Print - Arteriosclerosis, Thrombosis, and Vascular Biology
Anuncio

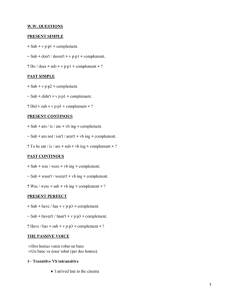
Original Article Proteomic Analysis of Intraluminal Thrombus Highlights Complement Activation in Human Abdominal Aortic Aneurysms Roxana Martinez-Pinna, Julio Madrigal-Matute, Carlos Tarin, Elena Burillo, Margarita Esteban-Salan, Carlos Pastor-Vargas, Jes S. Lindholt, Juan Antonio Lopez, Enrique Calvo, Melina Vega de Ceniga, Olivier Meilhac, Jesus Egido, Luis M. Blanco-Colio, Jean-Baptiste Michel, Jose Luis Martin-Ventura Downloaded from http://atvb.ahajournals.org/ by guest on November 20, 2016 Objective—To identify proteins related to intraluminal thrombus biological activities that could help to find novel pathological mechanisms and therapeutic targets for human abdominal aortic aneurysm (AAA). Approach and Results—Tissue-conditioned media from patients with AAA were analyzed by a mass spectrometry–based strategy using liquid chromatography coupled to tandem mass spectrometry. Global pathway analysis by Ingenuity software highlighted the presence of several circulating proteins, among them were proteins from the complement system. Complement C3 concentration and activation were assessed in plasma from AAA patients (small AAA, AAA diameter=3–5 cm and large AAA, AAA diameter >5 cm), showing decreased C3 levels and activation in large AAA patients. No association of a combination of single-nucleotide polymorphisms in complement genes between large and small AAA patients was observed. Intense extracellular C3 inmunostaining, along with C9, was observed in AAA thrombus. Analysis of C3 in AAA tissue homogenates and tissue-conditioned media showed increased levels of C3 in AAA thrombus, as well as proteolytic fragments (C3a/C3c/C3dg), suggesting its local deposition and activation. Finally, the functional role of local complement activation in polymorphonuclear (PMN) cell activation was tested, showing that C3 blockade by anti-C3 antibody was able to decrease thrombus-induced neutrophil chemotaxis and reactive oxygen species production. Conclusions—A decrease of systemic C3 concentration and activity in the later stages of AAA associated with local complement retention, consumption, and proteolysis in the thrombus could induce PMN chemotaxis and activation, playing a detrimental role in AAA progression. (Arterioscler Thromb Vasc Biol. 2013;33:00-00.) Key Words: aortic aneurysm, abdominal ◼ complement system proteins ◼ inflammation ◼ neutrophils ◼ thrombosis C linical and pathophysiological evidence indicates that intraluminal thrombus (ILT) plays a role in the evolution of abdominal aortic aneurysms (AAA).1 The eccentric distribution of the ILT was associated with continuous expansion,2 and aortic ILT volume is associated with AAA growth.3–5 It has been reported that large ILT areas were significantly associated with increased AAA expansion.3 Speelman et al4 demonstrated that larger ILT in AAA was not only associated with a higher AAA growth rate, but also with a lower wall stress. These data suggest that weakening of the AAA wall, under the biological dynamics of ILT, might play a more imminent role in the process of AAA growth than the stress acting on the wall. A recent study has confirmed the association of ILT volume with AAA growth and also with cardiovascular events.5 Finally, radiological signs of ILT lysis could precede aortic rupture (crescent sign).1 In parallel, accumulating data suggest that biological activities associated with leukocyte, platelet, and red blood cell accumulation in ILT play an important role in AAA progression.6–11 Thus, the identification of novel proteins related to ILT biological activities could help to find novel pathogenic mechanisms, as well as therapeutic targets, of AAA. In previous studies, following a strategy based on the analysis of AAA tissue-conditioned media by gel- or array-based proteomic techniques, we identified proteins related to different pathological processes involved in AAA, such as oxidation10 and proteolysis.12 To further explore the pathophysiology of ILT in human AAA by increasing the number of identified proteins, ILT and wall-conditioned media were analyzed in this study using liquid chromatography and tandem mass spectrometry (MS). Global pathway analysis of identified peptides/proteins by Ingenuity software highlighted Received on: November 29, 2012; final version accepted on: May 9, 2013. From the Vascular Research Lab (R.M.-P., J.M.-M., C.T., E.B.) and Immunology Lab (C.P.-V.), IIS-Fundación Jiménez Diaz-Autonoma University, Madrid, Spain; Hospital de Galdakao, Vizcaya, Spain (M.E.-S., M.V.d.C.); Departments of Cardiovascular and Thoracic Surgery, University Hospital of Odense and Viborg, Denmark (J.S.L.); Unidad de Proteómica, Centro Nacional de Investigaciones Cardiovasculares, Madrid, Spain (J.A.L.); and Inserm, U698, Univ Paris, Paris, France (O.M., J.-B.M.). The online-only Data Supplement is available with this article at http://atvb.ahajournals.org/lookup/suppl/doi:10.1161/ATVBAHA.112.301191/-/DC1. Correspondence to Jose Luis Martin-Ventura, PhD, Vascular Research Lab, IIS-Fundacion Jimenez Diaz, Autonoma University, Av Reyes Católicos 2, 28040 Madrid, Spain. E-mail [email protected] © 2013 American Heart Association, Inc. Arterioscler Thromb Vasc Biol is available at http://atvb.ahajournals.org 1 DOI: 10.1161/ATVBAHA.112.301191 2 Arterioscler Thromb Vasc Biol August 2013 Downloaded from http://atvb.ahajournals.org/ by guest on November 20, 2016 that complement system components were highly enriched in AAA tissue-conditioned media. The complement system plays a major role in innate immunity, participating in host defense responses against microorganisms via opsonization, chemoattraction of leukocytes, cell activation, and bridging innate and adaptive immunity.13–16 However, disturbances in this defense machinery contribute to the pathogenesis of various autoimmune diseases, such as systemic lupus erythematosus. Systemic lupus erythematosus is characterized by decreased circulating complement components associated with their deposition and activation in host tissues. As complement proteins are mainly synthesized by the liver, we hypothesized that the high levels of complement peptides/proteins identified in AAA thrombus-conditioned media could be related to its trapping from the blood and by increased proteolytic activation. To test this hypothesis, we first assessed C3 concentration and activity in blood of AAA patients at different stages of the disease. Second, we analyzed the presence and activation of C3 in AAA tissue and tissue-conditioned media. Finally, we studied the effect of complement activation in human AAA thrombus on neutrophil chemotaxis and oxidation, key mechanisms involved in AAA pathogenesis. Materials and Methods Materials and Methods are available in the online-only Supplement. Results Liquid Chromatography and Tandem MS Analysis of Proteins From AAA Tissue-Conditioned Media Proteins obtained from AAA thrombus- and wall-conditioned media were trypsin digested, and the resulting peptides were then fractionated by 2-dimensional liquid chromatography using a strong cation exchange column followed by C18 reversed phase chromatography. Finally, the MS and MS/ MS spectra were used for protein identification. Table II in the online-only Data Supplement lists all the proteins identified in AAA tissue supernatants, where 60% of them were classically secreted. To organize identified proteins, Ingenuity software was used to find the most enriched canonical pathways in our samples. A total of 257 proteins extracted from the protein lists corresponding to thrombus and wall layer supernatants were analyzed in the same data set. Among others, coagulation and complement systems have been found as relatively enriched in the AAA tissue supernatants (compared with the human genome database; Figure 1A). Interestingly, several complement-related proteins (eg, C3, C9, clusterin, factor H) were identified, which are represented in gray color in Figure 1B. Systemic C3 Concentrations and Activity in AAA Patients As C3 is the central molecule in the complement cascade, we analyzed serum concentrations of C3 in a first cohort of healthy controls (n=28) and AAA patients at follow-up (small AAA, AAA diameter=3–5 cm [n=62]) or at surgery (large AAA, AAA diameter >5 cm, [n=28]). Clinical characteristics are shown in Tables 1 and 2. Increased C3 concentrations were observed in small AAA patients compared with both controls and large AAA patients (controls=148±5 versus small AAA=177±4 versus large AAA=124±8 mg/dL; P<0.01). Logistic regression analysis showed that association between increased C3 in small AAA patients and controls remained significant when adjusted by age but was lost when adjusted for risk factors (not shown), whereas the decreased C3 in large versus small AAA patients persisted after adjustment for risk factors (Table III in the online-only Data Supplement). Plasma C3 concentrations correlated with lipid levels (r=0.4 for lowdensity lipoprotein and triglycerides and r=−0.4 for highdensity