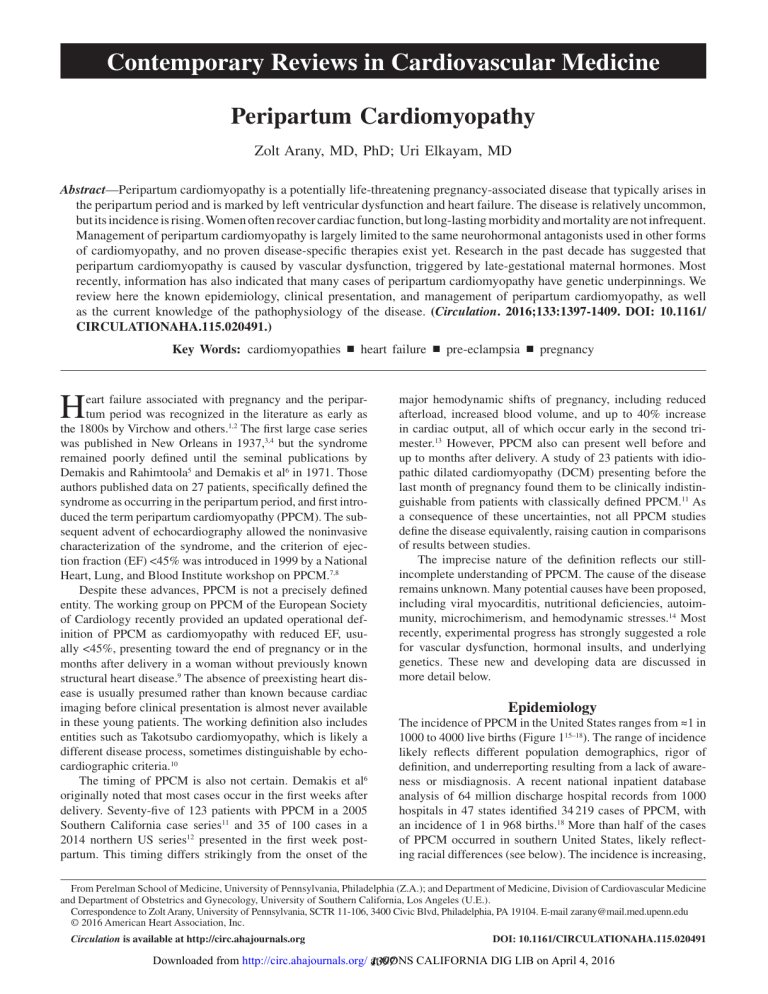
Contemporary Reviews in Cardiovascular Medicine Peripartum Cardiomyopathy Zolt Arany, MD, PhD; Uri Elkayam, MD Abstract—Peripartum cardiomyopathy is a potentially life-threatening pregnancy-associated disease that typically arises in the peripartum period and is marked by left ventricular dysfunction and heart failure. The disease is relatively uncommon, but its incidence is rising. Women often recover cardiac function, but long-lasting morbidity and mortality are not infrequent. Management of peripartum cardiomyopathy is largely limited to the same neurohormonal antagonists used in other forms of cardiomyopathy, and no proven disease-specific therapies exist yet. Research in the past decade has suggested that peripartum cardiomyopathy is caused by vascular dysfunction, triggered by late-gestational maternal hormones. Most recently, information has also indicated that many cases of peripartum cardiomyopathy have genetic underpinnings. We review here the known epidemiology, clinical presentation, and management of peripartum cardiomyopathy, as well as the current knowledge of the pathophysiology of the disease. (Circulation. 2016;133:1397-1409. DOI: 10.1161/ CIRCULATIONAHA.115.020491.) Key Words: cardiomyopathies ◼ heart failure ◼ pre-eclampsia ◼ pregnancy H eart failure associated with pregnancy and the peripartum period was recognized in the literature as early as the 1800s by Virchow and others.1,2 The first large case series was published in New Orleans in 1937,3,4 but the syndrome remained poorly defined until the seminal publications by Demakis and Rahimtoola5 and Demakis et al6 in 1971. Those authors published data on 27 patients, specifically defined the syndrome as occurring in the peripartum period, and first introduced the term peripartum cardiomyopathy (PPCM). The subsequent advent of echocardiography allowed the noninvasive characterization of the syndrome, and the criterion of ejection fraction (EF) <45% was introduced in 1999 by a National Heart, Lung, and Blood Institute workshop on PPCM.7,8 Despite these advances, PPCM is not a precisely defined entity. The working group on PPCM of the European Society of Cardiology recently provided an updated operational definition of PPCM as cardiomyopathy with reduced EF, usually <45%, presenting toward the end of pregnancy or in the months after delivery in a woman without previously known structural heart disease.9 The absence of preexisting heart disease is usually presumed rather than known because cardiac imaging before clinical presentation is almost never available in these young patients. The working definition also includes entities such as Takotsubo cardiomyopathy, which is likely a different disease process, sometimes distinguishable by echocardiographic criteria.10 The timing of PPCM is also not certain. Demakis et al6 originally noted that most cases occur in the first weeks after delivery. Seventy-five of 123 patients with PPCM in a 2005 Southern California case series11 and 35 of 100 cases in a 2014 northern US series12 presented in the first week postpartum. This timing differs strikingly from the onset of the major hemodynamic shifts of pregnancy, including reduced afterload, increased blood volume, and up to 40% increase in cardiac output, all of which occur early in the second trimester.13 However, PPCM also can present well before and up to months after delivery. A study of 23 patients with idiopathic dilated cardiomyopathy (DCM) presenting before the last month of pregnancy found them to be clinically indistinguishable from patients with classically defined PPCM.11 As a consequence of these uncertainties, not all PPCM studies define the disease equivalently, raising caution in comparisons of results between studies. The imprecise nature of the definition reflects our stillincomplete understanding of PPCM. The cause of the disease remains unknown. Many potential causes have been proposed, including viral myocarditis, nutritional deficiencies, autoimmunity, microchimerism, and hemodynamic stresses.14 Most recently, experimental progress has strongly suggested a role for vascular dysfunction, hormonal insults, and underlying genetics. These new and developing data are discussed in more detail below. Epidemiology The incidence of PPCM in the United States ranges from ≈1 in 1000 to 4000 live births (Figure 115–18). The range of incidence likely reflects different population demographics, rigor of definition, and underreporting resulting from a lack of awareness or misdiagnosis. A recent national inpatient database analysis of 64 million discharge hospital records from 1000 hospitals in 47 states identified 34 219 cases of PPCM, with an incidence of 1 in 968 births.18 More than half of the cases of PPCM occurred in southern United States, likely reflecting racial differences (see below). The incidence is increasing, From Perelman School of Medicine, University of Pennsylvania, Philadelphia (Z.A.); and Department of Medicine, Division of Cardiovascular Medicine and Department of Obstetrics and Gynecology, University of Southern California, Los Angeles (U.E.). Correspondence to Zolt Arany, University of Pennsylvania, SCTR 11-106, 3400 Civic Blvd, Philadelphia, PA 19104. E-mail [email protected] © 2016 American Heart Association, Inc. Circulation is available at http://circ.ahajournals.org DOI: 10.1161/CIRCULATIONAHA.115.020491 Downloaded from http://circ.ahajournals.org/ at CONS CALIFORNIA DIG LIB on April 4, 2016 1397 1398 Circulation April 5, 2016 Figure 1. Recent multi-institutional estimates of peripartum cardiomyopathy (PPCM) incidence in the United States. Data taken from Mielniczuk et al,15 Brar et al,16 Gunderson et al,17 and Kolte et al.18 for example, in the above study from 8.5 to 11.8 per 10 000 live births between 2004 and 2011 and in a previous study also of national hospital discharges from 2.3 to 4.5 per 10 000 live births between 1990 and 2002.15 The increasing incidence may reflect increased awareness and diagnosis, rising maternal age, changing demographics, or rising multifetal pregnancies. As the apparent incidence of PPCM increases and as treatments of other complications of pregnancy improve, PPCM increasingly contributes to mortality. In a population study of maternal cardiovascular deaths in California between 2002 and 2006, PPCM was the leading cause (23%).19 The incidence of PPCM outside the United States is less well documented. Data in Africa and Asia suggest an incidence of ≈1 in 1000 live births.20–23 There are, however, striking “hot spots” of PPCM, the cause of which remains unclear. In Haiti, the incidence of PPCM may be as much as 1 in 300 live births,24 possibly related to racial background, nutritional deficiencies, or a high prevalence of preeclampsia. In northern Nigeria, the incidence of PPCM has been reported as high as 1 in 100 live births,25 originally ascribed to indigenous customs of hot baths and high salt intake in the peripartum period, although a recent case-control study of 39 PPCM cases does not support this conclusion.26 Associated Conditions Age The incidence of PPCM is strongly associated with age. Even though the disease can strike women of any age, >50% of cases occur in women >30 years of age,15,16,18,27 with an odds ratio of 10 in a comparison of women >40 and <20 years of age.18 Race The incidence of PPCM in the United States is notably higher in blacks. More than 40% of cases in the nationwide studies described above occurred in black women,15,18 and half occurred in the southern United States.18 A population study in California noted an incidence of PPCM in blacks of 1 in 1421, nearly 3 times that in whites (1 in 4075).16 A singlecenter case-control study in Georgia and Tennessee found a 16-fold higher incidence of PPCM in black women compared to white women.28 A case-control study of 52 black and 104 white patients with PPCM in Southern California showed that black patients are typically younger, have a higher prevalence of hypertension, present later, and have a lower rate of recovery of left ventricular (LV) EF.29 In a 2012 statewide population study of cases in North Carolina in 2003, the incidence of PPCM in black women was 4 times that of white women (1:1087 versus 1:4266), and the fatality rate at 5-year follow-up was also 4 times as high (24% versus 6%).30 In summary, PPCM strikes black women more often, and these women fare worse (prognosis is described in more detail below). Preeclampsia and Hypertension Preeclampsia and hypertension strongly predispose to PPCM. A recent meta-analysis of 22 studies covering 979 cases of PPCM showed an overall prevalence of preeclampsia of 22%, >4 times the 3% to 5% population prevalence.31 Any hypertensive disorder (preeclampsia, gestational hypertension, or chronic hypertension) was present in 37% (range, 29%–45%) of cases. No clear geographic or racial differences were detected. A recent study of hospital discharge records in 6 states identified 535 patients with PPCM, of whom 29.3% had preeclampsia and 46.9% had hypertension (odds ratio, 13.6 and 13.4, respectively).32 The prevalence of preeclampsia in many of these studies may be underestimated because preeclampsia is often underreported and misclassified and because the presence of preeclampsia is often used as an exclusion criterion from the diagnosis of PPCM. PPCM is also frequently found in association with eclampsia, with an odds ratio of 12.9 in a California population study of 1888 patients with eclampsia33 and 27.9 in the multistate hospital discharge study of PPCM cases noted above.18 It is important to realize that preeclampsia or pregnancyinduced hypertension can also trigger pulmonary edema in the absence of PPCM. A recent report directly compared 30 cases of PPCM with 53 cases of hypertension-associated heart failure in pregnancy in a single referral center in South Africa and found that hypertension-associated heart failure typically presented before delivery, was associated with cardiac hypertrophy and preserved EF, and had a better prognosis.34 Even in the absence of clinical heart failure, a number of echocardiographic studies have shown that preeclampsia causes diastolic dysfunction, measured by various parameters, including E/E’, myocardial performance index, and myocardial strain.35–37 The diastolic dysfunction is in part independent from blood pressure elevations and can persist up to 1 year after delivery and resolution of preeclampsia. Preeclampsia thus instigates significant cardiac toxicity, which can be clinically silent but can also present as pulmonary edema with preserved EF or as part of PPCM. However, it