- Ninguna Categoria
Food Allergy & Growth: Identifying At-Risk Children
Anuncio
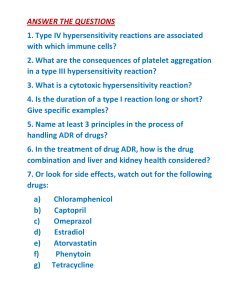
Clinical Commentary Review Identifying Children at Risk of Growth and Nutrient Deficiencies in the Food Allergy Clinic Carina Venter, PhDa, Rosan Meyer, PhDb,c,d, Maureen Bauer, MDa, J. Andrew Bird, MDe, David M. Fleischer, MDa, Anna Nowak-Wegrzyn, MD, PhDf,g, Aikaterini Anagnostou, MD, PhDh,i, Brian P. Vickery, MDj,k, Julie Wang, MDl, and Marion Groetch, MSl Dallas and Houston, Texas; New York, NY; Atlanta, Ga; Aurora, Colo; London and Winchester, United Kingdom; Leuven, Belgium; and Olsztyn, Poland BACKGROUND: Food allergies affect growth in children by decreasing the availability of nutrients through decreased dietary intake, increased dietary needs, foodemedication interactions, and psychosocial burden. Guidelines on food allergy management frequently recommend nutrition counseling and growth monitoring of children with food allergies. OBJECTIVE: To provide clear guidance for clinicians to identify children with food allergies who are at nutritional risk and ensure prompt intervention. METHODS: We provide a narrative review summarizing information from national and international guidelines, retrospective studies, population studies, review articles, case reports, and case series to identify those with food allergy at greatest nutritional risk, determine the impact of nutritional interventions on growth, and develop guidance for risk reduction in children with food allergies. RESULTS: Children with food allergies are at increased risk of nutritional deficiencies and poor growth. Nutritional assessment and intervention can improve outcomes. Identifying poor growth is an important step in the nutrition assessment. Therefore, growth should be assessed at each allergy evaluation. Interventions to ensure adequate dietary intake for growth include appropriately prescribed elimination diets, breastfeeding support and assessment, supplemental formula, vitamin and/or mineral supplementation, appropriate milk substitutes, and timely introduction of nutrient-dense complementary foods. a Council National Peanut Board; receives royalties from UpToDate; and serves as a consultant for Aquestive, DBV Technologies, Genentech, and Nasus, all of which are outside the submitted work. institution has received research support from Aimmune Therapeutics and DBV Technologies; serves as a non-paid member of the Medical Advisory Board for Food Allergy & Anaphylaxis Connection Team and the Medical Advisory Council National Peanut Board; receives royalties from UpToDate; and serves as a consultant for Aquestive, DBV Technologies, Genentech, and Nasus, all of which are outside the submitted work. A. NowakWegrzyn receives research support from NIAID, Alladapt Immunotherapeutics, Regeneron, DBV, and Siolta Therapeutics; speaking fees from Nestlé, Danone, and Thermo Fisher; and royalties from UpToDate. She serves as an associate editor for the Annals of Allergy, Asthma & Immunology, director of the American Academy of Allergy, Asthma & Immunology board, and the chair of the Medical Advisory Board of the International FPIES Association. A. Anagnostou reports institutional grants from FARE, Aimmune Therapeutics, and Novartis; and personal fees from Aimmune, ALK, Novartis, and Genentech. B.P. Vickery reports grants from Abbott, Alladapt, Genentech, NIH-NIAID, and Siolta; grants and personal fees from Aimmune, DBV, FARE, Novartis, and Regeneron; personal fees from AllerGenis, Aravax, Reacta Biosciences, and Sanofi; and stock options from Moonlight Therapeutics. J. Wang receives research support from the National Institute of Allergy and Infectious Diseases, Aimmune, DBV Technologies, and Siolta; consultancy fees from ALK Abello and Jubilant HollisterStier; and royalty payments from UpToDate. M. Groetch receives royalties from UpToDate and the Academy of Nutrition and Dietetics and consulting fees from Food Allergy Research Education; serves on the Medical Advisory Board of IFPIES, as a Senior Advisor to FARE, and as a Health Sciences Advisor for APFED; is on the editorial board of Journal of Food Allergy; and has no commercial interests to disclose. The other author declares no relevant conflicts of interest. Received for publication November 27, 2023; revised January 16, 2024; accepted for publication January 19, 2024. Available online January 25, 2024. Corresponding author: Carina Venter, PhD, Section of Pediatric Allergy and Immunology, Children’s Hospital Colorado, 13123 East 16th Ave, Box B518, Anschutz Medical Campus, Aurora, CO 80045. E-mail: Carina.Venter@ childrenscolorado.org. 2213-2198 Ó 2024 American Academy of Allergy, Asthma & Immunology https://doi.org/10.1016/j.jaip.2024.01.027 Section of Pediatric Allergy and Immunology, Children’s Hospital Colorado, University of Colorado, Aurora, Colo b Department of Medicine, Imperial College London, London, United Kingdom c Department of Nutrition and Dietetics, University of Winchester, Winchester, United Kingdom d Department of Medicine, KU Leuven, Leuven, Belgium e Department of Pediatrics, Division of Allergy and Immunology, UT Southwestern Medical Center, Dallas, Texas f Hassenfeld Children’s Hospital, Department of Pediatrics, NYU Grossman School of Medicine, New York, NY g Department of Pediatrics, Gastroenterology and Nutrition, Collegium Medicum, University of Warmia and Mazury, Olsztyn, Poland h Section of Allergy and Immunology, Baylor College of Medicine, Houston, Texas i Section of Allergy and Immunology, Department of Pediatrics, Texas Children’s Hospital, Houston, Texas j Children’s Healthcare of Atlanta, Atlanta, Ga k Department of Pediatrics, Emory University, Atlanta, Ga l Division of Pediatric Allergy and Immunology, Icahn School of Medicine at Mount Sinai, New York, NY Conflicts of interest: C. Venter reports grants from Reckitt Benckiser and personal fees from Reckitt Benckiser, Nestlé Nutrition Institute, Danone, Abbott Nutrition, and HAL Allergy outside the submitted work. R. Meyer reports honoraria for lectures from Nestlé Nutrition Institute, Danone/Nutricia, Abbott Nutrition, and Reckitt Benckiser; personal consulting fees from Else Nutrition and Abbott Nutrition; participation as Primary Investigator in a study supported by Danone; and advisory board member for Nestlé Health Science, all outside the submitted work. J.A. Bird reports consultancy with AllerGenis, Allergy Therapeutics Ltd, DBV Technologies, Food Allergy Research & Education (FARE), HAL Allergy, Genentech, Novartis, and Nutricia; and receives grant funding to his institution from Aimmune, Astellas, DBV Technologies, FARE, Genentech, NIHeNational Institute of Allergies and Infectious Diseases (NIAID), Novartis, Siolta, and Regeneron. He is a non-paid member of the American Academy of Pediatrics (AAP) Section of Allergy and Immunology Executive Committee, International FPIES Association medical advisory board, and Texas Department of State Health Services Stock Epinephrine Advisory Committee and is an independent study monitor for Vedanta (uncompensated). D.M. Fleischer’s institution has received research support from Aimmune Therapeutics, ARS Pharmaceuticals, and DBV Technologies; he serves as a non-paid member of the Medical Advisory Board for Food Allergy & Anaphylaxis Connection Team and the Medical Advisory 579 580 VENTER ET AL J ALLERGY CLIN IMMUNOL PRACT MARCH 2024 TABLE I. Practical pointers related to nutritional risk Abbreviations used AD- Atopic dermatitis ARFID- Avoidant restrictive food intake disorder CM- Cow’s milk CMA- Cow’s milk allergy EHF- Extensively hydrolyzed formula FA- Food allergy FPIES- Food proteineinduced enterocolitis syndrome PPI- Proton pump inhibitor VMS- Vitamin and/or mineral supplementation Access to foods of appropriate nutritional value is an ongoing concern. CONCLUSION: Nutrition intervention or referral to registered dietitian nutritionists with additional training and/or experience in food allergy may result in improved growth and nutrition outcomes. Ó 2024 American Academy of Allergy, Asthma & Immunology (J Allergy Clin Immunol Pract 2024;12:579-89) Key words: Food allergy; Malnutrition; Nutrients; Registered dietitian/nutritionist; Management; Allergist INTRODUCTION Many publications have highlighted nutrition and growth concerns in infants and children with food allergies (FA). The importance of nutrition counseling and growth assessment is highlighted in most FA management guidelines.1,2 The Guidelines for the Diagnosis and Management of Food Allergy in the United States: Summary of the National Institute of Allergies and Infectious DiseaseseSponsored Expert Panel Report1 specifically recommends nutritional counseling and regular growth monitoring for all children with FA (Guideline 23). The European Academy of Allergy and Clinical Immunology Food Allergy and Anaphylaxis Guidelines: Diagnosis and Management of Food Allergy3 state that the clinical assessment of patients should include assessing nutritional status and growth. The newly published Global Allergy and Asthma European Network guidelines2 concluded that there is potential for suboptimal nutrition and growth in children with FA, and it is important that only documented food allergens be avoided. Although nutrition counseling by a registered dietitian nutritionist (RDN) with training and/or experience in managing FA may be ideal,1-3 clinicians working in the area of FA report a lack of access to specialist