Immunobiology of the human MHC class I chain
Anuncio
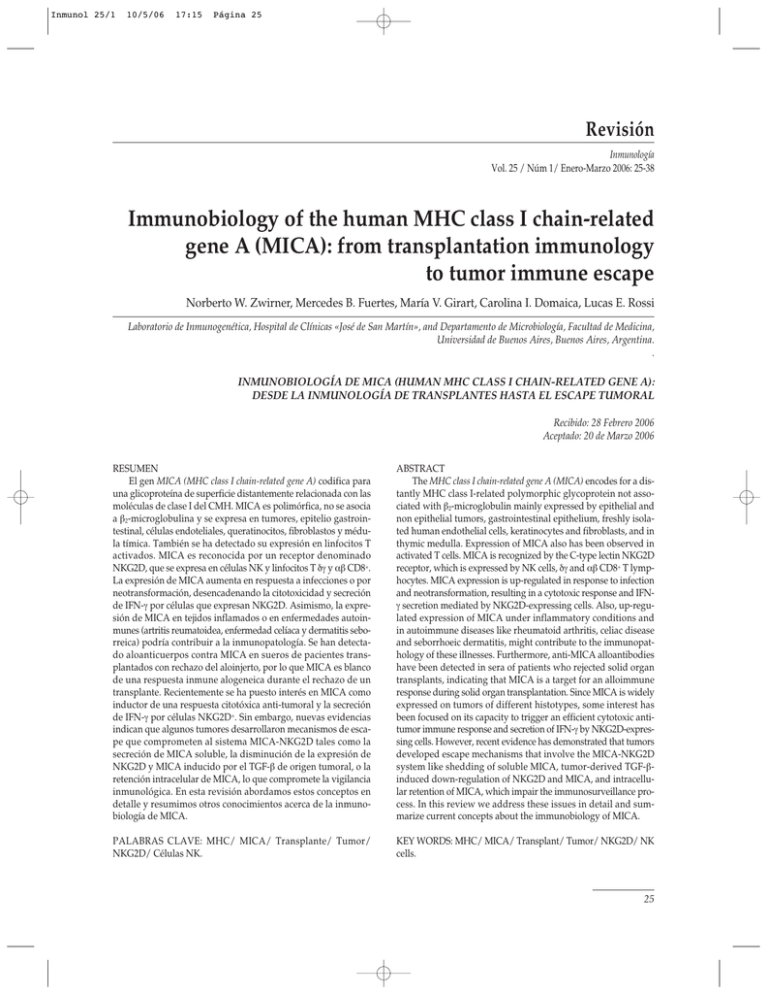
Inmunol 25/1 10/5/06 17:15 Página 25 Revisión Inmunología Vol. 25 / Núm 1/ Enero-Marzo 2006: 25-38 Immunobiology of the human MHC class I chain-related gene A (MICA): from transplantation immunology to tumor immune escape Norberto W. Zwirner, Mercedes B. Fuertes, María V. Girart, Carolina I. Domaica, Lucas E. Rossi Laboratorio de Inmunogenética, Hospital de Clínicas «José de San Martín», and Departamento de Microbiología, Facultad de Medicina, Universidad de Buenos Aires, Buenos Aires, Argentina. . INMUNOBIOLOGÍA DE MICA (HUMAN MHC CLASS I CHAIN-RELATED GENE A): DESDE LA INMUNOLOGÍA DE TRANSPLANTES HASTA EL ESCAPE TUMORAL Recibido: 28 Febrero 2006 Aceptado: 20 de Marzo 2006 RESUMEN El gen MICA (MHC class I chain-related gene A) codifica para una glicoproteína de superficie distantemente relacionada con las moléculas de clase I del CMH. MICA es polimórfica, no se asocia a β2-microglobulina y se expresa en tumores, epitelio gastrointestinal, células endoteliales, queratinocitos, fibroblastos y médula tímica. También se ha detectado su expresión en linfocitos T activados. MICA es reconocida por un receptor denominado NKG2D, que se expresa en células NK y linfocitos T δγ y αβ CD8+. La expresión de MICA aumenta en respuesta a infecciones o por neotransformación, desencadenando la citotoxicidad y secreción de IFN-γ por células que expresan NKG2D. Asimismo, la expresión de MICA en tejidos inflamados o en enfermedades autoinmunes (artritis reumatoidea, enfermedad celíaca y dermatitis seborreica) podría contribuir a la inmunopatología. Se han detectado aloanticuerpos contra MICA en sueros de pacientes transplantados con rechazo del aloinjerto, por lo que MICA es blanco de una respuesta inmune alogeneica durante el rechazo de un transplante. Recientemente se ha puesto interés en MICA como inductor de una respuesta citotóxica anti-tumoral y la secreción de IFN-γ por células NKG2D+. Sin embargo, nuevas evidencias indican que algunos tumores desarrollaron mecanismos de escape que comprometen al sistema MICA-NKG2D tales como la secreción de MICA soluble, la disminución de la expresión de NKG2D y MICA inducido por el TGF-β de origen tumoral, o la retención intracelular de MICA, lo que compromete la vigilancia inmunológica. En esta revisión abordamos estos conceptos en detalle y resumimos otros conocimientos acerca de la inmunobiología de MICA. ABSTRACT The MHC class I chain-related gene A (MICA) encodes for a distantly MHC class I-related polymorphic glycoprotein not associated with β2-microglobulin mainly expressed by epithelial and non epithelial tumors, gastrointestinal epithelium, freshly isolated human endothelial cells, keratinocytes and fibroblasts, and in thymic medulla. Expression of MICA also has been observed in activated T cells. MICA is recognized by the C-type lectin NKG2D receptor, which is expressed by NK cells, δγ and αβ CD8+ T lymphocytes. MICA expression is up-regulated in response to infection and neotransformation, resulting in a cytotoxic response and IFNγ secretion mediated by NKG2D-expressing cells. Also, up-regulated expression of MICA under inflammatory conditions and in autoimmune diseases like rheumatoid arthritis, celiac disease and seborrhoeic dermatitis, might contribute to the immunopathology of these illnesses. Furthermore, anti-MICA alloantibodies have been detected in sera of patients who rejected solid organ transplants, indicating that MICA is a target for an alloimmune response during solid organ transplantation. Since MICA is widely expressed on tumors of different histotypes, some interest has been focused on its capacity to trigger an efficient cytotoxic antitumor immune response and secretion of IFN-γ by NKG2D-expressing cells. However, recent evidence has demonstrated that tumors developed escape mechanisms that involve the MICA-NKG2D system like shedding of soluble MICA, tumor-derived TGF-βinduced down-regulation of NKG2D and MICA, and intracellular retention of MICA, which impair the immunosurveillance process. In this review we address these issues in detail and summarize current concepts about the immunobiology of MICA. PALABRAS CLAVE: MHC/ MICA/ Transplante/ Tumor/ NKG2D/ Células NK. KEY WORDS: MHC/ MICA/ Transplant/ Tumor/ NKG2D/ NK cells. 25 Inmunol 25/1 10/5/06 17:15 Página 26 IMMUNOBIOLOGY OF THE HUMAN MHC CLASS I CHAIN-RELATED GENE A (MICA) ... INTRODUCTION The human major histocompatibility complex (MHC) comprises a cluster of genes mapping to the short arm of chromosome 6. Most of them encode polypeptides mainly involved in antigen presentation to T lymphocytes. In 1994, a new family of polymorphic genes that map within the MHC class I region was described(1). This family was named MHC class I chain-related (MIC, Fig. 1), and comprises 2 functional genes (MICA and MICB) and several pseudogenes MICC to MICF(2). Simultaneously, others described a gene family that was named PERB11(3), but it was soon realized that PERB11.1 is MICA and that PERB11.2 is MICB. MICA has an overall homology of 83% with MICB, but their homology with the classical MHC class I genes is quite low, being between 15 and 35%(1). Typically, MICA encodes for a polypeptide of 383 amino acids that is expressed on the cell surface of different cells and resembles the domain organization of the α chain of MHC class I molecules (one leader peptide encoded by exon 1, three extracellular globular domains encoded by exons 2 to 4, one transmembrane domain encoded by exon 5 and a cytoplasmic tail encoded by exon 6). However, MICA does not associate with β2-microglobulin(4, 5). The polypeptide has a Mr of approximately 42-44 kDa, but the mature protein has a Mr of ~65kDa. This difference is due to glycosilation at 8 potential N-glycosilation sites located along the 3 extracellular domains(4). Recently, alternative spliced forms of MICA lacking exon 3 have been detected(6). Although these polypeptides can reach the cell surface, it is currently unknown if they are functional. The crystal structure of MICA has revealed some unusual characteristics for a MHC class I-encoded molecule(7). It was confirmed that MICA does not associate with β2-microglobulin and it was observed that the putative peptide-binding groove is too narrow to accommodate a ligand, suggesting that MICA is not an antigen presenting molecule. EXPRESSION OF MICA MICA equivalent genes are present in different species but not in the mouse genome(1, 8). However, two putative orthologous genes to MICA and MICB have been described in the mouse genome(9). Like the other MHC class I genes, MICA is codominantly expressed(10). MICA transcripts were first detected in human epithelial and fibroblast cell lines(1). When antibodies (Ab) against MICA became available, it was demonstrated that MICA was expressed by human epithelial and fibroblast cell lines(4, 5, 11), freshly isolated human endothelial cells, and fibroblasts(12), tumors of different histotypes(13), some melanomas and T 26 VOL. 25 NUM. 1/ 2006 Figure 1. Map of the human MHC class I region showing the location of the MIC genes. Classical human MHC class I genes (HLA-A, -B and -C) are indicated as gray boxes, non-classical MHC class I genes (HLA-E, -F and -G) are indicated as hatched boxes, the MIC gene family members are indicated as white boxes, and the TNF gene is indicated as a black box. y is used to indicate the pseudogenes of the MIC gene family. cell leukemia cell lines(14), in thymic medulla(15), and in gastrointestinal epithelium(4). Expression of MICA was also observed in human keratinocytes (5), which showed no expression of this molecule on the cell surface(12, 16). The detection of MICA in tumors suggested that its expression might be related to the process of neotransformation. MICA is not expressed by resting T or B lymphocytes, but PHA-activated CD4+ and CD8+ T cell blasts express MICA(5). This expression could also be triggered by stimulation with allogeneic peripheral blood mononuclear cells (PBMCs), and involves TCR/CD3 engagement and costimulation through CD28(17), involving different cytoplasmic mediators(18) and NF-κB (19). These results suggest that MICA can be induced not only upon neotransformation, but also during cell activation, two cellular processes coincidentally regulated by NF-κB(20-23). However, low surface expression of MICA was observed on activated T lymphocytes(17). RECOGNITION OF MICA BY NKG2D After the description that MICA is expressed at the cell surface(4), research was focused on the identification of its putative receptor. Initially, it was observed that Vδ1 γδ T lymphocyte cell lines established from tumor infiltrating lymphocytes present in tumors of patients with adenocarcinomas recognize MICA-transfected cells or MICA-expressing tumor targets, triggering a cytotoxic response that could be blocked by anti-MICA or anti-γδ TCR monoclonal Abs (mAbs)(11). However, it was later demonstrated that the