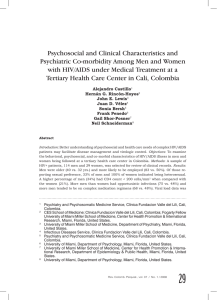
Accelerated Course of Human Immunodeficiency Virus
Anuncio

Accelerated Course of Human Immunodeficiency Virus Infection in Gay Men Who Conceal Their Homosexual Identity STEVE W. COLE, PHD, MARGARET E. KEMENY, PHD, SHELLEY E. TAYLOR, PHD, BARBARA R. VISSCHER, MD, AND JOHN L. FAHEY, MD Research linking psychological inhibition to physical illness led us to examine whether human immunodeficiency virus (HIV) infection might progress more rapidly among gay men who conceal their homosexual identity than among those who do not. We also sought to determine whether any accelerated course of HIV infection among "closeted" gay men might be attributable to differences in health-relevant behavior (e.g., health practices, sexual behavior) or psychosocial characteristics (e.g., depression, anxiety, social support, repressive coping style). Data came from a longitudinal psychosocial study associated with the Los Angeles site of the Multicenter AIDS Cohort Study. Eighty gay men, HIV-seropositive but otherwise healthy at study entry (CD4 T lymphocytes = 30-60% of total lymphocytes), were examined at 6-month intervals for 9 years. Indicators of HIV progression included time to a critically low CD4 T lymphocyte level (15% of total peripheral blood lymphocytes), time to AIDS diagnosis, and time to AIDS mortality. On all measures, HIV infection advanced more rapidly in a dose-response relationship to the degree participants concealed their homosexual identity. Sample characteristics and statistical controls ruled out explanations based on demographic characteristics, health practices, sexual behavior, and antiretroviral therapy. Mediational analyses indicated that observed effects were not attributable to differences in depression, anxiety, social support, or repressive coping style. HIV infection appears to progress more rapidly in gay men who conceal their homosexual identity. These results are consistent with hypotheses about the health effects of psychological inhibition, but further research is required to definitively identify the psychosocial, behavioral, and physiological mechanisms underlying these findings. Key words: HIV/AIDS, CD4 T lymphocytes, disease progression, homosexuality, psychological inhibition, psychosocial characteristics. INTRODUCTION Infection with the human immunodeficiency virus 1 (HIV-lj has a highly variable course, with some individuals progressing rapidly to acquired immune disease syndrome (AIDS) and others remaining asymptomatic and immunologically healthy for long periods of time (1-5). Although some variation in disease progression can be attributed to characteristics of the virus (e.g., viral strain) and the host immune system (e.g., human histocompatability leukocyte antigen genotype), these characteristics alone do not appear to fully explain the substantial individual differences in HIV progression (1). As a result, a great deal of research has concentrated on identi- From the Departments of Psychology (S.W.C., S.E.T), Psychiatry and Biobehavioral Sciences (M.E.K.), Microbiology and Immunology (J.L.F.), and the School of Public Health (B.R.V.), University of California, Los Angeles, Los Angeles, California. Address reprint requests to: Steve W. Cole, PhD, UCLA Department of Psychology, 405 Hilgard Ave., Los Angeles, CA 900241563. Received for publication February 15, 1995; revision received September 18, 1995. Psychosomatic Medicine 58:219-231 (1996) 0033-3174/96/5803-0219$03.00/0 Copyright © 1996 by the American Psychosi tying other factors that might influence the course of HIV infection (1, 5). Psychosocial characteristics of the host are one type of cofactor that has received a great deal of attention in this regard (6-7). Perhaps the most classic of all psychosomatic hypotheses suggests that inhibiting the expression of thoughts, feelings, or social behaviors can be harmful to one's physical health. The roots of this hypothesis are often traced back to the second century Greek physician Galen, who described a heightened incidence of cancer among those with inhibited, "melancholic" personalities (8). Galen believed that differences in both personality and physical health stemmed from their common basis in the balance of bodily humors (e.g., an excess of black bile among the cancer-prone melancholic). Later researchers proposed that psychological inhibition is actually physiologically harmful (9). Experimental studies have shown that inhibiting the expression of emotions and self-threatening knowledge can increase activity in the sympathetic division of the autonomic nervous system (10-13), and high levels of sympathetic activity are capable of suppressing some aspects of immune function (e.g., in vivo: levels of circulating lymphocytes and monocytes, antibody production, immediate and delayed219 S. W. COLE et al. type hypersensitivity reactions, and activity in secondary lymphoid organs, and in vitro: cytokine production, lymphocyte maturation, motility, proliferation, and cytolysis, and phagocyte chemotaxis and lysosomal activity) (14-19). Studies in which participants disinhibited psychological material by expressing thoughts and feelings associated with traumatic personal experiences have demonstrated short term improvements in some measures of physical health (e.g., physician visits) and immune function (e.g., latent virus control, antibody response, and mitogen-induced lymphoproliferation) as well as reductions in sympathetic nervous system activity (20-25). In addition to these experimental results, some epidemiological studies have documented associations between inhibited psychosocial characteristics (e.g., reduced emotional expression) and the incidence and progression of cancer (26-27), hypertension (28-29), and some types of autoimmune disease (30). These epidemiological claims are controversial, and the evidence is uneven, particularly in the case of cancer (26-27). However, such findings do converge with the experimental evidence in suggesting a possible link between psychological inhibition and physical illness. Relationships between psychological inhibition and physical health may have important implications for the course of HIV infection in gay men. Many gay men inhibit the expression of their homosexual identity to avoid stigmatization, ostracism, and physical assault (31-33). To determine whether inhibition-linked alterations in immune function might potentially hasten the course of HIV infection, we examined the relationship between concealing homosexual identity and HIV progression in data from a 9-year longitudinal study of 80 (initially healthy) seropositive gay men participating in a psychosocial study associated with the University of California of Los Angeles (UCLA) site of the Multicenter AIDS Cohort Study (MACS) (34). HIV progression was measured by time from MACS entry to three end points: a critically low CD4 level, diagnosis of an AIDS-defining condition [under the 1987 Centers for Disease Control (CDC) case definition], and death due to HIV-related pathology. Times to each end point were analyzed using standard survival analytic statistical models, and all analyses controlled for any potential differences in age, disease progression at study entry (marked by CD4 level at MACS entry), antiretroviral use, unsafe sexual practices, and several other biobehavioral characteristics that could conceivably influence immune function or HIV progression (e.g., recreational drug use, sleep disturbance, exercise) (6, 35). Anxiety, 220 depression, repressive coping style, and social support were also examined as psychosocial variables that might potentially mediate concealment-related differences in disease progression. Results of these analyses indicate that HIV infection did indeed progress more rapidly among those participants who concealed their homosexual identity. Moreover, these progression differences could not be attributed to differences in demographic characteristics, health-relevant behavioral habits, or psychosocial characteristics such as anxiety, depression, repressive coping style, or social support. METHOD Participants The MACS/Natural History of AIDS Psychosocial Study. Between 1984 and 1986, 1759 gay and bisexual men were recruited into the Los Angeles sample of MACS (34). No participant knew his HIV serostatus at study entry (HIV antibody testing was not yet available), all were over 18 years of age, and none had been diagnosed with cancer or any AIDS-defining condition. The present analyses focused on the 988 MACS participants who were subsequently found to be HIV-seropositive at study entry. At 6-month intervals, blood samples