Fecal Occult Blood & Colonoscopy Need in Familial CRC Risk
Anuncio

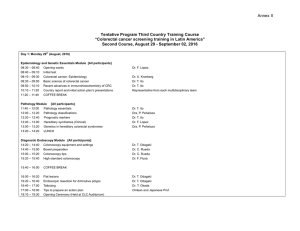
Alimentary Pharmacology & Therapeutics Can quantification of faecal occult blood predetermine the need for colonoscopy in patients at risk for non-syndromic familial colorectal cancer? Z. LEVI*, P. ROZEN* , à, R. HAZAZI*, A. VILKIN*, A. WAKED*, E. MAOZ , S. BIRKENFELD *Gastroenterology Department, Rabin Medical Center, Beilinson Hospital, Petach Tikva; Gastroenterology Units, Clalit Health Services, Tel Aviv; àTel Aviv University Medical School, Tel Aviv University, Tel Aviv, Israel Correspondence to: Dr P. Rozen, Department of Gastroenterology, Tel Aviv Medical Center, 6 Weizmann Street, Tel Aviv 64239, Israel. E-mail: [email protected] Publication data Submitted 17 July 2006 First decision 24 July 2006 Resubmitted 18 August 2006 Resubmitted 8 September 2006 Accepted 8 September 2006 & Y. NIV* , à SUMMARY Background Patients at risk for non-syndromic (Lynch or polyposis) familial colorectal neoplasia undergo colonoscopic surveillance at intervals determined by clinically ascertained protocols. The quantitative immunochemical faecal occult blood test for human haemoglobin is specific and sensitive for significant colorectal neoplasia (cancer or advanced adenomatous polyp). Aim To determine immunochemical faecal occult blood test efficacy for identifying significant neoplasia in at-risk patients undergoing elective colonoscopy. Methods We retrospectively identified consecutive at-risk patients who provided three immunochemical faecal occult blood tests before colonoscopy. Quantitative haemoglobin analysis was performed by the OC-MICRO automated instrument using the 100 ng Hb/mL threshold to determine positivity. Results In 252 at-risk patients undergoing colonoscopy; five had cancer, 14 an advanced adenoma and 46 a non-advanced adenoma. The immunochemical faecal occult blood test was positive in 31 patients (12.3%). Sensitivity, specificity, positive and negative predictive values for cancer were: 100%, 90%, 16% and 100%, and for all significant neoplasia: 74%, 93%, 45% and 98%. With 88% fewer colonoscopies, all colorectal cancers and 74% of all significant neoplasia would have been identified by this one-time immunochemical faecal occult blood test screening. Conclusions A sensitive, non-invasive, interval screening test might be useful to predetermine the need for colonoscopy in this at-risk population and minimize unnecessary examinations. This favourable retrospective evaluation will be extended to a prospective study. Aliment Pharmacol Ther 24, 1475–1481 ª 2006 The Authors Journal compilation ª 2006 Blackwell Publishing Ltd doi:10.1111/j.1365-2036.2006.03152.x 1475 1476 Z . L E V I et al. INTRODUCTION Patients and relatives at risk for non-syndromic (Lynch or polyposis) familial colorectal cancer (CRC) undergo colonoscopic surveillance at intervals determined by protocols based on accumulated clinical experience. Other than for the defined genetic syndromes, which have established diagnostic and follow-up endoscopy protocols, the increased risk to the asymptomatic relative is estimated from the youngest age and number of affected first-degree relatives.1–3 These screening and follow-up protocols are implemented in order to detect and treat asymptomatic early CRC and/or all clinically significant colorectal neoplasia that are of potential risk to the patient. ‘Significant’ neoplasia includes CRC or ‘advanced’ adenomatous polyps; this latter category included adenomas ‡10 mm, or having more than 20% of villous histology or any amount of high-grade dysplasia independent of size.4 The commonly used guaiac faecal occult bloodscreening test (FOBT) is faulted by its relatively low sensitivity for significant colorectal neoplasia and low specificity because of non-specificity for human haemoglobin (Hb).5,6 Published experience using the HemoccultTM (Beckman Coulter, Fullerton, CA, USA) guaiac FOBT in high-risk patients, showed