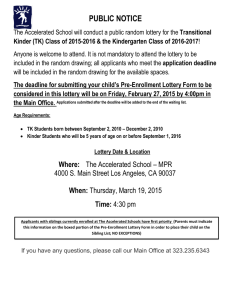
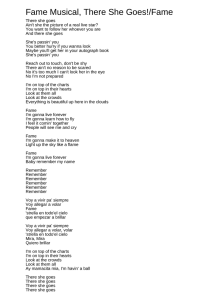
1621 C OPYRIGHT Ó 2014 BY T HE J OURNAL OF B ONE AND J OINT S URGERY, I NCORPORATED Accelerated Rehabilitation Compared with a Standard Protocol After Distal Radial Fractures Treated with Volar Open Reduction and Internal Fixation A Prospective, Randomized, Controlled Study Jess L. Brehmer, MD, and Jeffrey B. Husband, MD Investigation performed at the TRIA Orthopaedic Center, University of Minnesota, Bloomington, Minnesota Background: There are relatively few studies in the literature that specifically evaluate accelerated rehabilitation protocols for distal radial fractures treated with open reduction and internal fixation (ORIF). The purpose of this study was to compare the early postoperative outcomes (at zero to twelve weeks postoperatively) of patients enrolled in an accelerated rehabilitation protocol with those of patients enrolled in a standard rehabilitation protocol following ORIF for a distal radial fracture. We hypothesized that patients with accelerated rehabilitation after volar ORIF for a distal radial fracture would have an earlier return to function compared with patients who followed a standard protocol. Methods: From November 2007 to November 2010, eighty-one patients with an unstable distal radial fracture were prospectively randomized to follow either an accelerated or a standard rehabilitation protocol after undergoing ORIF with a volar plate for a distal radial fracture. Both groups began with gentle active range of motion at three to five days postoperatively. At two weeks, the accelerated group initiated wrist/forearm passive range of motion and strengthening exercises, whereas the standard group initiated passive range of motion and strengthening at six weeks postoperatively. Patients were assessed at three to five days, two weeks, three weeks, four weeks, six weeks, eight weeks, twelve weeks, and six months postoperatively. Outcomes included Disabilities of the Arm, Shoulder and Hand (DASH) scores (primary outcome) and measurements of wrist flexion/extension, supination, pronation, grip strength, and palmar pinch. Results: The patients in the accelerated group had better mobility, strength, and DASH scores at the early postoperative time points (zero to eight weeks postoperatively) compared with the patients in the standard rehabilitation group. The difference between the groups was both clinically relevant and statistically significant. Conclusions: Patients who follow an accelerated rehabilitation protocol that emphasizes motion immediately postoperatively and initiates strengthening at two weeks after volar ORIF of a distal radial fracture have an earlier return to function than patients who follow a more standard rehabilitation protocol. Level of Evidence: Therapeutic Level I. See Instructions for Authors for a complete description of levels of evidence. Peer Review: This article was reviewed by the Editor-in-Chief and one Deputy Editor, and it underwent blinded review by two or more outside experts. It was also reviewed by an expert in methodology and statistics. The Deputy Editor reviewed each revision of the article, and it underwent a final review by the Editor-in-Chief prior to publication. Final corrections and clarifications occurred during one or more exchanges between the author(s) and copyeditors. D istal radial fractures are common. Open reduction and internal fixation (ORIF) with a volar fixed-angle plate is commonly used for the management of distal radial fractures to allow early mobilization and strengthening1-12. With many rehabilitation protocols for distal radial fractures treated with volar ORIF, the wrist is immobilized for several weeks postoperatively, and wrist strengthening exercises are initiated at approximately six to eight weeks Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. None of the authors, or their institution(s), have had any financial relationship, in the thirty-six months prior to submission of this work, with any entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. In addition, no author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article. J Bone Joint Surg Am. 2014;96:1621-30 d http://dx.doi.org/10.2106/JBJS.M.00860 1622 TH E JO U R NA L O F B O N E & JO I N T SU RG E RY J B J S . O RG V O LU M E 96 -A N U M B E R 19 O C T O B E R 1, 2 014 d d d postoperatively1-31. Few studies have dealt specifically with early rehabilitation following distal radial fractures. We found only one article, by Lozano-Calderón et al.25, that compared an early-motion cohort with a late-motion cohort; one group started range-of-motion exercises within two weeks postoperatively and the other, at six weeks postoperatively. LozanoCalderón et