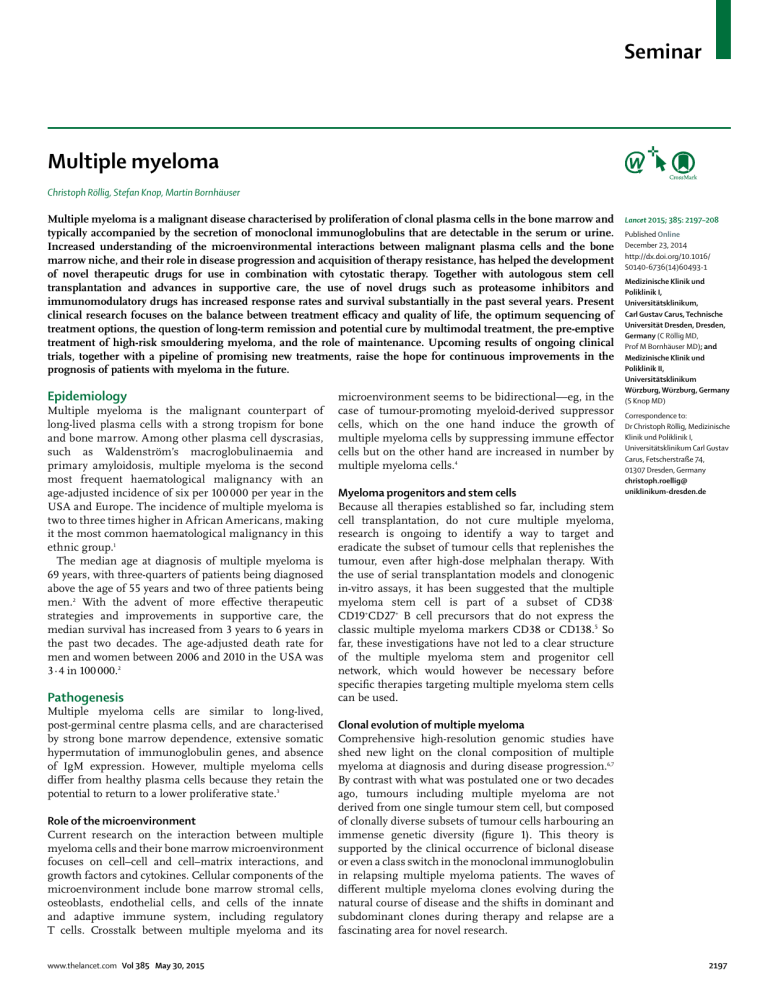
Seminar Multiple myeloma Christoph Röllig, Stefan Knop, Martin Bornhäuser Multiple myeloma is a malignant disease characterised by proliferation of clonal plasma cells in the bone marrow and typically accompanied by the secretion of monoclonal immunoglobulins that are detectable in the serum or urine. Increased understanding of the microenvironmental interactions between malignant plasma cells and the bone marrow niche, and their role in disease progression and acquisition of therapy resistance, has helped the development of novel therapeutic drugs for use in combination with cytostatic therapy. Together with autologous stem cell transplantation and advances in supportive care, the use of novel drugs such as proteasome inhibitors and immunomodulatory drugs has increased response rates and survival substantially in the past several years. Present clinical research focuses on the balance between treatment efficacy and quality of life, the optimum sequencing of treatment options, the question of long-term remission and potential cure by multimodal treatment, the pre-emptive treatment of high-risk smouldering myeloma, and the role of maintenance. Upcoming results of ongoing clinical trials, together with a pipeline of promising new treatments, raise the hope for continuous improvements in the prognosis of patients with myeloma in the future. Epidemiology Multiple myeloma is the malignant counterpart of long-lived plasma cells with a strong tropism for bone and bone marrow. Among other plasma cell dyscrasias, such as Waldenström’s macroglobulinaemia and primary amyloidosis, multiple myeloma is the second most frequent haematological malignancy with an age-adjusted incidence of six per 100 000 per year in the USA and Europe. The incidence of multiple myeloma is two to three times higher in African Americans, making it the most common haematological malignancy in this ethnic group.1 The median age at diagnosis of multiple myeloma is 69 years, with three-quarters of patients being diagnosed above the age of 55 years and two of three patients being men.2 With the advent of more effective therapeutic strategies and improvements in supportive care, the median survival has increased from 3 years to 6 years in the past two decades. The age-adjusted death rate for men and women between 2006 and 2010 in the USA was 3·4 in 100 000.2 Pathogenesis Multiple myeloma cells are similar to long-lived, post-germinal centre plasma cells, and are characterised by strong bone marrow dependence, extensive somatic hypermutation of immunoglobulin genes, and absence of IgM expression. However, multiple myeloma cells differ from healthy plasma cells because they retain the potential to return to a lower proliferative state.3 Role of the microenvironment Current research on the interaction between multiple myeloma cells and their bone marrow microenvironment focuses on cell–cell and cell–matrix interactions, and growth factors and cytokines. Cellular components of the microenvironment include bone marrow stromal cells, osteoblasts, endothelial cells, and cells of the innate and adaptive immune system, including regulatory T cells. Crosstalk between multiple myeloma and its www.thelancet.com Vol 385 May 30, 2015 microenvironment seems to be bidirectional—eg, in the case of tumour-promoting myeloid-derived suppressor cells, which on the one hand induce the growth of multiple myeloma cells by suppressing immune effector cells but on the other hand are increased in number by multiple myeloma cells.4 Myeloma progenitors and stem cells Lancet 2015; 385: 2197–208 Published Online December 23, 2014 http://dx.doi.org/10.1016/ S0140-6736(14)60493-1 Medizinische Klinik und Poliklinik I, Universitätsklinikum, Carl Gustav Carus, Technische Universität Dresden, Dresden, Germany (C RÖllig MD, Prof M Bornhäuser MD); and Medizinische Klinik und Poliklinik II, Universitätsklinikum Würzburg, Würzburg, Germany (S Knop MD) Correspondence to: Dr Christoph Röllig, Medizinische Klinik und Poliklinik I, Universitätsklinikum Carl Gustav Carus, Fetscherstraße 74, 01307 Dresden, Germany christoph.roellig@ uniklinikum-dresden.de Because all therapies established so far, including stem cell transplantation, do not cure multiple myeloma, research is ongoing to identify a way to target and eradicate the subset of tumour cells that replenishes the tumour, even after high-dose melphalan therapy. With the use of serial transplantation models and clonogenic in-vitro assays, it has been suggested that the multiple myeloma stem cell is part of a subset of CD38CD19+CD27+ B cell precursors that do not express the classic multiple myeloma markers CD38 or CD138.5 So far, these investigations have not led to a clear structure of the multiple myeloma stem and progenitor cell network, which would however be necessary before specific therapies targeting multiple myeloma stem cells can be used. Clonal evolution of multiple myeloma Comprehensive high-resolution genomic studies have shed new light on the clonal composition of multiple myeloma at diagnosis and during disease progression.6,7 By contrast with what was postulated one or two decades ago, tumours including multiple myeloma are not derived from one single tumour stem cell, but composed of clonally diverse subsets of tumour cells harbouring an immense genetic diversity (figure 1). This theory is supported by the clinical occurrence of biclonal disease or even a class switch in the monoclonal immunoglobulin in relapsing multiple myeloma patients. The waves of different multiple myeloma clones evolving during the natural course of disease and the shifts in dominant and subdominant clones during therapy and relapse are a fascinating area for novel research. 2197 Seminar Monoclonal gammopathy of unknown significance Myeloma Progenitor clones competing for bone marrow niche Relapse or plasma cell leukaemia Dominant diagnostic clone Mutation x Therapy Tumour initiating cell Mutation x (A) clone with unique mutations = diagnostic clone Mutation x Mutation xy Minor diagnostic subclone Mutation z Mutation xy (B) dominant clone already detectable as minor subclone at diagnosis Mutation z (C) clone with unique mutations = diagnostic clone Figure 1: Clonal composition of multiple myeloma during disease progression and therapy During the progression from monoclonal gammopathy to multiple myeloma, tumour initiating cells can give rise to subclones that are predominantly detected in diagnostic samples and harbour unique mutations, x, which might also be detectable later on in relapsed disease. (A) Especially in high-risk disease, minor subclones that might have been hardly detectable at the time of initial diagnosis might acquire additional driving mutations, xy, during therapy, which later dominate the clonal composition at relapse. (B) Subclones derived from tumour-initiating cells not detectable at the time of initial diagnosis might awake from dormancy at a later point in time and evolve as the dominating clone at relapse with a different founding mutation, z. (C) Whereas clones with unique non-linear mutations x or z are supposed to be more susceptible to salvage therapy, subclones driven by newly acquired mutations (xy) are likely to be resistant to conventional therapies. Test Blood Serum protein electrophoresis and immunofixation Serum immunoglobulins quantitative Serum free light chain assay Total serum protein, serum albumin, creatinine, calcium, electrolytes, lactate dehydrogenase, β2-microglobulin Haemoglobin, white blood cell count, differential count, platelet count Urine Urine protein electrophoresis and immunofixation 24 h urine for total protein, light chains Bone marrow Aspirate and biopsy for plasma cell count, morphology, amyloid* Cytogenetic evaluation and fluorescence in-situ hybridisation for the detection of del 13, del 17p13, t(4;14), t(11;14), t(14;16), 1q+ Bones Skeletal survey (conventional x-ray) or low-dose CT scan without contrast Whole body MRI*, PET-CT* Tissue biopsy for solitary or extraosseous plasmacytoma* *Useful under some circumstances. Table 1: Diagnostic workup for multiple myeloma Symptoms, diagnostic workup, and disease monitoring The most common clinical manifestations of symptomatic multiple myeloma are anaemia, infections, lytic or osteopenic bone disease, or renal failure, but patients with multiple myeloma might be diagnosed at an asymptomatic stage by chance. Generally, multiple myeloma is diagnosed at an earlier stage today than in the past.8 Back pain, particularly in older patients, or unclear anaemia should prompt screening for the presence of multiple myeloma. 