5 mg/kg) rather than nondepolarizing NMBAs for RSII because it provides excellent intubating conditions within 30 to 60 seconds. [61]. Paralysis is achieved once fasciculations have stopped, at which point intubation can be performed. If a defasciculating dose of a nondepolarizing NMBA is administered in addition, the dose of succinylcholine must be increased to 1.5 to 2 mg/kg IV to overcome the antagonism between nondepolarizing and depolarizing NMBAs. (See "Clinical use of neuromuscular blocking agents in anesthesia", section on 'Drug interactions'.) Succinylcholine causes muscle fasciculations in most patients, which tend to be more severe in younger and more muscular patients. Administration of succinylcholine can increase intragastric pressure, primarily as a result of fasciculation of abdominal musculature, though this effect is variable [62]. A study of thiopental/succinylcholine induction in young, unpremedicated male patients reported increases in intragastric pressure as high as 30 cmH2O over baseline. The increase was prevented by administration of a defasciculating dose of nondepolarizing NMBA (eg, vecuronium, rocuronium, cisatracurium). The potential increase in intragastric pressure may be of particular concern in patients with reduced competence of the lower esophageal sphincter, such as those with abdominal distention, hiatal hernia, pregnancy, and gastroesophageal reflux. (See 'Defasciculation' below.) When masseter muscle spasm occurs after succinylcholine, administration of a nondepolarizing NMDA may or may not successfully resolve the spasm [63]. If endotracheal intubation is not possible, mask ventilation should be attempted, and preparations for a surgical airway should be made. Rarely, masseter muscle spasm progresses to spasm in extremities and may herald malignant hyperthermia. Isolated masseter spasm usually resolves over approximately 20 minutes [64]. Succinylcholine is discussed more fully separately. (See "Clinical use of neuromuscular blocking agents in anesthesia", section on 'Succinylcholine'.) Defasciculation — We do not routinely administer a defasciculating dose of nondepolarizing NMBA before succinylcholine, though other clinicians do. A small dose of nondepolarizing NMBA has been shown to reduce the fasciculations, myalgias, and the increase in intragastric pressure that result from administration of succinylcholine [62,65]. The defasciculating dose should be 10 percent of the ED95 for the chosen drug (ie, 2 mg rocuronium IV, 1.5 mg cisatracurium IV, or 0.3 mg vecuronium IV) given two to three minutes prior to induction. (The ED95 is the median dose of NMBA which results in 95 percent twitch depression, and is typically much lower than the intubating dose) (table 2). (See "Clinical use of neuromuscular blocking agents in anesthesia", section on 'Endotracheal intubation'.) Higher doses may result in signs of paralysis, including diplopia and difficulty breathing or swallowing, and should be avoided. If a defasciculating dose is administered, the dose of succinylcholine must be increased to 1.5 to 2 mg/kg IV to overcome the antagonism between nondepolarizing and depolarizing NMBAs [66]. Without fasciculations as a marker for paralysis, a peripheral nerve stimulator may be used to confirm adequate relaxation for intubation. A number of other drugs have been studied as pretreatment to prevent fasciculations and myalgias, with variable results. A meta-analysis of randomized trials concluded that succinylcholine-induced fasciculations are best prevented with pretreatment with NMBAs, lidocaine, or magnesium [65]. Alternatives to succinylcholine Nondepolarizing NMBAs — All nondepolarizing NMBAs have a slower time to onset and longer duration of action than succinylcholine. When the use of succinylcholine is contraindicated, high doses of nondepolarizing NMBA can be administered to speed the onset of paralysis. However, the clinical duration of paralysis will be much longer with the use of these higher doses. This may be problematic when shorter surgery is planned or when nerve monitoring will be used during surgery. In addition, if airway management proves difficult, prolonged paralysis eliminates the option of awakening the patient to allow spontaneous ventilation. (See "Clinical use of neuromuscular blocking agents in anesthesia", section on 'Nondepolarizing neuromuscular blocking agents'.) ● Rocuronium – When administered for RSII, rocuronium is the nondepolarizing NMBA that allows the