were taken, participants were examined for signs and symptoms of AIDS, and interviewers assessed variables potentially relevant to the course of HIV infection (e.g., demographic characteristics, drug use, health practices, sexual behavior). Beginning in 1987, 333 HIV-positive MACS participants volunteered to participate in the Natural History of AIDS Psychosocial Study (NHAPS), a project focusing on cognitive, emotional, social, and behavioral factors associated with HIV infection (3637). Participants completed psychosocial questionnaires at 6-month intervals coinciding with MACS examinations. In 1987 and 1988,192 of these participants completed an additional set of questionnaires that solicited information about psychosocial characteristics, including homosexual identity and AIDS-related social support. To ensure that advanced HIV infection did not influence any of the psychosocial variables measured in this study, analysis was restricted to individuals with normal CD4 levels (30-60% of peripheral blood lymphocytes) at MACS entry. This resulted in a group of 80 HIV-seropositive MACS/NHAPS participants in the earliest stages of infection (median CD4 level = 686 cells/mm3, interquartile range = 524-829). Median age was 34 years (range 23-50), 96% were Caucasian (3% Hispanic, 1% Asian), 86% attended college, and 60% held jobs in the managerial/professional sector of the U.S. Census occupational classification (22% technical/sales, 12% service, 6% other). This group of 80 subjects was representative of the entire sample of seropositive Los Angeles MACS participants on each MACS-assessed variable examined in this analysis (except initial CD4 level) and was representative of the remaining 253 HIV-seropositive NHAPS participants on each NHAPS-assessed variable (all differences < .2 SD). Between entry into MACS and September 1993, 34% of these individuals received an AIDS-related diagnosis (1987 CDC case definition), and 26% died of an AIDS-related disorder. All data were collected in accord with Institutional Review Board procedures at UCLA. Psychosomatic Medicine 58:219-231 (1996) CONCEALED HOMOSEXUALITY Measures Four types of variables were assessed: psychosocial characteristics (including degree of concealed homosexual identity), HIVrelevant diagnostic events (AIDS diagnosis and AIDS-related mortality), HIV-relevant immune parameters (CD4 and CD8 T lymphocyte levels), and demographic and biobehavioral characteristics that could potentially affect immune parameters or HIV progression (e.g., health practices and sexual behavior). Unless otherwise indicated, all psychosocial, biobehavioral, and demographic variables were measured at entry into the NHAPS (i.e., either through NHAPS instruments or the immediately preceding MACS interview). General deficit in perceived social support was summarized by averaging deficit scores across sources. Repressive Coping Style. Individuals who tended not to experience the negative or threatening aspects of an event were identified by scores below the sample median (5.5) on the Bendig short form of the TMAS and above the sample 75th percentile (13.0) on Strahan and Gerbasi's 20-item revision of the MarloweCrowne Scale of Social Desirability (44). [For more on the definition and measurement of repressive coping style, see Weinberg et al. (45).] Diagnostic Measures Psychosocial Measures Concealed Homosexual Identity. All participants indicated being either "exclusively homosexual," or "predominantly homosexual," and "only insignificantly heterosexual." As in previous studies (32-33, 38), the degree to which respondents concealed their homosexual identity was measured by a 5-category index asking respondents to judge themselves as being ("relative to other gay men"): "definitely in the closet, in the closet most of the time, half in and half out, out of the closet most of the time, or completely out of the closet." Affect and Mood. Depression was measured by the Center for Epidemiologic Studies Depression scale (CES-D) (39), a 20-item scale measuring affective and vegetative symptoms of depression, and by the depression-dejection subscale of the Profile of Mood States (POMS) (40), a 65-item instrument measuring the intensity of six moods (depression-dejection, tension-anxiety, anger-hostility, fatigue-inertia, confusion-bewilderment, and vigor-activity) over the previous week. Anxiety was measured by the 20-item Bendig short form of the Taylor Manifest Anxiety Scale (TMAS) (41) and the POMS tension-anxiety subscale. Social Support. The presence of a primary partner was assessed by responses to the question "Are you currently in an intimate relationship (with a spouse or partner)?" and, if yes, "How long have you been in this relationship?" Relationships of at least a 6-month duration were counted as stable, intimate relationships, and all participants who reported such relationships indicated that their partner was a male. Satisfaction with social relationships was measured by the 20-item UCLA Loneliness scale (42). Subjective isolation was measured by responses to the question "Is there someone you can talk to about things that are important to you—someone you can count on for understanding and support?" Response options were "No, no one" (scored 0), "Yes, one person" (scored 1), "2 or 3 people like that" (scored 2.5), "4 or 5 people like that" (scored 4.5), and "6 or more people like that" (scored 6). AIDS-specific social support was assessed by a modified version of the UCLA Social Support Inventory (43). This 15-item instrument assesses the degree to which respondents want, receive, and are satisfied with, the support they get from intimate partners, gay friends, straight friends, and parents as respondents face the threat of AIDS. Each dimension of subjective social support (desired/received/satisfaction) is assessed for each of five sources (partner/gay friends/straight friends/mother/father). All responses were given on 5-point scales with verbal anchors ranging from "never" to "all the time" (desired and received) or from "very dissatisfied" to "very satisfied" (satisfaction). Summary measures for each dimension were obtained by averaging across responses for each source. Discrepancies between desired and received support may also be relevant, so a deficit score (received - desired) was computed for each source. Psychosomatic Medicine 58:219-231 (1996) Diagnosis of HIV Infection. HIV serostatus was determined by enzyme-linked immunosorbent assay for anti-HIV-1 antibodies with positive results confirmed by Western blot for HIV-i gene products (46). Diagnosis of AIDS. All diagnoses of AIDS-defining conditions were made by physicians associated with MACS or were based on medical records supplied to MACS by the participant's primary physician. Case definition followed the 1987 CDC criteria (47). AIDS-Related Mortality. Cause and date of death information was based on death certificate searches routinely conducted by MACS. All deaths occurring in this sample were AIDS-related, and the present analyses were based on death certificates available through August, 1993. Immunological Measures T Lymphocyte Levels. Blood was drawn at each MACS visit, and levels of CD4 and CD8 T lymphocytes were measured by two-color (CD4: Leu-3+ Leu-4+; CD8: Leu-2+ Leu-4 + ) flow cytometry on whole blood (48). CD4 levels were reported as both number (per cubic millimeter of peripheral blood) and percentage of total lymphocytes. Percentage of CD4 was used as the primary measure of CD4 loss because previous research has shown it to be a more reliable indicator of HIV progression (49-50). Measures of Immune-Relevant Background Characteristics Demographic and biobehavioral characteristics that may influence immune function and HIV progression included age, cigarette, drug, and alcohol use, exercise, and sleep disturbance (6, 35). In addition, the course of HIV infection may also be affected by the use of antiretroviral therapies (e.g., AZT/zidovudine) (51) and by rates of unprotected anal-receptive intercourse (2). The number of anonymous sexual contacts may also relate to the number or virulence of HIV strains contracted. The MACS interview assesses age (birth date), antiretroviral use (yes/no), the number of partners in unprotected anal-receptive intercourse (per 6-month period between visits), the number of anonymous sexual partners ("you would not be able to find this person again"; per 6-month period between visits), as well as a number of other forms of sexual contact (e.g., anal-insertive, oral-genital, and oral-anal contact). Anal-insertive contact, oral-genital contact, and oral-anal contact are not discussed in detail