is equally important to realize that PPCM is not simply a manifestation of severe preeclampsia. More than 90% of women with preeclampsia, even if severe, do not develop PPCM, and conversely, at least 50% of women with PPCM do not have preeclampsia. The 2 diseases are thus different entities with a strong association and overlap. This strong association suggests that PPCM and preeclampsia may share pathophysiological mechanisms, as discussed in more Downloaded from http://circ.ahajournals.org/ at CONS CALIFORNIA DIG LIB on April 4, 2016 Arany and Elkayam Peripartum Cardiomyopathy 1399 detail below. In short, suspicion for PPCM should not be lowered in the presence of preeclampsia. Doing so could delay appropriate treatment. Multiple Gestations PPCM frequently presents in cases of multigestational status. In the meta-analysis noted above, the average rate of twin gestations in cases of PPCM across 16 studies was 9%,31 well above the average estimated prevalence of 3%.38 A number of cases of PPCM with triplet pregnancies have also been reported.39–41 Other associated conditions have been reported but less well substantiated, including substance abuse, anemia, asthma, prolonged tocolysis, diabetes mellitus, obesity, and malnutrition. Presentation and Diagnosis The majority of PPCM cases present postpartum, mostly in the week after delivery, whereas a small subset present during the second and third trimesters (Figure 2).6,11,13,42 Most women present with signs and symptoms of heart failure, including orthopnea and paroxysmal nocturnal dyspnea. These symptoms can be confused with those of normal pregnancy, especially of late gestation, a fact that often leads to missed or delayed diagnosis of PPCM and to underestimation of the incidence of this condition. Physical examination often reveals signs of heart failure, including tachycardia, elevated jugular venous pressure, pulmonary rales, and peripheral edema. Signs of LV dilatation, including third heart sound and displaced apical impulse, are sometimes but not often noted because PPCM can occur even without LV enlargement. ECG typically shows sinus tachycardia with nonspecific changes, and chest radiography usually shows cardiac enlargement and pulmonary venous congestion. Catastrophic presentations can occur, with severe respiratory distress and low-output cardiac failure necessitating pharmacological and mechanical support.43 The differential diagnosis includes pulmonary causes (eg, pneumonia facilitated by the immune tolerance elicited during pregnancy or pulmonary embolism resulting from the hypercoagulable peripartum period), acute pulmonary edema from prolonged tocolysis or preeclampsia, and cardiac causes, including myocardial infarction or Takotsubo cardiomyopathy. Echocardiography is generally sufficient to differentiate from these causes and usually shows LV dilatation of variable degrees, LV systolic dysfunction, right ventricular and biatrial enlargement, mitral and tricuspid regurgitation, and pulmonary hypertension.8,41 Biomarkers No specific diagnostic biomarkers for PPCM are currently available. Levels of brain natriuretic peptide and troponin do not normally rise during or after pregnancy and are typically elevated in PPCM. Recent work (described in more detail below) has suggested that microRNAs, specifically miR146a, may serve as a novel biomarker for PPCM compared with unaffected postpartum women or women with idiopathic DCM.44 More research is needed, however, including testing to determine whether miR-146a levels differentiate PPCM from peripartum myocardial infarction and other acute vascular events. Treatment and Complications There are limited data on treatment approaches to PPCM, and only 2 randomized, controlled trials comprising a total of 44 patients have been reported (discussed further below).45–47 Treatment for PPCM is thus based largely on clinical experience and extrapolation from data with other forms of systolic heart failure. Treatment is focused, as with other forms of systolic failure, on controlling volume status, neutralizing maladaptive neurohormonal responses, and preventing thromboembolic and arrhythmic complications. Diuretic agents, including loop diuretics, and nitrates are the agents of choice for volume control, although caution is required if used before delivery to avoid hypotension and impaired uterine perfusion. Neurohormonal blockade with angiotensin-converting enzyme inhibitor inhibitors or angiotensin receptor blockers can be used postpartum but is contraindicated before delivery, during which time a combination of organic nitrates and hydralazine can be used instead. β-Blockade should be considered and is likely safe during pregnancy. Metoprolol tartrate may be favored in light of a more extensive clinical experience compared with other β-blockers. In addition, Figure 2. Comparison of timing during and after pregnancy of hemodynamic changes, exemplified as cardiac output (CO; in black), elevations in prolactin and soluble Fms-like tyrosine kinase 1 (sFlt1) hormones (red), and incidence of peripartum cardiomyopathy (PPCM; blue bars). Modified from Elkayam42 and Liu and Arany.13 *Prl levels stay elevated in women who nurse. Downloaded from http://circ.ahajournals.org/ at CONS CALIFORNIA DIG LIB on April 4, 2016 1400 Circulation April 5, 2016 β-1–selective agents may be preferable during pregnancy to avoid promoting uterine activity. Digoxin can be safely used during pregnancy, but its role in the treatment of systolic heart failure is currently being debated.48,49 Studies of new experimental therapies have thus far been equivocal or negative. A small 1999 nonrandomized study of 6 patients given intravenous immunoglobulin showed improvement compared with 11 historical control subjects,50 but no further studies have been conducted. (A subsequent placebocontrolled, randomized trial of intravenous immunoglobulin in 62 patients with recent-onset DCM, although none of them with PPCM, did not show improvements with intravenous immunoglobulin treatment.51) Another 2002 South African study reported improved outcomes in 30 patients receiving pentoxifylline compared with 29 historical control subjects,45 but again, no further studies have been conducted. A 2011 randomized, controlled trial of 24 women with PPCM comparing levosimendan, a calcium sensitizer used in acutely decompensated heart failure, with placebo showed no differences in clinical or echocardiographic outcomes.52 Bromocriptine and Cessation of Breastfeeding Recent mechanistic research (discussed below) has implicated the hormone prolactin in the origin of PPCM and suggested that inhibition of pituitary prolactin secretion with cessation of lactation or with bromocriptine, an ergot alkaloid and dopamine D2-receptor agonist, may be beneficial.53 Bromocriptine is approved by the US Food and Drug Administration for the treatment of Parkinson disease, galactorrhea, and certain pituitary tumors. It has been shown to improve cardiovascular outcomes in diabetes mellitus54 and to have favorable neurohormonal and hemodynamic effects in patients with heart failure.55 A small 2010 randomized, open-label, singlecenter trial of bromocriptine in 20 African women with newly diagnosed PPCM showed improvements in LV recovery at 6 months (27% versus 58%; P=0.012) and in combined heart failure end points. In a prospective, observational registry in Germany, the use of bromocriptine was twice as common in women showing echocardiographic improvement (n=82) than in those who did not (n=14; P=0.013).56 However, enthusiasm for these early results has been tempered by the small size of the unblinded, randomized, controlled trial study, the surprisingly frequent adverse outcomes in the control arm of the study, and the potential danger of using bromocriptine in the peripartum period. Bromocriptine was deemed in 1982 to be safe to the fetus,57 but its approval for the suppression of lactation was withdrawn in the United States in 1995 as a result of concerns about adverse maternal vascular events.58 Moreover, potential harm to the newborn by suppression of lactation must be considered, in particular in the developing world where undernutrition and unsafe water supplies account for the majority of childhood mortality, rendering reliance on breast milk critical.59 A retrospective Internet-recruited study in the United States showed that breastfeeding was associated with a better, rather than worse, maternal outcome.60 In summary, the use of bromocriptine and voluntary cessation of lactation remain investigational and of uncertain benefit at this time. We hope that the results of an ongoing prospective, randomized, controlled trial of bromocriptine in 60 patients in Germany61 will provide more information on the efficacy and safety of bromocriptine. Thromboembolism and Anticoagulation PPCM is associated with higher rates of thromboembolism than other forms of cardiomyopathy.42 The peripartum period is a hypercoagulable state,62 likely an evolutionary adaptation to minimize postpartum hemorrhaging (historically the most common cause of maternal death). Cardiac dilation, endothelial injury, and immobility additionally contribute to clotting propensity in PPCM. In the nationwide inpatient database described above, thromboembolism was the most common serious complication at 6.6%.18 Numerous cases of clots in the left and right ventricles have been reported,63–67 and thromboembolic events can sometimes constitute the presenting symptoms of PPCM.67,68 A study of 33 PPCM cases in Senegal reported LV thrombus in 30% of the patients.69 In light of this high risk of thromboembolism, anticoagulation is advisable in PPCM at least during pregnancy and the first 2 months postpartum. Heparin and unfractionated heparin are safe during pregnancy, and the former is preferred near term because of its shorter half-life. Arrhythmias and Antiarrhythmic Therapies Data on the prevalence of ventricular arrhythmias in PPCM are limited. Sudden death is frequently reported as a cause of mortality, suggesting a high prevalence of arrhythmias. For example, in a retrospective review of 182 patients in California, 38% of fatalities were ascribed to sudden death.67 One report of 19 patients in Senegal who underwent 24-hour Holter monitoring revealed nonsustained ventricular tachycardia in 4 patients.70 Ventricular tachycardia can persist, requiring ablation.71 A retrospective case-control analysis in 19 women with PPCM who received a permanent implantable cardioverter-defibrillator (ICD) for primary prevention compared with 60 control women with nonischemic DCM reported a 37% incidence of