lipoprotein; P<0.001 for all) and aortic size (r=−0.4; P<0.005). Linear regression analysis between C3 and aortic size was also independent of risk factors (Table IV in the online-only Data Supplement). To confirm previous data, we further analyzed a second cohort of patients (Tables 1 and 2), showing that large AAA patients (n=39) have significantly decreased C3 plasma concentrations compared with small AAA patients (n=26; 122±4 versus 138±4 mg/dL; P<0.01; Figure 2A), which persisted after adjustment for risk factors (Table III in the online-only Data Supplement). A nonsignificant negative correlation was shown for C3 and aortic size (r=−0.2; P=0.1; Figure 2C). To test whether complement activity is modified in plasma of AAA patients at different stages of evolution, we performed an alternative pathway (AP) 50 assay that measures the ability of the patient’s plasma to lyse rabbit erythrocytes. Accordingly, large AAA patients have decreased complement activity compared with small AAA patients (42±5 versus 75±4% lysis; P<0.01; Figure 2B). Logistic regression analysis showed that the significant association between AP50 in large AAA compared with small AAA patients persisted after adjustment for risk factors (Table III in the online-only Data Supplement). AP50 correlated with aortic size (r=−0.4; P<0.005; Figure 2D), which persisted after adjustment for risk factors (Table IV in the online-only Data Supplement). Genetic Association Study No association of single-nucleotide polymorphisms (SNPs) in the complement cascade in AAA patient and control studies has been recently described.17,18 To get further insight into a potential genetic association between complement and AAA evolution, we analyzed whether the decrease in C3 concentrations and activity in large versus small AAA patients could be related to a particular combination of SNPs in complement genes (complotypes), as described for other disorders, such as age-related macular degeneration.19 However, no association was found between these complotypes and AAA in patients at different stages of the disease (large versus small AAA). In plasma samples available from these patients (n=138), we further confirmed that C3 concentrations were decreased in large AAA patients (n=66) compared with small AAA patients (n=72; 194±5 versus 210±5 mg/dL; P<0.05). Logistic regression analysis showed that the significant association between decreased plasma C3 in large AAA compared with small AAA patients persisted after adjustment for risk factors (Table III in the online-only Data Supplement). A nonsignificant negative correlation was shown for C3 and aortic size (r=−0.2; P=0.07). Martinez-Pinna et al Complement Activation in Human AAA 3 Downloaded from http://atvb.ahajournals.org/ by guest on November 20, 2016 Figure 1. Ingenuity pathway analysis of identified proteins by liquid chromatography and tandem mass spectrometry (MS). A, The bar graphic shows the canonical pathway distribution represented by gene enrichment. Ratios show the number of genes associated with each pathway found in our experiment with respect to the human genome database. Fisher exact test provides P<0.05 for the 7 most abundant canonical pathways. B, Detailed inspection of the complement system cascade, where proteins identified by MS in abdominal aortic aneurysm tissue-conditioned media are represented in gray color. Protein groups or complex are yellow encircled, and receptors of different complement components are represented at the bottom of the figure. Local Complement Retention and Activation in AAA We analyzed the presence of C3 in AAA tissue by immunohistochemistry, showing an intense extracellular staining in the ILT and, to a lesser extent, in the wall, whereas healthy wall shows weak staining (Figure 3A). Similarly, high C9 staining was observed in AAA thrombus compared with wall and healthy wall (Figure I in the online-only Data Supplement). Interestingly, C3 and C9 deposition was observed in similar areas of the thrombus, suggesting complement activation (Figure 3B). Whereas C3 was mainly present in acellular areas of the thrombus, C3 in the wall was also associated with α-actin–positive cells in the media (Figure II in the onlineonly Data Supplement) and, to a lesser extent, with CD15/ Table 1. Clinical Characteristics of AAA Patients in First Cohort Table 2. Clinical Characteristics of AAA Patients in Second Cohort Small AAA (n=62) Sex (men/women) Age, y±SD Large AAA (n=28) 62/0 28/0 69.9±6.7 73.4±6.6 Small AAA (n=26) Large AAA (n=39) Sex (men/women) 24/2 37/2 Age, y±SD 79±5 70±10 Dyslipidemia, % 56.5 37 Dyslipidemia, % 46 53 Current smoking, % 37.1 42.9 Current smoking, % 15 30 Diabetes mellitus, % 19.4 3.6 Diabetes mellitus, % 30 7 Hypertension, % 64.5 64.3 Hypertension, % 73 46 Heart disease, % 32.3 21.4 Heart disease, % 23 23 AAA indicates abdominal aortic aneurysm. AAA indicates abdominal aortic aneurysm. 4 Arterioscler Thromb Vasc Biol August 2013 Figure 2. Systemic C3 concentration and activity in abdominal aortic aneurysm (AAA) patients. C3 concentration (A) and activity (alternative pathway [AP] 50, B) in plasma of small AAA patients (n=26) and large AAA patients (n=39). Correlation of C3 concentration (C) and activity (D) with aortic size. Downloaded from http://atvb.ahajournals.org/ by guest on November 20, 2016 CD68-positive cells mainly in adventitia (Figure III in the online-only Data Supplement), suggesting the possible synthesis by resident or infiltrating cells in the wall. To test this hypothesis, we performed both real-time polymerase chain reaction and Western blot of tissue homogenates. No detectable C3 mRNA was obtained from 3 of 6 thrombi analyzed, and very low levels were observed in the rest (0.01±0.02 a.u.). No differences were observed in C3 mRNA levels between healthy and AAA wall (0.22±0.1 versus 0.28±0.05 a.u., not shown). In contrast, C3 protein levels in tissue homogenates were higher in ILT compared with pathological wall and healthy wall, confirming the results observed by immunohistochemistry (Figure 4A). We further tested C3 concentration and activation in the conditioned media of human ILT and wall of AAA, as well as in healthy media. C3 levels were increased in the AAA thrombus compared with the pathological wall and healthy wall (5.6±0.5 versus 2.4±0.2 versus 0.9±0.2 µg/mL; P<0.001 for all comparisons). Furthermore, C3 proteolytic fragments of 35 to 40 kDa (corresponding to the molecular weight of C3c/C3dg; Figure 4A–4C) appear mainly in tissue and tissueconditioned media of ILT and, to a lesser extent, in the wall (media and adventitia) of AAA, whereas almost no proteolytic fragments were observed in healthy wall. Because complement activation could involve proteolytic degradation of C3 by proteases, such as plasmin or elastase,13 abundantly present in ILT,6,7 we assessed whether proteolysis of C3 in the thrombus of AAA could take place ex vivo. In this respect, when native C3 was incubated with the luminal part of the thrombus, the 35 to 40 kDa fragments observed in ILT-conditioned media were increased (Figure 4D). Role of Complement Activation in AAA ThrombusInduced PMN Chemotaxis and Activation As we did not observe the first fragment of C3 activation, C3a, by Western blot probably as a result of its low molecular weight, we analyzed the presence of C3a in tissue-conditioned media by ELISA. We have observed that C3a levels are increased in ILT compared with the wall of AAA and also the healthy wall (P<0.001 for all comparisons; Figure 5A). Furthermore, because C3a is involved in PMN chemotaxis and reactive oxygen species production, we address the functional role of complement activation by proteolysis in ILT. Neutrophils were allowed to migrate through a filter into a lower chamber containing thrombus-conditioned media, and the effect of C3 blocking was assessed. Neutrophils were attracted by luminal thrombus, and C3 blockade by anti-C3 antibody was able to decrease such effect (P<0.001; Figure 5B). Similar effect was observed when native C3 was used as a positive control (not shown). Furthermore, incubation of thrombusconditioned media with fresh neutrophils increased reactive oxygen species levels, which was prevented by anti-C3 antibody (Figure 5C). Discussion In the present article, the combination of nano-liquid chromatography and LTQ-Orbitrap MS allowed us to identify larger lists of proteins from AAA tissue-conditioned media compared with array or gel-based approaches.10,12 Several proteins previously associated with different AAA pathological mechanisms have been identified (eg, immune–inflammatory response [clusterin], thrombosis [fibrinogen]). Interestingly, a recent proteomic study has also shown increased levels of clusterin, a complement lysis inhibitor able to block the terminal complement cascade in AAA thrombus-conditioned media.20 In contrast, clusterin concentrations were decreased in AAA plasma, and the authors suggested that ILT could sequester systemic proteins.20 In agreement, the functional distribution of the identified proteins in our study has shown an enrichment in circulating proteins (eg, coagulation