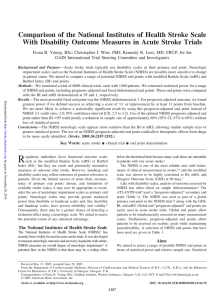
Original Paper Cerebrovasc Dis 2012;34:272–281 DOI: 10.1159/000342652 Received: February 6, 2012 Accepted: August 13, 2012 Published online: October 20, 2012 Stroke and Transient Ischemic Attack Incidence Rate in Spain: The IBERICTUS Study Jaime Díaz-Guzmán a Jose-A. Egido b Rafael Gabriel-Sánchez d Gloria Barberá-Comes f Blanca Fuentes-Gimeno e Cristina Fernández-Pérez c on behalf of the IBERICTUS Study Investigators of the Stroke Project of the Spanish Cerebrovascular Diseases Study Group a Stroke Unit, Neurology Department, University Hospital Doce de Octubre, Complutense Faculty of Medicine, Stroke Unit, Neurology Department and c Clinical Epidemiology Unit, University Hospital Clínico San Carlos, d Investigation Unit, University Hospital La Paz and CEIIS, and e Stroke Centre, Department of Neurology, Hospital Universitario La Paz, Universidad Autónoma de Madrid, IdiPAZ Health Research Institute, Madrid, and f Medical Department for Thrombosis, Sanofi-Aventis, Barcelona, Spain b Abstract Background: In Spain, stroke is a major public health concern, but large population-based studies are scarce and date from the 1990s. We estimated the incidence and in-hospital mortality of stroke through a multicentered populationbased stroke register in 5 geographical areas of Spain, i.e. Lugo, Almería, Segovia, Talavera de la Reina and Mallorca, representing north, south, central (!2) and Mediterranean areas of Spain, respectively, the aim and novelty being that all methodologies were standardized, and diagnoses were verified by a neurologist using neuroimaging techniques. Methods: The register identified subjects 117 years of age who suffered a first-ever stroke or transient ischemic attack (TIA) between 1 January and 31 December 2006. Stroke and TIA were defined according to the WHO criteria. The Lau- © 2012 S. Karger AG, Basel 1015–9770/12/0344–0272$38.00/0 Fax +41 61 306 12 34 E-Mail [email protected] www.karger.com Accessible online at: www.karger.com/ced sanne Stroke Registry definitions were used to classify ischemic stroke subtypes, as follows: (1) large-artery atherosclerosis (LAA); (2) cardioembolism (CE); (3) lacunar stroke or small-artery occlusion (SAO); (4) stroke of other infrequent cause (SIC), and (5) stroke of undetermined cause (UND). We used several complementary data sources such as hospital discharge registers, emergency room registers and primary care surveillance systems. Results: In the 1-year study period, we identified 2,700 first-ever cerebrovascular episodes (53% men; 2,257 strokes + 443 TIA episodes). Brain CT in the acute stage was performed in 99% of cases. Of a total of 2,257 stroke patients, 1,817 (81%) had cerebral infarction, 350 (16%) had intracerebral hemorrhage, 59 (3%) had subarachnoid hemorrhage (SAH) and 31 (1%) had unclassifiable stroke. The overall unadjusted annual incidence for all cerebrovascular events was 187 per 100,000 [95% confidence interval (CI) 180–194; incidence for men: 202, 95% CI 189–210; incidence for women: 187, 95% CI 180–194]. The subtype of ischemic stroke could be determined in 1,779 patients and was classified as LAA in 624 (35%), CE in 352 (20%), SAO in 316 Jaime Díaz-Guzmán, MD, PhD Stroke Unit, Neurology Department, University Hospital Doce de Octubre Complutense Faculty of Medicine Avda Córdoba s/n, ES–28045 Madrid (Spain) E-Mail jdiaz.hdoc @ salud.madrid.org Downloaded by: Kainan University 203.64.11.45 - 2/3/2015 3:20:43 PM Key Words Epidemiology ⴢ Stroke ⴢ Incidence ⴢ Transient ischemic attack ⴢ Subarachnoid hemorrhage Copyright © 2012 S. Karger AG, Basel Introduction cidence of ischemic attack and hospital deaths from stroke in the Spanish population. The data were derived from 5 geographically disparate areas of Spain. Materials and Methods Study Design and Population IBERICTUS is a prospective, population-based study aimed at identifying all first stroke and transient ischemic attack (TIA) events in Spain. The study accessed the data on stroke and TIA recorded in 5 major cities, namely Lugo, Almería, Segovia, Talavera de la Reina and Mallorca, representing north, south, central (!2) and Mediterranean areas of Spain, respectively, with care provision for 1,440,979 citizens. Data sources, procedures and stroke definitions have been described in detail elsewhere [5]. In brief, we included all the cases presenting within the period of the study. The individuals were 117 years of age (with no upper age limit) and had suffered a first episode of acute cerebrovascular disease diagnosed by the attending neurologist. The geographical areas were selected on the basis of our Spanish NHS data indicating possible differences in stroke incidence in the different regions. Also, these regions provided a minimum