actual receptor for MICA is another cell surface molecule that belongs to the C-type lectin family of receptors named NKG2D(24). Since soluble MICA tetramers can bind to various Vδ1 γδTCRs expressed on transfected cells(25), it appears that MICA can be engaged by the Vδ1 Inmunol 25/1 10/5/06 17:15 Página 27 INMUNOLOGÍA γδTCR and by NKG2D. This dual recognition may provide a fine-tuning to protect the intestinal mucosa from abnormal activation of Vδ1 γδTCR T cells. NKG2D is mainly expressed by all human NK cells, δγ T lymphocytes, and αβ CD8+ T lymphocytes, being a type II cell surface glycoprotein with a Mr of ~42 kDa that displays minor homology with other members of the NKG2 family of receptors. NKG2D is expressed at the cell surface as a homodimer associated with an adaptor protein called DAP10(26), which is necessary to elicit the activation of a specific signal transduction cascade upon engagement of MICA(27-30). The crystal structure of the MICA-NKG2D complex has revealed that NKG2D binds as a homodimer to one molecule of MICA(31). One of the NKG2D molecules binds mostly to the α1 domain of MICA, while the other NKG2D molecule binds mostly to the α2 domain of MICA. The NKG2D homodimer overlays MICA diagonally in a similar way as the αβTCR overlays the MHC class I molecules. The central section of the α2 domain of MICA (residues 152-161), disordered in the crystal structure of isolated MICA(7), is ordered when bound to NKG2D and takes part of the interface between these 2 molecules. It is likely that this induced fit is promoted by NKG2D. Moreover, the hypothetical binding pocket of MICA remained free of any ligand, confirming that MICA is not an antigen-presenting molecule. The half-life for the MICA-NKG2D complex indicates that it is more stable than the complexes formed by the TCR and the MHC class I molecules. Although it is not our intention to provide a detailed description of NKG2D since excellent reviews have been published(28, 32-39), we want to mention that humans and mice have NKG2D and that this receptor is promiscuous in terms of ligand recognition. Human NKG2D ligands (NKG2DLs) are MICA and MICB (40) , and a group of glycosylphosphatidylinositol (GPI)-bound surface molecules called UL16 binding protein (ULBP)-1, -2, -3(41) and –4(42). Mice, which lack the whole MIC gene family, have the retinoic acid early inducible gene (Rae)-1β (a GPI-anchored, cell surface glycoprotein), the minor histocompatibility antigen H60 (an integral transmembrane protein), and the murine UL16-binding protein-like transcript 1 (MULT-1)(43) as NKG2DLs. All exhibit low sequence homology with their human counterparts(44) although human NKG2D binds mouse NKG2DLs(40) and mouse NKG2D can recognize some human NKG2DLs (45), most likely reflecting a selective advantage of preserving the NKG2D receptor in both species regardless of the recognized ligand. The MICA-NKG2D system is a versatile ligand-receptor pair since NKG2D can act as primary receptor or costimulatory N. WALTER ZWIRNER ET AL. molecule during anti-tumor immune responses(11,14,25,45,46), infection(47, 48) or autoimmunity(49, 50). How this dual function is achieved and regulated is still an open question. In mice, alternative splicing of NKG2D mRNA leads to two distinct polypeptides that associate differentially with the DAP10 or DAP12 adaptor proteins and determines whether NKG2D functions as costimulatory molecule for CD8+ T lymphocytes or as primary recognition receptor for NK cells(51). However, these alternative splicing variants and differential association with DAP10 or DAP12 has not been observed for human NKG2D. POLYMORPHISM OF MICA AND ALLELE FREQUENCY More than 50 alleles of MICA have been described (an updated list of them can be found at www.anthonynolan. org.uk/HIG) and linkage disequilibria between alleles of the MICA locus and of the HLA-B and HLA-C loci was found(52-54). Polymorphic regions in the MICA gene are clustered along exons 2 to 5. Polymorphisms in exons 2 to 4 are nucleotide substitutions that encode for amino acid substitutions in the α1, α2 and α3 domains. Conversely, the polymorphism in exon 5 consists of a different number of GCT repeats that encode for 4 to 10 Ala residues in the transmembrane domain. MICA*008 is the most common allele in North American Caucasoids (allele frequencies higher than 50%(55, 56)) and the hallmark of this allele is that, together with MICA*023 and MICA*028, it has an insertion that generates a premature stop codon in exon 5 which makes the transmembrane domain shorter, and also lacks the cytoplasmic tail. Besides, the encoded protein is efficiently expressed at the cell surface(4, 5), where it can engage NKG2D. Alleles that have this mutation are aberrantly sorted into polarized cells(57), which may limit the recognition by NK and γδ T cells during immunosurveillance in the intestinal epithelium against infections or neotransformation. Considering that NKG2D is monomorphic, it is puzzling why MICA is highly polymorphic. Different MICA alleles vary in their affinity for NKG2D(40) and these variations may affect the thresholds of recognition by NK cells and T lymphocytes. However, there are still no evidences about the relevance of these affinity differences during cell-cell interactions, especially considering that most of the polymorphic residues of MICA do not take part of the regions involved in the contact with NKG2D. Interestingly, it has been published that MICA expression is modulated differentially in cells infected with cytomegalovirus (CMV), depending on the MICA allele of the target cell(58). Cells with 27 Inmunol 25/1 10/5/06 17:15 Página 28 IMMUNOBIOLOGY OF THE HUMAN MHC CLASS I CHAIN-RELATED GENE A (MICA) ... VOL. 25 NUM. 1/ 2006 the truncated MICA*008 protein maintain MICA expression at the cell surface, while cells that express other full length MICA proteins are induced to down-regulate MICA expression upon CMV infection. Therefore, MICA*008 may promote the cytolysis of CMV-infected cells and confer resistance to CMV infection, explaining why this truncated protein is the most frequent in the population. MICA IN ORGAN TRANSPLANTATION Due to its polymorphic nature, it was assumed that MICA could be a novel transplantation antigen or alloantigen. Anti-MICA specific Ab were detected in sera of transplant recipients with different types of rejection episodes(59), these Ab were absent before the transplant, and they were effectors of complement mediated cytotoxicity(60). This suggests that anti-MICA Ab may play a role in solid organ transplantation outcome most likely by binding to the endothelial cells of the graft and inducing cell destruction, vascular injury and organ loss (Fig. 2). Although more work is necessary to analyze the relevance of these alloantibodies in the rejection process, their presence correlated with the development of acute rejection(61). Also, they were are able to bind to kidney microvascular endothelial cells and to MICA-transfected cells, fix complement and lyse such target cells and induce a thrombotic phenotype in endothelial cells. In some cases, these alloantibodies developed in the absence of anti-MHC alloantibodies suggesting that anti-MICA alloantibodies alone may induce rejection. In addition, renal and pancreatic allografts with acute or chronic rejection express MICA (62). Since ischemiareperfusion injury induced to a solid organ induces a stress response in the graft that is associated with the hypoxia and activation of immune response genes(63, 64), some cytokines and other proinflammatory mediators induced by the ischemia-reperfusion may also up-regulate the expression of MICA on the cell surface of endothelial and stromal cells of the grafted organ. Although this circuit of ischemiareperfusion injury - proinflammatory cytokines - MICA expression may trigger graft rejection, studies to establish the relationship and timing of MICA expression, cellular infiltration and rejection are necessary to establish the actual role of MICA during the graft rejection. Also, it is likely that clinical testing for the presence of anti-MICA alloantibodies might be implemented to avoid early rejections. However, the problem would be the source of the cells to be used in such testing since PBMCs, regularly used for standard cross-matches for anti-HLA antibodies(65), do not express MICA(5). Simultaneously, molecular typing strategies to genotype MICA (3, 52-55, 66-76) may avoid the 28 Figure 2. Proposed effects of anti-MICA alloantibodies during solid organ transplantation. The alloantibodies bind to the endothelial cells of the graft and trigger effector mechanisms like activation of the complement cascade, Abdependent cellular cytotoxicity mediated by FcRγ expressing cells (ADCC) and direct toxic effect like induction of thrombosis. The destruction of the endothelium (vascular injury) in turn promotes the graft disfunction and organ rejection. transplantation of MICA-mismatched grafts and lead to a better