Stem Cell Transplants - MD Anderson Cancer Center
Anuncio
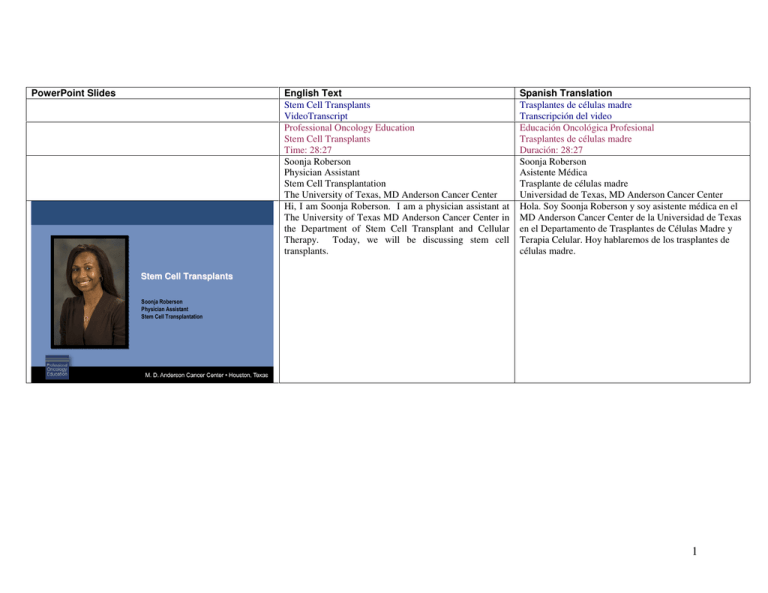
PowerPoint Slides Stem Cell Transplants English Text Stem Cell Transplants VideoTranscript Professional Oncology Education Stem Cell Transplants Time: 28:27 Soonja Roberson Physician Assistant Stem Cell Transplantation The University of Texas, MD Anderson Cancer Center Hi, I am Soonja Roberson. I am a physician assistant at The University of Texas MD Anderson Cancer Center in the Department of Stem Cell Transplant and Cellular Therapy. Today, we will be discussing stem cell transplants. Spanish Translation Trasplantes de células madre Transcripción del video Educación Oncológica Profesional Trasplantes de células madre Duración: 28:27 Soonja Roberson Asistente Médica Trasplante de células madre Universidad de Texas, MD Anderson Cancer Center Hola. Soy Soonja Roberson y soy asistente médica en el MD Anderson Cancer Center de la Universidad de Texas en el Departamento de Trasplantes de Células Madre y Terapia Celular. Hoy hablaremos de los trasplantes de células madre. Stem Cell Transplants Soonja Roberson Physician Assistant Stem Cell Transplantation 1 Stem Cell Transplants Objectives • Upon completion of this lesson, participants will be able to: Upon completion of this lesson, participants will be able to: describe the purpose and methods of stem cell transplant; define HLA typing and identify the differences between various kinds of matches; identify possible complications of stem cell transplant. Al finalizar esta lección, los participantes podrán describir el propósito y los métodos de trasplante de células madre, definir la tipificación de HLA e identificar diferencias entre distintos tipos de compatibilidad y posibles complicaciones del trasplante. Hematopoietic stem cells are progenitor cells found in the bone marrow. They have capacity for self-renewal and the ability to proliferate and differentiate. These cells are denoted by flow cytometry, by cell surface marker known as CD34. Las células madre hematopoyéticas son células progenitoras de la médula ósea con capacidad de autorrenovarse, proliferar y diferenciarse. En la citometría de flujo se indican con el marcador de superficie celular CD34. – Describe the purpose and methods of stem cell transplant – Define HLA typing and identify the differences between various kinds of matches – Identify possible complications of stem cell transplant Stem Cell Transplants Hematopoietic Stem Cells • Progenitor cells found in the bone marrow – Capacity for self renewal – Ability to proliferate and differentiate • Denoted by flow cytometry by cell surface marker CD34 2 Stem Cell Transplants Stem Cell Transplants Benefits of Stem Cell Transplant • Ability to give higher doses of chemotherapy • Capable of transferring immune competent cells (graft) from a normal donor to an immune incompetent recipient (host) via peripheral blood or marrow This is a diagram of normal hematopoiesis. At the top, you will see a pluripotent stem cell has the ability for self-renewal and the ability to differentiate into both myeloid and lymphoid cell lines. The myeloid phenotype will give rise to red blood cells, platelets, macrophages, eosinophils, basophils, and neutrophils. The lymphoid cell line will give rise to T-cell lymphocytes and B-cell lymphocytes that are responsible for antibody production. En este diagrama de la hematopoyesis normal, la parte superior muestra una célula madre pluripotente con capacidad de autorrenovación y diferenciación de linaje mieloide y linfoide. El fenotipo mieloide produce glóbulos rojos, plaquetas, macrófagos, eosinófilos, basófilos y neutrófilos. El linaje linfoide genera linfocitos de células T y B, responsables de producir anticuerpos. There are many benefits to stem cell transplant. They give you the ability to give high doses of chemotherapy. You also can transfer immune competent cells known as the graft from a normal donor to an immune incompetent recipient known as the host via peripheral blood or bone marrow. Stem cell transplant relies heavily on a donor’s immune system to produce a heavy graft versus tumor effect rather than relying solely on chemotherapy alone. El trasplante de células madre ofrece muchos beneficios, como administrar altas dosis de quimioterapia y transferir células inmunocompetentes o injertos de un donante sano a un destinatario inmunitario incompetente o huésped, utilizando sangre periférica o médula ósea. Este trasplante depende en gran medida de que el efecto del injerto en el sistema inmunológico del donante predomine sobre el tumor, sin depender sólo de la quimioterapia. • Relies heavily on donor’s immune system to produce graft versus tumor effect rather than chemotherapy alone 3 Stem Cell Transplants Types of Transplants • Autologous – recipient's own stem cells – – – – Lower incidence of treatment-related mortality Can be performed in older patients Higher risk of relapse Relatively low rate of long-term complications • Allogeneic – donor derived stem cells – Higher treatment-related mortality – Lower risk of relapse – Higher rate of short and long-term complications There are several types of transplants. The first is autologous, in which the recipient’s own stem cells are used. In this type of setting, there is a lower incidence of treatment-related mortality. Therefore, this treatment can be given in patients of older age. However, the downside is there is a higher risk of relapse and a relatively low rate of long-term complications. In the allogeneic setting, you use donor-derived stem cells. In this setting, there is a higher rate of treatment-related mortality; however, a lower risk of relapse and a higher rate of short and longterm complications. More commonly now is umbilical cord blood, which is also easily accessible, but has the potential of causing more infectious complications. Hay varios tipos de trasplantes. Uno es el autólogo, que utiliza las propias células del receptor y tiene una menor incidencia de mortalidad relacionada con el tratamiento. Por ello, puede usarse en pacientes de edad avanzada. Su desventaja es un mayor riesgo de recurrencia, pero tiene una tasa relativamente baja de complicaciones a largo plazo. El trasplante alogénico usa células madre derivadas de donantes. Tiene una mayor tasa de mortalidad relacionada con el tratamiento, menor riesgo de recurrencia y mayor tasa de complicaciones a corto y a largo plazo. Actualmente, se utiliza mucho la sangre del cordón umbilical, fácilmente accesible pero con más complicaciones infecciosas. The timing of transplant is very critical. Transplant must be done at the maximal tumor response. Hence, patients should either be in a complete remission or a very good partial remission, which means greater than 50% decrease in disease burden. The patient can have no active infections at the time of transplant, no evidence of CNS or leptomeningeal disease, no uncontrolled chronic illnesses. They must have adequate organ function. They must have an adequate performance status, meaning they must be able to perform activities of daily living without significant side effects. And you must have an identified donor in the allogeneic setting, and be able to collect an adequate number of stem cells. El momento del trasplante es crítico, pues debe hacerse con máxima respuesta tumoral. Los pacientes deben estar en remisión completa o parcial buena, con más del 50% de disminución de la carga de la enfermedad. En el momento del trasplante, el paciente no puede tener infecciones activas ni evidencia de enfermedad leptomeníngea o del sistema nervioso central, ni enfermedades crónicas no controladas. Debe tener una función orgánica y un estado funcional adecuados, y ser capaz de realizar actividades de la vida diaria sin mayores efectos secundarios. En el