allergy-trained RDNs. Therefore, this work aims to provide clear guidance for clinicians to identify children with FA who are at nutritional risk and steps to mitigate those risks by clinicians who may not have access to allergy specialist RDNs. When available, prompt referral to a suitably trained registered or licensed RDNs can be helpful and guidance on locating a RDN is provided (Table I). FACTORS THAT MAY CONTRIBUTE TO NUTRITION RISK Number of foods avoided and specific FA Number of FA growth parameters. A systematic review reported that avoidance of multiple foods, defined as two or more Factors that may be associated with increased risk All types of food allergies can increase risk for changes in growth and nutrient intake, although cow’s milk allergy in infants and young children poses a particular nutritional risk Nutritional risk may increase with the number of foods avoided Cow’s milk allergy Atopic dermatitis Eosinophilic esophagitis Food proteineinduced enterocolitis syndrome Feeding difficulties Low food security Lack of suitable nutritional alternatives may increase risk Long-term medication use Additional food restrictions owing to cultural, religious, or personal choice may increase risk Factors that may reduce risk or improve nutritional status Appropriately prescribed elimination diets Nutrition counseling Nutrition support and assessment during breast-feeding when maternal avoidance diet is required Appropriate choice of supplemental formulas (when formula feeding) and vitamin mineral supplements, when needed Nutrition assessment before commencing plant-based beverages Timely introduction of nutrient-dense complementary foods Biomarkers for vitamin mineral assessment Ideally only targeted nutritional biomarkers should be performed, following from assessment of dietary intake, the foods eliminated, and growth status. Core biochemical markers for food allergy include the bone profile with 25[OH] vitamin D, phosphate, iron profile including hemoglobin, mean corpuscular volume, hematocrit, ferritin, and C-reactive protein in the presence of failure-to-thrive zinc status. Other markers including vitamin A, vitamin B12, and folate may be useful in some patients, depending on the nutrition assessment. Growth assessment Weight, length or height, and head circumference (age <2 y) should be regularly assessed and plotted on the appropriate growth chart. Online z-score calculator may be used.4 Practical pointers for physicians Measure height, weight, head circumference (age <2 y) and plot on growth chart at every appointment to assess growth over time Timely referral to registered dietitian nutritionist for assessment of nutrient intake Timely referral for feeding therapy if concerns for feeding difficulties, refusal, or aversions Consider iron studies (including serum ferritin and C-reactive protein), 25[OH] vitamin D, and zinc in children with multiple food avoidance, picky eating, or food phobia Find a dietitian who can support your practice For food allergyetrained dietitians, consult the Food Allergy Research & Education Web site5 and Find a Nutrition Expert on eatright.org.6 Many dietitians provide telehealth. Dietitians are nationally accredited. Some states also have licensure for dietitians. Therefore, a dietitian can provide telehealth only when licensed in the state where the patient is located. However, many states do not have specific licensure restrictions, so any dietitian can provide telehealth services. If you practice in a state that has licensure restrictions, a dietitian may be willing to apply for licensure in your state to support your patients. VENTER ET AL J ALLERGY CLIN IMMUNOL PRACT VOLUME 12, NUMBER 3 581 TABLE II. Defining faltering growth and malnutrition (undernutrition)4 Terminology Faltering growth/failure to thrive Malnutrition, undernutrition Wasting Malnutrition, undernutrition Stunting Definition There is no consensus on the definition, but the most common one used is a sustained decrease in growth velocity, in which weight for age or weight for length/height falls by 2 major percentiles over time e2 to e2.9 z-score weight for height (moderate undernutrition) e3 and below z-score weight for height (severe undernutrition) e2 to e2.9 z-score height for age (moderate undernutrition) e3 and below z-score height for age (severe undernutrition) Malnutrition Middle to upper-arm circumference e2 to e2.9 z-score (moderate undernutrition) e3 and below z-score (severe undernutrition) The World Health Organization uses z-scores to define undernutrition as defined here. However, some authors refer to weight for height, weight for age, and height for age using percentiles. A z-score of 0 refers to the 50th percentile. Percentiles relating to other z-scores depend on the growth chart used. These z-scores are universally applicable irrespective of the growth chart used. foods, was associated with reduced longitudinal growth parameters (height and weight) (Table II) in four of six studies identified, irrespective of the type of FA involved.7 A UK growth survey on children with confirmed FA found that that avoiding three or more foods affected weight for age, but not the other growth parameters.8 However, a prospective study in children with a confirmed noneimmunoglobulin E-mediated food allergy (IgE-FA), also from the United Kingdom, found that the number of foods excluded did not affect growth. Nevertheless, assessing growth is an important aspect of all FA evaluations (Table I). Specific FA and growth parameters. Tuokkola et al9 reported on children with any form of allergy to cow’s milk (CM) and/or wheat, rye, and barley, who were assessed at 1, 3, and 5 years. They reported that avoiding CM led to lower height for age z-scores compared with a healthy control group. Medeiros et al10 reported that in a group of 26 children with any form of CM allergy (CMA), 11.5% were stunted (Table II), 7.7% were wasted, and 23% were underweight (e2 z-score weight for age) compared with 0%, 0%, and 3.3% in the control group, respectively. In another study that focused on any form of CMA, height for age was significantly lower in affected children compared with controls.11,12 In a retrospective study of 9,938 children with an electronic medical record code for FA, those avoiding CM were significantly shorter and weighed less than a matched control group without FA.13 Food allergies and nutrient intake Foods containing the top nine major food allergens are typically high-protein foods providing a range of nutrients (Table III).14 As nutrient requirements change over the course of the life span (Table IV), the effect of avoiding certain foods may also differ across various age groups.15 Data are inconsistent regarding the consequences of avoiding certain foods on overall nutrient intake and growth parameters. Some studies indicate a particular concern relating to CM avoidance in children up to age 16 years,9,16,17 supported by data that intake of baked CM products versus complete avoidance16 improves nutritional status. Studies reporting on nutrient intake, in which an RDN and appropriate nutrition interventions were in place, did not show an association between food avoidance and nutrient intake.8,18,19 Thus, although it is unclear whether multiple FAs affect growth, it is shown that avoiding multiple foods will affect dietary intake in the absence of nutrition intervention. Data support that CM-avoidant children12,13,16,20 in particular require dietary guidance to ensure adequate nutrition. The aim is to prevent nutritional deficiencies and growth impairment (Table I). Immunoglobulinemediated FA Immunoglobulin E-FA has been reported to affect growth in children. A Finnish study indicated that both height for age and weight for height were lower in children with IgE-FA (mainly CMA) compared with controls.21 This was supported by data from the United States indicating that more children with FA had lower height for age percentiles than children without FA.22 Other studies indicated low weight for height,23 low weight and height for age,17 and increased numbers of malnourished23 children with IgE-FA. NoneIgE mediated FA Several studies investigated the role of non-IgE mediated FA on growth. Studies from the United Kingdom reporting on nonIgE mediated FA in children indicated that 9% of children were stunted, 2.2% were wasted and 2.2% and 10% were overweight at age less than 5 and greater than 5 years, respectively.8 Another study from this group, mean age 27 months, with IgE-mediated FA, noneIgE mediated FA, and mixed IgE-mediated FA, reported that 11.5% were stunted and 3.7% were wasted.24 Vieira et al25 described that in a cohort of children from Brazil with gastrointestinal predominant CMA, 23.9% of children were stunted, 11.3% were wasted, and 15.1% were underweight. Food proteineinduced enterocolitis syndrome Children with food proteineinduced enterocolitis syndrome (FPIES) avoiding three or more foods26 have an increased risk for food aversion and poor weight gain. Although most children with FPIES react to a single food, some avoid additional foods prophylactically27 owing to parental concerns. In a large cohort of 410 children with FPIES, 69% avoided at least two food groups because of FPIES.28 The high psychosocial burden28,29 on caregivers can contribute to altered feeding practices, leading to the delayed development of feeding skills and reduced 582 VENTER ET AL J ALLERGY CLIN IMMUNOL PRACT MARCH 2024 TABLE III. Nutrients