a modest sensitivity for cancer and low positive predictive value for any neoplasia.7 Therefore, at present, patients with a family history of non-syndromic CRC are advised not only to rely on guaiac FOBT screening, but to undergo periodic total colonoscopic surveillance.1,3 However, unnecessary colonoscopy examinations are both a clinical and economic burden with an associated morbidity. In a recent evaluation of colonoscopy utilization in the United States, it was found that 22.4% were performed because of a family history of CRC.8 A periodically performed, sensitive and specific, non-invasive interval screening test might be useful to predetermine the timing of the need for colonoscopy. We have an ongoing colonoscopic evaluation of a quantitative immunochemical faecal occult blood test for human Hb (I-FOBT) and, like others, found it to be highly sensitive and specific for significant colorectal neoplasia, more so than a sensitive guaiac FOBT.6,9–11 The aim of this study was to analyse our initial results and identify those examinees that had a colonoscopy examination for a family history of non-syndromic CRC, to see whether the I-FOBT had identified the presence of significant colorectal neoplasia in these at-risk relatives, and at what sensitivity and specificity. Based on these retrospective results we would then decide if a prospective study was justified. MATERIALS AND METHODS Patients These were consecutive, ambulatory patients undergoing colonoscopy who were invited to participate in our ongoing endoscopic evaluation of an I-FOBT. To date, the overall compliance and successful completion of the protocol is 54%. We now analysed the subgroup having a family history of CRC, and volunteering for the study. The patients, referred by their treating doctor for colonoscopy, had been considered to be at increased risk because of their family history. All were interviewed and a two-generation family history of cancer was taken. They were grouped, using accepted criteria, as: those having had a first-degree relative aged £60 years with colorectal neoplasia or ‡2 such relatives of any age (Group 1); those who had a single first-degree relative with colorectal neoplasia but aged >60 years old, and others who had a family history of a second-degree relative with colorectal neoplasia (Group 2).1 The 108 patients in Group 1 included 88% who were asymptomatic and the remainder had anaemia (one), change in bowel habits (six) or abdominal pain (five). Previous colonoscopy had been performed in 41 (38%), at a mean 3 2 years before, and colorectal neoplasia had been diagnosed in 15 (14%). The 144 patients in Group 2 included 69% who were asymptomatic and the remainder had anaemia (seven), change in bowel habits (17) or abdominal pain (21). Previous colonoscopy had been performed in 52 (36%), at a mean 4 3 years before, and colorectal neoplasia had been diagnosed in 22 (15%). Exclusions included patients with known or suspected genetic syndromes for colorectal neoplasia, visible rectal bleeding, a known diagnosis of inflammatory bowel disease, haematuria, menstruation at that time and non-co-operation with preparing a faecal test. Colonoscopy was to the caecum or to an obstructing carcinoma if present. Otherwise, an incomplete examination was repeated or excluded from analysis. All lesions were noted, biopsied or removed. Patients’ electronic data files were available from the three participating endoscopy units belonging to the same Medical Organization. ª 2006 The Authors, Aliment Pharmacol Ther 24, 1475–1481 Journal compilation ª 2006 Blackwell Publishing Ltd F A E C A L O C C U L T B L O O D - S C R E E N I N G T E S T I N F A M I L I A L C A N C E R 1477 Numbers of polyps were noted, as were their sites. Adenomas were grouped by size: <10 mm, ‡10 mm; number; and also by their histology: tubular, tubulovillous, villous; dysplasia was classified as low- or high-grade. ‘Significant’ neoplasia included CRC or ‘advanced’ adenomatous polyps; all