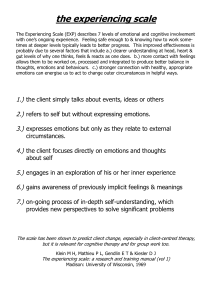
Stroke ORIGINAL CONTRIBUTION Rehabilitation of Cognitive Deficits Poststroke: Systematic Review and Meta-Analysis of Randomized Controlled Trials Mairead O'Donoghue , BSc; Siobhan Leahy , PhD; Pauline Boland , PhD; Rose Galvin , PhD; John McManus, MD; Sara Hayes , PhD BACKGROUND: Despite the prevalence of cognitive impairment poststroke, there is uncertainty regarding interventions to improve cognitive function poststroke. This systematic review and meta-analysis evaluate the effectiveness of rehabilitation interventions across multiple domains of cognitive function. METHODS: Five databases were searched from inception to August 2019. Eligible studies included randomized controlled trials of rehabilitation interventions for people with stroke when compared with other active interventions or standard care where cognitive function was an outcome. Downloaded from http://ahajournals.org by [email protected] on February 4, 2022 RESULTS: Sixty-four randomized controlled trials (n=4005 participants) were included. Multiple component interventions improved general cognitive functioning (MD, 1.56 [95% CI, 0.69–2.43]) and memory (standardized MD, 0.49 [95% CI, 0.27– 0.72]) compared with standard care. Physical activity interventions improved neglect (MD, 13.99 [95% CI, 12.67–15.32]) and balance (MD, 2.97 [95% CI, 0.71–5.23]) compared with active controls. Noninvasive brain stimulation impacted neglect (MD, 20.79 [95% CI, 14.53–27.04) and functional status (MD, 14.02 [95% CI, 8.41–19.62]) compared with active controls. Neither cognitive rehabilitation (MD, 0.37 [95% CI, −0.94 to 1.69]) nor occupational-based interventions (MD, 0.45 [95% CI, −1.33 to 2.23]) had a significant effect on cognitive function compared with standard care. CONCLUSIONS: There is some evidence to support multiple component interventions, physical activity interventions, and noninvasive brain stimulation improving cognitive function poststroke. Findings must be interpreted with caution given the overall moderate to high risk of bias, heterogeneity of interventions, and outcome measures across studies. GRAPHIC ABSTRACT: A graphic abstract is available for this article. Key Words: activities of daily living ◼ brain ◼ cognition ◼ meta-analysis ◼ stroke ◼ systematic review S troke is one of the leading causes of death and disability worldwide.1 Cognitive impairment is reported in up to 57% of ischemic stroke survivors at 6 months poststroke2 and is shown to be independently associated with lower quality of life,3 higher rates of mortality and institutionalization,4 increased carer burden,5 and increased healthcare costs.6 A priority-setting partnership in the United Kingdom identified that cognitive impairment poststroke was among the top 10 research priorities for people living with stroke.7 Recent international consensus-based core recommendations identify cognitive function poststroke as an area of unmet need for people poststroke.8 However, much rehabilitation focus is placed on motor deficits, often neglecting hidden cognitive deficits.9,10 For example, a meta-summary of qualitative studies exploring stroke survivors’ experiences of rehabilitation found that an emphasis is placed on the rehabilitation of Correspondence to: Mairéad O’Donoghue, BSc, Physiotherapy Department, School of Allied Health, University of Limerick, Ireland, V94 T9PX. Email mairead. [email protected] Supplemental Material is available at https://www.ahajournals.org/doi/suppl/10.1161/STROKEAHA.121.034218. For Sources of Funding and Disclosures, see page xxx. © 2022 American Heart Association, Inc. Stroke is available at www.ahajournals.org/journal/str Stroke. 2022;53:00–00. DOI: 10.1161/STROKEAHA.121.034218 May 2022 1 Original Contribution Donoghue et al Nonstandard Abbreviations and Acronyms MoCA Montreal Cognitive Assessment NIBS noninvasive brain stimulation rTMSrepetitive transcranial magnetic stimulation Downloaded from http://ahajournals.org by [email protected] on February 4, 2022 physical deficits over nonphysical needs such as social reintegration.11 As illustrated by the diversity and range of neuropsychological assessments, cognition is not a unitary concept.12,13 Cognitive impairment poststroke encompasses a variety of deficits across multiple domains and typically includes memory, attention, executive function, language, and visuoperceptual ability.14 Various cognitive domains enable complex mental processes to occur, which allow an individual to select and process information within their environment.15 Cognitive rehabilitation is defined as “a systematic functionally orientated intervention of therapeutic cognitive activities based on the assessment and understanding of the patient’s brain behavior deficits”.15 Previous Cochrane reviews have explored the effectiveness of cognitive rehabilitation interventions on a specific domain of cognitive function poststroke, such as attention, memory, executive function, limb apraxia, neglect, and perception.16–21 An overview by Gillespie et al22 synthesized evidence across these Cochrane reviews and reported favorable outcomes of cognitive rehabilitation across the domains of attention, spatial neglect, and motor apraxia immediately postintervention, but these improvements are not likely to persist in the long term and do not improve the everyday functioning of the individual poststroke.22 Focusing on outcomes relating to any single domain of cognitive function poststroke may be overly simplistic, given the often diffuse and interconnected cognitive impairments present in individuals poststroke.23 Studies focusing on the rehabilitation of single cognitive domains fail to capture the interrelated and highly overlapping nature of cognitive domains.12,23,24 There remains a need to move beyond the narrow scope of specific cognitive rehabilitation interventions focusing on one specific domain of cognitive function. A breadth of intervention modalities impact cognitive function for people living with stroke, including virtual reality training, physical activity interventions and neuro-feedback therapy,25–27 and many more. Given the known interactions of cognitive domains required for optimal function and quality of life poststroke, alongside the broad range of possible interventions, the effects of interventions across all domains of cognitive function poststroke requires examination. 