appropriate ICD therapy over a mean 3-year follow-up in the women with PPCM and a strong trend for higher incidence than in the women with nonischemic DCM.72 A recent single-center study in Germany of 7 women with severely reduced EF (mean, 18%) who received wearable cardioverter/defibrillator life vests documented 4 events of ventricular fibrillation with successful shock therapy in 3 of the women over a mean follow-up of 81 days.73 In contrast, however, a larger retrospective registry study of aftermarket wearable cardioverter/defibrillators in 107 women with PPCM (average EF, 22%) revealed no shocks for ventricular tachycardia or fibrillation over an average follow-up of 4 months.74 Only 20% of the women went on to receive a permanent ICD, largely for persistent ventricular dysfunction. Thus, because of the high rate of recovery in PPCM, early implantation of permanent ICD should be avoided, and there is no clear data-driven basis for recommending early use of a wearable cardioverter/defibrillator. However, it might be reasonable to consider wearable cardioverter/defibrillators in patients with EF <30%, who have been shown to be at high risk of complications, including mortality (see below), as a bridge to recovery or ICD implantation in patients who fail to recover on optimal medical therapy. Downloaded from http://circ.ahajournals.org/ at CONS CALIFORNIA DIG LIB on April 4, 2016 Arany and Elkayam Peripartum Cardiomyopathy 1401 Cardiac Assist Devices inferior and age-adjusted survival is lower, perhaps reflecting younger age and higher allosensitization.83 Patients with PPCM can present with severe depression of LV function and demonstrate a rapid deterioration. Inotropes, intra-aortic balloon pumps, LV and biventricular assist devices, and extracorporeal membrane oxygenation should be considered in these cases and have been used successfully.75–79 Aggressive treatment should generally be sought in light of the frequent recovery of patients with PPCM. When recovery does not occur, cardiac assist devices can serve as a bridge to transplantation. Four women (4%) in the IPAC study died. Recent national inpatient databases reveal in-hospital mortalities of 1.3%,18,32 but they do not include postdischarge information. Longer-term follow-up in 100 patients in 2 Midwestern academic centers showed a mortality of 11% over a mean of 8 years. In a statewide North Carolina study, mortality was 16% at 7 years.30 Obstetric Management Racial and Geographic Differences Cases of PPCM that occur during late gestation, although less common than postpartum, require special consideration. As noted above, certain medications such as angiotensin-converting enzyme inhibitors and excessive volume depletion must be avoided. No published data exist to guide decisions on timing and mode of delivery; in particular, no data exist to indicate that early delivery or elective caesarian delivery can ameliorate PPCM or improve fetal outcomes. Mean birth weight, size, and Apgar scores are lower in neonates born to women with PPCM, likely reflecting earlier gestational age at delivery.17 Stillbirths are more common (odds ratio, 3.8; P<0.0001 in a population study of 535 patients32). Decisions on management and timing and mode of delivery should therefore be made by a team of cardiologists and obstetricians. Early delivery needs to be weighed against the risks to the newborn and should generally be reserved for cases of impending peril to mother or fetus. Prognosis in the United States is notably worse in blacks. In a 2013 retrospective analysis of 52 black and 104 white patients in 2 centers in California and Louisiana, black patients had 34% lower rates of LV recovery (40% versus 61%; P=0.02) and a higher incidence of mortality or cardiac transplantation (P=0.03) despite similar EFs (28%) on presentation.29 In the IPAC study, black patients presented with a lower EF (31% versus 36%; P=0.008), had a lower average EF at the 1-year follow-up (47% versus 56%; P=0003), and had a lower rate of recovery (defined as EF >50%: 59% versus 77%; P=0.03). In a North Carolina statewide registry, 7-year mortality was 24% in black patients compared with 6% in white patients.30 The causes for the differences in outcome are uncertain and could include genetic differences (perhaps linked to the higher incidence of PPCM in this population [see above]) and differences in socioeconomic resources, access to health care, delay in diagnosis, and other environmental variables. Outcome in Hispanic women, on the other hand, does not appear significantly worse than in non-Hispanic whites.32 Fewer data exist on prognosis outside the United States. A prospective PPCM national registry in Germany that began in 2004 has thus far reported 115 patients. At 6 months, 47% of patients had fully recovered, 2% died, and 15% had major events or persistent cardiomyopathy with EF <35%.56 In a single-center study of 45 patients with PPCM in Pakistan, 71% recovered LV function within 6 months, and no deaths were reported, although 9% of women experienced a thromboembolic stroke.84 In a nationwide study of 104 PPCM patients in Japan, 4 women died (4%), and 63% of survivors recovered LVEF (>50%) at 6 months.85 These outcomes are similar to contemporary outcomes in the United States (see above). On the other hand, a recent single-center study of 30 patients in Cape Town, South Africa, reported 5 deaths (17%) in a mean follow-up duration of 3.5 years34 (accounting for the majority of deaths in a larger cohort of 152 patients presenting with cardiovascular disease in pregnancy86). In a larger study of 176 patients in Soweto, South Africa, 13% died and 25% had persistent LVEF <35% at 6 months.87 Only 21% of the survivors had fully recovered LVEF (>55%). The large majority of women in these studies were of African origin, perhaps explaining some of the difference in outcome. Similarly poor outcomes were reported in a 2-center study in Istanbul, Turkey, in which 10 of 42 patients (24%) with PPCM died, and only 30% of the patients had recovered LV function at 6 months.88 In summary, outcomes remain poor Prognosis The prognosis of PPCM in the United States has improved since its description in 1971. The recently completed prospective Investigations of Pregnancy Associated Cardiomyopathy (IPAC) study enrolled 100 women from multiple centers throughout the United States and followed their clinical course for 12 months with careful clinical evaluations, including repeated echocardiography. This study found that 71% of the women recovered LVEF to >50%, whereas only 13% had major events or persistent cardiomyopathy with EF <35%.80 Recovery occurred almost uniformly by 6 months, with little change in EF thereafter, as has been noted by previous studies.11,81 Recovery of LVEF after 6 months can sometimes occur, however, and should not be ruled out. Transplantation Despite the frequent good outcomes in patients with PPCM, a significant fraction of patients eventually require transplantation, often with bridging via mechanically assisted circulatory support. A study of 99 patients with PPCM who received durable mechanically assisted circulatory support between 2006 and 2012 reported that outcomes were generally better than for the 1159 women with nonPPCM cardiomyopathy but 48% went on to receive cardiac transplantation.82 Only 4 patients had the explant removed because of recovery. Five percent of cardiac transplantations in women in the United States are performed for an indication of PPCM.83 Compared with women receiving transplantations for other indications, graft survival is Mortality Downloaded from http://circ.ahajournals.org/ at CONS CALIFORNIA DIG LIB on April 4, 2016 1402 Circulation April 5, 2016 for women of certain ancestries and in certain geographic areas, especially Africa. the presence of preeclampsia with PPCM portends improved outcome thus remains uncertain. Predictors of Recovery Recurrence With Recurrent Pregnancies In addition to racial background and in part independently from it, EF at presentation best predicts rate of recovery. In the IPAC study, only one third of the 27 women with LVEF <30% at presentation recovered EF to >50% at 1 year. None of the women who also had evidence of dilation (LV end-diastolic diameter >6.0 cm) recovered compared with recovery in nearly 90% of the 65 women who presented with LVEF >30% (P=0.003).80 Events (death, LV assist device, or heart transplantation) occurred almost exclusively in women with LVEF <30% at presentation compared with those with LVEF ≥30% (82% versus 99% event-free survival; P=0.004; Figure 3). In a recent study of 187 patients (mostly from California), mean EF was 31% in women who recovered EF to >50% at 6 months versus 23% in women who did not (P<0.0001).89 Similarly, in the German cohort, mean presenting EF was 28% in women who improved versus 17% in those who did not (P<0.0001).56 However, it is important to note that reduced EF is not a specific predictor of failure to recover and thus should not be an indication for premature device implantation or cardiac transplantation.89 Interestingly, LVEF at presentation in the Soweto study did not predict outcome in this large cohort,87 in contrast to US studies. Lower levels of plasma troponin or brain natriuretic peptide have also been associated with improved outcomes.90 However, like LVEF, their predictive accuracy is not sufficient to affect clinical decisions. There is ongoing debate on the question of whether the presence of hypertension or preeclampsia predicts better outcomes. In patients in whom these conditions contribute to the development of PPCM, resolution of preeclampsia or gestational hypertension may, for example, accelerate resolution. Consistent with this notion, in the German cohort, 49% of women who improved had hypertension compared with only 7% of those who did not improve (P=0.009).56 In the Soweto study, blood pressure had an odds ratio of 0.97 per 1 mm Hg for poor recovery (P=0.02).87 In the nationwide Japanese study of 102 women, of whom 41% had hypertension during pregnancy, the presence of hypertension was independently associated with shorter hospital stay and moderately improved EF at the 7-month follow-up (59% versus 51%; P<0.05).85 On the other hand, preeclampsia or hypertension was not associated with improved outcomes in the IPAC study.80 Whether The question of the risks of carrying a second pregnancy often looms large in women who have had PPCM. A recent comprehensive review of the literature on this topic,91 covering 191 recurrent pregnancies, showed that the risk of relapse in patients with persistent LV dysfunction before their