and complement systems). As complement proteins are mainly synthesized by the liver, we hypothesized that the high levels Martinez-Pinna et al Complement Activation in Human AAA 5 Downloaded from http://atvb.ahajournals.org/ by guest on November 20, 2016 Figure 3. Local complement retention in abdominal aortic aneurysm (AAA) tissue. Immunohistochemistry of C3 in thrombus (A), wall (C), and healthy wall (D). Negative control (nonspecific IgG; B). C3 (E) and C9 (F) immunostaining is performed in serial sections of AAA thrombus. Magnification, ×20 (inset, ×120, showing areas with polymorphonuclears). of complement peptides/proteins identified in AAA thrombus-conditioned media could be related to its trapping from the blood and by increased proteolytic activation. We first analyzed C3 concentrations in AAA patients and controls. Circulating C3 levels were increased in small AAA patients compared with controls, probably suggesting an initial hepatic response to vascular injury. However, when we performed a multivariate analysis, including risk factors, no significant differences were observed between small AAA patients and controls in agreement with previous data,21 discarding its potential use as a diagnostic biomarker. Regarding risk factors, we have observed a positive correlation between C3 and lipid levels. Lipids have been previously suggested as a potential mechanism leading to complement activation in experimental and human hypercholesterolemia.22 Furthermore, it has been proposed that IgG is an initial mechanism leading to C3 activation in an experimental model of AAA,23 and increased IgG concentrations have been recently observed in small AAA patients versus controls. However, IgG concentrations decline in large AAA patients.24 In agreement, we have shown that C3 concentrations are decreased in large compared with small AAA patients, which was independent of different risk factors. In addition, when we performed an AP50 assay to test whether complement activity is modified during AAA evolution, we showed a negative association of complement activity with later stages of disease and with aortic size, independent of risk factors. On the whole, our data suggest that systemic C3 increases in the initial phases of AAA, probably as a response to injury of the wall to increased lipid and IgG concentrations, whereas a decrease in systemic complement concentration and activation takes place in the later stages of AAA. Complement deficiencies (inherited or acquired) could be linked to the development of autoimmunity, as shown in systemic lupus erythematosus where decreased complement 6 Arterioscler Thromb Vasc Biol August 2013 A C T W H B T M D M T H C3dg C3c C3b iC3b C3 ADV T HM T+C3 HADV C3 Downloaded from http://atvb.ahajournals.org/ by guest on November 20, 2016 Figure 4. Local complement activation in abdominal aortic aneurysm (AAA) tissue and tissue-conditioned media. A, Representative Western blot of C3 in tissue homogenates of human AAA thrombus (T), pathological wall (W=media+adventitia), and healthy wall (H=media+adventitia). B, Representative Western blot of C3 in tissue-conditioned media of human AAA thrombus (T), pathological wall (media, M, and adventitia, ADV), and healthy wall (media, HM, and adventitia, HADV). C, Representative Western blot of C3 in tissue-conditioned media of human AAA pathological wall (media, M), thrombus (T), and healthy wall (H). Fragments of C3 (C3dg, C3c, C3b, iC3b) or native C3 purified as described.20 D, Representative Western blot of C3 in thrombus-conditioned media incubated with native C3. Arrows indicate proteolytic fragments of C3. components are observed. To check whether genetic anomalies in complement genes could take place in AAA evolution, we performed a genetic study analyzing a particular combination of SNPs in complement genes (complotypes). This approach has been also described for other disorders, such as age-related macular degeneration.19 No association on any of the combination of SNPs analyzed was found between small and large AAA patients, similar to previous studies where those individual SNPs were assessed in AAA patients and controls.17,18 It has been suggested that the acquired diminution in circulating complement proteins in autoimmune diseases could be associated with deposition of complement components in host tissue.13 In this respect, complement proteins have been previously detected in human AAA wall.17,25,26 We observed that C3 protein levels were increased in tissue and tissue-conditioned media of AAA wall compared with healthy aortic wall, whereas C3 mRNA is similarly present in pathological and healthy wall in agreement with Hinterseher et al.17 But, Hinterseher et al17 did not show C3 staining in the thrombus. In contrast, we have shown that human AAA thrombus displays an intense extracellular staining, along with increased protein levels in tissue homogenates and tissueconditioned media of ILT compared with wall. Differences between both immunohistological studies could be related to the different antibodies used. Furthermore, C3 in thrombus from acute myocardial infarction has also been observed.27 Because the liver is the major source of complement proteins in humans and low/undetectable C3 mRNA levels were observed in thrombus homogenates, the high extracellular levels of C3 observed in AAA thrombus should be associated with its retention from serum and subsequent activation. In this regard, high C9 immunostaining was also shown in acellular areas of the thrombus and wall compared with healthy wall. In agreement, Pagano et al26 showed C5B9 in the luminal side of the wall, whereas no staining was observed in healthy wall. Similarly, Tulamo et al28 also observed complement activation and C5B9 formation in the less cellular part of intracranial artery aneurysm wall. Finally, we showed intense C9 immunostaining associated with C3 deposition, suggesting complement activation in AAA thrombus. Complement activation involves the classical pathway, the lectin pathway, the AP, and the extrinsic pathway.13 The classical pathway can be activated by antibodies or by other stimulus, such as CRP. The AP is part of the innate (nonantigen-specific) immune system and is important in antibodyindependent defense against bacterial infection. The extrinsic pathway involves proteolytic degradation of C3 by proteases, such as elastase, and phagocytes. Furthermore, other components of the coagulation system, such as plasmin, could also participate in complement activation.16 In this respect, human AAA thrombus could be a privileged site for complement activation because proteases and PMNs are abundant in the ILT of AAA.6,7 When we analyzed C3 levels in AAA tissue and tissue-conditioned media by Western blot, we observed proteolytic fragments of C3 in AAA thrombus and thrombus-conditioned media. Furthermore, these products of C3 Martinez-Pinna et al Complement Activation in Human AAA 7 Downloaded from http://atvb.ahajournals.org/ by guest on November 20, 2016 Figure 5. Role of complement activation in abdominal aortic aneurysm (AAA) thrombus-induced chemotaxis. A, ELISA of C3a in tissueconditioned media of human AAA thrombus (T, n=10), pathological wall (media [M, n=10] and adventitia [ADV, n=10]), and healthy wall (media [HM, n=10] and adventitia [HADV, n=10]). * and † P<0.001 for T vs M and ADV and M and ADV vs HM and HADV, respectively. B, Chemotaxis assay showing polymorphonuclear (PMN) migration toward the thrombus (T), thrombus preincubated with anti-C3 (T+antiC3 at 1:100 or 1:10 dilution), and thrombus preincubated with anti-IgG (T+IgG, for nonspecific chemotaxis). *P<0.001 for anti-C3 vs T. C, NADPH-dependent reactive oxygen species (ROS) production in PMNs stimulated during 2 minutes with thrombus-conditioned media, thrombus preincubated with anti-C3 (T+anti-C3 at 1:100 or 1:10 dilution), or thrombus preincubated with anti-IgG (T+IgG). *P<0.05 for anti-C3 vs T. proteolysis and activation were increased when native C3 protein was coincubated with the luminal part of AAA, supporting that in vivo proteolysis of C3 protein could take place within the thrombus of AAA. In addition, C3c/C3dg levels were increased in AAA wall compared with healthy wall. These proteolytic products could participate in the shift from innate to adaptive immunity, characteristic of the adventitial response in AAA.29 Finally, given that C3a is released in the initial step of the proteolytic processing of C3, C3a levels were assessed in AAA tissue and healthy wall. In agreement with the results obtained for C3, C3a was increased in conditioned media of ILT and wall compared with healthy aorta wall, further supporting proteolysis of C3 in AAA tissue. C3aR mRNA is upregulated in AAA tissue,17 favoring the potential interaction with C3a in AAA and its functional consequences. In this respect, it is already described that the complement acts as a critical mediator of neutrophil recruitment in AAA mice lesions.26 Interestingly, we have observed that PMN chemotaxis induced by the ILT could be modulated by incubation with an anti-C3 antibody. Furthermore, C3a