contexto alogénico, el donante debe estar identificado y recolectarse una cantidad suficiente de células madre. • Umbilical cord blood – Easily accessible – More infectious complications Stem Cell Transplants Timing of Transplant • Maximal tumor response (complete vs. partial remission) • No active infections • No active CNS or leptomeningeal disease • No uncontrolled chronic illnesses • Adequate organ function • Adequate performance status • Identified donor (allogeneic only) • Adequate stem cell collection 4 Stem Cell Transplants Indications for Transplant • High risk leukemias – – – – – • • • • • Induction failures Poor risk cytogenetics Relapsed disease Therapy related MDS or AML ALL – MLL gene, Philadelphia chromosome Tyrosine-kinase resistant CML or blast crisis Refractory CLL or transformed large cell lymphomas Relapsed or refractory Hodgkin’s lymphoma Relapsed non-Hodgkin’s lymphoma Chemo-sensitive multiple myeloma Stem Cell Transplants Preparation for Transplant • Chemotherapy preparative regimen – Ablative • • • • Myeloid/lymphoid malignancies Younger/healthier Highly immunosuppressive More risk of toxicity/less risk of relapse – Reduced intensity or non-myelobalative • • • • • Lymphomas/myelomas/leukemia Heavily pretreated or prior transplant Older Immunosuppressive Less toxicity/potential increased risk of rejection There are many indications for stem cell transplant. Most commonly transplants are done for patients with high-risk leukemias. In that setting, those patients either have induction failure, or who have poor risk cytogenetics, who have relapsed disease after standard chemotherapy, or who have treatment-related myelodysplastic syndrome, or AML, or who have high-risk ALL, meaning they have the MLL gene mutation or Philadelphia chromosome by molecular or FISH testing. In addition, patients with tyrosine-kinase resistant CML or blast crisis, refractory CLL or transformed large B-cell lymphoma, refractory or relapsed Hodgkin's lymphoma, relapsed Hodgkin’s lymphoma, and chemosensitive multiple myeloma. Hay muchas indicaciones para los trasplantes de células madre. Las más comunes son leucemias de alto riesgo en pacientes con insuficiencia inductiva, escaso riesgo citogenético, recurrencia luego de quimioterapia estándar, síndrome mielodisplásico relacionado con el tratamiento, leucemia mieoloide aguda, riesgo por mutación del gen de leucemia de linaje mixto, o cromosoma Filadelfia por análisis molecular o hibridación fluorescente in situ. Se recomienda para la leucemia mieloide crónica resistente a la tirosina quinasa o crisis blástica, el carcinoma pulmonar de Lewis resistente, el linfoma de células B grandes transformado, el linfoma de Hodgkin resistente o recurrente, y el mieloma múltiple quimiosensible. There are several types of preparative regimens for indication for transplant. This means the chemotherapy that the patient is receiving prior to their stem cell collection. The chemotherapy preparative regimen can either be ablative or reduced intensity or nonmyeloablative. Ablative means that the bone marrow is completely ablated by the chemotherapy. This is typically used in myeloid and lymphoid malignancies and is reserved for younger and healthier patients because the treatment is much stronger. The therapy is very highly immunosuppressive. Therefore, there is more risk of toxicity, but, hence, less risk of relapse. In the reduced intensity setting, this is typically reserved for patients with lymphomas, myelomas in older patients with leukemia. Most of these patients are heavily pre-treated or have had a prior transplant. Most of these patients are also older. However, reduced intensity also causes some immunosuppression. There is, however, less toxicity, again because the therapy is less high dose and because the therapy is less high dose there is a potential risk of rejection. Para el trasplante, hay varios regímenes de preparación, es decir, la quimioterapia que recibe el paciente antes de la recolección. El régimen de preparación de quimioterapia puede ser ablativo, de intensidad reducida o no mieloablativo. “Ablativo” significa que la médula ósea es completamente anulada por la quimioterapia. Este tratamiento suele usarse en neoplasias linfoides y mieloides, y se reserva para pacientes más jóvenes y saludables, ya que es más intenso. La terapia es altamente inmunosupresora, con un mayor riesgo de toxicidad y menor riesgo de recurrencia. El tratamiento de intensidad reducida es para linfomas o mielomas en pacientes mayores con leucemia. Casi todos ya habrán sido extensamente tratados y habrán recibido un trasplante previo, y tendrán mayor edad. La intensidad reducida también causa cierta inmunosupresión; no obstante, hay menos toxicidad porque la terapia no es a dosis tan altas y por eso existe un riesgo de rechazo. 5 Let’s first discuss autologous transplant in detail. Primero describiremos el trasplante autólogo. In the autologous setting, we use the patient’s own stem cells. This can be collected either via peripheral blood or bone marrow stem cells collected prior to the high-dose chemotherapy that will be given. This type of treatment is indicated in chemosensitive, recurrent Hodgkin’s lymphoma, chemosensitive, low-grade, or intermediate grade lymphomas, and multiple myeloma. En este trasplante utilizamos las propias células madre del paciente. Pueden recolectarse utilizando sangre periférica o médula ósea antes de administrar altas dosis de quimioterapia. Este tratamiento se indica en pacientes con linfoma de Hodgkin recurrente y quimiosensible, linfomas de grado bajo o intermedio, y mieloma múltiple. Stem Cell Transplants Autologous Transplant Stem Cell Transplants Autologous Transplant • Uses patient’s own stem cells for transplant • Peripheral blood or bone marrow stem cells collected prior to high dose treatment • Indicated for: – Chemosensitive recurrent Hodgkin’s lymphoma – Chemosensitive low grade or intermediate grade lymphomas – Multiple myeloma 6 Stem Cell Transplants Stem Cell Collection • Completed before high dose regimen given • Collected either via peripheral blood or bone marrow harvest • Collected after bone marrow stimulation either with growth factors or growth factors plus chemotherapy – Chemotherapy plus growth factors usually yields higher CD34 count than growth factors alone in heavily pretreated patients • Stems cells are cryopreserved until time of transplant • Adequate cell dose – Autologous transplant > 2 million CD34+/kg of recipient's weight – Allogeneic transplant > 4 million CD34+/kg of recipient's weight Stem Cell Transplants Autologous Transplant Process • Collection of stem cells • Administration of high dose chemotherapy given over week’s time • Within 24-48 hours after completion of chemotherapy, stems cells are infused via central venous access As stated before, the stem cell collection is done prior to the high-dose regimen being given. The cells again are collected via either peripheral blood or bone marrow harvest. If the cells are collected via peripheral blood, the bone marrow needs to be stimulated by a growth factor known as Neupogen®. In some cases, we also give chemotherapy in addition to the growth factor. By giving chemotherapy in addition to the growth factor, particularly in patients with lymphoma who have been heavily pretreated, it helps yield a higher CD34 count and hence increases the number of stem cells collected pretransplant. Once the cells are collected, they are cryopreserved until the time of transplant. An adequate stem cell dose in the autologous setting is greater than 2 million CD34 cells/kg of the recipient’s weight. In the allogeneic setting, the cell dose is greater than 4 million CD34 cells/kg of the recipient’s weight. The autologous transplant process is very simple. First, the cells are collected