recurrent pregnancy is much higher than in those who have normalized LV function: 48% of the former group (n=93) had significant deterioration of LV function and 16% died, whereas 27% of the latter group showed deterioration and no deaths were reported. The risk of worsening PPCM with recurrent pregnancy is thus substantial. The best predictor for relapse and deterioration of cardiac function is prepregnancy LVEF, but normalized LV function does not guarantee an uncomplicated subsequent pregnancy. Demonstration of adequate cardiac reserve on exercise echocardiography in patients with recovered LV function has been suggested to confer additional prognostic value, but this remains uncertain.92 Many women, however, strongly desire subsequent pregnancies. The decision of whether to proceed is therefore difficult and highly individual. No firm recommendations on this subject can be made on the basis of available data. Nevertheless, waiting for normalization of LV function in the absence of medications is prudent, and women should be advised that they have a high risk of recurrence even if their LV function has recovered, which could lead to a severe and at times persistent decline in LV function or life-threatening complications, and that long-term outcomes are currently not known.91 A team-based approach to decision making, including well-informed clinicians and patients, is highly advocated. If the decision to proceed with pregnancy is made, close monitoring of symptoms, LV function, and brain natriuretic peptide is highly recommended during and after pregnancy.91 Figure 3. Events in 97 women with peripartum cardiomyopathy (PPCM) in the Investigations of Pregnancy Associated Cardiomyopathy (IPAC) study. Data from McNamara et al.80 Treatment After Recovery Because of a lack of long-term follow-up data in women with PPCM, it is not clear if and when women with the condition can be considered to have fully recovered. This is an important issue, bearing on the decision of whether to discontinue longterm medications in young and otherwise healthy women. One study of 15 patients with full LVEF recovery who stopped taking angiotensin-converting enzyme inhibitors or β-blockers reported no deterioration of LV function during a 2-year follow-up.81 Limited cardiac magnetic resonance imaging data do not detect persistent myocardial damage in women in PPCM.93 On the other hand, others have reported deterioration of recovered LV function in a limited number of patients.67 Moreover, an early echocardiographic study of women with recovered LV function revealed decreased contractile reserve in response to dobutamine challenge,94 indicating the presence of persistent subclinical dysfunction. In addition, as discussed above, women with recovered LVEF remain at high risk of recurrence with subsequent pregnancies. Together, these data suggest that cellular and molecular recovery may lag significantly behind echocardiographic recovery. A reasonable approach to the discontinuation of medications in women Downloaded from http://circ.ahajournals.org/ at CONS CALIFORNIA DIG LIB on April 4, 2016 Arany and Elkayam Peripartum Cardiomyopathy 1403 with complete recovery of LV function would include waiting until a few months after LV function has recovered, weaning of medications one at a time, and providing close clinical and echocardiographic monitoring during the discontinuation process, followed by annual assessment of LV function. Pathophysiology of PPCM Hemodynamics and Other Proposed Causes PPCM has often been ascribed to a failed hemodynamic stress test during pregnancy. Indeed, pregnancy triggers large hemodynamic shifts that significantly increase cardiac workload (Figure 2).13 Blood volume and red blood cell mass increase, leading to increased preload. Cardiac output increases by 20% to 50%, a consequence of both increased heart rate by ≈15% to 30% and increased stroke volume by 15% to 25%. Total vascular resistance decreases by 30%, although afterload increases again by the end of pregnancy. All of these changes occur between the first and second trimesters, and patients with known preexisting structural cardiac disease typically present with clinical heart failure at this time in pregnancy.95 In striking contrast, PPCM overwhelmingly presents during the peripartum period (Figure 2). Delivery poses an additional hemodynamic stress, but factors that modify that stress, including caesarian delivery, do not appear to modify the risk of developing PPCM. Hemodynamic stresses are thus not likely to be significant etiologic contributors to PPCM. Myocarditis has often been put forward as a cause of PPCM, driven largely by the frequent but variable observation of inflammatory infiltrates on right-sided heart endomyocardial biopsies.14 However, similar infiltrates are often found in endomyocardial biopsies from control groups. For example, in 1 study, 71% of women with PPCM and 73% of matched control subjects harbored evidence of coxsackie or echovirus infection.96 Similarly, a polymerase chain reaction study on endomyocardial biopsy specimens from 26 patients with PPCM revealed a 30.7% prevalence of viral genomes often implicated in myocarditis, including parvovirus B19, but the prevalence was identical (30.3%) in a control group.97,98 The specificity of these findings is thus poor, and the role of myocarditis in PPCM remains uncertain. Right-sided heart biopsies are no longer indicated in the diagnostic workup of PPCM and are rarely done. Similarly, reports of cardiac magnetic resonance imaging in the acute phase of PPCM in a small number of patients have suggested the presence of inflammation in some patients,99,100 although a recent evaluation of 40 patients in the IPAC study showed a pattern suggestive of myocarditis in only 1 patient (unpublished data, Erik B. Schelbert, MD, 2016). The utility of magnetic resonance imaging in the diagnosis of PPCM is thus uncertain at this time. A number of other potential causes for PPCM have also been proposed, with limited supporting data thus far. Microchimerism, with fetus-derived cells that can persist in the immune-suppressed pregnant state and may lodge in the maternal heart, has been proposed as a trigger for autoimmunity after delivery.7 On the other hand, microchimeric fetal cells that traffic the heart have been proposed to help injured myocardium and to be beneficial.101 Various forms of malnutrition have also been proposed, including iron and selenium deficiencies, and may represent special aggravating circumstances unique to geographical areas. For example, a recent case-control study of 39 patients in Nigeria, where the incidence of PPCM is disproportionally high, revealed mean serum selenium levels that were half that in controls (P<0.001),26 although this observation is not seen elsewhere in sub-Saharan Africa.102 In short, until recently, the causes of PPCM have remained unclear. Recent work, however, has significantly advanced our understanding of the disease. The results are beginning to elucidate 2 novel aspects of PPCM: a critical toxic role for late-gestational hormones on the maternal vasculature and an increasing understanding of the genetic underpinnings of PPCM. These recent developments are discussed below The Vasculo-Hormonal Hypothesis Prolactin A landmark 2007 article first introduced the notion that PPCM is a vascular disease triggered by the hormonal changes of late pregnancy. Although the idea was proposed in the past,103 experimental support for it was lacking. The authors developed a mouse model of PPCM in which the STAT3 transcription factor was genetically deleted specifically in cardiomyocytes. In support of generating this model, expression of STAT3 was reduced in the LVs from patients with end-stage heart failure caused by PPCM compared with nonfailing control subjects. Loss of STAT3 in murine hearts leads to reduced expression of genes that protect the heart against reactive oxygen species, most notably manganese superoxide dismutase (MnSOD), which neutralizes superoxides generated by the robust mitochondrial activity in beating cardiomyocytes. The consequent rise in reactive oxygen species leads to the secretion, via a still unclear mechanism, of cathepsin D. This extracellular peptidase then cleaves prolactin, a hormone specific to late pregnancy, into a 16-kDa fragment that promotes apoptosis in endothelial cells. As a result, STAT3 cardiac knockout mice reveal significant vascular dropout during late pregnancy and consequent pregnancy-induced DCM, that is, PPCM (Figure 4). The most compelling aspect of this study, which is proof of the key role played by prolactin, came from blocking prolactin secretion from the pituitary with bromocriptine. Treatment of STAT3 cardiac knockout mice with bromocriptine completely reversed the observed PPCM. The same group recently probed more deeply into how the 16-kDa prolactin fragment triggers endothelial and cardiomyocyte damage.44,104 They showed that 16-kDa prolactin induces endothelial cells to package miR-146a into exosomes, small lipid-encapsulated particles, which are then secreted and taken up by cardiomyocytes. The miR-146a internalized into cardiomyocytes then suppresses the neuregulin/ErbB pathway, thereby promoting cardiomyocyte apoptosis. Strikingly, circulating levels of miR-146a are dramatically elevated in women with PPCM. Moreover, the levels drop significantly with bromocriptine treatment, demonstrating that prolactin drives miR-146a secretion. As outlined above, miR-146a may thus be useful as a biomarker of PPCM. In addition, miR-146a may become a viable therapeutic target because microRNAs can be efficiently and specifically inhibited clinically. Indeed, Downloaded from http://circ.ahajournals.org/ at CONS CALIFORNIA DIG LIB on April 4, 2016 1404 Circulation April 5, 2016 Figure 4. Vasculo-hormonal hypothesis of the pathophysiology of peripartum cardiomyopathy (PPCM). See text for details. treatment of the STAT3 model of PPCM with locked nucleic acid (LNA)–modified antisense oligonucleotides to silence miR-146a partially rescued cardiac capillary density and contractile function. Moreover, LNA–miR-146a did not inhibit lactation because the linolenic acid acts downstream of the 16-kDa prolactin action. Thus, unlike with bromocriptine, therapy with LNA-miR-146a would allow continued nursing of the newborn. These data thus convincingly showed that, at least in this murine model, a peripartum hormone (prolactin) plus a cardiac predisposition (in this case, absence of STAT3 in the heart) conspire to trigger vasculopathy and consequently PPCM. Soluble Fms-Like Tyrosine Kinase 1 A very