al. found no difference between the groups at three or six months postoperatively and ultimately concluded that wrist immobilization for six weeks does not lead to decreased wrist motion or strength over the long term25. In the current study, the postoperative time points at which we implemented the accelerated rehabilitation protocol and assessed the return of patient function were earlier than those in the study by Lozano-Calderón et al. When designing a rehabilitation protocol, one must consider the forces during rehabilitation exercises as well as the ultimate strength of the implants used32-34. Putnam et al.22 reported that males have an average grip force of 104 lb (464 N) and that 2.24 lb (10 N) of grip force translates into 5.8 lb (26 N) of force in the distal radial metaphysis. During power grip, the distal radial metaphysis experiences 541.8 lb (2410 N). Putnam et al. recommended that grip forces in early rehabilitation be <37.5 lb (<169 N). In the present study, we used the Hand Innovations DVR plate (Biomet, Warsaw, Indiana) which has been reported to have an ultimate strength of 23 to 230 lb (102 to 1023 N)32-34. Thus, limiting early rehabilitation grip forces to 37.5 lb (169 N) is within the strength parameters for this implant33. In the current study, we implemented an accelerated rehabilitation protocol and compared patient function in the initial three postoperative months between patients who followed this protocol with that of patients who followed a more traditional rehabilitation protocol. In the accelerated rehabilitation protocol, motion is started three to five days postoperatively, and strengthening exercises are initiated at two weeks postoperatively with the goal of attaining earlier functional recovery. Our objective was to prospectively compare early clinical outcomes—i.e., motion, strength, and return to function—between traditional and accelerated rehabilitation protocols. Materials and Methods T his prospective, randomized study was approved by our institutional review board. From November 2006 to November 2010, eighty-one patients who met our inclusion criteria were prospectively enrolled. Patient sample size for each group was based on estimates derived with use of the Disabilities of the Arm, Shoulder and Hand (DASH) score as the primary outcome measure. We planned the study of a continuous response variable in independent control and 35-37 experimental groups. In previous studies , the response within each subject group was normally distributed with a standard deviation of 14.68. Using 10.1 as the minimal clinically important difference in the DASH score, we determined that we would need to enroll between seventy and eighty patients in total (thirty-five or forty patients per group) to achieve 80% power, with alpha of 37 0.05 . Inclusion criteria were (1) a patient age of eighteen to eighty-five years, (2) an isolated distal radial fracture confirmed by radiographs, and (3) volar ORIF of a distal radial fracture. All fractures were treated with a Hand Innovations DVR plate. Exclusion criteria were (1) a previous distal radial A C C E L E R AT E D R E H A B I L I TAT I O N V S . S TA N D A R D P R O T O C O L A F T E R D I S TA L R A D I A L F R A C T U R E S T R E AT E D W I T H V O L A R ORIF fracture on the affected side; (2) a professional athlete; (3) bilateral distal radial fracture; (4) another concurrent fracture; and (5) a distal radial fracture for which, in the surgeon’s judgment, fixation of fracture fragments could not be achieved to allow participation in the accelerated rehabilitation protocol. There was no standardization of surgical technique. Fixation was obtained for all enrolled patients. Initially a Workers’ Compensation claim was an exclusion criterion for enrollment into the study. However, due to low patient enrollment, this was changed partway through the study to increase patient enrollment. All patients were randomized after consent for study enrollment was obtained. Consent was obtained preoperatively or, when that was not possible (e.g., because the patient was first seen at a nearby hospital or the study coordinator was not available), postoperatively but prior to the initiation of therapy. The surgery as well as postoperative hand therapy visits took place at an ambulatory surgery center in a major metropolitan area (TRIA Orthopaedic Center, Bloomington, Minnesota). Five surgeons contributed patients to this study. Enrollment was performed by a research coordinator who was blinded to fracture severity and, if consent had been obtained postoperatively but before initiation of therapy, to the operative result. All participating surgeons were blinded to each patient’s randomization group as the surgeons’ postoperative care was the