provided by food containing common food allergens Nutrients at risk Eliminated food Protein Carbohydrate Fat Milk Egg Wheat Soy Peanuts, tree nuts, and seeds Seafood Peanut x x x x x x x x x x x Fiber Calcium Vitamin D Vitamin B12 x x x x x x x Iodine Biotin Iron x x x x Omega -3 fatty acids x x x x x Folate x x x x x x x Reprinted with permission from Durban R, et al. Dietary management of food allergy. Immunol Allergy Clin North Am 2021;41:233-70.14 TABLE IV. Changes in food intake nutrient requirements over the life span Age group Infants and children Children Teenagers Increased nutritional requirements Energy, protein, essential fatty acids, >6 mo: iron, zinc iodinea Increased risk Delayed introduction of foods Cow’s milk allergy Multiple food allergies Family inability to manage food allergy Nursery inability to provide nutritious, safe foods Feeding difficulties Energy, protein, essential fatty acids, iron, calcium >4 y: zinc >9 y: iodine Food aversions/phobia Family inability to manage food allergy Nursery/preschool inability to provide nutritious, safe foods Energy, protein, calcium, phosphorus, magnesium, zinc, iodine Females: iron Longer-term food aversions Not consuming food allergen that have been outgrown Increased requirements with increased activity (sports) Family inability to manage food allergy School inability to provide nutritious safe foods Social events where safe food is unavailable aA risk for iodine deficiency has been found specifically in children with cow’s milk allergy. intake. Indeed, parents of children with FPIES reported greater feeding difficulty than did those with children with IgE-FA.30 They were also significantly more likely to report adverse impacts of feeding on the caregiver and family. Faltering growth can be a feature of chronic FPIES.31 Impaired absorption and excessive gastrointestinal losses can result from ongoing inflammation. Hematologic and metabolic disturbances can also be seen in chronic FPIES. The International Consensus Guidelines for the Diagnosis and Management of Food ProteineInduced Enterocolitis Syndrome32 recommend guidance during complementary food introduction to ensure nutritional adequacy. They also strongly recommend consulting with an RDN to facilitate complementary feeding. Eosinophilic esophagitis/eosinophilic gastrointestinal diseases Growth restriction can be seen in patients with eosinophilic gastrointestinal diseases, and faltering growth has been reported in 10% to 24% of patients with EoE.33 Impairments in growth result from a variety of factors. Recurrent gastrointestinal symptoms such as pain and vomiting prevent adequate nutritional intake. Eosinophilic esophagitis (EoE) can lead to feeding dysfunction34,35 because of dysphagia and/or esophageal strictures. Altered feeding behaviors such as EoE symptoms can also trigger anxiety and/or eating disorders (including food aversions).27,36,37 This may further contribute to nutritional inadequacy.27 Similar to FPIES, chronic inflammation in itself is a state that may lead to impairments in growth.38 IS ATOPIC DERMATITIS ASSOCIATED WITH GROWTH IMPAIRMENT? Associations between atopic dermatitis (AD) disease severity and growth have been reported, particularly in younger children.39 A Japanese birth cohort study40 found an association between impairment in growth parameters (height, weight, and body mass index) in children who had early-onset persistent AD. This association may occur for a variety of reasons. Dietary restrictions are often pursued by families of children with AD,41-43 but frequently without physician recommendation or RDN input.41,44 Unsupervised dietary manipulation can result in the lower intake of energy, protein, fat, and nutrients, leading to a negative impact on growth parameters. Children with AD can have sleep disturbances45 and insufficient sleep.45,46 Atopic dermatitis has been associated with impaired growth (height). A mechanism for this is interruption of growth hormone release owing to poor sleep.47 Early-onset AD is also a risk factor for FA, so the contribution of FA (or food avoidance) to growth in children with AD is uncertain. Severe AD can result in protein loss through the skin, and there are reports of hypoproteinemia48 as a complication of AD. Chronic skin inflammation49,50 and superinfection can also VENTER ET AL J ALLERGY CLIN IMMUNOL PRACT VOLUME 12, NUMBER 3 TABLE V. Avoidant/restrictive food intake disorder criteria56 Criteria Grade Significant weight loss (or failure to achieve expected weight gain or faltering growth in children) Significant nutritional deficiency Dependence on enteral feeding or oral nutritional supplements Marked interference with psychosocial functioning A1 A2 A3 A4 negatively affect systemic metabolism. Zinc is a cofactor for enzymes involved in energy metabolism and has a direct impact on growth through the pituitary growth hormoneeinsulin-like growth factor-1 axis, which is responsive to zinc status.51 A retrospective study on 189 children with AD, 30% of whom had concomitant FA, found that 25% of children had low zinc levels and concomitant severe AD.52 The latter study did not find an association among FA, the number of foods eliminated, and low zinc levels, suggesting a different cause for this. IS FOOD REFUSAL ASSOCIATED WITH FA? Food refusal is commonly reported in children with FA, ranging from aversions to breast-feeding or bottle feeding to the refusal of specific food texture characteristics, and to the more severe spectrum including avoidant restrictive food intake disorder (ARFID).53 Food refusal increases the risk for both macronutrient and micronutrient deficiencies,54 and these are more commonly reported in ARFID.55 This is partly due to Diagnostic and Statistical Manual of Mental Disorders diagnostic criteria (Table V), including the persistent failure to meet nutritional needs (Table I). Avoidant restrictive food intake disorder emerged as an eating disorder only in 2013; it coexists with other medical conditions.57 In the context of FA, case reports of ARFID started to emerge in EoE58,59 followed by a case series of patients aged 6 months to 18 years who presented to an FA clinic.60 During the 4-month recruitment period, 54 children were assessed, 34 of whom met Diagnostic and Statistical Manual of Mental Disorders criteria for A1-A3 and a proposed FAespecific criterion for A4.60 More research is needed on feeding issues in children along the spectrum of FA, to prevent food refusal and progression to ARFID and develop more specific management options. ARE MEDICATIONS USED IN FA ASSOCIATED WITH NUTRITIONAL RISK? Medication use Medications commonly prescribed for children with FA include antihistamines, corticosteroids, and epinephrine.2,61 For FPIES, common drugs include ondansetron,32 and for EoE treatment they can include proton pump inhibitors (PPIs), swallowed inhaled corticosteroids, and biologics such as dupilumab.62,63 Other forms of noneIgE mediated FA are treated according to the presenting symptoms and may include PPIs, corticosteroids, antihistamines, and immunosuppressive drugs such as cyclosporine or methotrexate for AD, although their use is less common since the approval of biologic therapies to treat moderate to severe AD.64,65 Corticosteroids in children with EoE. Despite concerns about potential effects on growth, a systematic review 583 concluded that the long-term use of swallowed inhaled corticosteroids was not associated with reduced growth or bone mineral density.66 Andreae et al67 showed that in a study with a mean follow-up of 20.4 months in which the longest followup was 68 months (5.7 years), swallowed fluticasone was not associated with growth impairment. This was also not highlighted as a concern by the Joint Task Force for the American Academy of Allergy, Asthma & Immunology, the American College of Allergy, Asthma and Immunology, and the American Gastroenterology Association in the EoE practice parameter.63 However, a systematic review reported that inhaled corticosteroids affected growth in children with persistent asthma, although the drug used and delivery device may have an impact on the effect seen on growth.68 Proton pump inhibitors. A systematic review on PPI treatment found that the long-term use of PPIs (more than 30 days)69,70 is associated with gut dysbiosis. Proton pump inhibitor effects on magnesium, calcium, iron, and sodium absorption need further clarification. Vitamin B12 absorption may be a particular concern in patients with acid-related diseases, particularly those who already have malnutrition.71 In addition, a study showed a negative association between chronic PPI use and bone mineral density classified as either within a year of the assessment or at the time of assessment.72 ARE SOCIAL DETERMINANTS OF HEALTH ASSOCIATED WITH NUTRITIONAL RISK IN CHILDREN WITH FA? The increasing prevalence of FA has been noted to affect underresourced marginalized populations disproportionately.73,74 Racial and socioeconomic disparities have similarly been noted in other aspects of FA care, including prevention,75,76 the presence of an epinephrine autoinjector prescription,77 increased rates of food-induced anaphylaxis,78 and decreased access to subspeciality care.78,79 Food insecurity is estimated to occur in 10.5% of US households, with higher disparities noted in households with children, in Black or Hispanic individuals, in those below the poverty threshold80 and in households with dietary restrictions