Screening and Assessment Measures for Use in AF-CBT
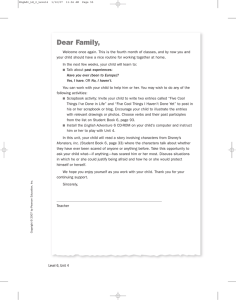
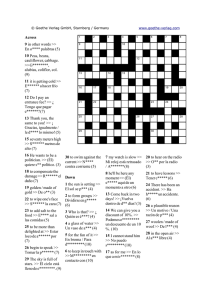
Anuncio
Screening and Assessment Measures for Use in AF-CBT (Version #7, 8-6-2015) David J. Kolko, Ph.D., ABPP, Elissa J. Brown, Ph.D. and Laurel Zelnik Note: We acknowledge the input from several colleagues in this document: Tracy Fehrenbach, Colleen Lang, Anna Loiterstein, Jennifer McQuaid, Komal Sharma-Patel, Kiara Porro, Kevin Rumbarger, Vanessa Rodriquez, Lisa Rosenfeld, and Carole Campbell Swiecicki. Table of Contents I. Purpose of Intake and Outcome Assessment in AF-CBT ................................................................................. 3 II. General Guidelines for Administration of Self-Report and Interview Measures ........................................... 3 III. Overview of Appropriate Assessment Targets/Measures in AF-CBT ............................................................ 5 IV. Screening Measures and Guidelines for Selecting Cases Appropriate for AF-CBT ....................................... 6 V. Information about Measures Recommended for Use in AF-CBT .................................................................. 6 Screen for AF-CBT Family Eligibility................................................................................................................. 7 General Guidelines for Identifying Appropriate Cases for AF-CBT ..................................................................8 Alabama Parenting Questionnaire ...................................................................................................................9 Background ........................................................................................................................................................ 9 Scoring................................................................................................................................................................ 9 Alabama Parenting Questionnaire – APQ (School Age Version)....................................................................10 Alabama Parenting Questionnaire – APQ (School Age Version – Español) ...................................................12 Brief Child Abuse Potential Inventory – B-CAP ..............................................................................................14 Background ...................................................................................................................................................... 14 Validity ............................................................................................................................................................. 14 Scoring.............................................................................................................................................................. 15 Brief CAP Inventory Form (B-CAP) .................................................................................................................16 Inventario del PAN (B-CAP) ............................................................................................................................18 Child PTSD Symptom Scale (CPSS) and Trauma Screen .................................................................................20 Background ...................................................................................................................................................... 20 1 Validity ............................................................................................................................................................. 20 Scoring.............................................................................................................................................................. 20 Trauma Screen ...............................................................................................................................................21 The Child PTSD Symptom Scale (CPSS) – Part I ..............................................................................................22 The Child PTSD Symptom Scale (CPSS) – Part II .............................................................................................23 Trauma Screen (Español) ..............................................................................................................................24 The Child PTSD Symptom Scale (CPSS) – Part I (Español) .............................................................................25 The Child PTSD Symptom Scale (CPSS) – Part II (Español) ............................................................................26 Strengths and Difficulties Questionnaire.................................................................................................27 Scoring.............................................................................................................................................................. 27 Strengths and Difficulties Questionnaire - SDQ .............................................................................................30 Strengths and Difficulties Questionnaire - SDQ .............................................................................................31 Cuestionario de Capacidades y Dificultades (SDQ-Cas) ................................................................................32 References .....................................................................................................................................................34 © 2012 Kolko & Brown 2 I. Purpose of Intake and Outcome Assessment in AF-CBT Assessment is an important part of good treatment. Therefore, we encourage practitioners who use AF-CBT to: (1) conduct an initial intake assessment that yields clinically-relevant information that can help to guide treatment, (2) collect ongoing information over the course of treatment designed to monitor treatment response on key clinical targets, and (3) conduct a discharge assessment using some of the assessment measures collected at intake to provide information about the impact of outcome of treatment. These three related functions are important to provide feedback about treatment needs, course/response, and outcome. What we mean by assessment is the collection of any referral record or report (e.g., CPS documents or caseworker reports, medical or health records) and other documents, formal standardized instruments, clinical interviews, and ongoing observations made to understand case needs/characteristics, clinical course and/or treatment outcome. Some assessments may be directed towards understanding individual characteristics; others may focus on family-system characteristics. Likewise, some information may reflect on specific topics related to verbal and physical aggression (e.g., harsh discipline, swearing, arguments) or PTSD-related symptoms, whereas other information may reflect more general topics or targets (e.g., social skills). It is important to consider all of these sources of potentially useful information in both selecting treatment components and in adapting treatment to the needs of the family. II. General Guidelines for Administration of Self-Report and Interview Measures The following are general guidelines for administration. It is helpful to identify an order for administration of any questionnaires or forms. Each questionnaire has slightly different rating scales and instructions for administration; yet, there are general instructions to keep in mind when administering questionnaires. Explain purpose of assessment and how information will be used (and who will have access to the results) • • • Purpose -- information needed to get your perspective on problems or issues for which you are here, guide treatment, identify your needs/goals, etc. Format/methods – we use existing forms that are designed to help us