has been involved in PMN respiratory burst.30 We observed that NADPHdependent reactive oxygen species production is increased when fresh PMNs are incubated with ILT-conditioned media, and this effect was prevented by C3 blockade. In any case, we should take into account that these functional activities of the thrombus could be also related to the presence of other factors, such as tissue factor, clotting factors (eg, Xa), or thrombin, among others. Thrombin is involved in the activation of the complement system, further confirming a coordinated action of the coagulation and complement systems.16 Interestingly, both systems have been associated with innate immunity into what Engelmann and Massberg31 recently described as immunothrombus. Thrombin also modulates fibrinolysis by activating the plasma carboxypeptidase, thrombin-activatable procarboxypeptidase B. In this respect, enhanced AAA formation in pCPB−/− mice was observed to be associated with plasmin generation.32 On the whole, all these data suggest that complement activation by proteases present in the thrombus could contribute to AAA pathogenesis. Several studies have recently demonstrated that genetic modification of different mediators of the complement pathway could reduce experimental AAA formation.23,26 However, complement activation is modulated by several complement inhibitors (eg, CD59, vitronectin). In this respect, Tulamo et al28 showed a differential distribution of complement inhibitors in different areas of the wall of intracranial artery aneurysms. These data suggest that a disturbed complement regulation is associated with an increased susceptibility to complement activation and inflammation and may be also cell loss.28 In our previous study, vitronectin was shown to be downregulated in tissue of ruptured AAA compared with nonruptured AAA.33 Finally, deficiency of CD59 accelerated, whereas transgenic overexpression of human CD59 attenuated, the progression of experimental AAA.34 At the therapeutic level, anti-C5 8 Arterioscler Thromb Vasc Biol August 2013 blockade was able to reverse atherosclerosis associated with a decrease in complement deposition.35 Because atherosclerosis and AAA share some pathological mechanisms, it could be interesting to address whether the therapeutic modulation of complement activators or inhibitors may have a protective role in AAA progression. On the whole, the decrease of systemic C3 concentration and activity in the later stages of AAA associated with local complement retention, consumption, and proteolysis in the thrombus could induce PMN activation, playing a detrimental role in AAA. Future studies targeting complement activation could be an attractive therapeutic strategy to prevent AAA progression. Acknowledgments Downloaded from http://atvb.ahajournals.org/ by guest on November 20, 2016 We thank Patricia Llamas Granada for technical assistance and Santiago Rodriguez de Cordoba for the reagents provided and for his helpful comments, suggestions, and critical revision of the content of the article. Sources of Funding The article has been supported by the EC, FAD project (FP-7, HEALTH F2-2008–200647), the Spanish MICIN (SAF2010/21852), Fundacion Ramon Areces, Ministerio de Sanidad y Consumo, Instituto de Salud Carlos III, Redes RECAVA (RD12/0042/00038), and biobancos (RD09/0076/00101). Disclosures None. References 1. Michel JB, Martin-Ventura JL, Egido J, Sakalihasan N, Treska V, Lindholt J, Allaire E, Thorsteinsdottir U, Cockerill G, Swedenborg J; FAD EU Consortium. Novel aspects of the pathogenesis of aneurysms of the abdominal aorta in humans. Cardiovasc Res. 2011;90:18–27. 2. Vega de Céniga M, Gómez R, Estallo L, de la Fuente N, Viviens B, Barba A. Analysis of expansion patterns in 4–4.9 cm abdominal aortic aneurysms, Ann Vasc Surg 2008;22:37–44. 3. Wolf YG, Thomas WS, Brennan FJ, Goff WG, Sise MJ, Bernstein EF. Computed tomography scanning findings associated with rapid expansion of abdominal aortic aneurysms. J Vasc Surg. 1994;20:529–535; discussion 535. 4. Speelman L, Schurink GW, Bosboom EM, Buth J, Breeuwer M, van de Vosse FN, Jacobs MH. The mechanical role of thrombus on the growth rate of an abdominal aortic aneurysm. J Vasc Surg. 2010;51:19–26. 5. Parr A, McCann M, Bradshaw B, Shahzad A, Buttner P, Golledge J. Thrombus volume is associated with cardiovascular events and aneurysm growth in patients who have abdominal aortic aneurysms. J Vasc Surg. 2011;53:28–35. 6. Fontaine V, Jacob MP, Houard X, Rossignol P, Plissonnier D, AnglesCano E, Michel JB. Involvement of the mural thrombus as a site of protease release and activation in human aortic aneurysms. Am J Pathol. 2002;161:1701–1710. 7. Fontaine V, Touat Z, Mtairag el M, Vranckx R, Louedec L, Houard X, Andreassian B, Sebbag U, Palombi T, Jacob MP, Meilhac O, Michel JB. Role of leukocyte elastase in preventing cellular re-colonization of the mural thrombus. Am J Pathol. 2004;164:2077–2087. 8. Touat Z, Ollivier V, Dai J, Huisse MG, Bezeaud A, Sebbag U, Palombi T, Rossignol P, Meilhac O, Guillin MC, Michel JB. Renewal of mural thrombus releases plasma markers and is involved in aortic abdominal aneurysm evolution. Am J Pathol. 2006;168:1022–1030. 9.Ramos-Mozo P, Rodriguez C, Pastor-Vargas C, Blanco-Colio LM, Martinez-Gonzalez J, Meilhac O, Michel JB, Vega de Ceniga M, Egido J, Martin-Ventura JL. Plasma profiling by a protein array approach identifies IGFBP-1 as a novel biomarker of abdominal aortic aneurysm. Atherosclerosis. 2012;221:544–550. 10. Martinez-Pinna R, Ramos-Mozo P, Madrigal-Matute J, Blanco-Colio LM, Lopez JA, Calvo E, Camafeita E, Lindholt JS, Meilhac O, Delbosc S, Michel JB, Vega de Ceniga M, Egido J, Martin-Ventura JL. Identification of peroxiredoxin-1 as a novel biomarker of abdominal aortic aneurysm. Arterioscler Thromb Vasc Biol. 2011;31:935–943. 11. Martin-Ventura JL, Madrigal-Matute J, Martinez-Pinna R, Ramos-Mozo P, Blanco-Colio LM, Moreno JA, Tarin C, Burillo E, Fernandez-Garcia CE, Egido J, Meilhac O, Michel JB. Erythrocytes, leukocytes and platelets as a source of oxidative stress in chronic vascular diseases: detoxifying mechanisms and potential therapeutic options. Thromb Haemost. 2012;108:435–442. 12. Dejouvencel T, Féron D, Rossignol P, Sapoval M, Kauffmann C, Piot JM, Michel JB, Fruitier-Arnaudin I, Meilhac O. Hemorphin 7 reflects hemoglobin proteolysis in abdominal aortic aneurysm. Arterioscler Thromb Vasc Biol. 2010;30:269–275. 13.Markiewski MM, Lambris JD. The role of complement in inflammatory diseases from behind the scenes into the spotlight. Am J Pathol. 2007;171:715–727. 14.Ehrnthaller C, Ignatius A, Gebhard F, Huber-Lang M. New insights of an old defense system: structure, function, and clinical relevance of the complement system. Mol Med. 2011;17:317–329. 15.Markiewski MM, Huber-Lang M, Younkin EM, Sarma JV, Riedemann N, McGuire SR, Lu KT, Kunkel R, Younger JG, Zetoune FS, Ward PA. Generation of C5a by phagocytic cells. Am J Pathol. 2002;161:1849–59. 16. Amara U, Flierl MA, Rittirsch D, Klos A, Chen H, Acker B, Brückner UB, Nilsson B, Gebhard F, Lambris JD, Huber-Lang M. Molecular intercommunication between the complement and coagulation systems. J Immunol. 2010;185:5628–5636. 17.Hinterseher I, Erdman R, Donoso LA, et al. Role of complement cascade in abdominal aortic aneurysms. Arterioscler Thromb Vasc Biol. 2011;31:1653–1660. 18.Bradley DT, Badger SA, Bown MJ, Sayers RD, Hughes AE. Coding polymorphisms in the genes of the alternative complement pathway and abdominal aortic aneurysm. Int J Immunogenet. 2011;38:243–248. 19. Harris CL, Heurich M, Rodriguez de Cordoba S, Morgan BP. The complotype: dictating risk for inflammation and infection. Trends Immunol. 2012;33:513–521. 20.Moxon JV, Padula MP, Clancy P, Emeto TI, Herbert BR, Norman PE, Golledge J. Proteomic analysis of intra-arterial thrombus secretions reveals a negative association of clusterin and thrombospondin-1 with abdominal aortic aneurysm. Atherosclerosis. 2011;219:432–439. 21.Parry DJ, Al-Barjas HS, Chappell L, Rashid ST, Ariëns RA, Scott DJ. Markers of inflammation in men with small abdominal aortic aneurysm. J Vasc Surg. 2010;52:145–151. 22. Verdeguer F, Castro C, Kubicek M, Pla D, Vila-Caballer M, Vinué A, Civeira F, Pocoví M, Calvete JJ, Andrés V. Complement regulation in murine and human hypercholesterolemia and role in the control of macrophage and smooth muscle cell proliferation. Cardiovasc Res. 2007;76:340–350. 23. Zhou HF, Yan H, Stover CM, Fernandez TM, Rodriguez de Cordoba S, Song WC, Wu X, Thompson RW, Schwaeble WJ, Atkinson JP, Hourcade DE, Pham CT. Antibody directs properdin-dependent activation of the complement alternative pathway in a mouse model of abdominal aortic aneurysm. Proc Natl Acad Sci U S A. 2012;109:E415–E422. 24. Hellenthal FA, Pulinx B, Welten RJ, Teijink JA, van Dieijen-Visser MP, Wodzig WK, Schurink GW. Circulating biomarkers and abdominal aortic aneurysm size. J Surg Res. 2012;176:672–678. 25. Capella JF, Paik DC, Yin NX, Gervasoni JE, Tilson MD. Complement activation and subclassification of tissue immunoglobulin G in the abdominal aortic aneurysm. J Surg Res. 1996;65:31–33. 