2198 The standard screening workup includes total serum protein, serum and urine protein electrophoresis (SPEP and UPEP), immunofixation in serum and urine, detection of immunoglobulin free light chains (FLC) in serum, and the following additional parameters: complete blood count, serum creatinine, and electrolytes including calcium, lactate dehydrogenase, and β2 microglobulin. In a patient with suspected multiple myeloma, a bone marrow sample should be obtained by aspiration or by doing a biopsy. If a monoclonal protein is detected through SPEP, UPEP, or by pathological FLC ratio and the plasma cell count is higher than or equal to 10%, a diagnosis of multiple myeloma is made. The same applies to patients with less than 10% plasma cells but with a monoclonal protein of more than or equal to 3 g/100 mL.9 In patients with non-secretory multiple myeloma, the diagnosis is based on the presence of more than 30% bone marrow plasma cells or the detection of plasmacytoma in a biopsy.10 A singular plasma cell lesion in the bone or at an extraosseous site with less than 10% plasma cell infiltration in the bone marrow and low monoclonal protein is defined as solitary plasmacytoma, a disorder distinctively different from systemic multiple myeloma both in terms of prognosis and treatment. In patients diagnosed with multiple myeloma, development of end-organ damage is the indication for treatment. Multiple myeloma without end-organ damage is referred to as smouldering multiple myeloma. Multiple myeloma patients should have a full radiographic skeletal www.thelancet.com Vol 385 May 30, 2015 Seminar survey done to detect lytic lesions, severe osteopenia, or pathological fractures.9 MRI or PET-CT can be used when symptomatic areas show no abnormality on routine radiographs.11 Table 1 summarises the diagnostic workup for patients with multiple myeloma. Patients with monoclonal gammopathy but with less than 10% bone marrow plasma cells or low M-protein are diagnosed with monoclonal gammopathy of unknown significance, and do not need treatment but do need regular follow-up because of the potential for progression to multiple myeloma; however, the risk of progression is only 1% per life-year.9 Disorders such as nephrotic syndrome and heart failure, neuropathy in non-diabetic patients, left ventricular hypertrophy on echocardiography without consistent electrocardiographic evidence or low limb lead voltages, hepatomegaly with normal imaging, or albuminuria should be assessed carefully to not overlook light-chain amyloidosis caused by free light-chain secretion.12,13 The appendix shows the diagnostic criteria for monoclonal gammopathy of unknown significance, smouldering and active multiple myeloma. To measure treatment response and monitor disease activity, the serum M-protein is the preferred surrogate marker. In patients with light chain secretion, the Bence-Jones proteinuria in a 24 h urine specimen should be used to monitor disease activity, and for patients with oligosecretory multiple myeloma, the FLC assay is useful to monitor disease activity, provided the FLC ratio is abnormal and the involved FLC level is at least 100 mg/L.14 In the rare non-secretory multiple myeloma, only the plasma cell count in the bone marrow and monitoring of clinical manifestations of organ damage can be used for response assessment and to monitor disease.15 Other techniques such as flow cytometry, fluorescent in-situ hybridisation or PCR using allele-specific oligonucleotides can contribute information on minimal residual disease in myeloma, refine the complete remission definition, and distinguish two response groups (minimal residual disease positive and negative) with clear differences in progression-free and overall survival.16 Disease management Indication for treatment Patients with smouldering multiple myeloma have no treatment indication and should be monitored for disease progression because early treatment with conventional therapy has shown no benefit.17–19 The risk of progression is highest in the first 5 years and decreases subsequently. The overall risk of progression is 10% per year for the first 5 years, about 3% per year for the next 5 years, and 1% per year for the next 10 years.17 Patients with high-risk smouldering multiple myeloma should be enrolled onto clinical trials End-organ damage is defined mainly by the CRAB criteria—hypercalcaemia, renal failure, anaemia, or bone lesions, which are related to a plasma cell proliferative disorder and cannot be explained by another unrelated www.thelancet.com Vol 385 May 30, 2015 disease or disorder. The appendix provides additional information about criteria for active multiple myeloma. Moreover, progressive myeloma-induced renal insufficiency should trigger initiation of treatment even before the creatinine threshold of 2 mg/dL (177 μmol/L) has been reached. Acute renal failure due to multiple myeloma can be reversible if treated early. After the confirmation of an underlying cast nephropathy, appropriate treatment should be initiated without delay.20,21 Once patients with renal impairment have achieved a remission, their outcomes are similar to patients with no renal insufficiency.22 Local disease control and systemic treatment Solitary osseous and extraosseous plasmacytomas are treated with curatively intended radiation therapy to the involved field with cumulative doses of 45 Gy or more.23,24 Additionally, if necessary, extraosseous lesions can be resected surgically. Although cure is the primary goal of treatment in solitary plasmacytoma, a progression to systemic multiple myeloma is possible and occurs in 30–60% of cases, therefore requiring regular follow-up.25 Patients diagnosed with systemic active multiple myeloma characterised by end-organ damage should be treated with systemic chemotherapy to prevent progression and reduce disease-induced symptoms. A very good partial remission or complete remission after systemic treatment is associated with an improved long-term outcome. Therefore, the aim of new treatment approaches is to increase response rates in all patients. In elderly patients, this concept should be considered in relation to possible side-effects and quality of life because improved response rates do not necessarily translate into a survival benefit.26–30 Surgery or radiotherapy might be necessary if bone-related complications are present. See Online for appendix Autologous stem cell transplantation Because myeloablative high-dose therapy with autologous stem cell transplantation prolongs survival substantially compared with conventional cytostatic treatments, it has become an essential part of multiple myeloma management.31,32 Because of its toxic effects and the advanced age of many multiple myeloma patients, the thorough assessment of eligibility is crucial.33 The most commonly used criteria for eligibility are the patient’s preference, a biological age up to 65–70 years, the absence of substantial heart, lung, kidney, or liver dysfunction, or other uncontrolled comorbidities such as diabetes. Eligible patients should receive myeloablative treatment with melphalan 200 mg/m² after remission induction by standard first-line treatment. Older patients or patients with substantially impaired organ function might receive reduced doses of melphalan (100–140 mg/m²) before infusion of autologous stem cells.34,35 Investigators in France showed that tandem transplantation was superior to single transplantation in a randomised trial; however, this benefit was restricted to 2199 Seminar Age <65 years and dose level 0 Age 65–75 years