graft survival. Finally, nothing is currently known about the possible role of MICA (and MICB) in bone marrow transplantation outcome. MICA AND INFECTION Up-regulated MICA expression has been observed in fibroblasts and endothelial cells upon in vitro infection with CMV and in vivo in patients with CMV interstitial pneumonia(48, 58), which sensitizes to NKG2D-dependent cytolysis and IFN-γ secretion by NK cells and CD8+ CD28– αβ T lymphocytes. Consequently, CMV-driven MICA up-regulation and NKG2Dmediated cytotoxicity of T and NK cells may contribute to Inmunol 25/1 10/5/06 INMUNOLOGÍA 17:15 Página 29 N. WALTER ZWIRNER ET AL. Figure 3. Regulated expression of MICA in different situations. Normal cells of different types usually do not express MICA (or express very low levels) but express MHC class I molecules (center of the figure). Different situations can lead to up-regulation of MICA expression. A) In vitro, it was observed that heat shock induces MICA on colon adenocarcinoma cells, which triggers a cytotoxic response and IFN-γ secretion by intestinal γδTCR T lymphocytes, contributing to the lysis of the MICA-expressing cells and to the restoration of the homeostasis of the epithelium. B) During viral infections (CMV), fibroblasts and endothelial cells up-regulate MICA expression and promote a cytotoxic response mediated by αβTCR CD28–CD8+NKG2D+ T lymphocytes; during Mycobacterium tuberculosis infection, MICA expression is induced on epithelial and dendritic cells, triggering a cytotoxic response mediated by Vγ2Vδ2 T lymphocytes. In both cases, infected cells are eliminated and MICA expression contributes to the immunity against these pathogens. C) Activation-induced expression of MICA was also observed in CD4+ and CD8+ T lymphocytes but this expression remained intracellular. Therefore, the functional consequences of MICA expression in activated T lymphocytes remain unknown. D) MICA expression is also induced by neotransformation, and tumors that express MICA can be eliminated by NKG2D-expressing cells like NK cells and CD8+ T lymphocytes, contributing to the immunosurveillance. E) In opposition to these beneficial effects, aberrant expression of MICA was also observed in enterocytes of the intestinal mucosa of patients with celiac disease, in which IL-15 appears to play an important role. Recognition of MICAexpressing cells by intestinal cytotoxic NKG2D+ lymphocytes appears to contribute to the tissue injury and villous atrophy. Also, synoviocytes of patients with rheumatoid arthritis aberrantly express MICA. This allows the recognition by CD4+ T lymphocytes that ectopically express NKG2D, most likely induced by IL15 and TNF-α. This recognition leads to the cytotoxicity against the synoviocytes and IFN-γ secretion that contributes to the immunopathology of the joint disease. 29 Inmunol 25/1 10/5/06 17:15 Página 30 IMMUNOBIOLOGY OF THE HUMAN MHC CLASS I CHAIN-RELATED GENE A (MICA) ... the immunological control of persistent viral infections, especially considering that MICA appears to be refractory to the CMV-driven immune escape mechanism that induces intracellular retention of MICB(77-79). However, other authors reported that MICA is actually down-regulated upon CMV infection unless the target cell expresses a truncated allele protein like MICA*008 that lacks the whole cytoplasmic tail of the protein(58). During Hepatitis C virus (HCV) infection, dendritic cells (DCs) from infected patients were unable to specifically upregulate MICA upon stimulation with IFN-α(80) but did upregulate MICA in response to IL-15(81). This effect contributed to a poor DC-NK cell cross-talk, and resulted in a dampened NK cell activation, IFN-γ secretion and cytotoxicity, contributing to the persistence of HCV infection. Regarding bacterial infections, infection of epithelial cell lines and DCs with M. tuberculosis induced up-regulated expression of MICA and elicited a cytotoxic response and IFN-γ secretion by Vδ2 γδ T lymphocytes(47). Although the relevance of this effect in vivo is hard to assess, in one patient it was observed that MICA expression was detected on DClike cells from a lymph node. Also, epithelial cell lines infected with Escherichia coli of the diarrheagenic group but not with other enteroinvasive bacteria, up-regulated MICA on the cell surface and triggered cytotoxicity and IFN-γ release by the NKL cell line(82). Hence, MICA is a molecule also involved in the anti-bacterial immune response. Accordingly, MICA expression is induced by infectionderived stress or danger signals, triggering a response by NKG2D-expressing lymphoid cells that leads to the cytolysis of the infected cells and secretion of IFN-γ. This contributes to the generation of a pro-inflammatory environment, promotes the elimination of infected cells, and contributes to the resolution of the infection and restoration of the homeostasis (Fig. 3). MICA AND INFLAMMATORY DISEASES Unlike MHC class I promoters, the MICA gene lacks the IFN-γ responsive element(1) and indeed, IFN-γ does not regulate the expression of MICA(5). However, IL-15(49,50,81,83,84) and IFN-α(80) up-regulate MICA expression. We observed up-regulated expression of MICA mRNA in skin biopsies of patients with seborrhoeic dermatitis that was accompanied by high levels of mRNA for different proinflammatory cytokines even in biopsies from areas of the skin without clinically visible lesions(85), suggesting the existence of an ongoing inflammation that predisposes healthy skin to develop overt disease. Although we ignore if the elevated MICA expression was caused directly by these 30 VOL. 25 NUM. 1/ 2006 proinflammatory cytokines, these results demonstrate that some inflammatory conditions are accompanied by upregulated MICA expression in vivo, which may contribute to the development of tissue injury and the immunopathology of different diseases. Anomalous MICA expression was also observed on synoviocytes from patients with rheumatoid arthritis(49). Recognition by NKG2D ectopically induced by TNF-α and IL-15 on CD4+CD28– T lymphocytes induced the proliferation of auto-aggressive NKG2D+CD4+CD28– T lymphocytes, and TNF-α and IFN-γ release, contributing to the immunopathology of the disease. Although the stimuli that induced MICA on synoviocytes remain unknown, it could be caused by the proinflammatory environment of the joints. Patients with active celiac disease with villous atrophy showed strong MICA expression at the surface of cells from the surface to the bottom of the crypts(50). MICA was also expressed in villous epithelial cells of the gut in normal or disease-free individuals, but this staining was mostly intracellular. IL-15, which is over-expressed in the intestine of patients with celiac disease(86-88), appears to be involved in this up-regulated expression of MICA and contributed to the cytotoxicity of NKG2D+ intraepithelial lymphocytes (IELs). These cells lysed epithelial target cell lines in a NKG2D-dependent way(50, 89), contributing to the villous atrophy. Conversely, an anti-inflammatory environment may contribute to the silencing of the expression of MICA. Accordingly, suppressing TGF-β production by human gliomas induced an up-regulation of MICA expression at the cell surface of the tumors(90). Therefore, the MICA gene appears to be turned-on in certain pro-inflammatory environments depending on the cell type and surrounding cytokines. In some instances, this expression may be beneficial (clearance of infected cells) but in other cases (autoimmune diseases) it may be detrimental for the host. However, the cytokines and pro- and antiinflammatory mediators that regulate MICA expression need to be further explored in order to be clinically exploited (Fig. 3). MICA, DCs, NK CELLS AND T LYMPHOCYTES Dendritic cells are sentinels of the immune system that regulate the development of the innate and adaptative immune response(91). Immature DCs do not express MICA, but IFN-α and IL-15, while promoting DC maturation, induce surface expression of MICA(80, 81). Therefore, these cytokines may participate in the cross-talk of these mature DCs with NKG2D-expressing cells. Cross talk between NK cells and Inmunol 25/1 10/5/06 17:15 Página 31 INMUNOLOGÍA DCs is an important step during the orchestration of the immune response(92-98). NK cells interact with DCs at sites of ongoing inflammatory reactions caused by invading pathogens and in secondary lymphoid organs(98-100), resulting in cellular activation and development of effector functions. The NK cell activating receptor NKp30 has been involved in this cross-talk, but the participation of NKG2D and recognition of MICA on mature DCs could not be demonstrated(101, 102). Most studies about the MICA-NKG2D system have been performed with NK cells, which constitute a key component of the innate immune system through their ability to lyse tumor or virus-infected target cells and provide an early source of immunoregulatory cytokines. Two populations of human NK cells have been