here because these behaviors were not significantly associated with either concealment or HIV progression. Incidence of unprotected analreceptive intercourse was summed over the entire study period to 221 S. W. COLE et al. stabilize substantial within-individual variation on this measure (intraclass correlation = .12). Other biobehavioral measures showed greater stability over time (intraclass correlations ranging between .40 and .72), and assessment of those variables was based on Ihe 6-month period preceding NHAPS entry. Any use of antiretrovirals before or during the course of the study was counted, and analyses treating antiretroviral use as a time-varying covariate produced results similar to those reported here. The MACS interview also assesses cigarette smoking, alcohol consumption, and the use of marijuana/hashish, nitrite inhalants ("poppers"), cocaine, barbiturates/tranquilizers/sedatives, and amphetamines. Use of each class of drug was scored dichotomously (none during previous 6 months vs. some), smoking responses were absent, present, or occasional (less than 1 cigarette per day), and alcohol consumption was measured dichotomously (no drinks containing alcohol during previous 6 months vs. some), with drinkers then classified as consuming a maximum of 3 or more drinks in any given 24-hour period vs. 2 or fewer (analyses based on average number of drinks per 24-hour period produced similar results, but average consumption levels were less predictive of HIV progression than maximum consumption levels). Dichotomous scores were created by grouping occasional smokers with nonsmokers and consumers of 2 or fewer drinks per 24-hour period with nondrinkers. NHAPS questionnaires include items assessing sleep disruption ("Over the last month, how many nights in an average week did you get less sleep than you needed?"; responses ranging from 0 to 7) and aerobic and anaerobic exercise ("Over the last month, how many days in an average week did you engage in aerobic exercise: vigorous and continuous activity such as running, swimming, bicycling?" and "Over the last month, how many days in an average week did you engage in anaerobic exercise: short bursts of activity such as tennis, walking, yoga, baseball, stretching?"; both with responses ranging from 0 to 7). Dichotomous scores were created by grouping those who reported an average of 2 or more nights of insufficient sleep per week (vs. 0 or 1) and those who reported either aerobic or anaerobic exercise an average of 1 day a week or more (vs. those who were sedentary). participants indicated that the risk of AIDS morbidity and mortality increased dramatically at this point (Fig. 1) (54). Similar results emerged using either 10% CD4 or 200 CD4 cells/mm3 as an immunological end point. Event times were censored at September 1993 if individuals failed to reach an end point by then (55). Time to critically low CD4 was censored at date of death for individuals who died before reaching this end point. Analyses Our general analytical strategy involved determining whether the inclusion of a measure of concealed homosexual identity significantly improved the predictive power of a statistical model of HIV progression times based on biobehavioral variables identified in previous research as significant predictors of disease progression or immune function. We then sought to determine whether any incremental predictive power associated with concealment could be attributed instead to differences in psychosocial characteristics such as anxiety, depression, repressive coping style, or social support. Accelerated failure-time survival analysis (55) was used to model times to 15% CD4, AIDS diagnosis, and death. Specification checks showed the data to be consistent with a log linear model of (possibly censored) survival times with Weibull-distributed residuals (55). To ensure the robustness of results, each analysis was repeated using a) Cox's semiparametric proportional hazards model (55), b) a linear accelerated failure time model with Weibull residuals, and c) linear Weibull, log linear Weibull, and Cox models of age at event (date of event - date of birth) rather than time from study entry (date of event — date of MACS entry). In every case, the six models produced substantively identical CD4 endpoint AIDS diagnosis AIDS mortality Measures of Disease Progression HIV infects cells expressing the CD4 surface protein (1). AIDS is characterized by the onset of opportunistic infections and neoplastic diseases after a selective decline in levels of CD4+ T lymphocytes ("helper T cells") (1). The rate of CD4 T cell decline varies across individuals (1-6); those who show more rapid loss rates are more likely to develop an AIDS-defining condition (52-53). We assessed the progress of HIV infection by a) time from MACS entry to a critically low CD4 level ( s 15% of total lymphocytes), b) time from MACS entry to first diagnosis of an AIDS-defining condition, and c) time from MACS entry to death from HIV-related pathology. CD4 T cell levels were expressed as a percentage of total lymphocytes. Similar results emerged from analyses based on arcsin-transformed percentages, log- and fourth root-transformed CD4 numbers, and log-transformed CD4/CD8 ratios. Results for percentage of CD4 are reported here because previous research has indicated that CD4 percentages are the best T cell marker of AIDS progression (49-50), and our results concur; log likelihoods for percentage-based models of AIDS progression and mortality exceeded those for count-based models by 9 to 11 units on equivalent degrees of freedom. Fifteen percent CD4 was selected as an immunological end point because preliminary analysis of data from 318 HIV-seropositive MACS/NHAPS 222 Q < o E CO 60 50 40 30 20 10 CD4 level (% total lymphocytes) Fig. 1. Six-month risk of AIDS diagnosis and mortality as a function of CD4 level. Psychosomatic Medicine 58:219-231 (1996) CONCEALED HOMOSEXUALITY results. Log linear Weibull results are reported here because clinical event-times are conventionally represented in a log linear format (55) and parametric results are likely to be more accurate than semiparametric results when the data follow a known hazard function (56). To aid interpretation, parameter estimates are expressed as a percentage change in expected event time (calculated as eh - 1, with b representing the log linear parameter estimate). Our basic model of HIV progression times included variables known to influence disease progression, including age, CD4 level at MACS entry1 (as a measure of disease progression at study entry; analyses using CD4 level at NHAPS entry produced similar results), antiretroviral use, and frequency of unprotected analreceptive intercourse (1, 2, 6, 51). This model also included behavioral variables that previous researchers have suggested be controlled in all analyses relating psychosocial factors to immune function (6, 35): cigarette smoking, heavy alcohol consumption, sleep disruption, exercise, and the use of five types of recreational drugs. MACS participants were predominantly white (96%), well educated (86% attended college), and affluent (68% with incomes > $30,000/year, 60% managerial/professional, 22% technical/sales, 12% service), so confounding by socioeconomic status and ethnicity could be ruled out. Responses to the concealment measure were analyzed as scores on a 5-point ordinal scale (1 = "completely out", 5 = "definitely in the closet"). We also assessed the dose-response relationship between concealment and disease progression by treating concealment scores as a 4-level grouping variable and by conducting trend analyses. (Few participants indicated being "definitely in the closet," so we grouped them with participants who indicated being "in the closet most of the time" to increase group size and to stabilize sampling variance. Substantively identical results emerged from analysis as a 5-level categorical variable, but the SE of parameter estimates for the fully closeted group was substantially inflated because of small group size.) To simplify the graphical presentation of results, concealment scores were also collapsed into two groups representing individuals who were relatively high in concealment (at least "half in the closet") and those who were relatively low ("mostly" or "completely out"). 