and dose level –1 Age >75 years and dose level –2 Bortezomib 1·3 mg/m² on days 1, 4, 8, and 11 every 3 weeks 1·3 mg/m² on days 1, 8, 15, and 22 every 5 weeks 1·0 mg/m² on days 1, 8, 15, and 22 every 5 weeks Cyclophosphamide 300 mg/m² orally on days 1, 8, 15, and 22 every 4 weeks 50–100 mg/m² orally on days 1, 8, 15, and 22 every 4 weeks 50 mg/m² orally every other day on days 1–21 every 4 weeks Dexamethasone 40 mg on days 1–4 and 15–18 or on days 1, 4, 8, 15, and 22 every 4 weeks 20–40 mg on days 1, 4, 8, 15, and 22 every 4 weeks 10–20 mg on days 1, 4, 8, 15, and 22 every 4 weeks Lenalidomide 25 mg on days 1–21 every 4 weeks 15 mg on days 1–21 every 4 weeks 10 mg on days 1–21 every 4 weeks Melphalan 0·25 mg/kg on days 1–4 every 4–6 weeks 0·18 mg/kg on days 1–4 every 4–6 weeks 0·13 mg/kg on days 1–4 every 4–6 weeks Prednisone 50 mg every other day 25 mg every other day 12·5 mg every other day Thalidomide 200 mg/day continuously 100 mg/day continuously 50 mg/day continuously Data from Ludwig and colleagues43 and Palumbo and Anderson.44 Table 2: Dose-adjustment recommendations depending on age and tolerability patients who did not achieve at least a very good partial remission after the first transplantation.36 The pooled results from a systematic review showed no significant difference between tandem and single autologous stem cell transplantations for the outcome of overall survival, but a superior event-free survival and response rate with tandem transplantation.37 Current practice in most centres is to do only one autologous stem cell transplantation initially. A reason for the use of this strategy is that the proportion of patients achieving complete remission after one high-dose chemotherapy has doubled in the era of novel compounds used during induction therapy. Moreover, stem cell transplantation might again be effectively done in relapse, as suggested by data from several non-randomised trials.38 Because the benefit of high-dose treatment has been shown before the use of novel drugs and meta-analyses showed an event-free survival advantage, but no clear overall survival benefit,39 the value of autologous stem cell transplantation has been a matter of debate for years. However, preliminary results from randomised comparisons incorporating novel drugs have shown the importance of high-dose treatment for sustained progression-free survival.40 Although immediate autologous stem cell transplantation in first-line treatment is the standard of care, retrospective analyses suggest that in the era of novel drugs its use could be postponed until the time of first relapse with no prognostic disadvantage for patients.41 Currently, two large randomised trials (NCT01191060, NCT01208766) are comparing immediate versus delayed transplantation at the time of first relapse or disease progression. First-line treatment in patients not eligible for transplantation Most multiple myeloma patients will not be eligible for high-dose therapy because of their older age. In this patient group, emphasis should be placed on tolerability of treatment to minimise excessive morbidity and mortality. Treatment should be given for several cycles because 2200 response quality often increases over time.42 Generally, however, this is only possible for treatments that have a favourable tolerability profile. Quality of life is also a major issue, particularly in a non-curable disease such as multiple myeloma. To prevent excessive treatment toxic effects and improve tolerability, age-adjusted dose reductions, modified application schedules (table 2), and adequate supportive measures are important considerations. Figure 2 shows an overview of treatment approaches used in newly diagnosed multiple myeloma patients. Standard treatment options combine traditional drugs such as melphalan and prednisone with novel treatments such as immunomodulatory drugs and proteasome inhibitors. The addition of the immunomodulatory drug thalidomide to melphalan and prednisone has been shown to increase response rates, progression-free survival, and potentially overall survival in several trials and a meta-analysis.45 Data from a large international trial showed that the combination of the proteasome inhibitor bortezomib and melphalan and prednisone had a statistically significantly higher efficacy than melphalan and prednisone alone and led to improved survival outcomes.46 No data from randomised trials comparing melphalan, prednisone, and thalidomide and melphalan, prednisone, and bortezomib regimens are available. However, findings from a recent meta-analysis suggested higher response rates with the melphalan, prednisone, and bortezomib regimen compared with the melphalan, prednisone, and thalidomide regimen, but there were no significant differences between the treatment regimens in progression-free survival and overall survival.47 Another indirect meta-analysis of this comparison showed no difference between melphalan, prednisone, and bortezomib and melphalan, prednisone, and thalidomide for all outcomes but a statistically significant benefit for complete response and grade 3 or 4 adverse events for melphalan, prednisone, and bortezomib.48 On the basis of the survival benefit, compared with the melphalan and prednisone combination, the combinations of melphalan, prednisone, and thalidomide and melphalan, prednisone, and bortezomib are the www.thelancet.com Vol 385 May 30, 2015 Seminar Patient with newly diagnosed multiple myeloma CRAB criteria? No Watch and wait Yes Symptomatic osseus or extraosseous lesion? Yes Consider radiotherapy or surgical treatment No Systemic treatment Assess comorbidities, age, patient’s preference Transplantation-eligible patient Three-drug regimen Bortezomib, cyclophosphamide, and dexamethasone Bortezomib, doxorubicin, and dexamethasone* Bortezomib, lenalidomide, and dexamethasone* Bortezomib, thalidomide, and dexamethasone* Transplantation-ineligible patient Two-drug regimen Lenalidomide and dexamethasone* Bortezomib and dexamethasone* Three-drug regimen Melphalan, prednisone, and bortezomib* Melphalan, prednisone, and thalidomide* Two-drug regimen Lenalidomide and dexamethasone* Bortezomib and dexamethasone* Melphalan and prednisone*† Bendamustine and prednisone*† Dexamethasone† Single autologous SCT*‡ Consider maintenance Figure 2: Clinical management of patients with newly diagnosed multiple myeloma The listed therapy combinations are selected and not inclusive of all regimens. *Treatment combinations with evidence from randomised-controlled trials. †Melphalan + prednisone, bendamustine + prednisone, or dexamethasone can be used if novel drugs are not available or contraindicated. ‡Consider allogeneic stem-cell transplantation in young patients with deletion 17p and HLA-identical siblings. preferred first-line treatments if available and tolerated. Data from two studies have shown that the combination of lenalidomide and dexamethasone is an effective treatment in elderly multiple myeloma patients.49,50 Preliminary data from a large randomised controlled trial suggest higher response rates and similar progression-free survival after first-line treatment with lenalidomide plus low-dose dexamethasone for a fixed number of cycles compared with melphalan, prednisone, and thalidomide.51 Prophylactic antithrombotic measures should be taken when thalidomide or lenalidomide are given,52,53 whereas prophylactic aciclovir is recommended in patients receiving bortezomib for the prevention of zoster reactivation.54,55 Careful clinical monitoring and dose adaptation is advisable to minimise the toxic effects of treatment, ensure adherence to treatment and, hence, provide the greatest opportunity for achievement of high response rates and long-term remission. To minimise toxicities of multiple myeloma treatments, dose reduction might be necessary in patients receiving thalidomide and lenalidomide, whereas laxatives might be needed for patients receiving thalidomide. Moreover, there are three main preventive strategies for bortezomib-induced polyneuropathy: expansion of the application intervals www.thelancet.com Vol 385 May 