such as FA.81 Similarly, because allergen-free foods are significantly more costly, lower socioeconomic status is associated with limited access to allergen-free foods,82 because many current federal nutrition programs do not incorporate the increase in cost for food-allergic families.83,84 A recent work group report from the American Academy of Allergy, Asthma & Immunology also indicated that the COVID-19 pandemic resulted in many more people facing food insecurity for the first time. The Latinx, Native American, and Black communities were disproportionately affected according to the survey.85 This disparity in access likely affects the nutritional status of the child owing to the lack of affordable, nutritious meals free of specific allergens.80 The lack of access to allergen-free meals has also been postulated to contribute to increased rates of accidental ingestions and hospital visits among those of lower socioeconomic status.83 The literature has demonstrated general nutritional disparities based on socioeconomic status.86 584 VENTER ET AL WHAT ARE MARKERS FOR NUTRITIONAL RISK AND ARE THERE SPECIFIC MARKERS FOR CHILDREN WITH FA THAT DIFFER FROM THOSE OF THE GENERAL PEDIATRIC POPULATION? The Child Nutrition Act of 1966 Section 17(b)87 clearly defines nutritional risk under five broad categories and includes detectable abnormal biochemical and anthropometrical measures that affect health and nutritionally related conditions that predispose persons to inadequate nutritional intake: detrimental or abnormal nutritional conditions detectable by biochemical or anthropometric measurements; other documented nutritionally related medical conditions; dietary deficiencies that impair or endanger health; conditions that directly affect the nutritional health of a person, such as alcoholism or drug abuse; and conditions that predispose persons to inadequate nutritional patterns or nutritionally related medical conditions, such as homelessness and migrancy. Growth in the child with FA can be disrupted by both physiologic and psychological factors, including the elimination of food allergens, which contribute essential nutrients. The availability of food alternatives and the psychological burden, which may lead to disrupted meal patterns, can have a role in nutrient delivery.21,88 Micronutrient deficiencies are linked to the elimination of specific foods (ie, CM) but also to a lack of nutritionally appropriate, allergen-free replacements and increased nutrient demand. There is increasing evidence indicating that comorbidities and ongoing chronic gut and skin inflammation affect growth, in particular height.21,39,89 Assessing growth Ideally, weight, length and height, and head circumference (age <2 years) measurements are accurately performed with each allergy evaluation to guide medical and dietary management.90 The frequency of growth assessment may require modification if faltering growth and/or malnutrition are present91 (Table I). Although these terms are often used interchangeably, they have different diagnostic criteria (Table II). Faltering growth is a decrease in the velocity of weight gain, which results in the child falling off the expected weight curve on the growth charts, as described in Table II, whereas malnutrition (or undernutrition) is primarily defined by a low weight for height (wasting) or a low height for age (stunting), as defined by the World Health Organization.92 Micronutrient intake Micronutrients are important cofactors for growth and general well-being (Table I). Children with FA have an increased risk for a variety of vitamin and mineral deficiencies.90 Four studies assessed nutrient intake compared with a healthy population and found that vitamins and/or minerals related to bone mineralization (ie, vitamin D, calcium, phosphate) in particular were lower in children with FA than in children without it.4 Boaventura et al93 assessed the dietary intake of children in Brazil with CMA versus children without it and found low serum levels of retinol and vitamin D in 25.9% and 70.3%, respectively, of children with CMA. Although this study did not assess the blood serum levels for vitamin D and retinol in the control group, a comparison with the published Brazilian general pediatric population indicated that vitamin A deficiency (based on retinol levels) in children aged less than 59 months was 17.9%94 and vitamin D deficiency in children ages less than 5 years was 4.3%,95 suggesting a higher prevalence of these deficiencies in J ALLERGY CLIN IMMUNOL PRACT MARCH 2024 children with CMA in Brazil. Calcium intake was significantly lower in the CMA group. Thomassen et al96 found that 58% of breast-fed infants with CMA had iodine deficiency, much higher than that reported in the general population. The most common vitamin and mineral deficiencies include vitamin D, calcium, iodine, iron, and zinc, but children with FA are at risk of developing deficiencies within the whole spectrum of micronutrients, as well as macronutrients such as essential fatty acids.96-99 Symptoms and medications need to be taken into account when considering nutritional biomarkers. In addition, health care professionals should be aware of the sensitivity and specificity of biomarkers and factors (ie, the acute inflammatory response when a child is unwell, kidney function) that can influence their accuracy100 (Table I). WHICH NUTRITION INTERVENTIONS IMPROVE NUTRITIONAL STATUS IN CHILDREN WITH FA? Nutrition counseling Berni Canani et al101 evaluated the impact of nutrition counseling on children with FA. The authors measured growth, dietary intake, and biomarkers of nutritional status in children with FA before and 6 months after nutrition counseling, including one session of counseling, and compared baseline measurements with those of children without FA. At baseline, energy and protein intakes were lower and wasting was more common (21% vs 3%; P < .001) in children with FA compared with children without FA. Six months after dietary counseling, total energy intake in children with FA was comparable to intake in those without FA at baseline. There was also a significant increase in iron, fiber, calcium, and zinc intake in children with FA after 6 months compared with baseline. Table VI lists alternative or common food sources of important nutrients that could be affected by elimination diets (Table I). Referral to an RDN, when available, for a comprehensive nutrition consultation (Tables VII and VIII) can improve dietary intake and growth101 and will support caregivers by developing an individualized plan to ensure the diet is safe and nutritionally adequate.102 Human milk Human milk (HM) is the ideal first food for infants. It contains essential nutrients for growth and development and nonessential components such as IgA and HM oligosaccharides known to support immune and gut microbial development.103 Both infant and maternal health benefit as a result of breastfeeding. Therefore all health care practitioners should encourage breast-feeding. The probability of IgE-mediated allergic reactions to food proteins in HM is low,104 and certain noneIgE mediated diseases such as FPIES are not commonly reported in infants exclusively fed HM.32 However, if an infant has immediate symptoms to HM after maternal ingestion of a specific food, or if the infant with noneIgE FA is symptomatic or not growing well, the suspected trigger food should be removed from the maternal diet for 2 to 4 weeks followed by a trial of reintroduction to determine whether symptoms recur. Maternal elimination diets are commonly prescribed for food proteineinduced allergic proctocolitis whose primary symptom is hematochezia, although a newer guideline105 suggests a wait and see approach when hematochezia is of short duration (<1 month), because it may be self-resolving. The risk of anemia and poor growth seems to be low in infants with ongoing mild VENTER ET AL J ALLERGY CLIN IMMUNOL PRACT VOLUME 12, NUMBER 3 585 TABLE VI. Food sources of important nutrients Nutrient Allergen Alternative sources Protein Calcium Milk, egg, fish, peanut, tree nuts, soy Milk Meat, poultry, seeds, legumes Fortified plant-based beverages, calcium-fortified tofu and other foods Marine algae oils, refined fish oil supplements and supplemented foods Fortified plant-based beverages, salmon, trout, fortified cereals, mushrooms exposed to ultraviolet light Iodized salt, seaweed Beef, poultry, enriched macaroni, long-grain rice, oats, beans Beef liver, beef, chicken, potato Long-chain polyunsaturated fatty acids Fatty fish Vitamin D Cow’s milk and fortified dairy products Iodine Selenium Milk, fish Brazil nut, fish, egg Choline Egg, soy, wheat germ, cod TABLE VII. Special factors to consider when assessing nutritional risk Areas of assessment to consider in breast-fed infant in the presence of poor growth Review the adequacy of the maternal diet, especially energy and protein intake Increased frequency and duration of infant feedings Feeding both breasts at each feeding If long infant sleeping duration, encourage expressing breast milk to maintain prolactin levels and milk volume Plan for appropriate introduction of solid foods (timely and nutritionally dense complementary foods) Follow country-specific guidance on nutrient intake and supplementation Dietary goals when transitioning a child from a suitable formula to a plantbased milk (all goals should be met) They eat a varied solid food diet with a variety of foods from