2 May 2022 Rehabilitation of Cognitive Deficits Poststroke To our knowledge, there is no systematic review that has examined the effectiveness of all types of rehabilitation interventions, across multiple domains of cognitive function poststroke. Therefore, in addition to general cognitive function, this review includes outcomes on cognitive deficits across the domains of attention, memory, executive function, perception, limb apraxia, and neglect, and examines the effectiveness of nonpharmacological rehabilitation interventions across these multiple domains of cognitive function poststroke. METHODS Study Design This systematic review and meta-analysis were conducted in accordance with the Preferred Items for Systematic Reviews Meta-Analyses statement.28 The review protocol was registered with the International Prospective Register of Systematic Reviews (https://www.crd.york.ac.uk/PROSPERO/; Unique identifier: CRD42019125289) and has been published previously.29 Data available on request from the authors. Eligibility Criteria Types of Study Randomized controlled trials and quasi-randomized control trials, as defined by the Cochrane Handbook for Systematic Reviews of Interventions were included.30 Feasibility studies and pilot studies were also included. Studies published in the English language with full text available were included. Participants Studies that included adults aged 18 years or older with a clinical diagnosis of ischemic or hemorrhagic stroke, in the acute, subacute, or chronic stage poststroke were included. As outlined in the review protocol, people poststroke with a confirmed cognitive impairment were to be included. However, the current review includes individuals poststroke with or without a confirmed cognitive impairment. Mixed cause studies (eg, traumatic brain injury and stroke mix) were included only if separate data for people poststroke was extractable. Interventions Interventions of which the primary or secondary aim is to improve cognitive function after stroke were included. Interventions of any duration or conducted at any time since stroke were included. Pharmacological interventions (including over-the-counter medications) were excluded. Controls Studies comparing an intervention that affects cognitive function poststroke with standard care, no treatment control, waitlist control, or active control were included. Outcomes Change in cognitive function postintervention in individuals poststroke was the primary outcome of interest. Outcome measures that focused on general cognitive status, or ≥1 domain-specific aspects of cognition such as executive function, attention, memory, perception, limb apraxia, and neglect Stroke. 2022;53:00–00. DOI: 10.1161/STROKEAHA.121.034218 Donoghue et al Search The following databases were searched: PubMed, Embase, CENTRAL, PsycInfo, and CinAHL. The Vista and ClinicTrials. gov databases were also searched for potentially eligible ongoing clinical trials. The search was carried out from inception to October 2019. For details of the search strategy, see the Supplemental Material. Screening The searches were exported and saved in a master reference management library (Clarivate Analytics Endnote X7) and duplicates were removed. Titles, abstracts, and full texts were screened independently by 2 review authors (M.O.D. and S.H., P.B., or R.G.). Any disagreements regarding full-text eligibility were resolved by discussion among all authors. Data Extraction Downloaded from http://ahajournals.org by [email protected] on February 4, 2022 Data, including author, study design, sample size, population characteristics (age, type of stroke, time since stroke), intervention characteristics (intervention type, intervention content, duration of intervention, setting of intervention), control group (standard care, waitlist control or active control), primary and secondary outcomes postintervention were extracted and entered into a standardized recording data extraction form. Study authors were contacted for missing data or further information. Data were recorded as mean and SD where possible for studies at postintervention and follow-up. group (standard control, active control, or waitlist control). Where studies presented data from multiple intervention/ control groups, all relevant interventions/control groups were combined into a single group and analyzed accordingly.30 Subgroup analysis was performed where pooled studies included participants that were <3 months poststroke, between 3 and 6 months poststroke, and >6 months poststroke. We previously outlined that a narrative synthesis would be provided on studies not included in the meta-analysis.29 However, due to the number of studies identified and range of outcome measures used, the characteristics of all studies (n=64) were reported but a narrative synthesis of studies that did not provide data for the meta-analysis was not performed. Outcomes are listed according to general cognitive functioning and the following cognitive domains: attention, memory, executive function, perception, apraxia, neglect. The impact of heterogeneity on results was assessed using the I2 statistic. When the I2 was <50% there was little concern about statistical heterogeneity.30 Random-effects models were used where there was statistical heterogeneity≥50%.30 RESULTS Searches yielded a total of 66 578 studies, with 25 215 duplicates removed, resulting in 41 363 titles and abstracts screened for eligibility. Following title and abstract screening, 277 full-text studies were screened for eligibility. Out of these full texts, 64 studies met the inclusion criteria, with 42 of these studies having suitable data for meta-analysis (Figure 1). The additional 22 studies were unsuitable for meta-analysis and so descriptive data is available for these studies. Please see the Supplemental Material. Risk of Bias Two authors (M.O.D. and either S.H., S.L., or R.G.) independently assessed the validity of studies using the Cochrane Risk of Bias Tool. Bias was assessed as low, unclear, or high for individual components from 5 domains: selection bias, performance bias, attrition bias, reporting bias, and other bias. Disagreements were resolved by group consensus. Data Synthesis Separate analyses were performed for trials comparing cognitive interventions with a standard care control, or with a waitlist control intervention, and trials comparing 2 active interventions. Interventions were classified into 6 categories for analysis as follows: multiple component interventions, cognitive rehabilitation interventions, physical activity interventions, noninvasive brain stimulation protocols (NIBS), occupational-based interventions, and other interventions. For details on the categorization of these interventions, please see the Supplemental Material. Meta-analyses were conducted using the Cochrane Review Manager software (RevMan 5.3). For continuous data, the treatment effect was calculated using standardized mean differences (SMD) and 95% CI where different studies used different scales to assess the same outcome and using mean differences (MD) and 95% CI where studies used the same scales to measure relevant outcomes. Analyses are presented according to the type of intervention compared with a control Stroke. 