same for the two groups. The only difference between the groups was the protocol that was followed for postoperative therapy. Due to the nature of the study, the hand therapists were not blinded. All measurements and assessments were performed postoperatively at scheduled outpatient hand therapy appointments by the unblinded treating therapist, which introduced a potential source of measurement bias. Randomization was performed by computerized random number generation. Patients were prospectively randomized into either the accelerated rehabilitation protocol group or the standard rehabilitation protocol group. We chose not to stratify this study according to fracture type because a group with multiple fracture types more closely resembles the typical scenario that clinicians encounter in their day-to-day practice. See the Appendix for the distribution of fracture types between the two groups. The primary outcome measure in this study was the DASH score, and the secondary outcome measures were range of motion and strength (grip and palmar pinch). From November 2006 to November 2010, 523 distal radial fractures (523 patients) underwent operative treatment at our institution; 411 met the inclusion criteria. Of these 411 patients (411 distal radial fractures), eightyone (eighty-one isolated distal radial fractures) consented to study enrollment. Initially, we planned to randomize 100 patients but, due to difficulty enrolling patients, enrollment was stopped at eighty-one patients, which according to our statistical calculations still provided sufficient statistical power. Most patients who refused to enroll in the study cited fear of being randomized into the standard group as their main reason for not consenting to enrollment. Ultimately, thirty-six patients were randomized into the accelerated rehabilitation protocol group and forty-five patients were randomized into the standard rehabilitation group. Postoperatively, three patients were removed from the study. One of these patients requested to be removed for unknown reasons whereas the other two became ineligible for the study—one because a malreduced fragment was noted on the first postoperative visit, requiring postponement of therapy, and one because of a concomitant occult contralateral distal radial fracture postoperatively. Intention-to-treat analysis was not performed as data were not collected on any of the three patients after they were removed from the study. This left a total of thirty-six patients in the accelerated group and forty-two patients in the standard group (Fig. 1). Patient Demographics Patients in the two groups were similar with respect to age, sex, occupation, and involvement of their dominant hand (see Appendix). Since we did not collect demographic data for eligible patients who refused enrollment, we do not know whether they were similar to those who enrolled. Twenty-one men and fifty-seven women participated in the study. The average age at the time of surgery was 55.3 years for the standard group and 49.8 years for the 1623 TH E JO U R NA L O F B O N E & JO I N T SU RG E RY J B J S . O RG V O LU M E 96 -A N U M B E R 19 O C T O B E R 1, 2 014 d d d A C C E L E R AT E D R E H A B I L I TAT I O N V S . S TA N D A R D P R O T O C O L A F T E R D I S TA L R A D I A L F R A C T U R E S T R E AT E D W I T H V O L A R ORIF Fig. 1 Patient enrollment diagram. *For the number and percentage of patients seen at each follow-up visit, see Table E-3 in the Appendix. accelerated group. The dominant upper extremity was affected in twenty-one patients in the standard group and fifteen patients in the accelerated group. Occupations were similar between the two groups. Five patients in the standard group and four patients in the accelerated group had jobs involving manual labor (carpenter, construction, automotive repair, press operator, bicycle repair, stock room, personal trainer). There were two active smokers in the standard group and six in the accelerated group. There were ten former smokers in the standard group and fourteen in the accelerated group. No other comorbid medical conditions were assessed. The average time from injury to surgical fixation was 4.9 days for the patients in the standard group and 5.4 days for the patients in the accelerated group. The distribution of fracture types, which is shown in the Appendix, did not differ significantly between the two groups. Interventions and Outcomes Following surgery, patients were treated with the rehabilitation protocol to which they had been randomized (Table I). The standard rehabil1-31 itation protocol was designed based on the literature as well as the 1624 TH E JO U R NA L O F B O N E & JO I N T SU RG E RY J B J S . O RG V O LU M E 96 -A N U M B E R 19 O C T O B E