population size of at least 100,000 persons per study site (table 1). The data on the at-risk population in each province, as well as the overall study area, were obtained from the official 2005 census of the Spanish National Institute of Statistics [6]. The overall study population totaled 1,440,979 individuals (online suppl. fig. 1; for all online suppl. material, see www.karger.com/doi/10.1159/000342652). The study was designed to meet the quality criteria proposed by Malmgren et al. [7] and Sudlow and Warlow [8] for ‘ideal’ population-based studies. The Ethics Committee (Institutional Review Board of the Segovia General Hospital) approved the study. Data were coded to ensure patient anonymity. Stroke is a major cause of mortality and long-term disability, with important socioeconomic consequences. According to the WHO, stroke is the second most common cause of mortality worldwide [1]. In the WHO Monitoring Trends and Determinants in Cardiovascular Disease Project, the attack rate was estimated at around 200/100,000 individuals per year [2]. Attack rates vary considerably geographically and, as such, extrapolations need to be made with caution [3]. Stroke is the second most common cause of death in Spain overall, while it is the principal cause in women. Despite this, there are few studies assessing its incidence; all the studies to date have been local, with considerable heterogeneity of methodology [4]. Compared to these studies, the novelty and aims of the IBERICTUS study are that it has the power to estimate epidemiological data simultaneously in 5 large patient populations. All patients were diagnosed in the acute stroke phase by the attending physician, and diagnoses were verified by specialist neurologists using neuroimaging technology. Mortality due to stroke is thought to be high in Spain, but the real impact is unknown. Various factors may account for this high mortality rate, including genetic and socioeconomic factors and the quality of health care available [3]. Reliable data on incidence rates are essential in the planning of health care resource distribution. The health care system in Spain is one in which the citizen has the right to access health care which is free at the point of delivery. Resource management, with minor variations, is within the jurisdiction of the governments of the autonomous regions of Spain. The IBERICTUS study is a population-based epidemiological registry that seeks to estimate the rates of in- Definition of Stroke Stroke and TIA were defined according to the WHO criteria as ‘rapidly developing clinical symptoms and/or signs of focal, and at times global (applied to patients in deep coma and to those with subarachnoid hemorrhage) loss of cerebral function with symptoms lasting 124 h (! 24 h for TIA) or leading to death, with no apparent cause other than of vascular origin’ [9]. The diagnosis was made by the attending physician and verified by a neurologist. The data on stroke and TIA morbidity and mortality were obtained from the hospitals’ admission department and discharge register, as well as the hospitals’ emergency department registry and the primary health care registers. The International Classification of Diseases (9th revision) was used to identify events as subarachnoid hemorrhage (SAH; n = 430), intracranial hemorrhage (ICH; n = 431), other unspecified ICHs (n = 432), occlusion and stenosis of precerebral arteries (n = 433), occlusion of cerebral arteries (n = 434), TIA (n = 435), acute/ other ill-defined cerebrovascular disease (n = 436/437) or late effects of cerebrovascular disease (n = 438). An adapted version of the Lausanne Stroke Registry [10] was used to classify the ischemic stroke subtypes as follows: (1) largeartery atherosclerosis (LAA); (2) cardioembolism (CE); (3) lacunar stroke or small-artery occlusion (SAO); (4) stroke of other Stroke Incidence Rate in Spain Cerebrovasc Dis 2012;34:272–281 273 Downloaded by: Kainan University 203.64.11.45 - 2/3/2015 3:20:43 PM (18%), SIC in 56 (3%) and UND in 431 (24%). The incidence rates per 100,000 (95% CI) standardized to the 2006 European population were as follows: all cerebrovascular events, 176 (169–182); all stroke (non-TIA), 147 (140–153); TIA, 29 (26– 32); ischemic stroke, 118 (112–123); intracerebral hemorrhage, 23 (21–26), and SAH, 4.2 (3.1–5.2). Incidence rates clearly increased with age in both genders, with a peak at or above 85 years of age. The in-hospital mortality was 14%. Conclusions: Our results show that the incidence of stroke and TIA in Spain is moderate compared to other Western and European countries. However, it is expected that these figures will change due to progressively aging populations. Table 1. Study centers participating in the assessment and recruitment of