1 All analyses relating concealment to disease progression controlled for CD4 level at study entry as a measure of disease progression at study entry. Regardless of whether initial CD4 levels were expressed as numbers or percentages, coefficients for concealment indicated similar reductions in times to each end point (e.g., in analyses of concealment scale scores, acceleration values ranged between —4.4 and -13.1% per scale point for number CD4 vs. -7.7 and -14.9% for percentage of CD4). However, analyses using CD4 number produced less significant p values because SE for all coefficients were inflated by the increased random variability associated with CD4 numbers. Relative to CD4 percentages (which depend only on relatively accurate flow cytometry results), CD4 numbers are known to show increased measurement error (due to measurement error in the white blood cell differential). As a result, CD4 numbers are known to be poorer predictors of HIV progression than CD4 percentage, and studies comparing the two suggest that percentage of CD4 be used instead of number of CD4 in analyses of HIV progression (49-50). Psychosomatic Medicine 58:219-231 (1996) RESULTS Concealed Homosexuality and Biobehavioral Characteristics All members of this sample reported being either exclusively or predominantly homosexual. Few (4%) of our participants reported being "definitely in the closet" or "in the closet most of the time." A larger number (14%) reported being "half in and half out," with the remainder being "mostly" (38%) or "completely out of the closet" (45%). This distribution of concealment scores is similar to that found in other recent studies of gay men in urban settings (38). Table 1 reports descriptive statistics for the distribution of potential biobehavioral confounders along with the correlation between each characteristic and the 5-level ordinal measure of concealment. Concealment was associated with increased rates of sleep disturbance and unprotected anal-receptive intercourse and decreased rates of physical exercise. Concealment was not significantly correlated with either CD4 level or HIV-related symptomatology at either MACS or NHAPS entry (both -.20 < r < .20, p > .40). Biobehavioral Characteristics and HIV Progression As in previous studies (2), we found that individual differences in times to each HIV-relevant end TABLE 1. Biobehavioral Characteristics Mean (SD) or Percentage Age (yr) Initial CD4 (% total lymphocytes) Antiretroviral use (during entire study) Frequency of unprotected analreceptive intercourse (mean/6 months during entire study) Exercise (average a 1 day/wk) Sleep disturbance (average a 2 nights/wk) Cigarette smoking (any in previous 6 mo) Alcohol consumption (£3 drinks max/24 h during previous 6 mo) Drug use (any in previous 6 mo) Marijuana/hashish Nitrite inhalants Cocaine Amphetamines Barbiturates/tranquilizers/sedatives Correlation P with Concealment 34.4 (6.13) -.032 .775 40.0 (7.17) .181 -.151 53.8 .195 .146 1.12 (1.72) .211 .060 75.0 57.5 -.287 .257 .010 .021 38.8 .030 .791 67.5 .159 .159 63.8 41.3 20.0 11.3 17.5 .049 .123 -.136 -.096 -.068 .664 .276 .228 .395 .550 223 S. W. COLE et al. point could be predicted from age, disease progression at MACS entry (indexed by CD4 level), and frequency of unprotected anal-receptive intercourse (all p < .05 in multivariate models controlling for all biobehavioral factors listed in Table 1). We also found, as have previous studies (57), that antiretroviral use was associated with significant differences in times to critically low CD4 level and times to AIDS diagnosis (both p < .05) but not times to AIDS mortality [p > .20). In addition, cocaine use, cigarette smoking, and use of barbiturates/tranquilizers/ sedatives each independently predicted times to all end points (all p < .05). None of the other biobehavioral characteristics listed in Table 1 predicted disease progression across all three end points, although several predicted times to one or two. As a set, biobehavioral variables accounted for 33, 54, and 85% of the total deviance in times to 15% CD4, AIDS diagnosis, and AIDS mortality, respectively (all p < .001). In each case, variations in age and CD4 level at study entry were the strongest predictors. Concealment and HIV Progression In every analysis conducted, adding measures of concealed homosexual identity significantly improved the predictive power of a basic model including initial CD4 level, age, antiretroviral use, unprotected anal-receptive intercourse, exercise, sleep disturbance, cigarette smoking, alcohol consumption, and recreational drug use (p < .05 for each likelihood ratio increment-to-fit test). Relative to participants who indicated being "mostly" or "completely out of the closet," those who reported being "half" or more "in the closet" experienced a 40% reduction in times to a critically low CD4 T lymphocyte level (p = .007), a 38% reduction in times to AIDS diagnosis (p = .002), and a 21% reduction in times to death (p = .012). Figures 2 and 3 portray the magnitude of these effects for CD4 T lymphocyte levels and for times to AIDS diagnosis and mortality. Parameter estimates from analyses treating degree of concealment as a 5-level score indicated a 7 to 14% reduction in time to each HIV-relevant end point with each successive degree of concealment (all p < .05). Trend analyses treating degree of concealment as a 4-level categorical score (Table 2) indicated a significant linear decline in times to each HIVrelevant end point as degree of concealment increased (all p < .05). After accounting for biobehavioral variables, concealment accounted for an additional 3 to 6% of the total deviance in times to each end point. 224 CD4 decline 0 2 4 6 8 Time since MACS entry (years) Fig. 2. CD4 loss rate. Median CD4 percentage ± bootstrap SE (78). CD4 percentages did not differ at study entry (p = AIDS and HIV mortality i Closet: AIDS Death ° U t : "AIDS "Delth" 2 4 6 8 10 Time since MACS entry (years). Fig. 3. Times to AIDS diagnosis and mortality. Estimates based on model controlling for biobehavioral characteristics listed in Table 1. Survivor functions are truncated at median event time to facilitate comparison and to avoid extrapolation beyond observed data. Across all three HIV-relevant end points, the lowest concealment score ("completely out") was associated with slightly shorter progression times than the next lowest score ("out most of the time"), but this difference was not statistically significant in any of the analyses conducted (all p > .20). The appearance of a statistically significant quadratic trend in AIDS mortality times (Table 2) suggested that the dose-response function may level off at the lowest levels of concealment. However, this hypothesis was not supported by significant quadratic trends in times to critical CD4 level or AIDS diagnosis (Table 2). Although these data offer partial support for the notion that HIV progression times may not differ for Psychosomatic Medicine 58:219-231 (1996) CONCEALED HOMOSEXUALITY TABLE 2. HIV Progression as a Function of Degree of Concealment Acceleration Coefficient (% change relative to mean event time) 15%CD4 AIDS diagnosis AIDS mortality Trend Analysis (p values) Completely Out Mostly Out Half Out Half In Less than Half Out Omnibus Linear Trend Quadratic Trend Cubic Trend +27.8 + 22.2 + 10.3 + 37.7 + 38.7 + 15.5 -17.3 -9.5 + 3.8 -31.3 -34.8 -24.4 .001 .006 .002 .027 .001 .001 .533 .112 .031 .245 .250 .878 those who are "mostly" or "completely out of the closet," they indicate a consistent linear dose-dependent decrease in HIV progression times as concealment increases through moderate to high levels (i.e., from "mostly out" to "half in and half out" to "in the closet most of the time" and "definitely in the closet"). Concealment was not significantly associated with either time from study entry to, or CD4 level at the commencement of antiretroviral therapy (both -.20 < r < .20, p > .40). However, to ensure that variations in the initiation and duration of antiretroviral treatment could not explain the observed progression differences, we also fitted Cox proportional hazards regression models treating antiretroviral use as a time-varying covariate. Again, degree of concealment (no matter how it was coded) significantly predicted times to each HIV-relevant end point (all p < .05). Psychosocial and Behavioral Mediators If concealing homosexual identity affects HIV progression only indirectly through its impact on mediating variables (e.g., social support, affective states), then a) putative mediators should correlate with degree of concealment, and b) statistical adjustment for the effects of these mediators should eliminate concealment-related differences in disease progression. We considered 17 psychosocial characteristics that might potentially mediate relationships between concealment and HIV progression, including individual differences in depression (CES-D, POMS depression-dejection), anxiety (TMAS, POMS