as discussed before. The high-dose chemotherapy is given over a week’s time. Within 24-48 hours after the completion of the chemotherapy, the stem cells are infused like a blood transfusion via central venous catheter. It takes about 2 to 3 weeks for the peripheral blood counts to recover following the highdose chemotherapy. During this time, patients are susceptible to infection and, therefore, prophylactic antibiotics are given as well as growth factors during their peri-transplant and post-transplant course. Ya mencioné que la recolección de células madre se realiza antes de un régimen de altas dosis de quimioterapia. Las células se toman de la sangre periférica o del cultivo de médula ósea. Si se recolectan de la sangre periférica, la médula debe estimularse con el factor de crecimiento Neupogen®. A veces también administramos quimioterapia, en cuyo caso, sobre todo en pacientes con linfoma extensamente tratados, ayuda a aumentar el recuento de CD34 y la cantidad de células madre recolectadas antes del trasplante. Una vez que estas se recolectan, son criopreservadas hasta el trasplante. En el contexto autólogo, una dosis adecuada de células madre debe ser superior a 2 millones de células CD34/kg de peso del receptor. En el alogénico, la dosis debe superar los 4 millones de células CD34/kg. El trasplante autólogo es muy simple. Primero, las células se recolectan como ya se explicó. La quimioterapia de alta dosis se administra por una semana. Luego de 24 a 48 horas de finalizada, las células madre se infunden por transfusión de sangre a través de un catéter venoso central. Tras la administración de estas altas dosis, el paciente recupera los recuentos de sangre periférica en 2 a 3 semanas. Durante ese tiempo, es susceptible a infecciones y se le administran antibióticos profilácticos y factor de crecimiento en los períodos peritrasplante y postrasplante. • Recovery of peripheral blood cells occurs within 2-3 weeks • Prophylactic antibiotics and growth factors support given as needed peri- and post-transplant 7 In contrast, allogeneic transplant… Por el contrario, el trasplante alogénico… …relies heavily on stem cells from a genetically HLA compatible donor. This donor can be either from the family, known as related, or from the National Marrow Donor Program, or the unrelated donor registry. These cells also can be collected via peripheral blood or bone marrow. Once again, chemotherapy is given prior to the stem cell infusion. In this setting, however, patients are given anti-rejection or immunosuppression medication prior to the stem cell infusion and are continued on the immunosuppressive medication up to 6 months after the stem cell infusion. … depende en gran medida de las células madre de un donante genéticamente compatible con antígenos de leucocitos humanos. Puede ser un familiar o pertenecer al Programa Nacional de Donantes de Médula Ósea o al registro de donantes no relacionados. Las células también pueden recolectarse de la sangre periférica o de la médula. La quimioterapia se administra antes de infundir células madre, pero los pacientes reciben medicación antirrechazo o inmunosupresora antes de la infusión y continúan con medicación durante 6 meses. Stem Cell Transplants Allogeneic Transplant Stem Cell Transplants Allogeneic Transplant • Treatment relies on collected stem cells from a genetically (HLA) compatible donor • Donor can be either related or unrelated • Stem cells collected via peripheral blood or bone marrow • Chemotherapy administered prior to stem cell infusion • Anti-rejection/immunosuppression given prior to stem cell infusion and continued up to 6 months post transplantation 8 Stem Cell Transplants Allogeneic Transplant • Benefits – Graft versus tumor effect – Potential lower relapse rate – Potential improvement in overall survival There are many benefits to an allogeneic transplant. First, is an allogeneic transplant provides a strong graft versus tumor effect and hence lowers the rate of relapse for the patient. In turn, this also increases the overall survival for the patient. However, there are many complications that can be fatal in the post-transplant setting. This includes graft versus host disease, which we will discuss later, infectious complications, and graft rejection or graft failure. El trasplante alogénico ofrece muchos beneficios, pues provee un fuerte efecto del injerto frente al tumor y reduce la tasa de recurrencia en el paciente, lo que aumenta la supervivencia general; sin embargo, hay muchas complicaciones que pueden resultar fatales en la etapa postrasplante, como la enfermedad de injerto contra huésped —que veremos más adelante—, complicaciones infecciosas y rechazo o fallo del injerto. HLA donors require a stringent HLA typing. HLA stands for human leukocyte antigen. It is DNA-based typing found on chromosome 6. We look at the major histocompatibility class I and II. Class I is denoted by the loci A, B, and C. Class II is denoted by the loci DR, DQ, and DP. Each individual inherits one set from each parent. And hence for a perfect match we would like to have a perfect 10/10 match. If we look at the primary three loci that causes the most increase in graft versus host disease: A, B, and DR, the minimum number of match you must have to have a successful transplant is 5 of 6, meaning you can have one mismatch in either one of those loci. If you look out further to class II, including DQ, the minimum match you can have is 10, and so on and so forth. This type of blood test is done on peripheral blood and takes about 2 weeks to have the final results. Los donantes de antígenos de leucocitos humanos, o HLA, requieren una estricta tipificación por el ADN del cromosoma 6. Analizamos entonces el complejo mayor de histocompatibilidad de las clases I y II. La clase I está representada por los locus A, B y C; la II, por los locus DR, DQ y DP. Toda persona hereda un conjunto de cada progenitor. Para una combinación perfecta, debemos tener una compatibilidad 10/10. Para los tres locus primarios que provocan el mayor aumento de la enfermedad de injerto contra huésped —A, B y DR—, la compatibilidad mínima para que el trasplante sea exitoso es 5 de 6, es decir, una incompatibilidad en cualquiera de los locus. Si observamos más detenidamente la clase II, incluido el locus DQ, la compatibilidad mínima es 10, y así sucesivamente. Este tipo de análisis se realiza en sangre periférica y demora unas 2 semanas. • Risks/complications – Graft versus host disease (GVHD) – Infectious complications – Graft rejection/failure Stem Cell Transplants Allogeneic Donor • Requires HLA (human leukocyte antigen) testing – DNA based – Divided into major histocompatibility (MHC) class I and class II • Class I is denoted by the A, B, C loci • Class II is denoted by DR, DQ, DP loci • Minimum of 5 out of 6 match (A,B, DR) • Minimum 9 out 10 match (A,B,C,DR, DQ) • Minimum 13 out of 14 match (A, B, C, DR, DQ, DP) • Performed on peripheral blood sample 9 Stem Cell Transplants Allogeneic Donor • Health status – – – – – – Age Past medical history Infectious disease testing CMV serology Pregnancy history Physical examination Stem Cell Transplants When assessing the donor, we look at their health status. We would like younger donors. We assess their past medical history. We look at infectious disease testing including hepatitis and HIV serologies. We look at CMV serology, pregnancy history, and the donor takes a thorough physical examination. Al evaluar a un donante, consideramos su estado de salud. Preferimos los donantes más jóvenes. Examinamos su historial médico y los análisis de enfermedades infecciosas, como los resultados serológicos de hepatitis, VIH y citomegalovirus, y los antecedentes de embarazo; y realizamos un examen físico completo. There are many types of stem cell sources: peripheral blood, bone marrow, and umbilical cord blood. Hay varias fuentes de células madre: la sangre periférica, la médula ósea y la sangre de cordón umbilical. Stem Cell Sources • Peripheral blood • Bone marrow • Umbilical cord blood 10 Stem Cell Transplants Stem Cell Sources • Peripheral blood • Bone marrow – Easily collected – Faster engraftment – Potential increased risk of graft versus host disease – Collected under general anesthesia – Slower engraftment of platelets – Potential decreased risk of graft versus host disease Stem Cell Transplants Umbilical Cord Blood • Advantages – Easily available via cord blood bank – Non-invasive collection – Minority targeted – Less stringent donor HLA matching – Potential decreased risk of graft versus host • Disadvantages – Lower cell dose • Slower engraftment • More infectious complications • Increased risk of graft failure Peripheral blood is easily collected. It is collected via venous catheter in the vein after stimulation by Neupogen because these cells are in the peripheral blood and are more susceptible and have seen antigen before, therefore, making them more immune competent, once given to the patient, the patient tends to engraft quicker, which means their counts tend to recover quicker after infusion. Because these cells are more immune competent and have been exposed to antigen, there is an increased risk of graft versus host disease for the patient. Unlike peripheral blood, in the bone marrow setting, these cells are collected via general anesthesia in the operating room. These cells are more naïve, they have not been circulating in the peripheral blood, and, therefore, have not seen antigen and, therefore, once given to the patient, the patient’s counts are slow to recover. This increases their risk of infection and bleeding complications post-transplant. But because these cells are naïve it decreases the patient’s risk of graft versus host disease. The third type of stem cell source is umbilical cord blood. They are many advantages to umbilical cord blood. First, cord blood units are found throughout the world in multiple banks throughout the United States and the world in general. These cells are collected noninvasively after the baby is born by an OB/GYN. Cord blood is minority targeted, generally selected for patients of African-American, or Asian origin. Because these cells are very immune-incompetent and very naïve, there is less DNA --- there is less stringent donor HLA typing, and these cells tend to cause less graft versus host disease. The disadvantage to umbilical cord blood is that these cell doses are small, and, therefore, once given to the patients it takes their counts many more weeks to recover and hence there is slower engraftment. Because the counts are slow to recover, patients are at more risk for infectious complications and of risk of actually La sangre periférica se recolecta fácilmente insertando un catéter venoso después de estimular con Neupogen®, porque estas células son más susceptibles. Ya han estado en contacto con antígenos y hay que hacerlas más inmunocompetentes al administrarlas al paciente; así, el injerto se adapta más rápidamente y los recuentos se recuperan más velozmente tras la infusión. Como son más inmunocompetentes y han sido expuestas al antígeno, hay un mayor riesgo de enfermedad de injerto contra huésped. A diferencia de la sangre periférica, las células medulares se recolectan con anestesia general en la sala de operaciones. Son menos reactivas, pues no han circulado en sangre periférica y no han tenido contacto con el antígeno. Una vez administradas, la recuperación de recuentos del paciente es más lenta, lo que aumenta el riesgo de complicaciones infecciosas y sangrado postrasplante. Como son menos reactivas, el riesgo de desarrollar dicha enfermedad es menor. El tercer tipo de fuente es la sangre de cordón umbilical, cuyas ventajas son numerosas. Existen unidades hemáticas de cordón umbilical en varios bancos de los Estados Unidos y, en general, en todo el mundo. Las células son recolectadas por el obstetra o ginecólogo de manera no invasiva después del nacimiento del bebé. La sangre umbilical se utiliza mucho en pacientes de minorías étnicas, generalmente de origen afroamericano o asiático. Como son muy inmunoincompetentes y poco reactivas, hay menos tipificación estricta de HLA y tienden a causar menos enfermedad de injerto contra huésped. La desventaja de esta sangre es que las células son escasas y, una vez que se administran, la recuperación de recuentos demora muchas semanas y el injerto tarda más en adaptarse. Con una recuperación de recuentos más lenta, los pacientes corren un mayor riesgo de complicaciones infecciosas y rechazo del injerto. 11 rejecting their graft. In the post-transplant setting… En el período postrasplante… …there are multiple complications. Obviously, these include infections due to the severe immunocompromised patient, graft versus host disease, organ damage from the chemotherapy, potential risk of graft failure or rejection, and also relapse is a major concern. … hay muchas complicaciones, como infecciones por una severa inmunodepresión del paciente, enfermedad de injerto contra huésped, daños a órganos por quimioterapia, riesgo de fallo o rechazo del injerto, y un grave potencial de recurrencia. Stem Cell Transplants Post-transplant Complications Stem Cell Transplants PostPost-transplant Complications • • • • • Infections Graft versus host disease Organ damage Graft failure/rejection Relapse 12 Stem Cell Transplants Infections • Major cause of mortality after transplant • Early (first 100 days) – Viruses • Herpes simplex (HSV), Cytomegalovirus (CMV), Varicella zoster virus (VZV) – Bacterial • Late In the infection setting, infections can be the major cause of mortality after transplant. In their early post-transplant course, meaning within their first 100 days, viruses are the most common infections that affect our patients. These include herpes simplex virus, cytomegalovirus, and varicella zoster. Also, bacterial infections are still common in the peri- and post-transplant course. In the late post-transplant course, meaning beyond day 100, Epstein Barr virus is the common viral complication and also fungal infections, particularly aspergillus, becomes a problem. Luego del trasplante, las infecciones pueden ser la causa principal de mortalidad. En los primeros 100 días del período inicial postrasplante, las más comunes en nuestros pacientes son los virus, como el del herpes simple, el citomegalovirus y la varicela zoster. Las infecciones bacterianas siguen siendo comunes en los períodos peritrasplante y postrasplante. En el período tardío postrasplante, pasados los 100 días, el virus de Epstein Barr es la complicación viral más común, y las infecciones micóticas, especialmente las de Aspergillus, también son problemáticas. To prevent these problems, the patients are given prophylactic antibiotics up to six months post-transplant, to cover both viruses, bacterial, and fungal infections. In addition, we also prophylax for pneumocystis infection. There is also stringent surveillance for CMV reactivation. And some patients are also prophylaxed against cytomegalovirus, particularly if they have had previous CMV infection. Para evitar esto, administramos antibióticos profilácticos hasta seis meses después del trasplante para prevenir infecciones virales, bacterianas y micóticas, y se hace profilaxis contra la infección neumocística. Hay una estricta supervisión de la reactivación del citomegalovirus, y algunos pacientes reciben tratamiento profiláctico adicional contra este virus, sobre todo si ya han estado infectados. – Viruses • Epstein-Barr (EBV), Cytomegalovirus (CMV) – Bacterial – Fungus Stem Cell Transplants Prophylaxis • Up until 6 months – – – – – Antiviral