identified. The major population (about 90%) is cytotoxic and shows a CD56dimCD16+ phenotype, whereas the remaining 10% of the NK cells are a source of immunoregulatory cytokines and present a CD56brightCD16dim or CD56brightCD16– phenotype(103, 104). Although NKG2D expression seems to be slightly higher in CD56dim than in CD56bright NK cells, these differences were not responsible for the differential IFN-γ production and proliferation of these NK cell subsets upon interaction with DCs matured with LPS(97). In addition, it remains unknown if engagement of NKG2D by MICA or other NKG2DLs on these cell subsets differentially affects their activation and effector functions, especially considering that CD56dim NK cells predominate in peripheral blood, while CD56bright NK cells constitute the major population of NK cells in secondary lymphoid organs(99,100,105), interact with DCs and shape the adaptative immune response(92,93,95,98,103,106-109). We have demonstrated that expression of MICA can be induced on CD4+ and CD8+ T lymphocytes upon activation but were unable to observe a strong surface expression(5, 17-19). Mostly, MICA remained inside the T cell, which may be a safeguard mechanism to protect activated T cells from early cytotoxicity by NK cells during a T cell-dependent immune response in an inflammatory environment, a virusinfected tissue or a tumor microenvironment, where NK and activated T cells are recruited and further stimulated with locally produced cytokines. Although activated T lymphocytes can be killed by NK cells(14, 110), it is possible that MICA needs an extra signal to become expressed on the cell surface on activated T cells, produced during the cross-talk of the activated T lymphocytes with other cell populations present in inflamed, virus-infected or neotransformed tissues. A cross-talk of activated CD4+ T cells and NK cells has been demonstrated recently(111) but such putative extra signal may also be provided by other cells present in such tissues. It is possible that activated T N. WALTER ZWIRNER ET AL. lymphocytes rapidly express MICA at high levels on the cell surface by mobilization from intracellular deposits. Recently, it was observed that MICA can be expressed at the cell surface on CD8+ T cells stimulated with anti-CD3 or anti-CD3 plus anti-NKG2D mAbs and cultured for 7 days in the presence of IL-2 or IL-7 plus IL-15(112), but the functional consequences of this surface expression remain to be elucidated. We believe that it is advantageous for an activated, effector T lymphocyte to keep MICA inside the cell, especially in stressed tissues where high concentrations of IL-15 secreted by dendritic cells and macrophages induce NKG2D upregulation and cytotoxicity of NK cells against stressed target cells(50). However, once the termination phase of the immune response is reached due to antigen exhaustion, activated T lymphocytes need to be cleared from the body and surface expression of MICA may contribute to the elimination of these activated T lymphocytes by NKG2D+ NK cells. The elucidation of the timing of in vivo surface expression of MICA on T lymphocytes in stressed tissues will reveal potential strategies to modulate NKG2D-mediated cytotoxicity mediated by NK cells against activated T lymphocytes in pathological situations. MICA IN TUMOR IMMUNOLOGY Neotransformation is a multi-step process that involves the accumulation of mutations and a genetic instability that result in the loss of cell cycle control and the selection of tumor variants. A novel interpretation of the tumor-host relationship has lead to the concept of the «cancer immunoediting»(113, 114). Others propose that tumors simply generate tumor escape phenotypes during their continuous growth in the presence of a functional immune system that imposes an immunological pressure (115). Besides, it is undisputed that tumors express or up-regulate molecules that are targets of cytotoxic response mediated by NK and CD8 T cells, and that an appropriate targeting of the immune response against such molecules is a crucial event in antitumor immunity. MICA expression has been observed in different epithelial and non-epithelial tumor cell lines and freshly isolated tumors of different histotypes like lung, breast, kidney, ovary, prostate, colon carcinomas, melanomas and acute myeloid leukemias, some T-cell acute lymphoblastic leukemias and multiple myeloma cells(4,5,11,13,14,45,46,116-126). Neo-expression of MICA appears to be related to the activation of the DNA damage pathway(127), although the study of the transcription factors involved in MICA gene expression is an open field that merits further exploration. Only a few reports about transcription factors that regulate MICA expression have 31 Inmunol 25/1 10/5/06 17:15 Página 32 IMMUNOBIOLOGY OF THE HUMAN MHC CLASS I CHAIN-RELATED GENE A (MICA) ... been published(19, 128). The knowledge of these pathways may reveal potential targets for immune intervention to induce efficient cytotoxic anti-tumor immune responses. Expression of MICA on different tumors promotes cytolysis and IFN-γ secretion by lymphoid NKG2D-expressing cells (4,11,14,24,28,30,39,40,45,46,119,121,129-134). NKG2D may act as a costimulatory molecule or as a primary receptor involved in target cell recognition. Therefore, it emerges as the major receptor involved in NK cell mediated lysis of epithelial and non-epithelial tumors. However, the cytotoxic potential of the MICA-NKG2D system is counterbalanced by the interaction of classical and non-classical MHC class I molecules of the tumor cells through interaction with KIR or other inhibitory receptors expressed by the NK cells(46). Despite this overwhelming in vitro evidence, in vivo evidences about the role of MICA in tumor growth control and clinical correlations with tumor aggressiveness are not so abundant. In melanomas, intensity of MICA expression did not correlate with the Breslow thickness or with the metastatic capacity(116). In colorectal cancer patients, it was observed that there is no correlation between clinicopathological parameters and intensity of MICA expression(135), although patient survival correlated with levels of MICA expression. Another study reported that invasive rectal tumors upregulate MICA whereas their levels of expression (mRNA levels) were lower in early tumors(123). Also, higher levels of MICA were found on tumor cells of patients with monoclonal gammopathy of unknown significance, compared to multiple myeloma cells, indicating that MICA expression is higher in some pre-neoplastic conditions than on cells of advanced stage tumors(136). Conversely, results obtained in our lab showed that benign melanomas (nevus) do not express MICA but that malign melanoma metastases express this NKG2DL (Fuertes M.B., unpublished results), which is in line with previous findings demonstrating MICA expression by malign melanomas of different degrees(116). Although these results may look puzzling, they should be interpreted in light of recent findings demonstrating that sustained expression of MICA or other NKG2DLs by tumors can elicit NKG2D down-regulation leading to a defect in NK cellmediated cytotoxicity(118, 122, 130, 137-144). These findings also conciliate puzzling results showing that MICA and other NKG2DLs are usually expressed on the surface of many tumors in immunocompetent hosts, despite the presence of cytotoxic NKG2D-expressing cells. Such down-regulation of NKG2D is reversible but imposes a functional impairment to the immunosurveillance exerted by NK cells and γδ and αβ CD8+ T lymphocytes(118,126,133,139,142). Surface downregulation of NKG2D is induced by soluble MICA (sMICA), which in turn derives from metalloprotease-mediated 32 VOL. 25 NUM. 1/ 2006 Figure 4. MICA in tumor immune escape. Most tumors induce surface expression of MICA as consequence of the neotransformation process. However, through the secretion of TGF-β they promote down-regulation of MICA from the cell surface, and through the secretion of tissue metalloproteases (MMPs), tumors shed soluble MICA (sMICA). Both, TGF-β and sMICA promote down-regulation of NKG2D from the cell surface of NK cell and CD8+ T lymphocytes. This leads to a deficient recognition of the tumor cells (cytotoxic effector cells become «blind» to MICA-expressing tumors) leading to a poor cytotoxic response and IFN-γ secretion, and promoting the tumor immune escape. proteolytic shedding from the tumor cell surface. Metalloproteases are usually involved in tumor progression and angiogenesis(145, 146), and they appear to be also involved in MICA cleavage. The presence of sMICA in serum of breast, lung, ovarian and colon cancer and melanoma patients impaired not only the cytotoxic response of the NKG2Dexpressing cells, but also their capacity to secrete IFNγ(139). Hence, the shedding of sMICA by tumors constitutes a novel tumor immune escape mechanism that makes the cytotoxic cells «blind» to the presence of MICA on the tumor cells and that