tension-anxiety), and other dimensions of affect (POMS fatigue-inertia, anger-hostility, vigor-activity, confusion-bewilderment), social support (UCLA Loneliness, number of confidants, four dimensions of AIDS-specific social support), repressive coping style, presence of a primary partner, and frequency of anonymous sexual contact. Table 3 reports descriptive statistics and correlations with concealment for each potential mediator. This sample Psychosomatic Medicine 58:219-231 (1996) showed relatively low levels of depression (e.g., 18% with CES-D scores ^ 16), anxiety, and social isolation and relatively high levels of social support. Of the 17 potential mediators considered, only the presence of repressive coping style correlated significantly with degree of concealment (point biserial r = .346, p < .01; for all other mediators, -.20 < r < .20, p > .05). However, none of these potential mediators consistently predicted HIV progression2, and estimates of concealment-related differences in HIV progression were not significantly reduced by control for any of these variables (including repressive coping style). In models controlling for each potential mediator or for all potential mediators simultaneously, ordinal concealment scores and trend analyses continued to indicate a significant negative dose-response relationship between degree of concealment and times to each HIV-relevant end point (all p < .05). As a result, the accelerated course of HIV infection in closeted participants cannot be attributed to differences in anxiety, depression, so- 2 Several potential mediators did predict times to one end point but not others. In analyses controlling for all biobehavioral predictors (Table 1), deficits in AIDS-specific social support (desired - received) were associated with longer times to a critically low CD4 level ( + 18.3%, p = .048) but not with significant differences in times to AIDS diagnosis or mortality. High levels of both desired and received AIDS-specific social support were associated with accelerated progression to AIDS mortality (-8.2% and -7.6%, respectively, p = .025 and .013) but no significant differences in times to AIDS diagnosis or critical CD4. In contrast to these results associating social support with accelerated disease progression, presence of a primary partner predicted longer times to AIDS diagnosis (+22.2%, p = .039) and AIDS mortality (+17.9%, p = .003) but not critical CD4. No significant predictions were made by anxiety, depression, POMS affective states, loneliness, satisfaction with AIDS-specific social support, repressive coping style, or rates of anonymous sexual contact. The small ratio of significant results to the total number of mediational analyses (5/51: 17 mediators X 3 end points) and the inconsistency of results across end points suggest that the scattered pattern of significant mediational predictions may reflect Type 1 errors rather than substantive effects. 225 S. W. COLE et al. TABLE 3. Potential Psychosocial Mediators Anxiety (20-point Bendig/TMAS) Depression Total CES-D CESDs 16 Mood (POMS) (mean on 0 - 4 scale) Depression-dejection Tension-anxiety Anger-hostility Fatigue-inertia Confusion-bewilderment Vigor-activity Repressive coping style (present) Primary partner (present a 6 mo) Number of close confidants Loneliness (total UCLA score) AIDS-specific social support (0-5 scale) Desired Received Satisfaction Deficit (Desired - Received) Anonymous sexual partners (6 mo) Mean (SD) or Percentage Correlation with Concealment 6.08 (4.23) -.06 .60 9.17(9.96) 18.4 -.01 -.03 .90 .77 0.69 (0.77) 1.20(0.84) 0.85 (0.75) 1.17 (0.94) 0.90 (0.78) 2.34 (0.79) 11.3 43.7 3.28(1.65) 37.2 (12.0) -.03 -.08 -.05 -.07 .00 -.20 .35 .01 -.18 .16 .76 .47 .68 .56 .98 .08 <.O1 .91 .10 .16 2.14(0.95) 2.12(0.92) 2.56 (0.99) 0.03 (0.66) 3.37(11.4) -.09 -.17 -.19 .11 -.05 .41 .12 .10 .34 .67 cial support, repressive coping style, primary partner status, or anonymous sexual contact. DISCUSSION In this sample of gay men, HIV infection advanced more rapidly among those who concealed their homosexual identity than among those who did not. Times to a critically low level of CD4 T lymphocytes, times to AIDS diagnosis, and times to AIDS-related mortality all declined significantly as degree of concealment increased from "mostly out of the closet" to "definitely in the closet." HIV infection did not progress significantly more rapidly among those who were "mostly out of the closet" than among those who were "completely out of the closet," suggesting that only moderate to high levels of concealment may be associated with significant accelerations in disease progression. The accelerated course of HIV infection in relatively closeted participants could not be attributed to differences in age, disease progression at study entry, medical treatment (e.g., antiretroviral use), health-relevant biobehavioral characteristics (e.g., sexual practices, alcohol and recreational drug use, cigarette smoking, exercise, sleep disturbance), or psychosocial characteristics (e.g., anxiety, depression, repressive coping style, social support). In 226 P addition, the present sample was homogeneous on other demographic dimensions that have been linked to disease progression (for example, gender, ethnicity, risk group, e.g., hemophiliac vs. homosexual), so these characteristics cannot explain the progression differences observed. As a set, biobehavioral characteristics predicted 33 to 85% of total deviance in times to each end point, with differences in age and CD4 level at study entry representing the strongest predictors. Degree of concealed homosexual identity predicted an additional 3 to 6% of total deviance in times to each end point, an effect that amounted to a 1.5- to 2-year difference in median HIV progression times for those "half" or "more" in the closet relative to those "mostly" or "completely" out. The magnitude of concealment-related differences was similar to those associated with most biobehavioral variables considered individually (e.g., antiretroviral use was associated with an approximate 1-1.5-year difference in times to critically low CD4 and AIDS diagnosis, as was a 10-year age differential, or a difference in initial CD4 level of 160 cell/mm3 or 10% of total lymphocytes). The present results are consistent with data from another study of 222 HIV-seronegative gay men in which we found an increased incidence of several infectious and neoplastic diseases as degree of concealment increased (58). Previous research also indicated increased rates of psychosomatic symptomPsychosomatic Medicine 58:219-231 (1996) CONCEALED HOMOSEXUALITY atology among closeted gay men (32). Thus, other data converge with the present findings in linking concealed homosexuality to heightened physical health risk. Other studies using different models of psychological inhibition (i.e., contexts unrelated to homosexual identity) have also shown effects on physical health outcomes (9, 23-24). Within the domain of HIV infection, these results are also consistent with other longitudinal studies linking HIV progression to psychosocial factors (e.g., bereavement, depression, denial, cognitive behavioral interventions, and expectancies about survival) (6-7, 37, 59-70), although other studies have failed to find such effects (e.g., for depression) (6-7, 71). When considering the health differences associated with concealed homosexuality, it is important to note that "passing" as a heterosexual is not a discrete proposition. Gay men may be "in" vs. "out" to various degrees (e.g., known vs. suspected vs. not suspected) and to various audiences (e.g., friends, family, co-workers, other gay men) (32-33). Most of our respondents reported intermediate levels of concealment, and ancillary analyses (not reported here) suggested that these individuals were in the closet to a greater extent at work and in public than they were among friends or family members. However, even partial concealment would require gay men to inhibit the expression of homosexual identity over significant periods of time in highly consequential settings (e.g., 8 hours a day at work). Although this sample contained few individuals at the most closeted end of the concealment continuum, the doseresponse relationship observed over intermediate levels of concealment supports the fundamental hypothesis relating degree of concealment to physical health risk. There are a variety of reasons why concealing homosexual identity might be associated with an accelerated course of HIV infection. These analyses were motivated by experimental research indicating that psychological inhibition can influence