learn about different aspects of your life that may be relevant to our work here together, such as xx, yy, and zz (e.g., parenting practices, social behavior, and how things are at home) Who has access to the data – it’s for me, your clinician, etc.; won’t/will be shared with xx. Stays in our records and is confidential, etc. Setting the Environment • • • Place the measures on the table where the participant can follow as you read the items aloud. Have the visuals for each questionnaire available. Have stickers available for use as reinforcement as necessary (particularly with younger children). Instructions for the Administrator With Caregivers • Do your best to maintain a neutral, but friendly, disposition: read the items and record the answers without making too much eye contact in order to give the participant a sense of privacy when answering; try not to make reaffirming statements such as “good” or “everybody says that.” When praising or encouraging a respondent, compliment them on taking their time to think before answering. Ask if they understand the items. You might 3 • also want to remind caregivers that their input is important, as they are “the most important person” in their child’s life. It is preferred that the clinician read all the questions aloud to caregivers whose literacy is questionable. However, if an adult participant insists on completing a measure on his/her own, read 3-4 questions from each measure and the corresponding response options aloud first, and then allow the participant to finish each measure on his/her own. Ideally, the administrator will stay in the room with the caregiver, so that s/he is available to answer any questions. If the caregiver completes the measures themselves, make sure you skim each measure when the caregiver is finished, to assure that all questions were answered. With Children • Be creative, enthusiastic, and use variation in your rate and tone of speech to keep child’s attention. Use reinforcers, such as stickers, as needed to motivate the child to keep working. Offer children short breaks as needed, either for stretching, snacking, or use of the bathroom. If possible, avoid giving breaks in the middle of a measure. Use lots of praise but do not praise a specific type of answer. For example, if a child says “Yes, I like school” in response to a questions, avoid making judgments about the value of this response such as “that’s great” or “I bet you do.” Rather, periodically thank the child for his/her general behavior like taking his/her time, thinking before answering, asking for clarification, or working so hard. • Our default is to read all questions to child participants. Again, if an older child or adolescent conveys understanding of the measure and its scaling, read 3-4 questions and the corresponding response options aloud, and then allow the participant to finish the measure on his/her own. With Caregivers and Children • Always read the instructions printed on the questionnaire and review the response choices before beginning. Use the visuals and re-explain the answer choices as needed. • Avoid using the term “test” when administering the questionnaires. Rather, use the term survey or question pages, even if it says “test form” in the directions. • Read each response option (e.g., T/F, always/sometimes/never) for at least the first and second items. For the rest of the items, read response options after every few items. o If a subject responds to a question with an inappropriate response (e.g., saying “yes” to a T/F option), ask them to choose a specific option from the scale. • If the participant seems to be responding carelessly (i.e., yes to all questions, responding before the question is complete), encourage him/her to listen to the entire question and think for at least a couple of seconds before responding. • If a participant inquires about reasons for questionnaire administration, you can indicate that you are trying to learn more about him/her (e.g., “I’m trying to get to know you better”; “I want to know your point of view”). • If a “red flag” arises during administration of a questionnaire (e.g., self-harm, suicidal ideation or report of additional abuse experiences), stay with the protocol for administering assessments. The administration of the questionnaire packet should rarely be interrupted to address these issues. The administrator should follow the particular organization’s policy for handling the issues that come up. Trouble Shooting Misunderstanding questions • When a child is wavering in their answer, or if they want the question to be more specific, try not to “interpret” the question or the child’s response by way of comments, facial expression, or repeating previous responses. 4 • • Rather, encourage the child to be clear in their response by asking them to pick the best answer for them, even if making that decision is hard. Be careful when administering questions with a double negative. Help the child understand what the question is asking by rearranging the words in the question if necessary. Do not put the question into your own words. Rewording a question by changing the order of the words is okay. The next step would be to define a particular word or phrase in the sentence. Avoid interpreting the meaning of an entire question: o First, repeat the question. If the participant continues to look to you for guidance, restate the question again using the exact words from the item but stating them in a different order. Reframing a question should always be the last resort. Standardization of administration is extremely important. o If the participant does not understand the meaning of a particular word in the item, you may choose a simple synonym of the word to use in the question. o If the participant is not sure of the specific meaning of the question but generally understands, encourage him/her to answer the question the best as they can based on their understanding. Specifically, you can instruct the participant to “use your best guess.” o If it is clear that the participant has no understanding of the question, this must be noted on the questionnaire and the item may be skipped. III. Overview of Appropriate Assessment Targets/Measures in AF-CBT AF-CBT is recommended for cases with significant abusive/aggressive behavior in the caregiver, externalizing or aggressive behaviors in the child/adolescent, and/or heightened levels of conflict or coercion in the family. The latest version of AF-CBT can accommodate cases with or without post-traumatic stress (PTS) symptoms, which may help to address related trauma or violence-specific symptoms. Thus, the current version of AF-CBT is designed to be helpful with cases who present with any or all of the following characteristics: 1) Child exhibits significant EXT behavior (e.g., defiance, oppositionality, aggression, antisocial behavior); 2) Caregiver exhibits significant EXT behavior (verbal and physical aggression) and/or has allegation, or is at-risk for child physical abuse (e.g., limited positive and/or heightened negative parenting skills, anger arousal/hostility); or 3) Family has high level of conflict/coercion and may be at risk for physical aggression/abuse (e.g., frequent verbal and physical escalation; safety threats). As noted above, an important secondary target of AF-CBT includes child/adolescent trauma-related symptoms, notably, PTSD, depression, anxiety, and anger. We have identified assessment measures based on some general inclusion criteria that are used to identify appropriate candidates for AF-CBT. The recommended measures can be completed on paper, one-to-one or group administration, or via interview. They have good psychometric properties (i.e., reliability, validity), and have been used across a variety of trauma types, age ranges, settings, and cultures. Most also are available in the public domain (i.e., free of charge). We