26.Pagano MB, Zhou HF, Ennis TL, Wu X, Lambris JD, Atkinson JP, Thompson RW, Hourcade DE, Pham CT. Complement-dependent neutrophil recruitment is critical for the development of elastase-induced abdominal aortic aneurysm. Circulation. 2009;119:1805–1813. 27. Distelmaier K, Adlbrecht C, Jakowitsch J, Winkler S, Dunkler D, Gerner C, Wagner O, Lang IM, Kubicek M. Local complement activation triggers neutrophil recruitment to the site of thrombus formation in acute myocardial infarction. Thromb Haemost. 2009;102:564–572. 28. Tulamo R, Frösen J, Paetau A, Seitsonen S, Hernesniemi J, Niemelä M, Järvelä I, Meri S. Lack of complement inhibitors in the outer intracranial artery aneurysm wall associates with complement terminal pathway activation. Am J Pathol. 2010;177:3224–3232. 29. Michel JB, Thaunat O, Houard X, Meilhac O, Caligiuri G, Nicoletti A. Topological determinants and consequences of adventitial responses to arterial wall injury. Arterioscler Thromb Vasc Biol. 2007;27:1259–1268. 30. Elsner J, Oppermann M, Czech W, Kapp A. C3a activates the respiratory burst in human polymorphonuclear neutrophilic leukocytes via pertussis toxin-sensitive G-proteins. Blood. 1994;83:3324–3331. 31.Engelmann B, Massberg S. Thrombosis as an intravascular effector of innate immunity. Nat Rev Immunol. 2013;13:34–45. Martinez-Pinna et al Complement Activation in Human AAA 9 32. Schultz G, Tedesco MM, Sho E, Nishimura T, Sharif S, Du X, Myles T, Morser J, Dalman RL, Leung LL. Enhanced abdominal aortic aneurysm formation in thrombin-activatable procarboxypeptidase B-deficient mice. Arterioscler Thromb Vasc Biol. 2010;30:1363–1370. 33. Urbonavicius S, Lindholt JS, Vorum H, Urbonaviciene G, Henneberg EW, Honoré B. Proteomic identification of differentially expressed proteins in aortic wall of patients with ruptured and nonruptured abdominal aortic aneurysms. J Vasc Surg. 2009;49:455–463. 34. Wu G, Chen T, Shahsafaei A, Hu W, Bronson RT, Shi GP, Halperin JA, Aktas H, Qin X. Complement regulator CD59 protects against angiotensin II-induced abdominal aortic aneurysms in mice. Circulation. 2010;121:1338–1346. 35. Wu G, Hu W, Shahsafaei A, Song W, Dobarro M, Sukhova GK, Bronson RR, Shi GP, Rother RP, Halperin JA, Qin X. Complement regulator CD59 protects against atherosclerosis by restricting the formation of complement membrane attack complex. Circ Res. 2009;104:550–558. Significance Downloaded from http://atvb.ahajournals.org/ by guest on November 20, 2016 Clinical and pathophysiological evidence indicates that intraluminal thrombus plays a role in evolution of abdominal aortic aneurysms (AAA). Intraluminal thrombus and wall-conditioned media were analyzed using a proteomic approach. Global pathway analysis of identified peptides/proteins highlighted that complement system components were highly enriched in AAA tissue-conditioned media. This could be related to its trapping from the blood (because decreased complement C3 concentration was associated with later stages of AAA in 3 different cohorts) and by increased proteolytic activation (as C3 fragments were observed in intraluminal thrombus). The functional consequences of complement retention and activation in AAA thrombus are related to increased polymorphonuclear chemotaxis and reactive oxygen species production, main mechanisms involved in AAA progression. Our data support an important role of complement activation not only in the initial phases of AAA formation (as demonstrated in experimental models of AAA) but also in human AAA progression associated with polymorphonuclear recruitment and activation in intraluminal thrombus. Downloaded from http://atvb.ahajournals.org/ by guest on November 20, 2016 Proteomic Analysis of Intraluminal Thrombus Highlights Complement Activation in Human Abdominal Aortic Aneurysms Roxana Martinez-Pinna, Julio Madrigal-Matute, Carlos Tarin, Elena Burillo, Margarita Esteban-Salan, Carlos Pastor-Vargas, Jes S. Lindholt, Juan Antonio Lopez, Enrique Calvo, Melina Vega de Ceniga, Olivier Meilhac, Jesus Egido, Luis M. Blanco-Colio, Jean-Baptiste Michel and Jose Luis Martin-Ventura Arterioscler Thromb Vasc Biol. published online May 23, 2013; Arteriosclerosis, Thrombosis, and Vascular Biology is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231 Copyright © 2013 American Heart Association, Inc. All rights reserved. Print ISSN: 1079-5642. Online ISSN: 1524-4636 The online version of this article, along with updated information and services, is located on the World Wide Web at: http://atvb.ahajournals.org/content/early/2013/05/23/ATVBAHA.112.301191 Data Supplement (unedited) at: http://atvb.ahajournals.org/content/suppl/2013/05/23/ATVBAHA.112.301191.DC1.html Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in Arteriosclerosis, Thrombosis, and Vascular Biology can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office. Once the online version of the published article for which permission is being requested is located, click Request Permissions in the middle column of the Web page under Services. Further information about this process is available in the Permissions and Rights Question and Answer document. Reprints: Information about reprints can be found online at: http://www.lww.com/reprints Subscriptions: Information about subscribing to Arteriosclerosis, Thrombosis, and Vascular Biology is online at: http://atvb.ahajournals.org//subscriptions/ Supplemental material online Supplemental tables Table I online.- Clinical characteristics of patients from the VIVA trial 1st degree relative with AAA Current smokers Diabetes Hypertension Use of ACE-inhibitors Use of beta-blocker Statin Low dose aspirin Peripheral arterial disease (PAD) Intermittent claudication Previous AMI Current angina pectoris: Age (years) Body mass index (BMI) Systolic blood pressure (mmHg) Diastolic bloodpressure (mmHg) Lowest ABI Maximal aortic diameter (mm) Aneurysmal growth rate (mm/year) ABI: Ankle brachial bloodpressure index AMI: Acute myocardial infarction N= 186 15 76 15 95 45 61 93 84 40 35 44 25 Mean 69.66 27.60 154.30 88.40 0.96 48.75 3.10 All AAA Small AAA (%) (%) 8.4 8.5 42.5 47.4 8.4 4.2 53.4 50.5 26.0 24.7 35.5 31.9 52.8 51.6 48.3 44.6 22.3 22.1 20.1 17.9 25.4 25.3 14.4 14.7 SD Mean (SD) 2.91 69.4 (2.9) 3.54 27.6(3.6) 21.67 156 (22.7) 12.00 88.3(12.3) 0.17 0.95(0.18) 15.42 37.0(5.18) 2.95 2.98(2.77) Large AAA (%) 8.0 36.4 12.5 52.4 29.8 40.0 57.5 54.7 21.6 21.7 27.7 16.9 Mean (SD) 70.0(2.8) 27.6 (3.5) 152(20.5) 88.5(11.8) 0.96(0.15) 70.0(2.84) 5.97(2.84) Table II online.- Proteins identified by LTQ-Orbitrap mass spectrometry Uniprot Code A4D0S4 A5D8V7 A6NJS3 A8K8V0 B2RMS9 D6RAK8 E9PQD6 F6THE9 G3V0G4 I3L499 O00400 O00574 O14672 O14744 O14994 O15264 O15466 O43749 O60508 O60673 O60885 O75179 O75385 O75920 O75970 O94776 O95218 O95477 O95831 P00450 P00734 P00738 P00747 P00846 P01011 P01023 P01024 P01042 P01583 Protein Name Laminin subunit beta-4 Coiled-coil domain-containing protein 151 Putative V-set and immunoglobulin domain Zinc finger protein 785 Inter-alpha (Globulin) inhibitor H4 (Plasma Kallikreinsensitive glycoprotein) Vitamin D-binding protein Serum amyloid A protein Butyrophilin-like protein 2 2-aminoadipic 6-semialdehyde dehydrogenase, isoform CRA_c Patched domain-containing protein 3 Acetyl-coenzyme A transporter 1 C-X-C chemokine receptor type 6 Disintegrin and metalloproteinase domain-containing protein 10 Protein arginine N-methyltransferase 5 Synapsin-3 Mitogen-activated protein kinase 13 Alpha-2,8-sialyltransferase 8E Olfactory receptor 1F1 Pre-mRNA-processing factor 17 DNA polymerase zeta catalytic subunit Bromodomain-containing protein 4 Ankyrin repeat domain-containing protein 17 Serine/threonine-protein kinase ULK1 Small EDRK-rich factor 1 Multiple PDZ domain protein Metastasis-associated protein MTA2 Zinc finger Ran-binding domain-containing protein 2 ATP-binding cassette sub-family A member 1 Apoptosis-inducing factor 1, mitochondrial Ceruloplasmin Prothrombin Haptoglobin Plasminogen ATP synthase subunit a Alpha-1-antichymotrypsin Alpha-2-macroglobulin Complement C3 Kininogen-1 Interleukin-1 alpha Secretory Predictions * S S S S S S S NC S NC NC NC S NC S NC S S S S NC S NC NC S NC NC S S S S S S NC S S S S S P02042 P02647 P02649 P02652 P02656 P02671 P02675 P02679 P02743 P02748 P02749 P02751 P02760 P02763 P02768 P02786 P02787 P02790 P02792 P02794 P03891 P03999 P04040 P04114 P04196 P04217 P05155 P06396 P06703 P07305 P07951 P07996 P08294 P08670 P0C0L4 P0C0L5 P10636 P10828 P10909 P11487 P12259 P13688 P16499 P16860 Hemoglobin subunit delta Apolipoprotein A-I Apolipoprotein E Apolipoprotein A-II Apolipoprotein C-III Fibrinogen alpha chain Fibrinogen beta chain Fibrinogen gamma chain Serum amyloid P-component Complement component C9 Beta-2-glycoprotein 1 Fibronectin Protein AMBP Alpha-1-acid glycoprotein 1 Serum albumin Transferrin receptor protein 1 Serotransferrin Hemopexin Ferritin light chain Ferritin heavy chain NADH-ubiquinone oxidoreductase chain 2 Short-wave-sensitive opsin 1 Catalase Apolipoprotein B-100 Histidine-rich glycoprotein Alpha-1B-glycoprotein Plasma protease C1 inhibitor Gelsolin Protein S100-A6 Histone H1.0 