similar vasculo-hormonal paradigm was recently recapitulated in a different mouse model of PPCM in which there is cardiac-specific deletion of proliferator-activated receptorgamma coactivator-1α (PGC-1α), a powerful transcriptional regulator.105 Like STAT3, PGC-1α drives the expression of MnSOD, thus suppressing reactive oxygen species. In addition, PCG-1α drives the expression of vascular endothelial growth factor (VEGF), the most widely studied angiogenic factor.106 Cardiac deletion of PGC-1α thus promotes vasculotoxicity by 2 pathways: the activation of an antivascular 16-kDa prolactin-mediated pathway (as in the STAT3 model) and the loss of a provascular VEGF-mediated pathway (Figure 4). Accordingly, only the combination of bromocriptine and VEGF therapies rescues PPCM in these animals. The observations above raised the question of what hormone during pregnancy is inhibiting the VEGF pathway and triggering PPCM in the PGC-1 model. During late gestation in placental mammals, the placenta secretes into the maternal circulation numerous hormones, including a soluble variant of the VEGF receptor 1, soluble Fms-like tyrosine kinase 1 (sFlt1). Most free VEGF in the maternal circulation is neutralized by sFlt1 during late gestation.107 The heart and other organs defend themselves from this insult in part by local secretion of VEGF, but this is diminished and insufficient in the PGC-1α model of PPCM. Administering sFlt1 to nulliparous PGC-1α animals was sufficient to cause cardiomyopathy, even in the absence of pregnancy, demonstrating that sFlt1 is a key component of the gravid state that triggers PPCM in these animals. Thus, sFlt1 and prolactin are 2 potentially vasculotoxic hormones of late gestation that can trigger PPCM in sensitized hosts. The placental secretion of sFlt1 is markedly elevated in preeclampsia107 and twin gestations.108 The maternal heart is thus exposed to significantly higher levels of sFlt1 in these conditions, likely explaining the strong epidemiological link between preeclampsia, twin gestations, and PPCM (discussed above). In fact, women with preeclampsia but without PPCM still have demonstrable subclinical cardiac dysfunction on echocardiography,35–37,105 and in a small study (n=20), the extent of dysfunction correlated well with circulating levels of sFlt1.105 Levels of sFlt1 are elevated in a subset of women with PPCM,105 and in the IPAC study, levels of sFlt1 correlated with clinical heart failure and adverse outcome.108a A small, nonrandomized, open pilot study (n=11) of extracorporeal removal of sFlt1 in early preterm preeclampsia showed promising results,109 and a single case study of plasma exchange in a woman with aggressive PPCM showed accelerated recovery of heart function.110 Together, these observations indicate that sFlt1, secreted from the placenta in late gestation, provides a toxic challenge to the heart and that, in the absence of appropriate defenses, PPCM can ensue. Together with the STAT3 model, the findings strongly support the notion that PPCM is a vascular disease, triggered by the hormonal milieu of the peripartum (Figure 4). This notion has a number of attractive explanatory attributes. First, it could explain why PPCM typically presents in the peripartum period, when hormonal changes are greatest, rather than much earlier in pregnancy, when hemodynamic changes are greatest (Figure 2). Second, the role of sFlt1 could explain the well-established epidemiological observations that PPCM is strongly associated with preeclampsia and with multiple gestations, both of which are marked by high Downloaded from http://circ.ahajournals.org/ at CONS CALIFORNIA DIG LIB on April 4, 2016 Arany and Elkayam Peripartum Cardiomyopathy 1405 secretion of sFlt1. Third, the removal of the toxic hormonal milieu after delivery could explain the frequently found rapid recovery of ventricular function in PPCM, not typically seen in other causes of DCM. The hormonal hypothesis also presents clinical diagnostic, prognostic, and therapeutic opportunities. sFlt1, miR-146a, or as-yet-undiscovered hormonal contributors could become useful biomarkers. Inhibition of prolactin (eg, with bromocriptine61) or of miR-146a (eg, with antagomirs), proangiogenic therapy (eg, with VEGF analogs), or removal of toxic hormones (eg, with apheresis109) could prove beneficial (Figure 4). These ideas, however, are still experimental at this stage. Genetics An enduring question in the pathogenesis of PPCM is what rare event predisposes to the disease. One possibility is genetic background. Arguing against this notion, PPCM is typically not a familial disease, and pedigrees of patients with PPCM have not been reported. Moreover, PPCM often does not recur with a second pregnancy, indicating that any genetic origin, if existing, is incompletely penetrant. A recent small echocardiographic study of sisters of women with PPCM (n=17) revealed no obvious cardiac abnormalities.111 However, some evidence has supported the notion that PPCM may have a hereditary or genetic component. A genome-wide association study in 79 patients identified a single-nucleotide polymorphism near the PTHLH gene as being associated with PPCM,112 and interestingly, PTHLH may regulate vascular homeostasis.113 Familial clustering of PPCM has been noted,114–117 and 15% of patients in a German cohort had a family history of cardiomyopathy (loosely defined as PPCM, idiopathic cardiomyopathy [DCM], sudden death, or arrhythmias in first-degree relatives).56 Two groups recently evaluated rare pedigrees of patients affected by both PPCM and DCM and identified variants in genes encoding myofibrillar proteins, including TTN, the gene encoding the sarcomere protein titin.118,119 Whether similar variants would be found in common, sporadic PPCM remains uncertain. Most recently, a genetic study was undertaken with 172 patients with PPCM who were not preselected for family history or other indexes of genetic origin.120 Targeted sequencing of 43 genes known to associate with DCM revealed a striking 15% prevalence in the patients with PPCM of high-impact nonsense, frameshift, and splicing variants (P=1.3×10−7 compared with the control group). Interestingly, the prevalence was similar to that found in a large cohort of DCM cases (17%; P=0.81). Strikingly, two thirds of identified truncating variants were in TTN (prevalence of 10%; P=2.7×10−10 versus 1.4% in reference population). Equally strikingly, 14 of these 17 TTN truncating variants were located in the A band of titin (P=0.0018 versus the reference population; Figure 5).120 Variants in subjects with DCM show a similar predilection for affecting the A band.121,122 These surprising findings indicate that PPCM often has a genetic cause and that PPCM shares a genetic origin with familial and sporadic DCM. Post hoc subgroup analyses also revealed interesting observations: (1) TTN variants were identified in both black and white women; (2) in the subset of women enrolled in the clinically well-characterized IPAC cohort (n=83), the presence of TTN variants correlated with lower EF at the 1-year follow-up (P=0.005); and (3) the burden of truncating TTN variants in subjects without hypertension was nearly 10-fold higher than in subjects with hypertension (23% versus 2.5%; P=0.005). These post hoc findings need further validation before clinical recommendations can be made. These genetic findings raise a number of questions. PPCM and DCM are not clinically identical. For example, patients with DCM recover LV function much less frequently than patients with PPCM, and DCM rarely occurs in young women. It thus remains enigmatic what genetic or environmental variables differentiate women who carry TTN truncating variants and develop PPCM from those women who develop DCM or from those who develop neither. It will also be of interest to elucidate the mechanistic interaction between truncations in TTN and late gestational antivascular insults. Figure 5. Sites within the TTN gene of truncating variants identified in women with peripartum cardiomyopathy (PPCM) and comparison with variants found in patients with dilated cardiomyopathy (DCM) and healthy control subjects. Top, Schematic of a sarcomere spanned by titin. Bottom, Schematic of the TTN open reading frame. Red indicates the Z band; blue, the I band; green, the A band; and purple, the M band. Reprinted with permission from Ware et al.120 Copyright © 2016, Massachusetts Medical Society. Downloaded from http://circ.ahajournals.org/ at CONS CALIFORNIA DIG LIB on April 4, 2016 1406 Circulation April 5, 2016 Conclusions Tremendous progress has been made in the last few years in our understanding of PPCM, both clinically and mechanistically. However, this exciting progress has not yet translated into tangible benefits for patients. No proven disease-specific efficacious therapies exist yet, and specific diagnostic or prognostic tests are lacking. Management of PPCM remains largely limited to the appropriate use of routine neurohormonal antagonists used in other forms of DCM. A number of developments would significantly aid the progress in understanding PPCM. First, in light of the relatively rare nature of PPCM, multicenter collaborations and registries are urgently needed. A worldwide prospective registry that began in 2012 is aiming at 1000 patients and has thus far reported 100 patients, half from Africa and only a handful from the United States.123 Second, further research support is needed. Currently, the National Institutes of Health does not support a single project that studies PPCM.124 Third, organized patient advocacy groups would help both galvanize support and recruit subjects for research; no such group currently exists. Advancement in the understanding of PPCM is at an inflection point. With appropriate coordinated efforts, progress in the next few years will be exponential, and translation to the clinic could become a reality. Disclosures None. References 1. Porak C. De L’influence reciproque de la grossesse et del maladies du Coeur [thesis]. Medical Faculty of Paris, France: 1880. 2. Ritchie C. Clinical contribution to the pathology, diagnosis, and treatment of certain chronic diseases of the heart. Edinburgh Med Surg J. 1849;185:333–342. 3. Hull E, Hafkesbring E. Toxic postpartal heart disease. N Orleans Med Surg J. 1937;89:550. 4. Hull E, Hidden E. Postpartal heart failure. Southern Med J. 1938;31:265. 5. Demakis JG, Rahimtoola SH. Peripartum cardiomyopathy. Circulation. 1971;44:964–968. 6. Demakis JG, Rahimtoola SH, Sutton GC, Meadows WR, Szanto PB, Tobin JR, Gunnar RM. Natural course of peripartum cardiomyopathy. Circulation. 1971;44:1053–1061. 