certainly recognize that many families referred for AF-CBT may present with problems or concerns in other areas which are relevant to clinical case conceptualization and which, to varying degrees, have been addressed in this treatment (e.g., limited readiness/willingness to change, child maladaptive attributions, such as self-blame; child social skills problems, caregiver’s inappropriate developmental expectations and views of child’s intentions). Further, other measures may be needed to assess changes in competencies or skills learned in each phase of AF-CBT. TF-CBT (Cohen et al., 2007) is generally regarded as the general treatment of choice for child/adolescent PTSD. So, we assume that most of the child/adolescent cases with primary PTSD (and in the absence of individual externalizing problems or family conflict/coercion) will get TF-CBT or similar interventions. Further, if there is serious caregiver 5 psychopathology (trauma history, PTSD, substance abuse, etc.) on top of the above, we would recommend MST-CAN (Swenson et al., 2010). IV. Screening Measures and Guidelines for Selecting Cases Appropriate for AF-CBT On the next pages you will find some materials designed to help you identify appropriate cases for AF-CBT. The first document is a measure that lists some of the eligibility criteria we use to determine if a case is appropriate for this treatment. The primary items look for caregiver physical abuse, high risk behavior, or physical discipline, family conflict, children externalizing behavior/aggression or trauma symptoms secondary to this caregiver/family history. This information can be obtained based on direct questions with a caregiver and/or based on a review of collateral informants or secondary materials/documents. The second document is an algorithm that outlines a pathway for understanding how to integrate the answers to these screening questions with other information about a case that might be used to support or contraindicate the use of AF-CBT in that case. We offer this algorithm as a general pathway to guide your decision-making about the appropriateness of the case for AF-CBT. It bears noting that the pathway is informed by both clinical and empirical considerations, but that it is not an empirically validated tool. In addition, we realize that there may be other important criteria that must be taken into consideration to ultimately decide which treatment a given family should and will get. V. Information about Measures Recommended for Use in AF-CBT Appended to the end of this file are several measures recommended for use in AF-CBT. We have chosen to include the Alabama Parenting Questionnaire (APQ), the Brief Child Abuse Potential Inventory (B-CAP), the Child PTSD Symptom Scale (CPSS), and the Strengths and Difficulties Questionnaire (SDQ). For each measure, we have included some background information, scoring guidelines, and a copy of the item content of each instrument in both English and Spanish. 6 Screen for AF-CBT Family Eligibility (v.6; 8.6.15) Name: Staff: Date: / / Sources of Info: Misc: Criteria for Eligibility: 1, 2, and 3 are “Yes,” plus any 4 or any 5 is a “Yes”. Yes 1. Child is age 5-17 No Unsure Yes No Yes No Yes No Yes No Unsure 4b. Caregiver has done something that resulted or could have resulted in an injury/harm to child Yes No Unsure 4c. Caregiver has likely used some type of excessive or harsh physical discipline with child Yes No Unsure 4d. Caregiver and child/family have conflicts and/or heated arguments, which may include caregiver verbal aggression/abuse Yes No Unsure 5a. Child has a pattern of exhibiting oppositional, argumentative, and/or explosive/angry behaviors Yes No Unsure 5b. Child has been verbally or physically aggressive, and/or exhibited other high-risk behaviors Yes No Unsure 5c. Child has trauma symptoms related to physical discipline or family conflict Yes No Unsure 5d. Child has a history of conflict, excessive or harsh physical discipline, or physical abuse or being injured by a caregiver. Yes No Unsure 2. A caregiver (biological, foster, or kinship) will participate in services 3. Child and caregiver appear appropriate for AF-CBT (i.e., they are willing, if they are separated, there is possibility of reunification; they are now or soon could be available, could participate adequately, and could benefit) 4a. Caregiver has an allegation or report of suspected physical abuse Comments: ________________________________________________________________________________________ 7 General Guidelines for Identifying Appropriate Cases for AF-CBT 8 Alabama Parenting Questionnaire One comprehensive measure that captures caregiver behavior and does not require a cost or any copyright restriction is the Alabama Parenting Questionnaire (APQ; Paul Frick, developer). We are suggesting that the APQ be used as a parent self-report and as a child report on the same parental practices. The 42 item scale includes six individual factors: Positive Parenting, Parental Involvement, Poor Parental Monitoring/Supervision, Inconsistent Discipline, Corporal Punishment, and Other Discipline. The items that load onto each scale are listed in the table below. On the next page is the proposed clinical cutoff for identifying families who could be considered as showing a “problem” on a given scale. For example, parents reporting a score that is less than or equal to 24 on the positive parenting practices scale can be considered as using too little positive parenting. We have included both the English and Spanish versions in the next few pages. Background Frick, P. J. (1991). Alabama parenting questionnaire. University of Alabama: Author Shelton, K. K., Frick, P. J., & Wootton, J. (1996). Assessment of parenting practices in families of elementary school-age children. Journal of Clinical Child Psychology, 25(3), 317-329 Elgar, F. J., Waschbusch, D. A., Dadds, M. R., & Sigvaldason, N. (2007). Development and validation of a short form of the alabama parenting questionnaire. Journal of Child and Family Studies, 16(2), 243-259. doi:10.1007/s10826-0069082-5 Scoring Scale 1 = Never 2 = Almost Never 3 = Sometimes 4 = Often 5 = Always Use the chart below to total up all the items for each individual factor. Clinical Cutoffs Chart Alabama Parenting Questionnaire (APQ) - Caregiver report Individual Factors Items (Sum) Positive Parenting Practices (2,5,13,16,18,27) Parental Involvement (1,4,7,9,11,14,15,20,23,26) Poor Parental Monitoring/Supervision (6,10,17,19,21,24,28, 29,30,32) Inconsistent Discipline (3,8,12,22,25,31) Corporal Punishment (33,35,38) Other Discipline (34,36,37,39,40, 41,42) 9 Problem Cutoff < 21 < 35 > 18 > 18 >7 n/a Alabama Parenting Questionnaire – APQ (School-age Version) Parent Form Parent Completing Form (Circle one): Mother Father Other: Instructions The following are a number of statements about your family. Please rate each item as to how often it TYPICALLY occurs in your home. The possible answers are (1)Never, (2) Almost Never, (3) Sometimes, (4) Often, and (5) Always. Please answer all items. 1. You have a friendly talk with your child. 