explains the low levels of surface MICA on highly aggressive, end-stage human tumors (Fig. 4). Additional tumor immune escape mechanisms that affect the functionality of the NKG2D system also exist. Tumorderived TGF-β induces the down-regulation of NKG2D from the NK cell surface, leading to an impairment of the anti-tumor cytotoxic response(90, 147). Therefore, tumor immune escape is a complex process that goes beyond the known Inmunol 25/1 10/5/06 17:15 Página 33 INMUNOLOGÍA capabilities of TGF-β(148, 149), galectin-1(150), FasL(151), and NCRdependent tumor-induced apoptosis of NK cells(152), and also compromises optimal interaction of the MICA-NKG2D system. Indeed, we recently described a novel tumor immune escape mechanism that relays on an intracellular retention of MICA in some melanomas that confers resistance to NK cell-mediated cytotoxicity (Fuertes M.B., submitted). It is likely that different tumors utilize these mechanisms to differentially subvert the immune system in order to survive in immunocompetent hosts. From a therapeutic point of view, interest has been centered into the possibilities of up-regulating the expression of NKG2DLs on tumor cells to boost their susceptibility to cytotoxic cells. Over-expression of Rae1 and H60 (mouse NKG2DLs) induced an efficient anti-tumor immune response in vivo(153, 154) and the anti-tumor effects mediated through NKG2D could be further enhanced by administration of IL21 (155). Over-expression of MICA on gliomas(45) or lung carcinomas(156) enhanced their sensitivity to NK cell- and T cell-mediated cytotoxicity in vitro and delayed the tumor growth in vivo in xenografted mice. However, in light of the described tumor immune escape mechanisms that compromise the MICA-NKG2D system, further research is necessary to fully understand the actual importance of such tumor immune escape mechanisms in vivo and how to overcome them before translating these gene therapy strategies to the treatment of cancer patients. In this regard, we observed that overexpression of MICA on melanomas that retain this molecule inside the cell not only restored its surface expression but also conferred susceptibility to NK cell-mediated cytotoxicity and induced a delayed in vivo growth in a xenogeneic model (Fuertes M.B., submitted), suggesting that at least some of the tumor immune escape mechanisms that compromise optimal signaling of the MICA-NKG2D system can be overcome by ectopic gene transfer immunotherapies. Therefore, novel immunotherapies based on the overexpression of MICA may reinforce the weakened anti-tumor immune response in a tumor-bearing patient and overcome some tumor immune escape mechanisms. Concluding remarks In only 12 years since the MICA gene was described, substantial progress has been made in the comprehension of its immunobiology and how this molecule participates in the fine-tuning of the innate and adaptive immune response. MICA has been shown to play a role in very different aspects of the immune response like transplant rejection, immune response against viruses and intracellular bacteria, inflammation, homeostasis of epithelia, and immune response against tumors. The biological function of MICA is achieved through N. WALTER ZWIRNER ET AL. interaction with the NKG2D receptor. According to the experimental evidence, we believe that MICA should be considered more as a cell homeostasis sensor than a cell stress sensor, whose up-regulated expression is induced not only by cell distress but also by strong proliferation and proinflammatory stimuli that disrupt the cellular homeostasis and elicits a cytotoxicity that eliminates altered cells, contributing to the restoration of the normal homeostasis. Moreover, MICA also participates in tumor immune escape mechanisms. However, there are many open issues that need to be further investigated. The development and implementation of typing strategies of MICA alleles for better matching in solid organ transplantation may improve their outcome. The role of MICA in bone marrow transplantation should be investigated, as well as its role in other autoimmune diseases. The pharmacologic modulation of MICA expression may favor the development of more effective immune responses against viral or bacterial infections, or may reduce the tissue injury observed in many autoimmune diseases. Thus, research focused on the development of compounds that affect the expression of MICA is an important forthcoming issue. To investigate the transcription factors that control MICA gene expression and design rational immuno or gene therapies that modulate MICA expression is also important to promote more effective immune responses against tumors and to overcome the tumor immune escape mechanisms that involve the MICA-NKG2D system. Such research areas will provide novel approaches to improve human health. ACKNOWLEDGMENTS We apologize to the authors of many relevant references not cited because of space limitations. We would like to thank Dr. Gabriel Rabinovich for his friendship and support, and for providing an outstading working environment. We also thank CONICET, ANPCYT, UBA and Fundación Antorchas for providing the grants with which the experiments were performed. N.W.Z. is a member of the Researcher Career of CONICET. M.B.F., M.V.G. and C.I.D. are postgraduate fellows of CONICET. L.E.R. holds a fellowship of the ANPCYT. CORRESPONDENCE TO: Norberto W. Zwirner, Ph.D. Laboratorio de Inmunogenética Hospital de Clínicas «José de San Martín» Av. Córdoba 2351, 3er piso. C1120AAF Buenos Aires, Argentina. Phone: 54-11-5950-8755/8756/8757. Fax: 54-11-5950-8758 E-mail: [email protected] 33 Inmunol 25/1 10/5/06 17:15 Página 34 IMMUNOBIOLOGY OF THE HUMAN MHC CLASS I CHAIN-RELATED GENE A (MICA) ... REFERENCES 1. Bahram S, Bresnahan M, Geraghty DE, Spies T. A second lineage of mammalian major histocompatibility complex class I genes. Proc Natl Acad Sci USA 1994;91:6259-6263. 2. Bahram S, Spies T. The MIC gene family. Res Immunol 1996;147:328333. 3. Leelayuwat C, Townend DC, Degli-Esposti MA, Abraham LJ, Dawkins RL. A new polymorphic and multicopy MHC gene family related to nonmammalian class I. Immunogenetics 1994;40:339351. 4. Groh V, Bahram S, Bauer S, Herman A, Beauchamp M, Spies T. Cell stress-regulated human major histocompatibility complex class I gene expressed in gastrointestinal epithelium. Proc Natl Acad Sci USA 1996;93:12445-12450. 5. Zwirner NW, Fernández-Viña MA, Stastny P. MICA, a new polymorphic HLA-related antigen, is expressed mainly by keratinocytes, endothelial cells, and monocytes. Immunogenetics 1997;47:139-148. 6. Zou Y, Stastny P. Alternatively spliced forms of MICA and MICB lacking exon 3 in a human cell line and evidence of presence of similar RNA in human peripheral blood mononuclear cells. Immunogenetics 2002;54:671-674. 7. Li P, Willie ST, Bauer S, Morris DL, Spies T, Strong RK. Crystal structure of the MHC class I homolog MIC-A, a gammadelta T cell ligand. Immunity 1999;10:577-584. 8. Steinle A, Groh V, Spies T. Diversification, expression, and gamma delta T cell recognition of evolutionarily distant members of the MIC family of major histocompatibility complex class I-related molecules. Proc Natl Acad Sci USA 1998;95:12510-12515. 9. Kasahara M, Watanabe Y, Sumasu M, Nagata T. A family of MHC class I-like genes located in the vicinity of the mouse leukocyte receptor complex. Proc Natl Acad Sci USA 2002;99:13687-13692. 10. Molinero LL, Marcos CY, Mirbaha F, Fainboim L, Stastny P, Zwirner NW. Codominant expression of the polymorphic MICA alloantigens encoded by genes in the HLA region. Eur J Immunogenet 2002;29:315319. 11. Groh V, Steinle A, Bauer S, Spies T. Recognition of stress-induced MHC molecules by intestinal epithelial gammadelta T cells. Science 1998;279:1737-1740. 12. Zwirner NW, Dole K, Stastny P. Differential surface expression of MICA by endothelial cells, fibroblasts, keratinocytes, and monocytes. Hum Immunol 1999;60:323-330. 13. Groh V, Rhinehart R, Secrist H, Bauer S, Grabstein KH, Spies T. Broad tumor-associated expression and recognition by tumorderived gamma delta T cells of MICA and MICB. Proc Natl Acad Sci USA 1999;96:6879-6884. 14. Pende D, Cantoni C, Rivera P, Vitale M, Castriconi R, Marcenaro S, et al. Role of NKG2D in tumor cell lysis mediated by human NK cells: cooperation with natural cytotoxicity receptors and capability of recognizing tumors of nonepithelial origin. Eur J Immunol 2001;31:1076-1086. 15. Hue S, Monteiro RC, Berrih-Aknin S, Caillat-Zucman S. Potential role of NKG2D/MHC class I-related chain A interaction in intrathymic maturation of single-positive CD8 T cells. J Immunol 2003;171:1909-1917. 