Tropomyosin beta chain Thrombospondin-1 Extracellular superoxide dismutase [Cu-Zn] Vimentin Complement C4-A Complement C4-B Microtubule-associated protein tau Thyroid hormone receptor beta Clusterin Fibroblast growth factor 3 Coagulation factor V Carcinoembryonic antigen-related cell adhesion molecule 1 Rod cGMP-specific 3',5'-cyclic phosphodiesterase subunit alpha Natriuretic peptides B NC S S S S NC NC S S S S S S S S S S S NC S NC NC NC S NC S S S S NC NC NC S S S S NC S S S S S NC S P17980 P20273 P20339 P22557 P22670 P22792 P23142 P24530 P26006 P27482 P29144 P29218 P31327 P32119 P35221 P35228 P35626 P36980 P37231 P40429 P41134 P43652 P46100 P46977 P47224 P47989 P48637 P49321 P49418 P49815 P49916 P50416 P51580 P51826 P51884 P52737 P54132 P59923 P60709 P63010 P68873 P69891 P69905 26S protease regulatory subunit 6A B-cell receptor CD22 Ras-related protein Rab-5A 5-aminolevulinate synthase, erythroid-specific, mitochondrial MHC class II regulatory factor RFX1 Carboxypeptidase N subunit 2 Fibulin-1 Endothelin B receptor Integrin alpha-3 Calmodulin-like protein 3 Tripeptidyl-peptidase 2 Inositol monophosphatase 1 Carbamoyl-phosphate synthase [ammonia], mitochondrial Peroxiredoxin-2 Catenin alpha-1 Nitric oxide synthase, inducible Beta-adrenergic receptor kinase 2 Complement factor H-related protein 2 Peroxisome proliferator-activated receptor gamma 60S ribosomal protein L13a DNA-binding protein inhibitor ID-1 Afamin Transcriptional regulator ATRX Dolichyl-diphosphooligosaccharide protein glycosyltransferase subunit STT3A Guanine nucleotide exchange factor MSS4 Xanthine dehydrogenase/oxidase Glutathione synthetase Nuclear autoantigenic sperm protein Amphiphysin Tuberin DNA ligase 3 Carnitine O-palmitoyltransferase 1, liver isoform Thiopurine S-methyltransferase AF4/FMR2 family member 3 Lumican Zinc finger protein 136 Bloom syndrome protein Zinc finger protein 445 Actin, cytoplasmic 1 AP-2 complex subunit beta Hemoglobin subunit beta Hemoglobin subunit gamma-1 Hemoglobin subunit alpha NC S S S S S S NC S S NC S S NC NC S NC S S S S NC S NC NC NC S NC NC NC S S NC S NC S NC S NC NC NC NC NC P80192 P82673 P98160 Q01524 Q04446 Q04725 Q06710 Q07020 Q07954 Q08379 Q08ER8 Q12788 Q12797 Q13017 Q13108 Q13114 Q13402 Q13683 Q14004 Q14767 Q14789 Q15063 Q15067 Q15431 Q15528 Q16666 Q4J6C6 Q4KMG0 Q53FM8 Q53G59 Q53WY6 Q59ER9 Q59FE5 Q59H18 Q5FWF5 Q5KSL6 Q5T5U3 Q5T686 Q5VT06 Q5VTL8 Q5VV42 Q5ZF01 Mitogen-activated protein kinase kinase kinase 9 28S ribosomal protein S35, mitochondrial Basement membrane-specific heparan sulfate proteoglycan core protein Defensin-6 1,4-alpha-glucan-branching enzyme Transducin-like enhancer protein 2 Paired box protein Pax-8 60S ribosomal protein L18 Prolow-density lipoprotein receptor-related protein 1 Golgin subfamily A member 2 Zinc finger protein 543 Transducin beta-like protein 3 Aspartyl/asparaginyl beta-hydroxylase Rho GTPase-activating protein 5 Melanoma ubiquitous mutated protein TNF receptor-associated factor 3 Unconventional myosin-VIIa Integrin alpha-7 Cyclin-dependent kinase 13 Latent-transforming growth factor beta-binding protein 2 Golgin subfamily B member 1 Periostin Peroxisomal acyl-coenzyme A oxidase 1 Synaptonemal complex protein 1 Mediator of RNA polymerase II transcription subunit 22 Gamma-interferon-inducible protein 16 Prolyl endopeptidase-like Cell adhesion molecule-related/down-regulated by oncogenes Fucose-1-phosphate guanyltransferase variant Kelch-like protein 12 Transthyretin B aggressive lymphoma gene variant A disintegrin and metalloproteinase with thrombospondin motifs 10 Serine/threonine-protein kinase TNNI3K N-acetyltransferase ESCO1 Diacylglycerol kinase kappa Rho GTPase-activating protein 21 Arginine vasopressin-induced protein 1 Centrosome-associated protein 350 Pre-mRNA-splicing factor 38B Threonylcarbamoyladenosine tRNA methylthiotransferase Activating signal cointegrator 1 complex subunit 3-like 1 S S S S S S NC NC S NC S S NC S S NC S S NC S NC S NC NC NC NC NC S NC S S NC S NC NC S NC S NC NC S S Q68CZ2 Q6IBW4 Q6P9A3 Q6U7Q0 Q6ZT12 Q70Z53 Q75T13 Q76I76 Q7Z4N2 Q7Z7C8 Q7Z7G8 Q861H1 Q86VE9 Q86Z14 Q8IVE3 Q8IWQ3 Q8IXT1 Q8IY21 Q8IYA6 Q8IYF1 Q8IYI6 Q8IYM0 Q8N119 Q8NBP0 Q8NE79 Q8NEL9 Q8NEN0 Q8NF91 Q8NI22 Q8TBF4 Q8TD19 Q8TEK3 Q8WZ42 Q92794 Q92876 Q92994 Q93100 Q969Y0 Q96DZ1 Q96EB6 Q96EC4 Q96I76 Q96J94 Tensin-3 Condensin-2 complex subunit H2 Zinc finger protein 549 Zinc finger protein 322 E3 ubiquitin-protein ligase UBR3 Protein FRA10AC1 GPI inositol-deacylase Protein phosphatase Slingshot homolog 2 Transient receptor potential cation channel subfamily M member 1 Transcription initiation factor TFIID subunit 8 Vacuolar protein sorting-associated protein 13B MHC class I antigen Serine incorporator 5 Beta-klotho Pleckstrin homology domain-containing family H member 2 Serine/threonine-protein kinase BRSK2 Nitric oxide-inducible gene protein Probable ATP-dependent RNA helicase DDX60 Cytoskeleton-associated protein 2-like RNA polymerase II transcription factor SIII subunit A2 Exocyst complex component 8 Protein FAM186B Matrix metalloproteinase-21 Tetratricopeptide repeat protein 13 Blood vessel epicardial substance Phospholipase DDHD1 Armadillo repeat-containing protein 2 Nesprin-1 Multiple coagulation factor deficiency protein 2 Zinc finger CCHC-type and RNA-binding motif-containing protein 1 Serine/threonine-protein kinase Nek9 Histone-lysine N-methyltransferase, H3 lysine-79 specific Titin Histone acetyltransferase KAT6A Kallikrein-6 Transcription factor IIIB 90 kDa subunit Phosphorylase b kinase regulatory subunit beta NXPE family member 3 Endoplasmic reticulum lectin 1 NAD-dependent protein deacetylase sirtuin-1 AHNAK nucleoprotein G patch domain-containing protein 3 Piwi-like protein 1 NC NC S S S NC S S NC NC NC S NC S S NC S S NC S NC NC S S S NC NC S S S NC NC S NC S S NC S S S S NC S Q96JS3 Q96NW4 Q96P70 Q96Q83 Q96RD9 Q96RW7 Q96S42 Q96SU4 Q96T58 Q99457 Q9BVI0 Q9BWV1 Q9BYK8 Q9BZ29 Q9BZF1 Q9BZH6 Q9GZS0 Q9H2D6 Q9H2X9 Q9H3L0 Q9H7D0 Q9H7X0 Q9H9P8 Q9HAH1 Q9NPC7 Q9NPI1 Q9NQR4 Q9NQW7 Q9NS00 Q9NU22 Q9NX55 Q9NYF8 Q9NYP7 Q9P0K1 Q9P212 Q9P2K8 Q9P2N7 Q9P2R3 Q9UHC7 Q9UKT4 Q9ULV0 PiggyBac transposable element-derived protein 1 Ankyrin repeat domain-containing protein 27 Importin-9 Alpha-ketoglutarate-dependent dioxygenase alkB homolog 3 Fc receptor-like protein 5 Hemicentin-1 Nodal homolog Oxysterol-binding protein-related protein 9 Msx2-interacting protein Nucleosome assembly protein 1-like 3 PHD finger protein 20 Brother of CDO Peroxisomal proliferator-activated receptor A Dedicator of cytokinesis protein 9 Oxysterol-binding protein-related protein 8 WD repeat-containing protein 11 Dynein intermediate chain 2, axonemal TRIO and F-actin-binding protein Solute carrier family 12 member 5 Methylmalonic aciduria and homocystinuria type D protein, mitochondrial Dedicator of cytokinesis protein 5 N-alpha-acetyltransferase 60 L-2-hydroxyglutarate dehydrogenase, mitochondrial Zinc finger protein 556 Myoneurin Bromodomain-containing protein 7 Omega-amidase NIT2 Xaa-Pro aminopeptidase 1 Glycoprotein-N-acetylgalactosamine 3-betagalactosyltransferase 1 Midasin Huntingtin-interacting protein K Bcl-2-associated transcription factor 1 Elongation of very long chain fatty acids protein 5 Disintegrin and metalloproteinase domain-containing protein 22 1-phosphatidylinositol 4,5-bisphosphate phosphodiesterase epsilon-1 Eukaryotic translation initiation factor 2-alpha kinase 4 Kelch-like protein 13 Ankyrin repeat and FYVE domain-containing protein 1 E3 ubiquitin-protein ligase makorin-1 F-box only protein 5 Unconventional myosin-Vb S S S S S NC S NC NC NC S S NC S NC NC NC S NC S NC NC S NC S NC S S S NC S NC NC S NC S S NC S S S Q9Y2G5 Q9Y4A5 Q9Y4D8 Q9Y6D5 Q9Y6J0 GDP-fucose protein O-fucosyltransferase 2 Transformation/transcription domain-associated protein Probable E3 ubiquitin-protein ligase C12orf51 Brefeldin A-inhibited guanine nucleotide-exchange protein 2 Calcineurin-binding protein cabin-1 S S NC S S * Secretory Predictions data provided by SecretomeP.1 Software (S: Classically secreted proteins; NC: Non-classically secreted proteins. Classically secreted: 155 proteins, 60% of total; Non-classically secreted: 102 proteins, 40% of total) Table III online. Logistic regression analysis with AAA stage as dependent variable a) First cohort B SE OR P-value (Constant) -,931 3,842 ,394 ,808 Age ,089 ,050 1,093 ,075 Dyslipidemia ,-,823 ,733 ,439 ,261 Current smoking 1,094 ,747 2,986 ,143 Diabetes -1,828 1,277 ,161 ,152 Hypertension ,533 ,710 1,703 ,453 Heart disease -,862 ,765 ,422 ,260 C3 -,042 ,011 ,959 ,000 B SE OR P-value (Constant) 26,759 7,499 4,2E11 ,000 Sex -,262 1,190 ,769 ,826 Age -,242 ,079 ,785 ,002 Dyslipidemia ,877 ,959 2,404 ,360 Current smoking -1,567 1,176 ,209 ,183 Diabetes -4,096 1,594 ,017 ,010 Hypertension -,875 ,979 ,417 ,372 Heart disease 1,247 1,099 3,479 ,257 C3 -0,052 ,019 ,949 ,007 AP50 -0,102 ,036 ,903 ,005 b) Second cohort c) Third cohort (VIVA trial) C3 Body mass index (kg(m2) Current smoking Diabetes mellitus Diastolic blood pressure (mmHg) Peripheral arterial disease (ABI<0.9) Constant B -,013 ,017 -1,141 ,974 S.E. ,006 ,065 ,449 ,977 OR ,987 