2. You let your child know when he/she is doing a good job with something 3. You threaten to punish your child and then do not actually punish him/her 4. You volunteer to help with special activities that your child is involved in (such as sports, boy/girl scouts, church youth groups) 5. You reward or give something extra to your child for obeying you or behaving well 6. Your child fails to leave you a note or to let you know where he/she is going 7. You play games or do other fun things with your child 8. Your child talks you out of punishing him/her after he/she has done something wrong 9. You ask your child about his/her day at school 10. Your child stays out in the evening past the time he/she is supposed to be home 11. You help your child with his/her homework 12. You feel that getting your child to obey you is more trouble than it is worth 13. You compliment your child when he/she does something well 14. You ask your child what his/her plans are for the coming day 15. You drive your child to a special activity 16. You praise your child if he/she behaves well 17. Your child is out with friends you do not know 18. You hug or kiss your child when he/she has done something well 19. Your child goes out without a set time to be home Never 1 Almost Never Sometimes Often Always 2 3 4 5 1 2 3 4 5 1 2 3 4 5 1 2 3 4 5 1 2 3 4 5 1 2 3 4 5 1 2 3 4 5 1 2 3 4 5 1 2 3 4 5 1 2 3 4 5 1 2 3 4 5 1 2 3 4 5 1 1 1 1 1 1 1 2 2 2 2 2 2 2 3 3 3 3 3 3 3 4 4 4 4 4 4 4 5 5 5 5 5 5 5 20. You talk to your child about his/her friends 1 2 3 4 5 21. Your child is out after dark without an adult 1 2 3 4 5 10 Never Almost Never Sometimes Often Always 22. You let your child out of a punishment early (e.g., lift restrictions earlier than you originally said) 1 2 3 4 5 23. Your child helps plan family activities 1 2 3 4 5 24. You get so busy that you forget where your child is and what he/she is doing 1 2 3 4 5 25. Your child is not punished when he/she has done something wrong 1 2 3 4 5 26. You attend PTA meetings, parent/teacher conference, or other meetings at your child’s school 1 2 3 4 5 27. You tell your child that you like it when he/she helps out around the house 1 2 3 4 5 28. You don’t check that your child comes home at the time he/she is supposed to 1 2 3 4 5 29. You don’t tell your child where you are going 1 2 3 4 5 30. Your child comes home from school more than an hour past the time you expect him/her 1 2 3 4 5 31. The punishment you give your child depends on your mood 32. Your child is at home without adult supervision 1 1 2 2 3 3 4 4 5 5 33. You spank your child with your hand when he/she has done something wrong 1 2 3 4 5 1 1 2 2 3 3 4 4 5 5 1 2 3 4 5 1 2 3 4 5 38. You hit your child with a belt, switch, or other object when he/she has done something wrong. 1 2 3 4 5 39. You yell or scream at your child when he/she has done something wrong 1 2 3 4 5 40. You calmly explain to your child why his/her behavior was wrong when he/she misbehaves 1 2 3 4 5 41. You use time out (make him/her sit or stand in a corner) as a punishment 1 2 3 4 5 42. You give your child extra chores as a punishment 1 2 3 4 5 34. You ignore your child when he/she is misbehaving 35. You slap your child when he/she has done something wrong 36. You take away privileges or money from your child as a punishment 37. You send your child to his/her room as a punishment 11 Alabama Parenting Questionnaire - APQ (School-age Version – Español) Parent Form Nombre del nino/Codigo: Persona que RESPONDE: Fecha: Instrucciones Las siguientes afirmaciones se refieren a situaciones sobre su familia. Por favor, evalue cada item segun lo que ocurre habitualmente en su hogar. Las posibles respuestas son: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. Tiene charlas amistosas con su hijo Le hace saber a su hijo cuando está haciendo un buen trabajo Amenaza con castigar a su hijo y luego realmente no lo hace Ayuda a su hijo en actividades propias (actividades que le gustan) en las que participa Premia o da algo extra a su hijo cuando le obedece o se porta bien Su hijo no le deja notas ni le dice adónde va Juega o hace otras cosas divertidas con su hijo Su hijo le convence para que no lo castigue después de haberse portado mal Le pregunta a su hijo sobre cómo le ha ido el día en el colegio Su hijo sigue estando fuera por la tarde/noche pasada la hora en que se supone que debería estar en casa Ayuda a su hijo con sus deberes Siente que el hecho de conseguir que su hijo le obedezca le da tantos problemas que no le compensa Felicita a su hijo cuando hace algo bien Le pregunta a su hijo qué va a hacer durante el día Lleva a su hijo a sus actividades preferidas Alaba a su hijo cuando se porta bien Su hijo sale con amigos a los que usted no conoce Abraza o besa a su hijo cuando ha hecho algo bien Su hijo sale sin tener una hora límite para volver a casa Habla con su hijo sobre sus amigos Permite que su hijo pueda escaparse de un castigo enseguida Su hijo colabora en las decisiones familiares Está tan ocupado que olvida dónde está su hijo y qué está haciendo 12 Nunca 1 1 1 Casi Nunca 2 2 2 A A Veces Menudo Siempre 3 4 5 3 4 5 3 4 5 1 2 3 4 5 1 2 3 4 5 1 1 2 2 3 3 4 4 5 5 1 2 3 4 5 1 2 3 4 5 1 2 3 4 5 1 2 3 4 5 1 2 3 4 5 1 1 1 1 1 1 1 1 1 1 2 2 2 2 2 2 2 2 2 2 3 3 3 3 3 3 3 3 3 3 4 4 4 4 4 4 4 4 4 4 5 5 5 5 5 5 5 5 5 5 1 2 3 4 5 24. No castiga a su hijo cuando hace algo malo 25. Acude a las reuniones de los padres con los profesores o a otras reuniones de la escuela de su hijo 26. Le dice a su hijo que le gusta cuando colabora en casa 27. No controla que su hijo vuelva a casa a la hora que debería hacerlo 28. No le dice a su hijo adónde se va usted 29. Su hijo vuelve a casa después de la escuela una hora más tarde de lo esperado 30. El castigo que le da a su hijo depende de su estado de ánimo 31. Su hijo está en casa sin supervisión de ningún adulto 32. Pega a su hijo con la mano cuando ha hecho algo malo 33. Ignora a su hijo cuando se ha portado mal 34. Abofetea a su hijo cuando hace algo malo 35. Quita privilegios o dinero a su hijo como castigo 36. Envía a su hijo a su habitación como castigo 37. Golpea a su hijo con un cinturón u otro objeto cuando hace algo malo 38. Da voces o grita a su hijo cuando hace algo malo 39. Explica calmadamente a su hijo por qué su conducta fue errónea cuando se ha portado mal 40. Usa "tiempo fuera " como castigo (es decir, manda a su hijo a una habitación, un rincón o lo sienta en una silla para que se esté un tiempo como castigo) 41. Pone a su hijo tareas extra como castigo 13 Nunca 1 Casi Nunca 2 A A Veces Menudo Siempre 3 4 5 1 2 3 4 5 1 2 3 4 5 1 2 3 4 5 1 2 3 4 5 1 2 3 4 5 1 1 1 1 1 1 1 2 2 2 2 2 2 2 3 3 3 3 3 3 3 4 4 4 4 4 4 4 5 5 5 5 5 5 5 1 2 3 4 5 1 2 3 4 5 1 2 3 4 5 1 2 3 4 5 1 2 3 4 5 Brief Child Abuse Potential Inventory – B-CAP We also recommend administering to caregivers the Brief Child Abuse Potential Inventory (B-CAP; Ondersman et al., 2005), which is based on the full version of the Child Abuse Potential Inventory (Milner, 1986), because of its utility in helping to identify caregivers who may be at high risk for physical abuse or child maltreatment (heightened abuse potential). The B-CAP has 24 items that form 9 factors, two of which are used to determine validity (e.g., random responses and lying), and seven others which are used to capture overall abuse risk potential. One of these factors, the Family Conflict Scale, is included within the overall abuse risk and is also shown as a separate subscale in the table below due to its importance to AF-CBT. The clinical cutoff that reflects heightened risk potential based on a modest criterion is 9 (Ondersman et al., 2005). The next few pages contain the B-CAP in both English and Spanish. Background Ondersman, S. J., Chaffin, M., Simpson, S., & LeBreton, J. (2005). The Brief Child Abuse Potential inventory: Development and validation. Journal of Clinical Child and Adolescent Psychology, 34, 301-311. A brief version of the Child Abuse Potential Inventory (CAP) was developed using a development sample of N = 1470, and cross-validated using an additional sample of N = 713. Items were selected to maximize: (a) CAP variance accounted for; (b) prediction of future child protective services reports; (c) item invariance across gender, age, and ethnicity; (d) factor stability; and (e) readability and acceptability. On cross-validation, scores from the resulting 24-item risk scale demonstrated an internal consistency estimate of .89, a stable 7-factor structure, and substantial correlations with the CAP abuse risk score (r = .96). The CAP risk cut-off was predicted with 93% sensitivity and 93% specificity (area under the ROC curve = .98), and the BCAP and CAP demonstrated similar patterns of external correlates. The BCAP may be useful as a time-efficient screener for abuse risk. In the development study cited above, a B-CAP cutoff of 9 best predicted the risk distinction of the full CAP using the cutoff of 166, and a B-CAP cutoff of 12 best predicted the CAP cutoff of 215. These cutoffs were based on a particular sample of relatively high-risk parents, and may not represent the best possible cutoffs for use in other samples or for other settings. Validity The B-CAP contains two validity scales – the Random Response Scale and the Lie Scale. If any item on the Random Response Scale is not correctly endorsed (i.e. if they are endorsed as “agree” for normal scored items, or endorsed as “disagree” for reverse scored items) this indicates that the B-CAP may not be valid as respondents may simply be selecting random responses. If more than 4 items from the Lie Scale are endorsed as “disagree” this indicates that the B-CAP may not be valid as the respondents may not be accurately representing the information. 