16. Tay GK, Hui J, Gaudieri S, Schmitt-Egenolf M, Martinez OP, Leelayuwat C, et al. PERB11 (MIC): a polymorphic MHC gene is 34 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. VOL. 25 NUM. 1/ 2006 expressed in skin and single nucleotide polymorphisms are associated with psoriasis. Clin Exp Immunol 2000;119:553-558. Molinero LL, Fuertes MB, Rabinovich GA, Fainboim L, Zwirner NW. Activation-induced expression of MICA on T lymphocytes involves engagement of CD3 and CD28. J Leukoc Biol 2002;71:791797. Molinero LL, Fuertes MB, Fainboim L, Rabinovich GA, Zwirner NW. Up-regulated expression of MICA on activated T lymphocytes involves Lck and Fyn kinases and signaling through MEK1/ERK, p38 MAP kinase, and calcineurin. J Leukoc Biol 2003;73:815-822. Molinero LL, Fuertes MB, Girart MV, Fainboim L, Rabinovich GA, Costas MA, Zwirner NW. NF-kB Regulates Expression of the MHC Class I-Related Chain A Gene in Activated T Lymphocytes. J Immunol 2004;173:5583-5590. Ballard DW. Molecular mechanisms in lymphocyte activation and growth. Immunol Res 2001;23:157-166. Kuo CT, Leiden JM. Transcriptional regulation of T lymphocyte development and function. Annu Rev Immunol 1999;17:149-187. Karin M, Greten FR. NF-kB: linking inflammation and immunity to cancer development and progression. Nat Rev Immunol 2005;5:749759. Karin M, Cao Y, Greten FR, Li ZW. NF-kB in cancer: from innocent bystander to major culprit. Nat Rev Cancer 2002;2:301-310. Bauer S, Groh V, Wu J, Steinle A, Phillips JH, Lanier LL, Spies T. Activation of NK cells and T cells by NKG2D, a receptor for stressinducible MICA. Science 1999;285:727-729. Wu J, Groh V, Spies T. T cell antigen receptor engagement and specificity in the recognition of stress-inducible MHC class Irelated chains by human epithelial gamma delta T cells. J Immunol 2002;169:1236-1240. Wu J, Song Y, Bakker AB, Bauer S, Spies T, Lanier LL, Phillips JH. An activating immunoreceptor complex formed by NKG2D and DAP10. Science 1999;285:730-732. Vivier E, Nunes JA, Vely F. Natural killer cell signaling pathways. Science 2004;306:1517-1519. Vivier E, Tomasello E, Paul P. Lymphocyte activation via NKG2D: towards a new paradigm in immune recognition? Curr Opin Immunol 2002;14:306-311. Andre P, Castriconi R, Espeli M, Anfossi N, Juarez T, Hue S, et al. Comparative analysis of human NK cell activation induced by NKG2D and natural cytotoxicity receptors. Eur J Immunol 2004;34:961-971. Billadeau DD, Upshaw JL, Schoon RA, Dick CJ, Leibson PJ. NKG2DDAP10 triggers human NK cell-mediated killing via a Sykindependent regulatory pathway. Nat Immunol 2003;4:557-564. Li P, Morris DL, Willcox BE, Steinle A, Spies T, Strong RK. Complex structure of the activating immunoreceptor NKG2D and its MHC class I-like ligand MICA. Nat Immunol 2001;2:443-451. Lanier LL. NKG2D in innate and adaptive immunity. Adv Exp Med Biol 2005;560:51-56. Strong RK, McFarland BJ. NKG2D and Related Immunoreceptors. Adv Protein Chem 2004;68:281-312. Moretta L, Moretta A. Unravelling natural killer cell function: triggering and inhibitory human NK receptors. EMBO J 2004;23:2559. Raulet DH. Roles of the NKG2D immunoreceptor and its ligands. Nat Rev Immunol 2003;3:781-790. Inmunol 25/1 10/5/06 17:15 Página 35 INMUNOLOGÍA 36. Cerwenka A, Lanier LL. NKG2D ligands: unconventional MHC class I-like molecules exploited by viruses and cancer. Tissue Antigens 2003;61:335-343. 37. Snyder MR, Weyand CM, Goronzy JJ. The double life of NK receptors: stimulation or co-stimulation? Trends Immunol 2004;25:2532. 38. Ogasawara K, Lanier LL. NKG2D in NK and T Cell-Mediated Immunity. J Clin Immunol 2005;25:534-540. 39. Moretta L, Bottino C, Pende D, Vitale M, Mingari MC, Moretta A. Different checkpoints in human NK-cell activation. Trends Immunol 2004;25:670-676. 40. Steinle A, Li P, Morris DL, Groh V, Lanier LL, Strong RK, Spies T. Interactions of human NKG2D with its ligands MICA, MICB, and homologs of the mouse RAE-1 protein family. Immunogenetics 2001;53:279-287. 41. Cosman D, Mullberg J, Sutherland CL, Chin W, Armitage R, Fanslow W, et al. ULBPs, novel MHC class I-related molecules, bind to CMV glycoprotein UL16 and stimulate NK cytotoxicity through the NKG2D receptor. Immunity 2001;14:123-133. 42. Chalupny JN, Sutherland CL, Lawrence WA, Rein-Weston A, Cosman D. ULBP4 is a novel ligand for human NKG2D. Biochem Biophys Res Commun 2003;305:129-135. 43. Carayannopoulos LN, Naidenko OV, Fremont DH, Yokoyama WM. Cutting edge: murine UL16-binding protein-like transcript 1: a newly described transcript encoding a high-affinity ligand for murine NKG2D. J Immunol 2002;169:4079-4083. 44. Diefenbach A, Jamieson AM, Liu SD, Shastri N, Raulet DH. Ligands for the murine NKG2D receptor: expression by tumor cells and activation of NK cells and macrophages. Nat Immunol 2000;1:119126. 45. Friese MA, Platten M, Lutz SZ, Naumann U, Aulwurm S, Bischof F, et al. MICA/NKG2D-mediated immunogene therapy of experimental gliomas. Cancer Res 2003;63:8996-9006. 46. Menier C, Riteau B, Carosella ED, Rouas-Freiss N. MICA triggering signal for NK cell tumor lysis is counteracted by HLA-G1-mediated inhibitory signal. Int J Cancer 2002;100:63-70. 47. Das H, Groh V, Kuijl C, Sugita M, Morita CT, Spies T, Bukowski JF. MICA engagement by human Vgamma2Vdelta2 T cells enhances their antigen-dependent effector function. Immunity 2001;15:8393. 48. Groh V, Rhinehart R, Randolph-Habecker J, Topp MS, Riddell SR, Spies T. Costimulation of CD8alphabeta T cells by NKG2D via engagement by MIC induced on virus-infected cells. Nat Immunol 2001;2:255-260. 49. Groh V, Bruhl A, El-Gabalawy H, Nelson JL, Spies T. Stimulation of T cell autoreactivity by anomalous expression of NKG2D and its MIC ligands in rheumatoid arthritis. Proc Natl Acad Sci USA 2003;100:9452-9457. 50. Hue S, Mention JJ, Monteiro RC, Zhang S, Cellier C, Schmitz J, et al. A direct role for NKG2D/MICA interaction in villous atrophy during celiac disease. Immunity 2004;21:367-377. 51. Diefenbach A, Tomasello E, Lucas M, Jamieson AM, Hsia JK, Vivier E, Raulet DH. Selective associations with signaling proteins determine stimulatory versus costimulatory activity of NKG2D. Nat Immunol 2002;3:1142-1149. 52. Stephens HA. MHC haplotypes, MICA genes and the 'wonderland' of NK receptor polymorphism. Trends Immunol 2002;23:385-6. N. WALTER ZWIRNER ET AL. 53. Stephens HA. MICA and MICB genes: can the enigma of their polymorphism be resolved? Trends Immunol 2001;22:378-385. 54. Collins RW. Human MHC class I chain related (MIC) genes: their biological function and relevance to disease and transplantation. Eur J Immunogenet 2004;31:105-14. 55. Petersdorf EW, Shuler KB, Longton GM, Spies T, Hansen JA. Population study of allelic diversity in the human MHC class Irelated MIC-A gene. Immunogenetics 1999;49:605-612. 56. Zhang Y, Lazaro AM, Lavingia B, Stastny P. Typing for all known MICA alleles by group-specific PCR and SSOP. Hum Immunol 2001;62:620-31. 57. Suemizu H, Radosavljevic M, Kimura M, Sadahiro S, Yoshimura S, Bahram S, Inoko H. A basolateral sorting motif in the MICA cytoplasmic tail. Proc Natl Acad Sci USA 2002;99:2971-2976. 58. Zou Y, Bresnahan W, Taylor RT, Stastny P. Effect of Human Cytomegalovirus on Expression of MHC Class I-Related Chains A. J Immunol 2005;174:3098-3104. 59. Zwirner NW, Marcos CY, Mirbaha F, Zou Y, Stastny P. Identification of MICA as a new polymorphic alloantigen recognized by antibodies in sera of organ transplant recipients. Hum Immunol 2000;61:917924. 60. Zou Y, Mirbaha F, Lázaro A, Zhang Y, Lavingia B, Stastny P. MICA is a target for complement-dependent cytotoxicity with mouse monoclonal antibodies and human alloantibodies. Hum Immunol 2002;63:30-39. 61. Sumitran-Holgersson S, Wilczek HE, Holgersson J, Soderstrom K. Identification of the nonclassical HLA molecules, mica, as targets for humoral immunity associated with irreversible rejection of kidney allografts. Transplantation 2002;74:268-277. 62. Hankey KG, Drachenberg CB, Papadimitriou JC, Klassen DK, Philosophe B, Bartlett ST, et al. MIC expression in renal and pancreatic allografts. Transplantation 2002;73:304-306. 63. Strehlau J, Pavlakis M, Lipman M, Shapiro M, Vasconcellos L, Harmon W, Strom TB. Quantitative detection of immune activation transcripts as a diagnostic tool in kidney transplantation. ProcNatl Acad Sci USA 1997;94:695-700. 64. Rauen U, de Groot H. New insights into the cellular and molecular mechanisms of cold storage injury. J Investig Med 2004;52:299-309. 65. Dyer PA, Middleton D. Histocompatibility testing: a practical approach. Oxford University Press, 1993. 66. Fodil N, Laloux L, Wanner V, Pellet P, Hauptmann G, Mizuki N, et al. Allelic repertoire of the human MHC class I MICA gene. Immunogenetics 1996;44:351-7. 67. Mendoza-Rincon J, Arguello JR, Perez-Rodriguez M, McWhinnie A, Marsh SG, Fischer G, Madrigal JA. Characterization of the MICA polymorphism by sequence-specific oligonucleotide probing. Immunogenetics 1999;49:471-8. 68. Romphruk AV, Naruse TK, Romphruk A, Kawata H, Puapairoj C, Kulski JK, et al. Diversity of MICA (PERB11.1) and HLA haplotypes in Northeastern Thais. Tissue Antigens 2001;58:83-9. 69. Ahmad T, Marshall SE, Mulcahy-Hawes K, Orchard T, Crawshaw J, Armuzzi A, et al. High resolution MIC genotyping: design and application to the investigation of inflammatory bowel disease susceptibility. Tissue Antigens 2002;60:164-79. 