each food group (protein foods, grains, and fruit/vegetables in addition to milk substitute). They get at least two-thirds of energy from the varied solid food diet. They consume 16 oz/500 mL milk substitute per day (this includes human milk, formula, and other dairy substitutes such as yogurt). They eat age-appropriate textures. They get enough energy, protein, fat, and micronutrients in the diet from solid foods and the available milk substitute. Complementary feeding goals Begin when the child is developmentally ready to eat, around age 6 mo (and not before age 4 mo) For breast-fed infants, nutrients of concern are iron, zinc, and protein. Recommend infant sources of iron and zinc such as iron-fortified cereal grains and pureed meats and beans, and recommend infant sources of protein such as pureed meat, fish, poultry, cooked egg, and infant-safe forms of nuts, seeds, and legumes Other nutrients of concern for all infants during complementary feeding include choline (egg, soy, meat, fish, and potato), potassium (fruits and vegetables), vitamin D (supplement per country-specific guidelines), and long-chain polyunsaturated fatty acids (fish and seeds such as flax and chia) food proteineinduced allergic proctocolitis when appropriately managed. Maternal elimination diets may burden the breastfeeding parent and may affect breast-feeding duration and infant and maternal health. Therefore they should be prescribed only when necessary. When breast-fed infants present with FA and maternal elimination diets are required, the maternal diet requires attention. A maternal diet low in energy and protein may affect HM volume and subsequently, infant growth.106 Maternal dietary intake of fatty acids is also a significant determinant of HM fatty acid levels, including essential long chain polyunsaturated fatty acids.107-109 Although some studies indicate that certain micronutrients in HM, such as iodine, B vitamins (B1, B2, B6, and B12), choline, vitamins A, C, and D, and selenium, are affected by maternal diet,109-113 a 2016 systematic review109 reported that most evidence of micronutrient content in HM is based on an indirect association with maternal diet. Specific micronutrient supplementation to a deficient maternal diet will rapidly replete deficient maternal stores. However, specialist advice is needed to choose the correct supplement specific for lactation and further tailoring may be needed for specific elimination diets (Table VII). Supporting breast-feeding and assessing the growth and nutrient intake of the infant are important steps at each primary care and allergy and immunology visit. In addition to assessing for allergic symptoms, a comprehensive breast-feeding assessment may help to address poor growth in the exclusively breast-fed infant. Improving growth in the exclusively breast-fed infant by addressing breast milk production can result in improved outcomes without the addition of supplemental formula.114 Formula feeding For children who are formula-fed, improvement in growth and nutritional status can occur with a change in the approach to feeding, such as initiating a hypoallergenic formula to substitute for intact CM-based formula. Improvement in growth and nutritional status occurs rapidly in infants with chronic FPIES or enteropathy whose feed is changed to remove the trigger food.32 In a randomized controlled trial comparing an extensively hydrolyzed formula (EHF)115 with a probiotic supplemented EHF, infants following a 6-month feeding of either formula had significant improvement in weight-for-age, length-for-age, and weight-for-length z-scores as well as restoration of a normal body mass index. There was no difference in growth parameters between the formulas.116 A 2020 systematic review117 of randomized controlled trials (15 trials in 18 publications) comparing EHF containing CM 586 VENTER ET AL TABLE VIII. What happens during a comprehensive nutrition consultation by a registered dietitian? Assessment Food- and nutrition-related history Current food and drink intake Nutrient intake compared with nutrient needs Feeding skills Anthropometrics and growth assessment Relevant biochemical data, medical tests, and procedures Relevant clinical history: medical, health, family, and social histories Nutrition diagnosis and intervention Identifying nutrition problems (diagnosis) and etiologies Developing individualized interventions to solve nutrition problems: food and nutrient delivery, counseling, education, coordination of care Developing a plan to meet macronutrient and micronutrient needs Monitoring Evaluate progress toward nutrition-related goals Food allergyespecific dietary counseling and education may include: Label reading and allergen labeling laws Understanding cross-contact Eating away from home Which foods to avoid Substitute foods; for instance, may advise on suitable infant formula, plant-based beverages, and vitamin and mineral supplementation Eating according to tolerance (ie, discussion about precautionary advisory labeling) Information about food allergen doses during and after oral immunotherapy proteins with other formulas suggested that all EHF formulas evaluated were well-tolerated by most children with CMA. Owing to the limited data available, the authors could not reach a conclusion about the benefit of one formula over another for improved growth parameters. They suggested the need for higher-quality studies to assess the safety and efficacy of EHF for managing CMA. Supplemental formulas or micronutrient supplements In a prospective observational study, Meyer et al8 recruited 130 children (median age 23.3 months) and prescribed a food elimination diet (94.8% CM elimination) for the diagnosis of suspected noneIgE mediated FA. At enrollment, 9% were stunted and 2.8% were wasted. Participants received elimination diet advice to address nutritional issues such as protein, energy, and essential vitamin and mineral intake. There was a statistically significant improvement in weight for age after the 4-week elimination diet. Height for age was also improved but did not reach statistical significance in the short follow up. Three-day food records indicated that energy in addition to protein intake, vitamin and/or mineral supplementation (VMS), and hypoallergenic formula intakes were positively associated with improved anthropometrics.8 The researchers further evaluated VMS in 110 children with FA, 32 of whom were taking VMS. Sixty percent of those who did not take a VMS had a low vitamin D intake, but low zinc, calcium, and selenium intake were also common. Of those taking supplements, many were either J ALLERGY CLIN IMMUNOL PRACT MARCH 2024 undersupplemented or oversupplemented. Children receiving hypoallergenic formulas were significantly (P ¼ .007) less likely to be receiving VMS than were those taking over the counter milk alternatives. The data indicated that even when using a hypoallergenic formula or taking a VMS, children with FA may not be meeting nutritional recommendations for specific nutrients, and nutritional assessment should be individualized to optimize dietary intake (Table III). To date, no specific guidelines have been published supporting health care professionals in the dietary management of faltering growth in children with FA. Therefore there has been a reliance on guidance for the general pediatric population. This includes the World Health Organization/Food and Agriculture Organization of the United Nations/United Nations University guidelines for catch-up growth and guidance for moderately malnourished children.94,118 The principle for optimal catch-up growth (defined at 70% lean mass and 30% fat mass) is to ensure that 8% to 12% of energy comes from protein. It has also been highlighted that whereas energy and protein consumption are critical, micronutrients are also essential for growth, including zinc, potassium, sodium, magnesium, and phosphate, and micronutrients are essential for the immune system (ie, vitamin D, vitamin A, folate). Meyer et al38 converted these guidelines in general pediatrics for clinical practice in FA, which may be useful for health care professionals working in this field. Therapies available for the dietary management of faltering growth include breast-feeding support, manipulation of hypoallergenic formulas, and sufficient complementary foods. Complementary foods Complementary feeding should begin around age 6 months (and not before age 4 months), once the infant is developmentally ready. They should follow country-specific guidance and encourage a diversity of foods to meet nutritional needs. For instance, the Dietary Guidelines for Americans 2020 to 2025119 highlights priority nutrients in this age group. Breast-fed infants beginning complementary feeding need especially nutrient-rich foods containing iron, zinc, and protein. Other nutrients of concern in older infants are vitamin D, choline, and potassium. Parents should be encouraged to introduce foods from all food groups that fit within country-specific recommendations, a family’s food culture, food preferences, and the budget. In the presence of faltering growth, complementary food (from age 6 months onward) can be useful in optimizing energy, protein, and micronutrient intake (Table VII). Cow’s milk allergy and milk substitutes. Children with CMA should have safe and nutritionally appropriate substitutes. The use of other mammalian milks (eg, goat, sheep) is not recommended for the management of CMA