advanced adenomatous polyps (AP) sized <10 mm were re-examined to confirm their histology diagnosis. Faecal sampling All participants received an oral and/or telephone explanation of the test and written instructions on preparing the I-FOBTs. The examinee was requested to prepare three daily or consecutive samples during the week before colonoscopy examination, without diet or medication limitations other than those requested before colonoscopy, namely stopping aspirin and anticoagulants. The faecal test sampling device is shaped like a small test tube with the faecal probe inserted into it and sealing it after faecal sampling. The probe tip is then in a closed amount of Hb-stabilizing buffer. Each sample tube has a unique bar code and before preparing the sample the patient writes on the tube his/her name and date of sample preparation. Samples were double closed in zip-lock bags and kept in a refrigerator at 4 C until processing within 2 weeks.11 Instrument for I-FOBT analysis The I-FOBT and instrument used for faecal Hb evaluation has been previously described in detail.10,11 In summary, for faecal Hb analysis and quantification of the I-FOBT the OC-MICROTM instrument (Eiken Chemical Co., Tokyo, Japan) was used. This desktop instrument is self-contained with reagent, buffer, washing and fluid-disposal bottles, requiring access to a standard power supply. Ten of the patient-prepared faecal sample tubes are loaded into the sample rack and in parallel there is another rack with the disposable reaction cells. The instrument automatically mixes the faecal-buffer solution with the latex–antihuman Hb antibody reagent. The flocculation is read as an optical change and compared with a standard calibration curve. Calibration is prepared for each day’s analysis using the provided known high- and low-value control test fluids. The range of measurements is 50–2000 ng Hb/mL, approximately equivalent to 40–400 lg Hb/g faeces.10,11 For pricing the immunochemical FOBT at ª 2006 The Authors, Aliment Pharmacol Ther 24, 1475–1481 Journal compilation ª 2006 Blackwell Publishing Ltd $20, we used the local agent’s price for three tests and added administration costs. In comparison, our Ministry of Health’s authorized pricing for three guaiac tests is $13. Analyses and statistical methods The diagnostic level of the I-FOBT for significant neoplasia was evaluated by four criteria: sensitivity, specificity and predictive positive and negative values. The statistical significance level was set to 0.05 and results are given as mean s.d. and 95% confidence intervals (CI). The SPSS for Windows Software, version 13.0 was used for analysis. For clinical correlation with faecal Hb levels, the most severe pathology finding (histology and polyp size) recorded was used for each examinee. Subjects having only hyperplastic polyps were included in the group not having neoplasia. For correlations of faecal Hb levels with adenomas, the analysis included APs and was then repeated without them. For the category ‘significant’ colorectal neoplasia, the analyses included only CRC or AP or both together. Receiver operator characteristic (ROC) curves were drawn in order to determine several faecal Hb cut-off values of I-FOBT that would discriminate between significant neoplasia and other (non-significant) polyps. I-FOBT analysis for correlating the highest amount of faecal Hb in the three tests and presence of neoplasia at colonoscopy was based on the 100 ng Hb/mL threshold. This was the threshold suggested both by the manufacturer and in published experience.12 Additional analyses were performed examining different threshold levels and also results obtained with just the first two I-FOBTs prepared by the examinees.13 Association between pathology findings with the I-FOBT level was examined by non-parametric tests: Mann– Whitney for two groups and one-way ANOVA on ranks for more than the two groups, multiple comparisons between each pair were underwent using the Gabriel, Dunnet and Games-Howell tests. In addition, several contrasts were implemented for comparisons between combinations of categories – all adenomas vs. normal; significant neoplasia vs. other polyps. For an evaluation of the clinical utility of the I-FOBT for detecting significant colorectal neoplasia, we compared the results to the colonoscopy examinations. We then calculated the number of colonoscopy examinations that would potentially result from the positive I-FOBT tests. 