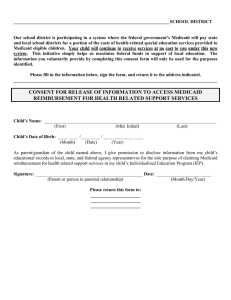
Here - National Academy for State Health Policy
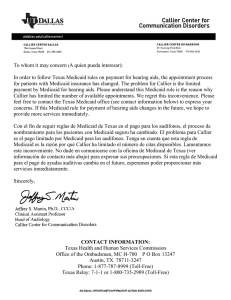
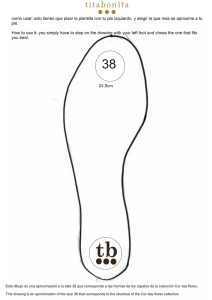
Anuncio
June, 2014 New Mexico Human Services Department, Medical Assistance Division PRESUMPTIVE ELIGIBILITY AND PRESUMPTIVE ELIGIBILITY PLUS (PE+) TRAINING MANUAL TABLE OF CONTENTS Chapter 1 - Medicaid Overview_______________________________________________ 5 Medicaid __________________________________________________________________ New Mexico Medicaid _______________________________________________________ Medicaid for Children ________________________________________________________ Centennial Care_____________________________________________________________ Fee for Servie Medicaid ______________________________________________________ Medicaid and the Affordable Care Act___________________________________________ Medicaid Expansion _________________________________________________________ Former Foster Care Coverage__________________________________________________ Centennial Care Managed Care Organizations ____________________________________ Choosing a Managed Care Organization _________________________________________ Value-Added Services ________________________________________________________ Centennial Care Managed Care Organization Contact Information ____________________ 5 5 6 6 7 7 7 8 8 8 9 9 Chapter 2 - Medicaid Presumptive Eligibility and Presuptive Eligibility Determiners _ 10 Presumptive Eligibility ______________________________________________________ Presumptive Eligibility Determiners ____________________________________________ Entities Eligible to Participate as Presumptive Eligibility Determiners _________________ Certification and Training ____________________________________________________ Performance Standards _____________________________________________________ Corrective Action Plan ______________________________________________________ 10 11 12 12 13 14 Chapter 3 - Presumptive Eligibility Determiner Specialty Types ___________________ 16 Presumptive Eligibilty Determiner Specialty Types ________________________________ 16 Presumptive Eligibility Determiners - Specialty Type 170 ___________________________ 16 Presumptive Eligibility Determiners - Specialty Type 171 ___________________________ 17 Chapter 4 - New Mexico Medicaid Categories Eligible for Presumptive Eligibililty ___ 18 Category 100 - Medicaid for Other Adults ______________________________________ Category 200 - Medicaid for Parent/Caretakers __________________________________ Category 300 - Pregnancy Medicaid____________________________________________ Category 301 - Pregnancy-Related Services______________________________________ Categories 400, 401, 402 and 403 - Regular Medicaid for Children ___________________ June, 2014 NM HSD/MAD - PE & PE+ Training Manual 19 20 21 22 23 Page 2 Categories 420 and 421 - Children's Health Insurance Program (CHIP) ________________ 24 Chapter 5 - Systems to Be Utilized By Presumptive Eligibility Determiners _________ 25 New Mexico Medicaid Portal _________________________________________________ Your Eligibilty System New Mexico for Presumptive Eligibility Determiners (YESNM-PE)__ Enrolling as a Presumptive Eligibility Determiner on the Portal ______________________ Registering as a User on the Portal ____________________________________________ Registering as a User on YESNM-PE ____________________________________________ 25 25 26 33 37 Chapter 6 - Electronic Screening for Presumptive Eligibility ______________________ 40 Checking Applicant Eligibility on the Portal ______________________________________ 40 Screening for Presumptive Eligibility on YESNM-PE _______________________________ 44 Entering a Presumptive Eligibility Approval on the Portal ___________________________58 Chapter 7 - Manual Screening for Presumptive Eligibility ________________________ 65 Chapter 8 - Completing Manual Forms _______________________________________ 67 Completing MAD 100 for Presumptive Eligibililty _________________________________ 67 Completing MAD 011 for Presumptive Eligibility _________________________________ 71 Chapter 9 - Manual Calculation of Household Size ______________________________ 73 Chapter 10 - Manually Calculating Medicaid Financial Eligibility __________________ 76 Federal Poverty Level Chart __________________________________________________ 76 Chapter 11 - Submitting Presumptive Eligibilty Approvals by Fax _________________ 79 Completing MAD 070 _______________________________________________________ 79 Chapter 12 - Submitting Paper Applications ___________________________________ 81 Submitting Applications for Ongoing Coverage ___________________________________ Central ASPEN Scanning Area (CASA)___________________________________________ Submitting Presumptive Eligibility Applicant Information Sheet _____________________ Presumptive Eligibilty Program Staff Contact Information __________________________ 81 81 81 82 Chapter 13 - Documents That May be Needed for Ongoing Medicaid- _____________ 83 Documents to Prove Citizenship, Immigrations Status and Identity __________________ 83 NM Department of Health Vital Records Web Portal ______________________________ 84 Proof of Income ___________________________________________________________ 84 Chapter 14 - Glossary and Acronyms _________________________________________ 85 June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 3 Chapter 15 - Quick Reference Information, Forms, Checklists and Worksheets ______ 92 Section 1 - Quick Reference Information Presumptive Eligibilty Contact and Resource Sheet Flow Process for Pesumptive Eligibility Training and Certification New Mexico Medicaid Web Portal and YESNM-PE Registration Workflow Electronic Presumptive Eligibility Screening Process Workflow Manual Screening for Presumptive Eligibility Workflow Federal Poverty Level with ACA Categories of Eligibity (MAD 222) Medicaid Categories of Eligibility Applicant Rights and Responsibilities - English Applicant Rights and Responsibilities - Spanish YESNM-PE Electronic Signature Page - English YESNM-PE Electronic Signature Page - Spanish Section 2 - Forms Presumptive Eigibility Determiner Agreement and Code of Conduct (MAD 219) Medicaid-Only Application - English (MAD 100) Medicaid-Only Application - Spanish (MAD 100 SP) Presumptive Eligibity Applicant Information form - English (MAD 011) Presumptive Eligibity Applicant Information form - Spanish (MAD 011 SP) Presumptive Eligibity Authorization Form (MAD 070) Section 3 - Checklists and Worksheets How to Determine Household Size flowchart Household Comp and Income Calculation Worksheet (MAD 008) Manual Presumptive Eligibility Submission Checklist o For Applicants Who Wish to Apply for Ongoing Medicaid Coverage o For Applicants Who DO NOT Wish to Apply for Ongoing Medicaid Coverage June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 4 Chapter 1 - Medicaid Overview Medicaid Medicaid is a partnership between each state and the federal government to provide low-cost or no cost health insurance to low-income individuals, families and some disabled individuals. States establish their own eligibility standards and determine the type, rate of payment, duration and scope of services based on parameters set by the United States Health and Human Services Department's Centers for Medicare and Medicaid Services (CMS). In New Mexico, the Human Services Department's (HSD) Medical Assistance Division (MAD) administers the Medicaid program. The HSD's Income Support Division (ISD) determines eligibility for all HSD programs but in some instances, Medicaid applications may be routed to MAD for processing Eligibility for all Medicaid programs is based on citizenship/immigration status, residency, income and other factors. The income guidelines used to determine Medicaid eligibility are based on the Federal Poverty Levels (FPL) as set by the United States Health and Human Services Department. FPLs are set based on household size and total income. Although there is no cost to enroll in Medicaid, some categories of eligibility may require minimal co pays for doctor visits, emergency room care and prescriptions. Benefit packages vary for different categories of eligibility. New Mexico Medicaid Currently, New Mexico has approximately 40 categories of Medicaid eligibility. Some of these categories include coverage for children, families, pregnant women, adults, long-term care recipients and individuals who are eligible for both Medicare and Medicaid benefits. All New Mexico Medicaid Categories of Eligibility (COEs) have a designated numeric COE listing associated with the COE name. A full listing of these COEs can be found at: http://www.hsd.state.nm.us/uploads/files/Looking%20For%20Information/General%20Information/R ules%20and%20Statutes/Medical%20Assistance%20Division/MAD%20NMAC%20Eligibility%20Program %20Manual/Eligibility%20Pamphlet%20011514.pdf Medicaid services in New Mexico are provided to most recipients through Centennial Care. Centennial Care is the name of the New Mexico Medicaid Managed Care program. Native Americans who are eligible for both Medicare and Medicaid or need nursing facility level of care are required to be enrolled in Centennial Care. All other Native Americans can choose to enroll in Centennial Care or access services through Fee for Service Medicaid. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 5 Coverage for most Medicaid programs must be renewed every 12 months. To renew, recipients should ensure that all information on file with HSD is up-to-date and accurate. Any changes in address, income, family size, pregnancy status or other factors that could affect eligibility should be reported to HSD/ISD. When a recipient's renewal date is approaching, HSD will send the recipient a notice informing them that it is time to renew. Any individual who does not complete the required renewal process or respond to HSD's request for more information may lose eligibility and their Medicaid coverage. Some applicants may be eligible for up to three months of Retroactive Medicaid coverage. This coverage may be able to assist with payment of any outstanding medical bills incurred in the threemonth retroactive time frame. To be eligible, the applicant must have met the eligibility standards in the prior months requested. The category of eligibility must also have been in effect in the prior months that the retroactive coverage is requested. Medicaid for Children Medicaid coverage may be available for children in families with household income up to 300% of the FPL for children who are five years old and younger; or up to 240% FPL for children between six and 18 years-old. Children's Medicaid coverage is provided through regular Medicaid or through the Children's Health Insurance Program (CHIP). CHIP coverage is generally available to children in families with incomes at the higher income threshold of Medicaid eligibility. Unlike regular children's Medicaid coverage, CHIP may have minimal co-pays for some services. In New Mexico, a recipient's enrollment in regular Medicaid or CHIP coverage is evident by the enrolled category of eligibility (COE). Regular Medicaid COEs include categories 400, 401, 402 and 403, while CHIP COEs are categories 420 and 421. Centennial Care Most New Mexico Medicaid recipients, including Native Americans who choose to enroll in Managed Care, will access their care through a Managed Care Organization (MCO). An MCO is an insurance company that contracts with providers and medical facilities to provide healthcare to its members. New Mexico's Medicaid Managed Care program is called Centennial Care. Centennial Care offers a full spectrum of physical health, behavioral health, and long-term care services, including the Community Benefit. The Community Benefit includes services like adult day health, respite care and personal care services that help to keep people in their homes and communities. Individuals who are enrolled in Centennial Care may have a Care Coordinator assigned to help them manage and coordinate services. Care Coordinators will be assigned to members based on a Health June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 6 Risk Assessment (HRA) that will be given to each Centennial Care enrollee. The HRAs may be given in person or by phone and are conducted by the member’s MCO. In Centennial Care, some categories of eligibility may require minimal co-pays; however, Native Americans are exempt from these co-pays. Fee for Service Medicaid Most Native Americans are not required to be in Centennial Care but can choose to enroll if they wish. Native Americans who are eligible for both Medicare and Medicaid or require a nursing facility level of care are required to be in Centennial Care. Native Americans who do not enroll in Centennial Care will receive their services through Fee-for-Service (FFS) Medicaid. FFS covers the basic Medicaid benefit package, such as preventive, specialty and behavioral health services, and emergency care. Enhanced Centennial Care services such as care coordination and an MCO's Value-Added Services are not available to FFS recipients. There are no co-pays for Native Americans enrolled in the New Mexico Medicaid program, whether they are in Centennial Care or FFS Medicaid. Native Americans enrolled in Centennial Care or in FFS Medicaid can get care from any Indian Health Services (IHS) facility or Tribal Health Clinic. Native Americans who enroll in Centennial Care can also keep their same doctor(s) at IHS. If a Native American is enrolled in Centennial Care, their MCO would pay the IHS doctors, lab, pharmacy, and other services. If the member needs to be referred to a specialist outside of IHS, the MCO would pay for the visit and, if needed, help arrange the transportation and/or cover the cost of transportation to the visit. Medicaid and the Affordable Care Act The Patient Protection and Affordable Care Act (ACA) is a United States federal statute signed into law by President Barack Obama on March 23, 2010. The ACA was enacted with the goals of increasing the quality and affordability of health insurance, lowering the uninsured rate by expanding public and private insurance coverage, and reducing the costs of healthcare for individuals and the government. It introduced a number of mechanisms—including mandates, subsidies, and insurance exchanges— meant to increase coverage and affordability. Medicaid Expansion One of the new health coverage options that the ACA has created includes an expanded Medicaid category for low-income adults. The Medicaid Expansion, as it is commonly called, provides coverage for a new adult population that was not eligible for Medicaid in the past. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 7 The Medicaid Expansion has its own set of eligibility requirements. As with most categories of Medicaid, this means that recipients must meet certain guidelines to be enrolled. These guidelines include citizenship, residency and income requirements that are based on the Federal Poverty Level (FPL). To be eligible for the Medicaid Expansion, individuals must have income that is at or below 133% of the FPL. Individuals with income between 134%-138% FPL may be eligible for a 5% of 100% of FPL income disregard that may make them eligible for coverage. The Medicaid Expansion is for nonpregnant individuals 19-64 years old. The Medicaid Expansion cannot cover individuals who are eligible for and/or receiving Medicare. Individuals who receive coverage under the Medicaid Expansion have a different benefit package than Standard Medicaid, which is called the Alternative Benefit Plan (ABP). A list of benefits covered under the ABP and a comparison of these benefits to Standard Medicaid can be found online at: http://www.hsd.state.nm.us/LookingForInformation/client-co-payments.aspx. The ABP includes nominal co-pays for certain services, depending on the income level of the recipient. Like other Medicaid categories, Native Americans recipients are exempt from these co-pays. Former Foster Care Coverage In addition to the Medicaid Expansion, the ACA requires states to cover individuals who were formerly recipients of foster care, up to age 26. New Mexico covers these individuals when they were recipients of foster care in New Mexico, but not when they received foster care in another state. These individuals are eligible for the full Standard Medicaid benefit package and must enroll in Centennial Care. Centennial Care Managed Care Organizations Most Medicaid recipients, including Native Americans who choose to be in Centennial Care and those who require a nursing facility level of care, will get their services from one of four Centennial Care MCOs. An MCO is an insurance company that contracts with providers and medical facilities to provide healthcare to its members. The four MCOs that provide Centennial Care services are: • Blue Cross Community Centennial • Molina Health Care of New Mexico, Inc. • Presbyterian Health Plan, Inc. • UnitedHealthcare Community Plan of New Mexico Choosing a Managed Care Organization Centennial Care members choose one of the four Centennial Care MCOs to provide their coverage. Medicaid applicants, including Native Americans who choose to be in Centennial Care, are encouraged to select an MCO at the time of application submission. This includes individuals who are applying for June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 8 Presumptive Eligibility. Native Americans who do not want to be enrolled in Centennial Care should identify themselves as Native American on their application and do not need to enter an MCO choice. Any Medicaid applicant who does not indicate that he/she is Native American and does not choose an MCO will be automatically assigned to an MCO. Value-Added Services All four Centennial Care MCOs offer the same basic benefits for each approved Medicaid category of eligibility. MCOs also offer Value-Added Services to their members. These are additional benefits that the MCOs are not contractually obligated to offer. Value-Added Services are submitted to and approved by HSD/MAD. These benefits vary from one MCO to the next and may also vary depending on the member's approved category of eligibility. An MCO's Value-Added Services are not available through Fee For Service Medicaid or during the Presumptive Eligibility approval span. Before a Medicaid recipient enrolls with any one of the MCOs, he/she should ensure that his/her providers are contracted with that MCO. Recipients should also evaluate the MCO's Value-Added Services to see which benefits best meet their needs. Providers Directories and information on ValueAdded Services can be accessed on each MCO’s web site or by calling the MCO's Member Services phone line. Centennial Care Managed Care Organization Contact Information Blue Cross Community Centennial (866) 689-1523 www.bcbsnm.com/coverage/medicaid Molina Health Care of New Mexico, Inc. (877) 373-8986 www.molinahealthcare.com/en-us/Pages/home.aspx Presbyterian Health Plan, Inc. (888) 977-2333 www.phs.org/pages/default.aspx UnitedHealthcare Community Plan of New Mexico (877) 236-0826 www.uhccommunityplan.com/ June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 9 Chapter 2 - Medicaid Presumptive Eligibility and Presumptive Eligibility Determiners Presumptive Eligibility Presumptive Eligibility (PE) is short-term Medicaid coverage for eligible individuals. PE is not available for every Medicaid category of eligibility but is available for children, pregnant women, former foster care recipients, and some adults. The goal of presumptive eligibility is to provide access to immediate care for eligible recipients and to ensure assistance with application submission and possible ongoing Medicaid coverage for those individuals. Individuals who are initially screened for PE are done so based on some of the same qualifying factors that help to determine ongoing eligibility. Individuals who are accurately screened for PE are most likely to be approved for ongoing coverage. To be eligible for PE, applicants must meet citizenship requirements. These requirements state that individuals applying for coverage must be a US Citizen, a US National or an eligible immigrant. Applicants are not required to supply a Social Security Number (SSN) to be screened or approved for PE but are required to if they wish to apply for ongoing Medicaid coverage. To be eligible for PE or ongoing Medicaid, applicants or recipients must be living in New Mexico on the date of application or final determination of eligibility. Applicants must also have demonstrated an intention to remain in the state. Residence in New Mexico is established by living in the state and carrying out the types of activities associated with day-to-day living, such as occupying a home, enrolling child(ren) in school, getting a state driver’s license, or renting a post office box. An applicant or recipient who is homeless is considered to have met the residence requirements if he or she intends to remain in the state. Eligible screenings and enrollments of individuals in PE coverage can only be made by certified Presumptive Eligibility Determiners (PEDs). PEDs must meet the PED certification requirements as established by the New Mexico Human Services Department's (HSD) Medical Assistance Division (MAD). Except in instances where technical difficulties prohibit its use, all PEDs must utilize the section of the on-line Your Eligibility System New Mexico (YESNM) designed for the exclusive use of PEDs to screen individuals for PE (YESNM-PE). YESNM-PE is only available for use by those individuals who have met the certification requirements of a PED. PEDs are required to submit the information used to determine an individual eligible for PE to HSD for auditing purposes. After screening an applicant for PE, the PED must also ask each applicant if they wish to be evaluated for ongoing Medicaid coverage. If the applicant chooses to be evaluated for ongoing coverage, the PED will indicate the applicant's choice and submit the information to HSD via June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 10 YESNM-PE. This information will be used to populate an on-line application for Medicaid eligibility, which will be evaluated for ongoing coverage. PE coverage will terminate for any applicant who has been approved for PE but who does not submit an application for ongoing Medicaid coverage on the last day of the month following their PE approval date. Any individual who has been approved for PE and who submits an application for ongoing Medicaid by the last day of the month following their PE approval will have PE coverage in effect until the day that the final application determination has been made. Failure of an applicant to submit any information requested by HSD that is needed to process the application for ongoing coverage in the timeframe requested will be grounds for a denial and will close the Presumptive Eligibility span. Presumptive Eligibility Determiners There are a number of Presumptive Eligibility Determiners (PEDs) throughout the state who are trained and certified to screen and enroll eligible individuals into PE coverage. Each certified PED is issued a unique PED number that is used in the submission of a PE determination. PE determinations can only be made by individuals who have met the PED certification requirements as established by HSD/MAD. These requirements include attending and participating in a stateauthorized training and the completion and passing of a PED program comprehension test. PEDs who were certified by HSD/MAD prior to October, 2013 are required to recertify in order to maintain their status of an active PED. Any PED who has not completed the new certification requirements that have gone into effect on January 1, 2014 will be disenrolled as a PED until the new certification requirements have been met. All PEDs are required to maintain applicant confidentiality and adhere to the Health Insurance Portability and Accountability Act (HIPAA) Privacy rules. PEDs must also agree to meet PED performance standards as outlined in the Presumptive Eligibility Determiner Agreement form (MAD Form219). This agreement form must be completed on the New Mexico Medicaid Portal (Portal) before a PED will be certified to perform PE determinations. All PEDs must utilize YESNM-PE to determine an applicant eligible for PE. They must also enter all PE approvals on the Portal on the day of the approval. Both systems must be utilized at all times unless a system error or power outage prevents their usage. In these extreme instances, a PED must manually determine the individual’s eligibility and submit the paperwork used to determine the eligibility to HSD for auditing purposes. The PED will then fax the PE approval to Xerox, the New Mexico Medicaid Fiscal Agent, on the day of the approval. PEDs utilizing the paper process must still ask the individual if they wish to be evaluated for ongoing coverage. If the individual wishes to apply for ongoing Medicaid eligibility, the PED must supply the applicant with a paper version of the Medicaid-only application June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 11 (MAD100; Rev 1/21/14). The PED must assist the individual with the completion of the application and submit the application to HSD for processing. This application must be submitted to HSD within two business days of the PE approval. Entities Eligible to Participate as Presumptive Eligibility Determiners Entities who may participate as PEDs must be: (a) a qualified hospital that participates as a provider under the Medicaid state plan or a Medicaid 1115 demonstration, notifies the Medicaid agency of its election to make presumptive eligibility determinations and agrees to make PE determinations consistent with state policies and procedures; or (b) a qualified hospital that has as not been disqualified by the Medicaid agency for failure to make PE determinations in accordance with applicable state policies and procedures or for (c) a federally qualified health center (FQHC), an Indian Health Service (IHS) facility, a department of health (DOH) clinic, a school, a children, youth and families department (CYFD) child care bureau staff member, a primary care provider who is contracted with at least one HSD contracted MCO, a head start agency, or staff at New Mexico Department of Corrections facilities, County Detention Centers and Jails; or (d) other entities that HSD has determined as an eligible presumptive eligibility participant Some of these entities are able to determine PE for any PE-eligible category; however, other entities are able to determine PE only for children and pregnant women. These distinctions are outlined further in Chapter 3 of this manual. Certification and Training All PEDs must participate in a state-authorized training. These trainings may be available as webinars, in-person sessions or self-paced on-line trainings. Pre-registration may be required for some sessions and class size limitations may apply. Once a training session has been completed, the trained individual must also take and pass a program comprehension test. A minimum passing score of 90% is required. Any individual who has scored below 90% is allowed to retake his/her test. If the second test also results in a score below 90%, the individual will be required to repeat the training and will again be given the opportunity to take a test to meet the 90% passing grade requirement. Once a passing score of 90% has been achieved, the individual must register as a PED and electronically “sign” the Presumptive Eligibility Determiner Agreement Form (MAD 219). Once this registration is June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 12 complete and submitted, it will be validated by HSD/MAD staff to ensure that the registrant has completed the training and passed with the minimum required test score. After validation, the individual will be registered as an eligible Determiner, and a Presumptive Eligibility Determiner number will be issued. This number will be unique to the PED and is not transferrable to any other individual or entity. The PED will be held accountable for any and all PE Determinations submitted under his/her PED number. Before screening an individual for PE, the PED should check the individual's eligibility in the Portal. PE coverage is available to a recipient once every 12 months or once per pregnancy. The Portal will show if the recipient has had a prior PE approval that may make them ineligible. Most recipients who are currently enrolled in Medicaid coverage are also ineligible for PE. When a PED has determined that an individual is eligible for PE, the PED will submit the determination to the New Mexico Fiscal Agent, Xerox, via the New Mexico Medicaid Portal. All PE submissions should be entered via the Portal unless there is a system error or power outage that necessitates the submission of the PE notification via fax. If the PE must be submitted by fax, the information must be completed on the Medicaid Presumptive Eligibility Authorization form (MAD 070; Rev 3/6/14) and faxed to Xerox within 24 hours of the PE determination. Performance Standards To ensure that applicants have been accurately screened for PE, all PEDs must adhere to the performance standards and procedures as outlined in the Presumptive Eligibility Determiner Agreement. These standards include: 100% of PE screening results submitted to HSD/MAD for auditing purposes PE Determiners will encourage all PE applicants to seek ongoing Medicaid eligibility 90% of applications received result in an approval of ongoing Medicaid eligibility Utilize the New Mexico Medicaid Portal to verify current individual eligibility and/or enrollment status Utilize the New Mexico Medicaid electronic PE screening tool, YESNM-PE, to screen for and submit PE screening applications Utilize the New Mexico Medicaid Portal to submit all PE approvals, unless a system error or power outage or lack of an applicant social security number necessitates the submission of the PE via fax. In instances where a fax approval is submitted, the PED must use the Presumptive Eligibility Approval form (MAD 070; Rev 3/6/14) for the submission. PEDs must submit the PE approval on the day of the PE determination Corrective Action Plan June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 13 PEDs are required to adhere to the performance standards, confidentiality clause and PE Determiner Code of Conduct as outlined in the Presumptive Eligibility Determiner Agreement and Code of Conduct Rev 3/19/14). PEDs must also follow the procedures for screening, determining and submission of all PE approvals. This includes the utilization of the automated systems developed by HSD for the use of PEDs (see Chapter 5 "Systems to be Utilized By Presumptively Eligibility Determiners"). In instances where these systems are not available, the PED is responsible for accurate and complete applicant PE screening and approvals. To ensure a successful PED program, HSD will rely on consistent, highly effective performance by its PEDs. In instances where a PED’s work performance falls short of established performance standards, HSD/MAD may implement corrective action measures for improvement, design a performance improvement plan for the PED or take further disciplinary action when necessary. HSD/MAD is in the process of finalizing the PED auditing process. In this process, a designated HSD/MAD PE Program Staff member will monitor, track and analyze PED performance. PED Program Staff will conduct an objective, constructive evaluation of a PED’s performance; clearly delineate areas earmarked for improvement; and make every attempt to support the PED in achieving program performance standard compliance. PE Program Staff may also conduct a performance “coaching” session(s) prior to making any corrective action decisions. A progressive corrective action plan, ranging from verbal coaching to immediate dismissal, will be used in an effort to improve a PED’s work performance. Progressive corrective action is not applicable in every situation. Overriding the progressive process and initiating the immediate suspension or termination of the PED may be at the sole discretion of HSD/MAD PE Program Staff. Any PED who violates client confidentially or privacy or manipulate client information in any way that might result in an incorrect PE determination will automatically be terminated as a PED and are not eligible for the progressive action process to a corrective plan. The normal steps in the progressive action process are as follows: Step 1: Verbal Warning: Performance Evaluation/Coaching Review PED Performance Standard Requirements HSD/MAD staff will verbally communicate the performance evaluation to the PED Identify the PED's performance issues Outline future work performance expectations Discuss ways to provide additional support or training Follow-up with PED with updates to let him/her know if work is improving Step 2: Written Warning June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 14 HSD/MAD staff will supply the PED with a written performance improvement plan describing: o Specific performance expectations/results the PED must meet o Specific steps the PED must take to improve his/her performance o The support to be provided by HSD/MAD PE Program staff o The date(s) by which the improvement must occur Step 3: Suspension A suspension is a defined period of time that the PED will not be allowed to determine presumptive eligibility for applicants. HSD/MAD PE Program Staff will: o Identify the reason for the suspension o Notify the PED of the action plan for reinstatement o Indentify time frame in which PED must retake PED training and pass with a minimum comprehension score of 90% PED will: o Complete the PED Certification Training o Pass the PED Training Test with a minimum score of 90% o Re-complete the PED Agreement and agree to all terms and conditions of the agreement Step 4: Dismissal or Termination June, 2014 Any PED who has not satisfactorily met performance standards as outlined in the PED Agreement and who has failed to meet the requirements of the Correction Action Plan will be terminated. Termination of a PED after the three-step correction action plan will make the PED ineligible to be recertified for a minimum of one year after the date of dismissal or termination After a time span of one year (termination or dismissal), the PED may be eligible to begin the recertification process of becoming an active PED NM HSD/MAD - PE & PE+ Training Manual Page 15 Chapter 3 - Presumptive Eligibility Determiner Specialty Types Presumptive Eligibility Determiner Specialty Types New Mexico Medicaid currently has over 40 categories of eligibility (COEs). Only some of these COEs are eligible for Presumptive Eligibility (PE) coverage. Prior to the implementation of the Affordable Care Act (ACA), many COEs were not accessible through the PE process. Only some categories that covered children or pregnant women were eligible for potential PE coverage. Beginning January 1, 2014 some adult categories, other than pregnancy, may also be eligible for PE coverage by certain approved Presumptive Eligibility Determiners (PEDs). Some PEDs have a specialty type that enables them to determine PE for more COEs than just children and pregnant women. Each person who is established as a valid PED will be certified with a provider specialty type. These specialty types, 170 or 171, dictate the COEs that the PED is able to determine for PE. PEDs who are certified as Specialty Type 170 are eligible to determine PE exclusively for children and pregnancy COEs. PEDs who are certified as Specialty Type 171 are able to screen for children and pregnancy coverage but also for some other adult COEs. Specialty Type 171 PEDs are also known as Presumptive Eligibility Plus (PE+) Determiners. Specific guidelines exist for each specialty type and the categories for which PE may be determined. PE determinations submitted by a PED not authorized for that Specialty Type would be rejected by the Xerox, New Mexico Fiscal Agent. For the purpose of this manual and training, all PE information will be applicable for all PEDs unless it is noted that it applies only to the PE+ Determiners. Presumptive Eligibility Determiner Specialty Type 170 PEDs who have been certified to determine PE with a 170 Specialty Type can determine PE for children and pregnancy coverage. The Children and Pregnancy COEs of New Mexico Medicaid that can be determined presumptively eligible by PEDs with Specialty Type 170 are: COE 300 COE Description Full Medicaid for Pregnant Women 301 400 401 Pregnancy-Related Services Only Children Ages 0-5 Children Ages 6-18 Federal Poverty Level (FPL) 0% up to app 47% FPL (fixed dollar amount) 47% up to 250% FPL 0% up to 200% FPL 0% up to 138% FPL 402 403 420 421 Children Ages 0-5 Children Ages 6-18 CHIP Children Ages 0-5 CHIP Children Ages 6-18 200% up to 240% FPL 138% up to 190% FPL 240% up to 300% FPL 190% up to 240% FPL A 5% income disregard of 100% of the FPL is applied to COEs in some instances June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 16 Presumptive Eligibility Determiner Specialty Type 171 PEDs who have been certified with Specialty Type 171 are also known as PE+ Determiners. In addition to the children and pregnancy COEs, PE+ Determiners may also determine PE for the "Other Adult" and "Parent Caretaker" COEs. The Children, Pregnancy, Adult and Parent/Caretaker COEs of New Mexico Medicaid that can be determined Presumptively Eligible by PEDs with Specialty Type 171 are: COE 100 200 COE Description Adult Group Ages 19-64 Parent/Caretaker Relative Federal Poverty Level (FPL) 0% up to 133% FPL 0% up to app 47% FPL (fixed dollar amount) 300 Full Medicaid for Pregnant Women 301 400 401 402 403 420 421 Pregnancy-Related Services Only Children Ages 0-5 Children Ages 6-18 Children Ages 0-5 Children Ages 6-18 CHIP Children Ages 0-5 CHIP Children Ages 6-18 A 5% income disregard is applied to COEs in some instances 0% up to app 47% FPL (fixed dollar amount) 47% up to 250% FPL 0% up to 200% FPL 0% up to 138% FPL 200% up to 240% FPL 138% up to 190% FPL 240% up to 300% FPL 190% up to 240% FPL PE+ Determiners are only eligible to participate as such if they are employed by and physically stationed at a specific location type. This will include hospitals that have elected to participate as a PE Provider location but does not extend to a hospital's associated clinics or to any PED who is stationed off-site from their normal work site. New Mexico has opted to further extend the number of eligible PE+ locations to include employees of Indian Health Services (IHS) medical facilities and clinics as well as staff at New Mexico Department of Corrections facilities, County Detention Centers and Jails. PE+ Determiners are required to adhere to the same training, certification and performance standards required of all PEDs. Any PED who does not meet these standards may be put on a corrective action plan and, if standards are still not met, may be required to retake a PED training course and program comprehension test before they are reinstated as a PED in good standing. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 17 Chapter 4 - New Mexico Medicaid Categories Eligible for Presumptive Eligibility Determinations Not all Medicaid categories of eligibility (COEs) are eligible for Presumptive Eligibility (PE) determinations. The Affordable Care Act (ACA) makes the PE process available for hospitals to screen individuals who would fall under the Other Adult and Parent/Caretaker categories (COEs 100 an 200) for possible PE coverage. Presumptive Eligibility Determiners (PEDs) who are certified to determine PE for these COES are Presumptive Eligibility Plus (PE+) Determiners. New Mexico has opted to further extend the number of eligible PE+ locations to include employees of Indian Health Services (IHS) medical facilities and clinics as well as staff at New Mexico Department of Corrections facilities, County Detention Centers and Jails. Other optional COEs that New Mexico has included in its PE program are for children in families with household income up to 300% of the Federal Poverty Level (FPL) and for pregnant women in families with household income up to 250% of the FPL. These are children's COES 400, 401, 402, 403, 420 and 421 and Pregnancy Medicaid COEs 300 and 301. New Mexico has had a PE program in place for these COEs for several years and will continue to do so for these optional categories. All Medicaid COEs have their own set of eligibility guidelines, benefit packages and program limitations. In some COEs, minimal co-pays may also exist.* Whether coverage is granted through PE or through a full Medicaid determination, all existing program standards apply for each COE. *NOTE: Native Americans are exempt from all Medicaid co-pays. To be eligible for PE, individuals must meet certain general guidelines that apply to PE but also those that are specific to each category of eligibility (COE). The general guidelines for PE are: Household income must be below the monthly limit for the applicable household size Individual must be a US Citizen, US National or an eligible immigrant Individual may not be currently enrolled in Medicaid (unless the individual becomes pregnant while enrolled in Family Planning Medicaid) The individual has not had a PE approval in the past twelve months. Or, if pregnant, has not had a PE approval for the same pregnancy. PE guidelines for specific COEs are outlined in the following section. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 18 Other Adults and Parent/Caretakers (Categories 100 and 200) Category 100 - Medicaid for Other Adults Adults who may be eligible for Medicaid in the Other Adult (Medicaid Expansion), or Category 100 COE, must be 19 through 64 years of age, have a countable household income of 133% or below of the FPL and must meet all other non-financial eligibility requirements. Individuals eligible for PE or on-going Medicaid eligibility for COE 100 will receive the benefits available in New Mexico's Alternative Benefit Package (ABP). Most applicants who have been approved for Other Adult PE will be required to choose a Managed care Organization (MCO) at the point of the PE approval. Native American applicants are exempt from this requirement and may choose to receive their services from an MCO or through Fee for Service (FFS) Medicaid. An MCO's Value-Added Services are not available through FFS Medicaid or during the PE approval span. Value-Added Services are only available to applicants who are approved for ongoing coverage and are enrolled with an MCO. Medicaid for Other Adults - COE 100 Category Age Income Guideline 100 19-64 Up to 133%* of the FPL *5% of 100% of FPL income disregard may apply to the Other Adult COE Adults age 19-64 Non-pregnant No longer eligible once age 65 has been reached PE may only be granted once every 12 months May not be enrolled in or be eligible for Medicare coverage Childless adults are eligible Countable household income must be 133% or below of the FPL (5% of 100% FPL income disregard may apply) Must meet all non-financial eligibility requirements Benefits available through the Alternative Benefit Package (ABP) and may include minimal copays.* THE ABP includes: o Ambulatory patient services o Prescription drugs o Emergency services o Rehabilitative and habilitative services and devices o Hospitalization o Laboratory services o Maternity and newborn care o Preventive services and chronic disease management o Behavioral health care (including substance abuse) June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 19 o Pediatric services, including oral and vision (19 and 20 year-olds only) o Medically-necessary services for 19 and 20 year-olds added (EPSDT -includes oral and vision care) o Nonemergency transportation o Dental services (prevention and maintenance) *NOTE: Native Americans are exempt from all Medicaid co-pays Category 200 - Medicaid for Parent/Caretakers Adults who may be eligible for Medicaid as a Parent/Caretaker, or Category 200 COE, must be the parent, stepparent or adoptive parent of a child who resides with them. When the parent(s) do not live with the child, specified relative(s) within the fifth degree of relationship by blood, marriage or adoption as determined by New Mexico statute chapter 45 uniform probate code may be eligible for COE 200. There are no age limitations for COE 200 but eligible enrollees must meet all financial and non-financial eligibility requirements. Households with countable income less than the income standard for the household size are financially eligible. Most applicants who have been approved for Parent/Caretaker PE will be required to choose an MCO at the point of the PE approval. Native American applicants are exempt from this requirement and may choose to receive their services from an MCO or through FFS Medicaid. An MCO's Value-Added Services are not available through FFS Medicaid or during the PE approval span. Value-Added Services are only available to applicants who are approved for ongoing coverage and are enrolled with an MCO. If a full Medicaid application is submitted and on-going eligibility is approved, the coverage will remain in effect for 12 months unless a change in situation causes the individual to no longer meet eligibility requirements (such as a child no longer being in the household). Medicaid for Parent/Caretakers - COE 200 Category Age Income Guideline 0% up to app 47% FPL (fixed dollar 200 19 + amount) *5% of 100% of FPL income disregard may apply to the Parent/Caretakers COE Must be a natural, step or adoptive parent of a child, provided they live with the child Specified relative(s) within the fifth degree of relationship by blood, marriage or adoption may be eligible PE may only be granted once every 12 months Meet all non-financial eligibility requirements Household with countable Income less than the income standard for the household size No age restrictions 5% disregard up to 100% of FPL may apply if applicant is 65 or older or is Medicare recipient June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 20 Pregnancy Medicaid and Pregnancy-Related Services Medicaid (Categories 300 and 301) Category 300 - Pregnancy Medicaid Women who are pregnant and who have a household income of up to approximately 47 % of the FPL (fixed dollar amount) may be eligible for Pregnancy Medicaid coverage. Individuals enrolled in this COE will receive full Medicaid benefits. Applicants/enrollees in this COE may have other insurance coverage in effect. There are no income disregards for COE 300. No proof of pregnancy is required beyond the applicant's self-attestation. During the PE eligibility span, ONLY ambulatory prenatal care is covered. This includes amniocentesis, sonograms, lab work, pregnancy-related prescriptions, pre-decision counseling, and miscarriages. Delivery expenses are not covered unless an application for on-going coverage has been submitted and the applicant has been determined eligible for on-going coverage. Most applicants who have been approved for Pregnancy PE will be required to choose an MCO at the point of the PE approval. Native American applicants are exempt from this requirement and may choose to receive their pregnancy services from an MCO or through FFS Medicaid. An MCO's ValueAdded Services are not available through FFS Medicaid or during the PE approval span. Value-Added Services are only available to applicants who are approved for ongoing coverage and who are enrolled with an MCO. An applicant who has been approved for on-going coverage and who is in her third trimester may continue to see her existing OB/GYN provider even if that provider is not contracted with a Centennial Care MCO. The Medicaid recipient should notify her MCO's Member Services Unit about her current OB/GYN provider. An applicant who has been approved for on-going COE 300 will remain covered for two months postpartum after their child is born, regardless of income or household changes. Category 300 Income Guideline 0% up to app 47% FPL (fixed dollar amount) Household income must be at or below approximately 47% of FPL (fixed dollar amount) No income disregards in effect Individual may have other insurance coverage Self-attestation of pregnancy acceptable Eligible for one PE determination for each pregnancy June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 21 Category 301 - Pregnancy-Related Medicaid Women who are pregnant and who have a household income of 47% to 250% of the FPL may be eligible for Pregnancy-Related Medicaid coverage. Individuals enrolled in this coverage will only have access to pregnancy-related services. Applicants/enrollees in this coverage may have other insurance coverage in effect. A 5% disregard up to 100% of FPL may apply. No proof of pregnancy is required beyond the applicant's self-attestation. During the PE eligibility span, ONLY ambulatory prenatal care is covered. This includes amniocentesis, sonograms, lab work, pregnancy-related prescriptions, pre-decision counseling, and miscarriages. Delivery expenses are not covered unless an application for on-going coverage has been submitted and the applicant has been determined eligible for the on-going coverage. Most applicants who have been approved for Pregnancy-Related PE will be required to choose an MCO at the point of the PE approval. Native American applicants are exempt from this requirement and may choose to receive their pregnancy-related services from an MCO or through FFS Medicaid. Individuals who receive services from an MCO may have Value-Added Benefits available to them that are comparable to those that are available through a full Medicaid COE. However, an MCO's ValueAdded Services are not available through FFS Medicaid or during the PE approval span. Value-Added Services are only available to applicants who are approved for ongoing coverage and are enrolled with an MCO. An applicant who has been approved for on-going coverage for COE 301 and who is in her third trimester may continue to see her existing OB/GYN provider even if that provider is not contracted with a Centennial Care MCO. The Medicaid recipient should notify her MCO's Member Services Unit about her current OB/GYN provider. An applicant who has been approved for on-going coverage through COE 301 will remain covered for two months post partum after their child is born, regardless of income or household changes. Category 301 Income Guideline 47%-250% FPL* *5% of 100% of FPL income disregard may apply Household income must be between 47% - 250% FPL 5% of 100% FPL income disregard in effect Individual may have other insurance coverage Self-attestation of pregnancy acceptable Eligible for one PE determination for each pregnancy June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 22 Children's Regular Medicaid and CHIP Coverage (Categories 400, 401, 402, 403, 420 and 421) Categories 400, 401, 402 and 403 - Regular Medicaid for Children Children 0 through 18 years of age in families with a household income up to 240% of the FPL may be eligible for regular Medicaid coverage. Regular Medicaid coverage provides children with full coverage medical services. In instances where the child has other primary health insurance in effect, Medicaid will act as supplemental coverage to help pay for services not covered by the primary carrier. Some minimal co-pays may apply for children approved for these categories. Native Americans are always exempt from co-pays. Most applicants who have been approved for Children's Medicaid PE will be required to choose an MCO at the point of the PE approval. Native American applicants are exempt from this requirement and may choose to receive their services from an MCO or through FFS. An MCO's Value-Added Services are not available through FFS Medicaid or during the PE approval span. Value-Added Services are only available to applicants who are approved for ongoing coverage and are enrolled with an MCO. If a full Medicaid application is submitted for a child, that child will be evaluated for on-going coverage. If a final eligibility approval for the applicant child is made by the HSD, the approval will result in 12 months continuous eligibility. Changes in household size or income will not impact the 12month coverage unless a change in situation makes the child otherwise ineligible for the approved COE (i.e.: move out of state, 19th birthday, etc). Regular Medicaid for Children - COEs 400, 401, 402 & 403 Category Age Income Guideline 400 401 402 403 0 - 5 years 6 - 18 years 0 - 5 years 6 - 18 years Up to 200% of the FPL Up to 138% of the FPL 200%- 240% of the FPL 138% - up to 190% FPL 5% of 100% of FPL income disregard may apply to all Children's COEs Provides full coverage Medicaid for children 0 through 18 years of age No longer eligible once age 19 has been reached PE may only be granted once every 12 months May have other forms of health insurance and still be eligible Voluntary drop of other health insurance does not affect on-going eligibility Co-pays for some services and medications may apply for non-Native American enrollees* Allowable household FPLs vary by age of child o Children ages 0-5: 0% - 240% o Children ages 6-18: 0% -190% *NOTE: Native Americans are exempt from all Medicaid co-pays June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 23 Categories 420 and 421 - Children’s Health Insurance Program (CHIP) Children 0 through 5 years of age in families with a household income up to 300% of the FPL and children 6 - 18 in families with a household income up to 240% may be eligible for Children's Health Insurance Program (CHIP) coverage. CHIP coverage provides children with full coverage medical services. Children enrolled in CHIP coverage may not have any other insurance in effect. Children who have applied for CHIP coverage will not be penalized for a voluntary drop of other coverage. Some minimal co-pays may apply. Most applicants who have been approved for CHIP PE will be required to choose an MCO at the point of the PE approval. Native American applicants are exempt from this requirement and may choose to receive their services from an MCO or through FFS Medicaid. An MCO's Value-Added Services are not available through FFS Medicaid or during the PE approval span. Value-Added Services are only available to applicants who are approved for ongoing coverage and who are enrolled with an MCO. If a full Medicaid application is submitted for a child, that child will be evaluated for on-going coverage. If a final eligibility approval for the applicant child is made by the HSD, the approval will result in 12 months continuous eligibility. Changes in household size or income will not impact the 12month coverage unless a change in situation makes the child otherwise ineligible for the approved COE (i.e.: move out of state, 19th birthday, etc). Children's Health Insurance Program (CHIP) COEs 420 & 421 Category Age Income Guideline 420 0-5 240%-up to 300% of the FPL* 421 6 - 18 190% up to 240% of the FPL* 5% of 100% of FPL income disregard may apply to CHIP COEs Provides full coverage Medicaid for children 0 through 18 years of age Eligibility ends once age of 19 has been reached PE may only be granted once every 12 months Children may not have any other form of health insurance coverage Voluntary drop of other health insurance does not affect eligibility Co-pays apply for non-Native American CHIP enrollees* Co-payment amounts may include: o $5 per doctor, dentist, outpatient, and urgent care visit o $2 per prescription o $5 per brand name prescription o $15 per emergency room visit o $25 per inpatient hospital admission o $50 for non-emergent use of the ER Allowable household FPLs vary by age of child o Children ages 0-5: 240% - 300% o Children ages 6-18: 190% - 240% *Native Americans are exempt from all Medicaid co-pays June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 24 Chapter 5 - Systems to be Utilized by Presumptive Eligibility Determiners The New Mexico Human Services Department's (HSD) Medical Assistance Division (MAD) has developed electronic systems to be used by Presumptive Eligibility Determiners (PEDs) to verify an individual's current Medicaid enrollment status, screen for Presumptive Eligibility (PE), submit PE determinations and submit applications for on-going Medicaid coverage. These systems include areas of the New Mexico Medicaid Portal (Portal) and the Your Eligibility System New Mexico (YESNM) that has been developed exclusively for use by PEDs (YESNM-PE). New Mexico Medicaid Portal The New Mexico Medicaid Portal (Portal) is an on-line public portal that can be used by Medicaid recipients or by Medicaid providers to access eligibility information. Recipients have the ability to access information about their coverage such as current enrollment status and information about their category of eligibility (COE). The Portal also has a section that is for the exclusive use of Medicaid providers, including PEDs. PEDs can use the provider section of the Portal to electronically "sign" their PE Determiner agreements, check an individual's eligibility status and submit PE determinations. The Portal is operated and maintained by the New Mexico Medicaid Fiscal Agent, Xerox, on behalf of HSD/MAD and can be accessed on line at https://nmmedicaid.acs-inc.com Your Eligibility System New Mexico for Presumptive Eligibility Determiners Beginning May, 2014, all screening for New Mexico Medicaid PE should be completed through Your Eligibility System New Mexico for PEDs (YESNM-PE). YESNM-PE has been developed for the use of certified PEDs for the express purpose of screening for and enrolling eligible individuals in PE coverage. Utilizing an internet connection, certified PEDs will enter information verbally supplied by the applicant directly into YESNM-PE. This will include such information as household size, financial information and citizenship status. This information will be used to screen the applicant for PE. If an individual is determined eligible for PE coverage, YESNM-PE will provide access to the Portal so that the PED may enter the individual's eligibility directly into the Portal. Access to Medicaid-covered services for that individual will be available immediately for their approved COE. Access to YESNM-PE screening tool and application submission portal is only available to individuals who have met the training, testing and certification requirements necessary to be a certified PED. Once all requirements are met, a PED will be allowed to register as an eligible user on both the Portal and YESNM -PE. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 25 All PEDs will be required to utilize both the Portal and YESNM-PE for PE screening and eligibility determinations unless system errors or power outages necessitate the submission of the PE notification or screening via fax. Any PED who consistently or repeatedly utilizes the paper process may be subject to disciplinary actions as outlined in the PED Corrective Action Plan standards (see page 14 of this manual). Enrolling as a Presumptive Eligibility Determiner on the Portal An individual applying to become a certified PED who has met the training and testing requirements must sign and agree to the conditions and regulations on the Presumptive Eligibility Determiner Agreement (MAD 219). This agreement should be signed electronically on the Portal. There are steps that must be followed for a PED to electronically sign the agreement form. All certified PEDs must be registered as users on the Portal. To register, the individual must first start the on-line enrollment process in the Provider section of the Portal. This process is completed once per user unless unforeseen circumstances or disenrollment by HSD of the PED for failure to comply with the PED standards and responsibilities necessitates re-registering. To begin the PED Provider Application process, the user should navigate to the Provider Section of the Portal Home page (https://nmmedicaid.acs-inc.com). The Provider section of the Portal is on the right hand side of the Portal home page. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 26 To begin the Provider Application process on the Portal, select "Provider Online Enrollment (NEW)" in the Provider section. The user will then be directed to the Provider Enrollment Application Section. A valid e-mail address is required to register as a user. This should be a valid work e-mail address, not an individual's personal e-mail address. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 27 Anyone registering on-line can start a new application or recall an application that had previously been started. Once an e-mail address has been entered, the user will be directed to an information page and must click "Accept" to move on in the registration process. On the next page, the user will be asked to choose a provider type. Choose "Presumptive Eligibility Determiner (MAD 219)." Any person who has never been a certified PED in New Mexico should choose "Initial Enrollment " Any person who had been a certified PED in New Mexico prior to October 2013 (whether currently Active or Inactive) , should select "Re-Enrollment." June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 28 Click "continue." The user will now be directed to choose a Specialty Type. Most PEDs will be certified as Specialty Type 170. These individuals will be permitted to perform PE determinations for Children and Pregnant Women. Certain entities will be certified as Specialty Type 171s. PEDs certified as Specialty Type 171s, also known as PE+ providers, will be qualified to perform June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 29 PE determinations for Children and Pregnancy as well as some other adult COEs. For more information on Specialty Types, please Chapter 3 of this manual. After the appropriate Specialty Type has been entered and the user has clicked "continue," they will be given a Provider Enrollment Reference number. This number should be saved in the event questions arise about the provider's application status. Click "Continue." Before the user is allowed to proceed with the PED registration process, they must read the Presumptive Eligibility Determiner Agreement (MAD 219) . This agreement outlines the terms, conditions and responsibilities of participation as a PED. This document should be read thoroughly and completely as applicants will be required to agree to these terms and electronically sign this document before they will be approved as a PED. For questions regarding this agreement, please contact a member of the MAD PE Program Staff at [email protected] A paper version of this agreement is included in this Chapter 15 of this manual. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 30 Click "Continue." The user will now be directed to the Provider Enrollment Applicant Information page. On this page, enter the name of the PED applicant's employer as well as the primary location where the PED will screen applicants for PE. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 31 By entering their name in the "PE Determiner's Signature" field, the PED applicant agrees to abide by the terms and conditions of the PE Determiner Agreement form. Entry of the PED applicant's name in this section will serve as the PED's electronic signature. Click "Continue." Click "Submit" to submit the provider registration application. A confirmation page notification will auto-generate after the application has been submitted. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 32 The PED applicant should print/save this confirmation page for their records. An e-mail confirmation of the provider enrollment will also be sent to the e-mail address that was previously listed on the "Provider Enrollment Application Information" page. Once the Provider Enrollment has been received by Xerox, the enrollment will be verified by MAD PE Program staff and a PED number will be issued to the PED applicant. The number will be sent to the PED by Xerox in a Provider Enrollment Welcome Packet. This number will be unique to the PED and is not transferrable to any other individual or entity. The PED will be held accountable for any and all PE determinations submitted under their PED number. Registering as a User on the Portal After the PED has received their Provider Enrollment Welcome Packet and PED number, they must also register as a user before they can utilize the Provider section of the Portal. To register, click on the "Log in" link in the Provider section of the Portal home page. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 33 Click on the "Web Registration" link on the Provider Enrollment Application Page. On the "Web Registration" page. Click on "Register Provider ID" Enter the PED Number issued by Xerox in the "Provider ID" section Enter 999999999 in the "EIN or SSN" section (PEDs are not required to provide a social security number) Enter the zip code of the employer's location in the "Location Zip Code" section. This should be the main location where the PED physically works most of the time. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 34 Create a user ID, then enter name and contact information. Click “Continue.” June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 35 Review the information entered. Be sure to write down or note the User Id. Click “Submit.” Review the Confirmation page and click “Log In.” A temporary password will be sent to the email address used during registration. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 36 After becoming a certified PED and completing the Portal registration process, the PED's access to the Portal will be used to check an individual's eligibility status and enter an applicant's PE approval. PEDs can also update their own information on the Portal if they have a change of employers or in contact information. When logging in to the Portal, PEDs will be required to have their User ID, Provider ID (PED number) and their password for each session log in. All steps necessary in checking an individual's eligibility status and the entry of a applicant's PE will be outlined in Chapter 6, "Electronic Screening for Presumptive Eligibility, "of this manual. Registering as a User on YESNM-PE PEDs who have been issued a PED Number will be required to use YESNM-PE to screen applicants for potential PE coverage. This screening tool is for the exclusive use of PEDs. It will allow a PED to submit information required to make an accurate PE determination. PEDs can also submit an application for ongoing Medicaid coverage on YESNM-PE if the applicant wishes to do so. If an ongoing application is submitted on YESNM-PE, the PED will have access to check the status of that application. To access YESNM-PE, go to www.yes.state.nm.us/jsp/access/myAccess/PELogin.jsp Certified PEDs will have the information that was supplied at the time of their PED registration automatically transferred to YESNM-PE. All PE screenings will be linked to the PED's assigned PED number. Each PED is responsible for any and all PE screenings and approvals and applications submitted for ongoing coverage submitted under their assigned PED number. To access YESNM-PE, each PED must register as a user. This requires creating a unique User ID name and password. This ID and password is required to be entered at each session login. To begin the user registration process on YESNM-PE, you must navigate to the area of YESNM designed exclusively for the use of PEDs. To access this page go to https://www.yes.state.nm.us/jsp/access/myAccess/PELogin.jsp June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 37 PEDs must then create a User ID and Password. To create a YESNM-PE User ID and Password, the PED must have their PED number. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 38 June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 39 Chapter 6 - Electronic Screening for Presumptive Eligibility Most people who are currently enrolled in a Medicaid category of eligibility (COE) are not eligible for Presumptive Eligibility (PE) coverage. To ensure that the applicant is not a current Medicaid recipient, a Presumptive Eligibility Determiner (PED) is required to check an applicant's current Medicaid eligibility status on the New Mexico Medicaid Portal (Portal). Any individual who is currently enrolled in Medicaid will appear as enrolled in the Portal along with their current COE. All PEDs must utilize the section of the Your Eligibility System New Mexico (YESNM) system designed for the exclusive use of PEDs (YESNM-PE) to screen applicants for PE. YESNM-PE is only available for use by those individuals who have met the certification requirements of a PED. PEDs must submit all PE approvals on the Portal on the day of the PE approval. Screening for and enrolling individuals in PE coverage can only be done by certified PEDs. PEDs are required to submit the information used to determine an individual eligible for PE to the New Mexico Human Services Department's (HSD) Medical Assistance Division (MAD) for auditing purposes. After screening an applicant for PE, the PED must also ask the applicant if they wish to be evaluated for ongoing Medicaid coverage. If the applicant chooses to be evaluated for ongoing coverage, the PED will indicate the individual's choice and submit the information to HSD via YESNM-PE. This information will be used to populate an on-line application for Medicaid eligibility, which will be evaluated for ongoing Medicaid eligibility. PE coverage will terminate for any individual who has been approved for PE but who does not submit an application for ongoing Medicaid coverage on the last day of the month following their PE approval. Any individual approved for PE who submits a Medicaid application by the last day of the month following the month in which his/her PE was approved will have PE coverage in effect until the day that the final application determination has been made. Failure of an applicant to submit any needed information requested by HSD to process the application for ongoing coverage in the timeframe requested will be grounds for a denial, and the PE span will close. Checking Applicant Eligibility on the Portal To check an applicant's enrollment status, log-on to the Portal at https://nmmedicaid.acs-inc.com. Click "Log-in to" in the Provider Section on the right hand side of the page. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 40 After log-in, click on "Inquiries" Then, click on "Eligibility." June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 41 To search an applicant's eligibility, multiple search parameters may be utilized. At least one of the search parameters is required. A beginning date of service is also a required field. Generally, the PED should enter a date of 12-months prior to the date that the applicant is being screened for a presumptive eligibility determination. If retroactive coverage is required, a full Medicaid application must be submitted. Retroactive coverage is not available through PE. If an applicant has had a PE determination or is currently enrolled in Medicaid coverage, they will be listed as "not eligible on the requested date(s) of service." This means that the individual is not eligible for PE at this time. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 42 Most individuals who are enrolled in a current Medicaid COE are not eligible for Medicaid PE. One exception to this is women currently enrolled in Family Planning Medicaid (COE 29). COE 29 has a very limited benefit package. If a woman becomes pregnant while enrolled in COE 29, she may be granted PE for Pregnancy coverage (COEs 300 and 301). During the PE eligibility span, ONLY ambulatory prenatal care is covered. This includes amniocentesis, sonograms, lab work, pregnancy-related prescriptions, pre-decision counseling, and miscarriages. Delivery services will not be covered unless an application for on-going coverage has been submitted and the applicant has been determined eligible for the on-going coverage. Any applicant who is not a current Medicaid recipient or a pregnant woman who is currently enrolled in COE 29, may be screened for PE. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 43 The PED should proceed to YESNM-PE to begin the applicant screening process. Screening for Presumptive Eligibility on YESNM-PE YESNM-PE has been developed for the use of PEDs to walk them through each step of the PE screening process. The PED will ask the applicant each question and will enter it in to the screening tool on the applicant's behalf. PEDs are required to enter each answer as it is supplied to them by the applicant. At the end of the screening tool process, the applicant will have to affirm that all information they have supplied to the PED is accurate and correct. PEDs must affirm that the information listed in the screening tool is the information that has been supplied by the applicant. Once the applicant's relevant household information has been gathered, the PE Determination Results page will be displayed. The PED will then utilize a link on PE Determination Results page to enter the PE on the Portal for eligible individuals. Once entered, the PED will return to the PE Determination Results Page where they can print the result page for the applicant. Applicants will then be given the option to submit the information gathered for the screening to HSD for an ongoing Medicaid application determination. An applicant's PE approval will not be affected if they choose not to submit an application for ongoing eligibility. However, applicants should be notified that their PE coverage would end on the last day of the month following the PE approval unless an application for ongoing eligibility has been received by HSD by that date. To begin screening for PE coverage, log-in to YESNM-PE at https://www.yes.state.nm.us/jsp/access/myAccess/PELogin.jsp June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 44 The PED will then be directed to the PED landing page. From this page, the PED may begin to screen a new applicant for PE or may recall a screening or application that has been started by the PED for the applicant. To begin a new screening, click "Screen for Presumptive Eligibility/submit application" and then click "Next." June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 45 The PED will then be directed to an informational page. This page explains that YESNM-PE is to screen for and apply for PE. PE is only available for specific Medicaid COEs. If the individual applying with wishes to apply for COEs that are not available through PE, they may do so through the application process on this site but they will not receive a possible eligibility result until the application has been processed by HSD. Any individual who wishes to apply for other New Mexico Public Assistance Programs, such as Food Assistance (Supplemental Nutrition Assistance Program - or SNAP), Energy Assistance (Low-Income Home Energy Assistance Program - or LIHEAP) or Cash Assistance should do so using the public access web application at www.Yes.state.nm.us or at their local HSD/ISD office. Application submission for these programs is not available through YESNM-PE. To proceed to the screening tool, click "Next." June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 46 The PED will be directed to the applicant data collection screens where information on the applicant and household members will be entered. All fields in YESNM-PE that are marked with a red asterisk (*) are required fields and must be completed before the PED can advance to the next screen. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 47 Any applicant who has a person that has been designated to make decisions on behalf of the applicant may indicate that in the "Authorized Representative" section of YESNM-PE. PEDs should never be listed as an applicant's "Authorized Representative." Next, the PED will be required to enter information about each household member and their relationship to the applicant. All household members should be listed in the household member section so that the household size may be accurately evaluated. Any individual in the household who does not wish to be screened for or apply for PE coverage should be still be listed as a household June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 48 member. To be screened for or apply for Medical Assistance, the PED must check on the "Medical Assistance" box in the Program Selection section of each individual's information screen. Any household member that has medical bills that were incurred within the past three months may be eligible for retroactive coverage to help pay those bills. This coverage must be requested in the Program Selection section as well. Retroactive Medicaid coverage is not available with a PE approval. Any individual who wishes to apply for retroactive coverage must do so by submitting an application for ongoing coverage. Any individual applying for PE or ongoing Medicaid coverage must meet U.S. Citizenship requirements. As a condition of PE, applicants are not required to supply a Social Security Number (SSN) with their PE application. However, any applicant wishes to apply for ongoing Medicaid eligibility may be required to supply their SSN before their application for ongoing coverage is processed. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 49 Race and Ethnicity information are asked of applicants but are not required fields and are not a factor in determining PE. All applicants are required to be a resident of New Mexico to receive New Mexico Medicaid benefits. Any household member(s) who is pregnant should indicate this on the "Other Information" section as it could affect the household size in determining eligibility. A verified due date of the pregnancy is not required but should be entered if known. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 50 After all household members have been added, the PED will be required to note the relationships of the members. More information may be asked about children in the home and their relationships to the adults listed in the household. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 51 Any parent who does not live with their child(ren) should be listed in the "More About Parents" section if the information is known. This information is not required as a condition of a PE determination. Applicants should be asked if household members are receiving benefits from another state or if each of the household members has other Medical Coverage as this may affect Medicaid eligibility. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 52 Any household member who has other medical coverage should have it noted as this may have an effect on the individual's PE and ongoing Medicaid eligibility. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 53 The PED will then be directed to a Household Summary Page. This should be reviewed by the PED with the applicant to ensure accuracy. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 54 The PED will then gather information regarding household income. This information will be used to help determine financial eligibility. After income has been entered, the "Job Income Summary" page should be reviewed for accuracy. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 55 Any additional information that may be relevant to a PE or ongoing Medicaid application determination may be entered by the PED in the "Additional Information" screen. All information that has been entered will be used to display the PE results on the "Presumptive Eligibility Results" page. This page will list any household members who may be granted PE with the COE for which they are eligible. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 56 Any individual may be granted PE if he or she: Has been determined eligible for PE (through the YESNM-PE or through a manual process) Has not had a PE granted in the past 12 months or has not had a previous PE granted for the same pregnancy Is not currently enrolled in New Mexico Medicaid (unless they become pregnant while enrolled in Family Planning coverage) Any individual who has been determined presumptively eligible for Medicaid coverage and who wishes to accept the PE coverage must have their PE approval submitted to Xerox. Any applicant who has provided a SSN on their PE application should have their PE approval submitted on the Portal. Any applicant who has not supplied his or her SSN, must have PE submitted via fax. For information on the manual determination and paper submission of PE, see Chapters 7 - 12 of this manual. In most cases, PE approvals entered on the Portal will appear within minutes of the PE entry. Providers who view applicant eligibility will see these results in real time. PE approvals submitted via fax may June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 57 take up to 2 business days (Monday-Friday) to appear in the Portal after the approval has been received by Xerox. This means that the applicant may not appear as "eligible" in the Portal for a Medicaid COE for at least two business days after the PE approval has been received by Xerox. To enter PE for any applicant who has been determined eligible, the PED should proceed to the Portal. Access to the Portal is available by clicking the "Click Here" link on the "Presumptive Eligibility Results" page. Entering a Presumptive Eligibility Approval in the Portal After clicking the link on the YESNM-PE Results Page, the PED will be directed to the Provider Log-in Page on the Portal where they will login with their User Name, Password and their Provider ID (PED number). After a successful login, the PED may enter the individual's PE span in the Portal. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 58 The PED must first select the COE to which the individual is being enrolled. Only Medicaid categories that are eligible for PE coverage are listed. Select the appropriate COE from the list. Complete the remainder of the information on the Presumptive Eligibility Submission Form. All fields on the form are required for the PE submission. Although the race code entry is a required field on this form, it is not required for PE. Any individual who does not wish to have a race code indicated should be listed as "Unknown." Native Americans eligible for PE who wish to be exempt from Managed Care should be identified as Native American so that they are not automatically enrolled with an MCO. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 59 Once all fields have been entered, click "Verify." If the verification step indicates that the applicant may be ineligible for PE coverage, the PE may not be entered on the Portal. PEDs who believe this message may have been received in error should contact Xerox by phone at 800-705-4452 or 505-246-0710. If the verification indicates that the individual is eligible for a PE approval, more information will be requested so that the new PE span may be entered. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 60 An MCO choice should be made by the applicant at the time of their PE approval entry. If one is not made, they will be auto-enrolled with an MCO. Native Americans who have been listed as "Native American" on the race code field will not be auto-enrolled with an MCO. Native Americans will be enrolled with an MCO only if an MCO choice has been made for the applicant. Click "Save" after all required fields have been completed. The PED will receive a confirmation of the successful PE submission. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 61 After a successful PE submission, the PED should exit the Portal and return to YESNM-PE. To print the PE Granted" information page for the applicants, the PED must first indicate which household members were granted PE through the Portal. This is a required field and "Yes" or "No" must be selected for each household member listed. The PED should also ask the applicant if they wish to apply for ongoing Medicaid coverage. This is a required field for each household application screened for PE on YESNM-PE. Any applicant who chooses to have their application submitted and evaluated for ongoing Medicaid coverage must be supplied with the "Applicant's Rights & Responsibilities" in Chapter 15 of this manual. All applicants should be asked if they wish to register to vote and asked if they wish to provide an email address where a survey about their enrollment experience may be sent. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 62 To submit the application, both the applicant and the PED must agree to sign the application electronically. All applicants must agree to the statements in the electronic signature section of the application. This information will also be printed for the applicant in the "Print My Applications" section to follow. A PED's electronic signature in this section affirms that they have supplied the applicant with all required information in the electronic signature process. Instant notification will let the PED know where the Medicaid application has been routed for processing. PEDs will be given a tracking number for the application submission. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 63 From this page, the PED will also print the Voter registration form (if the applicant has opted to register), print the application for ongoing coverage and print the PE Screening results page. Applicants should be given copies of all print outs for their records. A PED may submit documents that may be needed to determine ongoing eligibility for an applicant by clicking "View and Submit Types of Proof" in the "Your next Steps" section and clicking "Next." PEDs will be walked through the document upload process. Once an application has been submitted, the applicant's PE coverage will remain in effect until a final Medicaid determination has been made on the application. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 64 Chapter 7 - Manual Screening for Presumptive Eligibility In any instance, such as lack of internet connectivity or power or system outages, in which the Presumptive Eligibility Determiner (PED) is unable to screen an applicant for Presumptive Eligibility (PE) on the Your Eligibility System New Mexico (YESNM) designed for PEDs (YESNM-PE), the PED will be required to calculate the PE determination manually. To complete the manual submission of a PE application, a PED must calculate the applicant's eligibility. The PED must evaluate household size, income and all other factors involved in an accurate eligibility determination. All information required for a determination must be asked of the applicant. PEDs will have determination and approval results submitted manually or through YESNM-PE held to the same performance standards required as a condition of the individual's participation as PEDs. To manually screen an individual for PE, the PED should utilize the Streamlined Medicaid Application (MAD 100) or the Presumptive Eligibility Applicant Information Form (MAD 011) to compile and determine the applicant's household information and financial eligibility. They should also utilize the Household Comp and Income Calculation Form (MAD 008) to determine the applicant's financial eligibility. After screening and determining the applicant PE eligible, the PED must submit the PE approval to Xerox, the New Mexico Medicaid Fiscal Agent. If the PED is unable to submit the PE approval on the Portal, they must do so via fax. All paper PE approvals must be submitted on the Presumptive Eligibility Authorization Form (MAD 070; Rev 3/6/14). This form is available for download on the Portal at www.nmmedicaid.acs-inc.com. In most cases, PE approvals entered on the Portal will appear within minutes of the PE entry. Providers who view applicant eligibility will see these results in real time. PE approvals submitted via fax may take up to 2 business days (Monday-Friday) to appear in the Portal after the approval has been received by Xerox. This means that the applicant may not appear as "eligible" in the Portal for a Medicaid COE for at least two business days after the PE approval has been received by Xerox. All documents used to make manual PE determinations must be submitted to HSD/MAD PE Program Staff via e-mail at [email protected] or by fax at 505-827-7200. Any PE applicant who has been determined presumptively eligible must also be asked if they wish to submit an application for ongoing Medicaid coverage. Any applicant who elects to apply for ongoing Medicaid coverage must be supplied with the Medicaid-Only Application (MAD 100; Rev 1/21/14). This application should be signed by the applicant and submitted by the PED to HSD within 48 hours of the PE submission. All MAD 100 applications submitted by PEDs on behalf of an applicant must be submitted to the Human Services Department's (HSD) Central ASPEN Scanning Area (CASA). All accompanying documents that may help with determining the applicant's ongoing Medicaid eligibility should be submitted along with the application. Applications submitted to CASA will be electronically routed to an HSD office for processing. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 65 Applications may be submitted to CASA by mail or fax. Central ASPEN Scanning Area PO BOX 830 Bernalillo, NM 87004 Phone: 800-283-4465 E-Fax: 855-804-8960 June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 66 Chapter 8 - Completing Manual Forms Beginning April, 2014, the Presumptive Eligibility (PE) process in New Mexico will be, primarily, an electronic one. Presumptive Eligibility Determiners (PEDs) will be required to use the electronic processes at all times possible. In the rare instances where PE determinations, approvals and submissions must be completed on paper, they may only be submitted using acceptable paper forms developed by the New Mexico Human Services Department's (HSD) Medical Assistance Division (MAD). Updates and revisions to forms will be made available - via e-mail, postal delivery or through webaccessed downloads to all active PEDs. Submission of out-dated or obsolete forms may delay or negate the acceptance, processing or entry of a PE determination. Before beginning the process of determining presumptive eligibility, the PED is required to check the current Medicaid enrollment status of all applicants. Applicants who are currently enrolled in most categories of Medicaid eligibility or those that have had a PE determi nation within the past 12 months are not eligible for PE coverage. When inquiry ability is not available on the New Mexico Medicaid Portal (Portal), PEDs must call the Medicaid Call Center's Automatic Voice Response System (AVRS) at 800-820-6901 to check an applicant's current enrollment status. It is the responsibility of PEDs to verify the eligibility of all PE applicants. Any PE approvals that have been submitted without proper prior verification of an applicant's eligibility status will be subject to PED audit and performance standards and may result in the revocation of the PED's PED number. Before screening for PE, the PED should ask the applicant if they wish to apply for PE and ongoing Medicaid coverage. If the applicant wishes to do both, the PED should use the New Mexico MedicaidOnly Application (MAD 100) to gather information for the PE screening and for the application for ongoing coverage. Completing the MAD 100 for Presumptive Eligibility When using the information on the MAD 100 to screen for PE, not all fields on the application are required to be completed to determine PE. However, any fields left blank that may be needed to determine ongoing Medicaid eligibility may be asked of the applicant at a later date by HSD staff. Therefore, applicants wishing to be evaluated for ongoing coverage should be encouraged to complete all fields on the MAD 100. To properly screen for PE, certain information must be gathered for the applicant and all applicable household members. This same information is needed whether the determination is made through an electronic or manual process. To begin the screening process, the PED should first ask the applicant information that will help determine household size and income. To complete this on the MAD 100, the information in the sections below is required, at the very least, for an accurate PE-only determination. On Page 2 of the MAD 100, the highlighted fields should be completed: June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 67 On page 3, Social Security Numbers (SSN) and Race & Ethnicity are not required fields. However, SSNs will be required when seeking ongoing coverage. Any Native American who wishes to remain exempt from Managed Care may be auto-assigned to a Managed Care Organization (MCO) if their Race is not known. If this occurs, the applicant may contact their local HSD Income Support Division (ISD) office to have their race code corrected and the enrollment with the MCO deleted. Page 3 also has required questions that relate to the tax filing status of household members. This will help to determine the financial eligibility of household members based on tax filer status. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 68 In section 5, only the pregnancy question is relevant to a PE determination screening. Section 6 must be completed so household income can be accurately evaluated. Other types of income may count towards a household's income and should be noted. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 69 Any household members with existing health coverage, including private insurance, Medicaid or Medicare, should be listed in the section below. Any applicant who is requesting retroactive coverage for unpaid medical bills for the past three months should list that information in this section. However, PE coverage will not be granted retroactively. Only approved ongoing Medicaid applications may be eligible for retroactive coverage. An MCO choice should be made at the time of application whether applying for PE or for ongoing Medicaid coverage. Native Americans may choose to be exempt from Managed Care. The person applying on behalf of the household members listed should read the information below and is required to sign the application. All information supplied will be used to evaluate the person(s) listed on the application who are seeking assistance for PE or for ongoing Medicaid coverage. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 70 After required fields have been completed and the PED is satisfied Citizenship and residency requirements have been met, financial eligibility must be determined. See Chapter 10 - "Manually Calculating Medicaid Financial Eligibility." Completing the MAD 011 for Presumptive Eligibility Any person or household who chooses to not apply for ongoing coverage at the time of initial PE screening may be asked the questions needed to determine PE on a separate form. This form will be submitted to the MAD PE Program Staff for auditing purposes but will not be evaluated for ongoing Medicaid eligibility. The household and financial information needed to determine PE should be gathered on the Presumptive Eligibility (PE) Applicant Information form (MAD 011) To complete the MAD 011, the PED must ask the applicant the information listed on the form. The person who is supplying the information, whether applying for him/herself or for some or all family members, is responsible for the accuracy of the information supplied. When possible, all information listed for each family member residing in the household should be completed. SSNs are not required to be supplied as a condition of PE. However, all PE applicants are required to meet Citizenship requirements. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 71 After applicant and household information has been gathered and the PED is satisfied that household members have been identified and Citizenship and residency requirements have been met, financial eligibility must be determined. See Chapter 10 - "Manually Calculating Medicaid Financial Eligibility." June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 72 Chapter 9 - Manual Calculation of Household Size Household size is one of the factors used to help determine Medicaid Eligibility. This is true for both Presumptive Eligibility (PE) and applications ongoing Medicaid coverage. When calculating household size, Presumptive Eligibility Determiners (PEDs) should ensure that all household members are listed on the Streamlined Medicaid Application (MAD 100) or on the Presumptive Eligibility Applicant Information Form (MAD 011). Household members listed will be used in determining the Household Composition. However, the "Assistance Unit" for that household only includes the individuals who are applying for benefits. Each individual in the Assistance Unit is evaluated for a budget group individually. Countable income will be based on which members are included in the budget group at an individual level. All individuals listed on the application are evaluated according to their living arrangement to determine if they can be included in an assistance group or budget group. In some cases, an individual can be counted as being in the home even if they are physically absent from the home. These individuals are considered to be "extended living." Extended living in the home includes: (1) attending college or boarding school; (2) receiving treatment in a title XIX Medicaid facility (including institutionalized when meeting a nursing facility (NF) level of care (LOC) and intermediate care facilities for the mentally retarded (ICF-MRs); (3) emergency absences: an individual absent from the home due to an emergency, who is expected to return to the household, continues to be a member of the household; (4) foster care placements: a child removed from the home by a child protective services agency (tribal, bureau of Indian affairs, or children, youth and families department) will be considered to be living in the home until the adjudicatory hearing; if the adjudicatory hearing results in custody being granted to some other entity, the child will be removed from the assistance unit and budget group; (5) a stay in a detention center: (a) regardless of adjudication status the individual continues to be a member of the household but will not be Medicaid eligible; (b) once an adjudicated individual leaves the detention center to receive inpatient services in a medical institution, the individual may be eligible during treatment if all other criteria are met; eligibility ceases to exist when the individual returns to the detention center. Extended living in the home also includes: (1) residential treatment centers; (2) group homes; and (3) free-standing psychiatric hospitals. To be included in the assistance unit of a Parent/Caretaker, a child must be living, or considered to be living, in the home of: (1) a biological or adoptive or step parent (there is a presumption that a child born to a married woman is the child of the husband); or (2) a specified relative who: June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 73 (a) is related within the fifth degree of relationship by blood, marriage or adoption, as determined by New Mexico statute Chapter 45 - Uniform Probate Code; a relationship based upon marriage, such as "in-law" or "step" relationships, continues to exist following the dissolution of the marriage by divorce or death; and (b) assumes responsibility for the day-to-day care and control of the child; the determination of whether an individual functions as the specified relative shall be made by the specified relative unless other information known to the worker clearly indicates otherwise; (3) a child considered to be living in the home: a child is considered to be part of the assistance unit and budget group as evidenced by the child's customary physical presence in the home; if a child is living in more than one household, the following applies: (a) the custodial parent is the parent with whom the child lives the greater number of nights; or (b) if the child spends equal amounts of time with each household, the child shall be considered to be living in the household of the parent with the higher MAGI. [8.291.430.13 NMAC - Rp, 8.291.430.13 NMAC, 1-1-14] 8.291.430.14 BASIS FOR DEFINING THE ASSISTANCE UNIT AND BUDGET GROUPS: At the time of application, an applicant or recipient and the department shall identify everyone who is to be considered for inclusion in an assistance unit and budget group. The composition of the assistance unit and budget group is based on the following factors: A. Assistance group: the assistance unit includes an individual who applies and who is determined eligible under one of the categories of eligibility outlined in 8.291.400.10 NMAC. B. Budget group: the budget group consists of the following types and will be established on an individual basis: (1) Tax filer(s): households that submit an application where an individual intends to file for federal taxes or will be claimed as a dependent on federal income taxes for the current year. (a) The budget group will consist of individuals who are listed on the application as the taxpayer and tax dependents. (b) If there are multiple taxpayers listed on a single application, the budget group(s) will be established based on who the taxpayer intends to claim as a dependent (including the taxpayer). Only the taxpayer and dependents listed on the application will be considered as part of the budget group. (c) In the case of a married couple living together, each spouse will be included in the household of the other spouse, regardless of whether they expect to file a joint tax return, a separate tax return or whether one spouse expects to be claimed as a tax dependent by the other spouse. (d) Exceptions to tax filer rules: the following individuals will be treated as nonfilers: (i) individuals other than a spouse or a biological, adopted, or step child who expect to be claimed as a tax dependent by another taxpayer outside of the household; (ii) individuals under 19 who expect to be claimed by one parent as a tax dependent and are living with both parents but whose parents do not expect to file a joint tax return; and June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 74 (iii) individuals under 19 who expect to be claimed as a tax dependent by a non-custodial parent. (2) Non-filer(s) are individuals applying for Medicaid who have not filed for taxes, do not intend to file for federal taxes, have not been claimed as a dependent on taxes in the current year or who meet an exception to tax filer rules in Paragraph (1) above. The following individuals may be included in a budget group when evaluating eligibility for an ACA related Medicaid eligibility category, provided that they live together: (a) the individual; (b) the individual’s spouse; (c) parents/step-parents; or (d) the individual’s biological, adopted and step children under the age of 19. (3) Households may submit an application that includes both filer and non-filers as defined in Subsections A and B above. The budget group(s) will be organized using the filer and nonfiler concepts, and eligibility will be established on an individual basis. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 75 Chapter 10 - Manually Calculating Medicaid Financial Eligibility To be eligible for Medicaid coverage, individuals must meet certain eligibility guidelines. Some of these factors could include citizenship, identity, age and medical factors. All categories of eligibility (COE) are based on income guidelines. Whether an applicant is being screened for Presumptive Eligibility (PE) or ongoing Medicaid coverage, income will be used in the eligibility determination. The income guidelines that help determine eligibility are based on the Federal Poverty Levels (FPL) as set by the United States Health and Human Services Department. FPLs are based on household size and total income. Medicaid eligibility FPLs change April 1 of each year. The current FPLs for Medicaid Eligibility that go into effect April 1, 2014 are below: In the past, a household's FPL was determined using a formula of family size, type of income received and deductions that the household might receive for some income. And, while that still holds true, the base income that is counted is calculated using an individual's Modified Adjusted Gross Income (MAGI). MAGI is a methodology for how income is counted and how household composition and family size are determined. MAGI is based on Federal Tax rules for determining adjusted gross income (with some modification). It is not a number on a tax form. In MAGI, there are no asset tests or income disregards other than those that may exist for some specific Medicaid COEs). Certain types of income are categorized as "Countable" in calculating MAGI. Types of income categorized as Countable include: Taxable wages/salary (before taxes taken out). Pre-tax contributions to dependent care accounts, health insurance premiums, flexible spending accounts, retirement accounts and commuter expenses are NOT included as income Self-employment (profit once business expenses are paid) Social Security benefits Unemployment benefits June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 76 Alimony received Most retirement benefits Interest (including tax-exempt interest) Net capital gains (profit after subtracting capital losses) Most investment income (profit after subtracting costs) Other taxable income such as canceled debts, court awards, jury duty pay not given to an employer, cash support and gambling, prizes or awards Foreign earned income Other types of income are categorized as Non Countable Income. These include: Supplemental Security Income (SSI) Child Support Received Veteran's benefits Worker's compensation payments Proceeds from life insurance, accident insurance or health insurance Federal tax credits and Federal income tax refunds Gifts and loans Inheritances Temporary Assistance to Needy Families (TANF) and other government cash assistance Although standard deductions do not apply, some exemptions exist for income received by a tax dependent in a household. These exemptions include the income of most children and tax dependents of the household who are not required to file a federal tax return. In most cases, a child's income does not count towards household income of his or her parent unless the child is required to file taxes. The child's income will not be counted in evaluating the child's eligibility, the eligibility of other household members or in the case of adult children who are tax dependents of their parent. However, if the child does not live with his or her parent, the child’s income will count for his or her own eligibility and the eligibility of the child’s other household members, such as siblings, regardless of whether the child’s income is high enough to require a tax return to be filed. Exception for other Tax Dependents Include income of a tax dependent in household income only if the tax dependent is expected to be required to file a tax return. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 77 Income of a tax dependent is included in household income of any household where both that tax dependent and his/her claiming tax filer are present, only if the tax dependent is expected to be required to file a tax return. o Applies to adult children who are tax dependents of their parent. This exception does not apply to a tax dependent’s income when determining the household income of any household where the tax dependent’s parent and the tax dependent’s claiming tax filer are not part of that household. In such cases, the tax dependent’s income counts toward household income regardless of whether or not he/she is expected to be required to file a tax return. Deductions may apply to the calculation of income for some individuals at certain income levels. A disregard of 5% of 100% of the current FPL, according to the individual’s budget group size, will be given according to some Affordable Care Act (ACA) COEs. Categories that may be eligible for this income disregard include some children's categories, pregnancy, parent/caretakers and other adults. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 78 Chapter 11 - Submitting a Presumptive Eligibility Approval by Fax After screening and determining that an applicant is eligible for Presumptive Eligibility (PE), the Presumptive Eligibility Determiner (PED) must submit the PE approval to Xerox, the New Mexico Medicaid Fiscal Agent, through the New Mexico Medicaid Portal (Portal). If the PED is unable to submit the PE approval on the Portal, they must do so via fax. All paper PE approvals must be submitted on the Presumptive Eligibility Approval Form (MAD 070; Rev 3/6/14). This form is available for download on the Portal at www.nmmedicaid.acs-inc.com. Completing a MAD 070 for Submission of a Presumptive Eligibility Approval The first step is to complete the PED Name and fax number in the upper right hand corner of the form. Next, the PED should list the information for each person to whom PE is being granted. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 79 A Managed Care Organization (MCO) choice should be made for each person being granted PE. If the applicant has no choice "None" may be entered. However they will be auto-assigned to an MCO unless they have indicated that they are Native American in the Race field. The PED should also list the category of eligibility (COE) that is being granted to the person listed as eligible. Only one choice can be made and should be appropriate to the COE that the individual has been determined eligible. The Eligibility Begin Date is the date that the individual has been approved for PE and the End Date will be the last day of the following month the of the PE unless an application for on-going eligibility has been received by that date. If an application is submitted by the end date, the PE coverage will remain in effect until a final determination for the ongoing coverage has been made. Any PE determinations that do not meet the age and eligibility restrictions for the specific COE granted may be rejected by Xerox. If a PE approval is rejected, Xerox will e-mail the PED with a notification that the PE submission has not been accepted. Each individual being granted PE should be listed on a separate line of the form. Once completed, the form must be faxed to Xerox. PE approvals submitted via fax may take up to 2 business days (Monday-Friday) after they have been received by Xerox to be entered in the Portal. The applicant will not appear as "eligible" in the Portal until the manual entry has occurred. All PEs granted must be submitted to Xerox on the date of approval. And all documentation related to the approval must be submitted the MAD PE Program Staff within 24 hours of the PE approval. Manual submissions must include the Presumptive Eligibility Applicant Information Form (MAD 011) OR the Medicaid-Only Application (MAD 100; Rev Date 1/21/14), the Household Comp and Income Calculation Worksheet (MAD 008) and the Presumptive Eligibility Authorization From (MAD 070). June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 80 Chapter 12 - Submitting Paper Applications or Information Sheets All information gathered by a Presumptive Eligibility Determiner (PED) to determine Presumptive Eligibility (PE) should be submitted to the Human Services Department (HSD). If the applicant has elected to apply for ongoing coverage, the information will be used to make a final eligibility determination. If the PE applicant has chosen not to apply for ongoing coverage, the information will be used to evaluate the accuracy of the PED's PE determination. Submitting Applications for Ongoing Medicaid Coverage Applicants who have elected to apply for ongoing Medicaid coverage should have completed the fields on the Medicaid-Only Application (MAD 100; Rev Date 1/21/14) needed to determine their Presumptive Eligibility (PE) approval or denial. This application will also be used to determine eligibility for ongoing coverage. Applicants who have been determined not eligible for PE may still submit an application for ongoing coverage. Signed MAD 100 applications should be forwarded to the Human Services Department's (HSD) Central ASPEN Scanning Area (CASA). Any fields that have been left blank on the application that may be needed to determine ongoing Medicaid eligibility may be asked of the applicant by HSD staff. Any documentation that an applicant has supplied at the time of their PE application should be submitted as well. This can include any proofs of income, citizenship, identity, etc. PEDs should also include the Household Comp and Income Calculation Worksheet (MAD 008) used to make the PE determination. Applications and documentation may be mailed or faxed to CASA within two days of the PE determination. CASA will index the application and documentation and electronically route all items to be processed by HSD staff. If more information is needed from the applicant to make a final eligibility determination, HSD will request it. Failure of an applicant to submit any information requested by HSD that is needed to make a final eligibility determination will be grounds for a denial. Once processed, the applicant will receive a final eligibility determination notice by mail. CASA Contact Information Central ASPEN Scanning Area PO BOX 830 Bernalillo, NM 87004 Phone: 800-283-4465 E-Fax: 855-804-8960 Submitting Presumptive Eligibility Applicant Information Sheets Applicants who do not wish to apply for ongoing coverage will not have their information evaluated for ongoing Medicaid eligibility. However, the PED must submit the information used to determine the PE applicant's PE approval or denial to HSD for auditing purposes. Information must be submitted by mail or faxed to the HSD/MAD PE Program Staff. Information should include the Presumptive Eligibility June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 81 Applicant Information Form (Mad 011) and the Household Comp and Income Calculation Worksheet (MAD 008) used to make the PE determination. HSD/MAD PE Program Staff will evaluate the accuracy of the PE determination. PEDs are held to the same Performance Standards for PE determinations, whether the determination is made electronically or manually and are responsible for the accuracy of all determinations. PE Program Staff Contact Information HSD/Medical Assistance Division Communication and Education Bureau PE Program Staff PO BOX 2348 Santa Fe, NM 87504-2348 Phone: 505-827-7717 FAX: 505-827-7200 June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 82 Chapter 13 - Documents that May Be Needed for Ongoing Medicaid Eligibility for all Medicaid categories of eligibility (COE) is based on citizenship/immigration status, residency, income and other factors. The income guidelines that are used to determine Medicaid eligibility are based on the Federal Poverty Levels (FPL) as set by the United States Health and Human Services Department. FPLs are set based on household size and total income. To be determined eligible for Medicaid coverage, verifications may be needed to prove an applicant's citizenship or immigration status and income eligibility. The New Mexico Human Services Department (HSD) will make every effort to use data sources to obtain all necessary verifications. If HSD is unable to obtain these verifications, proof of the information will be requested from the applicant. Applicants will be notified by mail of any verification required. They will also be given a timeframe in which the information must be supplied. Failure to provide the information in the timeframe requested may result in a denial of the Medicaid application. Documents Used to Prove Citizenship, Immigration Status and Identity Medicaid applicants must meet citizenship and identity requirements to be determined eligible for coverage. U.S. citizens are Medicaid eligible, as are legal permanent residents and legal immigrants. A legal immigrant is a non-U.S. citizen who has permission to live and/or work in the U.S. as demonstrated by providing documents issued by the U.S. Citizenship and Immigration Services. Lawfully residing children and pregnant women, including those who are in nonimmigrant status, can be Medicaid eligible. In New Mexico, individuals may also be required to show proof of identity to receive Medicaid services. Certain documents are acceptable to provide these necessary verifications. Some documents are acceptable proof of both citizenship and identity while others are only acceptable as citizenship OR identity. For documents that prove only citizenship or identity, one of each type is required. Some of the most common proofs of citizenship and identity are listed below. Type of Proof Certificate of Indian Blood (CIB) or Certificate of Degree of Indian Blood (CDIB) Certificate of Naturalization (DHS Form N-550 or N570) Certificate of U.S. Citizenship (DHS Form N-56- 0r N561) Federal, State or Local Government-Issued Identification Card (w/ photo) Military Dependent's Identification Card NM Department of Health Birth Record Web Portal Verification School-Issued Identity Card (w/Photo) State-Issued Driver's License (Current & Valid w/Photo) State-Issued Identity Card (Current & Valid w/Photo) U.S. Birth Certificate U.S. Passport (Expired or Unexpired) June, 2014 Citizenship NM HSD/MAD - PE & PE+ Training Manual Identity Citizenship & Identity X X X X X X X X X X X Page 83 For a complete listing of documents deemed acceptable as proof of citizenship and identity, go to http://www.hsd.state.nm.us/uploads/files/Looking%20For%20Information/08_100_0130.pdf For the lawfully residing policy and nonimmigrant status descriptions, go to http://www.hsd.state.nm.us/uploads/FileLinks/1279f87fd1af45bfabc9f4bf1706d624/12_01_Lawfully_ Residing_Children_and_Pregnant_Women_1.pdf The New Mexico Department of Health's (DOH) Vital Records Bureau Birth Record Web Portal Verification site can be searched to obtain verification of most individuals born in New Mexico after 1919. This proof may be used to verify an individual's citizenship status. This site is for the use of employees of state agencies or for individuals who have been certified as New Mexico HSD Presumptive Eligibility Determiners (PEDs). The site may be accessed at https://www.health.state.nm.us/partners/bc_confirm.php. After navigating to the site, the following security message will appear. Click on “continue to the website (not recommended).” To search for a New Mexico birth record on this site, the applicant's information must be entered into the portal exactly as it appears on the individual's birth certificate. The following information must be entered: First Name; Last Name Date of Birth (mm/dd/yyyy) County of Birth Gender Mother’s First Name Mother’s Maiden Name If a birth record is found, it should be submitted with the application for ongoing Medicaid eligibility. Proof of Income To meet Medicaid financial eligibility requirements, proof of income may be required of the applicant. HSD will utilize data matches to obtain income verifications. Any applicant who has financial information such as proof of wages from employment (past 4 weeks of income), social security statements or tax information for countable income should supply proofs of this income with their Medicaid application. For more information on countable and non-countable income types, please see Chapter 10 of this manual. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 84 Chapter 14 - Glossary of Terms and Acronyms ABP - Alternative Benefit Plan ACA - Affordable Care Act Alternative Benefit Plan (ABP) - Most adults who qualify for the Medicaid category known as the “Other Adult Group” receive services under the New Mexico Alternative Benefit Plan (ABP). The ABP covers doctor visits, preventive care, hospital care, emergency and urgent care, specialist visits, behavioral health care, substance abuse treatment, prescriptions, certain dental services, and more. Some recipients will have to pay small co-pays for certain services, depending on their income. AVRS - Automatic Voice Response System Categories of Eligibility (COEs) - Medicaid Categories of Eligibility. Medicaid COEs include coverage for children, families, pregnant women, adults, long-term care recipients and individuals who are eligible for both Medicare and Medicaid benefits. All New Mexico Medicaid COEs have a designated numeric COE listing associated with the COE name. Centers for Medicare and Medicaid Services (CMS) - A federal agency within the United States Department of Health and Human Services (DHHS) that administers the Medicare program and works in partnership with state governments to administer Medicaid, the Children's Health Insurance Program (CHIP), and health insurance portability standards. Children, Youth and Families Department (CYFD) - New Mexico Children, Youth and Families Department Children's Health Insurance Program (CHIP) - CHIP coverage is generally available to children in families with incomes at the higher income threshold of Medicaid eligibility. Unlike regular children's Medicaid coverage, CHIP may have minimal co-pays for some services. In New Mexico, the categories of eligibility for CHIP are categories 420 and 421. CHIP - Children's Health Insurance Program CMS - Centers for Medicare and Medicaid Services COE - Category of Eligibility Countable Income - The amount of income remaining after all applicable deductions and disregards have been deducted from the GROSS income. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 85 CYFD - New Mexico Children, Youth and Families Department DOH - New Mexico Department of Health Early and Periodic Screening, Diagnostic and Treatment (EPSDT) - Provides comprehensive and preventive health care services for children under age 21 who are enrolled in Medicaid. EPSDT is key to ensuring that children and adolescents receive appropriate preventive, dental, mental health, and developmental and specialty services. EPSDT - Early and Periodic Screening, Diagnostic and Treatment Federal Poverty Levels (FPL) - The income guidelines that are used to determine Medicaid eligibility. FPLs are set by the United States Health and Human Services Department and are based on household size and total income. Federally Qualified Health Center (FQHC) - FQHCs include all organizations receiving grants under Section 330 of the Public Health Service Act. FQHCs qualify for enhanced reimbursement from Medicare and Medicaid, as well as other benefits. FQHCs must serve an underserved area or population, offer a sliding fee scale, provide comprehensive services, have an ongoing quality assurance program, and have a governing board of directors. Fee For Service (FFS) - A Medicaid delivery system where health care providers are paid for each service (like an office visit, test, or procedure). FFS covers the basic Medicaid benefit package, such as preventive, specialty and behavioral health services, and emergency care. Most Native Americans can choose to receive Medicaid services through FFS or Managed Care. Native Americans who are eligible for both Medicare and Medicaid or require a nursing facility level of care are required to be in Managed Care and do not have the option of receiving Medicaid services through FFS. FFS - Fee for Service FPL - Federal Poverty Level FQHC - Federally Qualified Health Center Health Insurance Portability and Accountability Act (HIPAA) - Provides national standards to protect the privacy of personal health information (PHI?). To improve the efficiency and effectiveness of the health care system, HIPAA included "Administrative Simplification" provisions that required the United States Department of Health and Human Services to adopt national standards for electronic health care transactions. Congress incorporated into HIPAA provisions that mandated the adoption of Federal privacy protections for individually identifiable health information. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 86 Health Risk Assessment (HRA) - A systematic approach to collecting information from individuals that identifies risk factors, provides individualized feedback, and links the person with at least one intervention to promote health, sustain function and/or prevent disease. Centennial Care members will receive an HRA by phone or in person by their Managed Care Organization. HIPAA - Health Insurance Portability and Accountability Act HRA - Health Risk Assessment HSD - New Mexico Human Services Department IHS - Indian Health Service Income Support Division (ISD) - The Division within the New Mexico Human Services Department that determines eligibility for the State's Public Assistance Programs. ISD field offices are located statewide. Indian Health Service (IHS) - An Agency within the Department of Health and Human Services responsible for providing federal health services to American Indians and Alaska Natives. The IHS is the principal federal health care provider and health advocate for Indian people, and its goal is to raise their health status to the highest possible level. The IHS provides a comprehensive health service delivery system for approximately 1.9 million American Indians and Alaska Natives who belong to 566 federally recognized tribes in 35 states. ISD - Income Support Division LIHEAP - Low Income Energy Assistance Program Legal Immigrant - A non-U.S. citizen who has permission to live and/or work in the U.S. as demonstrated by providing documents issued by the U.S. Citizenship and Immigration Services. Low Income Home Energy Assistance Program (LIHEAP) - Assists eligible New Mexico residents and families with their heating and cooling costs. LIHEAP is federally funded through the Department of Health and Human Services. The federal government establishes funding levels annually. MAD - Medical Assistance Division MAD 008 - Household Comp and Income Calculation Worksheet MAD 011 - Presumptive Eligibility (PE) Applicant Information Form MAD 070 - Presumptive Eligibility Authorization Form MAD 100 - New Mexico Medicaid-only application June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 87 MAD 219 - Presumptive Eligibility Determiner Agreement and Code of Conduct MAD 222 - Federal Poverty Level Guidelines (Revised each April 1 for Medicaid Categories of Eligibility) MAGI - Modified Adjusted Gross Income Managed Care Organization (MCO) - An insurance company that contracts with providers and medical facilities to provide healthcare to its members. New Mexico's Medicaid Managed Care program is called Centennial Care and there are four MCOs contracted to provide Centennial care services. The four MCOs are Blue Cross Community Centennial, Molina Healthcare of New Mexico, Presbyterian Health Plan and UnitedHealth care Community Plan of New Mexico. MCO - Managed Care Organization Medicaid – A state, federally funded, health coverage program for people who meet certain requirements. There are numerous categories of Medicaid, each with specific eligibility requirements and benefit packages. States establish their own eligibility standards; determine the type, amount, rate of payment; and duration and scope of services based on broad national parameters set by CMS (Centers for Medicare and Medicaid Services, a federal agency). Medicaid Call Center's Automatic Voice Response System (AVRS) - Unmanned telephone system where providers can check Medicaid client eligibility. Medical Assistance Division (MAD) - The Division with the New Mexico Human Services Department that administers the State's Medicaid program and, in some cases, may also process Medicaid eligibility applications. Medicare -- is a national social insurance program administered by the U.S. Federal Government since 1965 that guarantees access to health insurance for Americans ages 65 and older and younger people with disabilities. Modified Adjusted Gross Income (MAGI) - The figure used to determine eligibility for lower costs in the Marketplace and for Medicaid and CHIP. Generally, modified adjusted gross income is an individual's adjusted gross income plus any tax-exempt Social Security, interest, or foreign income they may have. New Mexico Human Services Departments (HSD) - Administrator of all New Mexico Public Assistance Programs including the Medicaid, Cash Assistance, the Supplemental Nutrition Assistance Program (SNAP) and the Low-Income Home Energy Assistance Program (LIHEAP). New Mexico Medicaid Portal (Portal) - An on-line public portal operated and maintained by the New Mexico Medicaid Fiscal Agent, Xerox, on behalf of the New Mexico Human Services Department's June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 88 Medical Assistance Division. The Portal can be used by Medicaid recipients or by Medicaid providers to access eligibility information. Patient Protection and Affordable Care Act (ACA) - A United States federal statute signed into law by President Barack Obama on March 23, 2010. The ACA was enacted with the goals of increasing the quality and affordability of health insurance, lowering the uninsured rate by expanding public and private insurance coverage, and reducing the costs of healthcare for individuals and the government. It introduced a number of mechanisms—including mandates, subsidies, and insurance exchanges— meant to increase coverage and affordability. PE - Presumptive Eligibility PE+ - Presumptive Eligibility Plus PED - Presumptive Eligibility Determiner PED Number - Presumptive Eligibility Determiner Number PHI - Personal Health information Portal - New Mexico Medicaid Portal Presumptive Eligibility (PE) - Short-term Medicaid coverage for eligible individuals. PE is not available for every Medicaid category of eligibility but is available for children, pregnant women, former foster care recipients, and some adults. Presumptive Eligibility Determiners (PEDs) - Individuals who are trained and certified to screen and enroll eligible individuals into Presumptive Eligibility coverage. PEDs who can determine PE for Children and Pregnancy only categories of eligibility are Specialty Type 170. Presumptive Eligibility Determiner Number -- The number a Presumptive Eligibility Determiner (PED) is assigned after completing a Presumptive Eligibility training and fulfilling all other certification requirements. This number is required in order to determine PE eligibility by accessing the New Mexico Medicaid Portal. Presumptive Eligibility Plus (PE+) Determiners - PEDs who have been certified with Specialty Type 171 are also known as PE+ Determiners. PE+ Determiners can determine eligibility for children, pregnancy, Other Adult and Parent Caretaker categories of eligibility. PE+ Determiners are only eligible to participate as such if they are employed by and physically stationed at a specific location type. This includes hospitals that have elected to participate as a PE Provider location but does not extend to a hospital's associated clinics or to any PED who is stationed off-site from their normal work site. PE+ June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 89 locations also include employees of Indian Health Services (IHS) medical facilities and clinics as well as staff at New Mexico Department of Corrections facilities, County Detention Centers and Jails. SNAP - Supplemental Nutrition Assistance Program (re-alphabetized) SSI - Supplemental Security Income SSN - Social Security Number Social Security Number (SSN) - A nine-digit number assigned to citizens, some temporary residents and permanent residents in order to track their income and determine benefit entitlements. The Social Security Number was created in 1936 and while the original intention was just to track earnings and benefits, it is now also used to identify individuals and sometimes track their credit record. Supplemental Nutrition Assistance Program (SNAP) - Serves as the first line of defense against hunger for New Mexico residents. It enables low-income families to buy nutritious food with coupons and Electronic Benefits Transfer (EBT) cards. SNAP recipients spend their benefits to buy eligible food in authorized retail food stores. Supplemental Security Income (SSI) - The monetary benefits received by retired workers who have paid in to the Social Security system during their working years. Social Security benefits are paid out on a monthly basis to retired workers and their surviving spouses. They are also paid to those who are permanently and totally disabled according to the strict criteria set forth by the Social Security Administration. TANF - Temporary Assistance to Needy Families Temporary Assistance to Needy Families (TANF) - The New Mexico Temporary Assistance for Needy Families (TANF) program, known as NMWorks, provides cash assistance and job training to eligible New Mexico families. This monthly cash assistance benefit should be used to meet family needs such as housing, utilities, and clothing costs. Value-Added Services - Services or benefits provided by a Managed Care Organization that are above and beyond what is contractually required to be provided to the MCO's members. Xerox -- The contracted Fiscal Agent for New Mexico Medicaid who processes claims for payment to Medicaid providers. Xerox operates and maintains New Mexico Medicaid Portal, Omnicaid system and AVRS systems on behalf of the New Mexico Human Services Department's Medical Assistance Division. YESNM - Your Eligibility System New Mexico YESNM-PE - Your Eligibility System New Mexico for Presumptive Eligibility Determiners June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 90 Your Eligibility System New Mexico (YESNM) - On-line application system used by the public to apply for New Mexico's Public Assistance Programs. Your Eligibility System New Mexico for Presumptive Eligibility Determiners (YESNM-PE) - The area of the YES-NM system designed for the exclusive use of Presumptive Eligibility Determiners to screen applicants for Presumptive Eligibility. June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 91 Chapter 15 - Quick Reference Information, Forms, Checklists and Worksheets The following quick reference materials, forms, checklists and worksheets can be found in this section. Section 1 - Quick Reference Information Presumptive Eligibilty Contact and Resource Sheet Flow Process for Pesumptive Eligibility Training and Certification New Mexico Medicaid Web Portal and YESNM-PE Registration Workflow Electronic Presumptive Eligibility Screening Process Workflow Manual Screening for Presumptive Eligibility Workflow Federal Poverty Level with ACA Categories of Eligibity (MAD 222) Medicaid Categories of Eligibility Applicant Rights and Responsibilities - English Applicant Rights and Responsibilities - Spanish YESNM-PE Electronic Signature Page - English YESNM-PE Electronic Signature Page - Spanish Section 2 - Forms Presumptive Eigibility Determiner Agreement and Code of Conduct (MAD 219) Medicaid-Only Application - English (MAD 100) Medicaid-Only Application - Spanish (MAD 100 SP) Presumptive Eligibity Applicant Information form - English (MAD 011) Presumptive Eligibity Applicant Information form - Spanish (MAD 011 SP) Presumptive Eligibity Authorization Form (MAD 070) Section 3 - Checklists and Worksheets How to Determine Household Size flowchart Household Comp and Income Calculation Worksheet (MAD 008) Manual Presumptive Eligibility Submission Checklist o For Applicants Who Wish to Apply for Ongoing Medicaid Coverage o For Applicants Who DO NOT Wish to Apply for Ongoing Medicaid Coverage June, 2014 NM HSD/MAD - PE & PE+ Training Manual Page 92 Presumptive Eligibility Contact & Resource Sheet Contact: Assistance For: E-Mail/URL: Claim & Eligibility Information FAQs [email protected] NM Medicaid Web Portal Provider Relations Help Desk User administration/web registration inquiry Xerox Help Desk (AVRS) Automated Voice Response System Eligibility information Client Eligibility Questions Medicaid Call Center General Client Questions YESNM-PE Screen for PE YESNM Customer Service YES Information Central ASPEN Scanning Area (CASA) Assistance with Mailing address: applications or documents - PO BOX 830 submitted through Aspen Bernalillo, NM 87004 800-283-4465 NM Medicaid Web Portal Customer Service for: Central ASPEN Scanning Area (CASA) nmmedicaid.acs-inc.com Phone/Fax #: 800-705-4452 505-246-0710 Fax#: 877-285-6790 800-705-4452 505-246-0710 800-820-6901 Xerox Medicaid Call Center: 888-997-2583 www.yes.state.nm.us/jsp/access/myAcc ess/PELogin.jsp www.yes.nm.state.us 800-283-4465 505-841-6700 CASA E-fax#: 855-804-8960 [email protected] Managed Care Organizations Blue Cross Community Centennial Molina Health Care of New Mexico, Inc. www.bcbsnm.com/coverage/medicaid (866) 689-1523 www.molinahealthcare.com/enus/Pages/home.aspx (877) 373-8986 Presbyterian Health Plan, Inc. www.phs.org/pages/default.aspx (888) 977-2333 UnitedHealthcare Community Plan of New Mexico www.uhccommunityplan.com (877) 236-0826 [email protected] 505-827-7717 PE Determiner Training Program HSD/MAD 3/2014 PED training, scheduling, questions & issues Fax #: 505-827-7200 Flow process for Presumptive Eligibility Training and Certification • Individuals from Providers contact MAD for upcomming trainings. • MAD will create a contact list and email individuals requesting training with dates and times. Pre Registration Registration and Training •Individual will access the link located in email from MAD and complete the registration process. •Individual will attend training on registered date and time. •Once training is complete the individual must complete a comprehension test with a minimum score of 90% •After passing score is achieved, the indivifual must register on the New Mexico Medicaid Web Portal (Portal). •Individual completes the online PE Determiner Agreement by submitting an electronic signature acknowledgement. •The individual is issued a Determiner number which they will use to complete the Portal registration. •individual registers as a USER on YESNM-PE to begin screening appicants for PE. PE Certification New Mexico Medicaid Web Portal & YESNM-PE Registration Workflow Individual achieves passing score on comprehension test. Individual accesses the New Mexico Medicaid Web Portal (Portal) to begin Provider enrollment registration process. (https://nmmedicaid.acs-inc.com) Individual completes the online electronic acknowledgement for the PE Determiner Agreement (MAD 219). Once the Welcome Packet and PED number are received, the PED must register as a USER on the Portal. After verification, a Welcome Packet and the individual`s unique PED number will be sent. Once the Provider enrollment has been completed, HSD/MAD PE Program Staff will verify for accuracy. To access the YESNM-PE screening tool, each PED must register as a user on YESNM-PE (https://www.yes.state.nm.us/jsp/ access/myAccess/PELogin.jsp) Registration Complete Electronic Presumptive Eligibility Screening Process Workflow Log-in to the Portal and verify client eligibility. Log into YESNM-PE and complete applicant information screens. At the YESNM-PE PE Determination Results page, access to a link will be given for the Portal. The PED will enter the PE approval into the portal. PE Screening Complete Applicants will be given the option to submit the information gathered for the screening to HSD for an ongoing Medicaid application determination. Once PE is entered in the Portal, the PED will return to the PE Determination Results page where they will print the results for the applicant. Manual Screening for Presumptive Eligibility Access the Medicaid Web Portal or call the Medicaid Call Centers Automatic Voice Response System (AVRS) at (800) 820-6901 to verify applicant eligibility. Ask Client if they want to apply for ongoing Medicaid coverage: YES NO *PED assists applicant with completion of MAD 100 *PED assistis applicant with completion of MAD 011 *PED calculates Household size *PED calculates Household size *PED calculates Financial Eligibility *PED calculates Financial Eligibility Is the client eligible for PE? Is the client eligible for PE? YES *PED faxes completed MAD 070 to Xerox NO *Submit forms - MAD 100, MAD 070, calculation worksheets and any additional applicant documents to Central ASPEN Scanning Area (CASA) *PED submits MAD 100 calculation worksheets and any additional applicant documents to Central ASPEN Scanning Area (CASA) CASA Fax: 855-804-8960 YES Xerox Fax: 877-285-6790 *PED Faxes completed MAD 070 to Xerox *PED submits forms MAD 011, MAD 070 & all calculation worksheets to MAD PE Program Staff NO *PED submits forms MAD 011, MAD 070 & all calculation worksheets to MAD PE Program Staff MAD PE Program Staff Fax: 505-827-7200 AFFORDA A BLE CARE E MEDICA AID PROGRAMS ral Pover rty Guide elines (FP PL) Feder Efffective 7/ /1/14 – 3 3/31/15 CATEGORY 100 0 – Covera age dults for Ad A Alternative Be enefit Coverage In ncome must be under 133 3% FPL N No resource standard N No Medicare HOUSE EHOLD SIZE MONT THLY INCO OME 1 2 3 4 5 6 7 8 $ 1,2 294 $ 1,7 744 $ 2,1 194 $ 2,6 644 $ 3,0 094 $ 3,5 544 $ 3,9 994 $ 4,4 444 $ 45 50 ----------------------------------------------------------------------------------------+1- - - - - - - - - - - - CATEGORY 200 0 – Parent aker Careta Full Medica aid Income mu ust be under fixed standard Household must have a relative child in household ce standard No resourc CA ATEGORY 301 – Pre gnancy Se ervices Only y 5% DISR REGARD - Amount Disregard ded when A Applicable Pregnancy Services S Income must be under 2 250% FPL 2 months post partum No resource e standard HO OUSEHOLD SIZ ZE M ONTHLY I INCOME 2 3 4 5 6 7 8 $ 3,278 $ 4,123 $ 4,969 $ 5,815 $ 6,661 $ 7,507 $ 8,353 $ 846 -----------------------------------------------------------------------------+1 1- - - - - - - - - - - - HOUSEHOL H D SIZE MONTHLY M INCOME I 1-------------2-------------3-------------4-------------5-------------6-------------7-------------8-------------+1+ ------------ Category 400 - Medicaid M forr Children Fu ull Medicaid Ch hildren unde er 19 years of age Income underr the following FPL: Children ag ges 0-5 ------0%-240% % Children ag ges 6-18-------0%-190% % No o resource Standard S Eliigible even if children have h health insurance or o ha ave voluntarrily dropped insurance Category 420 - Children's C Health Insura ance Progra am (CHIP)) Fu ull Medicaid Income underr the following FPL: Children ag ges 0-5 --------240%-3 300% Children ag ges 6-18--------190%-240% Do o NOT have existing ins surance Co o-payments on doctor visits, v prescriptions, etc c. Na ative Americ can children n do not mak ke co-payments MAD D 222 Revised 07/01/20 014 $ $ $ $ $ $ $ $ $ 451 608 765 923 1,080 1,238 1,395 1,553 158 Category Category Category Category Category Category 100 200 300 301 400 420 HOUSEHOLD SIZE 1 2 3 4 5 6 7 8 (only iff Medicare eligible) M MONTHLY DI ISREGARD ----------------------------------------------------------------------------------------+1- - - - - - - - - - - - $ $ $ $ $ $ $ $ $ 49 66 83 99 116 133 150 167 17 CATEGO ORY 300 – Full Coverage e for Pregn nant Women Full Medicaid Income e must be und der Standard of Need 2 months post partu um No reso ource standarrd Hou sehold e Size 1--- --------------------2--- --------------------3--- --------------------4--- --------------------5--- --------------------6--- --------------------7--- --------------------8--- --------------------+1----------------------- Mo onthly Gross s Income 2 240% 300 0% $2 2,334 $2,,918 $3 3,146 $3,,933 $3 3,959 $4,,948 $4 4,770 $5,,963 $5 5,582 $6,,978 $6 6,395 $7 7,206 $8 8,018 $8 812 $7,,993 $9,,008 $10 0,023 $1,,015 COE Descriptions ACA January 1, 2014 New COE COE Description & FPL Former Medicaid COEs Prior to January 1, 2014 Old COE COE Description 027 Four Months transitional Medicaid 027 Four Months transitional Medicaid 028 12 month transitional Medicaid 028 12 month transitional Medicaid 029 Family Planning 0%-185% 029 031 Newborns 031 Newborns 085 Emergency Medical Services for Aliens Family Planning 085 Emergency Medical Services for Aliens 100 Other Adults * (age 19-64) 0%-133% 200 Parent Caretaker* 0-47% 072 Family Medicaid 300 Full Medicaid for Pregnant Women 0%-138% 030 Full Medicaid Pregnant Women 301 Pregnancy-Related Medicaid * 138%-250% 035 400 Children’s Medicaid (ages 0-5) 0%-138% 032 401 Children’s Medicaid (ages 6-18) 0%-138% 032 402 Children’s Medicaid (ages 0-5) 138%-240% 403 Children’s Medicaid (ages 6-18) 138%-240% 036 036 Pregnancy Related Only Children’s Medicaid (ages 0-5) Children’s Medicaid (ages 6-19) Children’s Medicaid (ages 0-5) Children’s Medicaid (ages 6-19) 1 Changes COE 027 was provided to individuals due to loss of COE 072 from increased earnings of child or spousal support. COE 027 is now provided due to loss of COE 200 from increased earnings of spousal support only. Child support is no longer countable under ACA rules. COE 028 was provided to individuals due to loss of COE 072 from increased earnings. COE 028 is now provided due to loss of COE 200 from increased earnings. Family planning individuals were transitioned to an ACA category if eligible. Those not eligible for an ACA category remain on family planning and are referred to the Exchange for minimum essential coverage. No changes. To be eligible, the newborn must be born to a woman who is eligible for and receiving Medicaid on the date the newborn is born. No changes. EMSA is available for all individuals eligible for any of the new ACA categories. COE 100 is a new category for adults (19-64). Other insurance can coexist with COE 100, except for Medicare. COE 072 will be replaced by COE 200 at recertification over the next year, if client remains eligible. Eligibility for an ACA category will be evaluated per individual. COE 200 is for adults only. A 5% disregard can be applied if the adult is receiving Medicare or is age 65 or over. Children on COE 072 will transition to one of the children’s Medicaid categories if eligible at recertification. COE 030 is replaced by the new COE 300. COE 030 was around 25% FPL. The new COE 300 provides full Medicaid up to 138% FPL. More women will qualify for full Medicaid for pregnant women due to the increase in FPL. COE 035 is replaced by COE 301. COE 032 will be replaced by the new COE 400 at recertification over the next year, if client remains eligible. COE 032 will be replaced by the new COE 401 at recertification over the next year, if client remains eligible. COE 036 will be replaced by the new COE 402 at recertification over the next year, if client remains eligible. COE 036 will be replaced by the new COE 403 at recertification over the next year, if client remains eligible. COE Descriptions 420 CHIP Medicaid (ages 0-5) 240%-300% 071 Children’s Medicaid (ages 0-5) 421 CHIP Medicaid (ages 6-18) 190%-240% 071 Children’s Medicaid (ages 6-19) Program ended 12/31/2013 062 063 064 State Coverage Insurance COE 071 will be replaced by the new COE 420 at recertification over the next year, if client remains eligible. COE 071 will be replaced by the new COE 421 at recertification over the next year, if client remains eligible. SCI ended 12/31/2013. Individuals were evaluated for an ACA category: 1. If eligible, they were placed on the ACA category. 2. If ineligible, evaluated for family planning and referred to the Exchange for minimum essential coverage. 3. If ineligible for family planning, eligibility was ended 12/31/2013 and client was referred to the Exchange for minimum essential coverage. *5% income disregard can be applied if needed. Non Modified Adjusted Gross Income (MAGI) Categories/No Changes COE COE Description 001, 003, 004 Supplemental Security Income (SSI)-The Social Security Administration determines eligibility for these categories. SSI provides cash benefits and Medicaid provides health care coverage for eligible individuals under aged (Category 001), blind (Category 003), or disabled (Category 004). 041, 044 Qualified Medicare Beneficiaries (QMB) - Medicaid covers payment of Medicare premium amounts for Parts A and B and the coinsurance and deductibles on Medicare-covered services. Medicaid does not pay for services which are not Medicare benefits, services denied by Medicare, or services furnished by providers who have not accepted Medicare assignment. Reimbursement is made to providers of covered services and not directly to recipients. 042 Qualified Individuals (QI1s) - Medicaid pays the Medicare part B premium. Applicants/recipients eligible for QI1 coverage under another Medicaid category may not be eligible for QI1. QI1 eligibility is funded by limited block grant funding beginning in 1998 and ending when the congressional extension period expires. Since payment of the Medicare part B premium is the only benefit, no Medicaid card is issued. 045 Specified Low-Income Medicare Beneficiaries (SLIMB) - Medicaid pays the Medicare part B premium. Applicants/recipients eligible for Medicaid coverage under another Medicaid category may also be eligible for SLIMB. SLIMB eligibility allows the state to receive federal matching funding for the purchase of Medicare part B. Since payment of the Medicare part B premium is the only benefit, no Medicaid card is issued and there is no interaction with the Medicaid claims processing contractor. 049/059 Refugee Medicaid Assistance (RMA)-RMA offers health coverage for refugees within the first eight months from their date of entry to the United States, when they do not qualify for Medicaid. RMA eligible refugees have access to a benefit package that parallels the full coverage Medicaid benefit package. This program is not funded by Medicaid. RMA is funded through a grant under Title IV of the Immigration and Nationality Act. The purpose of this grant is to provide for the effective resettlement of refugees and to assist them to achieve economic self-sufficiency as quickly as possible. 2 COE Descriptions 052 Breast and Cervical Cancer (BCC)- a program for uninsured women under the age of 65 years, who meet the screening criteria , an income test of 250% of the Federal Poverty Guidelines and diagnostic testing by a contracted Centers for Disease Control and Prevention’s provider resulting in a diagnosis of breast or cervical cancer including pre-cancerous conditions. Women who have met CDC screening criteria and identified as needing treatment for a diagnosis of breast or cervical cancer, including pre-cancerous conditions will be referred for treatment that includes the completion of a Medicaid application for the BCC program. The Breast and Cervical Cancer Prevention and Treatment Act allows states to extend presumptive eligibility to applicants in order to ensure that needed treatment begins as early as possible. 074 Working Disabled Individuals (WDI) - The working disabled individuals program covers disabled individuals who are employed or disabled individuals who have lost eligibility for supplemental security income (SSI) and Medicaid due to initial receipt of social security disability insurance ( SSDI) and who are not yet qualified for Medicare; this group is referred to as “medigap”; once the medigap individual begins receiving Medicare, they must become employed to retain eligibility for WDI. 081, 083, 084 Institutional Care Medicaid-Provides Medicaid to individuals requiring institutional care in nursing facilities (NFs) designated as High NFs or Low NFs, Intermediate Care Facilities for the Mentally Retarded (ICF-MRs) or acute care hospitals. These individuals must meet all SSI eligibility criteria except income. As of January 1, 2014 the maximum allowable countable income limit is $2,163 per month. 090, 091, 092, 093, 094, 095, 096 Home and Community-Based Waivers-Recipients in these programs are persons who qualify both financially and medically for institutional care but who remain in the community. The Department of Health or Aging and Long Term Services Department must determine that adequate care can be provided to the individual in the community at a lesser cost than in an institutional setting. CYFD Categories Medicaid is provided for children in state substitute care programs and in adoption subsidy situations. The Children, Youth and Families Department make eligibility determinations for these categories. To be eligible on the basis of income, a child in a substitute care placement must have an income below the maximum AFDC standard of need 5 for one person. COE COE Description 017 Adoption Subsidy established by other states 037 Adoption Subsidy in state 047 Adoption Subsidy placed out of NM 066 Foster Care 086 Foster Care with state other than NM 3 Applicant's Rights and Responsibilities If you are a person with a disability and you require this information in an alternative format, or require a special accommodation to participate in any public hearing, program or services, please contact the NM Human Services Department toll-free at 1-800-432-6217 or through the New Mexico Relay System TDD at 1-800-659-8331 or by dialing 711. The Department requests at least 10 days advance notice to provide requested alternative formats and special accommodations. Your Civil Rights All programs administered by the Human Services Department (HSD) are equal opportunity programs. If you believe you have been treated unfairly because of race, color, national origin, age, disability, and where applicable, sex, marital status, familial status, parental status, religion, sexual orientation, genetic information, political beliefs, reprisal, or because all or part of an individual's income is derived from any public assistance program, you may file a complaint. Complaints of discrimination may be filed with the New Mexico Human Services Department central office or the local Human Services county office. Complaints of discrimination about the SNAP/Food program may be filed with the USDA, Director, Office of Civil Rights, Room 326, W. Whitten Bldg., 1400 Independence Ave, S.W. Washington, DC 20250-9410 or call (202) 720-5964 (voice and TDD). Complaints of discrimination about Cash Assistance and Medical Assistance programs may be filed with the Office of Civil Rights, Department of Health & Human Services, 1301 Young Street, Suite 1169, Dallas, TX 75202 or call (800) 368-1019 (voice) and (214) 767-8940 (TDD). Your Privacy The information you give HSD will be used to determine whether your household is eligible or continues to be eligible to take part in HSD programs. We will check this information through computer matching programs or other means. This information will also be used to make sure that you meet program rules and help us to manage the program. This information may be given to other Federal and State agencies for official examination, and to law enforcement officials for the purpose of picking up persons fleeing to avoid the law. If you get benefits that you were not eligible for and have to pay them back, this is called a claim. If your household gets a claim against it, the information on this application including all Social Security Numbers, may be given to Federal and State agencies, as well as private claims collection agencies for claims collection action. Providing the requested information, including Social Security Numbers of each household member is voluntary. However, each person applying for assistance must give a Social Security Number or it will result in the denial of program benefits to each individual applicant failing to give a Social Security Number. Non-Citizen Immigrants not requesting assistance for themselves do not need to give immigration status information or Social Security Numbers. Any Social Security Numbers given will be used & disclosed in the same manner as Social Security Numbers of eligible household members. We also check with other agencies, the federal Income and Eligibility Verification Service (IEVS) and The Public Assistance Reporting Information System (PARIS) about the information that you give us. This information may affect your household eligibility and benefit amount. Child Support Enforcement Division By accepting Cash or Medical Assistance, you assign (give) HSD rights to collect child support from the child's absent parent(s). You must help HSD find the absent parent(s) unless there is a good reason not to do so such as domestic violence; ask ISD. If it is decided that you have to work with the Child Support Office to establish or enforce child support and you do not, cash benefits may be reduced and eventually lost, and adults may lose their medical assistance. Non-Citizen Immigrant Eligibility What types of Non-Citizen Immigrants are eligible for HSD assistance programs? For most programs, non-citizens must have a "qualified" immigrant status and meet certain other conditions to qualify. Most non-citizens in the following categories can get benefits if they meet all other program eligibility requirements: Lawful Perm. Res. (LPRs) Refugees Asylees Cuban Haitian Entrants Amerasians Paroled to U.S. - 1 year Withholding of Deportation Certain: Battered women and children Veterans, active duty military Hmong or Laotian Tribe Canada/Mexico born Native American Human Trafficking Victims Certain non-citizens, including undocumented non-citizens may be eligible for emergency medical services including pregnant women's labor and delivery. Is there a waiting period (bar) before non-citizen immigrants can get benefits? The general rule now is that most qualified immigrant children are eligible to receive SNAP/Food, Medical, Cash and Energy Assistance. However some "qualified" immigrant adults can get benefits after they have been in the United States in "qualified" immigrant status for five years and some immigrants can get them right away. In general, adults in certain humanitarian immigration categories (such as Refugees and Asylees), people with military connections, credit for 10 years of work history in the US, and persons receiving disability benefits may be eligible right away. Derechos y Responsabilidades Si usted es una persona con una discapacidad y Ud. requiere esta información en un formato alternativo o requiere un acomodamiento especial para poder participar en cualquier audiencia pública, programa o servicio, comuníquese con el Departamento de Servicios Humanos de NM gratis al 1-800-432-6217 o a través del sistema de relais de Nuevo México TDD en 1-800-659-8331 o llamando al 711. Las peticiones del Departamento de por lo menos 10 días por anticipado para poder proporcionar los formatos alternativos y acomodamientos especiales. Sus Derechos Civiles Todos los programas administrados por el Departamento de Servicios Humanos (HSD) son programas de oportunidades iguales. Si usted cree que ha sido tratado injustamente debido a la raza, el color, origen nacional, la edad, la incapacidad, y donde aplicable, el sexo, el estado civil, estatus familiar, estatus paternal, la religión, orientación sexual, información genética, las creencias políticas, la represalia, o porque todo o la parte de los ingresos de un individuo son derivados de cualquier programa de ayuda estatal, puede presentar una queja. Las quejas de discriminación se pueden presentar en la oficina central del Departamento de Servicios Humanos de Nuevo México, ATTN: Quality Improvement Section, Pollon Plaza, P. O. Box 2348, Santa Fe, Nuevo Mexico 87504-2348 o en la oficina local de su condado.Las quejas de discriminación sobre el Programa de Ayuda de Nutrición Suplemental se pueden presentar con el USDA, Director, Office of Adjudication, 1400 Independence Ave. SW, Washington, DC 20250-9410 o llame 1-866-632-9992 o 202-401-0216 (TDD). Su Privacidad La información que Ud. da a HSD será utilizada para determinar si su casa tiene elegibilidad o continúa a tener elegibilidad para participar en los programas de HSD. Verificaremos esta información por programas de computadora. Esta información también será utilizada para asegurar de que Ud. sigue las reglas del programa y para ayudarnos a manejar el programa. Esta información puede ser dada a otras agencias federales y estatales para un examen oficial, y los agentes del orden con el propósito de recoger a personas que huyen de la ley. Si usted recibe beneficios de que usted no era elegible y tiene que pagarlos, esto se llama un reclamo. Si su familia recibe una demanda en contra de ella, la información en esta solicitud incluyendo todos los números de Seguro Social, puede ser dada a las agencias federales y estatales, así como agencias privadas de colección de reclamos por la acción de cobro. Proporcionar la información solicitada, incluyendo números de seguro social de cada miembro de la familia es voluntario. Sin embargo, cada persona que solicita asistencia debe dar un número de Seguro Social o resultará en la negación de los beneficios del programa a cada solicitante individual que no da un número de Seguro Social. Ciudadanos no inmigrantes no solicitando asistencia por sí mismos no necesitan dar información de estatus migratorio o números de Seguro Social. Los números de seguro social dados serán usados y revelados de la misma manera como números de seguro social de los miembros elegibles del hogar. También comprobamos con otras agencias el ingreso federal y el Servicio de Verificación de Elegibilidad (IEVS) y en el Sistema de Información Reportada de Asistencia Pública (PARIS) acerca de la información que usted nos da. Esta información puede afectar su elegibilidad del hogar y la cantidad de beneficios. División de Sostenimiento de Niños Al aceptar asistencia en efectivo o médica, usted asigna (otorga) a HSD derechos para cobrar el sostenimiento de niños del padre ausente del niño (s). Usted debe ayudar a HSD a encontrar al padre ausente (s) a menos que haya una Buena razón para no hacerlo, como la violencia doméstica, pregúntele a ISD. Si se decide que usted tiene que trabajar con la Oficina de Sostenimiento de Niño para establecer o hacer cumplir el sostenimiento y usted no lo hace, los beneficios en efectivo pueden ser reducidos y eventualmente perdidos, y los adultos pueden perder su asistencia médica. Elegibilidad de Inmigrantes No Ciudadanos (a)¿Qué tipos de Inmigrantes no ciudadanos son elegibles para programas de asistencia de HSD? Para la mayoría de los programas, los no ciudadanos deben tener un estado de inmigrante "calificado" y cumplir otras condiciones para calificar. La mayoría de los no ciudadanos en las categorías siguientes pueden obtener beneficios si cumplen con todos los requisitos de elegibilidad del programa: Residente Permanente Legal (LPR) Refugiados Asilados Entrados cubanos haitianos Amerasiáticos Libertad condicional a EE.UU. - 1 año Retención de la deportación Ciertos: Mujeres y niños maltratados Veteranos, militares en servicio activo Hmong de Laos o Tribu Nativo Americano nacido en Canadá / México Las víctimas de tráfico de personas Algunos no ciudadanos, incluidos los no ciudadanos indocumentados pueden ser elegibles para los servicios médicos de emergencia, incluyendo el parto y alivio de las mujeres embarazadas. (b) ¿Existe un período de espera (bar) antes de que los inmigrantes no ciudadanos pueden obtener beneficios? La regla general es que ahora la mayoría de los niños inmigrantes calificados son elegibles para recibir SNAP / Comida, Medicaid, Efectivo y Asistencia de Energía. Sin embargo, algunos adultos inmigrantes "calificados" pueden recibir beneficios después de haber estado en los Estados Unidos en condición de inmigrante "calificado" durante cinco años y algunos inmigrantes pueden obtener de inmediato. En general, los adultos en ciertas categorías de inmigración humanitarias (como refugiados y asilados), las personas con conexiones militares, el crédito por 10 años de historia de trabajo en los EE.UU., y las personas que reciben beneficios por incapacidad pueden ser elegibles de inmediato. Electronic Signature An applicant's signature makes this application valid. The application for ongoing eligibility cannot be processed without a signature. A signature is also an indication that: • I understand that making false statement or hiding information could mean State & Federal penalties & I have given HSD true, correct and complete information. • • I am declaring the identity of the children under age of 16 for whom I am applying. I will give proof of things I report to HSD. If I cannot get proof, I know that I can ask HSD to help me & I will let HSD to contact other people & companies to get proof. I will let HSD give limited information to approved agencies which give other related help for which I may be eligible. I understand that if I receive benefits for which I am not eligible, that I may have to pay HSD back for those benefits. I know that HSD will check the information that I give. HSD may use computers or other means to check the information on this form. I know that HSD will check the immigration status of people who apply for or get benefits. I understand that immigration for any household member that I am applying for may be subject to verification by USCIS (INS), and that it may affect the household's eligibility and level of benefits. I understand that I must cooperate with Quality Control (QC). QC is a part of HSD. QC reviews cases to make sure we determine who can get help correctly. I understand that I must give HSD any money I receive for medical services which have already been paid for by Medicaid. If I fail to do so, I, or the person(s) for whom I am applying, may lose Medicaid coverage for at least one year AND until the amount owed to Medicaid has been paid back in full. • • • • • • I affirm under penalty of perjury that the verbal statements I have given to the Presumptive Eligibility Determiner who has assisted me with the completion of this application are true and correct. This includes statements about the persons in my home, income and all other information used to determine ongoing Medicaid eligibility. Firma Electrónica Su firma hace que esta aplicación sea válida y no puede ser procesada sin la firma. Su firma también es una indicación de lo siguiente: Entiendo que si hago declaraciones falsas u oculto información podría significar penalizaciones Estatales y Federales y he dado a HSD información verdadera, correcta y completa. Estoy declarando la identidad de los niños menores de 16 años de edad para quien estoy solicitando. Voy a dar prueba de lo que reporte a HSD. Si no puedo conseguir la prueba, sé que puedo pedir que HSD me ayude y dejaré que HSD se ponga en contacto con otras personas y las empresas para obtener. Dejaré que HSD dé información limitada a las agencias acreditadas que dan otro tipo de ayuda relacionada para que yo pueda ser elegible. Entiendo que si recibo beneficios para los cuales no soy elegible, que tendré que pagar a HSD por esos beneficios. Yo sé que HSD revisará la información que dé. HSD puede usar computadoras u otras maneras para revisar la información en este formulario. Yo sé que HSD verificará el estatus migratorio de las personas que solicitan o reciben beneficios. Entiendo que la inmigración de cualquier miembro de la casa que estoy solicitando puede ser objeto de verificación por parte de USCIS (INS), y que puede afectar la elegibilidad del hogar y el nivel de los beneficios. Yo entiendo que tengo que cooperar con el control de calidad (QC). QC es una parte de HSD. QC revisa caso para asegurar que determinamos correctamente quién puede obtener ayuda. Entiendo que debo dar a HSD cualquier dinero que recibo por los servicios médicos que ya han sido pagados por Medicaid. Si yo no lo hago, yo o la persona(s) para quien estoy solicitando, podría perder la cobertura de Medicaid por lo menos un año y hasta que el monto adeudado a Medicaid se ha pagado en su totalidad. Yo afirmo bajo pena de perjurio que las declaraciones verbales que he dado al determinante de Elegibilidad Presunta que me ha asistido con la finalización de esta solicitud son verdaderas y correctas. Esto incluye declaraciones acerca de las personas en mi hogar, el ingreso y el esto de la información utilizada para determinar la elegibilidad para Medicaid en curso. PRESUMPTIVE ELIGIBILITY DETERMINER AGREEMENT AND CODE OF CONDUCT HSD and (Presumptive Eligibility Determiner Name) enter into this Agreement to allow the person named above to be certified as a Medicaid Presumptive Eligibility Determiner (PED). PEDs are authorized to make Presumptive Eligibility (PE), or short-term, Medicaid determinations for eligible individuals. The goal of presumptive eligibility is to provide access to immediate care for eligible recipients and to ensure assistance with application submission and possible ongoing Medicaid coverage for those individuals. PE is not available for all Medicaid categories of eligibility and is limited to those as outlined by the New Mexico Human Services Department's (HSD’s) Medical Assistance Division (MAD). Individuals who are initially screened for PE are done so based on some of the same qualifying factors that help to determine ongoing eligibility. Individuals who are accurately screened for PE are most likely to be approved for ongoing coverage. Eligible screenings and enrollments of individuals in PE coverage can only be made by certified PEDs. PEDs must meet the PED certification requirements as established by HSD/MAD. Eligible entities approved to participate as PEDs include: (a) a qualified hospital that participates as a provider under the Medicaid state plan or a Medicaid 1115 demonstration, notifies the Medicaid agency of its election to make presumptive eligibility determinations and agrees to make PE determinations consistent with State policies and procedures; or for (b) a qualified hospital that has as not been disqualified by the Medicaid agency for failure to make PE determinations in accordance with applicable state policies and procedures; or for (c) a Federally Qualified Health Center (FQHC), an Indian Health Service (IHS) facility, a Department of Health (DOH) clinic, a school, a Children, Youth and Families Department (CYFD) Child Care Bureau staff member, a primary care provider who is contracted with at least one HSD contracted MCO, a Head Start Agency; or (d) other entities that HSD has determined as an eligible Presumptive Eligibility participant including eligible employees of the New Mexico Department of Corrections, County Jails or Detention Centers DETERMINER CODE OF CONDUCT DISCLOSURE OR MISUSE OF CONFIDENTIAL OR OFFICIAL INFORMATION AND PERFORMANCE STANDARDS HSD serves the citizens of New Mexico. PEDs are considered agents of the State and must conduct the State’s business with the highest standards of integrity. HSD provides services to eligible New Mexicans with public funds and is accountable for those funds. PEDs must conduct themselves in a professional manner in all dealings with the public. It is never acceptable to convey an indifferent, hostile or careless attitude toward clients, even if clients are abusive. If a client continues to be abusive or threatening, please courteously refer them to an ISD office. PEDs shall disqualify themselves from participating in any official action affecting