cases Segovia (Castilla y León) Talavera Lugo (Castilla La Mancha) (Galicia) Mallorca (Islas Baleares) Almería (Andalucía) Population 131,535 127,508 313,673 647,036 221,227 Population density citizens/km2 23 446 32 218 76 Geographic location 40°57ⴕN 4°10ⴕW 39°57ⴕ30ⴕⴕN 4°49ⴕ58ⴕⴕW 43°01ⴕN 7°33ⴕW 39°58ⴕ00ⴕⴕN 3°08ⴕ00ⴕⴕE 36°50ⴕN 2°27ⴕW Climate continental Mediterranean mild continental continental oceanic Mediterranean subdesert Mediterranean Reference hospital (‘hot pursuit’) Hospital Provincial, Hospital Nuestra Segovia Señora del Prado Hospital Costa de Burela Complejo Hospitalario Xeral-Calde, Lugo Hospital Comarcal de Monforte de Lemos Complejo Asistencial Son Dureta Hospital Son Llatzer Hospital Joan March Hospital General de Mallorca Hospital Sant Joan de Deu Hospital d’Alcudia Fundación Hospital Manacor Hospital General de Muro Hospital Torrecárdenas Nearby general hospitals in or out of the districts of study 0 1 1 0 2 Probability that some patients were hospitalized outside the catchment area low very low very low none low Primary care health registers, 3-monthly check (‘cold pursuit’) Sentinel Physician Network 3 additional cases (over 251) Sentinel Physician Network 0 additional cases (over 209) not done not done (over 832) regional administration primary care health register 7 additional cases (over 985) not done (see text) not done (see text) not done (see text) not done (see text) not done (see text) infrequent cause (SIC), and (5) stroke of undetermined cause (UND). Ischemic strokes were classified by the attending physician mainly on the basis of case history, clinical examination and risk factor profile. For various reasons such as, for example, scarce clinical information, the ischemic stroke subtype was defined as ‘not classified’ (NC). If CT scans had not been performed, the stroke type (ischemic or hemorrhagic) was also defined as NC. To ensure the validity of the diagnosis of acute stroke assigned in the hospital discharge register or death register, a reliability study of interobserver agreement was conducted prior to the conduct of the IBERICTUS study. The kappa index of agreement between the participant observers was 0.72 [95% confidence interval (CI) 0.68–0.77] for the classification of clinical type (as ischemic, hemorrhagic or undetermined) and 0.62 (95% CI 0.57–0.68) for the classification of etiology of the ischemic stroke (as LAA, CE, SAO, SIC or UND) [11]. The proportion of cases in the registry that had not had a brain CT at the time of diagnosis was only 0.9%. Statistical Analyses Stroke incidence is reported as age-unadjusted and standardized rates according to the Spanish and European standard population using the direct method [12, 13]. The incidence rates and 274 Cerebrovasc Dis 2012;34:272–281 the respective 95% CIs were calculated using normal approximation to the binomial distribution. We employed one-way ANOVA for the comparison of means. The EpiDat 3.1 and SPSS for Windows (version 14.0) statistical packages were used throughout. Results Between 1 January and 31 December 2006, 2,700 first cerebrovascular events (2,257 strokes and 443 TIAs) were identified in individuals aged 117 years (254 cases in Segovia, 209 in Talavera, 832 in Lugo, 992 in Mallorca, 413 in Almería). The hospitalization rate for stroke was 2,086/2,257 (92.4%), and for TIA, it was 126/443 (28.4%). Table 2 shows the sociodemographic characteristics and clinical assessment of patients in the study sample. The mean 8 SD age of the patients was 73.9 8 13.4 years, with a range of 18–101 years. The patients were older in Segovia, Talavera and Lugo than in Mallorca and Almería (p ! 0.05). Women represented 47% of the patients (aged Díaz-Guzmán et al. Downloaded by: Kainan University 203.64.11.45 - 2/3/2015 3:20:43 PM Detected via death certificate scrutiny (over 413) Table 2. Patients’ characteristics and methods of assessment in the IBERICTUS study Source of information, % Discharge reports/clinical history Emergency reports/primary care Women, % Age, years1 Length of in-hospital stay, days1 CT scanning performed in acute stage, % Type of stroke, % Ischemic Hemorrhagic TIA Undetermined In-hospital mortality, % 1 IBERICTUS (n = 2,700) Segovia (n = 254) Talavera (n = 209) Lugo (n = 832) 90.1 9.9 46.6 73.98813.39 10.9814.36 99.1 71.7 20.3 47.6 76.21812.73 9.33816.53 96.5 79.4 98.8 20.6 1.2 49.8 48.2 76.72811.34 75.96812.36 9.66812.94 13.08814.91 94.3 100 91.5 85.7 8.5 14.3 45 45 72.05814.08 71.86814.04 10.59815.20 8.9588.85 99.7 100 67.3 15.1 16.4 1.1 11.6 61.8 15 17.7 5.5 14.2 63.2 16.7 13.9 6.2 14.8 70.4 13.9 15.3 0.4 9.8 68.1 15.9 16 0 15.1 Mallorca (n = 992) Almería (n = 413) 63.7 16 20.3 0 5.8 Mean 8 SD. Table 3. Age- and gender-specific unadjusted annual incidence rates of first-ever stroke (including TIAs) per 100,000 population and in-hospital mortality Number of men at risk Incidence, men n rate, % 18–24 25–34 35–44 45–54 55–64 65–74 75–84 >84 77,182 152,612 141,453 115,177 88,997 73,496 49,815 13,218 2 12 50 110 211 361 505 191 Total 711,950 1, 442 Age group years Incidence, women 95% CI Number of women at risk Incidence, total 95% CI Total number at risk n rate, % n rate, % 95% CI 2.6 7.9 35.3 95.5 237.1 491.2 1,013.8 1,445.0 0–6.2 3.4–12.3 25.5–45.1 77.7–113.4 205.1–269.1 440.5–541.9 925.3–1102.2 1,240.1–1,649.9 73,060 140,843 134,070 109,525 90,264 84,106 69,814 27,347 2 12 29 39 103 217 484 372 2.7 8.5 21.6 35.6 114.1 258.0 693.3 1,360.3 0–6.5 3.7–13.3 13.8–29.5 24.4–46.8 92.1–136.1 223.7–292.3 631.5–755 122.1–1,498.5 150,242 293,455 275,523 224,702 179,261 157,602 119,629 40,565 4 24 79 149 314 578 989 563 2.7 0.1–5.3 8.2 4.9–11.5 28.7 22.3–35 66.3 55.7–77 175.2 155.8–194.5 366.7 336.8–396.6 826.7 775.2–878.2 1,387.9 1,273.3–1,502.5 202.5 189.4–210.1 729,029 1,258 172.6 1,440,979 2,700 163.0–182.1 187.4 180.3–194.4 In-hospital mortality, men In-hospital mortality, women In-hospital mortality, total n n rate, % 95% CI rate, % 95% CI n rate, % 95% CI 18–34 35–44 45–54 55–64 65–74 75–84 >84 0 3 8 20 23 66 42 0 6 7.3 9.5 6.4 13.1 22.0 0 0–12.8 2.2–12.3 5.3–13.6 3.8–9.0 9.9–16.2 15.3–28.6 0 1 5 10 26 37 73 0 3.4 12.8 9.7 12.0 7.6 19.6 0 0–10.2 1.6–24.1 3.7–15.7 7.4–16.6 5.2–10.1 15.1–24.1 0 4 13 30 49 103 115 0 5.1 8.7 9.6 8.5 10.4 20.4 0 0.1–10 4.0–13.5 6.1–13.0 6.1–10.9 8.4–12.4 16.7–24.2 Total 162 11.2 9.5–13.0 152 12.1 10.2–14.0 314 11.5 10.3–12.9 Stroke Incidence Rate in Spain Cerebrovasc Dis 2012;34:272–281 275 Downloaded by: Kainan University 203.64.11.45 - 2/3/2015 3:20:43 PM Age group years 100 TIA 90 Incidence rate (×100,000) 80 70 60 50 M M 40 W All M W All 30 M W W 20 M All W All M W All All 10 0 Segovia Talavera Lugo Mallorca Almería 300 Incidence rate (×100,000) Hemorrhagic stroke Ischemic stroke M 250 IBERICTUS W All 200 150 M W M M All M W All M All All All W W Almería IBERICTUS W 100 50 0 Segovia 76.9 8 12.8 years), and 53% were men (aged 71.4 8 13.3 years). Eighty percent of cases were 665 years of age. A brain CT scan was performed in 2,676 patients (99.1%). Of a total of 2,257 stroke patients, 1,817 (80.5%) had ischemic stroke, 350 (15.5%) had ICH, 59 (2.6%) had SAH and 31 (1.4%) had an NC type of stroke. TIA was diagnosed in 16.4% of cases (table 2). The subtype of ischemic stroke could be determined in 1,779 patients according to the modified Lausanne Stroke Registry criteria as follows: LAA in 624 (35%), CE in 352 (20%), SAO in 316 (18%), SIC in 56 (3%) and UND in 431 (24%) patients. The overall in-hospital mortality was 11% (314 patients). The fatality rates segregated by province were: Segovia, 14% (95% CI 9.7–18.7%); Talavera, 15% (95% CI 9.8–19.9%); Lugo, 15% (95% CI 12.6–17.6%); Mallorca, 10% (95% CI 7.9–11.7%), and Almería 6% (95% CI 3.4– 8.2%). The in-hospital fatality rate was 11.2% for men and 12.1% for women (table 3), and it increased with age (on276 Cerebrovasc Dis 2012;34:272–281 Talavera Lugo Mallorca line suppl. table 2). The mean length of hospitalization for cerebrovascular disease was 11 8 14.8 days. Segregated by stroke subtype, the fatality rate was 28% for ICH, 24% for SAH, 13% for NC, 11% for ischemic stroke and 0.2% for TIA. The crude (unadjusted) annual incidence rate of firstever stroke was 187/100,000 (95% CI 180–194), and age-standardized to the European population it was 176/100,000 (95% CI 169–182). The crude incidence rate for men (202/100,000, 95% CI 189–210) was higher than that for women (173/100,000, 95% CI 163–182; fig. 1). After standardization to the European population, the higher incidence rate for men remained statistically significant compared to that for women, i.e. 190 (95% CI 180–200) versus 159 (95% CI 150–168) per 100,000 (table 4). The crude incidence rates according to stroke subtype are shown in figure 2. Díaz-Guzmán et al. Downloaded by: Kainan University 203.64.11.45 - 2/3/2015 3:20:43 PM Fig. 1. Crude incidence rates (!100,000 person-years) in the IBERICTUS study. W = Women; M = men. IBERICTUS Segovia Talavera Lugo rate rate 95% CI rate 95% CI rate 163 137 151 132–193 108–165 130–172 130 135 134 102–159 107–163 114–154 126 119 124 99–153 93–146 105–143 110 119 116 37 17 27 22–51 7–28 18–36 93 90 92 95% CI All cerebrovascular events Men 190 180–200 Women 159 150–168 Total 176 169–182 All strokes (non-TIA) Men 160 151–169 Women 131 123–140 Total 147 140–153 TIA Men 30 26–34 Women 27 24–31 Total 29 26–32 Ischemic stroke Men 128 119–136 Women 106 99–114 Total 118 112–123 ICH Men 27 23–30 Women 18 15–21 Total 23 21–26 SAH Men 3.1 1.8–4.4 Women 5.2 3.5–6.8 Total 4.2 3.1–5.2 Undefined Men 2.4 1.2–3.5 Women 1 0.6–2.4 