2022;53:00–00. DOI: 10.1161/STROKEAHA.121.034218 Characteristics of Included Studies Of the 64 studies included in this review, 21 were multiple component interventions, 16 were cognitive rehabilitation interventions, 11 were physical activity interventions, 6 were NIBS protocols, 5 were occupational-based interventions, and 5 were other interventions. For the characteristics of included studies, please see the Supplemental Material. The 64 included studies yielded a total of 4005 participants. Sample sizes ranged from nine participants to 225 participants. The mean age of participants was 62.5 years, ranging from 45 years to 76 years. The mean time since stroke onset was 20.03 months, ranging from 48 hours since stroke onset to 6.25 years poststroke. Twenty studies (31%) were conducted in the acute phase (≤3 months poststroke), 12 studies (19%) were conducted in the subacute phase (>3-6 months poststroke), 18 studies (28%) were conducted during the chronic stage (>6 months poststroke), and 14 studies (22%) had no data relating to time since stroke. Twenty-five studies (39%) included both ischemic and hemorrhagic types of stroke, 8 studies (12.5 %) reported May 2022 3 Original Contribution in line with Australian Clinical Guidelines for Stroke (2020) were included. Cognitive outcome measures related to cognitive domains other than those listed were excluded. Cognitive screening tools were also included. Secondary outcome measures included quality of life, using stroke-specific or generic quality of life measures, functional abilities, mobility, balance, and depression. Rehabilitation of Cognitive Deficits Poststroke Rehabilitation of Cognitive Deficits Poststroke Original Contribution Donoghue et al Downloaded from http://ahajournals.org by [email protected] on February 4, 2022 Figure 1. PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow chart of study selection. *The characteristics of all studies (n=64) were reported but a narrative synthesis of studies that did not provide data for the meta-analysis was not performed (n=22). on ischemic stroke only, 8 studies (12.5%) reported on left-sided/ right-sided stroke, and 23 studies (36%) had no data relating to type of stroke. 4 May 2022 Twenty-four studies (38%) recruited their participants from an inpatient acute setting, 15 studies (23%) recruited from a rehabilitation setting, 18 studies (28%) Stroke. 2022;53:00–00. DOI: 10.1161/STROKEAHA.121.034218 Donoghue et al I2=0%). For figures of these results, please see the Supplemental Material. Multiple Component Interventions Memory Four studies reported a measure of memory using the forward digital span test, the letter-number sequencing test, and the Digital Span test post multiple component intervention compared with a standard control. There was an effect in favor of the intervention group (SMD, 0.49 [95% CI, 0.27–0.72]; I2= 0%; Figure 3). Subgroup analysis demonstrated that studies >6 months did not show an effect in favor of the intervention group (SMD, 0.32 [95% CI, −0.03 to 0.67]; I2=0%). Two studies, one between 3 and 6 months poststroke and one >6 months poststroke, reported a measure of spatial and visual memory using the forward Visual Span Test post multiple component intervention compared with a standard control. There was an effect in favor of the intervention group (MD, 0.98 [95% CI, 0.33–1.64]; I2=0%). For figures of these results, please see the Supplemental Material. There was no evidence of an effect in favor of multiple component interventions compared with a standard control group for the cognitive domains of general cognitive function as measured by the MiniMental State Examination (MD, 1.20 [95% CI, −0.28 to 2.67]), attention (MD, 0.01 [95% CI, −0.08 to 0.11]), perception (SMD, 0.14 [95% CI, −0.16 to 0.45]), and on secondary outcomes of depression (SMD, −0.26 [95% CI, −0.57 to 0.06]) and quality of life (SMD, 0.19 [95% CI, −0.24 to 0.63]). There was no evidence of an effect in favor of multiple component interventions compared with an active control for the domain of neglect (MD, 4.98 [95% CI, −33.29 to 43.24]). General Cognitive Function Three studies reported a measure of general cognitive function using the Montreal Cognitive Assessment, post multiple component intervention compared with standard control. There was a significant effect in favor of the intervention group (MD, 1.56 [95% CI, 0.69–2.43]; I2=30%; Figure 2). This effect was maintained for studies <3 months poststroke (MD, 2.38 [95% CI, 0.97–3.80]; Secondary Outcomes Four studies reported a measure of functional status using the Barthel Index, the modified Barthel Index, and the Functional Independence Measure post multiple component intervention compared with a standard control. An effect was found in favor of the intervention group (SMD, 0.33 [95% CI, 0.05–0.62]; I2=61%). Subgroup analysis did not show an effect for studies that were <3 Risk of Bias The risk of bias in the 64 included studies was generally mixed, with a high risk of performance bias due to incomplete blinding of participants or personnel in 22 studies, a high risk of other bias due to inadequate sample sizes or conflicts of interest in 15 studies, a high risk of detection bias due to lack of blinded outcome assessment in nine studies, a high risk of attrition bias due to incomplete outcome data in 6 studies, a high risk of reporting bias associated with selective reporting of outcomes in 2 studies, and a high risk of selection bias associated with random sequence generation in one study. For complete Cochrane Risk of Bias results, please see the Supplemental Material. Effect of Interventions Downloaded from http://ahajournals.org by [email protected] on February 4, 2022 Results of the meta-analysis are presented below according to intervention type. Data have been pooled in accordance with each intervention classification as follows: multiple component interventions, cognitive rehabilitation interventions, physical activity interventions, NIBS protocols, occupational-based interventions, and other interventions. Figure 2. Forest plot of general cognitive function outcomes, multiple component intervention vs standard control. Stroke. 2022;53:00–00. DOI: 10.1161/STROKEAHA.121.034218 May 2022 5 Original Contribution recruited from an outpatient service, and 7 studies (11%) recruited from both an inpatient and outpatient setting. Forty-one studies (64%) recruited their participants from an inpatient acute setting, 13 studies (20%) recruited from an outpatient service, whereas 4 studies (6.5%) recruited from both an inpatient and outpatient setting. Six studies (9.5%) recruited from community settings. Rehabilitation of Cognitive Deficits Poststroke Rehabilitation of Cognitive Deficits Poststroke Original Contribution Donoghue et al Figure 3. Forest plot of memory outcomes, multiple component intervention vs standard control. months poststroke or >6 months poststroke. For figures of these results, please see the Supplemental Material. Cognitive Rehabilitation Interventions Downloaded from http://ahajournals.org by [email protected] on February 4, 2022 There was no evidence of an effect in favor of cognitive rehabilitation interventions when compared with a standard control for general cognitive function (MD, 0.37 [95% CI, −0.94 to 1.69]), memory (MD, 1.54 [95% CI, −1.90 to 4.98]), executive function (MD, 0.44 [95% CI, −1.94 to 2.82]), neglect (SMD, 0.26 [95% CI, −0.18 to 0.71]), or on secondary outcomes of quality of life (SMD, 0.17 [95% CI, −0.18 to 0.52]). There was no evidence of an effect in favor of cognitive rehabilitation interventions when compared with an active control for general cognitive functioning (MD, 0.83 [95% CI, −1.04 to 2.71]), memory (MD, −2.27 [95% CI, −6.06 to 1.52]), executive function (MD, −53.45 [95% CI, −148.26 to 41.36]), or attention (SMD, −0.05 [95% CI, −1.02 to 0.91]). There was no evidence of an effect in favor of cognitive rehabilitation interventions when compared with a waitlist control for the cognitive domain of memory (SMD, 0.63 [95% CI, −0.27 to 1.52]). Physical Activity Interventions Neglect Two studies, both <3 months poststroke, reported a measure of neglect using the Star Cancellation Test when comparing a physical activity intervention to an active control group of sham mirror therapy. There was an effect in favor of the control group (MD, 13.99 [95% CI, 12.67–15.32]; I2=0%)(Figure 4). Secondary Outcomes Two studies, both >6 months poststroke, reported a measure of balance using the Berg Balance Scale when compared with an active control group (stretching group). There was an effect in favor of the intervention group (MD, 2.97 [95% CI, 0.71–5.23]; I2=0%). For figures of these results, please see the Supplemental Material. There was no evidence of an effect of physical activity interventions when compared with an active control for the cognitive domains executive function (MD, –1.92 [95% CI, –28.68 to 24.84]). NIBS Interventions Neglect Three studies reported a measure of neglect using the line bisection test when compared with an active control of sham repetitive transcranial magnetic stimulation therapy (rTMS). There was an effect in favor of the intervention group (MD, 20.79 [95% CI, 14.53– 27.04]; I2=79%)(Figure 5). Subgroup analysis of studies between 3-6 months also found an effect in favor of the intervention group (MD, 18.74 [95% CI, 11.50– 25.99]; I2=78%). For figures of these results, please see the Supplemental Material. Two studies, one <3 months poststroke and one between 3 and 6 months poststroke reported a measure of neglect using the Star Cancellation Test when compared with an active control of sham rTMS therapy. There was an effect in favor of the active control group (MD, −5.57 [95% CI, −8.53 to −2.61]; I2=99%; Figure 6). Secondary Outcomes Two studies, one <3 months poststroke and one >6 months poststroke, reported a measure of functional status using the Modified Barthel Index and the Korean version of the Modified Barthel Index when compared with an active control of rTMS therapy. There was an effect in favor of the intervention group (MD, 14.02 [95% CI, 8.41–19.62]; I2=0%). For figures of these results, please see the Supplemental Material. Figure 4. Forest plot of neglect outcomes, physical activity (mirror therapy) intervention vs sham mirror therapy. 6 May 2022 Stroke. 2022;53:00–00. DOI: 10.1161/STROKEAHA.121.034218 Donoghue et al Rehabilitation of Cognitive Deficits Poststroke Occupational-Based Interventions There was no evidence of an effect of occupationalbased interventions when compared with a standard control for general cognitive functioning (MD, 0.45 [95% CI, −1.33 to 2.23]) or the secondary outcome of functional status (SMD, 0.31 [95% CI, −0.03 to 0.65]). Subgroup analysis revealed that studies <3 months poststroke showed an effect in favor of the intervention group for general cognitive functioning (MD, 0.39 [95% CI, 0.02– 0.76]; I2=0%). For figures of these results, please see the Supplemental Material. Other Interventions Downloaded from http://ahajournals.org by [email protected] on February 4, 2022 There was no evidence of an effect of other interventions, that is, prism adaptation therapy, when compared with an active control group for the cognitive domain of neglect (SMD, 0.40 [95% CI, −0.06 to 0.85]). DISCUSSION This comprehensive systematic review examined the totality of evidence regarding the effectiveness of nonpharmacological interventions on cognitive deficits poststroke. Findings exhibited the range of rehabilitation approaches that may be effective in improving cognitive deficits poststroke. Multiple component interventions demonstrated favorable effects on outcomes of general cognitive functioning and memory when compared with standard care. Physical activity interventions and NIBS protocols were also effective on a range of cognitive and secondary outcomes. Despite research involving over 4000 individuals across 64 randomized controlled trials, the evidence base presented in this review demonstrated several methodological shortcomings and unanswered questions regarding the optimal design and delivery of interventions to rehabilitate cognitive deficits poststroke. Furthermore, the overall moderate certainty of evidence and high risk of bias for various methodological domains must be acknowledged. The most consistent evidence in this review supported multiple component interventions, with significant improvement demonstrated for general cognitive function and memory. Evidence from three pooled studies using multiple component interventions indicated a positive effect in general cognitive functioning. Within this analysis of multiple component interventions, cognitive rehabilitation training was used in conjunction with a form of physical activity, such as systemic coordination training,31 conventional occupational therapy/physiotherapy,32 or an acupuncture treatment.33 However, given the very low clinically meaningful effect of this outcome,34 the practical and clinical importance of multiple component interventions on outcomes of general cognitive function should be interpreted with caution. Evidence from 2 pooled studies indicated a large effect for spatial and visual memory outcomes post computerized cognitive rehabilitation,35 in conjunction with traditional rehabilitation therapy consisting of physical therapy and occupational therapy.36 Previous evidence suggests that a combination of physical activity and cognitive rehabilitation may facilitate greater improvements in relation to cognitive impairment in both older adults and individuals poststroke, respectively.37,38 Although there is relatively limited literature regarding the use of multiple component interventions in individuals poststroke, combined cognitive interventions and physical activity have shown positive effects on cognitive functioning in persons with dementia39 and traumatic brain injury.40 In their review of evidence-based cognitive rehabilitation, Cicerone et al40 recommended that programs of comprehensive, holistic neuropsychological rehabilitation can improve outcomes relating to community integration and Figure 6. Forest plot of neglect outcomes (Star Cancellation Test), repetitive transcranial magnetic stimulation (rTMS) protocol vs sham rTMS protocol. Stroke. 