fastest onset of action and the best intubating conditions, with the least side effects. A relatively high dose of rocuronium is required for RSII. In a meta-analysis of 50 trials that compared the use of succinylcholine with rocuronium for RSII, succinylcholine >1m/kg IV provided superior intubating conditions compared with rocuronium 0.6 to 0.7 mg/kg IV, but there was no difference in intubating conditions when rocuronium 0.9 to 1.0 mg/kg IV was administered [67]. The onset and duration of neuromuscular block depends on the dose. After induction of anesthesia with thiopental, rocuronium 0.9 to 1.2 mg/kg IV achieves maximal neuromuscular block in 55 to 75 seconds, with clinical duration (recovery of twitch to 25 percent of control) of 53 to 73 minutes [68]. In contrast, succinylcholine 1.5 mg IV achieves maximal block in 45 to 60 seconds, with a clinical duration of 6 to 10 minutes [69]. Sugammadex is a novel medication that can reverse the effects of rocuronium. Sugammadex functions as a chelating agent for rocuronium and can rapidly reverse neuromuscular blockade even after the administration of high doses of rocuronium [70]. Importantly, sugammadex may not reverse the effects of muscle relaxation quickly enough to consider it a "rescue" medication in the cannot intubate, cannot ventilate scenario, especially in the setting of other depressant medications [71]. Sugammadex is discussed more fully separately. (See "Clinical use of neuromuscular blocking agents in anesthesia", section on 'Sugammadex'.) While less desirable than rocuronium, cisatracurium and vecuronium are two other commonly used nondepolarizing NMBAs that can be used for RSII. As compared with rocuronium, the onset of paralysis with each of these is slower. Rapid onset of paralysis can be achieved by administration of a high dose, which results in prolonged duration of action, or by using a priming dose, that is, a small dose (10 percent of the intubating dose), of NMBA two to four minutes prior to the intubating dose of the drug. Since the priming dose of NMBA may cause signs of paralysis, including diplopia, blurry vision, difficulty swallowing, and risk of aspiration [72], we do not routinely administer a priming dose of NMBA. Recommended doses of vecuronium and cisatracurium for RSII are as follows: ● Vecuronium – 0.1 mg/kg IV (approximately 2 x ED95) results in a time to maximum block of 2.4 minutes with a clinical duration (recovery of twitch to 25 percent of control) of 44 minutes [73]. Like Rocuronium, Vecuronium can be reversed with sugammadex. ● Cisatracurium – 0.4 mg/kg IV (approximately 8 x ED95) results in a time to maximum block of 1.9 minutes with a clinical duration (recovery of twitch to 25 percent of control) of 91 minutes [74]. If a nondepolarizing NMBA is used (instead of succinylcholine or for defasciculation), fasciculations do not occur as a marker of paralysis. A peripheral nerve stimulator can be used to confirm adequate paralysis and optimum intubating conditions prior to laryngoscopy. (See 'Succinylcholine' above.) Remifentanil intubation — Remifentanil, an ultrashort-acting narcotic, is particularly useful for intubation when succinylcholine is contraindicated and when the prolonged duration of action of NMBAs is undesirable. For a high-dose remifentanil intubation, the administration of propofol (2 to 2.5 mg/kg IV) followed by remifentanil (3 to 5 mcg/kg IV) provides good to excellent intubating conditions at 1 to 2.5 minutes after induction [75-77]. We give ephedrine (10 mg IV) along with the propofol for this type of induction to avoid the profound bradycardia and hypotension that may result from these doses of remifentanil and propofol. Propofol 2 mg/kg IV has been shown to provide better intubating conditions than thiopental 6 mg/kg IV or etomidate 0.3 mg/kg IV when given for induction with remifentanil 3 mcg/kg IV without NMBAs [78]. Doses of propofol and remifentanil should be reduced for the elderly and for other patients who are at risk for hypotension with induction. (See "General anesthesia: Intravenous induction agents", section on 'Dosing considerations'.) MASK VENTILATION Ventilation by mask is traditionally not performed prior to intubation during RSII, to avoid inflating the stomach and thereby increasing the chance of regurgitation. Without the application of cricoid pressure, bag-mask ventilation with inflation pressure over 20 cmH2O can result in inflation and, potentially, distention of the stomach [33]. However, a number of studies have shown that cricoid pressure prevents gastric insufflation during mask ventilation in children and adults without airway obstruction and, in adults, with airway pressures up to 60 cmH2O [31-33]. Patients without decreased oxygen reserve or increased oxygen consumption should not desaturate during RSII without mask ventilation. For patients expected to desaturate rapidly with apnea (eg, those with decreased functional residual capacity because of obesity or increased intraabdominal pressure; those with sepsis or fever), gentle, low-pressure mask ventilation with cricoid pressure is not likely to inflate or distend the stomach. Modified RSII — There is no standard definition of "modified RSII," but most commonly it refers to the combination of cricoid pressure and mask ventilation during induction and intubation [79]. The modification of RSII may be either the addition of mask ventilation to an otherwise traditional RSII, or the application of cricoid pressure to a routine induction and intubation. Common scenarios in which modified RSII may be chosen include the following: ● When airway evaluation suggests that intubation may be difficult for a patient who is at high risk of aspiration, gentle mask ventilation may be attempted prior to administration of a neuromuscular blocking agent (NMBA) to prove that ventilation will be possible if intubation is difficult or prolonged. In this situation, one very low-pressure breath may be all that is required. ● Mask ventilation may be performed for patients who are likely to desaturate with apnea, despite preoxygenation. In this situation, several low-pressure breaths (<20 cmH2O) may be required while waiting for paralysis. ● For the patient who may be at unclear but potentially higher risk of regurgitation and aspiration, cricoid pressure may be applied during routine induction. Examples include patients with asymptomatic hiatal hernia, morbid obesity without symptoms of gastroesophageal reflux disease, and patients who have fasted appropriately but who are receiving opioids. CHOICE OF LARYNGOSCOPE As the goal of RSII is to intubate as rapidly as possible, the anesthesia clinician should use the laryngoscope and blade most likely to succeed on the first attempt. In most cases, this will be a standard laryngoscope used for direct laryngoscopy with a Macintosh or miller blade. However, when a difficult airway is expected, a video laryngoscope may be a better choice, assuming the clinician is facile with its use. (See "Airway management for induction of general anesthesia", section on 'Prediction of the difficult airway'.) A number of trials have compared videolaryngoscopy with direct laryngoscopy with regard to first-attempt success at intubation and time to intubation, both particularly important for RSII, with variable results. Though studies consistently find a better glottic view with video laryngoscopes, a meta-analysis of trials comparing one type of video laryngoscope with direct laryngoscopy reported no difference in successful first-attempt intubation or time to intubation [80]. In contrast, in another study, 200 patients with predicted difficult airways based on Mallampati classification grade 3 or 4 (figure 4) were randomly assigned to intubation with a video laryngoscope versus direct laryngoscopy [81]. Videolaryngoscopy resulted in a higher first-attempt intubation rate, decreased time to intubation, and a reduced number of optimizing maneuvers. No matter which laryngoscope is chosen for RSII, a backup plan and the necessary equipment must be immediately available and at the bedside if difficult airway management is expected. All anesthesia clinicians should be familiar with a difficult airway algorithm (algorithm 1). (See "Airway management for induction of general anesthesia", section on 'Preparation for induction of anesthesia'.) For RSII, we place a stylette in the endotracheal tube to add rigidity, to facilitate placement through the vocal cords, and to increase the chance of success on the first attempt at laryngoscopy. It is important to recognize that increasing the rigidity of the endotracheal tube can also potentially increase the risk of injury to the vocal cords or trachea. Once the tip of the tube is placed through the vocal cords, the stylette should be removed to avoid trauma to the anterior trachea and the tube advanced under direct vision. POTENTIAL COMPLICATIONS OF RSII The decision to perform RSII, to modify the