30, 2015 from days 1, 4, 8, and 11 to days 1, 8, 15, and 22 per cycle; use of the subcutaneous administration route as opposed to intravenous application; and dose reduction. First-line treatment in patients eligible for transplantation Patients eligible for high-dose treatment of multiple myeloma tend to be younger and fitter than those who are not eligible. Because there seems to be a positive correlation between depth of response and survival,56–62 the goal with primary therapy is to achieve a maximum response before high-dose treatment that translates into even higher remission rates after autologous stem cell transplantation. Accordingly, more effective and intensive treatments are used to improve outcomes. Similarly to non-transplantation-eligible patients, the combination of novel drugs thalidomide,63 bortezomib,64 or lenalidomide49 with standard drugs for multiple myeloma treatment has resulted in higher response rates than the historical standard of vincristine plus doxorubicin (adriamycin) plus dexamethasone.65,66 Therefore, combinations with novel drugs should be used for primary treatment, provided that they are available and not medically contraindicated (figure 2). The triple combination including either one or two novel drugs results in higher 2201 Seminar response rates than the combination of two drugs—eg, bortezomib plus dexamethasone plus either cyclophosphamide67–70 or doxorubicin71,72 or thalidomide27,73 or lenalidomide.69,74 The addition of a fourth drug to primary treatment does not seem to further increase response rates.28,69 On the basis of these findings, experts and guidelines preferentially recommend the use of a triple combination or if contraindications exist, a double combination for three to six cycles for primary treatment in transplant-eligible patients.43,44,65,75,76 There is a need for high-level evidence from randomised-controlled trials comparing different first-line regimens and two-drug versus three-drug combinations, not only regarding progression but also overall survival. Consolidation and maintenance To further reduce the tumour burden after autologous stem cell transplantation, a limited number of treatment cycles can be administered afterwards. This treatment is referred to as consolidation and can improve the depth of response.77,78 However, the emergence of novel agents with a lower toxic effect profile than with more traditional anti-multiple myeloma drugs led to a renaissance in the concept of continuous treatment or maintenance. Historical approaches with steroids79,80 or interferon81,82 showed little efficacy and serious limitations because of long-term side-effects and low tolerability. As thalidomide was the first of the novel drugs, the largest number of patients has received thalidomide continuously. Three meta-analyses of trial results in transplantation-eligible patients showed a benefit in progression-free survival and overall survival when thalidomide maintenance was compared with no maintenance.83–85 These positive results should be considered in relation to substantial long-term toxic effects, leading to a short treatment, mainly as a result of peripheral polyneuropathy. In the large MRC IX trial of thalidomide maintenance, patients with high-risk cytogenetics had a statistically significantly shorter overall survival after thalidomide maintenance than did those without maintenance. This difference was caused by a higher incidence of resistant disease that did not respond to salvage treatment in the thalidomide maintenance group.86 In four clinical trials administering thalidomide after melphalan, prednisone, and thalidomide in elderly patients,87–90 only one trial showed a small statistically significant benefit in overall survival.88 The maintenance of lenalidomide, the second novel drug, has been extensively studied in three large randomised trials. As opposed to thalidomide, longterm application is feasible because of a more favourable toxicity profile with mainly haematological side-effects. The IFM 2005-0278 and CALGB 10010491 trials applied lenalidomide maintenance after high-dose treatment in a randomised placebo-controlled design until disease progression. With a median follow-up of 45 months in the IFM 2005-02 trial, progression-free survival was 2202 significantly prolonged with lenalidomide versus placebo (41 months vs 23 months; p<0·001). After a median follow up of 34 months in the CALGB 100104 trial, patients receiving maintenance with lenalidomide versus placebo had a median time to progression of 46 months versus 27 months (p<0·001). Although the IFM 2005–02 trial showed no significant benefit in overall survival, a difference in 3-year overall survival of 88% versus 80% in favour of lenalidomide has been shown in the CALGB 100104 trial (p=0·03). Another trial explored lenalidomide maintenance in elderly patients who were not eligible for high-dose treatment. Patients were randomly assigned to receive either nine cycles of melphalan and prednisone or melphalan and prednisone plus lenalidomide or melphalan, prednisone, and lenalidomide followed by lenalidomide maintenance. Progression-free survival after melphalan, prednisone, and lenalidomide was 14 months, but after the same combination followed by lenalidomide maintenance, it was 31 months. Overall survival in all three study groups was not significantly different after a median follow-up of 30 months.26 In all three trials, the incidence of second primary malignancies was higher in the treatment groups receiving continous lenalidomide than in patients without lenlidomide maintenance—between 7%26 and 9·5%91 versus about 3%26 to 4%.78,91 The preliminary results of the FIRST trial showed a statistically significant improvement in progression-free survival and overall survival when firstline lenalidomide plus dexamethasone treatment was given continuously until progression compared with a fixed number of cycles.51 Although the third established novel drug bortezomib is given parenterally, its feasibility for continuous treatment has been shown in a large Dutch-German randomised trial, which compared bortezomib maintenance after bortezomib-based induction and thalidomide maintenance after induction with vincristine, doxorubicin, and dexamethasone. Bortezomib was given intravenously every 2 weeks for 2 years. Bortezomib maintenance was better tolerated than thalidomide. The main adverse events during maintenance were infections, polyneuropathy, and gastrointestinal symptoms. After a median follow-up of 41 months, progression-free survival was significantly prolonged in the bortezomib group (35 months vs 28 months, p=0·002). An overall survival advantage after 5 years was 61% versus 55% and became significant only after adjustment for unbalanced risk factors in a multivariate Cox regression model.72 No increased risk of second primary malignancies was observed with bortezomib maintenance.72 Investigators of a second randomised trial explored the value of six cycles of bortezomib consolidation after autologous stem cell transplantation compared with no consolidation. After a median follow-up of 38 months, the median progressionfree survival was 27 months versus 20 months (p=0·05) www.thelancet.com Vol 385 May 30, 2015 Seminar in favour of bortezomib consolidation and the 3-year overall survival was 80% in both groups. Tolerability was acceptable with more severe poly neuropathy after bortezomib consolidation.92 Generally, the concept of maintenance is still a matter of debate. Supporters emphasise the increased duration of progression-free survival, a trend for an overall survival benefit, and the acceptable tolerability with manageable side-effects. Opponents argue in favour of a treatment-free interval as an important factor for patients’ quality of life, and highlight the inconclusive results regarding overall survival, the side-effects, the risk of second primary malignancies and high costs. So far, none of the drugs assessed has been approved for maintenance therapy. Experts recommend that treatment decisions for individual patients must carefully balance potential