Antibacterial Antifungal Pneumocystis carinii CMV surveillance for activation vs. prophylaxis 13 Stem Cell Transplants Graft Versus Host Disease (GVHD) • What is it? – Inflammatory response mediated by donor cell’s (graft) reactivity to host cells characterized by • antigen presentation and T cell recognition • cytokine release • tissue damage Linked to HLA compatibility Develops in > 50% patients Acute or chronic Can be life threatening if uncontrolled or refractory to front-line treatment • Prophylaxis given up to 6 months post transplant • • • • Graft versus host disease, as discussed before is a major complication post-transplant. So what is graft versus host disease? It is an inflammatory response mediated by the donor cells, which is the graft reactivity to the host cells characterized by antigen presentation and T-cell recognition. There is a strong cytokine release due to damage of the patient’s tissue from the chemotherapy. This cytokine release leads to an inflammatory response that causes tissue damage for the patient. Graft versus host disease is highly linked to the HLA compatibility. Hence, the more incompatibility you have, the more risk of graft versus host disease. Graft versus host disease, or GVHD, occurs in approximately 50% of our patients despite being prophylaxed against it. We describe GVHD as either acute or chronic, depending on the time at which it occurs after the transplant. In the acute setting, this occurs within the first 100 days after the stem cells are infused, and in the chronic setting, this occurs after the first 100 days. If graft versus host disease is not controlled or treated properly, it can be life threatening. And again, as stated before, we do give prophylaxis but, once patients develop the GVHD, they must be treated aggressively. Como mencionamos anteriormente, la enfermedad de injerto contra huésped es una importante complicación en el período postrasplante. ¿Qué es esta enfermedad? Es una respuesta inflamatoria mediada por las células del donante como una reacción del injerto a las células huésped, caracterizada por la presentación del antígeno y el reconocimiento de las células T. Hay una gran liberación de citoquinas por los daños de la quimioterapia a los tejidos, lo que conduce a una respuesta inflamatoria perjudicial. Esta enfermedad está muy vinculada a la compatibilidad HLA. Cuanta más incompatibilidad hay, tanto mayor es el riesgo. A pesar del tratamiento profiláctico, la enfermedad de injerto contra huésped, o GVDH, ocurre en un 50% de nuestros pacientes. La describimos como aguda o crónica, según el momento en que ocurra luego del trasplante. En la fase aguda, ocurre dentro de los primeros 100 días de infundir células madre; en la crónica, demora más tiempo. Si no se controla o no se trata adecuadamente, puede ser mortal. Ya mencioné que utilizamos profilaxis pero, una vez que un paciente la desarrolla, debe ser tratado agresivamente. 14 Stem Cell Transplants GVHD Risk Factors • Age of recipient – Older > younger • HLA match of donor to recipient – Mismatch > perfect match • Stem cell source – Peripheral blood > bone marrow • Gender mismatching – Female --> male recipient > male --> female recipient • Intensity of preparative regimen – Ablative > reduced intensity • GVHD prophylaxis Stem Cell Transplants GVHD Manifestations • Skin – Erythematous, maculopapular rash – Hyperpigmentation – Scleroderma • Gastrointestinal tract – Oral pain/sensitivity, decreased saliva, abdominal cramping, nausea, vomiting, diarrhea • • • • Liver – hepatitis, elevated bilirubin Lung – shortness of breath Eyes – dry, red, irritated eyes Fascia – joint stiffness, swelling, pain There are many risks for graft versus host disease. First, age is major risk, the older the patient the greater the risk. HLA matching, the more mismatches you have, the more risk of GVHD you may have. The stem cells source, peripheral blood causing more graft versus host disease than bone marrow, again due to the fact that peripheral blood is more immune competent than bone marrow. Gender mismatching, we typically like to have a female donor give to another female donor because females who have had children produce more antibodies and this produces more risk of graft versus host disease when given to a male recipient. The intensity of the preparative regimen, the ablative regimens tend to cause more graft versus host disease because there is more tissue damage from this strong chemotherapy, which can incite graft versus host disease and the type of prophylaxis that is given to the patients. There are many kinds of GVHD manifestations. The skin is a common organ system affected by graft versus host disease. In the acute setting, the typical presentation can be a fine maculopapular rash that is erythematous and it may or may not be pruritic. In the chronic setting, we see more hyperpigmentation and scleroderma, much like autoimmune scleroderma. In the GI tract, GVHD can affect anywhere from the mouth to the rectum. Oral symptoms can include sensitivity, poor appetite, [and] decreased saliva. You can also have abdominal cramping, nausea, vomiting, diarrhea, weight loss, and malabsorption. GVHD also affects other organ systems including the liver, which causes hepatitis and jaundice. Pulmonary system is affected, which results in shortness of breath. Eyes can be affected, which can cause dry eye syndrome, also dry, irritated eyes. And also the fascia can be affected, which leads to joint stiffness, pain, and swelling. Existen muchos riesgos de desarrollarla. La edad es un riesgo importante: a mayor edad, mayor riesgo. Otro factor es la compatibilidad HLA: a menor coincidencia o más incompatibilidad, tanto mayor es el riesgo. Y la fuente de células madre, pues la sangre periférica causa más instancias que la médula ósea por ser más inmunocompetente que esta. Otro factor es el sexo no coincidente: en general, preferimos una donante femenina para otra donante femenina, ya que las mujeres que han tenido hijos producen más anticuerpos y eso causa mayor riesgo de enfermedad en destinatarios masculinos. Además, tenemos la intensidad del régimen de preparación: los regímenes ablativos causan más instancias, porque hay más daños tisulares provocados por una quimioterapia intensa, lo que puede estimular la enfermedad. Por último, tenemos el tipo de profilaxis utilizada. Hay numerosas manifestaciones de GVDH. La piel es un sistema orgánico comúnmente afectado por ella. En la fase aguda, la típica presentación suele ser una erupción maculopapular fina y eritematosa, con o sin prurito. En la fase crónica, hay más hiperpigmentación y esclerodermia, muy similar a la esclerodermia autoinmune. En el tracto gastrointestinal, la enfermedad puede afectar desde la boca hasta el recto. Los síntomas orales son sensibilidad, falta de apetito y disminución de la saliva. Puede haber cólicos, náuseas, vómitos, diarrea, pérdida de peso y mala absorción. La GVDH también afecta otros órganos, como el hígado, causando hepatitis o ictericia. Asimismo, el sistema pulmonar puede verse afectado por falta de aliento. En los ojos, provoca el síndrome del ojo seco y ojos secos e irritados. Puede afectar la fascia, lo que conduce a rigidez, dolor e inflamación articular. 15 Stem Cell Transplants Cutaneous GVHD Stem Cell Transplants Hyperacute Cutaneous GVHD This is a picture of acute cutaneous graft versus host disease evidenced by erythema in a macular rash that may or may not be pruritic. Este es un cuadro cutáneo agudo de la enfermedad, evidenciada por eritema en una erupción macular, que puede o no ser pruriginosa. This is a picture of hyperacute cutaneous graft versus host disease. Hyperacute meaning the GVHD has occurred within the first 30 days after stem cell infusion. This is a very angry, red, painful rash the patient has experienced after the stem cell infusion Esta es una reacción cutánea hiperaguda de la enfermedad, la cual se manifiesta dentro de los primeros 30 días tras la infusión de células madre. Es una erupción intensa, roja y dolorosa que el paciente experimenta después de la infusión. 