owing to a high level of cross-reactivity and nutritional concerns.120 Plant-based beverages are often nutritionally inadequate to support normal growth and development compared with infant formulas or breast milk. These beverages are not suitable for children aged less than 1 year and may not be suitable in children aged 1 to 2 years (Table VII). Inappropriate milk substitutes can lead to poor growth, severe growth deficiency disorders, and, in rare cases, kwashiorkor/ marasmus, electrolyte disorders, kidney stones, and severe nutrient deficiencies including iron deficiency anemia, rickets, and scurvy.8,121-123 J ALLERGY CLIN IMMUNOL PRACT VOLUME 12, NUMBER 3 Plant-based beverages include soy, coconut, almond, rice, oat, hazelnut, cashew, walnut, pea, sesame, hemp, tiger nut, and quinoa. These beverages differ in terms of nutritional composition and characteristics. In general, soy and pea protein beverages contain protein quantities comparable to those of CM and may contain comparable calcium and vitamin D when adequately fortified, but they may be lower in fat and other micronutrients. Most other forms of plant-based beverages are inappropriate replacements for CM in toddlers and young children for whom milk remains an important part of the diet.124 For children aged greater than 1 year, continued feeding with HM or nutritionally complete substitute formula may be beneficial, alongside a varied solid food diet, because plant-based beverages may still be nutritionally inappropriate. The North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition124 suggests that when HM or infant or toddler formula constitutes a substantial source of otherwise absent or reduced nutrients in the child’s restricted diet, plant-based beverages may be inappropriate. Therefore, the use of plant-based beverages may be considered only on an individual basis after age 1 year in children who meet specific dietary goals14 (Table VII). For children who do not yet meet all of these dietary goals, clinicians may encourage continued breast-feeding or nutritionally complete formula while providing nutrition counseling to meet age-appropriate nutrition goals before transitioning to plant-based beverages (Table VII). Based on clinical need, these plant-based alternatives may be used in toddlers aged greater than 2 years who are eating well.125 SUMMARY AND CONCLUSIONS Food allergies are a growing public health concern that affects dietary intake. It is important to support nutritional needs and quality of life in patients with FA. Nutrition care is especially important for infants and young children because inadequate nutritional intake can directly affect growth and development. Clinicians should assess growth in children with FA as indicated by national guidelines and be aware of the indicators of nutritional risk (Tables I, VII, and VIII). Food allergy teams would benefit from including an RDN with additional training and/or experience in managing FA, because the complexity of management is ever-evolving and stretches beyond avoiding the allergen.126 Further research is needed to determine the impact of emerging FA therapies on nutritional status. Acknowledgments C. Venter, M. Groetch, R. Meyer, and J. Wang initiated the paper. All authors drafted the first version of different aspects of the paper. All authors reviewed and commented on various drafts of the paper. REFERENCES 1. Boyce JA, Assa’ad A, Burks AW, Jones SM, Sampson HA, Wood RA, et al. Guidelines for the diagnosis and management of food allergy in the United States: summary of the NIAID-Sponsored Expert Panel Report. Nutrition 2011;27:253-67. 2. Muraro A, de Silva D, Halken S, Worm M, Khaleva E, Arasi S, et al. Managing food allergy: GA2LEN guideline 2022. World Allergy Organ J 2022;15: 100687. 3. Muraro A, Werfel T, Hoffmann-Sommergruber K, Roberts G, Beyer K, Bindslev-Jensen C, et al. EAACI food allergy and anaphylaxis guidelines: diagnosis and management of food allergy. Allergy 2014;69:1008-25. 4. Calculator.net. Accessed January 29, 2024. https://www.calculator.net/z-scorecalculator.html VENTER ET AL 587 5. Food Allergy Research & Education. FARE trained registered dietitians. Accessed January 29, 2024. https://www.foodallergy.org/resources/fare-train ed-registered-dietitians 6. EatRight.org. Fina a nutrition expert. Accessed January 29, 2024. https://www. eatright.org/find-a-nutrition-expert 7. Sova C, Feuling MB, Baumler M, Gleason L, Tam JS, Zafra H, et al. Systematic review of nutrient intake and growth in children with multiple IgEmediated food allergies. Nutr Clin Pract 2013;28:669-75. 8. Meyer R, De Koker C, Dziubak R, Godwin H, Dominguez-Ortega G, Chebar Lozinsky A, et al. The impact of the elimination diet on growth and nutrient intake in children with food protein induced gastrointestinal allergies. Clin Transl Allergy 2016;6:25. 9. Tuokkola J, Luukkainen P, Nevalainen J, Ahonen S, Toppari J, Ilonen J, et al. Eliminating cows’ milk, but not wheat, barley or rye, increases the risk of growth deceleration and nutritional inadequacies. Acta Paediatr 2017;106:1142-9. 10. Medeiros LC, Speridião PG, Sdepanian VL, Fagundes-Neto U, Morais MB. Nutrient intake and nutritional status of children following a diet free from cow’s milk and cow’s milk by-products [in Portuguese]. J Pediatr (Rio J) 2004; 80:363-70. 11. Jensen VB, Jørgensen IM, Rasmussen KB, Mølgaard C, Prahl P. Bone mineral status in children with cow milk allergy. Pediatr Allergy Immunol 2004;15:562-5. 12. Sinai T, Goldberg MR, Nachshon L, Amitzur-Levy R, Yichie T, Katz Y, et al. reduced final height and inadequate nutritional intake in cow’s milk-allergic young adults. J Allergy Clin Immunol Pract 2019;7:509-15. 13. Mehta H, Ramesh M, Feuille E, Groetch M, Wang J. Growth comparison in children with and without food allergies in 2 different demographic populations. J Pediatr 2014;165:842-8. 14. Durban R, Groetch M, Meyer R, Coleman Collins S, Elverson W, Friebert A, et al. Dietary management of food allergy. Immunol Allergy Clin North Am 2021;41:233-70. 15. Groetch MV, Venter C. Nutritional management of food allergies. J Food Allergy 2020;2:11. 16. Mehta P, Furuta GT, Brennan T, Henry ML, Maune NC, Sundaram SS, et al. Nutritional state and feeding behaviors of children with eosinophilic esophagitis and gastroesophageal reflux disease. J Pediatr Gastroenterol Nutr 2018; 66:603-8. 17. Robbins KA, Guerrerio AL, Hauck SA, Henry BJ, Keet CA, Brereton NH, et al. Growth and nutrition in children with food allergy requiring amino acidbased nutritional formulas. J Allergy Clin Immunol 2014;134:1463-1466.e5. 18. Meyer R, De Koker C, Dziubak R, Venter C, Dominguez-Ortega G, Cutts R, et al. Malnutrition in children with food allergies in the UK. J Hum Nutr Diet 2014;27:227-35. 19. Berry MJ, Adams J, Voutilainen H, Feustel PJ, Celestin J, Jarvinen KM. Impact of elimination diets on growth and nutritional status in children with multiple food allergies. Pediatr Allergy Immunol 2015;26:133-8. 20. Meyer R, Wright K, Vieira MC, Chong KW, Chatchatee P, Vlieg-Boarstra BJ, et al. International survey on growth indices and impacting factors in children with food allergies. J Hum Nutr Diet 2019;32:175-84. 21. Isolauri E, Sutas Y, Salo MK, Isosomppi R, Kaila M. Elimination diet in cow’s milk allergy: risk for impaired growth in young children. J Pediatr 1998;132: 1004-9. 22. Christie L, Hine RJ, Parker JG, Burks W. Food allergies in children affect nutrient intake and growth. J Am Diet Assoc 2002;102:1648-51. 23. Flammarion S, Santos C, Guimber D, Jouannic L, Thumerelle C, Gottrand F, et al. Diet and nutritional status of children with food allergies. Pediatr Allergy Immunol 2011;22:161-5. 24. Meyer R, Rommel N, Van Oudenhove L, Fleming C, Dziubak R, Shah N. Feeding difficulties in children with food protein-induced gastrointestinal allergies. J Gastroenterol Hepatol 2014;29:1764-9. 25. Vieira MC, Morais MB, Spolidoro JV, Toporovski MS, Cardoso AL, Araujo GT, et al. A survey on clinical presentation and nutritional status of infants with suspected cow’ milk allergy. BMC Pediatr 2010;10:25. 26. Venter C, Sommer I, Moonesinghe H, Grundy J, Glasbey G, Patil V, et al. Health-related quality of life in children with perceived and diagnosed food hypersensitivity. Pediatr Allergy Immunol 2015;26:126-32. 27. Groetch M, Baker MG, Durban R, Meyer R, Venter C, Muraro A. The practical dietary management of food protein-induced enterocolitis syndrome. Ann Allergy Asthma Immunol 2021;127:28-35. 28. Maciag MC, Bartnikas LM, Sicherer SH, Herbert LJ, Young MC, Matney F, et al. A slice of food protein-induced enterocolitis syndrome (FPIES): insights from 441 children with FPIES as provided by caregivers in the International FPIES Association. J Allergy Clin Immunol Pract 2020;8:1702-9. 29. Su KW, Patil SU, Stockbridge JL, Martin VM, Virkud YV, Huang J-L, et al. Food aversion and poor weight gain in food protein-induced enterocolitis 588 VENTER ET AL syndrome: a retrospective study. J Allergy Clin Immunol 2020;145: 1430-1437.e11. 30. Flom JD, Groetch M, Kovtun K, Westcott-Chavez A, Schultz F, NowakWegrzyn A. Feeding difficulties in children with food protein-induced enterocolitis syndrome. J Allergy Clin Immunol Pract 2023;11: 2939-2941.e3. 31. Blackman AC, Anvari S, Davis CM, Anagnostou A. Emerging triggers of food protein-induced enterocolitis syndrome: lessons from a pediatric cohort of 74 children in the United States. Annals Allergy Asthma Immunol 2019;122: 407-11. 