Add-On Omalizumab in Persistent Difficult-To-Treat Asthma: a
Anuncio
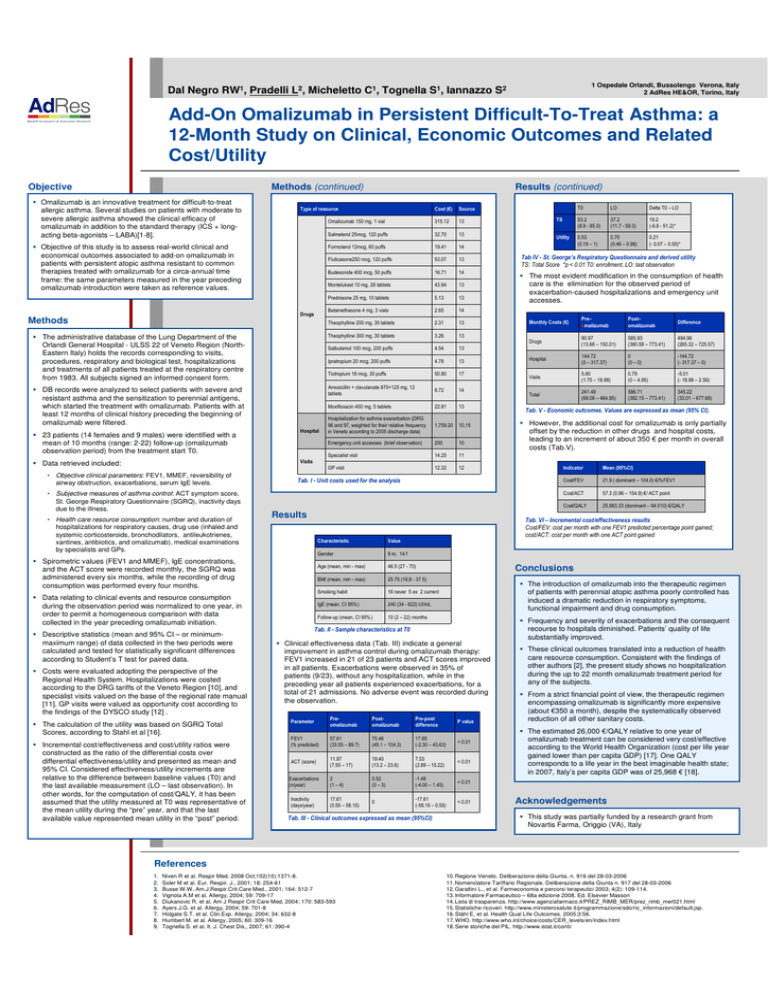
1 Ospedale Orlandi, Bussolengo Verona, Italy 2 AdRes HE&OR, Torino, Italy Dal Negro RW1, Pradelli L2, Micheletto C1, Tognella S1, Iannazzo S2 Add-On Omalizumab in Persistent Difficult-To-Treat Asthma: a 12-Month Study on Clinical, Economic Outcomes and Related Cost/Utility Objective Methods (continued) Omalizumab is an innovative treatment for difficult-to-treat allergic asthma. Several studies on patients with moderate to severe allergic asthma showed the clinical efficacy of omalizumab in addition to the standard therapy (ICS + longacting beta-agonists – LABA)[1-8]. Results (continued) Type of resource Cost (€) Source Omalizumab 150 mg, 1 vial 315.12 13 Salmeterol 25mcg, 120 puffs 32.70 13 Formoterol 12mcg, 60 puffs 19.41 14 Fluticasone250 mcg, 120 puffs 53.07 13 Budesonide 400 mcg, 50 puffs 16.71 14 Montelukast 10 mg, 28 tablets 43.94 13 Prednisone 25 mg, 10 tablets 5.13 13 Betamethasone 4 mg, 3 vials 2.65 14 Theophylline 200 mg, 30 tablets 2.31 13 The administrative database of the Lung Department of the Orlandi General Hospital - ULSS 22 of Veneto Region (NorthEastern Italy) holds the records corresponding to visits, procedures, respiratory and biological test, hospitalizations and treatments of all patients treated at the respiratory centre from 1983. All subjects signed an informed consent form. Theophylline 300 mg, 30 tablets 3.26 13 Salbutamol 100 mcg, 200 puffs 4.54 13 DB records were analyzed to select patients with severe and resistant asthma and the sensitization to perennial antigens, which started the treatment with omalizumab. Patients with at least 12 months of clinical history preceding the beginning of omalizumab were filtered. Objective of this study is to assess real-world clinical and economical outcomes associated to add-on omalizumab in patients with persistent atopic asthma resistant to common therapies treated with omalizumab for a circa-annual time frame: the same parameters measured in the year preceding omalizumab introduction were taken as reference values. Drugs Methods 23 patients (14 females and 9 males) were identified with a mean of 10 months (range: 2-22) follow-up (omalizumab observation period) from the treatment start T0. Hospital Ipratropium 20 mcg, 200 puffs 4.78 13 Tiotropium 18 mcg, 30 puffs 50.80 17 Amoxicillin + clavulanate 875+125 mg, 12 tablets 8.72 14 Moxifloxacin 400 mg, 5 tablets 22.81 13 Hospitalization for asthma exacerbation (DRG 96 and 97, weighted for their relative frequency in Veneto according to 2005 discharge data) 1,759.20 10,15 Emergency unit accesses (brief observation) 200 10 Specialist visit 14.25 11 GP visit 12.32 12 T0 LO Delta T0 – LO TS 53.2 (8.9 - 85.0) 37.2 (11.7 - 59.3) 19.2 (-6.8 - 51.2)* Utility 0.53 (0.18 – 1) 0.70 (0.46 – 0.98) 0.21 (- 0.07 – 0.55)* Tab IV - St. George’s Respiratory Questionnaire and derived utility TS: Total Score *p < 0.01 T0: enrollment, LO: last observation The most evident modification in the consumption of health care is the elimination for the observed period of exacerbation-caused hospitalizations and emergency unit accesses. Monthly Costs (€) Pre– omalizumab Post– omalizumab Difference Drugs 90.97 (13.68 – 150.01) 585.93 (390.58 – 773.41) 494.96 (265.32 – 725.57) Hospital 144.72 (0 – 317.37) 0 (0 – 0) -144.72 (- 317.37 – 0) Visits 5.80 (1.75 – 18.98) 0.79 (0 – 4.95) -5.01 (- 18.98 – 2.56) Total 241.49 (69.08 – 464.95) 586.71 (392.15 – 773.41) 345.22 (33.01 – 677.68) Tab. V - Economic outcomes. Values are expressed as mean (95% CI). However, the additional cost for omalizumab is only partially offset by the reduction in other drugs and hospital costs, leading to an increment of about 350 € per month in overall costs (Tab.V). Visits Data retrieved included: • Objective clinical parameters: FEV1, MMEF, reversibility of airway obstruction, exacerbations, serum IgE levels. • Subjective measures of asthma control: ACT symptom score, St. George Respiratory Questionnaire (SGRQ), inactivity days due to the illness. • Health care resource consumption: number and duration of hospitalizations for respiratory causes, drug use (inhaled and systemic corticosteroids, bronchodilators, antileukotrienes, xantines, antibiotics, and omalizumab), medical examinations by specialists and GPs. Tab. I - Unit costs used for the analysis Results Data relating to clinical events and resource consumption during the observation period was normalized to one year, in order to permit a homogeneous comparison with data collected in the year preceding omalizumab initiation. Costs were evaluated adopting the perspective of the Regional Health System. Hospitalizations were costed according to the DRG tariffs of the Veneto Region [10], and specialist visits valued on the base of the regional rate manual [11]. GP visits were valued as opportunity cost according to the findings of the DYSCO study [12] . The calculation of the utility was based on SGRQ Total Scores, according to Stahl et al [16]. Incremental cost/effectiveness and cost/utility ratios were constructed as the ratio of the differential costs over differential effectiveness/utility and presented as mean and 95% CI. Considered effectiveness/utility increments are relative to the difference between baseline values (T0) and the last available measurement (LO – last observation). In other words, for the computation of cost/QALY, it has been assumed that the utility measured at T0 was representative of the mean utility during the “pre” year, and that the last available value represented mean utility in the “post” period. Mean (95%CI) Cost/FEV 21.9 ( dominant – 104.0) €/%FEV1 Cost/ACT 57.3 (0.96 – 154.9) €/ ACT point Cost/QALY 25,983.33 (dominant – 94.010) €/QALY Tab. VI – Incremental cost/effectiveness results Cost/FEV: cost per month with one FEV1 predicted percentage point gained; cost/ACT: cost per month with one ACT point gained Spirometric values (FEV1 and MMEF), IgE concentrations, and the ACT score were recorded monthly, the SGRQ was administered every six months, while the recording of drug consumption was performed every four months. Descriptive statistics (mean and 95% CI – or minimummaximum range) of data collected in the two periods were calculated and tested for statistically significant differences according to Student’s T test for paired data. Indicator Characteristic Value Gender 9 m, 14 f Age (mean, min - max) 46.5 (27 - 70) BMI (mean, min - max) 25.75 (19.8 - 37.5) Smoking habit 16 never 5 ex 2 current IgE (mean, CI 95%) 240 (34 - 622) UI/mL Follow-up (mean, CI 95%) 10 (2 – 22) months Conclusions The introduction of omalizumab into