16 Stem Cell Transplants Ocular GVHD Stem Cell Transplants Oral GVHD This is an example of ocular graft versus host disease where the patient’s eye is very red, irritated, and injected [speaker intended to say “infected”]. Esta es una manifestación ocular en la que el ojo del paciente está muy enrojecido, irritado e infectado. Oral graft versus host disease manifested by pain [and] redness in the oral mucosa. There are also can be changes on the hard palate and tongue. La enfermedad oral se manifiesta por dolor y enrojecimiento de la mucosa oral. Puede haber cambios en el paladar duro y la lengua. 17 Stem Cell Transplants Diagnosis • Clinical • Pathology – Biopsy of the affected site and clinical presentation • Diagnostic/radiographic data The clinical diagnosis of graft versus host disease can be made by the history and physical examination, although biopsy to get a pathological diagnosis is also essential. Most commonly, we can easily do skin, liver, and bowel biopsies. For the lung, we typically rely on pulmonary function testing looking at residual volume and forced vital capacity. And we also use high-resolution CT scanning to assess any abnormalities within the lung parenchyma. Para el diagnóstico clínico, puede analizarse el historial y efectuarse un examen físico, pero es esencial hacer una biopsia de diagnóstico patológico. Podemos realizar más fácilmente biopsias de la piel, el hígado y el intestino. Para los pulmones, solemos basarnos en pruebas de función pulmonar por volumen residual y capacidad vital forzada. La tomografía de alta resolución permite evaluar anomalías del parénquima pulmonar. Treatment for graft versus host disease can either be systemic or localized depending on the extensiveness of the disease. If there is more than one organ system affected, high-dose steroids are given. This is given in the form of Medrol, at 1 to 2 mg/kg of the patient’s weight. Once the patient starts to respond in their clinical symptoms then the Medrol is tapered. There is about a 50% response rate when steroids are given up front. In addition to steroids, however, immunosuppression must also be given in the form of tacrolimus. Blood levels of tacrolimus must be monitored closely. Supratherapeutic levels can cause both neuro and renal toxicity. Subtherapeutic levels can cause inappropriate treatment and inappropriate response of the clinical symptoms. In addition to oral medications, a procedure called photophoresis can also be utilized for both skin and GI symptoms. In this setting, a patient is taken to the apheresis unit, their stem cells are pulled out like dialysis. The cells are injected with psoralen, which makes them sensitive to UV light. The cells are then zapped with UV light and then re-injected into the patient. In this setting, El tratamiento de la enfermedad de injerto contra huésped puede ser sistémico o localizado, según la extensión. Si hay más de un sistema de órganos afectado, se administran altas dosis de esteroides en forma de Medrol® (1 a 2 mg/kg de peso del paciente). Una vez que este comienza a responder en su sintomatología clínica, reducimos gradualmente el Medrol®. Si los esteroides se administran inicialmente, la tasa de respuesta es de un 50%; sin embargo, además de los esteroides, la inmunosupresión también debe administrarse en forma de tacrolimus. Sus niveles en sangre deben monitorearse atentamente. Los niveles supraterapéuticos pueden causar toxicidad renal y neurológica; los subterapéuticos, un tratamiento y una respuesta inadecuados de los síntomas. Además de medicamentos orales, también puede utilizarse fotoforesis, tanto para la piel como para los síntomas gastrointestinales. El paciente es llevado a la unidad de aféresis. Sus células madre son extraídas como en la diálisis y se les inyectan psoralenos, que las hace sensibles a la luz UV. Luego de iluminarlas, son reinyectadas. El objetivo es suspender los esteroides lo – Lung involvement can be assessed by pulmonary function tests and high resolution computed tomography Stem Cell Transplants GVHD Treatment • Systemic involvement – Methylprednisolone @ 1-2 mg/kg initially then taper • ~50% response rate – Immunosuppression: tacrolimus – Photopheresis • Localized involvement – Eyes - punctal plugs, steroid eye drops – Mouth - dexamethasone mouth wash – Skin - topical steroid cream, topical moisturizers 18 Stem Cell Transplants GVHD Treatment • Second line agents – – – – – Mycophenolate mofetil Infliximab Cyclosporine Anti-thymoglobulin ~10% long term survival your goal is to try to get the patient off of the steroids as soon as possible. Photopheresis is given over several months, two to three times per week, until the symptoms have subsided. For localized treatment, particularly the eyes, mouth, and skin, it is easy to use either eye drops or mouthwash or topical creams. In the event that steroids are not successful, there are second-line agents that patients can --- that can be used for patients. This includes mycophenolate mofetil also known as CellCept®, infliximab, which is mostly used for the GI tract, cyclosporine, and anti-thymoglobulin. All these regimens are successful as a second-line agent, but if patients do not respond to these second-line agents there is about 10% long-term survival. antes posible. La fotoforesis se administra durante varios meses, de dos a tres veces por semana, hasta eliminar los síntomas. Para un tratamiento localizado, particularmente en ojos, boca y piel, es más fácil utilizar gotas oculares, enjuague bucal o cremas tópicas. Si los esteroides no tienen éxito, hay una segunda línea de agentes, tales como el mofetil micofenolato, también conocido como CellCept®; infliximab, que se utiliza mucho para tratar el tracto gastrointestinal; ciclosporina y antitimoglobulina. Todos estos regímenes son adecuados como agentes de segunda línea, pero si el paciente no responde a estos fármacos, la supervivencia a largo plazo es del 10%. 19 Stem Cell Transplants Goal of GVHD Treatment • Suppress immune reaction without suppressing graft – Follow tacrolimus, cyclosporine level • Improve quality of life • Prevent superimposed infections • Prevent secondary complications from high dose steroids – Diabetes – Avascular necrosis – Osteopenia The goal of graft versus host disease treatment is to, number one; suppress the immune system without suppressing the graft. So, if a patient has a major flare of graft versus host disease, you have to get control of the immune response of the graft cells. You want to suppress the cells overactiveness, but you do not want to suppress the cells too much such that the patient may relapse. You need to follow the tacrolimus levels again because supratherapeutic or subtherapeutic levels can be detrimental. You also want to improve the patient’s quality of life. Sometimes, in some cases, patients have severe nausea, vomiting, weight loss, cachexia, bad skin rash, bad mouth pain, and so you want to control the symptoms, either again with systemic treatment or localized treatment. Because the patients will be immunocompromised with the immunosuppressive medication, patients must be prophylaxed against [speaker intended to say, “with”] antibiotics. Once again, you want to try to prevent or decrease the incidence of superimposed infections. You also would like to decrease the incidence of secondary complications from the high-dose steroids, namely diabetes, avascular necrosis of the hips or shoulders, and also osteopenia, and osteoporosis. El objetivo del tratamiento de esta enfermedad es, en primer lugar, suprimir el sistema inmunológico y no el injerto. Si un paciente tiene un brote importante, debemos controlar la respuesta inmunológica de las células injertadas. Se debe suprimir su hiperactividad, pero no demasiado como para inducir una recurrencia. Se deben controlar los niveles de tacrolimus, ya que los niveles supraterapéuticos o subterapéuticos pueden ser perjudiciales. También queremos mejorar la calidad de vida del paciente. A veces, los pacientes experimentan náuseas intensas, vómitos, pérdida de peso, caquexia, erupciones dérmicas graves o dolor bucal intenso, que podemos controlar con tratamientos sistémicos o localizados. Como están inmunocomprometidos por la medicación inmunosupresora, se les debe administrar profilaxis antibiótica para prevenir o disminuir la incidencia de infecciones superpuestas. También es deseable disminuir la incidencia de las complicaciones secundarias derivadas de las altas dosis de esteroides, tales como diabetes, necrosis avascular de cadera u hombro, osteopenia y osteoporosis. 