2022;53:00–00. DOI: 10.1161/STROKEAHA.121.034218 May 2022 7 Original Contribution Figure 5. Forest plot of neglect outcomes (line bisection test), repetitive transcranial magnetic stimulation (rTMS) vs sham rTMS. Original Contribution Donoghue et al Downloaded from http://ahajournals.org by [email protected] on February 4, 2022 functional independence and recommends that such programs be provided to reduce both cognitive and functional impairments. However, it should be noted that these recommendations were based on studies examining a mixed cohort of individuals poststroke and posttraumatic brain injury and should be extrapolated with caution. Furthermore, given the heterogeneity of interventions across studies in the current review, it remains difficult to make recommendations regarding the optimal design and delivery of a multiple component intervention for individual’s poststroke. Nevertheless, the provision of two or more interventions may be more effective compared with usual care and as such, a combination is, therefore, more likely than many single-component interventions to reduce cognitive dysfunction poststroke. In addition to the benefits of physical activity when combined with a form of cognitive training, this review found favorable results of single-component physical activity interventions. Trials by Pandian et al41 and Thieme et al42 found a significant improvement on outcomes of neglect post mirror therapy interventions of 4 and 5 weeks duration respectively. Both these studies were conducted in the acute to subacute phases poststroke and were in comparison with an active control group of sham mirror therapy. Mirror therapy is a feasible and effective intervention that can facilitate both motor and sensory improvements in the acute, subacute, and chronic phases poststroke.43 It remains unclear whether the intensity of exercise training affects cognitive outcomes poststroke.26 The benefits of physical activity on cognitive function are widely known in older adult populations.44,45 Physical activity and exercise prescription are recommended in the management of not only multiple physical but also psychosocial domains poststroke.46 However, uncertainty remains regarding the effects of such interventions specifically on cognitive function poststroke. A review by Cumming et al26 evaluated the effect of increased physical activity on cognitive functioning in individuals poststroke. Although this review demonstrated a significant effect favoring the use of physical activity interventions compared with active control groups on outcomes of neglect and balance, there was large variability between trials regarding the optimal frequency, intensity, timing, and type of physical activity intervention provided. Moreover, the assessment of cognitive function was rarely the primary outcome measure of these trials. Given the methodological shortcomings and small pool of studies within this review by Cumming et al,26 there was insufficient evidence to support clear recommendations for clinical practice. In their updated review examining the effects of fitness training poststroke, Saunders et al47 noted that outcomes of cognitive function in particular lack investigation, despite being ranked as the most important research priority relating to life after stroke.7 8 May 2022 Rehabilitation of Cognitive Deficits Poststroke Although meta-analytic evidence from the current review failed to demonstrate favorable effects of cognitive rehabilitation interventions on cognitive or secondary outcomes, Cicerone et al40 recommend external compensation strategies as a practice standard for the rehabilitation of memory deficits poststroke. However, in their updated review of cognitive rehabilitation for memory deficits poststroke, das Nair et al17 report insufficient evidence for memory rehabilitation due to poor methodological quality of current studies. Similar to the current review, das Nair et al17 noted lack of long-term effects of cognitive intervention on memory outcomes. In their updated meta-analysis, Loetscher et al48 examined 6 randomized controlled trials comparing cognitive rehabilitation with a standard care control group on outcomes of attention. Although there were no significant improvements in global attentional measures, the domain of divided attention improved significantly, but these effects did not persist long-term.48 Their review highlighted insufficient data to determine whether outcomes varied according to the frequency, intensity, or type of intervention.48 Given the key features of intervention design. that is, frequency, intensity, time, and type of cognitive rehabilitation interventions have yet to be established,8 it is unclear whether the intensity and duration of these interventions were justified. Meta-analytic evidence from this review suggests that NIBS protocols have a favorable effect on outcomes of neglect and performance in activities of daily living poststroke. NIBS, specifically rTMS, was found to have a large effect on neglect outcomes in the acute and subacute phase poststroke when compared with a sham stimulation group.49–51 Two of these studies combined NIBS with another treatment such as conventional therapy or sensory cueing respectively.49,51 Our review adds to the existing body of evidence and supports the findings of Salazar et al52 where NIBS, specifically rTMS and transcranial direct current stimulation, in conjunction with other therapies (such as visuospatial scanning training, conventional rehabilitation treatment, or feedback training) improved neglect in the acute and subacute phase poststroke. Thus, this combined approach, much like that of multiple component interventions, may result in more favorable clinical improvements on symptoms of neglect in individuals poststroke. However, this effect is limited as a result of the large heterogeneity observed in these analyses, suggesting that further studies are needed to determine the effects of NIBS protocols on outcomes of neglect. Subgroup analysis demonstrated favorable results of occupational-based interventions conducted less than 3 months poststroke on general cognitive functioning. Individual trials included in this review by Ntsiea et al53 and Skidmore et al54 found favorable effects in functional ability after a specific workplace intervention and a strategy training intervention respectively. These interventions incorporated goal setting and Stroke. 2022;53:00–00. DOI: 10.1161/STROKEAHA.121.034218 Donoghue et al Stroke. 2022;53:00–00. DOI: 10.1161/STROKEAHA.121.034218 that the MoCA displays excellent sensitivity but poor specificity.60 To this end, the MoCA may be particularly useful in people poststroke given the diffuse nature of cognitive impairment poststroke while also showing to have acceptable responsiveness and criterion validity in people poststroke receiving rehabilitation.34 Furthermore, it is not clear whether improvements in cognitive functioning lead to improvements in daily functioning or quality of life for the person poststroke. Nine out of the 42 included studies in our metaanalysis demonstrated improved measures of quality of life and/ or daily functioning outcomes, along with improved cognitive outcomes. Given the relatively small number of trials that reported improvements in these measures, there are insufficient trials to support or refute the use of the above interventions to improve quality of life and functional outcomes poststroke while simultaneously improving cognitive function. Although it is important to show the functional significance of these rehabilitation interventions, a causative effect of improved cognitive outcomes leading to improved