1478 Z . L E V I et al. The Ethics Committee of the Rabin Medical Center approved the study in 2004. All participants gave an informed signed consent for the I-FOBT and colonoscopy examination. Faecal occult blood results At the Hb threshold of 100 ng Hb/mL, 31 patients had an elevated I-FOBT so the overall positivity rate was 12.3%. I-FOBT results according to endoscopy and pathology diagnosis, is given in Table 1. The mean faecal Hb levels in patients having a normal colonoscopy examination were not different from the mean level in patients with non-APs. However, the mean faecal Hb level in patients with AP or CRC was significantly higher than in patients with a normal colonoscopy examinations or having only non-advanced adenomas (P < 0.001; Table 1, Figure 1). RESULTS Patient and colonoscopy results The data from 252 examinees were analysed. Group 1 had 108 patients and included 87 relatives of adenoma or CRC patients aged £60 years and 21 having >1 such relative of any ages. Group 2 had 144 patients and included 116 who had a single first-degree relative with colorectal neoplasia but aged >60 years old and 28 who had a family history of a second-degree relative with colorectal neoplasia.1,2 Together, they included 46.2% males and their mean age was 57.7 11.2 years. Colonoscopy detected significant neoplasia in 19 patients (7.4%). These included one with CRC and two with an AP in Group 1; four with CRC and 12 with an AP in Group 2. Altogether, there were five patients with CRC and 14 with an AP. The mean age of patients with significant neoplasia was older than that of patients without significant neoplasia (62.2 10.4 vs. 57.3 11.2, P ¼ 0.07). Non-APs were detected in a further 46 patients (18.2%) and hyperplastic polyps in 35 patients (13.8%). Of all the polyps, 55.8% were tubular adenomas, 7.4% were tubular-villous and the remainder was hyperplastic polyps. High-grade dysplasia was found in adenomas of four patients (6.7%). The size of 58.3% of the adenomatous polyps was <5 mm, 25.0% were 6–9 mm, and 16.7% were ‡10 mm; 40.0% of the patients with polyps had single adenomas. Correlations of diagnosis with faecal haemoglobin levels At the standard 100 ng/mL faecal haemoglobin threshold: Colorectal cancer: Five patients were identified by colonoscopy; all were identified by the elevated faecal Hb. Advanced adenomatous polyps: Fourteen patients were identified by colonoscopy, nine of them (64.3%) were identified by the elevated faecal Hb. Significant neoplasia: These include the five patients with CRC and 14 with APs identified by colonoscopy, together 14 of these 19 (74%) were identified by their elevated faecal Hb. The I-FOBT sensitivity, specificity, positive and negative predictive results for the detection of CRC were 100%, 90%, 16% and 100%; and for the detection of all significant neoplasia were 74%, 93%, 45% and 98% (Table 2, Figure 2). At differing faecal haemoglobin thresholds: We examined the results obtained by using a lower or Table 1. Immunochemical faecal Hb levels detected according to colonoscopy and pathology findings (n ¼ 252) Diagnosis N Faecal Hb [ng/mL; mean s.d. (95% CI)] Normal Non-AP AP Cancer CRC + AP 187 46 14 5 19 36 69 598 1220 762 114 268 904 881 917 (20–54) (0–146) (125–1072) (448–1992) (349–1174) P-value* N.S. <0.001 <0.001 <0.001 Hb, haemoglobin; CI, confidence intervals; AP, advanced adenomatous polyps; CRC, colorectal cancer. * When compared with the normal and non-AP groups. Includes patients with non-adenomatous (hyperplastic) polyps. ª 2006 The Authors, Aliment Pharmacol Ther 24, 1475–1481 Journal compilation ª 2006 Blackwell Publishing Ltd F A E C A L O C C U L T B L O O D - S C R E E N I N G T E S T I N F A M I L I A L C A N C E R 1479 ROC curves: analysis for OC-MICRO OC-MICRO Results (Hb) by Diagnostic Category 3500 100% 3000 80% Sensitivity ngHb/mL 2500 2000 1500 60% 40% 1000 Cancer (n = 5) CRC + AP (n = 19) 20% 500 AP (n = 14) Non-AP (n = 46) 0 –500 Normal, Hyperplastic Non-Advanced Adenomas (n = 46) (n = 187) AP (n = 14) Cancer (n = 5) AP + Cancer (n = 19) 0% 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% 1 - Specificity Diagnosis Figure 2. Receiver operator characteristic curve for sensitivity and specificity for each diagnostic category at the ng Hb/mL level of faecal haemoglobin (Hb) measured. At the 100 ng Hg threshold there is high sensitivity for colorectal cancer (CRC) and also advanced adenomatous polyps (AP) and for both together, with low sensitivity for non-AP as a category. Figure 1. Box plots for each diagnostic category of faecal haemoglobin (Hb) values, at the 100 ng Hb threshold. Dark line indicates median Hb value, shaded block covers the upper and adjacent two lower quartiles, and bars are the maximum and minimum levels measured. Colorectal cancer (CRC) and/or advanced adenomatous polyp (AP) measurements are significantly elevated when compared with the normal hyperplastic polyp and non-AP groups (P < 0.001). Estimation of number of colonoscopy examinations needed higher faecal Hb threshold and also by utilizing just the first two I-FOBTs collected (Table 3). Lowering the threshold to 75 ng Hb/mL, did not improve the sensitivity or specificity for cancer or all significant neoplasia. Conversely, using a higher threshold of 150– 200 ng Hb/mL decreased the sensitivity for cancer by 20% and for all significant neoplasia by 16%. The improvement in specificity was only 1–2%. Analysing the first two I-FOBTs collected, the sensitivity at 100 ng Hb/mL for cancer was maintained, but for all significant neoplasia was reduced by 11% with an improved specificity of 2–3%. To identify all the five CRCs, 31 colonoscopy examinations would have been performed for a positive I-FOBT, i.e. six were needed to identify each cancer. To identify 14 of all the 19 significant neoplasia, 31 colonoscopy examinations would also have been performed for a positive I-FOBT, i.e. 2.2 colonoscopy examinations would have been needed for each significant neoplasm. So, these 14 lesions (74% of all the significant neoplasia detected by colonoscopy) could have been identified with 31 colonoscopy examinations, i.e. 88% fewer colonoscopy examinations at this one-time screening round. Table 2. Sensitivity, specificity, predictive values and 95% CIs at the faecal haemoglobin threshold of 100 ng/mL* Group Pathology Number Sensitivity [(%) CI] Specificity [(%) CI] PPV [(%) CI] NPV [(%) CI] 1 (N ¼ 108) 2 (N ¼ 144) All (N ¼ 252) CRC + AP CRC + AP CRC CRC + AP 3 16 5 19 33 81 100 (100–100) 74 (54–94) 94 91 90 (86–93) 93 (89–96) 14 54 16 (3–29) 45 (28–63) 98 98 100 (100–100) 98 (96–100) * Utilizing the highest of the three I-FOBT measurements in each patient. CI, confidence interval; CRC, colorectal cancer; AP, advanced adenomatous polyps; PPV, positive predictive value; NPV, negative predictive value. ª 2006 The Authors, Aliment Pharmacol Ther 24, 1475–1481 Journal compilation ª 2006 Blackwell Publishing Ltd 1480 Z . L E V I et al. Table 3. Sensitivity, specificity, predictive values and 95% CIs for cancer (n ¼ 5), cancer + advanced adenomas (n ¼ 19) at different faecal haemoglobin thresholds* and numbers of tests prepared by the 252 examinees Threshold (ng/mL)/ number of tests prepared 75/three tests 100/three tests 100/two tests 150/three tests 200/three tests Pathology Sensitivity [% (95% CI)] Specificity [% (95% CI)] PPV [% (95% CI)] NPV [% (95% CI)] CRC CRC CRC CRC CRC CRC CRC CRC CRC CRC 100 74 100 74 100 63 80 58 80 58 88 92 90 93 93 95 91 93 92 94 15 41 16 