20 Stem Cell Transplants Graft Failure/Rejection • Graft failure – Primary – prolonged pancytopenia with bone marrow aplasia – Secondary – initial engraftment then subsequent decline of peripheral blood counts and loss of donor graft • Graft rejection – Recipient cells reject against graft (donor) cells Another complication of stem cell transplant is graft failure or graft rejection. There are two types of graft failure. The first is primary graft failure. This occurs when the patient is given high-dose chemotherapy. The stem cells are infused, but the patient’s counts do not recover and hence the patient remains pancytopenic for several months --- for several weeks (excuse me). When assessing the bone marrow examination, the bone marrow biopsy itself would be aplastic. The second form of graft failure is secondary graft failure. This occurs when the patient does have initial engraftment, which means their counts do recover after the stem cell infusion. However, over the subsequent weeks, the blood counts slowly decline. When assessing the patient’s bone marrow or peripheral blood, you notice gradual decline in the amount of donor cells in the patient’s blood. This is called secondary graft failure. In contrast to graft failure, there is also graft rejection in which the patient is given high-dose chemotherapy, stem cells are infused, the patient’s counts recover, but when assessing the bone marrow or peripheral blood, the recovered counts are the patient’s and not the donor’s. And hence the patient has rejected the graft and there are no graft cells in the donor’s specimen --- (I am sorry) there are no graft cells in the patient’s bone marrow or peripheral blood. Otra complicación del trasplante de células madre es el fallo o rechazo del injerto. Hay dos tipos de fallo. El primero es el fallo primario, que ocurre cuando el paciente recibe altas dosis de quimioterapia. Las células madre son infundidas, pero los recuentos del paciente no se recuperan y este permanece pancitopénico por varias semanas. Al examinar la médula ósea, la biopsia muestra aplasia. El segundo tipo es el fallo secundario del injerto. Ocurre cuando inicialmente el injerto se adapta al paciente, cuyos recuentos se recuperan después de la infusión de células madre; sin embargo, en las semanas siguientes, el recuento sanguíneo decae lentamente. Al evaluar la médula ósea o la sangre periférica del paciente, se observa una disminución gradual de las células del donante en la sangre, que es el fallo secundario. En contraste con los fallos del injerto, también existe el rechazo: el paciente recibe altas dosis de quimioterapia, se le infunden las células madre y sus recuentos se recuperan, pero al evaluar la médula ósea o la sangre periférica, los recuentos recuperados son los del paciente y no los del donante. Por lo tanto, el paciente ha rechazado el injerto y no hay células del injerto en su médula ósea ni en la sangre periférica. 21 Stem Cell Transplants Relapsed Disease • Treatment – Supportive care – Reduction and discontinuation of immunosuppression – Chemotherapy – Donor lymphocyte infusion Stem Cell Transplants Donor Lymphocyte Infusion (DLI) • T cell lymphocyte infusion given after allogeneic transplant with or without chemotherapy • No immunosuppression given prior to infusion • Can induce strong graft versus tumor effect • Can increase or produce graft versus host disease • Indicated for – Relapsed disease – Progressive disease – Residual disease • Contraindicated – Active graft versus host disease The final and almost worst complication is unfortunately relapsed disease. In this setting, there are still potential treatments for the patient. The patient can either choose to pursue supportive care and not receive any further treatment depending on how debilitated they are from their primary transplant. Another treatment is to reduce or discontinue the immunosuppression. So in the setting of relapse you can always taper or decrease the immunosuppression, i.e., the tacrolimus, and try to incite some graft versus host disease. If the patient is physically capable, you also can give chemotherapy by itself and see what kind of response you get in the patient’s disease. La complicación final y casi la más grave es, desafortunadamente, la recurrencia de la enfermedad. En este contexto, aún existen tratamientos potenciales para el paciente, quien puede optar por continuar el cuidado de apoyo o no recibir ningún tratamiento adicional, según el grado de debilidad después del trasplante primario. Otra alternativa es reducir o interrumpir la inmunosupresión. Si hay recurrencia, siempre se la puede disminuir gradualmente (es decir, el tacrolimus) y tratar de estimular la enfermedad de injerto contra huésped. Si el paciente es físicamente capaz, se le puede administrar solamente quimioterapia y ver qué tipo de respuesta se obtiene. The fourth and final treatment is called a donor lymphocyte infusion. A donor lymphocyte infusion or DLI is when you give T-cell lymphocytes to the recipients. This is either given with or without chemotherapy. The T-lymphocytes are collected from the donor without any growth factors or any other stimulation. The T-cells are infused into the recipient without any immunosuppression or no tacrolimus. You hope to incite a strong graft versus tumor effect, but you also can increase or produce graft versus host disease. The reason being, is again, you are giving T-lymphocytes without any immunosuppression. So the risk of graft versus host disease increases. This type of treatment is indicated in the relapsed disease setting, in [a] progressive disease setting, and in patients with residual disease after transplant. A DLI is absolutely contraindicated if the patient has active graft versus host disease. By giving a DLI to a patient with active graft versus host disease, you can incite fatal graft versus host disease. El cuarto y último tratamiento es la infusión de linfocitos de donante. También se denomina DLI y consiste en administrar linfocitos de células T al receptor. Este procedimiento puede ser concomitante con la quimioterapia. Los linfocitos T se recolectan del donante sin usar factores de crecimiento u otros estímulos. Las células T se infunden al receptor sin utilizar inmunosupresión (como tacrolimus) para incentivar el efecto del injerto contra el tumor, aunque esto puede exacerbar o inducir la enfermedad de injerto contra huésped, pues se administran linfocitos T sin inmunosupresión. Esto aumenta el riesgo de desarrollar la enfermedad. Este tratamiento está indicado en caso de recurrencia o progresión, y en pacientes con enfermedad residual postrasplante. La DLI está absolutamente contraindicada si el paciente tiene enfermedad de injerto contra huésped activa. Al infundir leucocitos de donante a un paciente con enfermedad activa, esta puede incentivarse y tornarse fatal. 