quality of life or daily functioning outcomes cannot be assumed from these results. Strengths and Limitations To our knowledge, this is the first systematic review that examined all types of rehabilitation interventions across multiple domains of cognitive function for people poststroke. This review complied with the Preferred Items for Systematic Reviews and Meta-Analyses guidelines28 and employed a comprehensive search and screening strategy of peer-reviewed research. Unlike previous research which has focused on outcomes within a specific cognitive domain, we have included six domains of cognitive function, as outlined in the Australian Clinical Guidelines for Stroke (2020), as well as general cognitive functioning. Moreover, the comprehensive intervention categorization of included studies provides more in-depth analysis of the effectiveness of a breadth of rehabilitation approaches. This review has several important limitations. Concerning the domains of cognition examined, this review did not capture the multi-dimensional constructs of each cognitive domain. For example, the domain of memory can be subclassified into working memory, episodic memory, procedural memory, semantic memory, and prospective memory.61 Although we recognize the interconnected neural network and hierarchical structure of cognitive performance,23 the analysis of inter-domain interactions occurring during recovery poststroke was beyond the scope of this review. Furthermore, findings need to be interpreted with caution and considered in the context of high risk of bias across the following domains of bias: selection bias, performance bias, detection bias, attrition bias, reporting bias, and other biases. May 2022 9 Original Contribution Downloaded from http://ahajournals.org by [email protected] on February 4, 2022 self-management strategies. These findings are in contrast to a previous Cochrane review of occupational therapy poststroke which found no differences between groups for outcomes of general cognitive functioning or basic activities of daily living as assessed using the Barthel Index.55 However, it is of note that only one trial met the criteria for inclusion in this review.55 Unlike previous research in this area, meta-analytic evidence from the current systematic review evaluated an extensive range of rehabilitation interventions, including multiple component interventions, physical activity interventions, cognitive rehabilitation interventions, NIBS protocols, occupational interventions, and other interventions such as art therapy, prism adaptation, and music therapy. Given the breadth of interventions included in this review, there was extensive heterogeneity in relation to the intervention content, the duration, and dose of the intervention, the delivery of the intervention, and the domain of cognition targeted. To address this, we categorized intervention type accordingly and limited the heterogeneity in the meta-analyses. Furthermore, many of the included studies employed a standard care control group, with few studies describing the actual standard treatment delivered to the control group. This variation between studies raises challenges when aiming to determine the effectiveness of these types of rehabilitation interventions on cognitive deficits poststroke. Studies should provide a comprehensive description of intervention design to facilitate reliable intervention implementation and also to allow for replication in subsequent research.56 Future trialists should consider the Template for Intervention Description and Replication checklist to guide comprehensive and systematic reporting of interventions.57 Another factor adding to the diversity across studies was the lack of consensus between trials regarding assessment of cognitive impairment poststroke. The recent consensus-based recommendations from the Stroke Recovery and Rehabilitation Roundtable highlighted that no consensus was reached regarding a single approach to assessment of cognitive function poststroke.8 The need for assessments that are easily implementable and target the assessment of cognition across multiple cognitive domains was advocated.8 The National Institute for Neurological Disorders and Stroke and the Canadian Stroke Network recommend the use of common protocols for neuropsychological assessment in stroke-related research,58 which would address a current methodological limitation within stroke rehabilitation trials when such assessments cannot be compared.22 In the current review, there was substantial variability in both the quality and the types of cognitive outcome measures used. The MoCA assesses 6 cognitive domains including episodic memory, working memory, attention/ concentration, executive function, language, and visuospatial ability.59 Pooled data from a recent review demonstrated Rehabilitation of Cognitive Deficits Poststroke Original Contribution Donoghue et al The comprehensive and pragmatic intervention categorization of included studies provides an in-depth analysis of the effectiveness of rehabilitation approaches. However, the possibility of misclassification of intervention categorization within the analyses is acknowledged. Furthermore, the variation across trials also limited further possible analyses and although we are adding to the novelty of this evidence base, the existence of few homogeneous trials is a limitation. Rehabilitation of Cognitive Deficits Poststroke 3. 4. 5. 6. Conclusions The evidence regarding the effects of rehabilitation interventions to improve cognitive impairment poststroke remains uncertain. The evidence base presented demonstrates moderate and high risk of bias and suggests there is insufficient evidence to support or refute the effectiveness of rehabilitation interventions on cognitive impairment poststroke. Multiple component interventions, particularly those with a physical activity component, seem to have a favorable effect on memory and overall cognitive functioning. There is some evidence in r of physical activity interventions and NIBS protocols on the cognitive domains of memory and neglect. However, these findings must be interpreted with caution given the moderate certainty of evidence and high risk of bias for various methodological domains, extensive heterogeneity of interventions as well as outcome measures included in these studies. 7. 8. 9. 10. 11. 12. 13. Downloaded from http://ahajournals.org by [email protected] on February 4, 2022 14. ARTICLE INFORMATION Received January 15, 2021; final revision received August 25, 2021; accepted October 29, 2021. 15. Affiliations School of Allied Health, Ageing Research Centre, Faculty of Education and Health Sciences, Health Research Institute, University of Limerick, Ireland (M.O.D., S.L., P.B., R.G., S.H.). Geriatric and Stroke Medicine, University Hospital Limerick, Ireland (J.M.). Acknowledgments This work was funded by a PhD stipend from the School of Allied Health, University of Limerick. 16. 17. 18. Sources of Funding None. Disclosures None. Supplemental Material Tables S1–S4 Figures S1–S5 References 1–69 19. 20. 21. 