R 1, 2 014 A C C E L E R AT E D R E H A B I L I TAT I O N V S . S TA N D A R D P R O T O C O L A F T E R D I S TA L R A D I A L F R A C T U R E S T R E AT E D W I T H V O L A R ORIF d d d TABLE I Accelerated and Standard Rehabilitation Protocols Postop. Time Point Accelerated Protocol 3-5 days d d Finger, elbow, shoulder active range of motion Wrist, forearm active range of motion Finger, elbow, shoulder active range of motion d Wrist, forearm active range of motion d Finger passive range of motion d d Edema control d d d Custom splint (30° wrist extension), removed for hygiene, dressing, eating, exercises Light putty strengthening 3 wk d Weaned from splint 4 wk d Isotonic strengthening d Medium putty strengthening d Discontinuation of splint use d Heavy putty strengthening d d 7 wk 8 wk 12 wk 6 mo Finger passive range of motion Edema control Custom splint (30° wrist extension), removed for hygiene, dressing, eating, exercises Wrist, forearm passive range of motion Isometrics d 6 wk d d d 2 wk Standard Protocol Wrist, forearm passive range of motion Light putty strengthening d Weaned from splint d Isometrics d Discontinuation of splint use d Medium putty strengthening d Isotonic strengthening d Heavy putty strengthening d Study visit for measurements d Study visit for measurements d Study visit for measurements d Study visit for measurements rehabilitation protocol already in place at our institution prior to this study. Both groups began with active range of motion (no active-assisted) of the shoulder, elbow, forearm, wrist, and digits at three to five days postoperatively. The groups began to diverge in their treatment at two weeks postoperatively, when the accelerated group started wrist/forearm passive range of motion and light strengthening with wrist isometrics and gripping with putty. At four weeks postoperatively, this group discontinued using the splint, and isotonic exercises were added. The standard group wore the splint until six weeks postoperatively, at which point passive range of motion and strengthening were initiated. The same splint—a custom volar splint in 30° extension—was used for both groups. Scar management began when sutures were removed in both groups. Patients were assessed at three to five days, two weeks, three weeks, four weeks, six weeks, eight weeks, twelve weeks, and six months postoperatively. At each visit, assessments consisted of the DASH score (primary outcome) as well as assessments at physical examination of wrist flexion and extension, wrist supination/pronation, grip strength, and palmar pinch strength (secondary outcomes). Postoperative radiographs were routinely obtained at two weeks, six weeks, and three months. A table in the Appendix TABLE II Postoperative DASH Scores DASH Score Standard group Preop. 3-5 Days 2 Wk 3 Wk 4 Wk 6 Wk 8 Wk 12 Wk 6 Mo 66 60 48 39 31 23 15 8 5 Accelerated group 65 55 39 30 21 13 5 3 P value 0.8 0.3 0.01* 0.02* 0.004* 0* 0.001* 0.04* 0.19 29.90 to 11.60 24.44 to 14.22 1.91 to 16.47 1.34 to 16.71 3.34 to 16.98 4.85 to 16.08 3.23 to 12.13 0.12 to 6.65 21.06 to 5.10 95% confidence interval *A significant difference between groups. 7 1625 TH E JO U R NA L O F B O N E & JO I N T SU RG E RY J B J S . O RG V O LU M E 96 -A N U M B E R 19 O C T O B E R 1, 2 014 d d d A C C E L E R AT E D R E H A B I L I TAT I O N V S . S TA N D A R D P R O T O C O L A F T E R D I S TA L R A D I A L F R A C T U R E S T R E AT E D W I T H V O L A R ORIF Fig. 2 Graph showing DASH scores of both groups at the postoperative time points. An asterisk indicates a significant difference between groups at that time point. Fig. 3 Graphs showing wrist extension, wrist flexion, forearm supination, and forearm pronation of the affected extremity at the postoperative time points. An asterisk indicates a significant difference between groups at that time point. 1626 TH E JO U R NA L O F B O N E & JO I N T SU RG E RY J B J S . O RG V O LU M E 96 -A N U M B E R 19 O C T O B E R 1, 2 014 d d d A C C E L E R AT E D R E H A B I L I TAT I O N V S . S TA N D A R D P R O T O C O L A F T E R D I S TA L R A D I A L F R A C T U R E S T R E AT E D W I T H V O L A R ORIF ä TABLE III Postoperative Range of Motion and Grip and Pinch Strengths on the Affected Side 2 Wk 3 Wk 4 Wk Wrist flexion (deg) Standard group Accelerated group P value 95% confidence interval 29 36 0.01* 211.86 to 21.99 33 36 45 0* 49 0* 216.94 to 26.92 217.89 to 28.24 Wrist extension (deg) Standard group 42 46 50 Accelerated group 44 51 56 P value 95% confidence interval 0.33 0.05* 0.01* 27.03 to 2.41 29.96 to 20.08 210.56 to 21.90 Forearm supination (deg) Standard group Accelerated group P value 95% confidence interval 51 52 61 56 0.31 63 0.02* 69 0.05* 214.00 to 4.55 220.20 to 22.14 215.99 to 20.09 Forearm