induction sequence, or to perform a standard sequence induction must take into account the individualized potential risks of each choice. Potential complications of RSII include difficulty with intubation, hypoxia, hypotension, active regurgitation, and aspiration. Difficult or failed airway — Difficult intubation is always a possibility during induction of anesthesia. If the preoperative airway evaluation suggests potential difficulty with intubation, an awake or, if necessary, inhalation induction may be chosen instead of RSII. Difficult intubation is not always predictable [82]. Thus, equipment, personnel, and a backup plan for airway management must always be ready when RSII is performed. Anesthesia clinicians should be familiar with a difficult airway algorithm (algorithm 1). (See "Approach to the difficult airway in adults outside the operating room".) Hypoxia — The most common risk of RSII is hypoxia, a potential result of oxygen desaturation during the period of apnea prior to intubation. Patients with poor oxygen reserves, such as obese patients, pregnant patients, and patients with pulmonary disease, may be at higher risk for arterial desaturation, despite preoxygenation. Low-pressure mask ventilation during RSII may prevent hypoxia and desaturation for such patients. (See 'Modified RSII' above.) Passive apneic oxygenation using high-flow oxygen through a nasal cannula and continuous positive airway pressure preoxygenation are strategies that may increase the time to apneic oxygen desaturation during RSII. (See 'Preoxygenation' above.) Hypotension — Hypotension is common after RSII, especially for those patients who present for emergency surgery with hemodynamic instability. Dysrhythmias and cardiac arrest can also occur in critically ill patients with poor cardiovascular reserve. The selection of induction agent, rate of administration, and the dose administered should be based on the patient's clinical condition and comorbidities. (See 'Induction agents' above.) Regurgitation — Regurgitation may occur during RSII, despite the maneuvers designed to prevent it. If the patient regurgitates, the head of the operating table should be quickly tipped down to allow material to drain away from the larynx. The head should be turned to the side and the oropharynx suctioned prior to intubation. The trachea should be suctioned prior to administration of a positive pressure breath. If active vomiting occurs, cricoid pressure should be released to avoid esophageal rupture [83]. Aspiration — Regurgitation and aspiration can occur during RSII, even when protocols are followed as suggested. The incidence of aspiration during emergency surgical procedures is approximately 0.15 percent [84]. The sequelae depend on the volume and type of material aspirated and the patient's comorbidities. Aspiration of small amounts of oral secretions may result in minor complications, such as cough or tracheal irritation, while aspiration of large-volume, particulate, or acidic material can result in infection, airway obstruction, acute respiratory distress syndrome, and death. Evaluation and management of aspiration pneumonia is discussed more fully separately. (See "Aspiration pneumonia in adults".) EMERGENCE FROM ANESTHESIA Patients at high risk of aspiration during induction of anesthesia are also at high risk of aspiration during emergence from anesthesia. In most cases, an orogastric tube should be passed during the anesthetic and suctioned and removed immediately prior to emergence. Patients should remain intubated with the endotracheal tube cuff inflated until responding to commands and until airway reflexes return. Patients should be transported to the recovery area with the head of the bed elevated to reduce the chance of reflux. SUMMARY AND RECOMMENDATIONS ● Rapid sequence induction and intubation (RSII) is routinely performed for patients at high risk of aspiration during the induction of general anesthesia. The risk of aspiration should be balanced against the risk of difficult intubation, hypoxia during apnea, and hypotension with RSII. (See 'General indications' above.) ● An essential goal of RSII is the achievement of adequate depth of anesthesia and, most often, paralysis for laryngoscopy, to prevent coughing, straining, and active vomiting with airway manipulation. ● For patients who are at high risk of aspiration, we suggest the administration of antacid medication before induction to increase the pH of gastric contents (Grade 2C). For pregnant patients and for those at high risk of aspiration, we routinely administer clear, nonparticulate antacid prior to induction (eg, sodium citrate-citric acid, 30 mL by mouth). For nonpregnant patients at high risk of aspiration who have not received a proton pump inhibitor or histamine- 2 receptor antagonist (H2RA) on the morning of surgery, we also administer an H2RA 40 to 60 minutes prior to induction (eg, ranitidine 50 mg IV). (See 'Premedication' above.) ● Components of RSII are designed to protect the airway with a cuffed endotracheal tube as quickly as possible after induction of anesthesia, while preventing passive or active regurgitation of stomach contents. They include: • Preoxygenation (see 'Preoxygenation' above) • Application of cricoid pressure (figure 2) (see 'Cricoid pressure during RSII' above) • Administration of an anesthesia induction agent, followed immediately by administration of succinylcholine (see 'Choice of medications' above) • Avoidance of mask ventilation prior to endotracheal intubation (see 'Mask ventilation' above) • Endotracheal intubation with inflation of the endotracheal tube cuff as quickly as possible (see 'Choice of laryngoscope' above) Not all of these components will be appropriate for every patient. ● An assistant who is familiar with correct application of cricoid pressure and with assistance with airway management should be present for RSII. A backup plan for airway management should be determined prior to induction, and the anesthesia clinician should be familiar with a difficult airway management algorithm (algorithm 1). (See 'Cricoid pressure during RSII' above.) ● We suggest the application of cricoid pressure during RSII (Grade 2C). Despite conflicting evidence regarding the effectiveness of cricoid pressure for preventing regurgitation, clinical experience suggests that, in most situations, it is not harmful and may be beneficial. We shift or release pressure if laryngoscopy proves difficult, and release cricoid pressure if active vomiting occurs. We avoid cricoid pressure in patients with acute cervical spinal cord injury. (See 'Cricoid pressure during RSII' above.) ● We typically titrate the anesthesia induction agent to loss of consciousness prior to the administration of a neuromuscular blocking agent (NMBA). We prefer propofol for hemodynamically stable patients. Ketamine and etomidate are alternatives for hemodynamically unstable patients. (See 'Induction agents' above.) ● For most cases, we suggest the use of succinylcholine (1 to 1.5 mg/kg) rather than nondepolarizing NMBAs for RSII (Grade 2C). If a defasciculating dose of a nondepolarizing NMBA is administered in addition, the dose of succinylcholine must be increased to 1.5 to 2 mg/kg IV to overcome the antagonism between nondepolarizing and depolarizing NMBAs. (See 'Succinylcholine' above.) ● If succinylcholine is contraindicated, rocuronium can provide rapid onset of paralysis but results in prolonged duration of action, which may be undesirable. High-dose remifentanil induction is an alternative to RSII with an NMBA. (See 'Alternatives to succinylcholine' above.) ● RSII may be modified to include low-pressure mask ventilation to prove the ability to ventilate prior to paralysis or to prevent hypoxia for patients with reduced oxygen reserve. (See 'Modified RSII' above.) ● Patients at high risk of aspiration during induction of anesthesia are also at high risk of aspiration during emergence from anesthesia. Prior to emergence, the stomach should be emptied using an orogastric or nasogastric tube. (See 'Emergence from anesthesia' above.) REFERENCES 1. Nishina K, Mikawa K, Takao Y, et al. A comparison of rabeprazole, lansoprazole, and ranitidine for improving preoperative gastric fluid property in adults undergoing elective surgery. Anesth Analg 2000; 90:717. 2. Escolano F, Castaño J, López R, et al. Effects of omeprazole, ranitidine, famotidine and placebo on gastric secretion in patients undergoing elective surgery. Br J Anaesth 1992; 69:404. 3. Stollings JL, Diedrich DA, Oyen LJ, Brown DR. Rapid-sequence intubation: a review of the process and considerations when choosing medications. Ann Pharmacother 2014; 48:62. 4. Mort TC. Complications of emergency tracheal intubation: hemodynamic alterations--part I. J Intensive Care Med 2007; 22:157. 5. Mort TC. The incidence and risk factors for cardiac arrest during emergency tracheal intubation: a justification for incorporating the ASA Guidelines in the remote location. J Clin Anesth 2004; 16:508. 