the therapeutic regimen of patients with perennial atopic asthma poorly controlled has induced a dramatic reduction in respiratory symptoms, functional impairment and drug consumption. Tab. II - Sample characteristics at T0 Clinical effectiveness data (Tab. III) indicate a general improvement in asthma control during omalizumab therapy: FEV1 increased in 21 of 23 patients and ACT scores improved in all patients. Exacerbations were observed in 35% of patients (9/23), without any hospitalization, while in the preceding year all patients experienced exacerbations, for a total of 21 admissions. No adverse event was recorded during the observation. Parameter Preomalizumab Postomalizumab Pre-post difference P value FEV1 (% predicted) 57.61 (33.55 – 89.7) 75.46 (45.1 – 104.3) 17.85 (-2.30 – 43.63) < 0.01 ACT (score) 11.87 (7.55 – 17) 19.40 (13.2 – 23.6) 7.53 (2.89 – 15.22) < 0.01 Exacerbations (n/year) 2 (1 – 4) 0.52 (0 – 3) -1.48 (-4.00 – 1.45) < 0.01 Inactivity (days/year) 17.61 (0.55 – 58.15) 0 -17.61 (-58.15 – 0.55) < 0.01 Tab. III - Clinical outcomes expressed as mean (95%CI) Frequency and severity of exacerbations and the consequent recourse to hospitals diminished. Patients’ quality of life substantially improved. These clinical outcomes translated into a reduction of health care resource consumption. Consistent with the findings of other authors [2], the present study shows no hospitalization during the up to 22 month omalizumab treatment period for any of the subjects. From a strict financial point of view, the therapeutic regimen encompassing omalizumab is significantly more expensive (about €350 a month), despite the systematically observed reduction of all other sanitary costs. The estimated 26,000 €/QALY relative to one year of omalizumab treatment can be considered very cost/effective according to the World Health Organization (cost per life year gained lower than per capita GDP) [17]. One QALY corresponds to a life year in the best imaginable health state; in 2007, Italy’s per capita GDP was of 25,968 € [18]. Acknowledgements This study was partially funded by a research grant from Novartis Farma, Origgio (VA), Italy References 1. 2. 3. 4. 5. 6. 7. 8. 9. Niven R et al. Respir Med. 2008 Oct;102(10):1371-8. Soler M et al. Eur. Respir. J., 2001; 18: 254-61 Busse W.W. Am.J.Respir.Crit.Care Med., 2001; 164: 512-7 Vignola A.M et al. Allergy, 2004; 59: 709-17 Diukanovic R. et al. Am J Respir Crit Care Med, 2004; 170: 583-593 Ayers J.G. et al. Allergy, 2004; 59: 701-8 Holgate S.T. et al. Clin.Exp. Allergy, 2004; 34: 632-8 Humbert M. et al. Allergy, 2005; 60: 309-16 Tognella S. et al. It. J. Chest Dis., 2007; 61: 390-4 10. Regione Veneto. Deliberazione della Giunta. n. 916 del 28-03-2006 11. Nomenclatore Tariffario Regionale. Deliberazione della Giunta n. 917 del 28-03-2006 12. Garattini L., et al. Farmeconomia e percorsi terapeutici 2003; 4(2): 109-114. 13. Informatore Farmaceutico – 68a edizione 2008. Ed. Elsevier Masson 14. Lista di trasparenza. http://www.agenziafarmaco.it/PREZ_RIMB_MER/prez_rimb_mer021.html 15. Statistiche ricoveri. http://www.ministerosalute.it/programmazione/sdo/ric_informazioni/default.jsp. 16. Ståhl E, et al. Health Qual Life Outcomes. 2005;3:56. 17. WHO. http://www.who.int/choice/costs/CER_levels/en/index.html 18. Serie storiche del PIL. http://www.istat.it/conti/