healthrelevant physiological parameters (e.g., specific aspects of sympathetic nervous system activity and immune function) (9-13, 20-22, 24-25). To the extent that living in the closet requires gay men to inhibit the expression of subjectively significant thoughts, feelings, and social behaviors, the present results are consistent with hypotheses suggesting a causal influence of psychological inhibition on physical health. However, the present data come from a nonexperimental analysis and are thus equally consistent with other possible hypotheses that do not imply any causal influence of concealment on physical health. Psychosomatic Medicine 58:219-231 (1996) For example, gay men who are in the closet may differ from those who are out by possessing a syndrome of neurophysiological and psychosocial characteristics known as "inhibited temperament" (7273). Previous research on the inhibited temperament syndrome has identified components that could influence both immune function (e.g., heightened activity in the sympathetic nervous system) and the social presentation of homosexual identity (e.g., heightened sensitivity to others and their evaluation of the self) (72-73). Both of these characteristics are believed to be associated with individual differences in activity in specific central nervous system structures (e.g., the amygdala and septo-hippocampal system) (72-74). Under this hypothesis, concealing vs. expressing a homosexual identity would not be expected to influence physical health outcomes unless it was accompanied by changes in central nervous system activity. This neurophysiological-temperamental hypothesis is clearly reminiscent of Galen's constitutional explanation for the association between psychological inhibition and physical illness (8, 73). Closeted gay men may also differ from those who are out in aspects of health-relevant behavior that could potentially influence HIV progression (e.g., drug use, sleep or exercise habits, sexual activities). At study entry, concealment was not confounded by antiretroviral treatment or recreational drug use (including cigarette smoking and heavy alcohol consumption). Concealment was weakly associated with higher rates of unprotected anal-receptive intercourse, higher rates of sleep disturbance, and lower rates of exercise. However, these variables were controlled in all disease progression analyses, and concealment remained a significant predictor of HIV progression despite such controls. In ancillary analyses (not reported here), we also considered the possibility that changes in behavior over the course of the study might have differed for those who were in vs. out of the closet. Random coefficients regression models examining patterns of behavior over time (75) suggested no significant relationship between concealment and changes in recreational drug use, sexual behavior, sleep disruption, or exercise. Thus differential changes in health-relevant behavior do not appear to account for the present results. Variations in social support are known to correlate with many physical health outcomes (76), and concealing homosexual identity might reduce the opportunity for, or effectiveness of, various types of social support. In this sample, most participants reported moderate to high levels of social support, and degree of concealment did not correlate signifi227 S. W. COLE et al. cantly with primary partner status, social isolation, subjective loneliness, or any dimension of AIDSspecific subjective social support (desired, received, desired — received deficit, or satisfaction with received support). Although some aspects of social support were inconsistently associated with times to some studied end points,2 concealment continued to predict disease progression despite control for all measures of social support. Caumartin and colleagues [77] have suggested that low levels of involvement in the gay community may predict accelerated mortality among gay men who have already developed AIDS. However, ancillary analyses of the present data failed to indicate any association between concealment and measures of involvement in the gay community or the number or fraction of friends who were homosexual or bisexual. These results were not surprising given the partial nature of concealment in this sample and given that this sample was recruited from the gay community in west Los Angeles. In other samples, variations in social support may be more marked than in this sample and thus more likely to correlate with physical health outcomes. In addition, aspects of social support not measured in this study (e.g., antagonistic "negative social support," participation in support groups for HIV-infected individuals) could potentially relate to the effects observed here. Some evidence has also suggested that affective states such as depression may relate to indices of HIV progression (e.g., declining CD4 levels) (70), although other studies have failed to find such effects (71). Levels of depression and anxiety were not high in this sample, and they did not correlate with either degree of concealment or HIV progression. Concealment was associated with the presence of a repressive coping style, but repressive style itself did not predict disease progression, and concealment continued to predict HIV progression despite control for differences in repressive style. Closeted gay men may be more reluctant than those who are out to engage in behaviors that might identify their homosexual orientation to others. This could bias decisions to participate in a study of a homosexuality-linked disease such as HIV infection. Although such biases might reduce the overall rate of participation among closeted individuals, this alone would not induce a correlation between concealment and disease progression among those who do elect to participate. Selective nonparticipation by those who subsequently showed relatively slow disease progression could induce such a correlation. However, such an effect would require participants to have information about their likely disease course 228 at study entry, and no such information was available to the individuals analyzed here (all were AIDSfree with normal CD4 levels at study entry, and none was aware of his HIV serostatus). Reluctance to be identified with a homosexualitylinked disease might also lead closeted participants to delay or forego medical treatments linked to HIV infection (e.g., antiretroviral therapy). Concealment was not significantly associated with either time from study entry to, or CD4 level at the commencement of antiretroviral therapy, and concealment continued to predict HIV progression despite control for antiretroviral use as a time-varying covariate. Potential delays in implementing other forms of treatment (e.g., prophylaxis against opportunistic infections, dietary changes, homeopathic or other "alternative therapies") could not be evaluated because these treatments were not measured in the present study. However, the lack of correlation between concealment and antiretroviral use suggests that closeted participants did not experience a generalized reluctance to seek appropriate medical treatment. Advancing HIV infection could conceivably influence a gay man's ability to conceal his homosexuality. However, such an effect would induce a negative relationship between disease progression and concealment, rather than the positive association observed in these data. In addition, concealment was measured prospectively in a concurrently healthy group of individuals, rendering it unlikely that overt symptomatology would influence degree of concealment in this analysis. Consistent with this conclusion, we found no significant relationship between concealment and either CD4 levels or HIV-related symptomatology at NHAPS entry (when concealment was assessed)3. The structure of this sample and the variables controlled ruled out a variety of potential explanations for the accelerated course of HIV infection observed in closeted participants (e.g., differences in anxiety, depression, repressive coping, positive social support, unsafe sexual practices, demographic characteristics, health practices, recreational drug use, antiretroviral treatment, participation biases stemming from reluctance to be identified with a 3 Negligible correlations between concealment and CD4 levels at study entry are not surprising because analyses were restricted to individuals who were healthy at study entry. However, the differential advance of HIV infection did induce significant negative correlations between concealment and CD4 levels during the later periods of the study. Psychosomatic Medicine 