1,018 ,320 2,647 Pvalue ,020 ,787 ,011 ,319 ,016 ,017 1,016 ,370 -,174 ,525 ,840 ,740 4,619 479,459 ,181 6,173 Table IV online. Linear regression analysis with AAA diameter as dependent variable a) First cohort Coefficients(a) Unstandardized Coefficients Standardized Coefficients Model T Sig. 2,402 ,019 B Std. Error (Constant) 33,971 14,141 Sex 4,482 5,693 ,083 ,787 ,434 Age ,226 ,165 ,147 1,374 ,173 Dyslipidemia -3,303 2,280 -,165 -1,449 ,152 Current smoking 5,251 2,242 ,257 2,343 ,022 Diabetes -2,526 3,044 -,091 -,830 ,409 Hypertension ,873 2,249 ,042 ,388 ,699 Heart disease -,138 2,402 -,006 -,057 ,954 C3 -8,02E02 ,025 -,330 -3,247 ,002 Beta b) Second cohort Coefficients(a) Unstandardized Coefficients Standardized Coefficients Model T Sig. 6,204 ,000 B Std. Error (Constant) 99,069 15,968 Sex -2,562 7,550 -,045 -,339 ,736 Age -,408 ,202 -,301 -2,024 ,049 Dyslipidemia -5,107 3,499 -,195 -1,459 ,151 Current smoking -2,918 4,295 -,098 -,679 ,500 Diabetes -5,968 4,717 -,177 -1,265 ,212 Hypertension 1,253 3,775 ,047 ,332 ,742 Heart disease 1,730 4,345 ,057 ,398 ,692 AP50 -,133 ,060 -,327 -2,230 ,031 Beta AAA thrombus A Negative B Healthy wall AAA wall C D Supplemental figure I. Immunohistochemistry of C9 in thrombus (A), wall (C) and Healthy wall (D). NegaBve control (non-­‐specific IgG) (B). MagnificaBon 20x. C3 A SMC B Supplemental figure II. Immunohistochemistry of C3 (A) and immunofluorescence of alpha-­‐acBn (B) in AAA wall. MagnificaBon 40x. C3 A CD15 B CD68 C Supplemental figure III. Immunohistochemistry of C3 (A), CD15 (B) and CD68 (C) in serial secBons of AAA wall. MagnificaBon 10x. Material and methods AAA patients Spanish patients In a first cohort, serum from 62 male patients with an asymptomatic infrarenal AAA was collected during clinical examination (aortic size = 3-5 cm, small AAA). Additionally, serum from 28 male patients with an asymptomatic infrarenal AAA was collected before surgical repair (aortic size > 5 cm, large AAA). Twenty-eight healthy male controls with non-dilated infrarenal aortas (aortic size < 3 cm, confirmed with abdominal ultrasound) and no risk factors were obtained from a screening program undertaken in our area of care. All these samples were obtained from Galdakao Ursansolo Hospital (Bilbao, Spain). In a second cohort, plasma samples were obtained from the biobank of IIS-FJD (Madrid, Spain) including 26 small AAA patients and 39 large AAA patients. Hypertension was defined as systolic blood pressure (sBP) >140 mmHg and/or diastolic pressure (dBP) ≥90 mmHg measured during the examination, after the participant had been sitting for at least 30 minutes, or the participant was already taking hypotensive medication. A patient was considered diabetic if he was under treatment (supervised diet, hypoglycaemic oral medication, insulin) or we found basal glycaemia >120 mg/dL and/or HbA1c >=6.5%. Hypercholesterolemia was defined as total basal cholesterol levels ≥200 mg/dl, LDL levels ≥100 mg/dl or the patients were receiving specific medication or a supervised diet. Cardiac disease included coronary heart disease, valvular disease, cardiomyopathy and arrhythmia. Clinical characteristics are summarized in Table 1. The studies were approved by Spanish center’s Research and Ethics Committees, and informed consent from the patients and the controls for their inclusion in the study was obtained. Danish patients Blood cells were obtained from 186 patients from the randomised population based Viborg Vascular (VIVA) screening trial screening 65-74 year old men for AAA, peripheral arterial disease and unrecognised hipertension (1). Informed consent was obtained from all subjects before participation, and the study was approved by the Local Ethics Committee of the Viborg Hospital, Denmark, and performed in accordance with the Helsinki Declaration. Cases were selected according to initial size and growth rate. Clinical characteristics of the patients are included in table 1 online. AAA tissue and tissue-conditioned media Sixteen AAA thrombus and wall samples were collected from patients enrolled in the RESAA protocol (2) undergoing surgery (three for MS analysis, ten for ELISA, western-blot and immunohistochemistry and six for homogenization). One part was included in paraffin for immunohistochemistry and the rest was dissected into thrombus and wall (media and adventitia) for incubation in a RPMI protein-free medium. All patients gave their informed written consent and the protocol was approved by a French ethics committee (CPB, Cochin Hospital). Twelve control aortas (six for immunohistochemistry and six for homogenization) were sampled from dead organ donors with the authorization of the French Biomedicine Agency (PFS 09007). These control aortic samples were macroscopically normal, devoid of early atheromatous lesions. Different layers of AAA thrombus and wall, as well as healthy walls, were cut into small pieces (5 mm2) and separately incubated in RPMI 1640 medium containing antibiotics and an antimycotic (Gibco) for 24 hours at 37°C (6 ml/g of wet tissue). The conditioned medium (supernatant containing proteins released by the tissue sample) was obtained after centrifugation as 3,000 g for 10 minutes at 20°C. In some cases, native C3 [purified as previously described in Alcorlo M et al, (3)] was incubated for 90 min at 37ºC with 1 µl of thrombusconditioned media and then subjected to western-blot. In addition, tissues were snapfrozen in N2 liquid and homogenates (0.2 g) were divided and resuspended for mRNA and protein analysis. Bidimensional nanoLC-MS/MS analysis Proteins from AAA–tissue conditioned media obtained from 3 patients were precipitated using 2D clean-up kit (GE Healthcare) and resuspended in Triethylammonium bicarbonate (TEAB) buffer for protein concentration measure by Bradford assay (Biorad). A total of 50 µg of protein was reduced with 5 mM Tris (2carboxiethyl) phosphine (TCEP) for 1 hour at 60ºC and alkylated using 10 mM smethylmethenethiosulponate (MMTS) at room temperature during 10 minutes. Later, proteins were digested with trypsin, at 37oC for 5h, at a ratio of 1:50 trypsin to protein. Digested samples were subjected to nano-liquid chromatography coupled to MS for protein identification. Peptides were injected onto a strong cation exchange (SCX) microprecolumn (500 µm I.D. and 15mm BioX-SCX TM, LC Packings, Amsterdam, The Netherlands) with a flow rate of 30µL/min as a first dimension separation. Peptides were eluted from the column as fractions by injecting three salt steps of increasing concentration of ammonium acetate (10, 100 and 2000 mM). Each of the three fractions together with the nonretained fraction was on line injected onto a C-18 reversed phase (RP) nano-column (100 mm I.D. and 12 cm, Mediterranea sea, Teknokroma) and analyzed in a continuous acetonitrile gradient consisting of 0-50% B in 90 min, 50-90% B in 1 min (B=95% acetonitrile, 0.5% acetic acid). A flow rate of 300 nL/min was used to elute peptides from the RP nano-column to an emitter nanospray needle for real time ionization and peptide fragmentation on an LTQOrbitrap XL mass spectrometer (Thermo Fisher). An enhanced FT-resolution spectrum (resolution = 30000) followed by the MS/MS spectra from most intense three parent ions (dissociated using CID activation) was analyzed along the chromatographic run (130 min). Dynamic exclusion was set at 1 min. Database Searching Tandem mass spectra were extracted by Proteome Discoverer v1.0 software (Thermo Fisher). Charge state deconvolution and deisotoping were not performed. For protein identification, fragmentation spectra were searched against a curated subset of a human database (human_ref.fasta; 2003, April; 39414 entries) using Sequest (Thermo Fisher Scientific version 1.0.43.2) and X-Tandem (The GPM, thegpm.org; version 2007.01.01.1) engines. Sequest and X-Tandem were searched allowing two missed trypsin cleavages, and a tolerance of 15 ppm or 0.8 Da was set for full MS or MS/MS spectra searches, respectively. Methane thiosulfate alkylation of cysteine residues and oxidation of methionine were allowed as variable modifications. Finally, Scaffold v.3.00.02 software (Proteome Software Inc) was used to validate MS/MS based peptide and protein identifications. Bioinformatics Pathway analysis were created using Ingenuity System software (Ingenuity System Software, Inc.). Enriched canonical pathways were calculated as the ratio between the number of genes for one pathway found in the experiment and the total number of genes destinated to that pathway. All the ratios shown are associated to p-values provided by Fisher’s exact test. These analyses were derived from all protein identifications obtained from the MS analyses. Predictions of protein secretions were made using a software package, publically available, hosted at the Technical University of Denmark, as described (4). Quantification of C3 and C3a Soluble concentrations of C3 in human plasma samples were automatically measured using VITROS chemistry products C3 reagents in the VITROS 5,1 FS and VITROS 5600 Integrated System analyzers, following the manufacturer´s instructions (OrthoClinical Diagnostics, Johnson & Johnson). Soluble concentrations of C3 in serum samples from first cohort or in plasma samples from third cohort were assayed automatically by timed nephelometry using a BNII Nephelometer (Siemens9). Both methods were standardized against the international reference preparation CRM 470 (RPPHS). C3 and C3a in conditioned media was measured with commercial kits (EC2101 Assaypro and 550499 BD, respectively) following the manufacturer’s instructions. AP50 assay To test the hemolitic capacity of the complement system, red blood cells (RBCs) from healthy rabbits were used together with human sera as described (5). Briefly, washed RBCs were resuspended to 1% (v/v) in AP-CFTD buffer (5 mM sodium barbitone pH 7.4, 150 mM NaCl, 7 mM MgCl2, 10 mM EGTA). 