a client or any other person related to them by blood or marriage, (e.g. a first cousin or closer relative); clients or other persons with whom they enjoy a personal relationship that could compromise or be reasonably perceived by Department management or the public as compromising the integrity of their official actions; or any client or any other person with whom that PE Determiner is engaged in a sexual relationship and/or is sharing living quarters. PEDs may not receive any financial benefits, as a result of his/her provision of services to a client, other than what may be provided for, by the Department. PEDs may not disclose confidential or official information, if the disclosure of such information is prohibited by law or regulation or would be contrary to the best interest of the Department or its clients. This includes confidential information from other governmental agencies that PE Determiners may access via electronic data connections. PEDs may not disclose or misuse confidential or official information not generally available to the public or acquired by virtue of his/her affiliation with the Human Services Department, for his/her own or another’s private gain. PEDs may have access to an applicant's of Personally Identifiable Information (PII) and Protected Health Information (PHI). Any unauthorized or unofficial use of the PII or PHI, including any misuse, may be prosecuted under New Mexico State statutes and The United States regulations and laws regarding the use of this information, particularly the Standards for Privacy of Individually Health Information 45 CFR Parts 160 and 164. PEDs shall conduct themselves in a law abiding manner at all times. The possession and/or use of illicit drugs and/or misuse of prescription drugs during work hours or reporting for work and/or being on department premises, under the influence of any of the above, is strictly prohibited and will subject the Determiner to immediate termination of their Determiner status. PEDs under investigations or charged with criminal activities and/or unethical practices will subject the Determiner to immediate termination of their Determiner status. PEDs shall remain objective and may not recommend an MCO to a client. This decision is to be made solely by the client, independent of a PED’s influence. PEDs agree to: Participate in trainings sponsored by HSD; Complete the PED certification process; Maintain client confidentiality; Assist PE clients who wish to apply for ongoing coverage with the completion of a Medicaid application. PEDs must submit the completed applications to HSD within 2 business days of the PE approval; Keep complete records on all PE clients; these records are subject to review by State and/or Federal agencies MAD 219 5/1/14 HSD agrees to: Make PED certification training sessions available for qualified individuals; Allow access to YESNM-PE and the Portal to PEDs in good standing; Supply initial forms needed for PE determinations PED PERFORMANCE STANDARDS To ensure applicants have been accurately screened for PE. All PEDs must adhere to the performance standards and procedures as outlined below: 100% of PE screening results are submitted to HSD/MAD for auditing purposes 90% of applications received result in an approval of ongoing Medicaid eligibility Utilize the New Mexico Medicaid Portal (Portal) to verify current individual eligibility and/or enrollment status Utilize the New Mexico Medicaid electronic PE screening tool, YESNM-PE, to screen for and submit PE screening applications Utilize the Portal to submit all PE approvals, unless a system error or power outage or a lack of an applicant’s Social Security Number necessitates the submission of the PE via fax. In instances where a fax approval is submitted, the PED must use the Presumptive Eligibility Approval form (MAD 070; Rev 3/6/14) for the submission. PEDs must submit the PE approval on the day of the PE determination HSD may terminate PED status immediately if the Code of Conduct is breached or if the PED fails to comply with HSD guidelines. PROVIDER STATUS AND AGREEMENT I affirm that I am eligible to participate as PED as I am employed by and physically doing business at an entity that meets the qualifications of a PE Provider location. I understand that as a PED, I will use HSD’s systems, forms and methodology to screen applicants for Medicaid PE. I will also encourage and assist all individuals that I screen for PE to submit an application for ongoing Medicaid coverage. As a PED, I understand that I am required to maintain client confidentiality and adhere to the Health Insurance Portability and Accountability Act (HIPAA) Privacy rules. Any HIPAA violations, misuse of client information or unethical practices will be grounds for immediate revocation of my status as a qualified PED. I understand that when I provide application assistance, I am acting solely on behalf of the applicant and not HSD, and I agree to assume all responsibility and liability for protecting case record information, PII and PHI that the applicant provides to me. I agree to notify HSD within 24 hours of the receipt of any unofficial or unauthorized verbal or written requests for any PII or PHI of applicants. I agree to communicate to HSD any questions or concerns about the security of PII and PHI of applicants, and I agree to notify HSD no later than 24 hours after I become aware of or suspect an actual or possible incident of unauthorized access of PII and PHI, computer security incident, weakness, misuse or violation of any policy related to the security and protection of client and applicant PII and PHI. I understand that I will not be paid for determining PE and that I cannot bill any additional time included in the office visit for determining PE for applicants. I understand that I must keep complete and thorough records on all PE clients and that these records are subject to review by state and/or federal agencies. I understand I must sign and abide by the Presumptive Eligibility Determiner Agreement and Code of Conduct. Failure to sign this Agreement or to comply with HSD guidelines for establishing PE status may result in denial of application for Determiner status or immediate termination of determiner status by HSD/MAD. PED Name PED Title PED’s Employer (No Abbreviations) PED’s Direct Telephone Number/Extension Physical Address City State Zip Code State Zip Code Billing Address City PED’s Work E-MAIL Address: By signing this document, I agree to abide by the PE Determiner Code of Conduct and comply with HSD's guidelines for establishing PE status and submission. Either party may terminate this Agreement without cause, with fourteen (14) days written notice. HSD may exercise its right to terminate a PE Determiner’s status immediately for cause if the PED breaches the Code of Conduct or fails to comply with HSD guidelines. Certified PE Determiner Name (Please Print) PE Determiner’s Signature Date Official Use Only Provider Type HSD/MAD PE Program Staff: 170 MAD 219 5/1/14 – Page 2 171 PED # Assigned Test Date Test Score Information Sheet for Medicaid Application for Assistance Human Services Department benefits: Medicaid: Provides health care for certain people and families with low incomes and resources. Depending on your income and resources you may qualify for full or partial benefits. (If you do not qualify for Medicaid, your application will be automatically forwarded to the Health Insurance Marketplace where you may be eligible for other health insurance affordability programs.) Depending on your income you may qualify for full or partial benefits. The following are types of Medicaid that you may qualify for: • • • • • Newborns Children up to age 18 Parent(s)/Caretaker(s) Pregnant women Low-income adults • Emergency Services for Aliens Apply for the benefits above online at: www.yes.state.nm.us/selfservice. Or Send your complete, signed application to your local Income Support Division office or mail it to: Health Insurance Marketplace • The marketplace is a way to shop for and compare health insurance plans for individuals and families who are not eligible for Medicaid. • You may qualify for a program that can help you pay for a health insurance even if you earn as much as $94,000 a year (for a family of 4). • New tax subsidies that can immediately help pay your premiums for health coverage may be available. To apply for health insurance online through the Health Insurance Marketplace, you can go to: www.bewellnm.com Or Central ASPEN Scanning Area (CASA) PO BOX 830 Bernalillo, NM 87004 Call 1-855-99NMHIX (996-6449) TTY: 1-855-889-4325 MAD100 01/21/2014 Page 1 of 13 MEDICAID APPLICATION FOR ASSISTANCE Si Ud. necesita este formulario en español, comuníquese con su trabajador(a). Intérpretes están disponibles gratuitamente. Check the assistance program(s) you are applying for: (adults not Assistance Programs seeking assistance for themselves may apply on behalf of other household members) Depending on your income an individual may qualify for full or partial benefits. The following are types of Medicaid that you may qualify for: • • • • • • MEDICAID (If you or your household does not qualify for Medicaid, your application will be automatically forwarded to the Health Insurance Marketplace where you or your household may be eligible for other health insurance affordability programs.) Newborns Children up to age 18 Parent(s)/Caretaker(s) Pregnant women Low-income adults Emergency Services for Aliens HEALTH INSURANCE MARKETPLACE The marketplace is a way to shop for and compare health insurance plans. Individuals and families who are not eligible for Medicaid may be eligible to receive a new tax subsidy that can immediately help pay for health insurance premiums. 1. Tell Us About You: If you need help filling in this application or in getting the needed information, contact your local ISD office. If you are applying for someone else, complete this section for that person. First Name, Middle Initial, Last Name E-Mail Address Best Time to Contact You Morning Street Address City County State Zip Code Telephone Number ( ) If your mailing address is different, please fill it in below. If not, please leave blank. Street or PO Box Address Are you a resident of New Mexico? YES NO City State Do you intend to remain in New Mexico? YES NO Zip Code Are you homeless? YES NO Do you want to receive information electronically? If YES, please fill out your most current e-mail address above. Yes No 2. Person to Represent You (Authorized Representative or Guardian) The authorized representative may or may not be the same individual designated as an authorized representative for the application processing or for meeting reporting requirements. The authorized representative designation must be made in writing. Do you want this person to: Name of Authorized Person(s) Apply for benefits on your behalf? Mailing Address Preferred Telephone # / TDD ( ) ( ) MAD100 01/21/2014 Page 2 of 13 3. Tell us About the People who live with You: Please list everyone that lives in your household even if you do not want to apply for them. You only have to give U.S. Citizenship and Social Security Numbers for those household members that you are applying for. Remember that you do not need to be a U.S. Citizen to apply. Receiving SNAP/food, energy or medical assistance will not prevent you from becoming a lawful permanent resident or U.S. Citizen. Non-citizen immigrants not requesting assistance for themselves do not need to give immigration status information, Social Security Numbers, or other similar proofs; however, they must give proof of income and things they own because part of their income and things they own may count towards the household’s eligibility for assistance. Certain benefits may be available for people without a Social Security Number; ask ISD. If needed, please use an additional sheet of paper for additional household members who do not fit on this page. List the names and information for yourself and all the people who live with you: Name (First and Last) 1. Relationship (Self) Sex M/F Date of Birth Race & Ethnicity (Optional) SSN # (Optional for non-applicants) Fill out this section only for each person applying for benefits. U.S. Citizen Y/N Legal immigrant status? Y/N Will you file federal income taxes for the current year? Y/N Will you claim this person on your current year’s tax return? Y/N M Y Y Y Y 2. M Y Y Y Y 3. M Y Y Y Y 4. M Y Y Y Y 5. M Y Y Y Y 6. M Y Y Y Y 7. M Y Y Y Y 8. M Y Y Y Y Racial and ethnic data on participating households is voluntary, it will not affect the eligibility or the amount of benefits your household will receive. Native Americans are urged to identify themselves as such because Native Americans are entitled to certain special protections under the law. The reason we ask everyone for racial and ethnic information is to assure that benefits are distributed without regard to race, color, or national origin. 4. Please answer these Federal Income Tax Questions only about the people listed in Section 3 who will NOT be claimed as the applicant’s tax dependents if they appear on a different tax return. *Applicant can still get Medicaid if they don’t file Federal taxes. Please list each individual tax filer and their dependent that are listed on the application, below. Tax filer 1.___________________ Dependent Name:_________________; Relationship:___________________ Dependent Name:_________________; Relationship:___________________ Tax filer 2.___________________ Dependent Name:_________________; Relationship:___________________ Dependent Name:_________________; Relationship:___________________ Tax filer 3.___________________ Dependent Name:_________________; Relationship:___________________ Dependent Name:_________________; Relationship:___________________ MAD100 01/21/2014 Page 3 of 13 5. Please Answer the Following Questions About the People You Listed in Section 3 who are seeking health coverage. List all individuals applying for coverage who have legal immigration status and add information below. Who?____________________; Document Type_________________; ID Number:___________________ Who?____________________; Document Type_________________; ID Number:___________________ Who?____________________; Document Type_________________; ID Number:___________________ Has any non-citizen applicant lived in the U.S. since 1996? Who ________________________ Is any non-citizen applicant or spouse or parent a veteran or on active duty with the U.S military? Who: ______________ Is any applicant getting benefits in another state? If, YES, Who? ________________________ Yes No Is any applicant already in or going into a nursing home, hospital or treatment facility? Who? _________________ If, YES, what type of facility: Nursing Home/ Nursing Facility Intermediate Care facility for the Mentally Retarded (ICFMR) Other: Hospital Yes No PACE If other, where? _________________________ Yes No Is anyone disabled? Who? _______________________________ Is any applicant in the household receiving Supplemental Security Income (SSI)? Yes No Who? ______________________________Which State? _____________________________ Is anyone in the household pregnant? Who? _____________________________ How many babies are expected from this pregnancy? ______ Estimated Due Date ______________ Yes No Name of the Father of the unborn? (optional)_____________________ Has any applicant received a Primary Freedom Of Choice letter for a Home and Community Based Services Waiver? If, YES, Who? _______________________________ In any applicant a former Foster care recipient under the age of 26? If Yes, Who? ___________________ Yes No Yes No 6. Tell Us About Your Earned Income Note: If you are offered health insurance from any employer please fill out the Employer Coverage form attached to this application. Have you or has anyone living with you received earned income or expect to receive income this month? If yes, please complete the chart below. Person with income Average number of hours worked? Income from? (work, selfemployment, odd job) How Often Received? (Yearly, Monthly, Biweekly, Weekly, etc) Yes No Don’t Know How much do they receive? Does this employer offer Health Insurance? (Y/N) If yes, fill out the employer coverage form attached. $ $ $ $ Y Y Y Y MAD100 01/21/2014 Page 4 of 13 Tell Us About Your Other Income: Examples of unearned income include, but are not limited to: Unemployment, Social Security, pensions, retirement, rental income, Indian monies, capital gains, dividends/interest, and per capita payments. Note: You don’t need to tell us about child support, veteran’s payment or Supplemental Security Income (SSI) Person with income Unearned Income from? How Often Received? How much do they receive? (Yearly, Monthly, Biweekly, Weekly, etc) $ $ $ 7. Will There be Changes in Income? Do you or anyone living with you have changes in income that is not steady from month to month? Examples include: Loss of job, decrease in hours, change in job, change in pay, and/or only working some of the months, out of the year? Person Income When Yes No Don’t know Why Deductions? If you pay for certain things that can be deducted on a federal income tax return, tell us about them. Alimony Paid $_________ How Often? _________ IRA Deductions $________ How Often? _________ Student Loan Interest $_________ How Often? _________ Other: Type _________________ How Much $_________ How Often? ____________ Other: Type _________________ How Much $_________ How Often? ____________ 8. Parents Not Living with Their Children By accepting medical assistance for your children, you assign (give) HSD rights to collect child support from an absent parent. Please list all the information for your children’s parent(s) who are not living with you: If you think cooperating to collect medical support will harm you or your children, you may not have to cooperate. Is any applicant a victim of Family Violence? Child Name Yes No Absent Parent Name 9. Health Care Information Has anyone in the household received medical services within the last 3 months that have not been paid? If yes, please list the members who have the bills and for which months. We may be able to help pay these bills. a._____________________________; b._____________________________; c._________________________ Yes No Does anyone in your household have health insurance? Yes No If Yes, please list all public and private health insurance including Medicare information for you and all people living with you. Medicare Claim # or Persons Covered Insurance Company Name Start Date Insurance Member ID # MAD100 01/21/2014 Page 5 of 13 10. Managed Care Organization (MCO) (If you are applying for Medicaid on or after December 1, 2013) This section will ONLY apply if you are found to be eligible for Medicaid. Beginning January 1, 2014 Medicaid services will provided by the four Managed Care Organizations (MCO(s) listed below. You have a choice of which MCO provides your services. If you do not choose an MCO by January 1, 2014, you will be automatically assigned to an MCO by the State. Once you are enrolled with an MCO, you will have the option to change the MCO within 90 days of enrollment. Special information for Native Americans about Managed Care Organizations If you are Native American, you are not required to choose an MCO. If you are in need of long- term care services or have Medicare, you will be required to choose one. I am a Native American. Yes No (If yes, please complete the Native American or Alaskan Native information after this section) Do you want to enroll in a Managed Care Organization? Yes No (If yes, please select an MCO below) Blue Cross Blue Shield (BCBS) By checking this box, I wish to enroll all Medicaid recipients in my household with this MCO. By checking this box, I wish to enroll all Medicaid recipients in my household with this MCO. or Only the Medicaid recipients from this household that are listed here should be enrolled with BCBS:__________________________________ or Only the Medicaid recipients from this household that are listed here should be enrolled with Molina:__________________________________ Presbyterian Health Plan By checking this box, I wish to enroll all Medicaid recipients in my household with this MCO. United Healthcare Community Plan By checking this box, I wish to enroll all Medicaid recipients in my household with this MCO. or Only the Medicaid recipients from this household that are listed here should be enrolled with Presbyterian:__________________________________ Molina Healthcare of New Mexico or Only the Medicaid recipients from this household that are listed here should be enrolled with United:__________________________________ Native American or Alaska Native Native American and Alaska Natives who enroll in Medicaid, the Children’s Health Insurance Program (CHIP), and the Health Insurance Marketplace can also get services from the Indian Health Services, tribal health programs, or urban Indian health programs. If you or your family members are Native American or Alaska Native, you may not have to pay cost sharing and may get special monthly enrollment periods. We are asking you to answer the following questions to make sure you and your family get the most help possible. NOTE: If you need more space please attach another piece of paper. Is any applicant a member of a federally recognized tribe? Yes No If yes, Who? ________________________ What Tribe? _______________________ Do these applicants ever get a service from the Indian Health Service, a tribal health program, or urban Indian health program or through a referral from one of these programs? Yes No If no, is this person eligible to get services from the Indian Health Service, tribal health programs, or urban Indian health programs or through a referral from one of these programs? Yes No Certain money received may not be counted for Medicaid or CHIP. Does the income reported in Section 6, include money from any of the following sources? Per capita payments from a tribe that come from natural resources, usage rights, leases or royalties? Yes No If Yes, Who________________ $____________ How Often? _____________ MAD100 01/21/2014 Page 6 of 13 Payments from natural resources, farming, ranching, fishing, leases or royalties from land designated as Indian trust land by the Department of Interior (including reservations and former reservations)? Money from selling things that have cultural significance? Yes No If Yes, Who________________ $____________ How Often? _____________ Yes No If Yes, Who________________ $____________ How Often? _____________ 11. Your Signature (Your authorized representative may also sign here) Your signature makes this application valid and cannot be processed unless signed. Your signature also is an indication of the following: I understand that making false statements or hiding information could mean State and Federal penalties and I have given HSD true, correct and complete information. I am declaring the identity of the children under age 16 for whom I am applying. I will give proof of things I report to HSD. If I cannot get proof, I know that I can ask HSD to help me and I will let HSD contact other people, and companies to get proof. I will let HSD give limited information to approved agencies which give other related help for which I may be eligible. I understand that if I receive benefits for which I am not eligible, that I may have to pay HSD back for those benefits. I confirm that no one applying for health insurance on this application is incarcerated (detained or jailed). If not, ______________ is incarcerated. I know that HSD will check the information that I give. HSD may use computers or other means to check the information on this form. I know that HSD will check the immigration status of people who apply for or get benefits. I understand that immigration status for any household member that I am applying for may be subject to verification by USCIS (INS), and that it may affect the household's eligibility and level of benefits. I understand that I must cooperate with Quality Control (QC). QC is a part of HSD. QC reviews cases to make sure we determine who can get help correctly. TRUSTS - I understand that if I, or the person(s) for whom I am applying, have set up a trust, or are the beneficiaries of a trust, I must give HSD a copy of the trust document, including all attachments and related information. HSD will analyze the trust to see if it affects the Medicaid benefits for which I am applying. ESTATE RECOVERY- I understand that, after my death, HSD can file a claim against my estate to recover the amounts that the state pays or paid on my behalf for medical assistance provided under the Medicaid program. This process is called “Estate Recovery.” “Estate Recovery” is required by federal and state law. “Estate Recovery” is required where Medicaid recipients are fifty-five (55) years of age or older and the state makes medical assistance payments on their behalf for nursing facilities services, home and community based services, and/or related hospital and prescription drug services. The amount recovered by HSD will not exceed the amount of medical assistance payments made on behalf of the Medicaid recipient. Some exclusion’s may apply. I understand that I must give HSD any money I receive for medical services which have already been paid for by Medicaid. If I fail to do so, I, or the person(s) for whom I am applying, may lose Medicaid coverage for at least one year AND until the amount owed to Medicaid has been paid back in full. A person who is applying for or receiving Medicaid Assistance shall assign to HSD all rights against any and all individuals for medical support or payments for medical expenses paid on the applicants’ or client’s behalf and the behalf of any other person for whom application is made or assistance is received. I, as the Authorized Representative, affirm and agree to be legally bound to maintain the confidentiality of any information regarding the applicant or beneficiary, shall not reassign any provider claims, if applicable, and shall adhere to all requirements set forth in 42 CFR 435.923(d). To withdraw your application for any program, initial the box of the program ► Medicaid Marketplace Applicant’s Signature Name of Witness (Witnessed only if applicant signs by mark or thumbprint) Date Signature of Applicant’s Authorized Representative Signature of Witness (Witnessed only if applicant signs by mark or thumbprint) Date SPECIAL NEEDS INFORMATION If you are a person with a disability and you require this information in an alternative format, or require a special accommodation to participate in any public hearing, program or services, please contact the NM Human Services Department toll-free at 1-800-432-6217 or through the New Mexico Relay System TDD at 1-800-659-8331 or by dialing 711. The Department requests at least 10 days advance notice to provide requested alternative formats and special accommodations. (08/22/08) 12. Register to Vote If YOU are NOT registered to vote where you live now, Would you like to register to vote here today? (Please check one) YES NO IF YOU DO NOT CHECK EITHER BOX, YOU WILL BE CONSIDERED TO HAVE DECIDED NOT TO REGISTER TO VOTE AT THIS TIME. The NATIONAL VOTER REGISTRATION ACT provides you with the opportunity to register to vote at this location. If you would like help in filling out a voter registration application form, we will help you. The decision whether to seek or accept help is yours. You may fill out the application form in private. IMPORTANT: Applying to register or declining to register to vote WILL NOT AFFECT the amount of assistance that you will be provided by this agency. Signature Date CONFIDENTIALITY: Whether you decide to register to vote or not, your decision will remain confidential. IF YOU BELIEVE THAT SOMEONE HAS INTERFERED with your right to register or to decline to register to vote, or your right to privacy in deciding whether to register or in applying to register to vote, or your right to choose your own political party or other political preference, you may file a complaint with the Office of the Secretary of State, 419 State Capital, Santa Fe, NM, 87503, (phone: 1-800-477-3632). MAD100 01/21/2014 Page 7 of 13 MAD100 01/21/2014 Page 8 of 13 Program Application Information 1. Special Needs Information (Applicant Information Pages) SPECIAL NEEDS INFORMATION If you are a person with a disability and you require this information in an alternative format, or require a special accommodation to participate in any public hearing, program or services, please contact the NM Human Services Department toll-free at 1-800-432-6217 or through the New Mexico Relay System TDD at 1-800-659-8331 or by dialing 711. The Department requests at least 10 days advance notice to provide requested alternative formats and special accommodations. (08/22/08) 2. Your Civil Rights All programs administered by the Human Services Department (HSD) are equal opportunity programs. If you believe you have been treated unfairly because of race, color, national origin, age, disability, and where applicable, sex, marital status, familial status, parental status, religion, sexual orientation, genetic information, political beliefs, reprisal, or because all or part of an individual’s income is derived from any public assistance program, you may file a complaint. Complaints of discrimination may be filed with the New Mexico Human Services Department central office or the local Human Services county office. In accordance with Federal Law and, this institution is prohibited from discriminating on the basis of race, color, national origin, sex, age, religion, political beliefs, or disability. To file a complaint of discrimination, write USDA, Director, Office of Adjudication, 1400 Independence Avenue, SW, Washington, D.C. 20250-9410 or call toll free (866) 632-9992 (Voice). Individuals who are hearing impaired or have speech disabilities may contact USDA through the Federal Relay Service at (800) 877-8339; or (800) 845-6136 (Spanish). 3. Your Privacy The information you give HSD will be used to determine whether your household is eligible or continues to be eligible to take part in HSD programs. We will check this information through computer matching programs or other means. This information will also be used to make sure that you meet program rules and help us to manage the program. This information may be given to other Federal and State agencies for official examination, and to law enforcement officials for the purpose of picking up persons fleeing to avoid the law. If you get benefits that you were not eligible for and have to pay them back, this is called a claim. If your household gets a claim against it, the information on this application including all Social Security Numbers, may be given to Federal and State agencies, as well as private claims collection agencies for claims collection action. Providing the requested information, including Social Security Numbers of each household member is voluntary. However, except for non-citizens applying for emergency services, HSD will not provide benefits to applicants who do not disclose their immigration status. HSD will not attempt to determine, via INS, the immigration status of non-applicant household members who do not provide their immigration status. Non-Citizen Immigrants not requesting assistance for themselves do not need to give immigration status information or Social Security Numbers. Any Social Security Numbers given will be used and disclosed in the same manner as Social Security Numbers of eligible household members. We also check with other agencies, the federal Income and Eligibility Verification Service (IEVS) and The Public Assistance Reporting Information System (PARIS) about the information that you give us. This information may affect your household eligibility and benefit amount. 4. Child Support Enforcement Division By accepting medical assistance, you assign (give) HSD rights to collect child support from the child’s absent parent(s). You must help HSD find the absent parent(s) unless there is a good reason not to do so such as domestic violence; ask a caseworker. If it is decided that you have to work with the Child Support office to establish or enforce child support and you do not, benefits may be eventually lost, and adults may lose their medical assistance. 5. Interview How soon can I have my required appointment for an interview? The Medical assistance programs on this application do not require an interview. 