pronation (deg) Standard group 73 75 79 Accelerated group 75 77 78 P value 95% confidence interval 0.61 0.55 0.79 26.9 to 4.1 28.2 to 4.4 24.2 to 5.5 Grip strength (lb [N]) Standard group 22 (98) 30 (133) 36 (160) Accelerated group P value 26 (116) 0.23 35 (156) 0.27 39 (173) 0.52 211.37 to 2.81 (250.58 to 12.50) 214.84 to 4.15 (266.01 to 18.46) 212.63 to 6.40 (256.18 to 28.47) 95% confidence interval Palmar pinch strength (lb [N]) Standard group 8 (36) 9 (40) 10 (44) Accelerated group 8 (36) 10 (44) 11 (49) P value 95% confidence interval 0.77 0.59 0.35 21.95 to 1.45 (28.67 to 6.45) 22.45 to 1.41 (210.90 to 6.27) 22.48 to 0.90 (211.03 to 4.00) *A significant difference between groups. lists the numbers of patients assessed at each of the various follow-up time points in this study. Group t test statistical analysis was performed on the data collected to compare outcomes between the two groups at each of the individual time points. We compared the outcomes between the two groups at each time point, as opposed to assessing recovery over time. Significance was set at p < 0.05. The minimally clinically important difference for the DASH score was 10.1 points. Source of Funding This study received limited financial support (from a research grant) from DePuy, Inc. No implants were provided. Results First Eight Weeks Postoperatively atients in the accelerated group consistently had lower DASH scores than patients in the standard group from P the three-to-five-day to eight-week postoperative time points (Table II and Fig. 2). The difference in DASH scores between the groups was statistically significant (p < 0.05) at each time period from two to eight weeks postoperatively, but the significant difference was clinically relevant only at four and six weeks postoperatively. Patients in the accelerated group had a better range of motion (flexion, extension, and supination) at each time interval from two to eight weeks postoperatively, and these differences were significant (p < 0.05) at each time interval from three to eight weeks postoperatively (Table III and Fig. 3). There was no difference in pronation. The only significant difference in strength between the two groups was in grip strength at six weeks (p = 0.02) (Table III and Fig. 4). 1627 TH E JO U R NA L O F B O N E & JO I N T SU RG E RY J B J S . O RG V O LU M E 96 -A N U M B E R 19 O C T O B E R 1, 2 014 d d d A C C E L E R AT E D R E H A B I L I TAT I O N V S . S TA N D A R D P R O T O C O L A F T E R D I S TA L R A D I A L F R A C T U R E S T R E AT E D W I T H V O L A R ORIF TABLE III (continued) 6 Wk 8 Wk 12 Wk 6 Mo 39 50 67 60 56 57 75 65 0.01* 0.01* 0.05* 221.11 to 211.14 211.81 to 21.65 213.80 to 22.23 211.36 to 0.05 52 60 68 69 65 0.002* 72 0.22 70 0.57 213.50 to 26.07 28.85 to 22.00 28.84 to 2.10 24.47 to 2.49 66 74 82 79 75 80 86 84 0* 62 0* 0.01* 0.03* 0.19 0.10 216.52 to 23.14 211.05 to 20.57 210.11 to 2.06 211.40 to 1.09 77 81 81 83 80 83 82 81 0.23 28.2 to 2.0 0.41 26.4 to 2.7 0.77 24.8 to 3.6 0.3 21.9 to 5.9 37 (165) 44 (196) 65 (289) 57 (254) 49 (218) 49 (218) 70 (311) 69 (306) 0.02* 0.21 0.31 0.02* 221.14 to 22.41 (294.04 to 210.72) 213.00 to 2.90 (257.83 to 12.90) 215.61 to 5.01 (269.44 to 22.29) 220.96 to 21.87 (293.23 to 28.32) 11 (49) 12 (53) 13 (58) 13 (58) 16 (71) 17 (76) 15 (67) 16 (71) 0.29 22.67 to 0.80 (211.00 to 3.560) 0.80 22.11 to 1.63 (29.39 to 7.25) Twelve-Week and Six-Month Follow-up The twelve-week and six-month follow-up data showed fewer differences between the two groups. The difference in DASH scores at twelve weeks was statistically significant (p = 0.04) but not clinically relevant (Table II and Fig. 2). The only statistically significant differences in range of motion and strength at twelve weeks and six months postoperatively were better wrist flexion (at twelve weeks [p = 0.01] and six months [p = 0.05]) and grip strength (at six months [p = 0.02]) in the accelerated group (Table III and Figs. 3 and 4). Subject attrition is shown in the Appendix. There was no patient crossover between the two arms of the study. Per our routine, radiographs were obtained at two weeks, six weeks, and three months postoperatively for all patients. No changes in fracture alignment were noted. All fractures healed 0.47 0.38 23.18 to 1.48 (214.15 to 6.58) 23.08 to 1.20 (213.70 to 5.34) by three months. There were no implant failures. One patient in the accelerated group required a reoperation to remove a screw protruding into the distal radioulnar joint seven weeks postoperatively. One patient in the accelerated group sustained a non-traumatic rupture of the ipsilateral extensor pollicis longus tendon one month postoperatively and underwent tendon transfer three months postoperatively. Four patients (two in each group) had posttraumatic carpal tunnel syndrome, which resolved spontaneously in all of them. There were no infections. There were fifteen ipsilateral ulnar styloid fractures in the standard group and thirteen in the accelerated group; all were treated nonoperatively. There was no significant difference between the two groups with regard to the distribution of fracture types; however, this was likely due to a small number of patients in each fracture cohort (see Appendix). 