6. Mort TC. Emergency tracheal intubation: complications associated with repeated laryngoscopic attempts. Anesth Analg 2004; 99:607. 7. Viegas OJ, Ravindran RS, Shumacker CA. Gastric fluid pH in patients receiving sodium citrate. Anesth Analg 1981; 60:521. 8. Manchikanti L, Marrero TC, Roush JR. Preanesthetic cimetidine and metoclopramide for acid aspiration prophylaxis in elective surgery. Anesthesiology 1984; 61:48. 9. Tanoubi I, Drolet P, Donati F. Optimizing preoxygenation in adults. Can J Anaesth 2009; 56:449. 10. Weingart SD, Levitan RM. Preoxygenation and prevention of desaturation during emergency airway management. Ann Emerg Med 2012; 59:165. 11. Ramachandran SK, Cosnowski A, Shanks A, Turner CR. Apneic oxygenation during prolonged laryngoscopy in obese patients: a randomized, controlled trial of nasal oxygen administration. J Clin Anesth 2010; 22:164. 12. Taha SK, Siddik-Sayyid SM, El-Khatib MF, et al. Nasopharyngeal oxygen insufflation following pre-oxygenation using the four deep breath technique. Anaesthesia 2006; 61:427. 13. Patel A, Nouraei SA. Transnasal Humidified Rapid-Insufflation Ventilatory Exchange (THRIVE): a physiological method of increasing apnoea time in patients with difficult airways. Anaesthesia 2015; 70:323. 14. Mir F, Patel A, Iqbal R, et al. A randomised controlled trial comparing transnasal humidified rapid insufflation ventilatory exchange (THRIVE) preoxygenation with facemask pre-oxygenation in patients undergoing rapid sequence induction of anaesthesia. Anaesthesia 2017; 72:439. 15. Gander S, Frascarolo P, Suter M, et al. Positive end-expiratory pressure during induction of general anesthesia increases duration of nonhypoxic apnea in morbidly obese patients. Anesth Analg 2005; 100:580. 16. Delay JM, Sebbane M, Jung B, et al. The effectiveness of noninvasive positive pressure ventilation to enhance preoxygenation in morbidly obese patients: a randomized controlled study. Anesth Analg 2008; 107:1707. 17. Futier E, Constantin JM, Pelosi P, et al. Noninvasive ventilation and alveolar recruitment maneuver improve respiratory function during and after intubation of morbidly obese patients: a randomized controlled study. Anesthesiology 2011; 114:1354. 18. Frerk C, Mitchell VS, McNarry AF, et al. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth 2015; 115:827. 19. SELLICK BA. Cricoid pressure to control regurgitation of stomach contents during induction of anaesthesia. Lancet 1961; 2:404. 20. Vanner RG, O'Dwyer JP, Pryle BJ, Reynolds F. Upper oesophageal sphincter pressure and the effect of cricoid pressure. Anaesthesia 1992; 47:95. 21. Vanner RG, Pryle BJ. Regurgitation and oesophageal rupture with cricoid pressure: a cadaver study. Anaesthesia 1992; 47:732. 22. Wraight WJ, Chamney AR, Howells TH. The determination of an effective cricoid pressure. Anaesthesia 1983; 38:461. 23. Link MS, Berkow LC, Kudenchuk PJ, et al. Part 7: Adult Advanced Cardiovascular Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015; 132:S444. 24. Algie CM, Mahar RK, Tan HB, et al. Effectiveness and risks of cricoid pressure during rapid sequence induction for endotracheal intubation. Cochrane Database Syst Rev 2015; :CD011656. 25. Mills P, Poole T, Curran J. Cricoid pressure and the pressor response to tracheal intubation. Anaesthesia 1988; 43:788. 26. Birenbaum A, Hajage D, Roche S, et al. Effect of Cricoid Pressure Compared With a Sham Procedure in the Rapid Sequence Induction of Anesthesia: The IRIS Randomized Clinical Trial. JAMA Surg 2019; 154:9. 27. Ellis DY, Harris T, Zideman D. Cricoid pressure in emergency department rapid sequence tracheal intubations: a risk-benefit analysis. Ann Emerg Med 2007; 50:653. 28. Salem MR, Joseph NJ, Heyman HJ, et al. Cricoid compression is effective in obliterating the esophageal lumen in the presence of a nasogastric tube. Anesthesiology 1985; 63:443. 29. Fanning GL. The efficacy of cricoid pressure in preventing regurgitation of gastric contents. Anesthesiology 1970; 32:553. 30. Salem MR, Wong AY, Fizzotti GF. Efficacy of cricoid pressure in preventing aspiration of gastric contents in paediatric patients. Br J Anaesth 1972; 44:401. 31. Salem MR, Wong AY, Mani M, Sellick BA. Efficacy of cricoid pressure in preventing gastric inflation during bag-mask ventilation in pediatric patients. Anesthesiology 1974; 40:96. 32. Moynihan RJ, Brock-Utne JG, Archer JH, et al. The effect of cricoid pressure on preventing gastric insufflation in infants and children. Anesthesiology 1993; 78:652. 