benefits against risks because a widely agreed on standard is not yet established (appendix).75,85 Allogeneic stem cell transplantation Allogeneic stem cell transplantation has been done for several decades in multiple myeloma patients. Despite improvements in tolerability of conditioning regimens, supportive care, and donor search, the more profound antitumour efficacy of allogeneic stem cell transplantation is partly offset by treatment-related complications that are mainly due to graft-versus-host disease. Although clear evidence for a graft-versus myeloma effect exists, as shown by the efficacy of donor lymphocyte infusions in patients relapsing after allogeneic stem cell transplantation, there is so far no survival plateau in most reports, suggesting that even allogeneic stem cell transplantation might not be a definitive cure in a considerable proportion of patients. Overall, the data tend not to support the routine use of allogeneic stem cell transplantation as an upfront therapy in unselected patients. Nevertheless, there is a small number of patients in the age range of 30–40 years in whom individualised decision making might favour the use of allogeneic stem cell transplantation after myeloablative conditioning therapy, since in these young patients the prospect of a 5–10 year survival with conventional strategies is unsatisfactory. Treatment at relapse or progression Treatment decisions in relapsed or progressive patients should carefully weigh efficacy against risk and reduction of patients’ quality of life. This is true not only for the treatment regimen but also for the time when treatment should be initiated. A clinical relapse characterised by symptoms or CRAB criteria should be treated immediately; however, a biochemical relapse—ie, a solitary increase in protein markers in blood or urine Patient with relapsed or progressive disease Transplantation-eligible patient‡ Previous stem-cell transplantation >12–18 months ago <12–18 months ago Consider re-induction and autologous stem-cell transplantation Transplantation-ineligible patient Previous treatment Without novel drugs With novel drugs <6–9 months ago >6–9 months ago Change regimen Consider repeating previous regimen Novel drug with or without steroid and with or without alkylator or anthracyclin Previous treatment contained lenalidomide or thalidomide† Bortezomib monotherapy* Bortezomib and dexamethasone Bortezomib and liposomal doxorubicin* Pomalidomide and dexamethasone* Bortezomib, cyclophosphamide, and dexamethasone Bortezomib, bendamustine, and dexamethasone Bortezomib, bendamustine, and prednisone Previous treatment contained bortezomib† Lenalidomide monotherapy Lenalidomide and dexamethasone* Pomalidomide and dexamethasone* Thalidomide and dexamethasone Lenalidomide, doxorubicin, and dexamethasone Lenalidomide, cyclophosphamide, and dexamethasone Lenalidomide, bendamustine, and dexamethasone Thalidomide, bendamustine, and dexamethasone Figure 3: Clinical management of patients diagnosed with relapsed or progressive multiple myeloma The listed therapy combinations are selected and not inclusive of all regimens. *Treatment combinations with evidence from randomised-controlled trials. †Patients refractory to lenalidomide or thalidomide and bortezomib are eligible for pomalidomide or carfilzomib or might benefit from cyclophosphamide, melphalan, or bendamustine with or without steroids.‡Consider allogeneic stem-cell transplantation in young patients with deletion 17p and HLA-identical sibling. www.thelancet.com Vol 385 May 30, 2015 2203 Seminar A Diagnosis after 1996 Diagnosis during or before 1996 100 Overall survival (%) 80 60 40 p<0·001 20 0 B 1971–76 1977–82 1983–88 1989–94 1995–2000 2001–06 100 Overall survival (%) 80 60 40 20 0 0 20 40 60 80 Time from diagnosis (months) 100 120 140 Figure 4: Overall survival after diagnosis in patients with multiple myeloma The analysis is based on a cohort of 2981 patients with newly diagnosed multiple myeloma seen between January, 1971, and December, 2006, at the Mayo Clinic, Rochester, MN, USA. (A) The Kaplan-Meier curves for overall survival from diagnosis. The groups were divided based on the date of diagnosis: between Jan 1, 1997, to Dec 31, 2006, versus on or before Dec 31, 1996. (B) The Kaplan-Meier curves for overall survival from the time of diagnosis are grouped into 6-year intervals based on the date of diagnosis (with permission of Blood).108 without CRAB criteria in an asymptomatic patient, should be observed for kinetics first, even in the presence of formal criteria for relapse or progression. As a rule, proliferative relapses should be treated more rapidly than slowly relapsing multiple myeloma. If the doubling time of the monoclonal protein is 2 months or less, treatment is indicated even in the absence of CRAB criteria.43 Various treatment options are available in case of relapse, ranging from conventional cytostatic agents such as melphalan, cyclophosphamide, bendamustine, liposomal doxorubicin, and steroids to novel drugs, including thalidomide, bortezomib, and lenalidomide. Most recommended treatment protocols comprise a combination of these drugs. Figure 3 shows an overview of treatment approaches in relapsed or progressive multiple myeloma. 2204 The new immunomodulatory drug pomalidomide has been approved by the US Food and Drug Administration and by the European Medicines Agency for the treatment of patients who have received at least two previous therapies, including lenalidomide and bortezomib, and have shown disease progression on or within 60 days of completion of the last therapy. The drug is active even in patients who are refractory to both lenalidomide and bortezomib treatment and led to statistically significantly higher response rates, progression-free survival, and overall survival than high-dose dexamethasone in randomised comparisons.93 The most frequently reported side-effects were haematological toxic effects and febrile neutropenia.93 Another approved drug carfi lzomib is a new proteasome inhibitor displaying activity in heavily pretreated patients with less neurotoxicity than bortezomib.94,95 Carfi lzomib is approved by the Food and Drug Administration for the treatment of patients who have received at least two previous therapies, including bortezomib and an immunomodulatory drug, and have shown disease progression on or within 60 days of the completion of the last therapy. The most frequent adverse events in early trials were fatigue, anaemia, nausea, and thrombocytopenia.94,95 The choice of a specific treatment protocol is determined by patient-related factors (eg, age, performance status, comorbidities, and pre-existing toxic effects), disease characteristics such as quality and duration of response, and aggressiveness of the disease.38,43 In patients with a history of recurrent or severe thromboembolic events, thalidomide, lenalidomide, and pomalidomide should be used with caution and with adequate prophylaxis. In patients with clinically significant neuropathy and gastrointestinal morbidity, bortezomib and thalidomide should be avoided or used in dose-reduced schedules. Renal insufficiency might restrict the applicable dose of melphalan, cyclophosphamide, doxorubicin, and lenalidomide. Steroids are part of most relapse protocols and particularly useful as monotherapy in patients with haematological insufficiency in whom most other drugs must be used at a reduced dose or not at all. Retreatment with a specific drug is generally feasible and meaningful if the relapse or progress has occurred after a prolonged treatment-free interval. Whereas this is defined as more than 6 months in the USA,76,96 European recommendations favour a treatment-free interval of more than 12 months after the end of the previous treatment.38,43 Many prospective and retrospective studies showed that reusing bortezomib in later treatment lines is feasible and can result in responses in a substantial proportion of patients. Retreatment with immunomodulatory drugs, mainly lenalidomide, is also feasible and can induce high response rates,38 even in relapse after