14 Scoring This chart demonstrates the scoring criteria for the B-CAP. Typically, items endorsed as “agree” should be given a score of 1. Items marked with a [*reverse score] should be reverse scored (any item endorsed as “disagree” should be given a score of 1). Please note, these item numbers refer to the item numbers on this Brief-CAP, and they do not correspond to the items on the original CAP. Individual Factors Validity Scales: Random Response Scale 2 (*reverse score), 18, 28 Lie Scale 4, 9, 15, 21, 26, 34 Content Scales: Abuse Risk Scale Family Conflict Scale Items (Sum) Sum all remaining items 1, 3, 5-8, 10-17, 19,-20, 22-25, 27, 29-33 (Note: Reverse score #1, 23, & 29) 6, 13, 17 Problem Cutoff Any item endorsed as “agree” (If any item endorsed, the information may be invalid) >4 items endorsed as “disagree” (Information may be invalid if >4 of these items is endorsed as such) >9 endorsed as “agree” except reverse scored items (High scores [>9] suggest greater risk for or likelihood of child maltreatment) >2 endorsed as “agree” (Moderate family conflict) 15 Brief CAP Inventory Form (B-CAP) Name: Age: Gender: Marital Status: Single Race: Black White Other (specify) Number of children in home Date: ID#: Male Female Married Separated Divorced Widowed Hispanic Am. Indian Highest Grade Completed Instructions The following questionnaire includes a series of statements which may be applied to yourself. Read each of the statements and determine if you AGREE or DISAGREE with the statement. If you do agree with a statement, mark the box in the agree column. If you disagree with a statement, mark the box in the disagree column. Be honest when giving your answers. Remember to read each statement; it is important not to skip any statement. Disagree 1. I am a happy person 2. I know what is the right and wrong way to act 3. People have caused me a lot of pain 4. I sometimes act without thinking 5. I am often lonely inside 6. My family fights a lot 7. Everything in a home should always be in its place 8. I often feel very upset 9. Sometimes I have bad thoughts 10. I sometimes worry that I will not have enough to eat 11. I am easily upset by my problems 12. Sometimes I feel all alone 13. My family has problems getting along 14. Children should never disobey 15. I sometimes lose my temper 16. I often feel worthless 17. My family has many problems 18. It is okay to let a child stay in dirty diapers for a while 19. I am often upset and do not know why 20. Children should be quiet and listen 21. I sometimes fail to keep all of my promises 22. I often feel very alone 23. My life is good 24. I am often upset 16 Agree Disagree Agree 25. Other people have made my life unhappy 26. I sometimes say bad words 27. I am often depressed 28. Children should not learn how to swim 29. My life is happy 30. I sometimes worry that my needs will not be met in the world 31. I often feel alone 32. A child needs very strict rules 33. Other people have made my life hard 34. People sometimes take advantage of me The CAP Inventory is copyrighted by Joel S. Miner. Ph.D. (1986). The subset of items contained in the B-CAP is being used with his permission by participants in an approved training program in AF-CBT. 17 Inventario del PAN (B-CAP) Nombre: Fecha: ID#: Edad: Sexo: Masculino Femenino Estado Civil: Soltero Casado Separado Divorciado Viudo Raza: Black White Hispanic Am. Indian Otro (specify) Numero de Hijos Ultimo año de studios terminado Instrucciones El siguiente cuestionario incluye una serie de declaraciones las cuales podrían ser aplicadas a Ud. mismo. Lea cada una de las declaraciones y determine si Ud. está de acuerdo o en desacuerdo con la declaración. Si Ud. está de acuerdo con una declaración, circule A para indicar acuerdo. Si Ud. está en desacuerdo con una declaración, circule DA para indicar desacuerdo. Recuerde leer cada declaración; es importante no omitir ninguna oración. A 1. Yo soy una persona feliz 2. Yo sé cual es la forma correcta e incorrect de actuar 3. La gente me ha causado mucho dolor 4. Yo algunas veces actύo sin pensar 5. Yo a menudo estoy solitario (a) adentro 6. Mi familia pelea mucho 7. Cada cosa en un hogar debería estar siempre en su lugar 8. Yo a menudo me siento muy turbado (a) 9. Algunas veces yo tengo malos pensamientos 10. Yo algunas veces me perocupo que me tender suficiente para comer 11. Yo soy fácilmente trastornado (a) por mis problemas 12. Algunas veces yo me siento completamente solo (a) en el mundo 13. Mi familia tiene problemas en llevársela bien 14. Los niños nunca deberían desobedecer 15. Yo algunas veces pierdo la paciencia 16. Yo a menudo siento que no valgo nada 17. Mi familia tiene muchos problemas 18. Está bien dejar a un niño con los pañales sucios por un rato 19. Yo estoy a menudo trastornada (o) y no sé por qué 20. Los niños deberían estar callados y escuchar 21. Yo fallo algunas veces en mantener todas mis promesas 22. Yo a menudo me siento muy solo (a) 23. Mi vida es Buena 18 DA A DA 24. Yo estoy a menudo turbado (a) 25. Otras personas han hecho mi vida infeliz 26. Yo algunas veces digo mala palabras 27. Yo estoy a menudo deprimido (a) 28. Los niños no deberían aprender a nadir 29. Mi vida es feliz 30. Yo algunas veces me preocupo que mis necesidades no serán satisfechas 31. Yo a menudo me siento solo (a) 32. Un niño necesita relas muy estrictas 33. Otras personas han hecho mi vida difícil 34. La gente algunas veces toma ventaja de mí The CAP Inventory is copyrighted by Joel S. Miner. Ph.D. (1986). The subset of items contained in the B-CAP is being used with his permission by participants in an approved training program in AF-CBT. 19 Child PTSD Symptom Scale (CPSS) and Trauma Screen We also recommend administering to children the Trauma Screen, a 15 item questionnaire designed to provide information on what specific events are underlying any PTSD symptoms the child is experiencing. There is also a four item part that assesses how the child felt while they were experiencing the traumatic event, which is taken from item A2 in the DSM IV; this is included to allow for diagnosis in addition to symptom severity. This scale was created by researchers at the University of Washington as a complement to the Child PTSD Symptom Scale. The Child PTSD Symptom Scale is a questionnaire designed to measure post traumatic stress disorder severity in children aged 8-18. The second part contains questions about daily functioning and is designed to measure severity of impairment. It is made up of 17 items in part 1 and 7 items in part 2. We suggest that the primary trauma from the Trauma Screen be used here. It takes about 20 minutes to administer as an interview measure and 10 minutes to complete as a self-report. The next few pages contain both the Trauma Screen and the CPSS in both English and Spanish. Background Foa, E. B., Johnson, K. M., Feeny, N. C., Treadwell, K. R. H. (2001). The Child PTSD Symptom Scale: A preliminary examination of its psychometric properties. Journal of linical Child Psychology, 30, 376–384. The Child PTSD Symptom Scale (CPSS) is a child version of the Foa et al. (1997) Posttraumatic Diagnostic Scale (PTDS) for adults. The CPSS maps on DSM-IV criteria, and yields a PTSD total score as well as scores on the re-experiencing, avoidance and hyperarousal subscales. The CPSS has 24-items, 17 of which correspond to the DSM-IV symptoms. In the first part of the questionnaire, respondents are asked to "fill in the number that best describes how often that problem has bothered [him/her] IN THE LAST TWO WEEKS." Answers are on a Likert-type scale. 