7. Pearson GD, Veille JC, Rahimtoola S, Hsia J, Oakley CM, Hosenpud JD, Ansari A, Baughman KL. Peripartum cardiomyopathy: National Heart, Lung, and Blood Institute and Office of Rare Diseases (National Institutes of Health) workshop recommendations and review. JAMA. 2000;283:1183–1188. 8. Hibbard JU, Lindheimer M, Lang RM. A modified definition for peripartum cardiomyopathy and prognosis based on echocardiography. Obstet Gynecol. 1999;94:311–316. 9. Sliwa K, Hilfiker-Kleiner D, Petrie MC, Mebazaa A, Pieske B, Buchmann E, Regitz-Zagrosek V, Schaufelberger M, Tavazzi L, van Veldhuisen DJ, Watkins H, Shah AJ, Seferovic PM, Elkayam U, Pankuweit S, Papp Z, Mouquet F, McMurray JJ; Heart Failure Association of the European Society of Cardiology Working Group on Peripartum Cardiomyopathy. Current state of knowledge on aetiology, diagnosis, management, and therapy of peripartum cardiomyopathy: a position statement from the Heart Failure Association of the European Society of Cardiology Working Group on Peripartum Cardiomyopathy. Eur J Heart Fail. 2010;12:767– 778. doi: 10.1093/eurjhf/hfq120. 10. Citro R, Giudice R, Mirra M, Petta R, Baldi C, Bossone E, Piscione F. Is Tako-tsubo syndrome in the postpartum period a clinical entity different from peripartum cardiomyopathy? J Cardiovasc Med (Hagerstown). 2013;14:568–575. doi: 10.2459/JCM.0b013e32835f1a49. 11. Elkayam U, Akhter MW, Singh H, Khan S, Bitar F, Hameed A, Shotan A. Pregnancy-associated cardiomyopathy: clinical characteristics and a comparison between early and late presentation. Circulation. 2005;111:2050– 2055. doi: 10.1161/01.CIR.0000162478.36652.7E. 12. Pillarisetti J, Kondur A, Alani A, Reddy M, Reddy M, Vacek J, Weiner CP, Ellerbeck E, Schreiber T, Lakkireddy D. Peripartum cardiomyopathy: predictors of recovery and current state of implantable cardioverter-defibrillator use. J Am Coll Cardiol. 2014;63(pt A):2831–2839. doi: 10.1016/j. jacc.2014.04.014. 13. Liu LX, Arany Z. Maternal cardiac metabolism in pregnancy. Cardiovasc Res. 2014;101:545–553. doi: 10.1093/cvr/cvu009. 14. Ntusi NB, Mayosi BM. Aetiology and risk factors of peripartum cardiomyopathy: a systematic review. Int J Cardiol. 2009;131:168–179. doi: 10.1016/j.ijcard.2008.06.054. 15. Mielniczuk LM, Williams K, Davis DR, Tang AS, Lemery R, Green MS, Gollob MH, Haddad H, Birnie DH. Frequency of peripartum cardiomyopathy. Am J Cardiol. 2006;97:1765–1768. doi: 10.1016/j. amjcard.2006.01.039. 16. Brar SS, Khan SS, Sandhu GK, Jorgensen MB, Parikh N, Hsu JW, Shen AY. Incidence, mortality, and racial differences in peripartum cardiomyopathy. Am J Cardiol. 2007;100:302–304. doi: 10.1016/j. amjcard.2007.02.092. 17. Gunderson EP, Croen LA, Chiang V, Yoshida CK, Walton D, Go AS. Epidemiology of peripartum cardiomyopathy: incidence, predictors, and outcomes. Obstet Gynecol. 2011;118:583–591. doi: 10.1097/ AOG.0b013e318229e6de. 18. Kolte D, Khera S, Aronow WS, Palaniswamy C, Mujib M, Ahn C, Jain D, Gass A, Ahmed A, Panza JA, Fonarow GC. Temporal trends in incidence and outcomes of peripartum cardiomyopathy in the United States: a nationwide population-based study. J Am Heart Assoc. 2014;3:e001056. doi: 10.1161/JAHA.114.001056. 19. Main EK, McCain CL, Morton CH, Holtby S, Lawton ES. Pregnancyrelated mortality in California: causes, characteristics, and improvement opportunities. Obstet Gynecol. 2015;125:938–947. doi: 10.1097/ AOG.0000000000000746. 20. Desai D, Moodley J, Naidoo D. Peripartum cardiomyopathy: experiences at King Edward VIII Hospital, Durban, South Africa and a review of the literature. Trop Doct. 1995;25:118–123. 21. Sliwa K, Damasceno A, Mayosi BM. Epidemiology and etiology of cardiomyopathy in Africa. Circulation. 2005;112:3577–3583. doi: 10.1161/ CIRCULATIONAHA.105.542894. 22. Hasan JA, Qureshi A, Ramejo BB, Kamran A. Peripartum cardiomyopathy characteristics and outcome in a tertiary care hospital. J Pak Med Assoc. 2010;60:377–380. 23. Pandit V, Shetty S, Kumar A, Sagir A. Incidence and outcome of peripartum cardiomyopathy from a tertiary hospital in South India. Trop Doct. 2009;39:168–169. doi: 10.1258/td.2008.080353. 24. Fett JD, Christie LG, Carraway RD, Murphy JG. Five-year prospective study of the incidence and prognosis of peripartum cardiomyopathy at a single institution. Mayo Clin Proc. 2005;80:1602–1606. doi: 10.4065/80.12.1602. 25. Isezuo SA, Abubakar SA. Epidemiologic profile of peripartum cardiomyopathy in a tertiary care hospital. Ethn Dis. 2007;17:228–233. 26. Karaye KM, Yahaya IA, Lindmark K, Henein MY. Serum selenium and ceruloplasmin in Nigerians with peripartum cardiomyopathy. Int J Mol Sci. 2015;16:7644–7654. doi: 10.3390/ijms16047644. 27. Witlin AG, Mabie WC, Sibai BM. Peripartum cardiomyopathy: an ominous diagnosis. Am J Obstet Gynecol. 1997;176(pt 1):182–188. 28. Gentry MB, Dias JK, Luis A, Patel R, Thornton J, Reed GL. AfricanAmerican women have a higher risk for developing peripartum cardiomyopathy. J Am Coll Cardiol. 2010;55:654–659. doi: 10.1016/j. jacc.2009.09.043. 29. Goland S, Modi K, Hatamizadeh P, Elkayam U. Differences in clinical profile of African-American women with peripartum cardiomyopathy in the United States. J Card Fail. 2013;19:214–218. doi: 10.1016/j. cardfail.2013.03.004. 30. Harper MA, Meyer RE, Berg CJ. Peripartum cardiomyopathy: population-based birth prevalence and 7-year mortality. Obstet Gynecol. 2012;120:1013–1019. doi: http://10.1097/AOG.0b013e31826e46a1. 31. Bello N, Rendon IS, Arany Z. The relationship between pre-eclampsia and peripartum cardiomyopathy: a systematic review and meta-analysis. J Am Coll Cardiol. 2013;62:1715–1723. doi: 10.1016/j.jacc.2013.08.717. 32. Kao DP, Hsich E, Lindenfeld J. Characteristics, adverse events, and racial differences among delivering mothers with peripartum cardiomyopathy. JACC Heart Fail. 2013;1:409–416. doi: 10.1016/j.jchf.2013.04.011. 33. Fong A, Chau CT, Pan D, Ogunyemi DA. Clinical morbidities, trends, and demographics of eclampsia: a population-based study. Am J Obstet Gynecol. 2013;209:229.e1–229.e7. doi: 10.1016/j.ajog.2013.05.050. 34. Ntusi NB, Badri M, Gumedze F, Sliwa K, Mayosi BM. Pregnancyassociated heart failure: a comparison of clinical presentation and Downloaded from http://circ.ahajournals.org/ at CONS CALIFORNIA DIG LIB on April 4, 2016 Arany and Elkayam Peripartum Cardiomyopathy 1407 35. 36. 37. 38. 39. 40. 41. 42. 43. 44. 45. 46. 47. 48. 49. 50. 51. 52. 53. outcome between hypertensive heart failure of pregnancy and idiopathic peripartum cardiomyopathy. PLoS One. 2015;10:e0133466. doi: 10.1371/ journal.pone.0133466. Melchiorre K, Sutherland GR, Baltabaeva A, Liberati M, Thilaganathan B. Maternal cardiac dysfunction and remodeling in women with preeclampsia at term. Hypertension. 2011;57:85–93. doi: 10.1161/ HYPERTENSIONAHA.110.162321. Melchiorre K, Sutherland GR, Liberati M, Thilaganathan B. Preeclampsia is associated with persistent postpartum cardiovascular impairment. Hypertension. 2011;58:709–715. doi: 10.1161/ HYPERTENSIONAHA.111.176537. Shahul S, Rhee J, Hacker MR, Gulati G, Mitchell JD, Hess P, Mahmood F, Arany Z, Rana S, Talmor D. Subclinical left ventricular dysfunction in preeclamptic women with preserved left ventricular ejection fraction: a 2D speckle-tracking imaging study. Circ Cardiovasc Imaging. 2012;5:734– 739. doi: 10.1161/CIRCIMAGING.112.973818. Russell RB, Petrini JR, Damus K, Mattison DR, Schwarz RH. The changing epidemiology of multiple births in the United States. Obstet Gynecol. 2003;101:129–135. Altun İ, Akın F, Biteker M. Peripartum cardiomyopathy and triplet pregnancy. Anatol J Cardiol. 2015;15:85–86. doi: 10.5152/akd.2014.5693. Günaydın ZY, Gürel YE, Erdoğan G, Kaya A. Peripartum cardiomyopathy associated with triplet pregnancy. Anadolu Kardiyol Derg. 2014;14:661– 662. doi: 10.5152/akd.2014.5668. Chapa JB, Heiberger HB, Weinert L, Decara J, Lang RM, Hibbard JU. Prognostic value of echocardiography in peripartum cardiomyopathy. Obstet Gynecol. 2005;105:1303–1308. doi: 10.1097/01. AOG.0000161382.30233.ba. Elkayam U. Clinical characteristics of peripartum cardiomyopathy in the United States: diagnosis, prognosis, and management. J Am Coll Cardiol. 2011;58:659–670. doi: 10.1016/j.jacc.2011.03.047. Arany ZP, Walker CM, Wang L. Case records of the Massachusetts General Hospital: case 22-2014: a 40-year-old woman with postpartum dyspnea and hypoxemia. N Engl J Med. 2014;371:261–269. doi: 10.1056/ NEJMcpc1304163. Halkein J, Tabruyn SP, Ricke-Hoch M, Haghikia A, Nguyen NQ, Scherr M, Castermans K, Malvaux L, Lambert V, Thiry M, Sliwa K, Noel A, Martial JA, Hilfiker-Kleiner D, Struman I. MicroRNA-146a is a therapeutic target and biomarker for peripartum cardiomyopathy. J Clin Invest. 2013;123:2143–2154. doi: 10.1172/JCI64365. Sliwa K, Skudicky D, Candy G, Bergemann A, Hopley M, Sareli P. The addition of pentoxifylline to conventional therapy improves outcome in patients with peripartum cardiomyopathy. Eur J Heart Fail. 2002;4:305–309. Desplantie O, Tremblay-Gravel M, Avram R, Marquis-Gravel G, Ducharme A, Jolicoeur EM; BRO-HF Initiative Investigators. The medical treatment of new-onset peripartum cardiomyopathy: a systematic review of prospective studies. Can J Cardiol. 2015;31:1421–1426. doi: 10.1016/j. cjca.2015.04.029. Sliwa K, Blauwet L, Tibazarwa K, Libhaber E, Smedema JP, Becker A, McMurray J, Yamac H, Labidi S, Struman I, Struhman I, HilfikerKleiner D. Evaluation of bromocriptine in the treatment of acute severe peripartum cardiomyopathy: a proof-of-concept pilot study. Circulation. 2010;121:1465–1473. doi: 10.1161/CIRCULATIONAHA.109.901496. Cleland JG, Cullington D. Digoxin: quo vadis? Circ Heart Fail. 2009;2:81–85. doi: 10.1161/CIRCHEARTFAILURE.109.859322. Chaggar PS, Shaw SM, Williams SG. Is foxglove effective in heart failure? Cardiovasc Ther. 2015;33:236–241. doi: 10.1111/1755-5922.12130. Bozkurt B, Villaneuva FS, Holubkov R, Tokarczyk T, Alvarez RJ Jr, MacGowan GA, Murali S, Rosenblum WD, Feldman AM, McNamara DM. Intravenous immune globulin in the therapy of peripartum cardiomyopathy. J Am Coll Cardiol. 1999;34:177–180. McNamara DM, Holubkov R, Starling RC, Dec GW, Loh E, Torre-Amione G, Gass A, Janosko K, Tokarczyk T, Kessler P, Mann DL, Feldman AM. Controlled trial of intravenous immune globulin in recent-onset dilated cardiomyopathy. Circulation. 2001;103:2254–2259. Biteker M, Duran NE, Kaya H, Gündüz S, Tanboğa HÎ, Gökdeniz T, Kahveci G, Akgün T, Yildiz M, Õzkan M. Effect of levosimendan and predictors of recovery in patients with peripartum cardiomyopathy, a randomized clinical trial. Clin Res Cardiol. 