lenalidomide maintenance.97 A repeated high-dose treatment with melphalan followed by autologous stem cell transplantation seems to be a viable option for patients www.thelancet.com Vol 385 May 30, 2015 Seminar in good physical health with a time of at least 18 months98,99 to 24 months43 from treatment to relapse or progression or if autologous stem cell transplantation was not given as first-line therapy.100,101 Particularly in patients refractory to novel drugs, sophisticated drug combinations and the participation in clinical trials using experimental drugs should be considered. Younger patients (age <50 years) with an HLA-identical sibling donor are candidates for allogeneic stem cell transplantation after dose-reduced conditioning and should be assessed for such an intervention, preferably in the first two years after initial diagnosis.102 Supportive care The most important supportive measure in multiple myeloma is the use of bisphosphonates in patients with skeletal manifestations because they reduce pathological vertebral fractures, skeletal related events, and bone pain.103 According to guidelines, bisphosphonates should be given for at least 2 years after initial diagnosis.104,105 Combination of bisphosphonates with vitamin D3 (cholecalciferol) and calcium might be used. All patients should receive a dental examination before initiation of bisphosphonates, and invasive dental procedures should be done with caution because of the risk of osteonecrosis of the jaw.106 The appendix mentions other important supportive measures. Future perspectives The growing knowledge about pathogenic mechanisms, the development of novel effective compounds that target both multiple myeloma cells and the microenvironment, and more effective supportive strategies have led to a prolonged median overall survival of patients with multiple myeloma over the past two decades.107 As shown in a single treatment centre, 5-year overall survival improved from 37% in patients treated between 1971 and 1996, to 52% between 1997 and 2006 (figure 4), and 66% between 2006 and 2010. These incremental increases in overall survival can be attributed mainly to the introduction of autologous stem cell transplantation, novel drugs and bisphosphonates.108,109 Nevertheless, multiple myeloma should still be regarded as an incurable disease for most patients. There is an ongoing cure-versus-control debate on whether multiple myeloma should be treated with an aggressive multidrug strategy targeting complete response or whether a sequential disease control approach should be pursued that emphasises quality of life and overall survival.75 Although a multimodal aggressive approach seems justified in younger patients with adverse prognosis—eg, the deletion 17p or extramedullary disease, treatment-related complications should be kept in mind, together with the fact that only a few long-term remissions and low (if any) survival plateaus have been shown so far, questioning the possibility of curing the disease. Moreover, it is not clear whether sustained complete remission is caused by less aggressive disease biology rather than therapy-induced www.thelancet.com Vol 385 May 30, 2015 Search strategy and selection criteria Data for this Seminar were identified by searches of PubMed, Embase, Web of Science, and Cochrane Library for reports published between Nov 1, 2008, and March 31, 2013, online accessible abstract collections from 2012 annual meetings of the American Society of Haematology, American Society of Clinical Oncology, and European Society of Haematology. Search terms used were “myeloma”, “pathogenesis”, “diagnosis”, “treatment”, and “therapy”; MeSH terms and filters for randomised trials were used if available. Information from systematic reviews and meta-analyses, randomised-controlled trials and evidence-based guidelines was preferentially used; case reports, case studies and non-English publications were excluded. cure and might, therefore, be a prognostic factor post hoc. Because cure or enduring remission is rare or impossible even after intensive interventions, the treatment goal in elderly, frail, or non-high-risk patients should be disease control, such as achievement of a stable plateau with transfusion independence, stable renal function, and non-progression of bone disease with low toxic effects, high quality of life, and improvement in survival rather than to achieve a complete remission. A major challenge in the near future will be to develop rational algorithms and combination therapies for biologically defined, distinct patient subgroups to prevent overtreatment in low-risk patients or in those who do not tolerate intensive interventions. However, more aggressive strategies might be used in younger and physically fit patients who are likely to derive long-term benefit from tailored intervention. Such stratified approaches are difficult to test for in prospective trials and need a collaborative effort of large study groups and international networks with state-of-the art molecular diagnostics. Advances in our knowledge of when to use a particular drug in the course of disease, together with the prospect of several promising substances in clinical development, will continue to improve the prognosis of multiple myeloma patients in the future. Contributions CR, SK, and MB reviewed published work. CR and MB extracted data. CR, SK, and MB wrote and revised the manuscript. CR and MB contributed to the design of tables and figures. All authors approved the final version of the manuscript. Declaration of interests CR has received speaker’s fees from Amgen, Celgene, Janssen, Novartis, and Amgen. SK has received consultancies, honoraria, and speaker’s fees from Celgene, Mundipharma, Janssen, Onyx, and travel or accommodation payments from Celgene. MB has received speaker’s fees from Celgene, Novartis, MedA, Genzyme, and Gilead, received a travel grant from Astellas, and has served on an advisory board for Riemser. References 1 Landgren O, Gridley G, Turesson I, et al. Risk of monoclonal gammopathy of undetermined significance (MGUS) and subsequent multiple myeloma among African American and white veterans in the United States. Blood 2006; 107: 904–06. 2205 Seminar 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 2206 National Cancer Institute. Surveillance epidemiology and end results program. SEER stat fact sheets on multiple myeloma. 2013. http://seer.cancer.gov/statfacts/html/mulmy.html (accessed April 24, 2013). Kuehl WM, Bergsagel PL. Molecular pathogenesis of multiple myeloma and its premalignant precursor. J Clin Invest 2012; 122: 3456–63. Görgün GT, Whitehill G, Anderson JL, et al. Tumor-promoting immune-suppressive myeloid-derived suppressor cells in the multiple myeloma microenvironment in humans. Blood 2013; 121: 2975–87. Matsui W, Wang Q, Barber JP, et al. Clonogenic multiple myeloma progenitors, stem cell properties, and drug resistance. Cancer Res 2008; 68: 190–97. Chapman MA, Lawrence MS, Keats JJ, et al. Initial genome sequencing and analysis of multiple myeloma. Nature 2011; 471: 467–72. Egan JB, Shi CX, Tembe W, et al. Whole-genome sequencing of multiple myeloma from diagnosis to plasma cell leukemia reveals genomic initiating events, evolution, and clonal tides. Blood 2012; 120: 1060–66. Riccardi A, Gobbi PG, Ucci G, et al. Changing clinical presentation of multiple myeloma. Eur J Cancer 1991; 27: 1401–05. Kyle RA, Rajkumar SV. Criteria for diagnosis, staging, risk stratification and response assessment of multiple myeloma. Leukemia 2009; 23: 3–9. Durie BG, Kyle RA, Belch A, et al, and the Scientific Advisors of the International Myeloma Foundation. Myeloma management guidelines: a consensus report from the Scientific Advisors of the International Myeloma Foundation. Hematol J 2003; 4: 379–98. Dimopoulos M, Terpos E, Comenzo RL, et al, and the IMWG. International myeloma working group consensus statement and guidelines regarding the current role of imaging techniques in the diagnosis and monitoring of multiple Myeloma. Leukemia 2009; 23: 1545–56. Dispenzieri A, Gertz MA, Buadi F. What do I need to know