Total 2 1.2–2.7 Mallorca Almería 95% CI rate 95% CI rate 95% CI 196 164 181 174–219 144–184 166–196 193 154 174 178–208 140–167 164–184 246 199 222 217–276 172–225 203–242 84–136 92–145 97–135 168 132 150 147–188 115–150 138–164 167 127 148 153–181 115–139 138–157 197 157 176 171–223 133–180 159–194 20 16 19 9–31 7–26 11–26 69 74 72 54–85 58–91 61–83 26 27 26.5 20–31 21–33 23–30 50 42 46 37–63 30–54 37–55 70–117 67–113 76–109 78 91 86 56–99 68–114 70–102 331 287 310 297–365 255–319 286–333 136 109 123 123–149 98–120 115–132 156 128 142 133–180 107–150 126–158 21 12 17 10–32 4–21 10–24 18 22 20 8–28 11–34 12–28 72 61 67 56–87 47–76 56–77 26 16 21 21–32 11–20 18–25 33 23 28 22–44 14–32 21–36 3.2 6.1 4.7 0–7.6 0.1–12.1 0.9–8.3 2.8 2.7 2.8 0–6.9 0–6.8 0–5.8 1.2 8.4 4.9 0–3.2 3.0–13.9 1.9–7.8 3.2 2.7 2.9 1.2–5.2 0.9–4.5 1.6–4.3 7.1 4.9 5.9 2.1–11.9 0.8–9.1 2.7–9.2 8 10 9 1–15 3–19 4–14 12 5 8 3–20 0–10 3–14 0 0 0 0 0 0 1.3 0 0.7 0.1–2.6 0 0.0–1.3 0 0 0 0 0 0 TIA and Stroke Ascertainment Standardized population-based studies provide the best source of information on stroke incidence and outcomes. We designed the study according to the quality recommendations of Sudlow and Warlow [8], recently updated to include large sample sizes in order to ensure a sufficient number of incident strokes in 1 year and, in addition, to generate age-specific data on first-ever-in-a- lifetime stroke (or TIA) in the oldest age groups [14]. Details of case ascertainment in each of our study locations have been published elsewhere [5]. In brief, almost all first-ever stroke patients in these locations of the Autonomous Regions of Spain are admitted to hospital if they seek medical help. Less than 2% of cases were identified in the primary care setting (‘cold’ pursuit method) in Mallorca, Segovia and Talavera (in the Sentinel Medical Net database) and in the Lugo database. It was not possible to obtain data on nonhospitalized patients from Almería. However, since it is the only hospital serving the study area, it is reasonable to assume the rate to be !5%. In Spain, because of the health care policy and cultural factors, there is a strong tendency to seek hospital consultation when a stroke or TIA is suspected. This enables neuroimaging to be performed in the acute phase (emergency room) in almost all patients, and, hence, the timing of this diagnostic procedure makes it unlikely that TIAs Stroke Incidence Rate in Spain Cerebrovasc Dis 2012;34:272–281 Discussion The present study is the first population-based stroke incidence study in Spain using current and homogeneous methodology applied concurrently in several geographical locations. The considerable sample sizes and universal application of CT in the assessments provide robust estimations of incident TIA as well as stroke and stroke subtypes. 277 Downloaded by: Kainan University 203.64.11.45 - 2/3/2015 3:20:43 PM Table 4. Age-standardized (to European population) incidence rates of stroke and subtypes (!100,000 inhabitants/year) TIA 180 160 Ischemic stroke 1,200 Men Women 1,000 140 120 800 100 600 80 400 60 40 200 20 0 0 18 25 35 250 45 55 65 75 18 85+ ICH 25 35 45 55 65 75 65 75 85+ SAH 30 25 200 20 150 15 100 10 50 5 0 0 18 25 35 45 55 65 Age (years) 75 85+ 18 25 35 45 55 85+ Age (years) Fig. 2. Crude incidence rates (!100,000 person-years) according to stroke subtype in the IBERICTUS study. 278 Cerebrovasc Dis 2012;34:272–281 stroke-related early death is usually of the hemorrhagic stroke subtype, we believe that there can be only a few possible stroke cases that had not been registered. Similar limitations affect most of the studies addressing the epidemiology of stroke, i.e. the nondetection of stroke patients among the older age groups who die suddenly away from the administrative monitoring of a hospital. Incidence It is difficult to compare data derived from different studies reliably since they may have been conducted at Díaz-Guzmán et al. Downloaded by: Kainan University 203.64.11.45 - 2/3/2015 3:20:43 PM and hemorrhagic and ischemic strokes could have been misclassified. By contrast, a very important study conducted in Oxfordshire in the UK [15] shows a very low hospitalization rate in stroke patients (56%), and this implies a delay in neuroimaging. Incidence data from death certificates and autopsy reports for fatal cases are hard to obtain because of legal and administrative restrictions operating in Spain. This is an unavoidable limitation of the IBERICTUS study. However, in our study the proportion of hemorrhagic strokes (15%) was comparable with other studies [16–20]. Since Subtypes of Stroke Because CT brain scans were performed early in our patients, our assignment of ischemic or hemorrhagic stroke can be made with confidence. A stroke subtype diagnosis (ischemic