40 ul of serum from control or AAA patients, 50 ul of EDTA 0.2 M and 100 ul of VBS (NaCl 0.14 M, Sodium 5,5diethylbarbiturate 1.45 mM, acid 5,5-diethylbarbituric 2.5 mM) were added to 200 ul of rabbit RBCs 1% (v/v) and incubated at 37°C for 30 minutes. To calculate lysis, 1.8 ml of VBS-EDTA (VBS= and 0.2 M EDTA) were added, cells were pelleted by centrifugation at 2.500 rpm for 10 min and hemoglobin release was measured by absorbance at at 412 nm. Control incubations included 0% lysis (buffer only) and 100% lysis (1.8 ml of H2O instead of VBS= 0.2 M EDTA). Percentage lysis 100*(A412 test sample-A412 0% control)/(A412 100% control-A412 0% control). DNA isolation and genetic study Genomic DNA was extracted from peripheral blood using EZ1 DNA Blood 350 µl Kit in an EZ1 Advance Robot (Qiagen) following standard procedures. DNA samples were genotyped for six single nucleotide polymorphisms (SNPs) (CFH Ile62Val, CFH c.1696+2019G>A, CFHR1 Glu175Gln, CFB Leu9His, CFB Arg32Gln/Trp) (6). The genotyping was performed using multiplex PCR and minisequencing methodology (ABI Snapshot; Applied Biosystems). Minisequecing reations were run in an automated sequencer (model 3730; ABI), and the fragments were analyzed with the appropriate software (GeneMapper Software 4.0; ABI). Immunohistochemistry AAA and control aorta samples were fixed in 3.7% paraformaldehyde and embedded in paraffin. Immunohistochemistry was performed using antiC3 (purified as described in 7) and anti-C9 (mAb B7, a generous gift of Prof. Paul Morgan, Cardiff University) as primary antibodies. Negative controls using the corresponding IgG were included for checking non-specific staining. The secondary antibody and ABComplex/HRP were added and sections were stained with 3,30-diaminobenzidine and mounted in DPX. For colocalization of C3 with C9, CD15 (clone Carb-3, DAKO) and CD68 (clone PG-M1, DAKO), immunohistochemistry in serial sections was performed. For colocalization of C3 with vascular smooth muscle cells (alpha-actin, clone 1A4 DAKO), immunohistochemistry followed by immunofluorescence was performed. Western blot Equal amounts of proteins from tissue or conditioned medium (30 µg or 5 µL previously normalized to tissue weight: 1 g/6 mL, respectively) were loaded onto 12.5% polyacrylamide gels, electrophoresed and transferred to nitrocellulose membranes. Then they were blocked with 7% milk powder in TBS-T for 1 hour and incubated overnight at 4ºC with antiC3 (7). Then the membranes were washed with TBS-T and incubated with anti-rabbit antibody (1:5000) for 1 hour at RT. After 4 washes, the signal was detected using the ECL chemiluminiscence kit (GE Healthcare). Real time PCR Total RNA was isolated from cells using TRIzol reagent (Invitrogen). One microgram of RNA was used to perform the reverse transcription with the high capacity cDNA archive kit (Applied Biosystems). Real-time PCR reactions were performed on an ABI Prism 7500 sequence detection PCR system (Applied Biosystems) according to the manufacturer’s protocol, using the DDCt method. Human mRNA levels for C3 and 18S were done by amplification of cDNA using SYBRw Premix Ex TaqTM (Takara Biotechnology). The primer sequences are: Forward C3 primer: AAGCGCATTCCGATTGAGGA, Reverse C3 primer: AAGACTTCCCCACCAGGTCT. The mRNA levels of C3 were normalized to the 18S mRNA content. Cell isolation, chemotaxis assay and measurement of NADPH-dependent ROS production Neutrophils were isolated from venous blood of healthy volunteers (with informed consent), sampled on EDTA. Red blood cells were aggregated by addition of 2% dextran for 20 minutes at 20°C and the upper phase containing leukocytes was centrifuged on Ficoll (20 minutes at 600 g, 20°C) (PAA Laboratories GmbH). The pellet containing neutrophils was submitted to a hypo-osmotic shock to eliminate residual erythrocytes. Transwell migration assays were performed using 96-well disposable chemotaxis chambers with a 8 µm polycarbonate filter (ChemoTX, Neuroprobe). Briefly, 29 ul of 3 different luminal thrombus conditioned media were added to the lower compartment of each well. Luminal thrombus were preincubated for 30 min at 37ºC in a humidified atmosphere (5% CO2), in the presence or in the absence of antiC3 or IgG (0.4 ug/ul) in 30 µL of RPMI. Polymorphonuclear cells (200.000) were added to the upper compartment. The chamber was then incubated at 37 °C in a humidified atmosphere (5% CO2) for 2 h. A standard curve, consisting of a 1:2 dilution cascade of polymorphonuclear cells (top standard, 200.000 cells in 29 µL), was constructed. After incubation, the framed filter was carefully removed and the number of cells that had migrated was determined reading fluorescence at 485ex/530em by comparison with the standard curve. Each experiment was performed in triplicate. Lucigenin-enhanced chemiluminescence assay was used to determine the NADPHdependent ROS production in fresh neutrophils as described (8). Briefly, 5 µL of 3 different luminal thrombus conditioned media were incubated for 2 min with 500,000 polymorphonuclear cells. Luminal thrombus were preincubated for 30 min at 37ºC in a humidified atmosphere (5% CO2), in the presence or in the absence of antiC3 or IgG (0,4 ug/ul) in 30 µL of RPMI. The reaction mixture comprised 50 mM phosphate buffer containing 1mM EGTA, pH 7.0, 5 µM lucigenin and 0.1 mM NADPH. The chemiluminescence, which was measured for 5 minutes after the addition of NADPH, was recorded in a luminometer Sirius (Berthold Detection System). No activity could be measured in the absence of NADPH. The ROS production was determined from the ratio of relative light units. Statistics Normality of data was checked by probability plots. Normally distributed C3 concentrations and activity are expressed as mean±SEM. P < 0.05 was considered to be statistically significant. Difference among the groups in the first cohort (control, small aaa and large aaa) was analyzed by one-way ANOVA test followed by post hoc Tukey Kramer test for multiple comparisons. Differences among the groups of the second cohort and third cohort (small AAA vs large AAA) were analyzed by t-test. Pearson correlation was used to determine correlations between two variables. Logistic or linear regression analysis adjusted by risk factors was conducted with AAA stage (small/large AAA) and aortic size as dependent variables, respectively. The Wilcoxon paired test was used to analyze differences in C3 and C3a levels between thrombus and wall supernatants of the same samples, while non-paired tests were used for pathological wall vs healthy wall supernatants comparisons. All the statistical analyses were performed by using SPSS 11.0 statistical package. References 1 Grøndal N, Søgaard R, Henneberg EW, Lindholt JS.The Viborg Vascular (VIVA) screening trial of 65-74 year old men in the central region of Denmark: study protocol.Trials. 2010 May 27;11:67. 2 Caligiuri G, Rossignol P, Julia P, Groyer E, Mouradian D, Urbain D, Misra N, Ollivier V, Sapoval M, Boutouyrie P, Kaveri SV, Nicoletti A, Lafont A. Reduced immunoregulatory CD31+ T cells in patients with atherosclerotic abdominal aortic aneurysm. Arterioscler Thromb Vasc Biol. 2006;26:618-23. 3 Alcorlo M, Martínez-Barricarte R, Fernández FJ, Rodríguez-Gallego C, Round A, Vega MC, Harris CL., Rodríguez de Córdoba S and Llorca O. Unique structure of iC3b resolved at a resolution of 24 A by 3D-electron microscopy. Proc. Natl. Acad Sci USA. 2011;108:13236-40 4 Emanuelsson O, Brunak S, von Heijne G, Nielsen H. Locating proteins in the cell using TargetP, SignalP and related tools. Nat Protoc. 2007;2:953-71 5 Van Dijk H, Rademaker PM, Willers JM. Determination of alternative pathway of complement activity in mouse serum using rabbit erythrocytes. J Immunol Methods. 1980;36:29-39. 6 Harris CL, Heurich M, Cordoba SR, Morgan BP. The complotype: dictating risk for inflammation and infection.Trends Immunol. 2012;33:513-21. 7 Muñoz E, Vidarte L, Casado MT, Pastor C, Vivanco F. The C(H)1 domain of IgG is not essential for C3 covalent binding: importance of the other constant domains as targets for C3. Int Immunol. 1998;10:97-106. 8 Manea A, Tanase LI, Raicu M, Simionescu M. Transcriptional regulation of NADPH oxidase isoforms, Nox1 and Nox4, by nuclear factor-kappaB in human aortic smooth muscle cells. Biochem Biophys Res Commun 2010;396:901-907