2011;100:571–577. doi: 10.1007/ s00392-010-0279-7. Hilfiker-Kleiner D, Kaminski K, Podewski E, Bonda T, Schaefer A, Sliwa K, Forster O, Quint A, Landmesser U, Doerries C, Luchtefeld M, Poli V, Schneider MD, Balligand JL, Desjardins F, Ansari A, Struman I, Nguyen NQ, Zschemisch NH, Klein G, Heusch G, Schulz R, Hilfiker A, Drexler H. 54. 55. 56. 57. 58. 59. 60. 61. 62. 63. 64. 65. 66. 67. 68. 69. 70. 71. 72. A cathepsin D-cleaved 16 kDa form of prolactin mediates postpartum cardiomyopathy. Cell. 2007;128:589–600. doi: 10.1016/j.cell.2006.12.036. Gaziano JM, Cincotta AH, O’Connor CM, Ezrokhi M, Rutty D, Ma ZJ, Scranton RE. Randomized clinical trial of quick-release bromocriptine among patients with type 2 diabetes on overall safety and cardiovascular outcomes. Diabetes Care. 2010;33:1503–1508. doi: 10.2337/dc09-2009. Francis GS, Parks R, Cohn JN. The effects of bromocriptine in patients with congestive heart failure. Am Heart J. 1983;106(pt 1):100–106. Haghikia A, Podewski E, Libhaber E, Labidi S, Fischer D, Roentgen P, Tsikas D, Jordan J, Lichtinghagen R, von Kaisenberg CS, Struman I, Bovy N, Sliwa K, Bauersachs J, Hilfiker-Kleiner D. Phenotyping and outcome on contemporary management in a German cohort of patients with peripartum cardiomyopathy. Basic Res Cardiol. 2013;108:366. doi: 10.1007/ s00395-013-0366-9. Turkalj I, Braun P, Krupp P. Surveillance of bromocriptine in pregnancy. JAMA. 1982;247:1589–1591. US Food and Drug Administration. Sandoz Pharmaceutical Corp.; bromocriptine mesylate (Parlodel); withdrawal of approval of the indication for the prevention of physiological lactation. Fed Reg. 1995;60:3404–3405. Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, Ezzati M, Grantham-McGregor S, Katz J, Martorell R, Uauy R; Maternal and Child Nutrition Study Group. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382:427–451. doi: 10.1016/S0140-6736(13)60937-X. Safirstein JG, Ro AS, Grandhi S, Wang L, Fett JD, Staniloae C. Predictors of left ventricular recovery in a cohort of peripartum cardiomyopathy patients recruited via the internet. Int J Cardiol. 2012;154:27–31. doi: 10.1016/j.ijcard.2010.08.065. Haghikia A, Podewski E, Berliner D, Sonnenschein K, Fischer D, Angermann CE, Böhm M, Röntgen P, Bauersachs J, Hilfiker-Kleiner D. Rationale and design of a randomized, controlled multicentre clinical trial to evaluate the effect of bromocriptine on left ventricular function in women with peripartum cardiomyopathy. Clin Res Cardiol. 2015;104:911–917. doi: 10.1007/s00392-015-0869-5. Greer IA. Clinical practice: pregnancy complicated by venous thrombosis. N Engl J Med. 2015;373:540–547. doi: 10.1056/NEJMcp1407434. Altuwaijri WA, Kirkpatrick ID, Jassal DS, Soni A. Vanishing left ventricular thrombus in a woman with peripartum cardiomyopathy: a case report. BMC Res Notes. 2012;5:544. doi: 10.1186/1756-0500-5-544. Shimamoto T, Marui A, Oda M, Tomita S, Nakajima H, Takeuchi T, Komeda M. A case of peripartum cardiomyopathy with recurrent left ventricular apical thrombus. Circ J. 2008;72:853–854. Kharwar RB, Chandra S, Dwivedi SK, Saran RK. A pedunculated left ventricular thrombus in a women with peripartum cardiomyopathy: evaluation by three dimensional echocardiography. J Cardiovasc Ultrasound. 2014;22:139–143. doi: 10.4250/jcu.2014.22.3.139. Kim DY, Islam S, Mondal NT, Mussell F, Rauchholz M. Biventricular thrombi associated with peripartum cardiomyopathy. J Health Popul Nutr. 2011;29:178–180. Goland S, Modi K, Bitar F, Janmohamed M, Mirocha JM, Czer LS, Illum S, Hatamizadeh P, Elkayam U. Clinical profile and predictors of complications in peripartum cardiomyopathy. J Card Fail. 2009;15:645–650. doi: 10.1016/j.cardfail.2009.03.008. Zehir R, Karabay CY, Kocabay G, Kalayci A, Akgun T, Kirma C. An unusual presentation of peripartum cardiomyopathy: recurrent transient ischemic attacks. Rev Port Cardiol. 2014;33:561.e1–561.e3. doi: 10.1016/j.repc.2014.02.025. Kane A, Mbaye M, Ndiaye MB, Diao M, Moreira PM, Mboup C, Diop IB, Sarr M, Kane A, Moreau JC, Ba SA. Evolution and thromboembolic complications of the idiopathic peripartal cardiomyopathy at Dakar University Hospital: forward-looking study about 33 cases [in French]. J Gynecol Obstet Biol Reprod (Paris). 2010;39:484–489. doi: 10.1016/j. jgyn.2010.01.008. Diao M, Diop IB, Kane A, Camara S, Kane A, Sarr M, Ba SA, Diouf SM. Electrocardiographic recording of long duration (Holter) of 24 hours during idiopathic cardiomyopathy of the peripartum [in French]. Arch Mal Coeur Vaiss. 2004;97:25–30. Tokuda M, Stevenson WG, Nagashima K, Rubin DA. Electrophysiological mapping and radiofrequency catheter ablation for ventricular tachycardia in a patient with peripartum cardiomyopathy. J Cardiovasc Electrophysiol. 2013;24:1299–1301. doi: 10.1111/jce.12250. DeBenedetti Zunino ME, Schuger C, Lahiri M. High rate of ventricular arrhythmias in women with peripartum cardiomyopathy and implanted cardioverter defibrillators. J Am Coll Cardiol. 2014;63. doi: 10.1016/ S0735-1097(14)60313-2. Downloaded from http://circ.ahajournals.org/ at CONS CALIFORNIA DIG LIB on April 4, 2016 1408 Circulation April 5, 2016 73. Duncker D, Haghikia A, König T, Hohmann S, Gutleben KJ, Westenfeld R, Oswald H, Klein H, Bauersachs J, Hilfiker-Kleiner D, Veltmann C. Risk for ventricular fibrillation in peripartum cardiomyopathy with severely reduced left ventricular function: value of the wearable cardioverter/defibrillator. Eur J Heart Fail. 2014;16:1331–1336. doi: 10.1002/ejhf.188. 74. Saltzberg MT, Szymkiewicz S, Bianco NR. Characteristics and outcomes of peripartum versus nonperipartum cardiomyopathy in women using a wearable cardiac defibrillator. J Card Fail. 2012;18:21–27. doi: 10.1016/j. cardfail.2011.09.004. 75. Su TW, Tseng YH, Wu TI, Lin PJ, Wu MY. Extracorporeal life support in adults with hemodynamic collapse from fulminant cardiomyopathies: the chance of bridging to recovery. ASAIO J. 2014;60:664–669. doi: 10.1097/ MAT.0000000000000141. 76. Park SH, Chin JY, Choi MS, Choi JH, Choi YJ, Jung KT. Extracorporeal membrane oxygenation saved a mother and her son from fulminant peripartum cardiomyopathy. J Obstet Gynaecol Res. 2014;40:1940–1943. doi: 10.1111/jog.12421. 77. Bouabdallaoui N, Mastroianni C, Revelli L, Demondion P, Lebreton G. Predelivery extracorporeal membrane oxygenation in a life-threatening peripartum cardiomyopathy: save both mother and child. Am J Emerg Med. 2015;33:1713.e1–1713.e2. doi: 10.1016/j.ajem.2015.03.014. 78. Gevaert S, Van Belleghem Y, Bouchez S, Herck I, De Somer F, De Block Y, Tromp F, Vandecasteele E, Martens F, De Pauw M. Acute and critically ill peripartum cardiomyopathy and “bridge to” therapeutic options: a single center experience with intra-aortic balloon pump, extra corporeal membrane oxygenation and continuous-flow left ventricular assist devices. Crit Care. 2011;15:R93. doi: 10.1186/cc10098. 79. Aggarwal A, Modi S, Kumar S, Korrapati C, Tatooles A, Pappas PS, Bhat G. Use of a single-circuit CentriMag® for biventricular support in postpartum cardiomyopathy. Perfusion. 2013;28:156–159. doi: 10.1177/0267659112464713. 80. McNamara DM, Elkayam U, Alharethi R, Damp J, Hsich E, Ewald G, Modi K, Alexis JD, Ramani GV, Semigran MJ, Haythe J, Markham DW, Marek J, Gorcsan J 3rd, Wu WC, Lin Y, Halder I, Pisarcik J, Cooper LT, Fett JD; IPAC Investigators. Clinical outcomes for peripartum cardiomyopathy in north america: results of the IPAC Study (Investigations of PregnancyAssociated Cardiomyopathy). J Am Coll Cardiol. 2015;66:905–914. doi: 10.1016/j.jacc.2015.06.1309. 81. Amos AM, Jaber WA, Russell SD. Improved outcomes in peripartum cardiomyopathy with contemporary. Am Heart J. 2006;152:509–513. doi: 10.1016/j.ahj.2006.02.008. 82. Loyaga-Rendon RY, Pamboukian SV, Tallaj JA, Acharya D, Cantor R, Starling RC, Naftel D, Kirklin J. Outcomes of patients with peripartum cardiomyopathy who received mechanical circulatory support: data from the Interagency Registry for Mechanically Assisted Circulatory Support. Circ Heart Fail. 2014;7:300–309. doi: 10.1161/CIRCHEARTFAILURE.113.000721. 83. Rasmusson K, Brunisholz K, Budge D, Horne BD, Alharethi R, Folsom J, Connolly JJ, Stehlik J, Kfoury A. Peripartum cardiomyopathy: post-transplant outcomes from the United Network for Organ Sharing Database. J Heart Lung Transplant. 2012;31:180–186. doi: 10.1016/j.healun.2011.11.018. 84. Laghari AH, Khan AH, Kazmi KA. Peripartum cardiomyopathy: ten year experience at a tertiary care hospital in Pakistan. BMC Res Notes. 2013;6:495. doi: 10.1186/1756-0500-6-495. 85. Kamiya CA, Kitakaze M, Ishibashi-Ueda H, Nakatani S, Murohara T, Tomoike H, Ikeda T. Different characteristics of peripartum cardiomyopathy between patients complicated with and without hypertensive disorders: results from the Japanese nationwide survey of peripartum cardiomyopathy. Circ J. 2011;75:1975–1981. 86. Sliwa K, Libhaber E, Elliott C, Momberg Z, Osman A, Zühlke L, Lachmann T, Nicholson L, Thienemann F, Roos-Hesselink J, Anthony J. Spectrum of cardiac disease in maternity in a low-resource cohort in South Africa. Heart. 2014;100:1967–1974. doi: 10.1136/heartjnl-2014-306199. 87. Blauwet LA, Libhaber E, Forster O, Tibazarwa K, Mebazaa A, HilfikerKleiner D, Sliwa K. Predictors of outcome in 176 South African patients with peripartum cardiomyopathy. Heart. 2013;99:308–313. doi: 10.1136/ heartjnl-2012-302760. 88. Biteker M, Ilhan E, Biteker G, Duman D, Bozkurt B. Delayed recovery in peripartum cardiomyopathy: an indication for long-term follow-up and sustained therapy. Eur J Heart Fail. 2012;14:895–901. doi: 10.1093/ eurjhf/hfs070. 89. Goland S, Bitar F, Modi K, Safirstein J, Ro A, Mirocha J, Khatri N, Elkayam U. Evaluation of the clinical relevance of baseline left ventricular ejection fraction as a predictor of recovery or persistence of severe dysfunction in women in the United States with peripartum cardiomyopathy. J Card Fail. 2011;17:426–430. doi: 10.1016/j.cardfail.2011.01.007. 90. Hu CL, Li YB, Zou YG, Zhang JM, Chen JB, Liu J, Tang YH, Tang QZ, Huang CX. Troponin T measurement can predict persistent left ventricular dysfunction in peripartum cardiomyopathy. Heart. 2007;93:488–490. doi: 10.1136/hrt.2006.087387. 91. Elkayam U. Risk of subsequent pregnancy in women with a history of peripartum cardiomyopathy. J Am Coll Cardiol. 2014;64:1629–1636. doi: 10.1016/j.jacc.2014.07.961. 92. Fett JD, Shah TP, McNamara DM. Why do some recovered peripartum cardiomyopathy mothers experience heart failure with a subsequent pregnancy? Curr Treat Options Cardiovasc Med. 2015;17:354. doi: 10.1007/s11936-014-0354-x. 93. Mouquet F, Lions C, de Groote P, Bouabdallaoui N, Willoteaux S, Dagorn J, Deruelle P, Lamblin N, Bauters C, Beregi JP. Characterisation of peripartum cardiomyopathy by cardiac magnetic resonance imaging. Eur Radiol. 