vs. hemorrhagic) was reached in 99% of cases. However, determining ischemic stroke subtyping may be difficult in a multicentered incidence study such as ours. Our interobserver concordance is only modest using the modified Lausanne criteria, as we had seen in the pilot study conducted prior to the start of the current IBERICTUS study [11]. The main interobserver discordance was with respect to ‘undetermined cause’ (27% of our ischemic stroke cases). Overall, the proportions of LAA (1/3), CE (1/5) and ‘lacunar’ stroke or SAO (1/6) are similar to other studies in Western countries and stroke registries. Ischemic and hemorrhagic strokes show similar increasing incidence rates with age and higher numbers in men in all age groups. One exception is SAH, for which the incidence in women is 1.76-fold (95% CI 1.04–3.01) that in men. This gender difference begins around 45 years of age and increases thereafter, except for the group aged 65–74 years. Our overall incidence of SAH (4.2/ 100,000 person-years) is similar to that observed in South and Central America but lower than in other regions [28]. Stroke Incidence Rate in Spain TIA Incidence In the IBERICTUS study, 16% of all first strokes were TIAs. Compared with other developed countries, the TIA incidence rates in Spain are higher than in Russia [29] and lower than in the USA [30, 31], England [32], Portugal [33] and Japan [34, 35], but very similar to the 15% observed in a recent nationwide study in the Netherlands [36]. TIA follows an identical age trend as that observed in stroke, with higher rates in men than in women across all age groups, except for the oldest age group, which is due, at least in part, to a cohort effect (see above). With the participation of specialist neurologists in classifying the events and the almost universal deployment of CT scanning in the acute phase of the transient neurological deficit, it is unlikely that events that ‘mimic’ ischemic brain events, such as structural lesions (i.e. subdural hematomas, tumors), had been erroneously included. In addition, cases of isolated acute dysarthria or dysphagia were not registered. However, because of the nature of the study we cannot exclude other nonvascular diagnoses such as migraine, epilepsy or transient hypoglycemia, which in some clinical series may account for up to 20% of cases [37]. Diffusion-weighted magnetic resonance imaging was not employed in the vast majority of the cases. One limitation of the present study is the nondetection of very short TIAs since patients suffering these attacks seldom seek medical attention. These patients can be detected in a prevalence study (for example, door-to-door methodology), but establishing the true incidence is very complicated. In-Hospital Mortality In this phase of our epidemiological study, we were unable to obtain data on the 28-day mortality rates because of Spanish laws limiting the investigation of deaths occurring once the patient has been discharged from hospital. Hence, it is difficult to compare in-hospital mortality with 28-day mortality from other studies. However, in-hospital mortality has been proposed as an indicator of health care quality, and a rate of 12%, such as observed in our study, is very acceptable. The case fatality rate in IBERICTUS was similar for men and women and increased exponentially with age in both genders, reaching peak values at the age of 85+ years. The geographical distribution shows higher in-hospital mortality rates in the northern (Lugo) and central provinces (Segovia and Talavera), a lower rate in the Mediterranean region (Mallorca) and lowest rate in southern Spain (Almería). Agestandardized rates of in-hospital mortality were particularly high, and statistically significantly so, in Lugo Cerebrovasc Dis 2012;34:272–281 279 Downloaded by: Kainan University 203.64.11.45 - 2/3/2015 3:20:43 PM different times and, even, using different inclusion criteria, but compared with other Western countries, the stroke incidence rates in Spain appear similar to those in Sweden [21], higher than in the USA [22], England [17], Germany [18], Poland [23] and France [23, 24], and lower than in Italy [19], Ukraine [25], Greece [26], Norway [20], Portugal [27] and Estonia [16] (online suppl. table 1). The incidence rates increase with age, with higher rates in men than in women across all age groups. There is a trend towards attenuation of differences in rates in the older age groups (185 years of age), probably due to fewer cases among men (‘true’ lower incidence rate) and a higher proportion of women in the population (ratio of women to men of 2:1). This disproportion of older women in the Spanish population is due, at least in part, to the high death rate amongst men during, and immediately after, the