1628 TH E JO U R NA L O F B O N E & JO I N T SU RG E RY J B J S . O RG V O LU M E 96 -A N U M B E R 19 O C T O B E R 1, 2 014 d d d A C C E L E R AT E D R E H A B I L I TAT I O N V S . S TA N D A R D P R O T O C O L A F T E R D I S TA L R A D I A L F R A C T U R E S T R E AT E D W I T H V O L A R ORIF Fig. 4 Graphs showing grip and palmar pinch strengths of the affected hand at the postoperative time points. 1 lb = 4.45 N. An asterisk indicates a significant difference between groups at that time point. Discussion e studied the early postoperative functional outcomes (in the first twelve weeks postoperatively) of patients who had been randomly assigned to undergo either an accelerated postoperative rehabilitation program or a standard rehabilitation protocol following volar fixation of a distal radial fracture. Our standard rehabilitation protocol, which allowed patients to start wrist motion three to five days after surgery but did not allow strengthening until six weeks postoperatively, may be considered by some to be aggressive as many surgeons do not initiate motion until several weeks postoperatively. The accel- W erated rehabilitation protocol allowed patients to start wrist motion three to five days after surgery and initiate strengthening at two weeks postoperatively. In 2008, Lozano-Calderón et al. compared patients who had started wrist motion within two weeks after volar ORIF of a distal radial fracture with those who had started wrist motion at six weeks25. At three and six months postoperatively, they found no significant difference between the two groups with regard to wrist motion, grip strength, radiographic findings, or scores on validated questionnaires, including the DASH. The authors made two interesting statements in their Discussion section: (1) 1629 TH E JO U R NA L O F B O N E & JO I N T SU RG E RY J B J S . O RG V O LU M E 96 -A N U M B E R 19 O C T O B E R 1, 2 014 d d d they mentioned that their results could have been different if wrist mobility had been initiated immediately after surgery and/or if data were collected before twelve weeks after surgery and (2) they called for further study to evaluate if postoperative pain would be a hindrance to progression of postoperative rehabilitation if motion were started immediately postoperatively. The present study addresses each of these points as we assessed the effectiveness of an accelerated rehabilitation protocol in facilitating an earlier return to function by patients treated with volar ORIF for a distal radial fracture. The DASH score was found to differ statistically (p < 0.05) and clinically (>10 points) between the two groups at four and six weeks after surgery. No consistent significant difference in grip or palmar pinch strength was found between the groups. The differences in the postoperative range of motion (except pronation) and DASH scores noted within the first eight weeks after surgery suggest an earlier return to function by patients who followed the accelerated rehabilitation protocol. Beyond twelve weeks there was little difference in postoperative outcomes between the two groups, a finding that is consistent with those of Lozano-Calderón et al. The outcomes in this study suggest that starting wrist motion within three to five days and starting strengthening at two weeks after volar ORIF of distal radial fractures results in an earlier return of clinically relevant function. This study had several weaknesses. Results were not stratified by patient age or fracture type and severity. The distribution of fracture types was not normal (did not lie within a bell-shaped curve), and there was no significant difference between the two groups based on fracture type. Although the surgeons were blinded to patient randomization, the therapists were not. The unblinded treating therapists performed assessments at scheduled therapy visits, introducing the possibility of measurement bias. Patient loss to follow-up was also a weakness, particularly at the later time points for both groups. Additionally, three patients were removed from the study, introducing the possibility of selection bias and decreasing the sample size of the standard therapy group. Compliance with splinting was not assessed; patients assigned to the standard protocol may have