22 Stem Cell Transplants Late Complications • Secondary malignancies • Cirrhosis (multi-factorial, transfusions, toxicity of prior chemotherapy, alcohol, hepatitis, GVHD) • Late infections (CMV, fungus, encapsulated bacteria) In the late phase of transplant, there can be other complications outside of infections. This can include secondary malignancies, i.e., head and neck malignancies. You also can develop cirrhosis or other organ damage. And this can be multifactorial either from prior chemotherapy, transfusion, hepatitis from drugs, and also graft versus host disease. Again, late infections are critical, CMV infection, fungal infection, encapsulated bacteria, and also Epstein Barr related infections. En la fase tardía del trasplante puede haber otras complicaciones además de infecciones, como tumores malignos secundarios de cabeza y cuello. El paciente también puede desarrollar cirrosis o daños en otros órganos. Esto puede ser multifactorial, ya sea por quimioterapia previa, transfusión, hepatitis por drogas y también enfermedad de injerto contra huésped. Son críticas las infecciones tardías por citomegalovirus, micosis, bacterias encapsuladas y el virus de Epstein Barr. In the post-transplant setting, you also want to make sure you re-vaccinate patients. Once patients are given their high-dose chemotherapy, they lose all antibodies of prior vaccinations and, hence, once they have no active infections, and are off immunosuppression, there is a revaccination schedule. This includes pneumococcal vaccination, influenza, tetanus, [and] hepatitis B. In the autologous setting, these vaccinations are given at one year after transplant. In the allogeneic setting, these vaccinations are given at least six months after discontinuation of the immunosuppression. Again, the patient can have no active infections and no active graft versus host disease. In addition, in order to assess how successful the transplant has been, you assess the chimerisms. Chimerisms are quantitative analysis of donor cells that can be assessed either via peripheral blood or bone marrow. Staging is done every three months post-transplant in the first year, and then every six months thereafter, on year two and three, and then annually. Bone densities and pulmonary function testing is also assessed at six months and then clinically as En la etapa de cuidado postrasplante debemos revacunar a los pacientes. Una vez que reciben altas dosis de quimioterapia, pierden todos los anticuerpos de las vacunas anteriores. Por lo tanto, cuando no tienen infecciones activas y ya no están inmunosuprimidos, aplicamos un programa de revacunación antineumocócica, antigripal, antitetánica y contra la hepatitis B. En el trasplante autólogo, estas vacunas se aplican un año después del trasplante. En el trasplante alogénico, al menos seis meses después de interrumpir la inmunosupresión. En estos casos, el paciente no debe tener ninguna infección activa y tampoco enfermedad de injerto contra huésped activa. Para valorar el éxito del trasplante, también se evalúa el quimerismo, que es un análisis cuantitativo de las células del donante a partir de la sangre periférica o de la médula ósea. La estadificación se realiza cada tres meses en la etapa postrasplante durante el primer año, cada seis meses en el segundo y tercer año, y luego anualmente. A los seis meses también se evalúan las densidades óseas y las pruebas de función pulmonar, y luego según el criterio clínico. • Post transplant EBV related lymphoproliferative disease (PTLD) Stem Cell Transplants Post Transplant Care • Vaccinations – – – – – Pneumococcal, influenza, tetanus, hepatitis B Given 1 year after autologous Given 6 months after cessation of immunosuppression No active infections No GVHD • Assessment of chimerisms – Quantitative analysis of donor cells • Staging every 3 months for 1 year then 6 months for 2-3 years then annually • Bone density and pulmonary function testing at 6 months then as clinically indicated 23 Stem Cell Transplants Stem Cell Transplants Conclusions • Stem cell transplant is an option for treatment of various hematologic malignancies • Stem cells can be collected from donors, umbilical cord blood or from the recipient • Ablative or reduced intensity chemotherapy is administered prior to stem cell transplant • In addition to potential advantages of graft versus tumor effect, various serious complications may occur including graft versus host disease, organ damage and graft rejection indicated. This is a diagram of the allogeneic transplantation in detail. The patient is given an ablative hematopoietic regimen. The first figure you will see denoted by A is the patient’s blood cells. The cells denoted by A with a subscript 1 are the leukemia cells. The patient again as stated above is given a preparative regimen. This B is denoted by the donor cells that are given to the patient. When assessing the patient, you note ---there is noted to be some cells denoted by B in the recipient. However, the patient is not full donor yet and there sometimes, a donor lymphocyte infusion is required, in addition to immunosuppression withdrawal, in order to incite complete donor chimera as evidenced by the last figure. Este es un diagrama detallado del trasplante alogénico. El paciente recibe un régimen hematopoyético ablativo. En la primera figura, la letra A indica las células hemáticas del paciente. Las que tienen el subíndice 1 son las células de la leucemia. El paciente recibe un régimen de preparación. La letra B indica las células de donante infundidas al paciente. Al evaluar al paciente, pueden observarse algunas células indicadas como B en el receptor; sin embargo, el paciente no es todavía donante y a veces se requiere una infusión de linfocitos del donante, además de la interrupción de la inmunosupresión, a fin de estimular una quimera completa del donante, tal como lo indica la última figura. In conclusion, stem cell transplant is an option for treatment for various hematologic diseases. Stem cells can be collected from donors, umbilical cord blood, or from the recipient, depending on which type of transplant the patient will receive. Ablative or reduced intensity chemotherapy is given prior to the stem cell transplant. In addition, there are potential advantages of graft versus tumor effect in the allogeneic setting. However, there are various serious complications that occur in the posttransplant setting to include graft versus host disease, organ damage, and graft failure. With all this being said, allogeneic transplants have the best chance of improving the patient’s overall survival, particularly in patients with relapsed disease who most likely will no longer respond to standard chemotherapy. Thank you very much for your time and attention. Please let us know if this presentation has been useful to you. El trasplante de células madre es una opción para el tratamiento de diversas enfermedades hematológicas. Las células madre pueden obtenerse de donantes, de sangre de cordón umbilical o del receptor, en función del tipo de trasplante a realizar. Antes del trasplante de células madre, se administra quimioterapia ablativa o de intensidad reducida. Además, en los trasplantes alogénicos, existen ventajas potenciales del efecto del injerto contra el tumor. Hay varias complicaciones graves en la etapa postrasplante, como la enfermedad de injerto contra huésped, daños orgánicos y el fallo del injerto. Por último, los trasplantes alogénicos son proclives a mejorar la supervivencia general, sobre todo en pacientes con recurrencia que probablemente ya no respondan a la quimioterapia estándar. Le agradezco su tiempo y atención, y espero que nos haga saber si esta presentación le ha resultado útil. 24