18FNa-fluoride has a higher extraction with respect to 99mTc
Anuncio
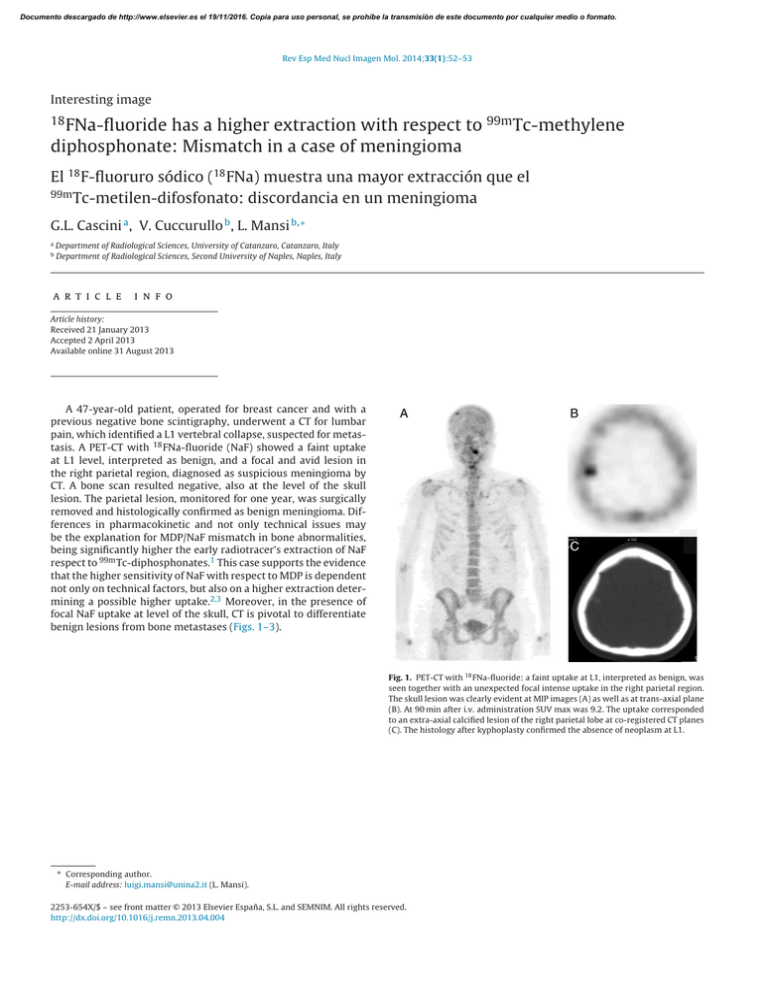
Documento descargado de http://www.elsevier.es el 19/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. Rev Esp Med Nucl Imagen Mol. 2014;33(1):52–53 Interesting image 18 FNa-fluoride has a higher extraction with respect to 99m Tc-methylene diphosphonate: Mismatch in a case of meningioma El 18 F-fluoruro sódico (18 FNa) muestra una mayor extracción que el 99m Tc-metilen-difosfonato: discordancia en un meningioma G.L. Cascini a , V. Cuccurullo b , L. Mansi b,∗ a b Department of Radiological Sciences, University of Catanzaro, Catanzaro, Italy Department of Radiological Sciences, Second University of Naples, Naples, Italy a r t i c l e i n f o Article history: Received 21 January 2013 Accepted 2 April 2013 Available online 31 August 2013 A 47-year-old patient, operated for breast cancer and with a previous negative bone scintigraphy, underwent a CT for lumbar pain, which identified a L1 vertebral collapse, suspected for metastasis. A PET-CT with 18 FNa-fluoride (NaF) showed a faint uptake at L1 level, interpreted as benign, and a focal and avid lesion in the right parietal region, diagnosed as suspicious meningioma by CT. A bone scan resulted negative, also at the level of the skull lesion. The parietal lesion, monitored for one year, was surgically removed and histologically confirmed as benign meningioma. Differences in pharmacokinetic and not only technical issues may be the explanation for MDP/NaF mismatch in bone abnormalities, being significantly higher the early radiotracer’s extraction of NaF respect to 99m Tc-diphosphonates.1 This case supports the evidence that the higher sensitivity of NaF with respect to MDP is dependent not only on technical factors, but also on a higher extraction determining a possible higher uptake.2,3 Moreover, in the presence of focal NaF uptake at level of the skull, CT is pivotal to differentiate benign lesions from bone metastases (Figs. 1–3). Fig. 1. PET-CT with 18 FNa-fluoride: a faint uptake at L1, interpreted as benign, was seen together with an unexpected focal intense uptake in the right parietal region. The skull lesion was clearly evident at MIP images (A) as well as at trans-axial plane (B). At 90 min after i.v. administration SUV max was 9.2. The uptake corresponded to an extra-axial calcified lesion of the right parietal lobe at co-registered CT planes (C). The histology after kyphoplasty confirmed the absence of neoplasm at L1. ∗ Corresponding author. E-mail address: [email protected] (L. Mansi). 2253-654X/$ – see front matter © 2013 Elsevier España, S.L. and SEMNIM. All rights reserved. http://dx.doi.org/10.1016/j.remn.2013.04.004 Documento descargado de http://www.elsevier.es el 19/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. G.L. Cascini et al. / Rev Esp Med Nucl Imagen Mol. 2014;33(1):52–53 53 Fig. 2. Diagnostic CT with bone (A) and brain (B) window at level of the lesion identified by 18 FNa-fluoride PET-CT. The small calcified lesion appears rounded and elongated with a broad attachment to the dura. Density was homogeneous in pre-contrast images (C) with a mild contrast enhancement in arterial phase (D). A meningioma with benign features was suspected, confirmed by histology at surgery performed one year later. Fig. 3. Bone scintigraphy 6 months after 18 FNa-fluoride PET-CT and before surgery. Whole body (A) acquisition demonstrated the absence of focal uptake in the skull. Only in dynamic vascular phase in anterior view (B) a mild transitory and progressive uptake appeared in the right parietal region (arrow), in agreement with a vascularized lesion showing a higher blood pool non accompanied by a significant deposition of MDP in the delayed osteoblastic phase, because of a low extraction. The corresponding axial planes on 18 FNa-fluoride PET (C) and 99m Tc-MDP-SPECT (D). Conflict of interest The authors have no conflicts of interest to declare. References 1. Cuccurullo V, Cascini G, Rossi A, Tamburrini O, Rotondo A, Mansi L. Pathophysiological premises to radiotracers for bone metastases. Q J Nucl Med Mol Imaging. 2011;55:353–73. 2. Langsteger W, Haim S, Knauer M, Waldenberger P, Emmanuel K, Loidl W, et al. Imaging of bone metastases in prostate cancer: an update. Q J Nucl Med Mol Imaging. 2012;56:447–58. 3. de Arcocha M, Portilla-Quattrociocchi H, Medina-Quiroz P, Carril JM. Current status of the use of 18 F-sodium fluoride in bone disease. Rev Esp Med Nucl Imagen Mol. 2012;31:51–7.