discarded their splints early, making their therapy protocol more similar to the accelerated protocol. Also, we did not collect data from patients who were eligible for but did not enroll in the study, possibly causing some sample bias. A C C E L E R AT E D R E H A B I L I TAT I O N V S . S TA N D A R D P R O T O C O L A F T E R D I S TA L R A D I A L F R A C T U R E S T R E AT E D W I T H V O L A R ORIF Because we had difficulty enrolling patients, we allowed those with a Workers’ Compensation claim to enroll partway through the study. However, we did not collect the number of Workers’ Compensation claims as part of the data, thus potentially introducing bias into the findings. The initial study plan was to randomize 100 patients, but we stopped after enrolling eighty-one patients because of difficulty with enrollment. Finally, we did not include secondary outcome data for the unaffected limb, which potentially could have been helpful for comparison or correlation with findings in the study by Lozano-Calderón et al.25. In conclusion, the results of our prospective randomized study suggest that starting range of motion immediately (three to five days) after volar ORIF of distal radial fractures and starting strengthening at two weeks postoperatively will facilitate an earlier return to clinically relevant function and potentially allow for an earlier return to daily, work, and sports activities. Appendix Tables showing the distribution of fracture classifications, patient demographics, and the numbers of patients available for follow-up at each data collection time point are available with the online version of this article as a data supplement at jbjs.org. n NOTE: The authors extend special thanks to Dr. Scott McPherson, Dr. Deb Bohn, Dr. Yvonne Grierson, Dr. Mark Wilczynski, Megan Reams, Julie Agel, Nancy Callinan, each of the TRIA hand therapists, Dr. Robby Sikka, and John Hanks, who all assisted with this study. Jess L. Brehmer, MD Department of Orthopaedic Surgery, University of Minnesota, 2512 South 7th Street, Suite R200, Minneapolis, MN 55454. E-mail address: [email protected] Jeffrey B. Husband, MD TRIA Orthopaedic Center, University of Minnesota, 8100 Northland Drive, Bloomington, MN 55431. E-mail address: [email protected] References 1. Orbay JL. The treatment of unstable distal radius fractures with volar fixation. Hand Surg. 2000 Dec;5(2):103-12. 2. Beharrie AW, Beredjiklian PK, Bozentka DJ. Functional outcomes after open reduction and internal fixation for treatment of displaced distal radius fractures in patients over 60 years of age. J Orthop Trauma. 2004 Nov-Dec; 18(10):680-6. 3. Smith DW, Brou KE, Henry MH. Early active rehabilitation for operatively stabilized distal radius fractures. J Hand Ther. 2004 Jan-Mar;17(1):43-9. 4. Rozental TD, Beredjiklian PK, Bozentka DJ. Functional outcome and complications following two types of dorsal plating for unstable fractures of the distal part of the radius. J Bone Joint Surg Am. 2003 Oct;85(10):1956-60. 5. Herron M, Faraj A, Craigen MAC. Dorsal plating for displaced intra-articular fractures of the distal radius. Injury. 2003 Jul;34(7):497-502. 6. Orbay JL, Fernandez DL. Volar fixation for dorsally displaced fractures of the distal radius: a preliminary report. J Hand Surg Am. 2002 Mar;27(2):205-15. 7. Krukhaug Y, Hove LM. Experience with the AO Pi-plate for displaced intra-articular fractures of the distal radius. Scand J Plast Reconstr Surg Hand Surg. 2004;38(5): 293-6. 8. Kamano M, Honda Y, Kazuki K, Yasudab M. Palmar plating with calcium phosphate bone cement for unstable Colles’ fractures. Clin Orthop Relat Res. 2003 Nov;(416):285-90. 9. Trumble TE, Culp RW, Hanel DP, Geissler WB, Berger RA. Intra-articular fractures of the distal aspect of the radius. Instr Course Lect. 1999;48: 465-80. 10. Smith DW, Henry MH. Volar fixed-angle plating of the distal radius. J Am Acad Orthop Surg. 2005 Jan-Feb;13(1):28-36. 11. Liporace FA, Gupta S, Jeong GK, Stracher M, Kummer F, Egol KA, Koval KJ. A biomechanical comparison of a dorsal 3.5-mm T-plate and a volar fixed-angle plate in a model of dorsally unstable distal radius fractures. J Orthop Trauma. 2005 Mar;19(3):187-91. 1630 TH E JO U R NA L O F B O N E & JO I N T SU RG E RY J B J S . O RG V O LU M E 96 -A N U M B E R 19 O C T O B E R 1, 2 014 d d d 12. Kaempffe FA, Walker KM. External fixation for distal radius fractures: effect of distraction on outcome. Clin Orthop Relat Res. 2000 Nov;(380):220-5. 13. Doi K, Hattori Y, Otsuka K, Abe Y, Yamamoto H. Intra-articular fractures of the distal aspect of the radius: arthroscopically assisted reduction compared with open reduction and internal fixation. J Bone Joint Surg Am. 1999 Aug;81(8): 1093-110. 