0 is not at all, 1 is once a week or less/once in a while, 2 is 2 to 4 times a week/half the time, and 3 is 5 or more times a week/almost always. In the second part of the questionnaire, respondents are asked about functional impairment, or how much the problems indicated in section one have interfered with specific areas of life. These 7 questions are scored dichotomously as absent (0) or present (1). Scores range from 0 -- 7, with higher scores indicating greater functional impairment. Validity In the original article (Foa et al., 2001) internal consistency ranged from .70 - .89 for the total and symptom scores. Retest reliability was good to excellent (.84 for total, .85 for re-experiencing, .63 for avoidance, and .76 for hyperarousal). Convergent validity was high: the CPSS correlated .80 with the Child Posttraumatic Stress Reaction Index (Pynoos et al., 1986). A discriminant functional analysis indicated that a linear combination of the 3 subscales significantly discriminated between diagnostic groups (Wilks lambda = .33, X2 (3) = 79.1, p<.0001). The CPSS subscales correctly classified 94.7% of the cases. Scoring Each of the 17 items corresponding to the DSM-IV criteria is rated on a scale from 0 to 3; thus, the total score ranges from 0 to 51. While the original article found that a score of 11 was an appropriate clinical cutoff score, they also mentioned that clinical experience shows that a score of 15 is most appropriate in PTSD. We have chosen to use the higher cutoff value here (>15) because we want to ensure a clinically significant level of PTSD. 20 Trauma Screen Name: Date: Instructions Many children go through frightening or stressful events. Below is a listed of frightening or stressful events that can happen. Mark YES if you have experienced any of these events. Mark NO if you have not experienced these events. Yes No 1. A severe natural disaster such as a flood, tornado, hurricane, earthquake, or fire 2. Serious accident or injury caused by a car or bike crash, being bitten by a dog, or caused by playing sports 3. Being robbed by threat, force, or weapon 4. Being slapped, punished, or beaten by a relative 5. Being slapped, knifed, or beaten by a stranger 6. Seeing a relative get slapped, punished, or beaten 7. Seeing somebody in your community being slapped, punished, or beaten 8. Being touched in your sexual/private parts by an adult/someone older who should not be touching you there 9. Being forced/pressured to have sex at a time when you could not say no 10. A family member or somebody close dying suddenly or in a violent way 11. Being attacked, shot, stabbed, or seriously injured 12. Seeing someone be attacked, shot, stabbed, or seriously injured or killed 13. Having a stressful or frightening medical procedure 14. Being around a war 15. Any other stressful or frightening event Describe: ____________________________________________________ Which of these events bothers you most? ________________________________________________________________ If you answered NO to all of the above questions, stop. If you answered YES to any of the above questions, please answer the following questions. When the event happened, did you feel: Fear that you were going to die or be seriously injured? Fear that someone else was seriously hurt? Unable to help yourself? Shame or disgust? 21 Yes No The Child PTSD Symptom Scale (CPSS) – Part I Instructions Below is a list of problems that kids sometimes have after experiencing an upsetting event. Read each one carefully and circle the number (0-3) that best describes how often that problem has bothered you IN THE LAST 2 WEEKS. Please write down your most distressing event (this should be the event you listed in the Trauma Screen): Length of time since the event: 0 1 2 3 Not at all or only at one time Once a week or less/ once in a while 2 to 4 times a week/ half the time 5 or more times a week/almost always 1. Having upsetting thoughts or images about the event that came into your head when you didn’t want them to 0 1 2 3 2. Having bad dreams or nightmares 0 1 2 3 0 1 2 3 0 1 2 3 0 1 2 3 6. Trying not to think about, talk about, or have feelings about the event 0 1 2 3 7. Trying to avoid activities, people, or places that remind you of the traumatic event 0 1 2 3 8. Not being able to remember an important part of the upsetting event 0 1 2 3 9. Having much less interest or doing things you used to do 0 1 2 3 10. Not feeling close to people around you 0 1 2 3 11. Not being able to have strong feelings (for example, being unable to cry or unable to feel happy) 0 1 2 3 12. Feeling as if your future plans or hopes will not come true (for example, you will not have a job or getting married or having kids) 0 1 2 3 13. Having trouble falling asleep 0 1 2 3 14. Feeling irritable or having fits of anger 0 1 2 3 0 1 2 3 0 1 2 3 0 1 2 3 3. Acting or feeling as if the event was happening again (hearing something or seeing a picture about it and feeling as if you are there again) 4. Feeling upset when you think about it or hear about the event (for example, feeling scared, angry, sad, guilty, etc) 5. Having feelings in your body when you think about or hear about the event (for example, breaking out into a sweat, heart beating fast) 15. Having trouble concentrating (for example, losing track of a story on the television, forgetting what you read, not paying attention in class) 16. Being overly careful (for example, checking to see who is around you and what is around you) 17. Being jumpy or easily startled (for example, when someone walks up behind you) 22 The Child PTSD Symptom Scale (CPSS) – Part II Instructions Indicate below if the problems you rated in Part 1 have gotten in the way with any of the following areas of your life DURING THE PAST 2 WEEKS. Yes 1. Chores and duties at home 2. Relationships with friends 3. Fun and hobby activities 4. Schoolwork 5. Relationships with your family 6. General happiness with your life 23 No Trauma Screen (Español) Nombre: Fecha: Instrucciones Muchos niños pasan por eventos espantosos o estresantes. Abajo es una lista de eventos espantosos o estresantes que pueden suceder. Marca Si, si has vivido alguno de estos eventos. Marca No, si no has vivido alguno de estos eventos. Sí No 1. Desastre natural que fue grave, como un inundación, tornado, huracán, terremoto o incendio/lumbre 2. Accidente grave o herida seria casuado por un choque de autos o bicicletas, ser mordido por un perro, o herida causado por jugando un deporte 3. Ser robado con amenaza, fuerza o arma. 4. Cacheteado/a, puñeteado/a o golpeado/a por un familiar 5. Cacheteado/a, puñeteado/a o golpeado/a por alguien desconocido 6. Ver un familiar ser cacheteado/a o, puñeteado/a o golpeado/a. 7. Ver alguien en tu comunidad ser cacheteado/a o, puñeteado/a o golpeado/a. 8. Ser tocado por un adulto o alguien mayor en tus partes sexuales/ privadas cuando no debieron 9. Ser forzado/a o presionado/a en tener sexo o en un tiempo en cuando no pudiste decir no 10. Un familiar o persona cercana moriendose de repente o de una manera violenta 11. Ser atacado, cucheteado, disparado o lastimado gravemente 12. Ver alguien ser