22. REFERENCES 1. Krishnamurthi RV, Ikeda T, Feigin VL. Global, regional and country-specific burden of ischaemic stroke, intracerebral haemorrhage and subarachnoid haemorrhage: a systematic analysis of the global burden of disease study 2017. Neuroepidemiology. 2020;54:171–179. doi: 10.1159/000506396 2. Mellon L, Brewer L, Hall P, Horgan F, Williams D, Hickey A; ASPIRE-S study group. Cognitive impairment six months after ischaemic stroke: a 10 May 2022 23. 24. profile from the ASPIRE-S study. BMC Neurol. 2015;15:31. doi: 10.1186/ s12883-015-0288-2 Cumming TB, Brodtmann A, Darby D, Bernhardt J. The importance of cognition to quality of life after stroke. J Psychosom Res. 2014;77:374–379. doi: 10.1016/j.jpsychores.2014.08.009 Patel MD, Coshall C, Rudd AG, Wolfe CD. Cognitive impairment after stroke: clinical determinants and its associations with long-term stroke outcomes. J Am Geriatr Soc. 2002;50:700–706. doi: 10.1046/j.1532-5415.2002.50165.x Atteih S, Mellon L, Hall P, Brewer L, Horgan F, Williams D, Hickey A; ASPIRE-S study group. Implications of stroke for caregiver outcomes: findings from the ASPIRE-S study. Int J Stroke. 2015;10:918–923. doi: 10.1111/ijs.12535 Claesson L, Lindén T, Skoog I, Blomstrand C. Cognitive impairment after stroke–Impact on activities of daily living and costs of care for elderly people. Cerebrovasc Dis. 2005;19:102–109. doi: 10.1159/000082787 Pollock A, St George B, Fenton M, Firkins L. Top 10 research priorities relating to life after stroke–consensus from stroke survivors, caregivers, and health professionals. Int J Stroke. 2014;9:313–320. doi: 10.1111/j.1747-4949.2012.00942.x McDonald MW, Black SE, Copland DA, Corbett D, Dijkhuizen RM, Farr TD, Jeffers MS, Kalaria RN, Karayanidis F, Leff AP, et al. Cognition in stroke rehabilitation and recovery research: consensus-based core recommendations from the second Stroke Recovery and Rehabilitation Roundtable. Int J Stroke. 2019;14:774–782. doi: 10.1177/1747493019873600 Hochstenbach JB, den Otter R, Mulder TW. Cognitive recovery after stroke: a 2-year follow-up. Arch Phys Med Rehabil. 2003;84:1499–1504. doi: 10.1016/s0003-9993(03)00370-8 Jacova C, Pearce LA, Costello R, McClure LA, Holliday SL, Hart RG, Benavente OR. Cognitive impairment in lacunar strokes: the SPS3 trial. Ann Neurol. 2012;72:351–362. doi: 10.1002/ana.23733 Peoples H, Satink T, Steultjens E. Stroke survivors’ experiences of rehabilitation: a systematic review of qualitative studies. Scand J Occup Ther. 2011;18:163–171. doi: 10.3109/11038128.2010.509887 Lezak M, Howieson D, Loring D. Neuropsychological Assessment. 5th edn Oxford University Press. 2012. Sachdev PS, Blacker D, Blazer DG, Ganguli M, Jeste DV, Paulsen JS, Petersen RC. Classifying neurocognitive disorders: the DSM-5 approach. Nat Rev Neurol. 2014;10:634–642. doi: 10.1038/nrneurol.2014.181 Jokinen H, Melkas S, Ylikoski R, Pohjasvaara T, Kaste M, Erkinjuntti T, Hietanen M. Post-stroke cognitive impairment is common even after successful clinical recovery. Eur J Neurol. 2015;22:1288–1294. doi: 10.1111/ene.12743 Cicerone KD, Dahlberg C, Kalmar K, Langenbahn DM, Malec JF, Bergquist TF, Felicetti T, Giacino JT, Harley JP, Harrington DE, et al. Evidence-based cognitive rehabilitation: recommendations for clinical practice. Arch Phys Med Rehabil. 2000;81:1596–1615. doi: 10.1053/apmr.2000.19240 Loetscher T, Lincoln NB. Cognitive rehabilitation for attention deficits following stroke. Cochrane Database Syst Rev. 2013;2013:CD002842. doi: 10.1002/14651858.CD002842.pub2 das Nair R, Cogger H, Worthington E, Lincoln NB. Cognitive rehabilitation for memory deficits after stroke: an updated review. Stroke. 2017;48:e28–e29. Chung CS, Pollock A, Campbell T, Durward BR, Hagen S. Cognitive rehabilitation for executive dysfunction in adults with stroke or other adult non‐progressive acquired brain damage. Cochrane Database Syst Rev. 2013;2013:CD008391. doi: 10.1002/14651858.CD008391.pub2 West C, Bowen A, Hesketh A, Vail A. Interventions for motor apraxia following stroke. Cochrane Database Syst Rev. 2008;2008:CD004132. doi: 10.1002/14651858.CD004132.pub2 Bowen A, Hazelton C, Pollock A, Lincoln NB. Cognitive rehabilitation for spatial neglect following stroke. Cochrane Database Syst Rev. 2013;2013:CD003586. doi: 10.1002/14651858.CD003586.pub3 Bowen A, Knapp P, Gillespie D, Nicolson DJ, Vail A. Non-pharmacological interventions for perceptual disorders following stroke and other adult-acquired, non-progressive brain injury. Cochrane Database Syst Rev. 2011;2011:CD007039. doi: 10.1002/14651858.CD007039.pub2 Gillespie DC, Bowen A, Chung CS, Cockburn J, Knapp P, Pollock A. Rehabilitation for post-stroke cognitive impairment: an overview of recommendations arising from systematic reviews of current evidence. Clin Rehabil. 2015;29:120–128. doi: 10.1177/0269215514538982 Ramsey L, Siegel J, Lang C, Strube M, Shulman G, Corbetta M. Behavioural clusters and predictors of performance during recovery from stroke. Nat Hum Behav. 2017;1:0038. doi: 10.1038/s41562-016-0038 Tatemichi TK, Desmond DW, Stern Y, Paik M, Sano M, Bagiella E. Cognitive impairment after stroke: frequency, patterns, and relationship to Stroke. 2022;53:00–00. DOI: 10.1161/STROKEAHA.121.034218 Donoghue et al 26. 27. 28. 29. 30. 31. 32. 33. 34. Downloaded from http://ahajournals.org by [email protected] on February 4, 2022 35. 36. 37. 38. 39. 40. 41. 42. 43. Stroke. 2022;53:00–00. DOI: 10.1161/STROKEAHA.121.034218 44. Colcombe S, Kramer AF. Fitness effects on the cognitive function of older adults: a meta-analytic study. Psychol Sci. 2003;14:125–130. doi: 10.1111/1467-9280.t01-1-01430 45. Kramer AF, Erickson KI. Capitalizing on cortical plasticity: influence of physical activity on cognition and brain function. Trends Cogn Sci. 2007;11:342– 348. doi: 10.1016/j.tics.2007.06.009 46. Billinger SA, Arena R, Bernhardt J, Eng JJ, Franklin BA, Johnson CM, MacKay-Lyons M, Macko RF, Mead GE, Roth EJ, et al; American Heart Association Stroke Council; Council on Cardiovascular and Stroke Nursing; Council on Lifestyle and Cardiometabolic Health; Council on Epidemiology and Prevention; Council on Clinical Cardiology. Physical activity and exercise recommendations for stroke survivors: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45:2532–2553. doi: 10.1161/ STR.0000000000000022 47. Saunders DH, Sanderson M, Hayes S, Johnson L, Kramer S, Carter D, Jarvis H, Brazzelli M, Mead GE. Physical fitness training for patients with stroke. Stroke. 2020;51:e299–e300. doi: 10.1161/STROKEAHA.120.030826 48. Loetscher T, Potter K, Wong D, das Nair R. Cognitive rehabilitation for attention deficits following stroke. Cochrane Database Syst Rev. 2019;2019:CD002842. doi: 10.1002/14651858.CD002842.pub3 49. Cha HG, Kim MK. Effects of repetitive transcranial magnetic stimulation on arm function and decreasing unilateral spatial neglect in subacute stroke: a randomized controlled trial. Clin Rehabil. 2016;30:649–656. doi: 10.1177/0269215515598817 50. Kim BR, Chun MH, Kim DY, Lee SJ. Effect of high- and low-frequency repetitive transcranial magnetic stimulation on visuospatial neglect in patients with acute stroke: a double-blind, sham-controlled trial. Arch Phys Med Rehabil. 