45 23 52 15 41 17 46 100 98 100 98 100 97 99.6 96 99.6 97 + AP + AP + AP + AP + AP (100–100) (54–94) (100–100) (54–94) (100–100) (42–85) (45–100) (36–80) (45–100) (36–80) (84–92) (89–95) (86–93) (89–96) (90–96) (93–98) (88–94) (90–96) (89–95) (92–97) (3–27) (25–58) (3–29) (28–63) (5–39) (32–73) (1–28) (22–59) (2–32) (22–66) (100–100) (96–100) (100–100) (96–100) (100–100) (95–99) (99–100) (94–99) (99–100) (94–99) * Utilizing the highest of the I-FOBT measurements in each patient. CI, confidence interval; CRC, colorectal cancer; AP, advanced adenomatous polyps; PPV, positive predictive value; NPV, negative predictive value. DISCUSSION This colonoscopy-controlled study allowed for a detailed retrospective evaluation of a small number of subjects at familial risk for colorectal neoplasia. It demonstrated that a one-time quantitative immunochemical determination of the faecal occult blood level would have led to the identification of 100% of CRC and 74% of all significant colorectal neoplasia, with significantly fewer colonoscopy examinations. This I-FOBT has the advantage of having a high sensitivity for significant neoplasia and not for the non-advanced adenomas that are not an immediate medical threat to the screenee. This differentiation would significantly reduce the number of follow-up colonoscopy examinations for clinically non-significant adenomas.3,8 The anticipation being that annual I-FOBT re-examination would eventually identify the minority of adenomas that progress to significant neoplasia. Even within a colonoscopy-screening program for high-risk patients interval neoplasia occurs. This has been attributed to non-recognition of the neoplastic lesion or inadequate therapy, e.g. incomplete polypectomy or mucosectomy or the genetically driven rapid progress to neoplasia in spite of the adequate examination. For these reasons, it has been suggested that the intervals between colonoscopy examinations be shortened or interval faecal occult blood testing also be performed as has already been tried successfully with the I-FOBT, Inform OBT (Enterix, Sydney, Australia).13,14 The latter approach seemed to us to be worthy of evaluation both from the aspects of cost–benefit and practicality. We therefore performed this pilot retrospective evaluation. The strengths of the study are a complete colonic examination of the participants and the quantification of the faecal Hb. A limitation of this retrospective study was the clinical criteria of family history used by the treating doctor to refer patients for colonoscopy, and that some patients also had mild symptoms. If the published protocols for screening families at risk had been followed, then a considerable number should not have been referred because of their family history, but entered into an averagerisk screening or diagnostic protocol.1–3,5 A further limitation is our definition of advanced adenomas. We did not include the cases having three or more adenomas without high-grade dysplasia or villous elements, but sized <1 cm, as was underwent in another study.13 We also used colonoscopy as our ‘gold’ standard, even though it too has been shown to be imperfect occasionally.13,14 However, in our published short follow-up study of a larger group of patients, we did not identify missed cancers occurring.10 In this high-risk population, at present we feel that a high sensitivity for all significant neoplasia is paramount and we accept a moderate specificity with the ª 2006 The Authors, Aliment Pharmacol Ther 24, 1475–1481 Journal compilation ª 2006 Blackwell Publishing Ltd F A E C A L O C C U L T B L O O D - S C R E E N I N G T E S T I N F A M I L I A L C A N C E R 1481 consequent need for colonoscopy examination. From this small retrospective analysis, we do not want to draw final conclusions on which is the optimal faecal Hb threshold and numbers of tests to be requested. We will learn from a larger, prospective trial, if we need to change the present policy. This favourable initial