Spanish Civil War (1936–1939). There are differences in the incidence of stroke between regions in Spain, with higher rates in the south and the northwest regions compared to the central and Mediterranean regions. These differences are in the process of undergoing more detailed analyses. Overall, there appears to be a gradient related to socioeconomic status and risk factor profile, and less likely to methodological issues. compared with the other provinces. These differences are not attributable to different subtypes of stroke between the areas but may be due, rather, to the overall health status of the population, as well as to improvements in the standard of care (e.g. specialized stroke units), or they may be artefactual due to different rates of hospital discharge (i.e. home or residential care). The methodology employed in the IBERICTUS study does not support more profound analyses of these differences in relation to mortality. In conclusion, the present study provides de novo and robust estimates of the incidence of first-ever stroke and TIA in Spain based on populations from different geographical areas. The data may provide important insights and perspective into the epidemiology of stroke in Europe. Acknowledgments Our thanks go to the Centro de Epidemiología, Investigación e Información en Salud (CEIIS) for help with the logistics of data retrieval and verification, to Margarita Alonso-Arroyo (CEIIS) for help with the statistical analyses and to other contributors in the different clinical centers (online suppl. appendices). Editorial assistance was provided by Dr. Peter R. Turner. Disclosure Statement This study was sponsored by Sanofi-Aventis via a donation to the Spanish Neurology Society. References 280 8 Sudlow CLM, Warlow CP: Comparing stroke incidence worldwide: what makes studies comparable? Stroke 1996; 27:550–558. 9 Aho K, Harmsen P, Hatano S, Marquardsen J, Smirnov VE, Strasser T: Cerebrovascular disease in the community: results of a WHO collaborative study. Bull World Health Organ 1980;58:113–130. 10 Castillo V, Bogousslavski J: Early classification of stroke. Cerebrovasc Dis 1997; 7(suppl 3):5–11. 11 Díaz-Guzmán J, Egido-Herrero JA, Fuentes B, Fernández-Pérez C, Gabriel-Sánchez R, Barberà G, Abilleira S; Proyecto Ictus del Grupo de Estudio de Enfermedades Cerebrovasculares de la Sociedad Española de Neurología: Incidence of strokes in Spain: the Iberictus study. Data from the pilot study. Rev Neurol 2009;48:61–65. 12 Spain demographics. http://www.ine.es (accessed March 2011). 13 European population. http://nui.epp.eurostat.ec.europa.eu/nui/show.do?dataset= demo_pjan&lang=en (accessed March 2011). 14 Feigin VL, Lawes CMM, Bennett DA, Anderson CS: Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol 2003;2:43–53. 15 Rothwell PM, Coull AJ, Giles MF, Howard SC, Silver LE, Bull LM, Gutnikov SA, Edwards P, Mant D, Sackley CM, Farmer A, Sandercock PA, Dennis MS, Warlow CP, Bamford JM, Anslow P; Oxford Vascular Study: Change in stroke incidence, mortality, case-fatality, severity, and risk factors in Oxfordshire, UK from 1981 to 2004 (Oxford Vascular Study). Lancet 2004; 363: 1925– 1933. Cerebrovasc Dis 2012;34:272–281 16 Vibo R, Körv J, Haldre S, Roose M: First-year results of the Third Stroke Registry in Tartu, Estonia. Cerebrovasc Dis 2004;18:227–231. 17 Wolf CDA, Giroud M, Kolomisky-Rabas P, Dundas R, Lemesle M, Heuschmann P, Rudd A: Variations in stroke incidence and survival in 3 areas of Europe. European Registries of Stroke (EROS) Collaboration. Stroke 2000;31:2074–2079. 18 Kolominsky-Rabas PL, Sarti C, Heuschmann PU, Graf C, Siemonsen S, Neundoerfer B, Katalinic A, Lang E, Gassmann KG, von Stockert TR: A prospective communitybased study of stroke in Germany – the Erlangen Stroke Project (ESPro). Stroke 1998; 29:2501–2506. 19 Carolei A, Marini C, Di Napoli M, Di Gianfilippo G, Santalucia P, Baldassarre M, De Matteis G, di Orio F: High stroke incidence in the prospective community-based L’Aquila registry (1994–1998). First year’s results. Stroke 1997; 28:2500–2506. 20 Ellekjaer H, Holmen J, Indredavik B, Terent A: Epidemiology of stroke in Inherred, Norway, 1994 to 1996. Stroke 1997;28:2180–2184. 21 Johansson B, Norrving B, Lindgren A: Increased stroke incidence in Lund-Orup, Sweden, between 1983 to 1985 and 1993 to 1995. Stroke 2000; 31:481–486. 22 Brown RD, Whisnant JP, Sicks JD, O’Fallon WM, Wiebers DO: Stroke incidence, prevalence, and survival: secular trends in Rochester, Minnesota, through 1989. Stroke 1996; 27:373–380. 23 European Registers of Stroke (EROS) Investigators: Incidence of stroke in Europe at the beginning of the 21st Century. Stroke 2009; 40:1557–1563. Díaz-Guzmán et al. Downloaded by: Kainan University 203.64.11.45 - 2/3/2015 3:20:43 PM 1 Bonita R, Mendis S, Truelsen T, Bogousslavsky J, Toole J, Yatsu F: The Global Stroke Initiative. Lancet Neurol 2004;3:391–393. 