2013;94:803–807. doi: 10.1016/j.apmr.2012.12.016 51. Yang NY, Fong KN, Li-Tsang CW, Zhou D. Effects of repetitive transcranial magnetic stimulation combined with sensory cueing on unilateral neglect in subacute patients with right hemispheric stroke: a randomized controlled study. Clin Rehabil. 2017;31:1154–1163. doi: 10.1177/ 0269215516679712 52. Salazar APS, Vaz PG, Marchese RR, Stein C, Pinto C, Pagnussat AS. Noninvasive brain stimulation improves hemispatial neglect after stroke: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2018;99:355–366. e1. doi: 10.1016/j.apmr.2017.07.009 53. Ntsiea MV, Van Aswegen H, Lord S, Olorunju S S. The effect of a workplace intervention programme on return to work after stroke: a randomised controlled trial. Clin Rehabil. 2015;29:663–673. doi: 10.1177/ 0269215514554241 54. Skidmore ER, Dawson DR, Butters MA, Grattan ES, Juengst SB, Whyte EM, Begley A, Holm MB, Becker JT. Strategy training shows promise for addressing disability in the first 6 months after stroke. Neurorehabil Neural Repair. 2015;29:668–676 doi: 10.1177/1545968314562113 55. Hoffmann T, Bennett S, Koh C, McKenna KT. Occupational therapy for cognitive impairment in stroke patients. Cochrane Database Syst Rev. 2010;2010:CD006430. doi: 10.1002/14651858.CD006430.pub2 56. Glasziou P, Chalmers I, Altman DG, Bastian H, Boutron I, Brice A, Jamtvedt G, Farmer A, Ghersi D, Groves T, et al. Taking healthcare interventions from trial to practice. BMJ. 2010;341:c3852. doi: 10.1136/bmj.c3852 57. Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, Altman DG, Barbour V, Macdonald H, Johnston M, et al. Better reporting of interventions: Template for Intervention Description and Replication (TIDieR) checklist and guide. BMJ. 2014;348:g1687. doi: 10.1136/bmj.g1687 58. Hachinski V, Iadecola C, Petersen RC, Breteler MM, Nyenhuis DL, Black SE, Powers WJ, DeCarli C, Merino JG, Kalaria RN, et al. National Institute of Neurological Disorders and Stroke-Canadian Stroke Network vascular cognitive impairment harmonization standards. Stroke. 2006;37:2220–2241. doi: 10.1161/01.STR.0000237236.88823.47 59. Julayanont P, Nasreddine ZS. Montreal Cognitive Assessment (MoCA): concept and clinical review. In: Cognitive screening instruments. Springer; 2017:139–195. 60. Lees R, Selvarajah J, Fenton C, Pendlebury ST, Langhorne P, Stott DJ, Quinn TJ. Test accuracy of cognitive screening tests for diagnosis of dementia and multidomain cognitive impairment in stroke. Stroke. 2014;45:3008–3018. doi: 10.1161/STROKEAHA.114.005842 61. Harvey PD. Domains of cognition and their assessment. Dialogues Clin Neurosci. 2019;21:227–237. doi: 10.31887/DCNS.2019.21.3/pharvey May 2022 11 Original Contribution 25. functional abilities. J Neurol Neurosurg Psychiatry. 1994;57:202–207. doi: 10.1136/jnnp.57.2.202 Shin H, Kim K. Virtual reality for cognitive rehabilitation after brain injury: a systematic review. J Phys Ther Sci. 2015;27:2999–3002. doi: 10.1589/jpts.27.2999 Cumming TB, Tyedin K, Churilov L, Morris ME, Bernhardt J. The effect of physical activity on cognitive function after stroke: a systematic review. Int Psychogeriatr. 2012;24:557–567. doi: 10.1017/S1041610211001980 Renton T, Tibbles A, Topolovec-Vranic J. Neurofeedback as a form of cognitive rehabilitation therapy following stroke: a systematic review. PLoS One. 2017;12:e0177290. doi: 10.1371/journal.pone.0177290 Page M, McKenzie J, Bossuyt P. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. MetaArXiv. Preprints. 2020. O Donoghue M, Boland P, Galvin R, Coote S, Hayes S. Rehabilitation of cognitive deficits poststroke: protocol for a systematic review and meta-analysis of randomised controlled trials of non-pharmacological interventions. BMJ Open. 2019;9:e031052. doi: 10.1136/bmjopen-2019-031052 Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savović J, Schulz KF, Weeks L, Sterne JAC. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928 Cheng C, Liu X, Fan W, Bai X, Liu Z. Comprehensive rehabilitation training decreases cognitive impairment, anxiety, and depression in poststroke patients: a randomized, controlled study. J Stroke Cerebrovasc Dis. 2018;27:2613–2622. doi: 10.1016/j.jstrokecerebrovasdis.2018.05.038 Rogers JM, Duckworth J, Middleton S, Steenbergen B, Wilson PH. Elements virtual rehabilitation improves motor, cognitive, and functional outcomes in adult stroke: evidence from a randomized controlled pilot study. J Neuroeng Rehabil. 2019;16:56. doi: 10.1186/s12984-019-0531-y Jiang C, Yang S, Tao J, Huang J, Li Y, Ye H, Chen S, Hong W, Chen L. Clinical efficacy of acupuncture treatment in combination with rehacom cognitive training for improving cognitive function in stroke: a 2 × 2 factorial design randomized controlled trial. J Am Med Dir Assoc. 2016;17:1114–1122. doi: 10.1016/j.jamda.2016.07.021 Wu CY, Hung SJ, Lin KC, Chen KH, Chen P, Tsay PK. Responsiveness, minimal clinically important difference, and validity of the MoCA in stroke rehabilitation. Occup Ther Int. 2019;2019:2517658. doi: 10.1155/2019/2517658 Hwi-Young C, Ki-Tae K, Jin-Hwa J. Effects of computer assisted cognitive rehabilitation on brain wave, memory and attention of stroke patients: a randomized control trial. J Phys Ther Sci. 2015;27:1029–1032. doi: 10.1589/jpts.27.1029 Yoo C, Yong MH, Chung J, Yang Y. Effect of computerized cognitive rehabilitation program on cognitive function and activities of living in stroke patients. J Phys Ther Sci. 2015;27:2487–2489. doi: 10.1589/jpts.27.2487 Law LL, Barnett F, Yau MK, Gray MA. Effects of combined cognitive and exercise interventions on cognition in older adults with and without cognitive impairment: a systematic review. Ageing Res Rev. 2014;15:61–75. doi: 10.1016/j.arr.2014.02.008 Liu-Ambrose T, Eng JJ. Exercise training and recreational activities to promote executive functions in chronic stroke: a proof-of-concept study. J Stroke Cerebrovasc Dis. 2015;24:130–137. doi: 10.1016/j. jstrokecerebrovasdis.2014.08.012 Burgener SC, Yang Y, Gilbert R, Marsh-Yant S. The effects of a multimodal intervention on outcomes of persons with early-stage dementia. Am J Alzheimers Dis Other Demen. 2008;23:382–394. doi: 10.1177/ 1533317508317527 Cicerone KD, Langenbahn DM, Braden C, Malec JF, Kalmar K, Fraas M, Felicetti T, Laatsch L, Harley JP, Bergquist T, et al. Evidence-based cognitive rehabilitation: updated review of the literature from 2003 through 2008. Arch Phys Med Rehabil. 2011;92:519–530. doi: 10.1016/j.apmr.2010.11.015 Pandian JD, Arora R, Kaur P, Sharma D, Vishwambaran DK, Arima H. Mirror therapy in unilateral neglect after stroke (MUST trial): a randomized controlled trial. Neurology. 2014;83:1012–1017. doi: 10.1212/WNL. 0000000000000773 Thieme H, Bayn M, Wurg M, Zange C, Pohl M, Behrens J. Mirror therapy for patients with severe arm paresis after stroke–a randomized controlled trial. Clin Rehabil. 2013;27:314–324. doi: 10.1177/0269215512455651 Gandhi DB, Sterba A, Khatter H, Pandian JD. Mirror therapy in stroke rehabilitation: current perspectives. Ther Clin Risk Manag. 2020;16:75–85. doi: 10.2147/TCRM.S206883 Rehabilitation of Cognitive Deficits Poststroke