33. Lawes EG, Campbell I, Mercer D. Inflation pressure, gastric insufflation and rapid sequence induction. Br J Anaesth 1987; 59:315. 34. Zeidan AM, Salem MR, Mazoit JX, et al. The effectiveness of cricoid pressure for occluding the esophageal entrance in anesthetized and paralyzed patients: an experimental and observational glidescope study. Anesth Analg 2014; 118:580. 35. Neelakanta G. Cricoid pressure is effective in preventing esophageal regurgitation. Anesthesiology 2003; 99:242. 36. Smith KJ, Ladak S, Choi PT, Dobranowski J. The cricoid cartilage and the esophagus are not aligned in close to half of adult patients. Can J Anaesth 2002; 49:503. 37. Smith KJ, Dobranowski J, Yip G, et al. Cricoid pressure displaces the esophagus: an observational study using magnetic resonance imaging. Anesthesiology 2003; 99:60. 38. Rice MJ, Mancuso AA, Gibbs C, et al. Cricoid pressure results in compression of the postcricoid hypopharynx: the esophageal position is irrelevant. Anesth Analg 2009; 109:1546. 39. Tournadre JP, Chassard D, Berrada KR, Boulétreau P. Cricoid cartilage pressure decreases lower esophageal sphincter tone. Anesthesiology 1997; 86:7. 40. Skinner HJ, Bedforth NM, Girling KJ, Mahajan RP. Effect of cricoid pressure on gastro-oesophageal reflux in awake subjects. Anaesthesia 1999; 54:798. 41. Harris T, Ellis DY, Foster L, Lockey D. Cricoid pressure and laryngeal manipulation in 402 pre-hospital emergency anaesthetics: essential safety measure or a hindrance to rapid safe intubation? Resuscitation 2010; 81:810. 42. El-Orbany M, Connolly LA. Rapid sequence induction and intubation: current controversy. Anesth Analg 2010; 110:1318. 43. Vanner RG, Clarke P, Moore WJ, Raftery S. The effect of cricoid pressure and neck support on the view at laryngoscopy. Anaesthesia 1997; 52:896. 44. Haslam N, Parker L, Duggan JE. Effect of cricoid pressure on the view at laryngoscopy. Anaesthesia 2005; 60:41. 45. Effect of Cricoid Pressure Compared With a Sham Procedure in the Rapid Sequence INduction of Anesthesia. JAMA Surg 2018. 46. Manning BJ, Winter DC, McGreal G, et al. Nasogastric intubation causes gastroesophageal reflux in patients undergoing elective laparotomy. Surgery 2001; 130:788. 47. Langley MS, Heel RC. Propofol. A review of its pharmacodynamic and pharmacokinetic properties and use as an intravenous anaesthetic. Drugs 1988; 35:334. 48. Scheffer GJ, Ten Voorde BJ, Karemaker JM, et al. Effects of thiopentone, etomidate and propofol on beat-to-beat cardiovascular signals in man. Anaesthesia 1993; 48:849. 49. Schenarts CL, Burton JH, Riker RR. Adrenocortical dysfunction following etomidate induction in emergency department patients. Acad Emerg Med 2001; 8:1. 50. Cherfan AJ, Arabi YM, Al-Dorzi HM, Kenny LP. Advantages and disadvantages of etomidate use for intubation of patients with sepsis. Pharmacotherapy 2012; 32:475. 51. Bruder EA, Ball IM, Ridi S, et al. Single induction dose of etomidate versus other induction agents for endotracheal intubation in critically ill patients. Cochrane Database Syst Rev 2015; 1:CD010225. 52. Pagel PS, Kampine JP, Schmeling WT, Warltier DC. Ketamine depresses myocardial contractility as evaluated by the preload recruitable stroke work relationship in chronically instrumented dogs with autonomic nervous system blockade. Anesthesiology 1992; 76:564. 53. Tweed WA, Minuck M, Mymin D. Circulatory responses to ketamine anesthesia. Anesthesiology 1972; 37:613. 54. Russo H, Bressolle F. Pharmacodynamics and pharmacokinetics of thiopental. Clin Pharmacokinet 1998; 35:95. 55. Eames WO, Rooke GA, Wu RS, Bishop MJ. Comparison of the effects of etomidate, propofol, and thiopental on respiratory resistance after tracheal intubation. Anesthesiology 1996; 84:1307. 56. Aouad MT, Sayyid SS, Zalaket MI, Baraka AS. Intravenous lidocaine as adjuvant to sevoflurane anesthesia for endotracheal intubation in children. Anesth Analg 2003; 96:1325. 57. Davidson JA, Gillespie JA. Tracheal intubation after induction of anaesthesia with propofol, alfentanil and i.v. lignocaine. Br J Anaesth 1993; 70:163. 58. Jakobsen CJ, Ahlburg P, Holdgård HO, et al. Comparison of intravenous and topical lidocaine as a suppressant of coughing after bronchoscopy during general anesthesia. Acta Anaesthesiol Scand 1991; 35:238. 59. Yukioka H, Hayashi M, Terai T, Fujimori M. Intravenous lidocaine as a suppressant of coughing during tracheal intubation in elderly patients. Anesth Analg 1993; 77:309. 