2008;18:2765–2769. doi: 10.1007/s00330-008-1067-x. 94. Lampert MB, Weinert L, Hibbard J, Korcarz C, Lindheimer M, Lang RM. Contractile reserve in patients with peripartum cardiomyopathy and recovered left ventricular function. Am J Obstet Gynecol. 1997;176(pt 1):189–195. 95. Ruys TP, Roos-Hesselink JW, Hall R, Subirana-Domènech MT, GrandoTing J, Estensen M, Crepaz R, Fesslova V, Gurvitz M, De Backer J, Johnson MR, Pieper PG. Heart failure in pregnant women with cardiac disease: data from the ROPAC. Heart. 2014;100:231–238. doi: 10.1136/ heartjnl-2013-304888. 96. Cénac A, Gaultier Y, Devillechabrolle A, Moulias R. Enterovirus infection in peripartum cardiomyopathy. Lancet. 1988;2:968–969. 97. Bültmann BD, Klingel K, Näbauer M, Wallwiener D, Kandolf R. High prevalence of viral genomes and inflammation in peripartum cardiomyopathy. Am J Obstet Gynecol. 2005;193:363–365. doi: 10.1016/j. ajog.2005.01.022. 98. Fett JD. Viral particles in endomyocardial biopsy tissue from peripartum cardiomyopathy patients. Am J Obstet Gynecol. 2006;195:330–331; author reply 331. doi: 10.1016/j.ajog.2005.10.810. 99. Arora NP, Mohamad T, Mahajan N, Danrad R, Kottam A, Li T, Afonso LC. Cardiac magnetic resonance imaging in peripartum cardiomyopathy. Am J Med. Sci. 2014;347:112–117. doi: 10.1097/MAJ.0b013e31828155e3. 100. Renz DM, Röttgen R, Habedank D, Wagner M, Böttcher J, Pfeil A, Dietz R, Kivelitz D, Elgeti T. New insights into peripartum cardiomyopathy using cardiac magnetic resonance imaging. Rofo. 2011;183:834–841. doi: 10.1055/s-0031-1281600. 101. Kara RJ, Bolli P, Karakikes I, Matsunaga I, Tripodi J, Tanweer O, Altman P, Shachter NS, Nakano A, Najfeld V, Chaudhry HW. Fetal cells traffic to injured maternal myocardium and undergo cardiac differentiation. Circ Res. 2012;110:82–93. doi: 10.1161/CIRCRESAHA.111.249037. 102. Cénac A, Sacca-Vehounkpe J, Poupon J, Dossou-Yovo-Akindes R, D’Almeida-Massougbodji M, Tchabi Y, Agboton H. Serum selenium and dilated cardiomyopathy in Cotonou, Benin [in French]. Med Trop (Mars). 2009;69:272–274. 103. Homans DC. Peripartum cardiomyopathy. N Engl J Med. 1985;312:1432– 1437. doi: 10.1056/NEJM198505303122206. 104. Bajou K, Herkenne S, Thijssen VL, D’Amico S, Nguyen NQ, Bouché A, Tabruyn S, Srahna M, Carabin JY, Nivelles O, Paques C, Cornelissen I, Lion M, Noel A, Gils A, Vinckier S, Declerck PJ, Griffioen AW, Dewerchin M, Martial JA, Carmeliet P, Struman I. PAI-1 mediates the antiangiogenic and profibrinolytic effects of 16K prolactin. Nat Med. 2014;20:741–747. doi: 10.1038/nm.3552. 105. Patten IS, Rana S, Shahul S, Rowe GC, Jang C, Liu L, Hacker MR, Rhee JS, Mitchell J, Mahmood F, Hess P, Farrell C, Koulisis N, Khankin EV, Burke SD, Tudorache I, Bauersachs J, del Monte F, Hilfiker-Kleiner D, Karumanchi SA, Arany Z. Cardiac angiogenic imbalance leads to peripartum cardiomyopathy. Nature. 2012;485:333–338. doi: 10.1038/ nature11040. 106. Arany Z, Foo SY, Ma Y, Ruas JL, Bommi-Reddy A, Girnun G, Cooper M, Laznik D, Chinsomboon J, Rangwala SM, Baek KH, Rosenzweig A, Spiegelman BM. HIF-independent regulation of VEGF and angiogenesis by the transcriptional coactivator PGC-1alpha. Nature. 2008;451:1008– 1012. doi: 10.1038/nature06613. 107. Powe CE, Levine RJ, Karumanchi SA. Preeclampsia, a disease of the maternal endothelium: the role of antiangiogenic factors and implications for later cardiovascular disease. Circulation. 2011;123:2856–2869. doi: 10.1161/CIRCULATIONAHA.109.853127. 108. Bdolah Y, Lam C, Rajakumar A, Shivalingappa V, Mutter W, Sachs BP, Lim KH, Bdolah-Abram T, Epstein FH, Karumanchi SA. Twin pregnancy and the risk of preeclampsia: bigger placenta or relative ischemia? Am J Obstet Gynecol. 2008;198:428.e1–428.e6. doi: 10.1016/j.ajog.2007.10.783. Downloaded from http://circ.ahajournals.org/ at CONS CALIFORNIA DIG LIB on April 4, 2016 Arany and Elkayam Peripartum Cardiomyopathy 1409 108a.Damp J, Givertz MM, Semigran M, Alharethi R, Ewald G, Felker GM, Bozkurt B, Boehmer J, Haythe J, Skopicki H, Hanley-Yanez K, Pisarcik J, Halder I, Gorcsan J 3rd, Rana S, Arany Z, Fett JD, McNamara DM; IPAC Investigators. Relaxin-2 and Soluble Flt1 Levels in Peripartum Cardiomyopathy: Results of the Multicenter IPAC Study. JACC Heart Fail. 2016 Feb 27. pii: S2213-1779(16)00018-4. doi: 10.1016/j. jchf.2016.01.004. 109.Thadhani R, Hagmann H, Schaarschmidt W, Roth B, Cingoez T, Karumanchi SA, Wenger J, Lucchesi KJ, Tamez H, Lindner T, Fridman A, Thome U, Kribs A, Danner M, Hamacher S, Mallmann P, Stepan H, Benzing T. Removal of soluble Fms-like tyrosine kinase-1 by dextran sulfate apheresis in preeclampsia. J Am Soc Nephrol. 2016;27:903–913. doi: 10.1681/ASN.2015020157. 110. Łasińska-Kowaraa M, Lango R, Kowalik M, Jarmoszewicz K. Accelerated heart function recovery after therapeutic plasma exchange in patient treated with biventricular mechanical circulatory support for severe peripartum cardiomyopathy. Eur J Cardiothorac Surg. 2014;46:1035–1036. doi: 10.1093/ejcts/ezu178. 111. Karaye KM, Lindmark K, Henein MY. Left ventricular structure and function among sisters of peripartum cardiomyopathy patients. Int J Cardiol. 2015;182:34–35. doi: 10.1016/j.ijcard.2014.12.102. 112. Horne BD, Rasmusson KD, Alharethi R, Budge D, Brunisholz KD, Metz T, Carlquist JF, Connolly JJ, Porter TF, Lappé DL, Muhlestein JB, Silver R, Stehlik J, Park JJ, May HT, Bair TL, Anderson JL, Renlund DG, Kfoury AG. Genome-wide significance and replication of the chromosome 12p11.22 locus near the PTHLH gene for peripartum cardiomyopathy. Circ Cardiovasc Genet. 2011;4:359–366. doi: 10.1161/ CIRCGENETICS.110.959205. 113. Bakre MM, Zhu Y, Yin H, Burton DW, Terkeltaub R, Deftos LJ, Varner JA. Parathyroid hormone-related peptide is a naturally occurring, protein kinase A-dependent angiogenesis inhibitor. Nat Med. 2002;8:995– 1003. doi: 10.1038/nm753. 114. Ntusi NB, Wonkam A, Shaboodien G, Badri M, Mayosi BM. Frequency and clinical genetics of familial dilated cardiomyopathy in Cape Town: implications for the evaluation of patients with unexplained cardiomyopathy. S Afr Med J. 2011;101:394–398. 115. Massad LS, Reiss CK, Mutch DG, Haskel EJ. Familial peripartum cardiomyopathy after molar pregnancy. Obstet Gynecol. 1993;81(pt 2):886–888. 116. Pearl W. Familial occurrence of peripartum cardiomyopathy. Am Heart J. 1995;129:421–422. 117. Pierce JA, Price BO, Joyce JW. Familial occurrence of postpartal heart failure. Arch Intern Med. 1963;111:651–655. 118.van Spaendonck-Zwarts KY, Posafalvi A, van den Berg MP, HilfikerKleiner D, Bollen IA, Sliwa K, Alders M, Almomani R, van Langen IM, van der Meer P, Sinke RJ, van der Velden J, Van Veldhuisen DJ, van Tintelen JP, Jongbloed JD. Titin gene mutations are common in families with both peripartum cardiomyopathy and dilated cardiomyopathy. Eur Heart J. 2014;35:2165–2173. doi: 10.1093/eurheartj/ehu050. 119. Morales A, Painter T, Li R, Siegfried JD, Li D, Norton N, Hershberger RE. Rare variant mutations in pregnancy-associated or peripartum cardiomyopathy. Circulation. 2010;121:2176–2182. doi: 10.1161/ CIRCULATIONAHA.109.931220. 120. Ware JS, Li J, Mazaika E, Yasso CM, DeSouza T, Cappola TP, Tsai EJ, Hilfiker-Kleiner D, Kamiya CA, Mazzarotto F, Cook SA, Halder I, Prasad SK, Pisarcik J, Hanley-Yanez K, Alharethi R, Damp J, Hsich E, Elkayam U, Sheppard R, Kealey A, Alexis J, Ramani G, Safirstein J, Boehmer J, Pauly DF, Wittstein IS, Thohan V, Zucker MJ, Liu P, Gorcsan J 3rd, McNamara DM, Seidman CE, Seidman JG, Arany Z; IMAC-2 and IPAC Investigators. Shared genetic predisposition in peripartum and dilated cardiomyopathies. N Engl J Med. 2016;374:233–241. doi: 10.1056/NEJMoa1505517. 121. Roberts AM, Ware JS, Herman DS, Schafer S, Baksi J, Bick AG, Buchan RJ, Walsh R, John S, Wilkinson S, Mazzarotto F, Felkin LE, Gong S, MacArthur JA, Cunningham F, Flannick J, Gabriel SB, Altshuler DM, Macdonald PS, Heinig M, Keogh AM, Hayward CS, Banner NR, Pennell DJ, O’Regan DP, San TR, de Marvao A, Dawes TJ, Gulati A, Birks EJ, Yacoub MH, Radke M, Gotthardt M, Wilson JG, O’Donnell CJ, Prasad SK, Barton PJ, Fatkin D, Hubner N, Seidman JG, Seidman CE, Cook SA. Integrated allelic, transcriptional, and phenomic dissection of the cardiac effects of titin truncations in health and disease. Sci Transl Med. 2015;7:270ra6. doi: 10.1126/scitranslmed.3010134. 122. Herman DS, Lam L, Taylor MR, Wang L, Teekakirikul P, Christodoulou D, Conner L, DePalma SR, McDonough B, Sparks E, Teodorescu DL, Cirino AL, Banner NR, Pennell DJ, Graw S, Merlo M, Di Lenarda A, Sinagra G, Bos JM, Ackerman MJ, Mitchell RN, Murry CE, Lakdawala NK, Ho CY, Barton PJ, Cook SA, Mestroni L, Seidman JG, Seidman CE. Truncations of titin causing dilated cardiomyopathy. N Engl J Med. 2012;366:619–628. doi: 10.1056/NEJMoa1110186. 123. Sliwa K, Hilfiker-Kleiner D, Mebazaa A, Petrie MC, Maggioni AP, Regitz-Zagrosek V, Schaufelberger M, Tavazzi L, van Veldhuisen DJ, Roos-Hesslink JW, Shah AJ, Seferovic PM, Elkayam U, van SpaendonckZwarts K, Bachelier-Walenta K, Mouquet F, Kraigher-Krainer E, Hall R, Ponikowski P, McMurray JJ, Pieske B. EURObservational Research Programme: a worldwide registry on peripartum cardiomyopathy (PPCM) in conjunction with the Heart Failure Association of the European Society of Cardiology Working Group on PPCM. Eur J Heart Fail. 2014;16:583–591. doi: 10.1002/ejhf.68. 124. National Institutes of Health. NIH RePORTer. https://projectreporter.nih. gov/reporter.cfm. Accessed October 15, 2015. Downloaded from http://circ.ahajournals.org/ at CONS CALIFORNIA DIG LIB on April 4, 2016 Peripartum Cardiomyopathy Zolt Arany and Uri Elkayam Circulation. 2016;133:1397-1409 doi: 10.1161/CIRCULATIONAHA.115.020491 Circulation is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231 Copyright © 2016 American Heart Association, Inc. All rights reserved. Print ISSN: 0009-7322. Online ISSN: 1524-4539 The online version of this article, along with updated information and services, is located on the World Wide Web at: http://circ.ahajournals.org/content/133/14/1397 Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in Circulation can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office. Once the online version of the published article for which permission is being requested is located, click Request Permissions in the middle column of the Web page under Services. Further information about this process is available in the Permissions and Rights Question and Answer document. Reprints: Information about reprints can be found online at: http://www.lww.com/reprints Subscriptions: Information about subscribing to Circulation is online at: http://circ.ahajournals.org//subscriptions/ Downloaded from http://circ.ahajournals.org/ at CONS CALIFORNIA DIG LIB on April 4, 2016