58:219-231 (1996) CONCEALED HOMOSEXUALITY homosexuality-linked disease, and causal influences of disease progression on concealment). Several other hypotheses could not be fully evaluated because these data contained no measures of putatively influential constructs (e.g., concealment-induced psychological inhibition, neurophysiological characteristics of "inhibited temperament," "negative social support," support group utilization). As a result, the mechanisms linking concealed homosexual identity to accelerated HIV progression remain unclear. Until such mechanisms are identified and the present findings replicated, these results should be interpreted with great caution. In particular, two important limitations inherent in the epidemiological design of the present study need to be borne in mind. First, these results are based on a study of relatively affluent, predominantly white, and initially healthy volunteers from the west Los Angeles metropolitan area. Although this sample is representative of all HIV-seropositive Los Angeles MACS participants on MACS-assessed variables and is representative of healthy NHAPS participants on NHAPS-assessed variables, it is unknown whether Los Angeles MACS/NHAPS participants are representative of gay men in general. Many researchers have questioned whether there even exists a population of "gay men in general" (as opposed to a multitude of subpopulations defined by geographic and demographic criteria). Even if such a population does exist, it would be impossible to evaluate sampling representativeness because stigmatization prevents the establishment of any valid sampling frame for homosexual men (38). Although the distribution of concealment scores in this sample was comparable to that found in other recent samples of gay men in urban settings (38), it still remains to be determined how these results might generalize to other groups of gay men. Second, the observational nature of this study does not permit any causal conclusions about the mechanism relating concealed homosexual identity to accelerated HIV progression. In particular, these results do not imply that "coming out of the closet" will improve physical health. Differences between individuals cannot inform us about the effects of a single individual's change in status. Even if changes in the public expression of homosexual identity were shown to affect health within individuals, any potential benefit would constitute only one of many factors to consider in determining when and to whom one should express aspects of homosexual identity. However, these data do raise the possibility that gay men may suffer significant health costs as Psychosomatic Medicine 58:219-231 (1996) they attempt to appease societal prejudice by concealing their sexual orientation. Whether such costs might be offset by potential benefits of concealment (e.g., sparing gay men stigmatization, ostracism, or physical assault) is an important consideration and a potentially fruitful topic for further research. However, these data suggest that the psychological, behavioral, and biological correlates of social identity may be relevant to understanding individual differences in physical health and illness. SUMMARY On the basis of hypotheses linking psychological inhibition to physical illness, we examined the rate at which HIV infection progressed in 80 gay men who varied in the extent to which they publicly expressed their homosexual identity. Those who were "half" or "more" in the closet reached a critically low level of CD4 T lymphocytes, AIDS diagnosis, and AIDS mortality significantly faster than did those who were "mostly" or "completely out of the closet." The accelerated course of HIV infection in closeted gay men could not be explained by differences in disease progression at study entry, medical treatment, HIV-relevant sexual practices, health-relevant behavioral practices (e.g., sleep disruption, exercise, recreational drug use), anxiety, depression, social support, or repressive coping style. These results parallel those of a similar study of 222 HIVseronegative gay men documenting a heightened incidence of infectious and neoplastic diseases as degree of concealment increased. Both findings are consistent with previous research linking psychological inhibition to alterations in measures of sympathetic nervous system activation, immune function, and physical health. This research was supported by funding from the National Institute of Mental Health (MH42918) and the National Institute of Allergy and Infectious Diseases (N01-A1-72631). Steve W. Cole was supported in part by NIMH Grant MH 15750, and Margaret E. Kemeny was supported in part by the NIMH Research Scientist Development Award MH 00820. Special thanks to Joanie Chung, MPH, and Mei Ling Shen, MPH, for their help in data management and to all MACS/NHAPS participants for their continual support and contribution. REFERENCES 1. Levy JA: Pathogenesis of human immunodeficiency virus infection. Microbiol Rev 57:183-289, 1993 229 S. W. COLE et al. Phair J, Jacobson L, Detels R, et al: Acquired Immune Deficiency Syndrome within 5 years of infection with Human Immunodeficiency Virus Type-1: The Multicenter AIDS Cohort Study. J Acquir Immun Defic Syndrome 5:490-496,1992 Sheppard HW, Lang W, Ascher MS, et al: The characterization of non-progressors: Long term HIV-1 infection with stable CD4+ T-cell levels. AIDS 7:1159-1166, 1993 Munoz A, Wang MC, Bass S, et al: Acquired Immunodeficiency Syndrome (AIDS)-free time after Human Immunodeficiency Syndrome Virus Type 1 (HIV-1) seroconversion in homosexual men. Multicenter ADDS Cohort Study Group. Am J Epidemiol 130:530-539, 1989 Detels R, English PA, Giorgi JV, et al: Patterns of CD4+ cell changes after HIV-1 infection indicate the existence of a codeterminant of AIDS. J Acquir Immun Defic Syndrome 1:390-395, 1988 Kemeny ME: Stressful events, psychological responses, and progression of HIV infection. In Glaser R, Kiecolt-Glaser J (eds), Handbook of Human Stress and Immunity. New York, Academic Press, 1994 Kemeny ME: Psychoneuroimmunology of HIV infection. Psychiatr Clin North Am 17:55-68, 1994 Siegel RE: Galen's System of Physiology and Medicine. New York, Karger, 1968 Pennebaker JW: Overcoming inhibition: Rethinking the roles of personality, cognition, and social behavior. In Traue HC, Pennebaker JW (eds), Emotion, Inhibition and Disease. Kirkland, WA, Hogrefe & Huber, 1993, 100-115 Gross JJ, Levinson RW: Emotional suppression: Physiology, self-report, and expressive behavior. J Pers Soc Psychol 64: 970-986, 1993 Koriat A, Melkman R, Averill JA, Lazarus R: The self-control of emotional reactions to a stressful film. ] Pers 40:601-619, 1972 Pennebaker JW, Chew CH: Behavioral inhibition and electrodermal activity during deception. J Pers Soc Psychol 49:14271433, 1985 Wegner DM, Shortt JW, Blake AW, et al: The suppression of exciting thoughts. J Pers Soc Psychol 58:409-418, 1990 Crary B, Hauser SL, Borysenko M, et al: Epinephrine-induced changes in the distribution of lymphocyte subsets in the peripheral blood of humans. J Immunol 131:1178-1181,1983 Felten DL, Felten SY, Bellinger DL, et al: Noradrenergic sympathetic neural interactions with the immune system: Structure and function. Immunol Rev 100:225-260, 1987 Ottaway CA, Husband AJ: Central nervous system influences on lymphocyte migration. Brain Behav Immun 6:97-116, 1992 Roszman TL, Carlson SL: Neurotransmitters and molecular signals in the immune response. In Ader R, Felten DL, Cohen N (eds), Psychoneuroimmunology, 2nd Edition. San Diego, Academic Press, 1991, 311-338 Sanders VM, Munson AE: Norepinephrine and the antibody response. Pharmacol Rev 37:229-248, 1985 Stein M, Schliefer SJ, Keller SE: Hypothalamic influences on immune response. In Ader R (ed), Psychoneuroimmunology. Orlando, FL, Academic Press, 1981, 429-448 Pennebaker JW, Hughes C, O'Heeron RC: The psychophysiology of confession: Linking inhibitory and psychosomatic processes. J Pers Soc Psychol 52:781-793, 1987 Pennebaker JW, Kiecolt-Glaser JK, Glaser R: Disclosure of traumas and immune function: Health implications for psychotherapy. J Consult Clin Psychol 56:239-245, 1988 Esterling BA, Antoni MH, Fletcher MA, et al: Emotional 230 disclosure through writing or speaking modulates latent Epstein-Barr virus reactivation. J Consult Clin Psychol 62: 130-140, 1994 23. Francis ME, Pennebaker JW: Putting stress into words: The impact of writing on physiological, absentee, and self-reported well-being measures. Am J Health Promo 6:280-287, 1992 24. Pennebaker JW, Beall SK: Confronting a traumatic event: Toward an understanding of inhibition and disease. J Abnorm