60. Grover VK, Reddy GM, Kak VK, Singh S. Intracranial pressure changes with different doses of lignocaine under general anaesthesia. Neurol India 1999; 47:118. 61. Perry JJ, Lee JS, Sillberg VA, Wells GA. Rocuronium versus succinylcholine for rapid sequence induction intubation. Cochrane Database Syst Rev 2008; :CD002788. 62. Miller RD, Way WL. Inhibition of succinylcholine-induced increased intragastric pressure by nondepolarizing muscle relaxants and lidocaine. Anesthesiology 1971; 34:185. 63. Gill M, Graeme K, Guenterberg K. Masseter spasm after succinylcholine administration. J Emerg Med 2005; 29:167. 64. Schwartz L, Rockoff MA, Koka BV. Masseter spasm with anesthesia: incidence and implications. Anesthesiology 1984; 61:772. 65. Schreiber JU, Lysakowski C, Fuchs-Buder T, Tramèr MR. Prevention of succinylcholine-induced fasciculation and myalgia: a meta-analysis of randomized trials. Anesthesiology 2005; 103:877. 66. Szalados JE, Donati F, Bevan DR. Effect of d-tubocurarine pretreatment on succinylcholine twitch augmentation and neuromuscular blockade. Anesth Analg 1990; 71:55. 67. Tran, D, Newton, et al. Rocuronium vs. succinylcholine for rapid sequence intubation: a Cochrane systematic review. Anaesthesia 2017; 72:765. 68. Magorian T, Flannery KB, Miller RD. Comparison of rocuronium, succinylcholine, and vecuronium for rapid-sequence induction of anesthesia in adult patients. Anesthesiology 1993; 79:913. 69. Naguib M, Samarkandi AH, El-Din ME, et al. The dose of succinylcholine required for excellent endotracheal intubating conditions. Anesth Analg 2006; 102:151. 70. Pühringer FK, Rex C, Sielenkämper AW, et al. Reversal of profound, high-dose rocuronium-induced neuromuscular blockade by sugammadex at two different time points: an international, multicenter, randomized, dose-finding, safety assessor-blinded, phase II trial. Anesthesiology 2008; 109:188. 71. Naguib M, Brewer L, LaPierre C, et al. The Myth of Rescue Reversal in "Can't Intubate, Can't Ventilate" Scenarios. Anesth Analg 2016; 123:82. 72. Engbaek J, Howardy-Hansen P, Ording H, Viby-Mogensen J. Precurarization with vecuronium and pancuronium in awake, healthy volunteers: the influence on neuromuscular transmission and pulmonary function. Acta Anaesthesiol Scand 1985; 29:117. 73. Agoston S, Salt P, Newton D, et al. The neuromuscular blocking action of ORG NC 45, a new pancuronium derivative, in anaesthetized patients. A pilot study. Br J Anaesth 1980; 52 Suppl 1:53S. 74. Belmont MR, Lien CA, Quessy S, et al. The clinical neuromuscular pharmacology of 51W89 in patients receiving nitrous oxide/opioid/barbiturate anesthesia. Anesthesiology 1995; 82:1139. 75. Bouvet L, Stoian A, Rimmelé T, et al. Optimal remifentanil dosage for providing excellent intubating conditions when co-administered with a single standard dose of propofol. Anaesthesia 2009; 64:719. 76. Trabold F, Casetta M, Duranteau J, et al. Propofol and remifentanil for intubation without muscle relaxant: the effect of the order of injection. Acta Anaesthesiol Scand 2004; 48:35. 77. Klemola UM, Mennander S, Saarnivaara L. Tracheal intubation without the use of muscle relaxants: remifentanil or alfentanil in combination with propofol. Acta Anaesthesiol Scand 2000; 44:465. 78. Erhan E, Ugur G, Gunusen I, et al. Propofol - not thiopental or etomidate - with remifentanil provides adequate intubating conditions in the absence of neuromuscular blockade. Can J Anaesth 2003; 50:108. 79. Ehrenfeld JM, Cassedy EA, Forbes VE, et al. Modified rapid sequence induction and intubation: a survey of United States current practice. Anesth Analg 2012; 115:95. 80. Griesdale DE, Liu D, McKinney J, Choi PT. Glidescope® video-laryngoscopy versus direct laryngoscopy for endotracheal intubation: a systematic review and meta-analysis. Can J Anaesth 2012; 59:41. 81. Jungbauer A, Schumann M, Brunkhorst V, et al. Expected difficult tracheal intubation: a prospective comparison of direct laryngoscopy and video laryngoscopy in 200 patients. Br J Anaesth 2009; 102:546. 82. Cook TM, MacDougall-Davis SR. Complications and failure of airway management. Br J Anaesth 2012; 109 Suppl 1:i68. 83. Ralph SJ, Wareham CA. Rupture of the oesophagus during cricoid pressure. Anaesthesia 1991; 46:40. 84. Neilipovitz DT, Crosby ET. No evidence for decreased incidence of aspiration after rapid sequence induction. Can J Anaesth 2007; 54:748. Topic 94214 Version 20.0 © 2019 UpToDate, Inc. All rights reserved.