14. Ring D, Jupiter JB. Percutaneous and limited open fixation of fractures of the distal radius. Clin Orthop Relat Res. 2000 Jun;(375):105-15. 15. Ring D, Prommersberger K, Jupiter JB. Combined dorsal and volar plate fixation of complex fractures of the distal part of the radius. J Bone Joint Surg Am. 2004 Aug;86(8):1646-52. 16. Solanki PV, Mulgaonkar KP, Rao SA. Effect of early mobilisation on grip strength, pinch strength and work of hand muscles in cases of closed diaphyseal fracture radius-ulna treated with dynamic compression plating. J Postgrad Med. 2000 Apr-Jun;46(2):84-7. 17. Jupiter JB, Ring D, Weitzel PP. Surgical treatment of redisplaced fractures of the distal radius in patients older than 60 years. J Hand Surg Am. 2002 Jul;27(4): 714-23. 18. Ruch DS, Ginn TA, Yang CC, Smith BP, Rushing J, Hanel DP. Use of a distraction plate for distal radial fractures with metaphyseal and diaphyseal comminution. J Bone Joint Surg Am. 2005 May;87(5):945-54. 19. Orbay JL, Fernandez DL. Volar fixed-angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg Am. 2004 Jan; 29(1):96-102. 20. Orbay JL, Badia A, Indriago IR, Infante A, Khouri RK, Gonzalez E, Fernandez DL. The extended flexor carpi radialis approach: a new perspective for the distal radius fracture. Tech Hand Up Extrem Surg. 2001 Dec;5(4):204-11. 21. Henry MH, Griggs SM, Levaro F, Clifton J, Masson MV. Volar approach to dorsal displaced fractures of the distal radius. Tech Hand Up Extrem Surg. 2001 Mar; 5(1):31-41. 22. Putnam MD, Meyer NJ, Nelson EW, Gesensway D, Lewis JL. Distal radial metaphyseal forces in an extrinsic grip model: implications for postfracture rehabilitation. J Hand Surg Am. 2000 May;25(3):469-75. 23. Gesensway D, Putnam MD, Mente PL, Lewis JL. Design and biomechanics of a plate for the distal radius. J Hand Surg Am. 1995 Nov;20(6):1021-7. 24. Cassidy C, Jupiter JB, Cohen M, Delli-Santi M, Fennell C, Leinberry C, Husband J, Ladd A, Seitz WR, Constanz B. Norian SRS cement compared with conventional fixation in distal radial fractures. A randomized study. J Bone Joint Surg Am. 2003 Nov;85(11):2127-37. A C C E L E R AT E D R E H A B I L I TAT I O N V S . S TA N D A R D P R O T O C O L A F T E R D I S TA L R A D I A L F R A C T U R E S T R E AT E D W I T H V O L A R ORIF 25. Lozano-Calderón SA, Souer S, Mudgal C, Jupiter JB, Ring D. Wrist mobilization following volar plate fixation of fractures of the distal part of the radius. J Bone Joint Surg Am. 2008 Jun;90(6):1297-304. 26. Slutsky DJ, Herman M. Rehabilitation of distal radius fractures: a biomechanical guide. Hand Clin. 2005 Aug;21(3):455-68. 27. Souer JS, Ring D, Matschke S, Audige L, Maren-Hubert M, Jupiter J. Comparison of functional outcome after volar plate fixation with 2.4-mm titanium versus 3.5-mm stainless-steel plate for extra-articular fracture of distal radius. J Hand Surg Am. 2010 Mar;35(3):398-405. Epub 2010 Feb 7. 28. Jupiter JB, Fernandez DL, Toh CL, Fellman T, Ring D. Operative treatment of volar intra-articular fractures of the distal end of the radius. J Bone Joint Surg Am. 1996 Dec;78(12):1817-28. 29. Trumble TE, Schmitt SR, Vedder NB. Factors affecting functional outcome of displaced intra-articular distal radius fractures. J Hand Surg Am. 1994 Mar;19(2): 325-40. 30. Fernandez DL, Geissler WB. Treatment of displaced articular fractures of the radius. J Hand Surg Am. 1991 May;16(3):375-84. 31. Hurov JR. Fractures of the distal radius: what are the expectations of therapy? A two-year retrospective study. J Hand Ther. 1997 Oct-Dec;10(4):269-76. 32. Sobky K, Baldini T, Thomas K, Bach J, Williams A, Wolf JM. Biomechanical comparison of different volar fracture fixation plates for distal radius fractures. Hand (N Y). 2008 Jun;3(2):96-101. Epub 2007 Sep 7. 33. Dahl WJ, Nassab PF, Burgess KM, Postak PD, Evans PJ, Seitz WH, Greenwald AS, Lawton JN. Biomechanical properties of fixed-angle volar distal radius plates under dynamic loading. J Hand Surg Am. 2012 Jul;37(7):1381-7. Epub 2012 Apr 27. 34. Levin SM, Nelson CO, Botts JD, Teplitz GA, Kwon Y, Serra-Hsu F. Biomechanical evaluation of volar locking plates for distal radius fractures. Hand (N Y). 2008 Mar;3(1):55-60. Epub 2007 Aug 7. 35. Brogren E, Hofer M, Petranek M, Wagner P, Dahlin LB, Atroshi I. Relationship between distal radius fracture malunion and arm-related disability: a prospective population-based cohort study with 1-year follow-up. BMC Musculoskelet Disord. 2011;12:9. Epub 2011 Jan 13. 36. Hunsaker FG, Cioffi DA, Amadio PC, Wright JG, Caughlin B. The American academy of orthopaedic surgeons outcomes instruments: normative values from the general population. J Bone Joint Surg Am. 2002 Feb;84(2):208-15. 37. Gummesson C, Atroshi I, Ekdahl C. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet Disord. 2003 Jun 16; 4:11. Epub 2003 Jun 16.