6. Proof Information (a) How many days will I have to give all the required proof I need? 10 days from the date of your application is best to receive benefits faster 45 days from the date of your application is typical – unless you need more time – If you need more time, ask for more time 60 days from the date of your application is the longest – When you ask for up to 3-ten-day extensions If you do not ask for an extension of time to bring in proof, your case may be denied after 30 days. (b) What proof should I bring to the interview? Your caseworker will NOT ask you to give proof of everything. You should be ready to give as many facts about your case as you can. If your caseworker has unresolved questions about your eligibility, you will be asked to give proof. Your caseworker will give you a list of everything you still need to give, along with a receipt for proof you provided. If you need help, ask your caseworker for help. MAD100 01/21/2014 Page 9 of 13 7. Non-Citizen Immigrant Eligibility (a) What types of Non-Citizen Immigrants are eligible for HSD assistance programs? For most programs, non-citizens must have a "qualified" immigrant status and meet certain other conditions to qualify. Most non-citizens in the following categories can get benefits if they meet all other program eligibility requirements: Lawful Perm. Res. (LPRs) Amerasians Certain: Refugees Paroled to U.S. – 1 year Battered women and children Canada/Mexico born Native American Asylees Withholding of Deportation Veterans, active duty military Human Trafficking Victims Cuban Haitian Entrants Hmong or Laotian Tribe Certain non-citizens, including undocumented non-citizens may be eligible for emergency medical services including pregnant women’s labor and delivery. (b) Is there a waiting period (bar) before non-citizen immigrants can get benefits? The general rule now is that most qualified immigrant children are eligible to receive Medical Assistance. However some “qualified” immigrant adults can get benefits after they have been in the United States in “qualified” immigrant status for five years, and some immigrants can get them right away. In general, adults in certain humanitarian immigration categories (such as Refugees and Asylees), people with military connections lawfully present pregnant women and children, credit for 10 years of work history in the US, and persons receiving disability benefits may be eligible right away. 8. After your Interview (a) How soon will my application be approved or denied? Medical – No later than 45 calendar days after the date of application (b) If I disagree with the eligibility decision or benefit level, can I have fair hearing? Yes - If you don't agree with a decision we make about your case, you can ask for a fair hearing in person, by telephone 1-800-432-6217 or (505) 827-8164, or in writing within 90-days of the date that a notice has been sent informing you of any action that has been taken on your case. Please mail your request to the HSD Hearing’s Bureau at PO Box 2348 Santa Fe, NM 87504. You have a right to look at your case file and any records HSD used to determine your eligibility before your hearing. You can ask a household member or someone else like a friend or relative to represent your household at the fair hearing. You also have the right to have an attorney or other legal representative at the hearing. (c) From what date are my benefits calculated? Medical – From the 1st day of the month you applied. You may be eligible for up to 3 prior months of Medicaid coverage. (d) How will I get my benefits? Medical - A Medicaid card will be mailed to you one working day after the date of approval. (e) How long can I get benefits before I have to renew them? Medical – Up to 12 months is typical (f) Do I have to report changes? Always report address changes within 10 calendar days for all types of assistance programs. Medical – For adults, report all changes within 10 calendar days. For families with children and pregnant women, you only have to report address changes within 10 calendar days. All other changes will have to be reported the next time you renew your case. 9. Notice of Rights CONFIDENTIALITY All information I give to HSD is confidential. This information will be given to HSD employees who need it to manage the programs for which I have applied. Confidential information may also be released to other federal and state agencies. All information will be used to determine eligibility and/or to provide services. (03/29/12) CIVIL RIGHTS STATEMENT All programs administered by the Human Services Department (HSD) are equal opportunity programs. If you believe you have been treated unfairly because of race, color, national origin, age, disability, and where applicable, sex, marital status, familial status, parental status, religion, sexual orientation, genetic information, political beliefs, reprisal, or because all or part of an individual’s income is derived from any public assistance program, you may file a complaint. Complaints of discrimination may be filed with the New Mexico Human Services Department central office, ATTN: Quality Improvement Section, Pollon Plaza, P. O. Box 2348, Santa Fe, New Mexico 87504-2348 or the local Human Services county office. Complaints of discrimination about the Supplemental Nutrition Assistance Program may be filed with the USDA, Director, Office of Adjudication, 1400 Independence Ave, S.W. Washington, DC 20250-9410 or call 1-866-632-9992 or 202-401-0216 (TDD). Complaints of discrimination about Medical Assistance programs may be filed with the Office of Civil Rights, Department of Health & Human Services, 1301 Young Street, Suite 1169, Dallas, TX 75202 or call 1-800-368-1019 (voice) and 1-214-767-8940 (TDD). (08/16/11) YOUR RIGHT TO A HEARING - You can ask for a hearing if you do not agree with a decision HSD has made regarding your application/benefits. A hearing will give you a chance to explain why you do not agree. You can ask for an HSD hearing by: • Completing and returning the bottom of a notice; • Writing or calling your local HSD office; or MAD100 01/21/2014 Page 10 of 13 • • Writing the department's Hearings Bureau at Human Services Department, P.O. Box 2348, Santa Fe, N.M. 87504-2348, or by calling 1-800432-6217 (press 6) or 505-476-6213. (Revised 08/16/11) Marketplace HEARING - I know that if I believe the Marketplace has made a mistake about my eligibility, I may appeal the action by contacting the Health Insurance Exchange at 1-800-318-2596 and properly inform it that I believe their action should be reviewed. I know I may authorize someone else to represent me in the appeals process. TIME LIMIT FOR ASKING FOR A HEARING - You have 90 days from the date of this notice to ask for a hearing. If you ask for a hearing within 13 days from the date of this notice, you will continue to get the same amount of benefits you received before we took the action in this notice. You will continue to get these benefits until the Department decides your case, unless another change is made to your case. Changes in benefits may be made after you have asked for a hearing if the reason for the change is not the same as the reason for the hearing. If you lose the hearing, you may have to pay back any benefits you received while the Department decided your case. (Revised 9/24/02) THE HEARING PROCESS - After you ask for a hearing, the Department or the Marketplace will send you a letter telling you the date, time and place where your hearing will be held. The hearing is usually at the HSD county office. The hearing will be conducted by a hearing officer from the HSD Hearings Bureau or the Marketplace. You or your representative can look at your case record and any proof we used to decide your case. You will tell why you believe HSD’s or Marketplace action was wrong. You may bring witnesses and present proof. You may question the county office or the Marketplace about the action taken and proof presented. You may represent yourself. You may be represented by a friend, household member or an attorney. For information on where you can get free legal help, call 1-800-340-9771. After the hearing, the hearing officer will make a report. The HSD Division Director or Marketplace Executive Director will decide whether the action was right or wrong. After the Director has decided your case, you will be sent a letter telling you of the decision and why the decision was made. (Revised 04/02/03) MAD100 01/21/2014 Page 11 of 13 Employer Coverage Form Applying for help with health insurance costs from the Health Insurance marketplace? The Health Insurance Marketplace application asks questions about any health coverage available through a current job (even if it’s from another person’s job, like a parent or spouse) to figure out if you might be able to get help paying for health insurance. Use this form to get the information you need from the employer who offers health coverage. We’ll verify this information, so it’s important to be accurate. If you have more than one job that offers health coverage, use a separate form for each employer. Employee Information The employee needs to fill out this section. Write down the employee’s information then you may request the information below from the employer. Use this completed form when you fill out a Health Insurance Marketplace application. Employee Name (First, Middle, Last) Social Security Number Employer Information Ask the employer for this information Employer name Employer Identification Number (EIN) Employer Address Employer Phone Number ( ) – State Zip code City Who can we contact about employee health coverage at this job? Name:____________________________ Phone:_________________ Email:_______________________ Tell us about the health plan offered by this employer. This employee isn’t eligible for coverage under this employer’s plan. The employee is eligible for coverage under this employer’s plan on___________________ (Start Date). What’s the name of the lowest cost self-only health plan this employee could enroll in at this job? (Only consider plans that meet the “minimum value standard” set by the Affordable Care Act.) Name:_______________________________________________________ No plans meet the “minimum value standard” How much would the employee have to pay in premiums for that plan? $__________ How Often? Weekly Every 2 weeks Twice a month Monthly Yearly Other___________ MAD100 01/21/2014 Page 12 of 13 Register to Vote PERSONAL INFORMATION NAME: Last First Middle Name or Initial 1 PHYSICAL STREET ADDRESS WHERE YOU LIVE NOW Street Address Apartment, Unit, or Lot # Gender M This information not to be copied Birth Date Social Security Number City Zip 2 ADDRESS WHERE YOU GET YOUR MAIL Address (If different from above) City Zip Site Code 3 If you are changing your name on this application, under what Last Name First Name Middle Name or Initial 4 full name were you previously registered? POLITICAL PARTY POLL WORKER DAY TIME TELEPHONE NUMBER (Optional) NOTE: You must name a major Party If you choose NO PARTY, May the County Clerk make this Would you like to serve political party to vote in primary Check this box 6 telephone number public for as an election day Democrat 5 elections. election purposes? Yes No precinct worker? Yes I hereby authorize you to cancel my previous City or Township County State 7 registration in the following county and state. Please answer the following questions: ATTESTATION OF QUALIFICATION 8 I swear/affirm that I am a citizen of the United States and a resident of the state of New Mexico; that I have not been denied the right to vote by a court of law by reason of mental incapacity; that I am, or will be at the time of the next election, 18 years of age; and if I have been convicted of a felony, I have completed all conditions of parole and supervised probation, served the entirety of sentence or have been granted a pardon by the governor. I further swear/affirm that I am authorizing cancellation of any prior registration to vote in the jurisdiction of my prior residence; and that all the information I have provided is correct. Are you a citizen of the United States? ………………………………… Yes No Will you be 18 years of age on or before election day? ……………… Yes No If you checked “No” to any of the questions above, do not complete this form. If you have been convicted of a felony and are currently on parole or supervised probation do not complete this form. TODAY’S DATE Month Day Year ______/ ______ /______ SIGN YOUR FULL NAME OR MARK ON THE LINE BELOW:. Name of agent who assisted you in filling out this form. VRA ID # 9 DO NOT WRITE IN SHADDED AREAS – FOR OFFICIAL USE ONLY Accepted for filing in County Registration Records: ___________ / _________________________________ / _________________________________ Date County Clerk Filing Clerk ID PCT MUN SCHOOL CC PRG DIST REP DIST SEN DIST HSD Site Code I- Registrarse para Votar Esta información no se debe copia INFORMACION PERSONAL NOMBRE: Apellido Su Nombre de Pila Otro Nombre o Inicial Género Fechade Nacimiento Número de Seguro Social H 1 DIRECCION DONDE UD. VIVE AHORA Número y Nombre de la Calle Departamento, Unidad o # de Lote Ciudad Zona Postal 2 DIRECCION DONDE UD. RECIBE SU CORRESPONDENCIA Dirección Ciudad Zona Postal Site Code 3 ¿Si Ud. Va cambier su nombre en esta solicitud, bajo que Apellido Nombre de Pila Otro Nombre o Inicial nombre completo estaba Ud. Matriculado antes? 4 EMPLEADO / A EN URNA ELECTORAL PARTIDO POLITICO NUMERO DE TELEFONO EN EL DIA (Opcional) AVISO: Ud. tiene que indicar Partido Si Ud. NO ELIGE ¿Con motivo del elecciones ¿Quiere Ud. trabajar en recinto 5 partido politico principal para Partido marque aquí electoral el dia de la elección? 6 puede divulgar el escribano votar en la elección primaria de Condado esté núm. De Si Democrata teléfono? Si No Por la presente autorizo que Ud. cancele mi matrícula Ciudad o División Condado Estado 7 previa en el condado y estado a continuación. Favor de contestar las preguntas a continuación: TESTIMONIO DE CALIFICACION Ud. ciudadano / a de los Estados Unidos? ……………….…… Si No ¿Habrá cumplido Ud. 18 años en o antes del dia de la elección? Si No Si Ud. marcó “NO” en cualquiera de las preguntas más arriba no termine de rellenar este formulario. Si usted fue condenado de un delito grave y actualmente esta en libertad condicional o probación supervisada, no llene esta forma. ¿Es 8 FECHA: Mes Dia Año ______/______ /______ 9 Nombre de la persona que le ayudó a llenar este formulario: Yo juro/afirmo que soy ciudadano de los Estados Unidos y residente del Estado de Nuevo México; que la corte no me ha denegado el derecho de votar por motivo de incapacidad psicológica; que tengo o tendré 18 años de edad en la fecha de la próxima elección y si he sido condenado de delito grave he cumplido todas las condiciones de libertad a prueba o el gobernador me ha concedido indulto. Ademas, juro o afirmo que autorizo la cancelación de toda matrícula anterior con el fin de votar en el territorio de mi residencia previa; y que la informacion proveido esta correcto. FIRME SU NOMBRE COMPLETO O MARQUE LA LÍNEA ABAJO: VRA ID # NO ESCRIBA EN LOS ESPACIOS EN COLOR GRIS – SOLO PARA USO OFICIAL ID PCT MUN PRG DIST Accepted for filing in County Registration Records SCHOOL CC ________ / ______________________________ / _____________________________ Date County Clerk Filing Clerk REP DIST SEN DIST ISDB 720 Issued 3/5/12 MAD100 01/21/2014 Page 13 of 13 Hoja de Información para la Solicitud de Asistencia de Medicaid Beneficios del Departamento de Servicios Humanos: Mercado de Seguros Médicos Medicaid: provee atención médica para ciertas personas y familias con bajos ingresos y recursos. Dependiendo de sus ingresos y recursos usted puede calificar para los beneficios completos o parciales. (Si usted no califica para Medicaid, su solicitud será enviada automáticamente al mercado de seguros médicos donde usted puede ser elegible para otros programas de seguro de salud de bajo costo.) Dependiendo de sus ingresos, usted puede calificar para beneficios completos o parciales. Los siguientes son los tipos de Medicaid para cual usted puede calificar: Recién Nacidos Niños hasta la edad de 18 Padres(s)/Guardián(s) Mujeres Embarazadas Adultos con bajos ingresos Servicios de Emergencia para Extranjeros Solicite los beneficios mencionados anteriormente en línea al: www.yes.state.nm.us/selfservice. O Mande su solicitud completa y firmada a su oficina local de la División de Asistencia Económica o envíela a: Central ASPEN Scanning Area (CASA) PO BOX 830 Bernalillo, NM 87004 El Mercado es una manera de comprar y comparar los planes de seguro de salud para los individuos y las familias que no son elegibles para Medicaid. Usted puede calificar para un programa que le puede ayudar a pagar por seguro de salud, incluso si usted gana hasta $94,000 al año (para una familia de 4). Nuevos subsidios de impuestos que pueden ayudar a pagar inmediatamente las primas para la cobertura de salud pueden estar disponibles. Para solicitar un seguro médico a través del Mercado de Seguros Médicos, usted puede ir a: https://www.healthcare.gov/ O Llame 1-800-318-2596 TTY: 1-855-889-4325 MAD 100 Page 1 of 13 SOLICITUD PARA ASISTENCIA DE MEDICAID Intérpretes están disponibles gratuitamente. Seleccione los programas de asistencia cuales usted está solicitando: (adultos que no buscan Programas de Asistencia ayuda para sí mismos pueden solicitar de parte de otros miembros del hogar) Dependiendo de los ingresos y recursos un individuo puede calificar para los beneficios completos o parciales. Los siguientes son los tipos de Medicaid para cuál usted puede calificar: MEDICAID (Si usted o su familia no califican para Medicaid, su solicitud será enviada automáticamente al mercado de seguros médicos donde usted o su familia puede ser elegible para otros programas de seguros médicos de bajo costo.) Recién Nacidos Los niños de hasta 18 años Padre(s)/Guardián(es) Mujeres embarazadas Adultos con bajos ingresos Servicios de Emergencia para Extranjeros MERCADO DE SEGUROS MÉDICOS El Mercado es una manera comprar y comparar los planes de seguro de salud. Los individuos y las familias que no son elegibles para Medicaid, pueden ser elegibles para recibir un nuevo subsidio de impuesto que puede ayudar a pagar inmediatamente las primas de seguro de salud. 1. Díganos sobre usted: Si necesita ayuda para llenar esta solicitud o para obtener la información necesaria, póngase en contacto con su oficina local de ISD. Si usted solicita de parte de otra persona, complete esta sección para esa persona. Primer nombre, inicial del segundo nombre, Apellido Correo electrónico Mejor hora para llamar Manana Dirección Física Ciudad Condado Estado Código Postal Número de Teléfono ( ) Si su dirección postal es diferente, por favor llene a continuación. Si no, deje en blanco. Dirección Física o de PO Box Ciudad Estado Código Postal ¿Es usted un residente de Nuevo México? ¿Tiene la intención quedarse en Nuevo México? ¿Es usted una persona sin hogar? SÍ NO SÍ NO SÍ NO ¿Quiere recibir información por vía electrónica? Si quiere recibir, por favor, rellene su dirección de correo SÍ No electrónico arriba. 2. Persona Que lo Representa (Representante Autorizado o Tutor Legal) El representante autorizado podría ser o no ser la misma persona designada como representante autorizado para el procesamiento de la solicitud o para cumplir con los requisitos de reportes. La designación de un representante autorizado debe hacerse por escrito. ¿Usted quiere que esta persona: Nombre de la persona(s) autorizada(s) ¿Solicite beneficios en su nombre? Dirección de Correo # de Teléfono Preferido / TDD ( ) ( ) MAD 100 Page 2 of 13 3. Díganos sobre la gente que vive con usted: Por favor, liste a todos que viven en su hogar, incluso si usted no desea solicitar para ellos. Sólo tiene que dar información de ciudadanía de los EE.UU. y el número de seguro social para los miembros de la familia para quien está solicitando. Recuerde que usted no tiene que ser ciudadano de los EE.UU. para solicitar. Recibir SNAP/comida, asistencia de energía o médica no evitará que usted se convierta en un residente permanente legal o ciudadano de los EE.UU.. Inmigrantes que no son ciudadanos que no solicitan asistencia por sí mismos no tienen que dar información de estatus migratorio, números de Seguro Social, u otras pruebas similares, sin embargo, deben dar prueba de sus ingresos y cosas que poseen debido a que parte de sus ingresos y cosas que poseen pueden contar hacia la elegibilidad del hogar para recibir asistencia. Ciertos beneficios pueden ser disponibles para las personas sin número de Seguro Social, pregúntele a ISD. Si es necesario, use una hoja de papel adicional para los miembros del hogar adicionales que no caben en esta página. Anote los nombres y la información para usted y todas las personas que viven con usted: Nombre (Primer Nombre y Apellido) 1. Parentesco (sí mismo) Sexo M/F Fecha de Nacimiento Raza y etnicidad (Opcional) Llene esta sección SÓLO para cada persona que está solicitando beneficios. ¿Estatus de Ciudadano SSN # de EE.UU. inmigrante (Opcional para S/N legal? no-solicitantes) S/N ¿Va a declarar sus impuestos federales del año en curso? S/N ¿Va a reclamar a esta persona en la declaración de impuestos del año en curso? S/N H S S S S 2. H S S S S 3. H S S S S 4. H S S S S 5. H S S S S 6. H S S S S 7. H S S S S 8. H S S S S Datos raciales y étnicos en los hogares participantes son voluntarios, no afectará a la elegibilidad o la cantidad de beneficios que su hogar va a recibir. Se les recomienda a los indígenas americanos a identificarse como tal porque los indígenas americanos tienen derecho a ciertas protecciones especiales bajo la ley. La razón por la cual le pedimos a todos por información racial y étnica es para asegurar que los beneficios se distribuyen sin distinción de raza, color u origen nacional. 4. Por favor conteste estas preguntas de ingresos de impuestos federales sobre la gente listada en la sección 3 que NO será reclamada como dependiente de impuestos si están en otra declaración de impuestos del solicitante * Solicitante todavía puede obtener Medicaid si no declara los impuestos federales. Enumere cada individuo con declaración de impuestos y sus dependientes que están indicados en la solicitud, a continuación. Pagador de impuestos 1.__________________ Nombre del dependiente:_________________; Parentesco:___________________ Nombre del dependiente:_________________; Parentesco:___________________ Pagador de impuestos 2.__________________ Nombre del dependiente:_________________; Parentesco:__________________ Nombre del dependiente:_________________; Parentesco:___________________ Pagador de impuestos 3.__________________ Nombre del dependiente:_________________; Parentesco:___________________ Nombre del dependiente:_________________; Parentesco:___________________ MAD 100 Page 3 of 13 5. Por favor conteste estas preguntas sobre la gente listada en la sección 3 que solicita cobertura de seguro médico. Liste a todas las personas que solicitan cobertura que tienen el estatus de inmigrante legal y llene la información a continuación. ¿Quién?____________________; Tipo de Documento_________________; Número de ID:___________________ ¿Quién?____________________; Tipo de Documento_________________; Número de ID:___________________ ¿Quién?____________________; Tipo de Documento_________________; Número de ID:___________________ ¿El solicitante que no es ciudadano ha vivido en los EE.UU. desde 1996? ¿Quién? ________________________ ¿Hay un solicitante que no es ciudadano o hay un cónyuge o padre que es un veterano o en servicio activo en el ejército de EE.UU.? ¿Quién? ______________ ¿Hay un solicitante que recibe beneficios en otro estado? Si, Sí, ¿Quién? ________________________ Sí No ¿Está alguno de los solicitantes viviendo o está por entrar a un hogar de ancianos, enfermos, hospital o centro de Sí No tratamiento? ¿Quién? _________________ Casa/ institución de Si, Sí, que tipo de institución: PACE Hospital ancianos/enfermos Centro de Atención Intermedia para Personas con Retraso Si otro ¿dónde? _________________________ Otro: Mental (ICFMR) Sí No ¿Hay alguien incapacitado? ¿Quién? _______________________________ ¿Hay un solicitante en el hogar que recibe Seguridad de Ingreso Suplementario (SSI)? Sí No ¿Quién? ______________________________¿Cuál Estado? _____________________________ ¿Hay alguien en el hogar que está embarazada? ¿Quién? _____________________________ Sí No ¿Cuantos bebés se esperan de este embarazo? ______ Fecha Prevista del Parto ______________ ¿Nombre del padre del bebé no nacido? (opcional) _____________________ ¿Hay alguien que ha recibido una carta de Libertad Primaria de Selección para una Exención de Servicios Basados en la Comunidad y el Hogar? Sí No Si hay, ¿Quién? _______________________________ ¿Hay algún solicitante que fue receptor del cuidado de crianza bajo la edad de 26 años? Si lo hay, ¿Quién? ___________________ Sí No 6. Díganos sobre sus ingresos ganados Nota: Si se le ofrece un seguro médico de un empleador, por favor rellene el siguiente formulario de Cobertura de Empleador adjunta a esta solicitud ¿Usted o alguien que vive con usted ha recibido ingreso del trabajo o espera recibir ingresos este mes? Si es así, por favor completar la tabla siguiente. Persona con ingresos ¿Promedia de Horas Trabajadas? ¿Ingresos de? (trabajo, trabajo por cuenta propia, otro trabajo) ¿Cada cuando recibido? (Anual, Mensual, Bisemanal, Semanal, etc) Sí No No sé ¿Este empleador ofrece Seguro de Salud? (S/N) ¿Cuánto reciben? $ $ $ $ Si contestó sí complete el formulario de la cobertura del empleador en la página 16. S S S S MAD 100 Page 4 of 13 Díganos Sobre Sus Otros Ingresos: Ejemplos de ingresos no devengados del trabajo incluyen, pero no están limitados a: el desempleo, Seguro Social, pensiones, la jubilación, los ingresos de rentas, el dinero indígena, ganancias de capital, dividendos / intereses y los pagos per cápita. Note: No es necesario que nos diga de sostenimiento de niños, los pagos de veteranos o Seguridad de Ingreso Suplementario (SSI) ¿De dónde viene el ¿Cada cuando recibido? Persona con ingreso Ingreso no devengado de ¿Cuánto reciben? (Anual, Mensual, Bisemanal, Semanal, etc) un trabajo? $ $ $ 7. ¿Habrá Cambios en los Ingresos? ¿Usted o alguien que vive con usted tiene cambios en los ingresos que no son constantes de mes a mes? Ejemplos incluyen: pérdida de empleo, reducción de horas, cambio de trabajo, cambio de pago y / o trabajando sólo algunos de los meses del año Persona Ingresos Cuando Sí No No sé Por qué ¿Deducciones? Si usted paga por ciertas cosas que se pueden deducir en la declaración de impuestos federales, díganos acerca de esas cosas. Pensión alimenticia pagada $_______ ¿Con qué frecuencia?_______ Deducciones IRA $_______ ¿Con qué frecuencia?_______ Interés de préstamo de estudiante $_________ ¿Con qué frecuencia?_________ Otro: Tipo _________________ ¿Cuánto? $_________ ¿Con qué frecuencia?____________ Otro: Tipo _________________ ¿Cuánto? $_________ ¿Con qué frecuencia?____________ 8. Padres que no viven con sus hijos Con la aceptación de la asistencia médica para sus hijos, usted asigna (otorga) HSD derechos para cobrar manutención de un padre ausente. Por favor escriba toda la información para los padres de sus hijos que no viven con usted: Si usted piensa que cooperar para recolectar apoyo médico le hará daño a usted o a sus hijos, es posible que no Sí No tenga que cooperar. ¿Es algún solicitante una víctima de violencia familiar? Nombre del niño Nombre de padre ausente (opcional) 9. Información de Atención Médica ¿Alguien en su hogar ha recibido servicios médicos en los últimos 3 meses que no han sido pagados? Si es sí, indique los miembros que tienen las cuentas y para cuales meses. Puede ser que nosotros podamos ayudar a pagar estas cuentas. a._____________________________; b._____________________________; c._________________________ Sí No Sí No ¿Alguien en su hogar tiene seguro de salud? Si es así, indique la información de los seguros de salud privados y públicos incluyendo a Medicare para usted y todas las personas que viven con usted. # de Reclamo de Medicare Personas Cubiertas Nombre de la compañía de seguros o # de ID de Miembro de Seguro Fecha de inicio MAD 100 Page 5 of 13 10. Organización de Cuidado Administrado (MCO) (Si usted está solicitando Medicaid a partir del 01 de diciembre 2013) Esta sección SÓLO aplica si se encuentra ser elegible para Medicaid. A partir del 1 de enero 2014 los servicios de Medicaid serán proporcionados por las cuatro organizaciones de cuidado administrada (MCO (s) se enumeran a continuación. Usted tiene la opción de cual MCO proporciona sus servicios. Si usted no elige una MCO antes del 1 de enero de 2014, se le asignará automáticamente a una MCO por el Estado. Una vez que está inscrito con una MCO, usted tendrá la opción de cambiar de MCO dentro de 90 días de inscripción. Información especial para indígenas Americanos sobre organizaciones de cuidado administrado Si usted es un indígena Americano, usted no es requerido a escoger una MCO. Si usted está con la necesidad de servicios de atención a largo plazo o tiene Medicare tendrá que escoger una MCO. Yo soy indígena americano. Sí No (Si es así, por favor llene la sección de información de indígena americano o indígena de Alaska después de esta sección ) ¿Quiere inscribirse en una organización de cuidado administrado? Sí No (Si quiere inscribirse, favor de seleccionar un MCO a continuación) Al marcar esta casilla, quiero inscribir a todos los beneficiarios de Medicaid en mi hogar con esta MCO. o Sólo los beneficiarios de Medicaid de este hogar que están listados aquí deben estar inscritos con BCBS:__________________________________ Blue Cross Blue Shield (BCBS) Al marcar esta casilla, quiero inscribir a todos los beneficiarios de Medicaid en mi hogar con esta MCO. o Sólo los beneficiarios de Medicaid de este hogar que están listados aquí deben estar inscritos con Molina:__________________________________ Presbyterian Health Plan Al marcar esta casilla, quiero inscribir a todos los beneficiarios de Medicaid en mi hogar con esta MCO. o Sólo los beneficiarios de Medicaid de este hogar que están listados aquí deben estar inscritos con Presbyterian:__________________________________ Molina Healthcare of New Mexico United Healthcare Community Plan Al marcar esta casilla, quiero inscribir a todos los beneficiarios de Medicaid en mi hogar con esta MCO. o Sólo los beneficiarios de Medicaid de este hogar que están listados aquí deben estar inscritos con United:__________________________________ Indígena Americano o Indígena de Alaska Indígenas Americanos e Indígenas de Alaska que se inscriben en Medicaid, el Programa de Seguro de Salud de Niños (CHIP), y el Mercado de Seguros Médicos también pueden recibir servicios de Servicios Médicos para Indígenas, programas de salud tribal, o programas de salud de indígenas urbanos. Si usted o sus miembros de su familia son Indígenas Americanos o Indígenas de Alaska, puede ser que no tengan que pagar reparto de costos y pueden recibir periodos especiales de inscripción. Le pedimos que conteste las siguientes preguntas para asegurar que usted y su familia reciban toda la ayuda posible. NOTA: Si necesita más espacio adjunte otra hoja de papel. ¿Algún solicitante es miembro de una tribu reconocida por el gobierno federal? Sí No Si es así, ¿Quién? ________________________. ¿Cuál Tribu? _______________________ ¿Estos solicitantes reciben servicio del Servicio de Salud Indígena, un programa de salud tribal, o el programa de salud Sí No para indígenas urbanos o a través de una referencia de uno de estos programas? Si no ¿Es esta persona elegible para recibir servicios del Servicio de Salud Indígena, programas de salud tribal, o programas de salud para indígenas urbanos o a través de una referencia de uno de estos programas? Sí No Cierto dinero recibido no se puede contar para Medicaid o CHIP. ¿El ingreso reportado en la Sección 6, incluye dinero de cualquiera de las siguientes fuentes? ¿Pagos per cápita de una tribu que provienen de los recursos naturales, los derechos de uso, los arrendamientos y las regalías? ¿Los pagos de los recursos naturales, la agricultura, la ganadería, la pesca, los arrendamientos y regalías de la tierra designada como tierras fiduciarias india por el Departamento de Interior (incluidas las reservas y las reservas anteriores)? ¿Dinero de la venta de las cosas que tienen importancia cultural? Sí No Sí No Sí No MAD 100 Page 6 of 13 11. Su Firma (Su representante autorizado también puede firmar aquí) Su firma hace que esta solicitud sea válida y no puede ser procesada sin la firma. Su firma también es una indicación de lo siguiente: Entiendo que hacer declaraciones falsas u ocultar información podría significar penas estatales y federales y he dado a HSD información verdadera, correcta y completa. Estoy declarando la identidad de los niños menores de 16 años para quien estoy solicitando. Voy a dar prueba de lo que yo reporte a HSD. Si no puedo conseguir la prueba, sé que puedo pedir que me ayude HSD y dejaré que HSD contacte a otras personas y empresas para obtener pruebas. Voy a dejar que HSD dé información limitada a las agencias aprobadas que dan otro tipo de ayuda relacionada con lo que puedo ser elegible. Entiendo que si recibo beneficios para los que no soy elegible, que voy a tener que pagarle a HSD esos beneficios. Yo confirmo que nadie que solicita un seguro de salud en esta solicitud está encarcelado (detenido o encarcelado). Si no, ______________ está encarcelado. Yo sé que HSD verificará la información que yo provea. HSD puede utilizar las computadoras u otros medios para verificar la información en este formulario. Yo sé que HSD verificará el estatus migratorio de las personas que solicitan o reciben beneficios. Entiendo que el estatus migratorio de cualquier miembro de la casa que estoy solicitando puede ser objeto de verificación por parte de USCIS (INS), y que puede afectar la elegibilidad del hogar y el nivel de beneficios. Entiendo que debo cooperar con el control de calidad (QC). QC es una parte de HSD. QC revisa casos para asegurarnos que determinamos correctamente quién puede obtener ayuda. FIDEICOMISOS - Entiendo que si yo o la persona (s) para quien estoy solicitando, he creado un fideicomiso, o son beneficiarios de un fideicomiso, debo dar a HSD una copia del documento de fideicomiso, incluyendo todos los accesorios e información relacionada. HSD analizará el fideicomiso para ver si afecta a los beneficios de Medicaid para los que estoy solicitando. RECUPERACIÓN DE BIENES - Entiendo que, después de mi muerte, HSD puede presentar una reclamación en contra de mi patrimonio para recuperar las sumas que el Estado paga o pago en mi nombre por la asistencia médica proporcionada bajo del programa de Medicaid. Este proceso se llama "recuperación de bienes." "Recuperación de Bienes" es requerido por la ley federal y estatal. "Recuperación de Bienes" es necesario cuando los beneficiarios de Medicaid tienen cincuenta y cinco (55) años de edad o más y el Estado hace pagos de asistencia médica en su nombre por los servicios de institución de enfermería, servicios basados en el hogar y en la comunidad, y/o servicios de hospitalización y medicamentos recetados. La cantidad recuperada por HSD no superará la cantidad de pagos de asistencia médica realizada en nombre del beneficiario de Medicaid. Se pueden aplicar algunas exclusiones. Entiendo que debo dar a HSD dinero que recibo por los servicios médicos que ya han sido pagados por Medicaid. Si yo no lo hago, yo o la persona(s) para quien estoy solicitando, podría perder la cobertura de Medicaid por lo menos durante un año y hasta que el monto adeudado a Medicaid ha sido pagado en su totalidad. Una persona que está solicitando o recibiendo Asistencia de Medicaid debe asignar a HSD todos los derechos contra cualquier y todos los individuos de apoyo médico o pagos por gastos médicos pagados en nombre del cliente y en nombre de cualquier otra persona para la que se solicite o se recibe ayuda. Para retirar su solicitud de cualquier programa, iníciale en la casilla del programa ► Medicaid Mercado Firma del solicitante Nombre del Testigo (Atestiguado sólo si el solicitante firma con una marca o huella) Fecha Firma del representante del solicitante Firma del Testigo (Atestiguado sólo si el solicitante firma con una marca o huella) Fecha INFORMACIÓN DE NECESIDADES ESPECIALES Si Ud. es una persona que tiene incapacidad y Ud. requiere esta información en un formato alternativo o requiere un acomodamiento especial para poder participar en cualquier audiencia pública, programa o servicio, comuníquese con el departamento de servicios humanos de NM gratis al número 1-800-432-6217, o a través del sistema de relaís de Nuevo México TDD en 1-800-659-8331 o puede oprimir 711. El departamento solicita la comunicación previa por lo menos de 10 días por anticipado para poder proporcionar los formatos alternativos a y acomodamientos especiales que Ud. solicite. (08/22/08) 12. Registrar para votar Si USTED NO está registrado para votar en el lugar donde vive ahora ¿Quiere registrarse para votar aquí hoy? (Escoja uno) SÍ NO La LEY NACIONAL DE REGISTRO DE VOTANTES pone a su disposición la oportunidad de registrase para votar en este lugar. Si desea ayuda para llenar el formulario para registrarse, nosotros le ayudaremos. La decisión de buscar o aceptar ayuda es suya. Usted puede llenar el formulario de solicitud en privado. IMPORTANTE: Solicitar para registrar o declinar para registrar a votar NO AFECTARÁ la ayuda que se le proporcionará por esta agencia. Firma Fecha CONFIDENCIALIDAD: Si Ud. decide registrarse o no, la decisión que Ud. tome permanecerá confidencial. SI UD. CREE QUE ALGUNA PERSONA HA INTERVENIDO con su derecho de registrarse para votar o declinar de registrarse para votar, o ha intervenido con su derecho a la privacidad en decidir si se registra para votar o al indicar que desea registrare, o su derecho a elegir el partido político, Ud. puede presentar su queja a la Oficina de la Secretaria de Estado, 419 State Capitol, Santa Fe, NM, 87503 (teléfono: 1-800-477-3632). MAD 100 Page 7 of 13 MAD 100 Page 8 of 13 Información de la Solicitud del Programa (Páginas de Información del Solicitante) 1. Información de Necesidades Especiales INFORMACIÓN DE NECESIDADES ESPECIALES: Si Ud. es una persona que tiene incapacidad y Ud. requiere esta información en un formato alternativo o requiere un acomodamiento especial para poder participar en cualquier audiencia pública, programa o servicio, comuníquese con el departamento de servicios humanos de NM gratis al número 1-800-432-6217, o a través del sistema de relaís de Nuevo México TDD en 1-800-659-8331 o puede oprimir 711. El departamento solicita la comunicación previa por lo menos de 10 días por anticipado para poder proporcionar los formatos alternativos a y acomodamientos especiales que Ud. solicite. (08/22/08) 2. Sus Derechos Civiles Todos los programas administrados por el Departamento de Servicios Humanos (HSD) son programas de oportunidades iguales. Si usted cree que ha sido tratado injustamente debido a la raza, el color, origen nacional, la edad, la incapacidad, y donde aplicable, el sexo, el estado civil, estatus familiar, estatus paternal, la religión, orientación sexual, información genética, las creencias políticas, la represalia, o porque todo o la parte de los ingresos de un individuo son derivados de cualquier programa de ayuda estatal, puede presentar una queja. Las quejas de discriminación se pueden presentar en la oficina central del Departamento de Servicios Humanos de Nuevo México o en la oficina de Servicios Humanos local de su condado. . De acuerdo con Ley Federal, esta institución tiene prohibido discriminar por motivos de raza, color, origen nacional, sexo, edad, religión, creencias políticas o incapacidad. Para presentar una queja por discriminación, escriba a USDA, Director, Office of Adjudication, 1400 Independence Avenue, SW, Washington, D.C. 20250-9410 o llame gratuitamente a (866) 632-9992 (Voz). Las personas con dificultades auditivas o incapacidades del habla pueden comunicarse con el USDA a través de los Servicios de Relais Federal al (800) 877-8339; o (800) 845-6136 (Español). 