2 Thorvaldsen P, Asplund K, Kuulasmaa K, Rajakangas AM, Shroll M: Stroke incidence, case fatality, and mortality in the WHO MONICA project. World Health Organization Monitoring Trends and Determinants in Cardiovascular Disease. Stroke 1995; 26: 361–367. 3 Asplund K, Bonita R, Kuulasmaa K, Rajakangas AM, Schaedlich H, Suzuki K, Thorvaldsen P, Tuomilehto J: Multinational comparisons of stroke epidemiology. Evaluation of case ascertainment in the WHO MONICA Stroke Study. World Health Organization Monitoring Trends and Determinants in Cardiovascular Disease. Stroke 1995; 26: 355–360. 4 Medrano Alberto MJ, Boix Martinez R, Cerrato Crespan E, Ramirez Santa-Pau M: Incidence and prevalence of ischaemic heart disease and cerebrovascular disease in Spain: a systematic review of the literature. Rev Esp Salud Pública 2006;80:5–15. 5 Díaz-Guzmán J, Egido-Herrero JA, GabrielSánchez R, Barberà G, Fuentes B, FernándezPérez C, Abilleira S; Proyecto Ictus del Grupo de Estudio de Enfermedades Cerebrovasculares de la Sociedad Española de Neurología: Incidence of strokes in Spain. Methodological foundations of the Iberictus Study (in Spanish). Rev Neurol 2008;47:617–623. 6 Population 2005 census of the Spanish National Institute of Statistics. http://www.ine. es (accessed March 2011). 7 Malmgren R, Warlow C, Bamford J, Sandercork P: Geographical and secular trends in stroke incidence. Lancet 1987; 2:1197–1198. Stroke Incidence Rate in Spain 29 Feigin VL, Shishkin SV, Tzirkin GM, Vinogradova TE, Tarasov AV, Vinogradov SP, Nikitin YP: A population-based study of transient ischemic attack incidence in Novosibirsk, Russia, 1987–1988 and 1996–1997. Stroke 2000;51:9–13. 30 Edlow JA, Kim S, Pelletier AJ, Camargo CA Jr: National study on emergency department visits for transient ischemic attack, 1992– 2001. Acad Emerg Med 2006;13:666–672. 31 Kleindorfer D, Panagos P, Pancioli A, Khoury J, Kissela B, Woo D, Schneider A, Alwell K, Jauch E, Miller R, Moomaw C, Shukla R, Broderick JP: Incidence and short-term prognosis of transient ischemic attack in a population-based study. Stroke 2005; 36: 720–723. 32 Rothwell PM, Warlow CP: Timing of TIAs preceding stroke: time window for prevention is very short. Neurology 2005; 64: 817– 820. 33 Correia M, Silva MR, Magalhaes R, Guimaraes L, Silva MC: Transient ischemic attacks in rural and urban northern Portugal: incidence and short-term prognosis. Stroke 2006;37:50–55. 34 Ueda K, Kiyohara Y, Hasuo Y, Yanai T, Kawano H, Wada J, Kato I, Kajiwara E, Omae T, Fujishima M: Transient cerebral ischemic attacks in a Japanese community, Hiyasama, Japan. Stroke 1987; 18:844–848. 35 Urakami K, Igo M, Takahashi K: An epidemiologic study of cerebrovascular disease in Western Japan: with special reference to transient ischemic attacks. Stroke 1987; 18: 396–401. 36 Vaartjes I, Reitsma JB, de Bruin A, Bergervan Sijl M, Bos MJ, Breteler MM, Grobbee DE, Bots ML: Nationwide incidence of first stroke and TIA in the Netherlands. Eur J Neurol 2008;15:1315–1323. 37 Amort M, Fluri F, Schäfer J, Weisskopf F, Katan M, Burow A, Bucher HC, Bonati LH, Lyrer PA, Engelter ST: Transient ischemic attack versus transient ischemic attack mimics: frequency, clinical characteristics and outcome. Cerebrovasc Dis 2011;32:57–64. Cerebrovasc Dis 2012;34:272–281 281 Downloaded by: Kainan University 203.64.11.45 - 2/3/2015 3:20:43 PM 24 Béjot Y, Rouaud O, Jacquin A, Osseby GV, Durier J, Manckoundia P, Pfitzenmeyer P, Moreau T, Giroud M: Stroke in the very old: incidence, risk factors, clinical features, outcomes and access to resources – a 22-year population-based study. Cerebrovasc Dis 2010;29:111–21 25 Mihalka L, Smolanka V, Bulecza B, Mulesa S, Bereczki D: A population study of stroke in West-Ukraine. Stroke 2001;32:2227–2231. 26 Vemmos KN, Bots ML, Tsibouris PK, et al: Stroke incidence and case-fatality in Southern Greece. Stroke 1999; 30:36–70. 27 Correia M, Silva MR, Matos I, Magalhaes R, Castro J, Ferro JM: Prospective communitybased study of stroke in Northern Portugal. Incidence and case fatality in rural and urban populations. Stroke 2004;35:2048–2053. 28 de Rooij NK, Linn FHH, van der Plas JA, Algra A, Rinkel GJE: Incidence of subarachnoid haemorrhage: a systematic review with emphasis on region, age, gender and time trends. J Neurol Neurosurg Psychiatry 2007; 78:1365–1372.
Anuncio
Documentos relacionados
Descargar
Anuncio
Añadir este documento a la recogida (s)
Puede agregar este documento a su colección de estudio (s)
Iniciar sesión Disponible sólo para usuarios autorizadosAñadir a este documento guardado
Puede agregar este documento a su lista guardada
Iniciar sesión Disponible sólo para usuarios autorizados