Evolution of solitary plasmacytoma of the sternum to multiple
Anuncio

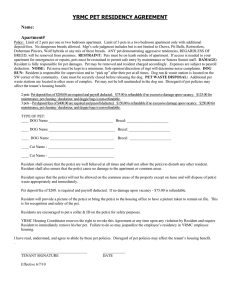
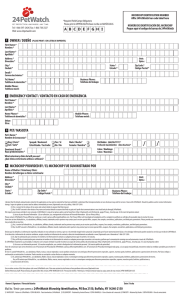
Documento descargado de http://www.elsevier.es el 18/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. Rev Esp Med Nucl Imagen Mol. 2013;32(5):328–329 Interesting image Evolution of solitary plasmacytoma of the sternum to multiple myeloma with multifocal extramedullary liver involvement. Contribution of 18 F-FDG PET–CT夽 Evolución de un plasmocitoma solitario del esternón a un mieloma múltiple con afectación extramedular multifocal hepática. Aportación de la 18 F-FDG PET-TAC J. Banzo a,∗ , L. Palomera b , M.A. Ubieto a , E. Bonafonte b , E.F. Rambalde c , S.M. Ayala c a Unidad de Medicina Nuclear, Grupo Hospitalario Quirón La Floresta (Proyecto OTRI [Oficinas de Transferencia de Resultados de Investigación] de Investigación, Grupo Hospitalario Quirón y Universidad de Zaragoza), Zaragoza, Spain b Servicio de Hematología, Hospital Clínico Universitario Lozano Blesa, Zaragoza, Spain c Servicio de Medicina Nuclear, Hospital Clínico Universitario Lozano Blesa, Zaragoza, Spain a r t i c l e i n f o Article history: Received 5 October 2012 Accepted 26 October 2012 Solitary plasmacytoma (SP) is a malignant tumor lesion characterized by an infiltrate of atypical plasma cells. According to its localization it may be in either bone or extramedullary.1 There is no evidence of systemic multiple myeloma (MM) in SP: imaging techniques show a single lesion, bone marrow biopsy is normal, <10% of plasma cells, and there is no organic dysfunction related to the hypercalcemia, anemia, renal failure or lytic bone alterations. A significant proportion of patients evolve to MM. Extramedullary disease (ED) may be synchronic with the infiltration of the bone marrow (BM) or may appear during the course of MM as a pattern of recurrence. An increase in the incidence of ED has been observed, probably in relation to the use of PET and MR in the diagnosis and the prolongation of life of patients with the use of new chemotherapy agents and autotransplantation of BM. Focal or multifocal hepatic ED is rare and is associated with a poor prognosis.2 The evaluation of MM by PET–CT is under debate, and despite the rise in the number of papers in the last years, it is difficult to know its diagnostic precision. In a recent metaanalysis, the sensitivity of PET and PET–CT in MM was of 61.1% for intramedullary involvement and 96% for ED.3 The new Durie–Salmon PLUS staging Fig. 1. 59-year-old patient with a history of sternal plasmacytoma treated with radiotherapy. Six months later the patient was admitted for somnolence, nausea and pain in the thoracic column and in the costal ribcage. Physical examination revealed deformity of the manubrium of the sternum and a low level of consciousness. Laboratory parameters were: Hb: 9.4 g/L, calcemia: 12.6 mg/dL, LDH: 635 U/L, urea: 59 mg/dL and creatinine: 1.6 mg/dL. Distorsion of the lambda chains was observed with a lack of expression of the heavy chains in serum and important urine elimination of the lambda chains (Bence–Jones protein: 9.2 g/24 h). The study with 18 F-FDG PET–CT demonstrated a destructive lesion in the manubrium of the sternum which was slightly hypermetabolic (arrows) with an infiltrate of plasma cells shown by biopsy. 夽 Please cite this article as: Banzo J, Palomera L, Ubieto MA, Bonafonte E, Rambalde EF, Ayala SM. Evolución de un plasmocitoma solitario del esternón a un mieloma múltiple con afectación extramedular multifocal hepática. Aportación de la 18 F-FDG PET-TAC. Rev Esp Med Nucl Imagen Mol. 2013;32:328–9. ∗ Corresponding author. E-mail address: [email protected] (J. Banzo). 2253-8089/$ – see front matter © 2012 Elsevier España, S.L. and SEMNIM. All rights reserved. Documento descargado de http://www.elsevier.es el 18/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. J. Banzo et al. / Rev Esp Med Nucl Imagen Mol. 2013;32(5):328–329 329 Fig. 2. Numerous hypermetabolic lesions in the humerus, costal ribcage, lumbar column, pelvis and femurs corresponding to lytic bone lesions, some with festooned endosteum or with a soft-tissue mass. Multiple hypermetabolic nodules in the right liver lobe (arrows). The liver biopsy showed aberrant plasma cells of plasmablastic appearance. With the diagnosis of MM with bone and liver plasmacytomas, treatment with bortezomib–prednisome–melphalan was initiated, showing an improvement in the symptomatology and reduction of the size of the hepatic lesions and the disappearance of Bence–Jones protein in urine. Four months later the disease progressed with the appearance of a large tumor in the right ankle and extrapleural masses, widening of the mediastinum, costal fractures and alveolar edema in the chest plaque, followed by patient death due to multiorgan failure. system incorporates advanced imaging techniques which include PET and MR, providing both with complementary information. The case presented here illustrates the capacity of PET–CT to diagnose rare multifocal ED in the liver in a patient with sternal SP evolving to MM (Figs. 1 and 2). References 1. Fernández López R, Borrego Dorado I, Paz Coll A, Vázquez Albertino R, Gómez Camarero P, Sanz Viedma S. Tomografía por emisión de positrones con 18 F-fluorodeoxy-glucosa en un caso de plasmacitoma solitario de paladar blando. Rev Esp Med Nucl. 2010;29:263–5. 2. Saboo SS, Fennessy F, Benajiba L, Laubach J, Anderson KC, Richardson PG. Imaging features of extramedullary, relapsed, and refractory multiple myeloma involving the liver across treatment with cyclophosphamide, lenalidomide, bortezomib, and dexamethasone. J Clin Oncol. 2012;30:e175–9. 3. Lu YY, Chen JH, Lin WY, Liang JA, Wang HY, Tsai SC, et al. FDG PET or PET/CT for detecting intramedullary and extramedullary lesions in multiple myeloma: a systematic review and meta-analysis. Clin Nucl Med. 2012;37: 833–7.