3. Su Privacidad La información que usted da a HSD será utilizada para determinar si su hogar tiene elegibilidad o continúa a tener elegibilidad para participar en los programas de HSD. Verificaremos esta información por programas de computadora. Esta información también será utilizada para asegurar de que usted sigue las reglas del programa y para ayudarnos a manejar el programa. Esta información puede ser dada a otras agencias Federales y del Estado para examen oficial, y a oficiales de la ley para el propósito de encontrar a personas que huyen para evitar la ley. Si usted recibe beneficios de que usted no fue elegible y tiene que pagarlos, esto se llama un reclamo. Si su casa recibe un reclamo contra su casa, la información en esta solicitud, incluyendo todos los números del seguro social, pueden ser dados a agencias Federales y del Estado, así como agencias privadas de colección de reclamos, para la acción de colección de reclamos. Dar la información solicitada, incluyendo números del seguro social de cada miembro de la casa es voluntario. Sin embargo, cada persona solicitando para asistencia debe dar un número de seguro social o resultará en la negación de beneficios del programa a cada individuo que no da un número del seguro social. Inmigrantes no ciudadanos que no están solicitando asistencia para sí mismos, no necesitan dar información de su estatus migratoria o número de seguro social. Cualquier número de seguro social proporcionado será utilizado y será revelado en la misma manera que números de seguro social de miembros de la casa que son elegibles. Nosotros también verificamos con otras agencias, el Servicio de Verificación de Elegibilidad e Ingresos Federales (IEVS) y el Sistema de Información Reportada de Asistencia Pública (PARIS) acerca de la información que usted nos da. Ésta información puede afectar su elegibilidad de la casa y cantidad de beneficio. 4. División de Sostenimiento de Niños Al aceptar asistencia médica, usted asigna (otorga) a HSD derechos para cobrar sostenimiento de niños al padre ausente del niño (s). Usted debe ayudar a HSD a encontrar al padre ausente (s) a menos que haya una buena razón para no hacerlo, como la violencia doméstica, pregúntele a un trabajador. Si se decide que usted tiene que cooperar con la Oficina de Sostenimiento de Niños para establecer o hacer cumplir la manutención y usted no lo hace, los beneficios pueden ser eventualmente perdidos, y los adultos pueden perder su asistencia médica. 5. Entrevista ¿En cuánto tiempo puedo tener mi cita requerida para una entrevista? Los programas de asistencia médica en esta solicitud no requieren una entrevista. 6. Información de Pruebas (a) ¿Cuántos días voy a tener para dar toda la prueba necesaria que necesito? 10 días a partir de la fecha de la solicitud es lo mejor para recibir los beneficios más rápido 45 días a partir de la fecha de su solicitud es típico - a menos que necesite más tiempo - Si usted necesita más tiempo, pida más tiempo 60 días a partir de la fecha de su solicitud es los más largo – Cuando Ud. pide hasta 3 extensiones de 10 días Si no solicita una extensión de tiempo para presentar la prueba, su caso puede ser negado después de 30 días. (b) ¿Qué pruebas debo llevar a la entrevista? Su trabajador NO le pedirá que dé prueba de todo. Usted debe estar preparado de presentar todos los datos de su caso que pueda. Si el trabajador tiene preguntas sin resolver acerca de su elegibilidad, se le pedirá a dar pruebas. Su trabajador le dará una lista de todo lo que todavía tiene que dar, junto con un recibo como prueba que usted proporcionó. Si usted necesita ayuda, pídale ayuda a su trabajador. MAD 100 Page 9 of 13 7. Elegibilidad de Inmigrantes No Ciudadanos (a) ¿Qué tipos de Inmigrantes no ciudadanos son elegibles para programas de asistencia de HSD? Para la mayoría de los programas, las personas que no son ciudadanos deben tener un estatus de inmigrante "calificado" y tienen otras ciertas condiciones para calificar. La mayoría de los no ciudadanos en las siguientes categorías pueden obtener beneficios si cumplen todos los demás requisitos de elegibilidad del programa Residente Permanente Legal (LPR) Amerasiáticos Ciertos: Refugiados Libertad condicional a EE.UU. - 1 año Mujeres y niños maltratados Indígena Americano nacido en Canadá Asilados Retención de la deportación Veteranos, militares en servicio activo Entrantes cubanos haitianos Tribu Hmong o de Laos /México Las víctimas de tráfico de personas Algunos no ciudadanos, incluidos los no ciudadanos indocumentados pueden ser elegibles para los servicios médicos de emergencia, incluyendo el parto y alivio de las mujeres embarazadas. (b) ¿Existe un período de espera (bar) antes de que los inmigrantes no ciudadanos pueden obtener beneficios? La regla general es que ahora la mayoría de los niños inmigrantes calificados son elegibles para recibir Asistencia Médica. Sin embargo, algunos adultos inmigrantes "calificados" pueden recibir beneficios después de haber estado en los Estados Unidos en condición de inmigrante "calificado" durante cinco años y algunos inmigrantes pueden obtener de inmediato. En general, los adultos en ciertas categorías de inmigración humanitarias (como refugiados y asilados), las personas con conexiones militares, mujeres embarazadas y niños presente legalmente, crédito por 10 años de historia de trabajo en los EE.UU., y las personas que reciben beneficios por incapacidad pueden ser elegibles de inmediato. 8. Después de su entrevista (a) ¿En cuánto tiempo será mi solicitud aprobada o negada? Médica – No más de 45 días naturales después de la fecha de solicitud (b) Si no estoy de acuerdo con la decisión de elegibilidad o beneficio ¿puedo tener una audiencia justa? Sí - Si no está de acuerdo con una decisión que tomamos sobre su caso, usted puede solicitar una audiencia justa en persona, por teléfono 1-800432-6217 o (505) 827-8164, o por escrito dentro de 90 - días siguientes a la fecha en que la notificación ha sido enviada para informarle de cualquier acción que se ha tomado en su caso. Por favor envíe su solicitud a la Oficina de la Audiencia HSD al PO Box 2348 Santa Fe, NM 87504. Usted tiene derecho a revisar el archivo de su caso y cualquier registro que HSD usa para determinar su elegibilidad antes de su audiencia. Usted puede pedir a un miembro de la familia u otra persona como un amigo o pariente que lo represente a su hogar en la audiencia justa. Usted también tiene el derecho de tener un abogado u otro representante legal en la audiencia. (c) ¿A partir de cual fecha se calculan mis beneficios? Médicos – A partir del primer día del mes en que solicitó. Usted puede ser elegible para recibir hasta 3 meses antes de la cobertura de Medicaid. (d) ¿Cómo voy a recibir mis beneficios? Médicos - Una tarjeta de Medicaid se le enviará a usted un día de trabajo después de la fecha de aprobación. (e) ¿Cuánto tiempo puedo recibir beneficios antes que tenga que renovarlos? Médicos – Hasta 12 meses es típico. l (f) ¿Tengo que reportar cambios? Siempre reporte cambios de dirección dentro de 10 días naturales para todos tipos de programas de asistencia. Médicos – Para adultos, reporte todos los cambios dentro de 10 días naturales. Para familias con niños y mujeres embarazadas, solo tiene que reportar cambios dentro de 10 días naturales. Todos los demás cambios se reportan la próxima vez que renueve su caso. MAD 100 Page 10 of 13 9. Aviso de Derechos CONFIDENCIALIDAD Toda la información que doy a HSD es confidencial. Esta información se dará a los empleados de HSD que la necesitan para administrar los programas que he solicitado. La información confidencial puede ser revelada a otras agencias federales y estatales. Toda la información se utilizará para determinar la elegibilidad y / o prestación de servicios. (03/29/12) SUS DERECHOS CIVILES Todos los programas administrados por el Departamento de Servicios Humanos (HSD) son programas de oportunidades iguales. Si usted cree que ha sido tratado injustamente debido a la raza, el color, origen nacional, la edad, la incapacidad, y donde aplicable, el sexo, el estado civil, estatus familiar, estatus paternal, la religión, orientación sexual, información genética, las creencias políticas, la represalia, o porque todo o la parte de los ingresos de un individuo son derivados de cualquier programa de ayuda estatal, puede presentar una queja. Las quejas de discriminación se pueden presentar en la oficina central del Departamento de Servicios Humanos de Nuevo México, ATTN: Quality Improvement Section, Pollon Plaza, P. O. Box 2348, Santa Fe, New Mexico 87504-2348 o en la oficina local de Servicios Humanos de su condado. Las quejas de discriminación sobre el Programa de Ayuda de Nutrición Suplemental se pueden presentar con el USDA, Director, Office of Adjudication, 1400 Independence Ave. SW, Washington, DC 20250-9410 o llame 1-866-632-9992 o 202-401-0216 (TDD). Las quejas de discriminación sobre el programa de Asistencia Médica se pueden presentar con la Office of Civil Rights, Department of Health and Human Services, 1301 Young Street, Suite 1169, Dallas, TX 75202 o llame 1800-368-1019 (voz) o 1-214-767-8940 (TDD). (08/16/11) SU DERECHO A UNA AUDIENCIA - Usted puede solicitar una audiencia si no está de acuerdo con una decisión HSD ha hecho respecto a su solicitud / beneficios. Una audiencia le dará la oportunidad de explicar por qué no está de acuerdo. Usted puede solicitar una audiencia de HSD : Completando y regresando la parte inferior de un aviso; Escribir o llamar a su oficina local de HSD, o Escribir a la Oficina de Audiencias del Departamento de Servicios Humanos, P.O. Box 2348, Santa Fe, N.M. 87504-2348, o llamando al 1-800432-6217 (presione 6) o 505-476-6213. (Revised 08/16/11) AUDIENCIA del Mercado - Sé que si yo creo que el Mercado de Seguros Médicos ha cometido un error sobre mi elegibilidad, puedo apelar la acción si contacto al Intercambio de Seguros Médicos al 1-800-318-2596 e informar adecuadamente que creo que su acción debe ser revisada. Sé que puedo autorizar a otra persona para que me represente en el proceso de apelación. PLAZO PARA SOLICITAR UNA AUDIENCIA - Usted tiene 90 días a partir de la fecha de este aviso para solicitar una audiencia. Si usted solicita una audiencia dentro de los 13 días a partir de la fecha de este aviso, usted continuará recibiendo la misma cantidad de beneficios que recibió antes de llegar a la acción en este aviso. Usted continuará recibiendo estos beneficios hasta que el Departamento decida el caso, a menos que se haga otro cambio en su caso. Los cambios en los beneficios se pueden hacer después de haber solicitado una audiencia si el motivo del cambio no es el mismo que el motivo de la audiencia. Si usted pierde la audiencia, tendrá que devolver los beneficios que recibió mientras el Departamento decidió su caso. (Revised 9/24/02) EL PROCESO DE AUDIENCIA - Después de pedir una audiencia, el Departamento o el Mercado le enviará una carta informándole la fecha, hora y lugar donde se realizará la audiencia. La audiencia es por lo general en la oficina del condado HSD. La audiencia será dirigida por un oficial de audiencias de la Oficina de Audiencias de HSD o del Mercado. Usted o su representante pueden ver su expediente y cualquier prueba que usamos para decidir su caso. Usted dirá por qué cree que la acción de HSD o del Mercado estaba equivocada. Usted puede presentar testigos y presentar pruebas. Usted puede cuestionar la oficina del condado o al Mercado acerca de las medidas adoptadas y la prueba presentada. Usted puede representarse a sí mismo. Usted puede ser representado por un amigo, un familiar o un abogado. Para obtener información sobre dónde puede obtener ayuda legal gratuita, llame a 1-800-340-9771. Después de la audiencia, el oficial de la audiencia hará un informe. El Director de la División HSD o al Director Ejecutivo del Mercado decidirá si la acción fue correcta o incorrecta. Después de que el Director decida su caso, se le enviará una carta informándole de la decisión y por qué se tomó la decisión. (Revised 04/02/03) MAD 100 Page 11 of 13 Formulario de Cobertura del Empleador ¿Solicita ayuda con los gastos de seguro de salud del Mercado de Seguros Médicos? La solicitud del Mercado de Seguros Médicos hace preguntas acerca de cualquier cobertura de salud disponible a través de un trabajo en curso (aunque sea de un trabajo de otra persona, como un padre o cónyuge) para averiguar si es posible que pueda obtener ayuda para pagar el seguro de salud. Utilice este formulario para obtener la información que necesita del empleador que ofrece cobertura de salud. Vamos a verificar esta información, así que es importante ser preciso. Si usted tiene más de un trabajo que ofrece cobertura de salud, use un formulario separado para cada empleador. Información de Empleado El empleado debe llenar esta sección. Anote la información del empleado, luego puede solicitar la siguiente información del empleador. Utilice este formulario completo al llenar una solicitud del mercado de Seguros de Médicos. Nombre de Empleado (Primer, Medio, Apellido) Número de Seguro Social Información del Empleador Pídale al empleador esta información Nombre del Empleador Número de Identificación de Empleador (EIN) Dirección del Empleador Número de Teléfono de Empleador ( ) – Estado Código postal Ciudad ¿A quién podemos contactar acerca de la cobertura de salud de los empleados en este trabajo? Nombre:_________________________ Teléfono:________________ Correo Electrónico:___________________ Díganos sobre el plan de salud que ofrece este empleador. Este empleado no es elegible para la cobertura bajo el plan del empleador. El empleado es elegible para la cobertura bajo el plan del empleador el ___________________ (Fecha de inicio). ¿Qué es el nombre del plan de salud solo para sí mismo de menos costo que este empleado podría inscribirse en este trabajo? (Sólo considerar los planes que cumplan con el "estándar de valor mínimo" establecido por la Ley de Cuidado de Salud A Bajo Precio.) Nombre:_______________________________________________________ No hay planes que cumplen con el "estándar de valor mínimo" ¿Cuánto tendría que pagar el empleado en primas correspondientes a ese plan? $__________ ¿Con qué frecuencia? Semanal Cada 2 semanas 2 veces al mes Mensual Anual Otro______ MAD 100 Page 12 of 13 Register to Vote PERSONAL INFORMATION NAME: Last First Middle Name or Initial 1 PHYSICAL STREET ADDRESS WHERE YOU LIVE NOW Street Address Apartment, Unit, or Lot # Gender M This information not to be copied Birth Date Social Security Number City Zip 2 ADDRESS WHERE YOU GET YOUR MAIL Address (If different from above) City Zip Site Code 3 If you are changing your name on this application, under what Last Name First Name Middle Name or Initial 4 full name were you previously registered? POLITICAL PARTY POLL WORKER DAY TIME TELEPHONE NUMBER (Optional) NOTE: You must name a major Party If you choose NO PARTY, May the County Clerk make this Would you like to serve political party to vote in primary Check this box 6 telephone number public for as an election day Democrat 5 elections. election purposes? Yes No precinct worker? Yes I hereby authorize you to cancel my previous City or Township County State 7 registration in the following county and state. Please answer the following questions: ATTESTATION OF QUALIFICATION 8 I swear/affirm that I am a citizen of the United States and a resident of the state of New Mexico; that I have not been denied the right to vote by a court of law by reason of mental incapacity; that I am, or will be at the time of the next election, 18 years of age; and if I have been convicted of a felony, I have completed all conditions of parole and supervised probation, served the entirety of sentence or have been granted a pardon by the governor. I further swear/affirm that I am authorizing cancellation of any prior registration to vote in the jurisdiction of my prior residence; and that all the information I have provided is correct. Are you a citizen of the United States? ………………………………… Yes No Will you be 18 years of age on or before election day? ……………… Yes No If you checked “No” to any of the questions above, do not complete this form. If you have been convicted of a felony and are currently on parole or supervised probation do not complete this form. TODAY’S DATE Month Day Year ______/ ______ /______ SIGN YOUR FULL NAME OR MARK ON THE LINE BELOW:. Name of agent who assisted you in filling out this form. VRA ID # 9 DO NOT WRITE IN SHADDED AREAS – FOR OFFICIAL USE ONLY Accepted for filing in County Registration Records: ___________ / _________________________________ / _________________________________ Date County Clerk Filing Clerk ID PCT MUN SCHOOL CC PRG DIST REP DIST SEN DIST HSD Site Code I- Registrarse para Votar 01 Esta información no se debe copia INFORMACIÓN PERSONAL NOMBRE: Apellido Primer Nombre Medio Nombre o Inicial Género Fecha de Nacimiento Número de Seguro Social 1 H DIRECCIÓN DONDE UD. VIVE AHORA Número y Nombre de la Calle Departamento, Unidad o # de Lote Ciudad Zona Postal 2 DIRECCIÓN DONDE UD. RECIBE SU CORRESPONDENCIA (Si es diferente del anterior) Dirección Ciudad Zona Postal Site Code 3 ¿Si Ud. Va cambiar su nombre en esta solicitud, bajo que Apellido Primer Nombre Medio Nombre o Inicial nombre completo estaba Ud. Matriculado antes? 4 EMPLEADO / A EN URNA ELECTORAL PARTIDO POLÍTICO NUMERO DE TELÉFONO EN EL DÍA (Opcional) AVISO: Ud. tiene que indicar Partido Si Ud. NO ELIGE ¿Puede el Secretario del ¿Quiere Ud. trabajar en recinto 5 partido politico principal para Partido marque aquí electoral el día de la elección? 6 Condado hacer público este votar en la elección primaria núm. de teléfono para fines Si Democrata electorales ? Sí No Por la presente autorizo que Ud. cancele mi matrícula Ciudad o División Condado Estado 7 previa en el condado y estado a continuación. Favor de contestar las preguntas a continuación: TESTIMONIO DE CALIFICACIÓN Ud. ciudadano / a de los Estados Unidos? ……………….…… Sí No ¿Habrá cumplido Ud. 18 años en o antes del día de la elección? Sí No Si Ud. marcó “NO” en cualquiera de las preguntas más arriba no termine de rellenar este formulario. Si usted fue condenado de un delito grave y actualmente está en libertad condicional o probación supervisada, no llene esta forma. ¿Es 8 FECHA DE HOY: Mes Día Año ______/______ /______ 9 Nombre de la persona que le ayudó a llenar este formulario: Yo juro/afirmo que soy ciudadano de los Estados Unidos y residente del Estado de Nuevo México; que la corte no me ha denegado el derecho de votar por motivo de incapacidad psicológica; que tengo o tendré 18 años de edad en la fecha de la próxima elección y si he sido condenado de delito grave he cumplido todas las condiciones de libertad a prueba o el gobernador me ha concedido indulto. Además, juro o afirmo que autorizo la cancelación de toda matrícula anterior con el fin de votar en el territorio de mi residencia previa; y que la información proveída está correcta. FIRME SU NOMBRE COMPLETO O MARQUE LA LÍNEA ABAJO: VRA ID # NO ESCRIBA EN LOS ESPACIOS EN COLOR GRIS – SOLO PARA USO OFICIAL (FOR OFFICIAL USE ONLY) ID PCT MUN PRG DIST REP DIST SEN Accepted for filing in County Registration Records SCHOOL CC ________ / ______________________________ / _____________________________ Date County Clerk Filing Clerk DIST ISDB 720 Issued 3/5/12 MAD 100 Page 13 of 13 PRESUMPTIVE ELIGIBILITY (PE) APPLICANT INFORMATION FORM Person Supplying Information on Behalf of Applicants and/or Household Members Listed Below First Name Middle Last Home Address City State Zip Phone Email State Zip Mailing Address (if different than above) Address City Family Members in the Household US Citizen, Relationship Name (First, Middle, Last) Applying For PE? Y Y Y Y Y Y Y Y to Person Supplying Information Date of Birth N N N N N N N N SSN (not required) US National or Eligible Immigrant? (not required) Living in New Mexico? Pregnant? Receiving Income from Work or Job? Y Y Y Y Y Y Y Y Y Y Y Y Y Y Y Y Y Y Y Y Y Y Y Y Y Y Y Y Y Y Y Y N N N N N N N N N N N N N N N N N N N N N N N N N N N N N N N N How Often? Enrolled in Medicaid or Medicare? Y Y Y Y Y Y Y Y N N N N N N N N Other Household Income per Month (before taxes): By signing below, you are swearing that all information you have supplied for the completing of this Presumptive Eligibility application is true and correct to the best of your knowledge. DO Include: Unemployment, Alimony, and Disability from the Social Security Administration DO NOT Include: SSI Payments, or Child Support Received All information supplied will be kept secure and private. Total Household Job Income per Month (before taxes): MAD 011 Revised 5/2/14 Signature of Person Supplying Info on Behalf of This Household FORMULARIO DE INFORMACIÓN PARA LA SOLICITUD DE PROBABLE ELIGIBILIDAD (SIGLAS EN INGLÉS: PE) Persona que proporciona la información en nombre del solicitante y/o los miembros de su familia que figuran más abajo Nombre Apellido Domicilio Ciudad Teléfono Correo Electrónico Estado Código Postal Estado Código Postal Dirección Postal (si es diferente a la de arriba) Dirección Ciudad Miembros que componen la familia ¿Ciudadano de EE.UU, Relación Nombre y Apellido Solicitar PE? Con la persona que proporciona la información Fecha de Nacimiento SI N SI N SI N SI N SI N SI N SI N SI N Total del Ingreso de la Familia por mes (antes de impuestos): Número de Seguro Social Residente de EE.UU o Inmigrante Elegible? (no necesario) (no necesario) ¿Reside en el Estado de Nuevo México? ¿Embarazada? ¿Recibe un ingreso de un trabajo? SI SI SI SI SI SI SI SI SI SI SI SI SI SI SI SI SI SI SI SI SI SI SI SI SI SI SI SI SI SI SI SI N N N N N N N N Otro Ingreso de la Familia por mes (antes de impuestos): POR FAVOR, incluir: Desempleo, Pensiones Alimenticias, y Incapacidad de la Administración de Seguro Social NO incluya: Pagos SSI o Manutención de niños N N N N N N N N N N N N N N N N ¿Cada cuánto tiempo? N N N N N N N N ¿Está registrado en Medicaid o Medicare? SI SI SI SI SI SI SI SI Al firmar abajo, Ud. jura que la información proporcionada al completar esta solicitud es verdadera y correcta según sus conocimientos. Toda la información proporcionada es confidencial y privada.. MAD 011 Revised 5/2/14 Firma de la persona solicitando en favor de su famila N N N N N N N N MEDICAID PRESUMPTIVE ELIGIBILITY AUTHORIZATION Determiner Name: Determiner Fax Number: 1-877-285-6790 Fax this form to: PE Determiner: List ONLY the individuals who are Eligible for PE. Type all information directly into this form. The PE eligibility End Date is the last day of the month following the PE approval. If an application for ongoing Medicaid eligibility is submitted by the PE Eligibility End Date, the PE will remain in effect until a final application determination has been made. FOR FISCAL AGENT USE ONLY ALL SPACES MUST BE COMPLETED NAME – Last, First, Middle Race Sex Date of Birth Social Security Number Geo/ Adm MCO Choice Children's Cat. (select one) Adult Cat. (select one) Eligibility Begin Date End Date MAILING ADDRESS – Street, PO Box R. Rte. None Select One Select One Select City, State, Zip Added Eligibility YES NO FOR FISCAL AGENT USE ONLY ALL SPACES MUST BE COMPLETED NAME – Last, First, Middle Race Sex Date of Birth Social Security Number Geo/ Adm MCO Choice Children's Cat. (select one) Adult Cat. (select one) Eligibility Begin Date End Date MAILING ADDRESS – Street, PO Box R. Rte. Added Eligibility YES NO None Select One Select One Select City, State, Zip FOR FISCAL AGENT USE ONLY ALL SPACES MUST BE COMPLETED NAME – Last, First, Middle Race Sex Date of Birth Social Security Number Geo/ Adm MCO Choice Children's Cat. (select one) Adult Cat. (select one) MAILING ADDRESS – Street, PO Box R. Rte. Eligibility Begin Date End Date Added Eligibility YES Select None Select One Select One City, State, Zip TO BE COMPLETED BY PE DETERMINER PE Determiner Name PE Determiner’s Signature PE Determiner’s Number PE Determiner Phone Number PE Determiner’s Agency Agency’s Business Address Determiner’s Fax Number: Determiner’s E-Mail: Agency’s Phone Number: Date Determiner’s Comments: Fiscal Agent’s Comments: MAD 070 Revised 3/6/14 Medicaid Fiscal Agent Staff Date NO How tto determine aa houseehold sizze Start Here Does the Indiviidual pect to file taaxes? exp YES Y Does the individual expect to b be claimed as a tax de ependent by anyone else? N o YES Does tthe individuaal meet anyy of the folloowing Exceptions? ? Does the Indiviidual expect to be claaimed as a a tax depend dent? N o No YES Does the D In ndividual exp pect to be claim med as a tax dep pendent by so omeone ou utside the home? Y E S Thee Household with no o tax filing status cconsists of th he in ndividual and d, if lliving with th he individual…… ….. ‐Expectts to be claim med as a tax dep pendent of ssomeone other than a spouuse or a parent. No ‐A child (under age 19) living with bo oth parents,, but the paren nts won’t filee a joint return. ‐ A child d (under agee 19) who expectts to be claim med by a non‐‐custodial paarent. YYES Th he Indiviiduals spouse; Th e individuals natuural, adopteed, andd step childreen undder the age o of 19. The Hou usehold con nsists of the Taxpayer, a spousee living with the payer, and all taxp perso ons whom th he taxpaayer expects to claaim as a tax depend dent. A pregn nant woman is counted d as herself plus the num mber of ch hildren she iis expeccted to deliver. No The Houssehold is of a taxpayeer, claiming him/her as a dependent, and all peersons whom the taxpayyer expects to claim as a taax dependent. ‐A pregnaant woman is counted as herself and the numbeer of children she is exxpected to deeliver. ‐If the in ndividual is married an nd living with the spouse, the d includes the Household spouse. A pregn nant woman n is countted as herself and thee number off child dren she is expecteed to deliverr. In the e case of individuals undder age 19; th he household includes tthe individuaal’s parents aand natural, adopted, an nd step‐siblings under age 19. HOUSEHOLD SIZE AND INCOME CALCULATION WORKSHEET STEP 1: Identify the Head of Household (HOH) and who is part of that household STEP 2: Identify individual’s relationship to Head of Household Individuals in Household Relationship STEP 3: Identify individual’s income Monthly Gross Income STEP 4: Identify individual’s tax status Tax Filer, Dependent, Non-Filer STEP 5: Refer to “How to Determine a Household Size” flow chart and mark a ”1” if the individual is included in the budget group HOH Ind. 2 Ind. 3 Ind. 4 Ind. 5 Ind. 6 STEP 6: List the number of unborn children for all pregnant women included in the Budget Group STEP 7: Add number of individuals in Budget Group (Add figures in STEP 5 to figure in STEP 6) Number of Unborn Children Total Individuals in Budget Group HOH SELF 0 Ind. 2 0 Ind. 3 0 Ind. 4 0 Ind. 5 0 Ind. 6 0 STEP 8: List all individuals requesting assistance STEP 9: List individual’s age Name Age STEP 10: List household Budget Group size from STEP 7 STEP 11: Add monthly gross income for each individual included in the household/Budget Group STEP 12: Refer to the MAD 222 to determine the category of eligibility Household Size (Budget Group) Total Monthly Gross Income for Budget Group* Medicaid Category of Eligibility** STEP 13: Apply disregard if applicable Subtract 5% Disregard (if applicable) STEP 14: Subtract disregard from total monthly gross income based on household size (if applicable) Total Monthly Gross Income for Budget Group with 5% Disregard (if Applicable) 0 0 0 0 0 0 MAD 008 Revised 6/25/14 *Subtract Federal Pre-Tax Deductions (dependent care accounts, health insurance premiums, flexible spending accounts, retirement accounts and/or commuter expenses) from Monthly Gross Income. ** Refer to MAD 222 for Categories of Eligibility and income guidelines. Manual Presumptive Eligibility Submission Checklist For Applicants Who Wish to Apply for Ongoing Medicaid Coverage If applicant is PE eligible and submitting an application for ongoing Medicaid coverage: FAX: Presumptive Eligibility Authorization Form (MAD 070; Rev 3/6/14) to Xerox: 877-285-6790 AND FAX: Presumptive Eligibility Authorization Form (MAD 070; Rev 3/6/14); NM Medicaid-Only Application (MAD 100; Rev 1/21/14); Household Comp and Income Calculation Worksheet (MAD 008) and Any proofs of income, citizenship & identity the applicant may have supplied to Central ASPEN Scanning Area (CASA): 855-804-8960 ___________________________________________________________________________ If applicant is NOT PE eligible but wishes to submit an application for ongoing Medicaid coverage: FAX: NM Medicaid-Only Application (MAD 100; Rev 1/21/14); Household Comp and Income Calculation Worksheet (MAD 008) and Any proofs of income, citizenship & identity the applicant may have supplied to Central ASPEN Scanning Area (CASA): 855-804-8960 ____________________________________________________________________________ Manual Presumptive Eligibility Submission Checklist For Applicants Who DO NOT Wish to Apply for Ongoing Medicaid Coverage If applicant is PE eligible but is NOT submitting an application for ongoing Medicaid FAX: Presumptive Eligibility Authorization Form (MAD 070; Rev 3/6/14) to Xerox: 877-285-6790 AND FAX: Presumptive Eligibility Authorization Form (MAD 070; Rev 3/6/14) Presumptive Eligibility Applicant Information Form (MAD 011); Household Comp and Income Calculation Worksheet (MAD 008) Any proofs of income, citizenship & identity the applicant may have supplied to MAD PE Program Staff: 505-827-7200 _____________________________________________________________________________ If applicant is NOT PE eligible and NOT submitting an application for ongoing Medicaid FAX: Presumptive Eligibility Applicant Information Form (MAD 011); Household Comp and Income Calculation Worksheet (MAD 008) Any proofs of income, citizenship & identity the applicant may have supplied to MAD PE Program Staff: 505-827-7200