32. Nowak-Wegrzyn A, Chehade M, Groetch ME, Spergel JM, Wood RA, Allen K, et al. International consensus guidelines for the diagnosis and management of food protein-induced enterocolitis syndrome: executive summaryWorkgroup Report of the Adverse Reactions to Foods Committee, American Academy of Allergy, Asthma & Immunology. J Allergy Clin Immunol 2017; 139:1111-1126.e4. 33. Votto M, De Filippo M, Olivero F, Raffaele A, Cereda E, De Amici M, et al. Malnutrition in eosinophilic gastrointestinal disorders. Nutrients 2020;13:128. 34. Wu YP, Franciosi JP, Rothenberg ME, Hommel KA. Behavioral feeding problems and parenting stress in eosinophilic gastrointestinal disorders in children. Pediatr Allergy Immunol 2012;23:730-5. 35. Mukkada VA, Haas A, Maune NC, Capocelli KE, Henry M, Gilman N, et al. Feeding dysfunction in children with eosinophilic gastrointestinal diseases. Pediatrics 2010;126:e672-7. 36. Röjler L, Garber JJ, Butwicka A, Roelstraete B, Ludvigsson JF. Individuals with eosinophilic esophagitis are at greater risk of later psychiatric disorder. Am J Gastroenterol 2022;117:1046-55. 37. Reed CC, Ketchem CJ, Miller TL, Dellon ES. Psychiatric comorbidities are highly prevalent in nonesophageal eosinophilic gastrointestinal diseases. Clin Gastroenterol Hepatol 2022;20:e664-70. 38. Meyer R, Venter C, Fox AT, Shah N. Practical dietary management of protein energy malnutrition in young children with cow’s milk protein allergy. Pediatr Allergy Immunol 2012;23:307-14. 39. Beck C, Koplin J, Dharmage S, Wake M, Gurrin L, McWilliam V, et al. Persistent food allergy and food allergy coexistent with eczema is associated with reduced growth in the first 4 years of life. J Allergy Clin Immunol Pract 2016;4:248-56. 40. Yamamoto-Hanada K, Suzuki Y, Yang L, Saito-Abe M, Sato M, Mezawa H, et al. Persistent eczema leads to both impaired growth and food allergy: JECS birth cohort. PLoS One 2021;16:e0260447. 41. Johnston GA, Bilbao RM, Graham-Brown RA. The use of dietary manipulation by parents of children with atopic dermatitis. Br J Dermatol 2004;150: 1186-9. 42. Webber SA, Graham-Brown RA, Hutchinson PE, Burns DA. Dietary manipulation in childhood atopic dermatitis. Br J Dermatol 1989;121:91-8. 43. Sinagra JL, Bordignon V, Ferraro C, Cristaudo A, Di Rocco M, Amorosi B, et al. Unnecessary milk elimination diets in children with atopic dermatitis. Pediatr Dermatol 2007;24:1-6. 44. Eigenmann PA, Beyer K, Lack G, Muraro A, Ong PY, Sicherer SH, et al. Are avoidance diets still warranted in children with atopic dermatitis? Pediatr Allergy Immunol 2020;31:19-26. 45. Ramirez FD, Chen S, Langan SM, Prather AA, McCulloch CE, Kidd SA, et al. Association of atopic dermatitis with sleep quality in children. JAMA Pediatr 2019;173:e190025. 46. Silverberg JI, Paller AS. Association between eczema and stature in 9 US population-based studies. JAMA Dermatol 2015;151:401-9. 47. David TJ, Ferguson AP, Newton RW. Nocturnal growth hormone release in children with short stature and atopic dermatitis. Acta Derm Venereol 1991;71: 229-31. 48. Nomura I, Katsunuma T, Tomikawa M, Shibata A, Kawahara H, Ohya Y, et al. Hypoproteinemia in severe childhood atopic dermatitis: a serious complication. Pediatr Allergy Immunol 2002;13:287-94. 49. Brunner PM, He H, Pavel AB, Czarnowicki T, Lefferdink R, Erickson T, et al. The blood proteomic signature of early-onset pediatric atopic dermatitis shows systemic inflammation and is distinct from adult long-standing disease. J Am Acad Dermatol 2019;81:510-9. 50. Furue M, Kadono T. "Inflammatory skin march" in atopic dermatitis and psoriasis. Inflamm Res 2017;66:833-42. 51. MacDonald RS. The role of zinc in growth and cell proliferation. J Nutr 2000; 130(5 suppl):1500S-8S. 52. Ehlayel MS, Bener A. Risk factors of zinc deficiency in children with atopic dermatitis. Eur Ann Allergy Clin Immunol 2020;52:18-22. 53. Meyer R. Nutritional disorders resulting from food allergy in children. Pediatr Allergy Immunol 2018;29:689-704. J ALLERGY CLIN IMMUNOL PRACT MARCH 2024 54. Chehade M, Meyer R, Beauregard A. Feeding difficulties in children with nonIgE mediated food allergic gastrointestinal disorders. Ann Allergy Asthma Immunol 2019;122:603-9. 55. Schmidt R, Hiemisch A, Kiess W, von Klitzing K, Schlensog-Schuster F, Hilbert A. Macro- and micronutrient intake in children with avoidant/restrictive food intake disorder. Nutrients 2021;13:400. 56. National Institutes of Health. DSM-5 changes: implications for child serious emotional disturbance. Accessed January 29, 2024. https://www.ncbi.nlm.nih. gov/books/NBK519712/table/ch3.t18/ 57. Fisher MM, Rosen DS, Ornstein RM, Mammel KA, Katzman DK, Rome ES, et al. Characteristics of avoidant/restrictive food intake disorder in children and adolescents: a "new disorder" in DSM-5. J Adolesc Health 2014;55:49-52. 58. Robson J, Laborda T, Fitzgerald S, Andersen J, Peterson K, O’Gorman M, et al. Avoidant/restrictive food intake disorder in diet-treated children with eosinophilic esophagitis. J Pediatr Gastroenterol Nutr 2019;69:57-60. 59. Eddy KT, Thomas JJ, Hastings E, Edkins K, Lamont E, Nevins CM, et al. Prevalence of DSM-5 avoidant/restrictive food intake disorder in a pediatric gastroenterology healthcare network. Int J Eat Disord 2015;48:464-70. 60. Patrawala MM, Vickery BP, Proctor KB, Scahill L, Stubbs KH, Sharp WG. Avoidant-restrictive food intake disorder (ARFID): a treatable complication of food allergy. J Allergy Clin Immunol Pract 2022;10:326-328.e2. 61. Zuberbier T, Wood RA, Bindslev-Jensen C, Fiocchi A, Chinthrajah RS, Worm M, et al. Omalizumab in IgE-mediated food allergy: a systematic review and meta-analysis. J Allergy Clin Immunol Pract 2023;11:1134-46. 62. Aceves SS, Dellon ES, Greenhawt M, Hirano I, Liacouras CA, Spergel JM. Clinical guidance for the use of dupilumab in eosinophilic esophagitis: a yardstick. Ann Allergy Asthma Immunol 2023;130:371-8. 63. Rank MA, Sharaf RN, Furuta GT, Aceves SS, Greenhawt M, Spergel JM, et al. Technical review on the management of eosinophilic esophagitis: a report From the AGA Institute and the Joint Task Force on Allergy-Immunology Practice Parameters. Gastroenterology 2020;158:1789-1810.e15. 64. Meyer R, Fleming C, Dominguez-Ortega G, Lindley K, Michaelis L, Thapar N, et al. Manifestations of food protein induced gastrointestinal allergies presenting to a single tertiary paediatric gastroenterology unit. World Allergy Organ J 2013;6:13. 65. Boguniewicz M, Fonacier L, Guttman-Yassky E, Ong PY, Silverberg JI. Atopic dermatitis yardstick update. Ann Allergy Asthma Immunol 2023;130:811-20. 66. Philpott H, Dougherty MK, Reed CC, Caldwell M, Kirk D, Torpy DJ, et al. Systematic review: adrenal insufficiency secondary to swallowed topical corticosteroids in eosinophilic oesophagitis. Aliment Pharmacol Ther 2018;47: 1071-8. 67. Andreae DA, Hanna MG, Magid MS, Malerba S, Andreae MH, Bagiella E, et al. Swallowed fluticasone propionate is an effective long-term maintenance therapy for children with eosinophilic esophagitis. Am J Gastroenterol 2016; 111:1187-97. 68. Axelsson I, Naumburg E, Prietsch SO, Zhang L. Inhaled corticosteroids in children with persistent asthma: effects of different drugs and delivery devices on growth. Cochrane Database Syst Rev 2019;6:Cd010126. 69. Hopkins AM, Badaoui S, Kichenadasse G, Karapetis CS, McKinnon RA, Rowland A, et al. Efficacy of atezolizumab in patients with advanced NSCLC receiving concomitant antibiotic or proton pump inhibitor treatment: pooled analysis of five randomized control trials. J Thorac Oncol 2022;17:758-67. 70. Castellana C, Pecere S, Furnari M, Telese A, Matteo MV, Haidry R, et al. Side effects of long-term use of proton pump inhibitors: practical considerations. Pol Arch Intern Med 2021;131:541-9. 71. Scarpignato C, Gatta L, Zullo A, Blandizzi C. Effective and safe proton pump inhibitor therapy in acid-related diseases - a position paper addressing benefits and potential harms of acid suppression. BMC Med 2016;14:179. 72. Henderson AF, Khan SM, Hornung LN, Mukkada VA, Kalkwarf HJ. Prevalence and predictors of compromised bone mineral density in pediatric eosinophilic esophagitis. J Pediatr Gastroenterol Nutr 2020;71:764-70. 73. Gupta RS, Warren CM, Smith BM, Blumenstock JA, Jiang J, Davis MM, et al. The public health impact of parent-reported childhood food allergies in the United States. Pediatrics 2018;142:e20181235. 74. Keet CA, Savage JH, Seopaul S, Peng RD, Wood RA, Matsui EC. Temporal trends and racial/ethnic disparity in self-reported pediatric food allergy in the United States. Ann Allergy Asthma Immunol 2014;112:222-229.e3. 75. Brewer AG, Jiang J, Warren CM, et al. Racial differences in timing of food allergen introduction. J Allergy Clin Immunol Pract 2022;10:329-332.e2. 76. Dupuis R, Phipatanakul W, Bartnikas LM. Social disparities in early childhood prevention and management of food allergy. J Allergy Clin Immunol 2023; 151:37-41. J ALLERGY CLIN IMMUNOL PRACT VOLUME 12, NUMBER 3 77. Coombs R, Simons E, Foty RG, Stieb DM, Dell SD. Socioeconomic factors and epinephrine prescription in children with peanut allergy. Paediatr Child Health 2011;16:341-4. 78. Mahdavinia M, Fox SR, Smith BM, James C, Palmisano EL, Mohammed A, et al. Racial differences in food allergy phenotype and health care utilization among US children. J Allergy Clin Immunol Pract 2017;5:352-357.e1. 79. Kanaley MK, Dyer AA, Negris OR, Fierstein JL, Ciaccio CE, Gupta RS, et al. Guideline-informed care among Medicaid-enrolled children with food allergy. Am J Manag Care 2020;26:505-12. 