70. Collins RW, Stephens HA, Clare MA, Vaughan RW. High resolution molecular phototyping of MICA and MICB alleles using sequence specific primers. Hum Immunol 2002;63:783-94. 35 Inmunol 25/1 10/5/06 17:15 Página 36 IMMUNOBIOLOGY OF THE HUMAN MHC CLASS I CHAIN-RELATED GENE A (MICA) ... 71. Zhang Y, Lazaro AM, Zou Y, Lavingia B, Moraes EM, Moraes RJ, Stastny P. MICA polymorphism in South American Indians. Immunogenetics 2002;53:900-906. 72. Katsuyama Y, Ota M, Ando H, Saito S, Mizuki N, Kera J, et al. Sequencing based typing for genetic polymorphisms in exons, 2, 3 and 4 of the MICA gene. Tissue Antigens 1999;54:178-184. 73. Visser CJ, Tilanus MG, Tatari Z, van der Zwan AW, Bakker R, Rozemuller EH, et al. Sequencing-based typing of MICA reveals 33 alleles: a study on linkage with classical HLA genes. Immunogenetics 1999;49:561-566. 74. Zhang Y, Han M, Vorhaben R, Giang C, Lavingia B, Stastny P. Study of MICA alleles in 201 African Americans by multiplexed single nucleotide extension (MSNE) typing. Hum Immunol 2003;64:130-136. 75. Stephens HA, Vaughan RW, Collins R, Kondeatis E, Theron J, Payne A. Towards a molecular phototyping system for allelic variants of MICA, encoded by polymorphisms in exons 2, 3 and 4 of MHC class I chain-related genes. Tissue Antigens 1999;53:167174. 76. Zhang Y, Lázaro AM, Lavingia B, Stastny P. Typing for all known MICA alleles by group-specific PCR and SSOP. Hum Immunol 2001;62:620-631. 77. Dunn C, Chalupny NJ, Sutherland CL, Dosch S, Sivakumar PV, Johnson DC, Cosman D. Human cytomegalovirus glycoprotein UL16 causes intracellular sequestration of NKG2D ligands, protecting against natural killer cell cytotoxicity. J Exp Med 2003;197:14271439. 78. Wu J, Chalupny NJ, Manley TJ, Riddell SR, Cosman D, Spies T. Intracellular retention of the MHC class I-related chain B ligand of NKG2D by the human cytomegalovirus UL16 glycoprotein. J Immunol 2003;170:4196-4200. 79. Welte SA, Sinzger C, Lutz SZ, Singh-Jasuja H, Sampaio KL, Eknigk U, et al. Selective intracellular retention of virally induced NKG2D ligands by the human cytomegalovirus UL16 glycoprotein. Eur J Immunol 2003;33:194-203. 80. Jinushi M, Takehara T, Kanto T, Tatsumi T, Groh V, Spies T, et al. Critical role of MHC class I-related chain A and B expression on IFN-α-stimulated dendritic cells in NK cell activation: impairment in chronic hepatitis C virus infection. J Immunol 2003;170:12491256. 81. Jinushi M, Takehara T, Tatsumi T, Kanto T, Groh V, Spies T, et al. Autocrine/paracrine IL-15 that is required for type I IFN-mediated dendritic cell expression of MHC class I-related chain A and B is impaired in hepatitis C virus infection. J Immunol 2003;171:54235429. 82. Tieng V, Le Bouguenec C, du Merle L, Bertheau P, Desreumaux P, Janin A, et al. Binding of Escherichia coli adhesin AfaE to CD55 triggers cell-surface expression of the MHC class I-related molecule MICA. Proc Natl Acad Sci USA 2002;99:2977-2982. 83. Dann SM, Wang HC, Gambarin KJ, Actor JK, Robinson P, Lewis DE, et al. Interleukin-15 activates human natural killer cells to clear the intestinal protozoan cryptosporidium. J Infect Dis 2005;192:1294-1302. 84. Roberts AI, Lee L, Schwarz E, Groh V, Spies T, Ebert EC, Jabri B. NKG2D receptors induced by IL-15 costimulate CD28-negative effector CTL in the tissue microenvironment. J Immunol 2001;167:552730. 85. Molinero LL, Gruber M, Leoni J, Woscoff A, Zwirner NW. Up- 36 VOL. 25 NUM. 1/ 2006 regulated expression of MICA and proinflammatory cytokines in skin biopsies from patients with seborrhoeic dermatitis. Clin Immunol 2003;106:50-54. 86. Maiuri L, Ciacci C, Auricchio S, Brown V, Quaratino S, Londei M. Interleukin 15 mediates epithelial changes in celiac disease. Gastroenterology 2000;119:996-1006. 87. Mention J-J, Ben Ahmed M, BegueBègue B, Barbe U, Verkarre V, Asnafi V, et al. Interleukin 15: a key to disrupted intraepithelial lymphocyte homeostasis and lymphomagenesis in celiac disease. Gastroenterology 2003;125:730-745. 88. Di Sabatino A, Ciccocioppo R, Cupelli F, Cinque B, Millimaggi D, Clarkson MM, et al. Epithelium-derived interleukin-15 regulates intraepithelial lymphocyte Th1 cytokine production, cytotoxicity and survival in coeliac disease. Gut 2005:doi10.1136/gut.2005.068684. 89. Meresse B, Chen Z, Ciszewski C, Tretiakova M, Bhagat G, Krausz TN, et al. Coordinated induction by IL15 of a TCR-independent NKG2D signaling pathway converts CTL into lymphokine-activated killer cells in celiac disease. Immunity 2004;21:357-366. 90. Friese MA, Wischhusen J, Wick W, Weiler M, Eisele G, Steinle A, Weller M. RNA Interference Targeting Transforming Growth Factor-b Enhances NKG2D-Mediated Antiglioma Immune Response, Inhibits Glioma Cell Migration and Invasiveness, and Abrogates Tumorigenicity In vivo. Cancer Res 2004;64:7596-7603. 91. Guermonprez P, Valladeau J, Zitvogel L, Thery C, Amigorena S. Antigen presentation and T cell stimulation by dendritic cells. Annu Rev Immunol 2002;20:621-667. 92. Fernandez NC, Lozier A, Flament C, Ricciardi-Castagnoli P, Bellet D, Suter M, et al. Dendritic cells directly trigger NK cell functions: cross-talk relevant in innate anti-tumor immune responses in vivo. Nat Med 1999;5:405-411. 93. Gerosa F, Baldani-Guerra B, Nisii C, Marchesini V, Carra G, Trinchieri G. Reciprocal activating interaction between natural killer cells and dendritic cells. J Exp Med 2002;195:327-333. 94. Zitvogel L, Terme M, Borg C, Trinchieri G. Dendritic cell-NK cell cross-talk: regulation and physiopathology. Curr Top Microbiol Immunol 2006;298:157-174. 95. Moretta A. Natural killer cells and dendritic cells: rendezvous in abused tissues. Nat Rev Immunol 2002;2:957-964. 96. Cooper MA, Fehniger TA, Fuchs A, Colonna M, Caligiuri MA. NK cell and DC interactions. Trends Immunol 2004;25:47-52. 97. Vitale M, Della Chiesa M, Carlomagno S, Romagnani C, Thiel A, Moretta L, Moretta A. The small subset of CD56brightCD16natural killer cells is selectively responsible for both cell proliferation and interferon-gamma production upon interaction with dendritic cells. Eur J Immunol 2004;34:1715-1722. 98. Martin-Fontecha A, Thomsen LL, Brett S, Gerard C, Lipp M, Lanzavecchia A, Sallusto F. Induced recruitment of NK cells to lymph nodes provides IFN-γ for T(H)1 priming. Nat Immunol 2004;5:1260-1265. 99. Fehniger TA, Cooper MA, Nuovo GJ, Cella M, Facchetti F, Colonna M, Caligiuri MA. CD56bright natural killer cells are present in human lymph nodes and are activated by T cell-derived IL-2: a potential new link between adaptive and innate immunity. Blood 2003;101:3052-3057. 100.Ferlazzo G, Thomas D, Lin SL, Goodman K, Morandi B, Muller WA, et al. The abundant NK cells in human secondary lymphoid tissues require activation to express killer cell Ig-like receptors and become cytolytic. J Immunol 2004;172:1455-1462. Inmunol 25/1 10/5/06 17:15 Página 37 INMUNOLOGÍA 101.Castriconi R, Cantoni C, della Chiesa M, Vitale M, Marcenaro E, Conte R, et al. Transforming growth factor beta 1 inhibits expression of NKp30 and NKG2D receptors: consequences for the NK-mediated killing of dendritic cells. Proc Natl Acad Sci USA 2003;100:41204125. 102.Ferlazzo G, Tsang ML, Moretta L, Melioli G, Steinman RM, Munz C. Human dendritic cells activate resting natural killer (NK) cells and are recognized via the NKp30 receptor by activated NK cells. J Exp Med 2002;195:343-351. 103.Cooper MA, Fehniger TA, Caligiuri MA. The biology of human natural killer-cell subsets. Trends Immunol 2001;22:633-640. 104.Robertson MJ. Role of chemokines in the biology of natural killer cells. J Leukoc Biol 2002;71:173-183. 105.Ferlazzo G, Pack M, Thomas D, Paludan C, Schmid D, Strowig T, er al. Distinct roles of IL-12 and IL-15 in human natural killer cell activation by dendritic cells from secondary lymphoid organs. Proc Natl Acad Sci USA 2004;101:16606-16611. 106.Adam C, King S, Allgeier T, Braumuller H, Luking C, Mysliwietz J, et al. DC-NK cell cross-talk as a novel CD4+ T cell-independent pathway for antitumor CTL induction. Blood 2005;106:338-344. 107.Walzer T, Dalod M, Vivier E, Zitvogel L. Natural killer cell-dendritic cell crosstalk in the initiation of immune responses. Expert Opin Biol Ther 2005;5 Suppl 1:S49-S59. 108.Walzer T, Dalod M, Robbins SH, Zitvogel L, Vivier E. Naturalkiller cells and dendritic cells: «l'union fait la force». Blood 2005;106:2252-2258. 109.Munz C, Dao T, Ferlazzo G, de Cos MA, Goodman K, Young JW. Mature myeloid dendritic cell subsets have distinct roles for activation and viability of circulating human natural killer cells. Blood 2005;105:266-273. 110.Rabinovich BA, Li J, Shannon J, Hurren R, Chalupny J, Cosman D, Miller RG. Activated, But Not Resting, T Cells Can Be Recognized and Killed by Syngeneic NK Cells J Immunol 2003;170:3572-3576. 111.Zingoni A, Sornasse T, Cocks BG, Tanaka Y, Santoni A, Lanier LL. Cross-Talk between Activated Human NK Cells and CD4+ T Cells via OX40-OX40 Ligand Interactions. J Immunol 2004;173:37163724. 