about immunoglobulin light chain (AL) amyloidosis? Blood Rev 2012; 26: 137–54. Merlini G, Wechalekar AD, Palladini G. Systemic light chain amyloidosis: an update for treating physicians. Blood 2013; 121: 5124–30. Dispenzieri A, Kyle R, Merlini G, et al, and the International Myeloma Working Group. International Myeloma Working Group guidelines for serum-free light chain analysis in multiple myeloma and related disorders. Leukemia 2009; 23: 215–24. Durie BG, Harousseau JL, Miguel JS, et al, and the International Myeloma Working Group. International uniform response criteria for multiple myeloma. Leukemia 2006; 20: 1467–73. Puig N, Sarasquete ME, Balanzategui A, et al. Critical evaluation of ASO RQ-PCR for minimal residual disease evaluation in multiple myeloma. A comparative analysis with flow cytometry. Leukemia 2014; 28: 391–97. Kyle RA, Remstein ED, Therneau TM, et al. Clinical course and prognosis of smoldering (asymptomatic) multiple myeloma. N Engl J Med 2007; 356: 2582–90. Kyle RA, Durie BG, Rajkumar SV, et al, and the International Myeloma Working Group. Monoclonal gammopathy of undetermined significance (MGUS) and smoldering (asymptomatic) multiple myeloma: IMWG consensus perspectives risk factors for progression and guidelines for monitoring and management. Leukemia 2010; 24: 1121–27. He Y, Wheatley K, Clark O, et al. Early versus deferred treatment for early stage multiple myeloma. Cochrane Database Syst Rev 2003; 1: CD004023. Leung N, Behrens J. Current approach to diagnosis and management of acute renal failure in myeloma patients. Adv Chronic Kidney Dis 2012; 19: 297–302. Kastritis E, Terpos E, Dimopoulos MA. Current treatments for renal failure due to multiple myeloma. Expert Opin Pharmacother 2013; 14: 1477–95. Chanan-Khan AA, San Miguel JF, Jagannath S, Ludwig H, Dimopoulos MA. Novel therapeutic agents for the management of patients with multiple myeloma and renal impairment. Clin Cancer Res 2012; 18: 2145–63. Dimopoulos MA, Goldstein J, Fuller L, Delasalle K, Alexanian R. Curability of solitary bone plasmacytoma. J Clin Oncol 1992; 10: 587–90. 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 Hu K, Yahalom J. Radiotherapy in the management of plasma cell tumors. Oncology (Williston Park) 2000; 14: 101–8, 111. Reed V, Shah J, Medeiros LJ, et al. Solitary plasmacytomas: outcome and prognostic factors after definitive radiation therapy. Cancer 2011; 117: 4468–74. Palumbo A, Hajek R, Delforge M, et al, and the MM-015 Investigators. Continuous lenalidomide treatment for newly diagnosed multiple myeloma. N Engl J Med 2012; 366: 1759–69. Cavo M, Tacchetti P, Patriarca F, et al, and the GIMEMA Italian Myeloma Network. Bortezomib with thalidomide plus dexamethasone compared with thalidomide plus dexamethasone as induction therapy before, and consolidation therapy after, double autologous stem-cell transplantation in newly diagnosed multiple myeloma: a randomised phase 3 study. Lancet 2010; 376: 2075–85. Rosiñol L, Oriol A, Teruel AI, et al, and the Programa para el Estudio y la Terapéutica de las Hemopatías Malignas/Grupo Español de Mieloma (PETHEMA/GEM) group. Superiority of bortezomib, thalidomide, and dexamethasone (VTD) as induction pretransplantation therapy in multiple myeloma: a randomized phase 3 PETHEMA/GEM study. Blood 2012; 120: 1589–96. Morgan GJ, Davies FE, Gregory WM, et al, and the National Cancer Research Institute Haematological Oncology Clinical Studies Group. Cyclophosphamide, thalidomide, and dexamethasone as induction therapy for newly diagnosed multiple myeloma patients destined for autologous stem-cell transplantation: MRC Myeloma IX randomized trial results. Haematologica 2012; 97: 442–50. Ludwig H, Hajek R, Tóthová E, et al. Thalidomide-dexamethasone compared with melphalan-prednisolone in elderly patients with multiple myeloma. Blood 2009; 113: 3435–42. Attal M, Harousseau JL, Stoppa AM, et al. A prospective, randomized trial of autologous bone marrow transplantation and chemotherapy in multiple myeloma. Intergroupe Français du Myélome. N Engl J Med 1996; 335: 91–97. Giralt S, Stadtmauer EA, Harousseau JL, et al, and the IMWG. International myeloma working group (IMWG) consensus statement and guidelines regarding the current status of stem cell collection and high-dose therapy for multiple myeloma and the role of plerixafor (AMD 3100). Leukemia 2009; 23: 1904–12. Koreth J, Cutler CS, Djulbegovic B, et al. High-dose therapy with single autologous transplantation versus chemotherapy for newly diagnosed multiple myeloma: A systematic review and meta-analysis of randomized controlled trials. Biol Blood Marrow Transplant 2007; 13: 183–96. Palumbo A, Bringhen S, Bruno B, et al. Melphalan 200 mg/m(2) versus melphalan 100 mg/m(2) in newly diagnosed myeloma patients: a prospective, multicenter phase 3 study. Blood 2010; 115: 1873–79. Palumbo A, Sezer O, Kyle R, et al, and the IMWG. International Myeloma Working Group guidelines for the management of multiple myeloma patients ineligible for standard high-dose chemotherapy with autologous stem cell transplantation. Leukemia 2009; 23: 1716–30. Attal M, Harousseau JL, Facon T, et al, and the InterGroupe Francophone du Myélome. Single versus double autologous stem-cell transplantation for multiple myeloma. N Engl J Med 2003; 349: 2495–502. Kumar A, Kharfan-Dabaja MA, Glasmacher A, Djulbegovic B. Tandem versus single autologous hematopoietic cell transplantation for the treatment of multiple myeloma: a systematic review and meta-analysis. J Natl Cancer Inst 2009; 101: 100–06. Mohty B, El-Cheikh J, Yakoub-Agha I, Avet-Loiseau H, Moreau P, Mohty M. Treatment strategies in relapsed and refractory multiple myeloma: a focus on drug sequencing and ‘retreatment’ approaches in the era of novel agents. Leukemia 2012; 26: 73–85. Kumar A, Galeb S, Djulbegovic B. Treatment of patients with multiple myeloma: an overview of systematic reviews. Acta Haematol 2011; 125: 8–22. Boccadoro M, Cavallo F, Gay F, et al. Melphalan/prednisone/ lenalidomide (MPR) versus high-dose melphalan and autologous transplantation (MEL200) plus lenalidomide maintenance or no maintenance in newly diagnosed multiple myeloma (MM) patients. J Clin Oncol 2013; 31 (suppl): 8509 (abstr). Kumar SK, Lacy MQ, Dispenzieri A, et al. Early versus delayed autologous transplantation after immunomodulatory agents-based induction therapy in patients with newly diagnosed multiple myeloma. Cancer 2012; 118: 1585–92. www.thelancet.com Vol 385 May 30, 2015 Seminar 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61 Harousseau JL, Palumbo A, Richardson PG, et al. Superior outcomes associated with complete response in newly diagnosed multiple myeloma patients treated with nonintensive therapy: analysis of the phase 3 VISTA study of bortezomib plus melphalanprednisone versus melphalan-prednisone. Blood 2010; 116: 3743–50. Ludwig H, Avet-Loiseau H, Bladé J, et al. European perspective on multiple myeloma treatment strategies: update following recent congresses. Oncologist 2012; 17: 592–606. Palumbo A, Anderson K. Multiple myeloma. N Engl J Med 2011; 364: 1046–60. Kapoor P, Rajkumar SV, Dispenzieri A, et al. Melphalan and prednisone versus melphalan, prednisone and thalidomide for elderly and/or transplant ineligible patients with multiple myeloma: a meta-analysis. Leukemia 2011; 25: 689–96. San Miguel JF, Schlag R, Khuageva NK, et al. Persistent overall survival benefit and no increased risk of second malignancies with bortezomib-melphalan-prednisone versus melphalan-prednisone in patients with previously untreated multiple myeloma. J Clin Oncol 2013; 31: 448–55. Yeh Y, Chambers J, Gaugris S, et al. Indirect Comparison of the Efficacy of Melphalan-Prednisone-Bortezomib Relative to Melphalan-Prednisone-Thalidomide and Melphalan-Prednisone for the First Line Treatment of Multiple Myeloma. ASH Annual Meeting Abstracts 2008; 112: 2367. Kumar A, Hozo I, Wheatley K, Djulbegovic B. Thalidomide versus bortezomib based regimens as first-line therapy for patients with multiple myeloma: a systematic review. Am J Hematol 2011; 86: 18–24. Zonder JA, Crowley J, Hussein MA, et al. Lenalidomide