atacado, cucheteado, disparado, lastimado gravemente, o matado 13. Procedimiento médico estresante o atemorizante 14. Estar al rededor de una guerra 15. Algun otro evento estresante o espantoso Describa: ____________________________________________________ Cual de los eventos te molesta mas? ____________________________________________________________________ Si es que contestaste NO a las preguntas arriba, PARA. Si es que contestaste SÍ para alguna de las preguntas arriba, porfavor contesta las siguientes preguntas. En cuando sucedio el evento, que sentiste? Miedo que me iba morir o que fuera gravemente herido Miedo que alguien mas moriera o fuera lastimado Sin poder ayudarme a mi mismo/a Verguenza o asco 24 Sí No The Child PTSD Symptom Scale (CPSS) – Part I (Español) Instrucciones Marca 0, 1, 2 o 3 para indicar con frecuencia has tenido los siguientes problemas en los ultimos dos semanas. Please write down your most distressing event (this should be the event you listed in the Trauma Screen): Length of time since the event: 0 Nunca 1 De vez en cuando 2 La mitad del tiempo 3 Casi siempre 1. Has tenido pensamientos o imagenes molestos sobre el evento aunque tu no querias pensar en eso 0 1 2 3 2. Has tenido sueños malos o pesadillas 0 1 2 3 0 1 2 3 0 1 2 3 0 1 2 3 6. Has tratado de no pensar, hablar, o de tener sentimientos acerca del evento 0 1 2 3 7. Has tratado de evitar actividades, personas, o lugares que te hacen recorder el evento traumatic (por ejemplo, no querer jugar afuera o ir a la escuela) 0 1 2 3 8. Has tenido dificultad en recorder una parte importante del evento 0 1 2 3 9. Has tenido mucho menos intéres o no has hecho las cosas que acostumbrabas hacer 0 1 2 3 10. Has tenido mucho menos intéres o no has hecho las cosas que acostumbrabas hacer. 0 1 2 3 11. Has tenido dificultad en en tener sentimientos Fuertes (por ejemplo, no poder llorar o sentirte muy feliz) 0 1 2 3 12. Has sentido como sit us planes del future o tus esperanzas no se harán realidad 0 1 2 3 13. Has tenido dificultad en quedarte o mantenerte dormido(a) 0 1 2 3 14. Te has sentido irritable o has tenido momentos de enojo 0 1 2 3 15. Has tenido dificultad en concentrarte 0 1 2 3 16. Has estado demasiado cuidadoso(a) y atento(a) 0 1 2 3 17. Te has asustado o te has sorprendido facilmente 0 1 2 3 3. Has actuado o has sentido como si el evento estuviera pasando de Nuevo (has escuchado algo o visto algo que te recuerda del evento y te has sentido como si estuviera pasando otra vez) 4. Te has sentido mal cuando piensas o escuchas algo sobre el evento (por ejemplo: sintiéndote asustado(a), enojado(a), triste o culpable) 5. Has tenido sensaciones en tu cuerpo cuando piensas o escuchas algo acerca del evento (por ejemplo: sudando de repente, el corazón palpitando rápido) 25 The Child PTSD Symptom Scale (CPSS) – Part II (Español) Instrucciones Ahora dí si los problemas que acabas de mencionar en la Parte 1 te han molestado conlas siguientes cosas. Marque Sí o No. Sí 1. Que haceres y obligaciones en casa 2. Con tus amistades 3. En hacer cosas divertidas 4. En hacer tu tarea 5. Llevarte bien con tu familia 6. Ser feliz con tu vida 26 No Strengths and Difficulties Questionnaire One comprehensive measure that captures child externalizing behavior (e.g., ODD/CD, aggression), as well as other relevant child problems, and that does not require a cost for use of a hard copy form is the Strengths and Difficulties Questionnaire (SDQ; Robert Goodman). The SDQ is 25-item clinical rating scale, completed by caregivers on 3-16 year olds. The subscales include: Total Difficulties, Emotional symptoms, Conduct problems, Hyperactivity, Peer problems, and Prosocial Behavior. There is one measure for children ages 4-10 and another measure for youth ages 11-17 for the English version; the Spanish version is for all ages (4-17). Both the English and Spanish versions are included. Scoring Scoring the Informant-Rated Strengths and Difficulties Questionnaire The 25 items in the SDQ comprise 5 scales of 5 items each. It is usually easiest to score all 5 scales first before working out the total difficulties score. ‘Somewhat True’ is always scored as 1, but the scoring of ‘Not True’ and ‘Certainly True” varies with the item, as shown below scale by scale. For each of the 5 scales, the score can range from 0 to 10 if all 5 items were completed. Scale score can be prorated if at least 3 items were completed. Not True Somewhat True Certainly True Often complains of headaches, stomach-aches… 0 1 2 Many worries, often seems worried 0 1 2 Often unhappy, downhearted or tearful 0 1 2 Nervous or clingy in new situations… 0 1 2 Many fears, easily scared 0 1 2 Conduct Problems Scale Not True Somewhat True Certainly True Often has temper tantrums or hot tempers 0 1 2 Generally obedient, usually does what… 2 1 0 Often fights with other children or bullies them 0 1 2 Often lies or cheats 0 1 2 Steals from home, school or elsewhere 0 1 2 Emotional Symptoms Scale 27 Not True Somewhat True Certainly True Restless, overactive, cannot stay still for long 0 1 2 Constantly fidgeting or squirming 0 1 2 Easily distracted, concentration wanders 0 1 2 Thinks things out before acting 2 1 0 Sees tasks through to the end, good attention span 2 1 0 Not True Somewhat True Certainly True Rather solitary, tends to play alone 0 1 2 Has at least one good friend 2 1 0 Generally liked by other children 2 1 0 Picked on or bullied by other children 0 1 2 Gets on better with adults than with other children 0 1 2 Not True Somewhat True Certainly True Considerate of other people’s feelings 0 1 2 Shares readily with other children 0 1 2 Helpful if someone is hurt, upset or feeling ill 0 1 2 Kind to younger children 0 1 2 Often volunteer to help others 0 1 2 Hyperactivity Scale Peer Problems Scale Prosocial Scale The Total Difficulties Score is generated by summing the scores from all the scales except the prosocial scale.The resultant scores can range from 0 to 40 (and is counted as missing if one of the component scores is missing). Interpreting Symptom Scores and Defining “Caseness” from Symptom Scores Although SDQ scores can often be used as continuous variables, it is sometimes convenient to classify scores as normal, borderline and abnormal. Using the banding in the table shown below, an abnormal score on one or both of the total difficulties scores can be used to identify likely “cases” with mental health disorders. This method is helpful in detecting mental health problems, and is best when combined with information gathered from multiple informants. It does, however, overestimate difficulties. Approximately 10% of a community sample will score in the abnormal band on any given score, and a further 10% will score in the borderline range. The exact proportions vary by country, age and gender (see SDQ website for normative data). You may want to set the threshold higher when avoiding false positives is important, and set the threshold lower when avoiding false negatives is more important. 