80. Tepler E, Wong KH, Soffer GK. Health disparities in pediatric food allergy. Ann Allergy Asthma Immunol 2022;129:417-23. 81. Guillaume JD, Jagai JS, Makelarski JA, Abramsohn EM, Tessler Lindau S, Verma R, et al. COVID-19-related food insecurity among households with dietary restrictions: a national survey. J Allergy Clin Immunol Pract 2021;9: 3323-3330.e3. 82. Coleman AT, Sharma H, Robinson A, Pappalardo AA, Vincent E, Fierstein JL, et al. Access to allergen-free food among Black and White children with food allergy in the FORWARD study. J Allergy Clin Immunol Pract 2022;10:182-8. 83. Brown E, Das R, Brewer AG, Martinez E, Bilaver LA, Gupta RS. Food insecure and allergic in a pandemic: a vulnerable population. J Allergy Clin Immunol Pract 2020;8:2149-51. 84. Scurlock AM, Brown E, Davis CM. Food insecurity in children and adults with food allergies. Ann Allergy Asthma Immunol 2022;129:424-9. 85. Shroba J, Das R, Bilaver L, Vincent E, Brown E, Polk B, et al. Food insecurity in the food allergic population: a work group report of the AAAAI Adverse Reactions to Foods Committee. J Allergy Clin Immunol Pract 2022;10:81-90. 86. Perez-Escamilla R, Bermudez O, Buccini GS, Kumanyika S, Lutter CK, Monsivais P, et al. Nutrition disparities and the global burden of malnutrition. BMJ 2018;361:k2252. 87. Child Nutrition Act of 1966. Accessed January 29, 2024. https://www.govinfo. gov/content/pkg/COMPS-10328/pdf/COMPS-10328.pdf 88. Stark CM, Nylund CM. Side effects and complications of proton pump inhibitors: a pediatric perspective. J Pediatr 2016;168:16-22. 89. Niewiem M, Grzybowska-Chlebowczyk U. Intestinal barrier permeability in allergic diseases. Nutrients 2022;14:1893. 90. American Academy of Pediatrics. Recommendations for preventive pediatric health care. Accessed January 29, 2024. https://downloads.aap.org/AAP/PDF/ periodicity_schedule.pdf 91. Golden MH. Proposed recommended nutrient densities for moderately malnourished children. Food Nutr Bull 2009;30(3 suppl):S267-342. 92. World Health Organization. Global database on child growth and malnutrition: child growth indicators and their interpretation. Accessed January 29, 2024. http://www.who.int/nutgrowthdb/about/introduction/en/index2.html 93. Boaventura RM, Mendonca RB, Fonseca FA, Mallozi M, Souza FS, Sarni ROS. Nutritional status and food intake of children with cow’s milk allergy. Allergol Immunopathol (Madr) 2019;47:544-50. 94. Lima DB, Damiani LP, Fujimori E. Vitamin A deficiency in Brazilian children and associated variables. Rev Paul Pediatr 2018;36:176-85. 95. Normando P, de Castro IRR, Bezerra FF, Berti TL, Bertoni N, de Aquino Lacerda EM, et al. Prevalence and predictors of vitamin D insufficiency in Brazilian children under 5 years of age: Brazilian National Survey on Child Nutrition (ENANI-2019). Br J Nutr 2024;131:312-20. 96. Thomassen RA, Kvammen JA, Eskerud MB, Juliusson PB, Henriksen C, Rugtveit J. Iodine status and growth in 0-2-year-old infants with cow’s milk protein allergy. J Pediatr Gastroenterol Nutr 2017;64:806-11. 97. Aldamiz-Echevarria L, Bilbao A, Andrade F, Elorz J, Prieto JA, RodriguezSoriano J. Fatty acid deficiency profile in children with food allergy managed with elimination diets. Acta Paediatr 2008;97:1572-6. 98. Noimark L, Cox HE. Nutritional problems related to food allergy in childhood. Pediatr Allergy Immunol 2008;19:188-95. 99. Ojuawo A, Lindley KJ, Milla PJ. Serum zinc, selenium and copper concentration in children with allergic colitis. East Afr Med J 1996;73:236-8. 100. Gerasimidis K, Bronsky J, Catchpole A, Embleton N, Fewtrell M, Hojsak I, et al. Assessment and interpretation of vitamin and trace element status in sick children: a position paper from the European Society for Paediatric Gastroenterology Hepatology, and Nutrition Committee on Nutrition. J Pediatr Gastroenterol Nutr 2020;70:873-81. 101. Berni Canani R, Leone L, D’Auria E, Riva E, Nocerino R, Ruotolo S, et al. The effects of dietary counseling on children with food allergy: a prospective, multicenter intervention study. J Acad Nutr Diet 2014;114:1432-9. 102. MacKenzie H, Grundy J, Glasbey G, Dean T, Venter C. Information and support from dietary consultation for mothers of children with food allergies. Ann Allergy Asthma Immunol 2015;114:23-9. VENTER ET AL 589 103. Davis EC, Castagna VP, Sela DA, Hillard MA, Lindberg S, Mantis NJ, et al. Gut microbiome and breast-feeding: implications for early immune development. J Allergy Clin Immunol 2022;150:523-34. 104. Gamirova A, Berbenyuk A, Levina D, Peshko D, Simpson MR, Azad MB, et al. Food proteins in human breast milk and probability of IgE-mediated allergic reaction in children during breastfeeding: a systematic review. J Allergy Clin Immunol Pract 2022;10:1312-1324.e8. 105. Mennini M, Fiocchi AG, Cafarotti A, Montesano M, Mauro A, Villa MP, et al. Food protein-induced allergic proctocolitis in infants: literature review and proposal of a management protocol. World Allergy Organ J 2020;13: 100471. 106. Reinhardt MC, Lauber E. Maternal diet, breast feeding and infants’ growth. A field study in the Ivory Coast (West Africa). J Trop Pediatr 1981;27: 229-36. 107. Bzikowska-Jura A, Czerwonogrodzka-Senczyna A, Jasinska-Melon E, Mojska H, Olędzka G, Wesołowska A, et al. The concentration of omega-3 fatty acids in human milk is related to their habitual but not current intake. Nutrients 2019;11:1585. 108. Zielinska-Pukos MA, Brys J, Wesolowska A, Hamulka J. Breastmilk PUFA strongly associated with maternal dietary intake but not anthropometric parameters and breastmilk carotenoids. Prostaglandins Leukot Essent Fatty Acids 2022;186:102505. 109. Bravi F, Wiens F, Decarli A, Dal Pont A, Agostoni C, Ferraroni M. Impact of maternal nutrition on breast-milk composition: a systematic review. Am J Clin Nutr 2016;104:646-62. 110. Kominiarek MA, Rajan P. Nutrition recommendations in pregnancy and lactation. Med Clin North Am 2016;100:1199-215. 111. Copp K, DeFranco EA, Kleiman J, Rogers LK, Morrow AL, Valentine CJ. Nutrition support team guide to maternal diet for the human-milk-fed infant. Nutr Clin Pract 2018;33:687-93. 112. Allen LH. B vitamins in breast milk: relative importance of maternal status and intake, and effects on infant status and function. Adv Nutr 2012;3:362-9. 113. Perrin MT, Pawlak R, Judd N, Cooper J, Donati GL. Major and trace mineral composition of milk from lactating women following vegan, vegetarian, and omnivore diets. Br J Nutr 2023;130:1005-12. 114. Spatz DL, Conover NM. Case report: managing growth failure while maintaining exclusive breastfeeding. J Pediatr Nurs 2021;61:47-50. 115. Asai Y, Yanishevsky Y, Clarke A, La Vieille S, Delaney JS, Alizadehfar R, et al. Rate, triggers, severity and management of anaphylaxis in adults treated in a Canadian emergency department. Int Arch Allergy Immunol 2014;164:246-52. 116. Dupont C, Hol J, Nieuwenhuis EE. Cow’s Milk Allergy Modified by Elimination and Lactobacilli study group. An extensively hydrolysed casein-based formula for infants with cows’ milk protein allergy: tolerance/hypoallergenicity and growth catch-up. Br J Nutr 2015;113:1102-12. 117. Stró_zyk A, Horvath A, Meyer R, Szajewska H. Efficacy and safety of hydrolyzed formulas for cow’s milk allergy management: a systematic review of randomized controlled trials. Clin Exp Allergy 2020;50:766-79. 118. WHO/FAO/UNU. Protein and Amino Acid Requirements in Human Nutrition: Joint WHO/FAO/UNU Expert Consultation. Geneva, Switzerland: WHO Technical Report Series No. 935, WHO; 2007. Accessed January 29, 2024. http://apps. who.int/iris/bitstream/1066543411/1/WHO_TRS_935_eng.pdf?ua¼1 119. US Department of Agriculture and US Department of Health and Human Services. Dietary Guidelines for Americans, 2020-2025. Washington, DC: U.S. Department of Agriculture; 2020. 120. Järvinen KM, Chatchatee P. Mammalian milk allergy: clinical suspicion, crossreactivities and diagnosis. Curr Opin Allergy Clin Immunol 2009;9:251-8. 121. Agostoni C, Terracciano L, Varin E, Fiocchi A. The nutritional value of protein-hydrolyzed formulae. Crit Rev Food Sci Nutr 2016;56:65-9. 122. Maslin K, Oliver EM, Scally KS, Atkinson J, Foote K, Venter C, et al. Nutritional adequacy of a cows’ milk exclusion diet in infancy. Clin Transl Allergy 2016;6:20. 123. Nachshon L, Goldberg MR, Schwartz N, Sinai T, Amitzur-Levy R, Elizur A, et al. Decreased bone mineral density in young adult IgE-mediated cow’s milkallergic patients. J Allergy Clin Immunol 2014;134:1108-1113.e3. 124. Merritt RJ, Fleet SE, Fifi A, Jump C, Schwartz S, Sentongo T, et al. North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition Position Paper: plant-based milks. J Pediatr Gastroenterol Nutr 2020;71:276-81. 125. Fiocchi A, Bognanni A, Bro_zek J, Ebisawa M, Schünemann H, WAO DRACMA guideline group. World Allergy Organization (WAO) Diagnosis and Rationale for Action against Cow’s Milk Allergy (DRACMA) Guidelines. Pediatr Allergy Immunol 2010;21(suppl 21):1-125. 126. Venter C, Groetch M, Netting M, Meyer R. A patient-specific approach to develop an exclusion diet to manage food allergy in infants and children. Clin Exp Allergy 2018;48:121-37.
Anuncio
Documentos relacionados
Descargar
Anuncio
Añadir este documento a la recogida (s)
Puede agregar este documento a su colección de estudio (s)
Iniciar sesión Disponible sólo para usuarios autorizadosAñadir a este documento guardado
Puede agregar este documento a su lista guardada
Iniciar sesión Disponible sólo para usuarios autorizados