112.Maasho K, Opoku-Anane J, Marusina AI, Coligan JE, Borrego F. NKG2D Is a Costimulatory Receptor for Human Naive CD8+ T Cells. J Immunol 2005;174:4480-4484. 113.Dunn GP, Old LJ, Schreiber RD. The three Es of cancer immunoediting. Annu Rev Immunol 2004;22:329-360. 114.Dunn GP, Bruce AT, Ikeda H, Old LJ, Schreiber RD. Cancer immunoediting: from immunosurveillance to tumor escape. Nat Immunol 2002;3:991-998. 115.Khong HT, Restifo NP. Natural selection of tumor variants in the generation of «tumor escape» phenotypes. Nat Immunol 2002;3:9991005. 116.Vetter CS, Groh V, thor Straten P, Spies T, Brocker EB, Becker JC. Expression of stress-induced MHC class I related chain molecules on human melanoma. J Invest Dermatol 2002;118:600-605. 117.Vetter CS, Lieb W, Brocker EB, Becker JC. Loss of nonclassical MHC molecules MIC-A/B expression during progression of uveal melanoma. Br J Cancer 2004;91:1495-1499. 118.Doubrovina ES, Doubrovin MM, Vider E, Sisson RB, O'Reilly RJ, Dupont B, Vyas YM. Evasion from NK cell immunity by MHC N. WALTER ZWIRNER ET AL. class I chain-related molecules expressing colon adenocarcinoma. J Immunol 2003;171:6891-6899. 119.Pende D, Rivera P, Marcenaro S, Chang C-C, Biassoni R, Conte R, et al. Major Histocompatibility Complex Class I-related Chain A and UL16-Binding Protein Expression on Tumor Cell Lines of Different Histotypes: Analysis of Tumor Susceptibility to NKG2D-dependent Natural Killer Cell Cytotoxicity. Cancer Res 2002;62:6178-6186. 120.Jinushi M, Takehara T, Tatsumi T, Kanto T, Groh V, Spies T, et al. Expression and role of MICA and MICB in human hepatocellular carcinomas and their regulation by retinoic acid. Int J Cancer 2003;104:354-361. 121.Maccalli C, Pende D, Castelli C, Mingari MC, Robbins PF, Parmiani G. NKG2D engagement of colorectal cancer-specific T cells strengthens TCR-mediated antigen stimulation and elicits TCR independent anti-tumor activity. Eur J Immunol 2003;33:20332043. 122.Salih HR, Antropius H, Gieseke F, Lutz SZ, Kanz L, Rammensee HG, Steinle A. Functional expression and release of ligands for the activating immunoreceptor NKG2D in leukemia. Blood 2003;102:1389-1396. 123.Wagsater D, Dimberg J, Hugander A, Sirsjo A, Ghaderi M. Analysis of MICA gene transcripts in human rectal cancers. Anticancer Res 2003;23:2525-2529. 124.Carbone E, Neri P, Mesuraca M, Fulciniti MT, Otsuki T, Pende D, et al. HLA class I, NKG2D, and natural cytotoxicity receptors regulate multiple myeloma cell recognition by natural killer cells. Blood 2005;105:251-258. 125.Romanski A, Bug G, Becker S, Kampfmann M, Seifried E, Hoelzer D, et al. Mechanisms of resistance to natural killer cell-mediated cytotoxicity in acute lymphoblastic leukemia. Exp Hematol 2005;33:344-52. 126.Costello RT, Sivori S, Marcenaro E, Lafage-Pochitaloff M, Mozziconacci MJ, Reviron D, et al. Defective expression and function of natural killer cell-triggering receptors in patients with acute myeloid leukemia. Blood 2002;99:3661-3667. 127.Gasser S, Orsulic S, Brown EJ, Raulet DH. The DNA damage pathway regulates innate immune system ligands of the NKG2D receptor. Nature 2005;436:1186-1190. 128.Routes JM, Ryan S, Morris K, Takaki R, Cerwenka A, Lanier LL. Adenovirus serotype 5 E1A sensitizes tumor cells to NKG2Ddependent NK cell lysis and tumor rejection. J Exp Med 2005;202:14771482. 129.Pende D, Rivera P, Marcenaro S, Chang CC, Biassoni R, Conte R, et al. Major histocompatibility complex class I-related chain A and UL16-binding protein expression on tumor cell lines of different histotypes: analysis of tumor susceptibility to NKG2Ddependent natural killer cell cytotoxicity. Cancer Res 2002;62:61786186. 130.Coudert JD, Zimmer J, Tomasello E, Cebecauer M, Colonna M, Vivier E, Held W. Altered NKG2D function in NK cells induced by chronic exposure to NKG2D ligand-expressing tumor cells. Blood 2005;106:1711-1717. 131.Girlanda S, Fortis C, Belloni D, Ferrero E, Ticozzi P, Sciorati C, et al. MICA expressed by multiple myeloma and monoclonal gammopathy of undetermined significance plasma cells costimulates pamidronate-activated gammadelta lymphocytes. Cancer Res 2005;65:7502-7508. 37 Inmunol 25/1 10/5/06 17:15 Página 38 IMMUNOBIOLOGY OF THE HUMAN MHC CLASS I CHAIN-RELATED GENE A (MICA) ... 132.Gonzalez S, Groh V, Spies T. Immunobiology of human NKG2D and its ligands. Curr Top Microbiol Immunol 2006;298:121-138. 133.Salih HR, Antropius H, Gieseke F, Lutz SZ, Kanz L, Rammensee H-G, Steinle A. Functional expression and release of ligands for the activating immunoreceptor NKG2D in leukemia. Blood 2003;102:1389-1396. 134.Wu JD, Higgins LM, Steinle A, Cosman D, Haugk K, Plymate SR. Prevalent expression of the immunostimulatory MHC class I chainrelated molecule is counteracted by shedding in prostate cancer. J Clin Invest 2004;114:560-568. 135.Watson NF, Spendlove I, Madjd Z, McGilvray R, Green AR, Ellis IO, et al. Expression of the stress-related MHC class I chain-related protein MICA is an indicator of good prognosis in colorectal cancer patients. Int J Cancer 2005;118:1445-1452. 136.Girlanda S, Fortis C, Belloni D, Ferrero E, Ticozzi P, Sciorati C, et al. MICA Expressed by Multiple Myeloma and Monoclonal Gammopathy of Undetermined Significance Plasma Cells Costimulates Pamidronate-Activated gd Lymphocytes. Cancer Res 2005;65:7502-7508. 137.Wiemann K, Mittrucker HW, Feger U, Welte SA, Yokoyama WM, Spies T, et al. Systemic NKG2D down-regulation impairs NK and CD8 T cell responses in vivo. J Immunol 2005;175:720-729. 138.Bahram S, Inoko H, Shiina T, Radosavljevic M. MIC and other NKG2D ligands: from none to too many. Curr Opin Immunol 2005;17:505-509. 139.Groh V, Wu J, Yee C, Spies T. Tumour-derived soluble MIC ligands impair expression of NKG2D and T-cell activation. Nature 2002;419:734-738. 140.Oppenheim DE, Roberts SJ, Clarke SL, Filler R, Lewis JM, Tigelaar RE, et al. Sustained localized expression of ligand for the activating NKG2D receptor impairs natural cytotoxicity in vivo and reduces tumor immunosurveillance. Nat Immunol 2005;6:928-937. 141.Raffaghello L, Prigione I, Airoldi I, Camoriano M, Levreri I, Gambini C, et al. Downregulation and/or release of NKG2D ligands as immune evasion strategy of human neuroblastoma. Neoplasia 2004;6:558-568. 142.Salih HR, Rammensee H-G, Steinle A. Down-Regulation of MICA on Human Tumors by Proteolytic Shedding. J Immunol 2002;169:40984102. 143.Holdenrieder S, Stieber P, Peterfi A, Nagel D, Steinle A, Salih HR. Soluble MICA in malignant diseases. Int J Cancer 2006;118:684687. 144.Wiemann K, Mittrucker H-W, Feger U, Welte SA, Yokoyama WM, 38 VOL. 25 NUM. 1/ 2006 Spies T, et al. Systemic NKG2D Down-Regulation Impairs NK and CD8 T Cell Responses In Vivo. J Immunol 2005;175:720-729. 145.Polette M, Nawrocki-Raby B, Gilles C, Clavel C, Birembaut P. Tumour invasion and matrix metalloproteinases. Crit Rev Oncol Hematol 2004;49:179-186. 146.Hojilla CV, Mohammed FF, Khokha R. Matrix metalloproteinases and their tissue inhibitors direct cell fate during cancer development. Br J Cancer 2003;89:1817-1821. 147.Lee JC, Lee KM, Kim DW, Heo DS. Elevated TGF-β1 secretion and down-modulation of NKG2D underlies impaired NK cytotoxicity in cancer patients. J Immunol 2004;172:7335-7340. 148.Glick AB. TGFβ1, back to the future: revisiting its role as a transforming growth factor. Cancer Biol Ther 2004;3:276-283. 149.Kim R, Emi M, Tanabe K, Uchida Y, Toge T. The role of Fas ligand and transforming growth factor beta in tumor progression: molecular mechanisms of immune privilege via Fas-mediated apoptosis and potential targets for cancer therapy. Cancer 2004;100:2281-2291. 150.Rubinstein N, Alvarez M, Zwirner NW, Toscano MA, Ilarregui JM, Bravo A, et al. Targeted inhibition of galectin-1 gene expression in tumor cells results in heightened T cell-mediated rejection; A potential mechanism of tumor-immune privilege. Cancer Cell 2004;5:241-251. 151.Rivoltini L, Carrabba M, Huber V, Castelli C, Novellino L, Dalerba P, et al. Immunity to cancer: attack and escape in T lymphocytetumor cell interaction. Immunol Rev 2002;188:97-113. 152.Poggi A, Massaro AM, Negrini S, Contini P, Zocchi MR. TumorInduced Apoptosis of Human IL-2-Activated NK Cells: Role of Natural Cytotoxicity Receptors. J Immunol 2005;174:2653-2660. 153.Cerwenka A, Baron JL, Lanier LL. Ectopic expression of retinoic acid early inducible-1 gene (RAE-1) permits natural killer cellmediated rejection of a MHC class I-bearing tumor in vivo. Proc Natl Acad Sci USA 2001;98:11521-11526. 154.Diefenbach A, Jensen ER, Jamieson AM, Raulet DH. Rae1 and H60 ligands of the NKG2D receptor stimulate tumour immunity. Nature 2001;413:165-171. 155.Takaki R, Hayakawa Y, Nelson A, Sivakumar PV, Hughes S, Smyth MJ, Lanier LL. IL-21 enhances tumor rejection through a NKG2Ddependent mechanism. J Immunol 2005;175:2167-2173. 156.Busche A, Goldmann T, Naumann U, Steinle A, Brandau S. Natural killer cell-mediated rejection of experimental human lung cancer by genetic overexpression of major histocompatibility complex class I chain-related gene a. Hum Gene Ther 2006;17:135146.