28 Strengths and Difficulties Questionnaire (SQD) -- Caregiver Report Clinical Cutoff Category Scale Normal Borderline Total Difficulties Score 0-13 14-16 Emotional Symptoms Score 0-3 4 Conduct Problems Score 0-2 3 Hyperactivity Score 0-5 6 Peer Problems Score 0-2 3 Prosocial Behavior Score 6-10 5 Abnormal 17-40 5-10 4-10 7-10 4-10 0-4 Strengths and Difficulties Questionnaire (SQD) -- Teacher Report Clinical Cutoff Category Scale Normal Borderline Total Difficulties Score 0-11 12-15 Emotional Symptoms Score 0-4 5 Conduct Problems Score 0-2 3 Hyperactivity Score 0-5 6 Peer Problems Score 0-3 4 Prosocial Behavior Score 6-10 5 Abnormal 16-40 6-10 4-10 7-10 5-10 0-4 29 Strengths and Difficulties Questionnaire - SDQ P or T 4-10 Instructions For each item, please mark the box for Not True, Somewhat True or Certainly True. It would help us if you answered all items as best you can even if you are not absolutely certain. Please give your answers on the basis of your child’s behavior over the last six months. Thank you very much for your help. Not True 1. Considerate of other people’s feelings 2. Restless, overactive, cannot stay still for long 3. Often complains of headaches, stomach-aches, or sickness 4. Shares readily with other young people, for example toys, treats, pencils 5. Often loses temper 6. Rather solitary, prefers to play alone 7. Generally well behaved, usually does what adults request 8. Many worries or often seems worried 9. Helpful if someone is hurt, upset or feeling ill Somewhat Certainly True True 10. Constantly fidgeting or squirming 11. Has at least one good friend 12. Often fights with other children or bullies them 13. Often unhappy, depressed or tearful 14. Generally liked by other children 15. Easily distracted, concentration wanders 16. Nervous in new situations, easily loses confidence 17. Kind to younger children 18. Often lies or cheats 19. Picked on or bullied by other children 20. Often volunteers to help others (parents, teachers, other children) 21. Thinks things out before acting 22. Steals from home, school or elsewhere 23. Gets along better with adults than with other children 24. Many fears, easily scared 25. Good attention span, sees work through to the end Signature_____________________________________________________________________ Date_______________ Parent/Teacher/Other (please specify):__________________________________________________________________ 30 Strengths and Difficulties Questionnaire - SDQ P or T 11-17 Instructions For each item, please mark the box for Not True, Somewhat True or Certainly True. It would help us if you answered all items as best you can even if you are not absolutely certain. Please give your answers on the basis of your child’s behavior over the last six months. Thank you very much for your help. Not True 1. Considerate of other people’s feelings 2. Restless, overactive, cannot stay still for long 3. Often complains of headaches, stomach-aches, or sickness 4. Shares readily with other young people, for example CDs, games, food 5. Often loses temper 6. Would rather be alone than with other young people 7. Generally well behaved, usually does what adults request 8. Many worries or often seems worried 9. Helpful if someone is hurt, upset or feeling ill Somewhat Certainly True True 10. Constantly fidgeting or squirming 11. Has at least one good friend 12. Often fights with other young people or bullies them 13. Often unhappy, depressed or tearful 14. Generally liked by other young people 15. Easily distracted, concentration wanders 16. Nervous in new situations, easily loses confidence 17. Kind to younger children 18. Often lies or cheats 19. Picked on or bullied by other young people 20. Often volunteers to help others (parents, teachers, children) 21. Thinks things out before acting 22. Steals from home, school or elsewhere 23. Gets along better with adults than with other young people 24. Many fears, easily scared 25. Good attention span, sees chores or homework through to the end Signature_____________________________________________________________________ Date_______________ Parent/Teacher/Other (please specify):__________________________________________________________________ 31 Cuestionario de Capacidades y Dificultades (SDQ-Cas) P or T 4-16 Instrucciones Por favor, ponga una cruz en el cuadro que usted cree que corresponde a cada una de las preguntas: No es cierto, Un tanto cierto, Absolutamente cierto. Nos sería de gran ayuda si respondiese a todas las preguntas lo major que pudiera, aunque no esté completamente seguro/a de la respuesta, o le parezca una pregunta rara. Por favor, responda a las preguntas basándose en el comportamiento del niño/a durante los ύltimos seis meses o durante el presente curso escolar. Muchas gracias por su ayuda. No es cierto 1. Tiene en cuenta los sentimientos de otras personas 2. Es inquieto/a, hiperactivo/a, no puede permanecer quieto/a por mucho tiempo 3. Se queja con frecuencia de dolor de cabeza, de estómago o de náuseas 4. Comparte frecuentemente con otros niños/as chucherías, juguetes, lápices, etc 5. Frecuentemente tiene rabietas o mal genio 6. Es más bien solitario/a y tiende a jugar solo/a 7. Por lo general es obediente, suele hacer lo que le piden los adultos 8. Tiene muchas preocupaciones, a menudo parece inquieto/a o preocupado/a 9. Ofrece ayuda cuando alguien resulta herido, disgustado, o enfermo 10. Está continuamente moviéndose y es revoltoso 11. Tiene por lo menos un/a buen/a amigo/a 12. Pelea con frecuencia con otros niños/as o se mete con ellos/ellas 13. Se siente a menudo infeliz, desanimado o lloroso 14. Por lo general cae bien a los otros niños/as 15. Se distrae con facilidad, su concentración tiende a dispersarse 16. Es nervioso/a o dependiente ante nuevas situaciones, fácilamente pierde la confianza en sí mismo/a 17. Trata bien a los niños/as más pequeños/as 18. A menudo miente o engaña 19. Los otros niños se meten con él/ella o se burlan de él/ella 20. A menudo se ofrece para ayudar (a padres, maestros, otros niños) 21. Piensa las cosas antes de hacerlas 22. Roba cosas en casa, en la escula o en otros sitios 32 Un tanto Absolutacierto mente cierto No es cierto Un tanto Absolutacierto mente cierto 23. Se lleva major con adultos que con otros niños/as 24. Tiene muchos miedos, se asusta fácilamente 25. Termina lo que empieza, tiene Buena concentracíon Firma_____________________________________________________________________ Fecha_________________ Madre/padre/maestro/otros (indique, por favor:) _________________________________________________________ 33 References Cohen, J. A., Mannarino, A. P., Perel, J. M., & Staron, V. (2007). A Pilot Randomized Controlled Trial of Combined TraumaFocused CBT and Sertraline for Childhood PTSD Symptoms. Journal of the American Academy of Child & Adolescent Psychiatry, 47(7), 811-819. Elgar, F. J., Waschbusch, D. A., Dadds, M. R., & Sigvaldason, N. (2007). Development and validation of a short form of the alabama parenting questionnaire. Journal of Child and Family Studies, 16(2), 243-259. doi:10.1007/s10826-0069082-5 Foa, E. B., Cashman, L., Jaycox, L., & Perry, K. (1997). The Validation of a Self-Report Measure of Posttraumatic Stress Disorder: The Posttraumatic Diagnostic Scale. Psychological Assessment, 9(4), 445-451. Foa, E. B., Johnson, K. M., Feeny, N. C., & Treadwell K. R. H. (2001). The Child PTSD Symptom Scale: A preliminary examination of its psychometric properties. Journal of Clinical Child & Adolescent Psychology, 30(3), 376-384. Frick, P. J. (1991). Alabama parenting questionnaire. University of Alabama: Author Goodman, R., Meltzer, H., Bailey, V. (1998). The strengths and difficulties questionnaire: A pilot study on the validity of the self-report version. European Child & Adolescent Psychiatry, 7(3), 125-130. Milner, J. S., & Ayoub, C. (1980) Evaluation of “At Risk” parents using the child abuse potential inventory. Journal of Clinical Psychology, 36(4), 945-948. Milner, J. S. (1986).The Child Abuse Potential Inventory: Manual (Second edition), Psytec Corporation, Webster, N.C. Ondersman, S. J., Chaffin, M., Simpson, S., & LeBreton, J. (2005). The Brief Child Abuse Potential Inventory: Development and validation. Journal of Clinical Child and Adolescent Psychology,34, 301-311. Pynoos,R. S. & Em, S. (1986) Witness to violence: the child interview. Journal of the American Academy of Child Psychiatry, 25, 306-319. Shelton, K. K., Frick, P. J., & Wootton, J. (1996). Assessment of parenting practices in families of elementary school-age children. Journal of Clinical Child Psychology, 25(3), 317-329 Swenson, C. C., Schaeffer, C. M., Henggeler, S. W., Faldowski, R., & Mayhew, A. M. (2010). Multisystemic therapy for child abuse and neglect: A randomized effectiveness trial. Journal of Family Psychology, 24(4), 497-507. 34