Psychol 95:274-281, 1986 25. Booth RJ, Petrie KJ, Pennebaker JW, et al: Disclosure of trauma and the immune response to hepatitis B vaccination. Abstract presented at the Meeting of the Psychoneuroimmunology Research Society, Key Biscane, FL, 1994 26. Contrada RJ, Leventhal H, O'Leary A: Personality and health. In Pervin LA (ed), Handbook of Personality: Theory and Research. New York, Guilford Press, 1990, 638-669 27. Gross J: Emotional expression in cancer onset and progression. Soc Sci Med 28:1239-1248, 1989 28. James SA: Psychosocial precursors of hypertension: A review of the epidemiologic literature. Circulation 76(Suppl l):I60166, 1987 29. Sommers-Flanagan J, Greenberg RP: Psychosocial variables and hypertension: A new look at an old controversy. J Nerv Ment Dis 177:15-24, 1989 30. Solomon GF, Moos RH: Emotions, immunity, and disease: A speculative theoretical integration. Arch Gen Psychiatry 11: 657-674, 1964 31. Herek GM: Hate crimes against lesbians and gay men. Am Psychol 44:948-955, 1989 32. Weinberg MS, Williams CJ: Male Homosexuals: Their Problems and Adaptations. New York, Oxford University Press, 1974 33. Bell AP, Weinberg MS: Homosexualities: A Study of Diversity Among Men and Women. New York, Simon and Schuster, 1978 34. Kaslow RA, Ostrow DG, Detels R, et al: The multicenter AIDS cohort study: Rationale, organization, and selected characteristics of the participants. Am J Epidemiol 126:310-318, 1987 35. Kiecolt-Glaser JK, Glaser R: Methodological issues in behavioral immunology research with humans. Brain Behav Immun 2:67-78, 1988 36. Taylor SE, Kemeny ME, Aspinwall LG, et al: Optimism, coping, psychological distress, and high-risk sexual behavior among men at risk for acquired immunodeficiency syndrome (AIDS). J Pers Soc Psychol 63460-473, 1992 37. Kemeny ME, Weiner H, Taylor SE, et al: Repeated bereavement, depressed mood, and immune parameters in HIV seropositive and seronegative homosexual men. Health Psychol 13:14-24, 1994 38. Martin JL, Dean L: Developing a community sample of gay men for an epidemiologic study of AIDS. Am Behav Sci 33:546-561, 1990 39. Radloff LS: The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas 1:386-401, 1977 40. McNair DM, Lorr M, Droppleman LF: Profile of Mood States. San Diego, Educational and Industrial Testing Service, 1980 41. Bendig AW: The development of a short form of the Manifest Anxiety Scale. J Consult Psychol 20:384, 1956 42. Russell D, Peplau LA, Cutrona CE: The revised UCLA Loneliness Scale: Concurrent and discriminant validity evidence. J Pers Soc Psychol 39:472-480, 1980 43. Schwarzer R, Dunkel-Schetter C, Kemeny ME: The multidi- Psychosomatic Medicine 58:219-231 (1996) CONCEALED HOMOSEXUALITY 44. 45. 46. 47. 48. 49. 50. 51. 52. 53. 54. 55. 56. 57. 58. 59. 60. 61. mensional nature of received social support in gay men at risk of HIV infection and AIDS. Am J Commun Psychol 22:319339, 1994 Strahan R, Gerbasi KC: Short, homogeneous versions of the Marlowe-Crowne Social Desirability Scale. J Clin Psychol 28:191-193, 1972 Weinberger DA, Schwartz GE, Davidson RE: Low anxious, high anxious and repressive coping styles: Psychometric patterns and behavioral and physiological responses to stress. J Abnorm Psychol 88:369-380, 1979 Nishanian P, Taylor JMG, Korns E, et al: Significance of quantitative enzyme-linked immunosorbent assay (ELISA) results in evaluation of three ELISAs and Western blot tests for detection of antibodies to human immune deficiency virus in a high risk population. J Clin Microb 25:395-400, 1987 Centers for Disease Control: Revision of the CDC surveillance case definition for Acquired Immunodeficiency Syndrome. MMWR Morb Mortal Wkly Rep 36:lS-15S, 1987 Giorgi JV, Cheng H-L, Margolick JB, et al: Quality control in the flow cytometric measurement of T-lymphocyte subsets: The Multicenter Aids Cohort Study (MACS) experience. Clin Immunol Immunopathol 55:173-186, 1990 Taylor JMG, Fahey JL, Detels R, et al: CD4 percentage, CD4 number, and CD4: CD8 ratio in HIV infection: Which to choose and how to use. ] Acquir Immun Defic Syndrome 2:114-124, 1989 Burcham J, Marmor M, Dubin N, et al: CD4% is the best predictor of development of AIDS in a cohort of HIV-infected homosexual men. AIDS 5:365-372, 1991 Saah AJ, Hoover DR, He Y, et al: Factors influencing survival after AIDS: Report from the Multicenter AIDS Cohort Study (MACS). J Acquir Immun Defic Syndrome 7:287-295, 1994 Fahey JL, Taylor JMG, Detels R, et al: The prognostic value of cellular and serologic markers in infection with human immunodeficiency virus type 1. N Engl J Med 322:166-172, 1990 Phillips AN, Lee CA, Elford J, et al: Serial CD4 lymphocyte counts and development of AIDS. Lancet 337:389-392, 1991 Phillips AN, Lee CA, Elford J, et al: The cumulative risk of AIDS as the CD4 lymphocyte count declines. J Acquir Immun Defic Syndrome 5:148-152, 1992 Kalbfleisch JD, Prentice RL: The Statistical Analysis of Failure Time Data. New York, Wiley, 1980 Miller RG: What price Kaplan-Meier? Biometrics 39:10771081, 1983 Aboulker JR, Swart AM: Preliminary analysis of the Concorde Trial. Lancet 341:889-890, 1993 Cole SW, Kemeny ME, Taylor SE, Visscher BR: Elevated physical health risk among gay men who conceal their homosexual identity. Health Psychol, in press Solano L, Costa M, Salvati S, et al: Psychosocial factors and clinical evolution in HIV-l infection: A longitudinal study. J Psychosom Res 37:39-51, 1993 Kemeny ME, Weiner H, Duran R, et al: Immune system changes following the death of a partner in HIV positive gay men. Psychosom Med, in press Goodkin K, Blaney NT, Feaster D, et al: Active coping style is associated with natural killer cell cytotoxicity in asymptom- Psychosomatic Medicine 58:219-231 (1996) atic HIV-l seropositve homosexual men. J Psychosom Res 36:635-650, 1992 62. Goodkin K, Fuchs I, Feaster D, et al: Life stressors and coping style are associated with immune measures in HIV-l infection: A preliminary report. Int J Psychiatry Med 22:155-172, 1992 63. Antoni MH, Baggett L, Ironson G, et al: Cognitive-behavioral stress management intervention buffers distress responses and immunologic changes following notification of HIV-l seropositivity. J Consult Clin Psychol 59:906-915, 1991 64. Esterling BA, Antoni MH, Schneiderman N, et al: Psychosocial modulation of antibody to Epstein-Barr viral capsid antigen and human herpesvirus type-6 in HIV-l infected and at-risk gay men. Psychosom Med 54:354-371, 1992 65. Kemeny ME, Reed GM, Taylor S, et al: Negative HIV-specific expectancies predict immunologic evidence of HIV progression. Health Psychol, in press 66. Reed GM, Kemeny ME, Taylor SE, et al: Negative HIV-specific expectancies and AIDS-related bereavement as predictors of symptom onset in asymptomatic HIV seropositive gay men. Health Psychol, in press 67. Reed GM, Kemeny ME, Taylor SE, et al: "Realistic acceptance" as a predictor of survival time in gay men with AIDS. Health Psychol 13:299-307, 1994 68. Soloman GF, Temoshok L, O'Leary A, et al: An intensive psychoimmunologic study of long-surviving persons with AIDS. Ann N Y Acad Sci 496:647-655, 1987 69. Ironson G, Friedman A, Klimas N, et al: Distress, denial, and low adherence to behavioral interventions predict faster disease progression in gay men infected with Human Immunodeficiency Virus. Int J Behav Med 1:90-105, 1994 70. Burack JH, Barrett DC, Stall RD, et al: Depressive symptoms and CD4 lymphocyte decline among HIV-infected men. J Am Med Assoc 270:2568-2573, 1993 71. Lyketsos CG, Hoover DR, Guccione M, et al: Depressive symptoms as predictors of medical outcomes in HIV infection. J Am Med Assoc 270:2563-2567, 1993 72. Kagan J: The concept of behavioral inhibition to the unfamiliar. In Reznick JS (ed), Perspectives on Behavioral Inhibition. Chicago, University of Chicago Press, 1989, 1-23 73. Kagan J: Galen's Prophecy: Temperament in Human Nature. New York, Basic Books, 1994 74. Gray JA: The neuropsychology of temperament. In Strelau J, Angleitner A (eds), Explorations in Temperament: International Perspectives on Theory and Measurement. New York, Plenum Press, 1991, 105-128 75. Gibbons RD, Hedeker D, Elkin I, et al: Some conceptual and statistical issues in analysis of longitudinal psychiatric data. Arch Gen Psychiatry 50:739-750, 1993 76. Berkman LF: The role of social relations in health promotion. Psychosom Med 57:245-254, 1995 77. Caumartin S, Joseph JG, Chmiel J: Premorbid psychosocial factors associated with differential survival time in AIDS patients. Abstract presented at the VII International Conference on AIDS, Florence, Italy, 1991 78. Efron B, Tibshirani RJ: An Introduction to the Bootstrap. New York, Chapman and Hall, 1993 231