clinical experience will now be extended to a prospective study of performing the interval I-FOBT in a larger and asymptomatic population at familial risk undergoing elective colonoscopy screening and follow-up. Eventually, this approach might reduce the burden of colonoscopies and could be more cost-effective in this large number of asymptomatic patients at increased risk for CRC, but having only a family history of non-syndromic colorectal neoplasia.3,8 REFERENCES 1 Rozen P, Levin B, Young GP. Who is at risk from familial colorectal cancer and how can they be managed? In: Rozen P, Young GP, Levin B, Spann SJ, eds. Colorectal Cancer in Clinical Practice, 2nd edn. London: Taylor and Francis, 2005: 67–84. 2 Offit K, Brown K. Quantitating familial cancer risk: a resource for clinical oncologists. J Clin Oncol 1994; 12: 1724–36. 3 Dove-Edwin I, Sasieni P, Adams J, Thomas HJW. Prevention of colorectal cancer by colonoscopic surveillance in individuals with a family history of colorectal cancer: 16 year, prospective, follow-up study. Br Med J 2005; 331: 1047–52. 4 Itzkowitz SH. Colonic polyps and polyposis syndromes. In: Feldman M, Friedman LS, Sleeisenger MH, eds. Gastrointestinal and Liver Disease, 7th edn. Philadelphia: Saunders, 2002: 2178. 5 Young GP, Rozen P, Levin B. How should we screen for early colorectal 6 7 8 9 10 ACKNOWLEDGEMENTS We acknowledge the medical and secretarial staff of the Endoscopy Units and the patients for their cooperation. We thank Dr Ester Shabtai and Doron Comaneshter for statistical analyses, and Ms Sally Zimmerman for secretarial assistance. Instrument and reagents were provided by Eiken – Japan, Alfa Wasserman – Italy and Pharmatrade – Israel. Support for administration of the study was provided by Eiken and the Katzman Family Foundation. Presented in part at the International Society for Hereditary Tumors (InSiGHT) Meeting, Newcastle, UK, 2005. neoplasia? In: Rozen P, Young GP, Levin B, Spann SJ, eds. Colorectal Cancer in Clinical Practice, 2nd edn. London: Taylor and Francis, 2005: 97–130. Levi Z, Hazazi R, Rozen P, Vilkin A, Waked A, Niv Y. A quantitative immunochemical fecal occult blood test is more efficient for detecting significant colorectal neoplasia than is a sensitive guaiac test. Aliment Pharmacol Ther 2006; 23: 1359–64. Caffarey SM, Broughton CIM, Marks CG. Faecal occult blood screening for colorectal neoplasia in a targeted high-risk population. Br J Surg 1993; 80: 1399– 400. Leiberman DA, Holub J, Eisen G, Kraemer D, Morris CD. Utilization of colonoscopy in the United States: results from a national consortium. Gastrointest Endosc 2005; 62: 875–83. Young GP. Fecal immunochemical tests (FIT) vs office-based guaiac fecal occult blood test (FOBT). Pract Gastroenterol 2004; 18: 46–56 (http://www.practicalgastro.com). Vilkin A, Rozen P, Levi Z, et al. Performance characteristics and evaluation ª 2006 The Authors, Aliment Pharmacol Ther 24, 1475–1481 Journal compilation ª 2006 Blackwell Publishing Ltd 11 12 13 14 of an automated developed and quantitative, immunochemical, fecal occult blood screening test. Am J Gastroenterol 2005; 100: 2519–26. Rozen P, Waked A, Vilkin A, Levi Z, Niv Y. Evaluation of a desk top instrument for the automated development and immunochemical quantification of fecal occult blood. Med Sci Monit 2006; 12: MT27–32. Castiglione G, Grazzini G, Miccinesi G, et al. Basic variables at different positivity thresholds of a quantitative immunochemical test for faecal occult blood. J Med Screen 2002; 9: 99–103. Bampton PA, Sandford JJ, Cole SR, et al. Interval faecal occult blood testing in a colonoscopy based screening programme detects additional pathology. Gut 2005; 54: 803–6. Schoenfeld PS, Fincher RK for the Military Colorectal Cancer Screening Trials Group. Colonoscopic surveillance of patients with a family history of colon cancer and a history of normal colonoscopy: is a five-year interval between colonoscopies appropriate? Clin Gastroenterol Hepatol 2003; 1: 310–4.