and high-dose dexamethasone compared with dexamethasone as initial therapy for multiple myeloma: a randomized Southwest Oncology Group trial (S0232). Blood 2010; 116: 5838–41. Rajkumar SV, Jacobus S, Callander NS, et al, and the Eastern Cooperative Oncology Group. Lenalidomide plus high-dose dexamethasone versus lenalidomide plus low-dose dexamethasone as initial therapy for newly diagnosed multiple myeloma: an open-label randomised controlled trial. Lancet Oncol 2010; 11: 29–37. Facon T, Dimopoulos M, Dispenzieri A, et al. Initial phase 3 results of the first (frontline investigation of lenalidomide + dexamethasone versus standard thalidomide) trial (MM-020/IFM 07 01) in newly diagnosed multiple myeloma (NDMM) patients (Pts) ineligible for stem cell transplantation (SCT). ASH Annu Meet Abstr 2013; 122: 2. Palumbo A, Rajkumar SV, Dimopoulos MA, et al, and the International Myeloma Working Group. Prevention of thalidomide- and lenalidomide-associated thrombosis in myeloma. Leukemia 2008; 22: 414–23. Larocca A, Cavallo F, Bringhen S, et al. Aspirin or enoxaparin thromboprophylaxis for patients with newly diagnosed multiple myeloma treated with lenalidomide. Blood 2012; 119: 933–39. Chanan-Khan A, Sonneveld P, Schuster MW, et al. Analysis of herpes zoster events among bortezomib-treated patients in the phase III APEX study. J Clin Oncol 2008; 26: 4784–90. Vickrey E, Allen S, Mehta J, Singhal S. Acyclovir to prevent reactivation of varicella zoster virus (herpes zoster) in multiple myeloma patients receiving bortezomib therapy. Cancer 2009; 115: 229–32. Chanan-Khan AA, Giralt S. Importance of achieving a complete response in multiple myeloma, and the impact of novel agents. J Clin Oncol 2010; 28: 2612–24. Harousseau JL, Attal M, Avet-Loiseau H. The role of complete response in multiple myeloma. Blood 2009; 114: 3139–46. Lahuerta JJ, Mateos MV, Martínez-López J, et al. Influence of pre- and post-transplantation responses on outcome of patients with multiple myeloma: sequential improvement of response and achievement of complete response are associated with longer survival. J Clin Oncol 2008; 26: 5775–82. van de Velde HJ, Liu X, Chen G, Cakana A, Deraedt W, Bayssas M. Complete response correlates with long-term survival and progression-free survival in high-dose therapy in multiple myeloma. Haematologica 2007; 92: 1399–406. Wang M, Delasalle K, Feng L, et al. CR represents an early index of potential long survival in multiple myeloma. Bone Marrow Transplant 2010; 45: 498–504. Moreau P, Attal M, Pégourié B, et al, and the IFM 2005-01 study investigators. Achievement of VGPR to induction therapy is an important prognostic factor for longer PFS in the IFM 2005-01 trial. Blood 2011; 117: 3041–44. www.thelancet.com Vol 385 May 30, 2015 62 63 64 65 66 67 68 69 70 71 72 73 74 75 76 77 78 79 Lokhorst HM, van der Holt B, Zweegman S, et al, and the Dutch-Belgian Hemato-Oncology Group (HOVON). A randomized phase 3 study on the effect of thalidomide combined with adriamycin, dexamethasone, and high-dose melphalan, followed by thalidomide maintenance in patients with multiple myeloma. Blood 2010; 115: 1113–20. Rajkumar SV, Blood E, Vesole D, Fonseca R, Greipp PR, and the Eastern Cooperative Oncology Group. Phase III clinical trial of thalidomide plus dexamethasone compared with dexamethasone alone in newly diagnosed multiple myeloma: a clinical trial coordinated by the Eastern Cooperative Oncology Group. J Clin Oncol 2006; 24: 431–36. Harousseau JL, Attal M, Avet-Loiseau H, et al. Bortezomib plus dexamethasone is superior to vincristine plus doxorubicin plus dexamethasone as induction treatment prior to autologous stem-cell transplantation in newly diagnosed multiple myeloma: results of the IFM 2005-01 phase III trial. J Clin Oncol 2010; 28: 4621–29. Stewart AK, Richardson PG, San-Miguel JF. How I treat multiple myeloma in younger patients. Blood 2009; 114: 5436–43. Palumbo A, Attal M, Roussel M. Shifts in the therapeutic paradigm for patients newly diagnosed with multiple myeloma: maintenance therapy and overall survival. Clin Cancer Res 2011; 17: 1253–63. Reeder CB, Reece DE, Kukreti V, et al. Cyclophosphamide, bortezomib and dexamethasone induction for newly diagnosed multiple myeloma: high response rates in a phase II clinical trial. Leukemia 2009; 23: 1337–41. Kropff M, Liebisch P, Knop S, et al, and the Deutsche Studiengruppe Multiples Myelom, DSMM. DSMM XI study: dose definition for intravenous cyclophosphamide in combination with bortezomib/dexamethasone for remission induction in patients with newly diagnosed myeloma. Ann Hematol 2009; 88: 1125–30. Kumar S, Flinn I, Richardson PG, et al. Randomized, multicenter, phase 2 study (EVOLUTION) of combinations of bortezomib, dexamethasone, cyclophosphamide, and lenalidomide in previously untreated multiple myeloma. Blood 2012; 119: 4375–82. Reeder CB, Reece DE, Kukreti V, et al. Once- versus twice-weekly bortezomib induction therapy with CyBorD in newly diagnosed multiple myeloma. Blood 2010; 115: 3416–17. Popat R, Oakervee HE, Hallam S, et al. Bortezomib, doxorubicin and dexamethasone (PAD) front-line treatment of multiple myeloma: updated results after long-term follow-up. Br J Haematol 2008; 141: 512–16. Sonneveld P, Schmidt-Wolf IG, van der Holt B, et al. Bortezomib induction and maintenance treatment in patients with newly diagnosed multiple myeloma: results of the randomized phase III HOVON-65/GMMG-HD4 trial. J Clin Oncol 2012; 30: 2946–55. Garderet L, Iacobelli S, Moreau P, et al. Superiority of the triple combination of bortezomib-thalidomide-dexamethasone over the dual combination of thalidomide-dexamethasone in patients with multiple myeloma progressing or relapsing after autologous transplantation: the MMVAR/IFM 2005-04 randomized phase III trial from the Chronic Leukemia Working Party of the European Group for Blood and Marrow Transplantation. J Clin Oncol 2012; 30: 2475–82. Richardson PG, Weller E, Lonial S, et al. Lenalidomide, bortezomib, and dexamethasone combination therapy in patients with newly diagnosed multiple myeloma. Blood 2010; 116: 679–86. Rajkumar SV. Multiple myeloma: 2012 update on diagnosis, risk-stratification, and management. Am J Hematol 2012; 87: 78–88. National Comprehensive Cancer Network. NCCN guidelines and derivative information products: user guide. 2013. http://www.nccn. org/professionals (accessed April 4, 2013). Ladetto M, Pagliano G, Ferrero S, et al. Major tumor shrinking and persistent molecular remissions after consolidation with bortezomib, thalidomide, and dexamethasone in patients with autografted myeloma. J Clin Oncol 2010; 28: 2077–84. Attal M, Lauwers-Cances V, Marit G, et al, and the IFM Investigators. Lenalidomide maintenance after stem-cell transplantation for multiple myeloma. N Engl J Med 2012; 366: 1782–91. Berenson JR, Crowley JJ, Grogan TM, et al. Maintenance therapy with alternate-day prednisone improves survival in multiple myeloma patients. Blood 2002; 99: 3163–68. 2207 Seminar 80 81 82 83 84 85 86 87 88 89 90 91 92 93 2208 Shustik C, Belch A, Robinson S, et al. A randomised comparison of melphalan with prednisone or dexamethasone as induction therapy and dexamethasone or observation as maintenance therapy in multiple myeloma: NCIC CTG MY.7. Br J Haematol 2007; 136: 203–11. Fritz E, Ludwig H. Interferon-alpha treatment in multiple myeloma: meta-analysis of 30 randomised trials among 3948 patients. Ann Oncol 2000; 11: 1427–36. Myeloma Trialists’ Collaborative Group. Interferon as therapy for multiple myeloma: an individual patient data overview of 24 randomized trials and 4012 patients. Br J Haematol 2001; 113: 1020–34. Nooka AK, Behera M, Boise LH, et al. Thalidomide As Maintenance Therapy in Multiple Myeloma (MM) Improves Progression Free Survival (PFS) and Overall Survival (OS): a meta-analysis. ASH Annu Meet Abstr 2011; 118: 1855. Hahn-Ast C, Lilienfeld-Toal M, Heteren P. Improved progression-free and overall survival with thalidomide maintenance therapy after autologous stem cell transplantation in multiple myeloma: a meta-analysis of five randomized trials. Haematologica 2011; 96 (suppl 2): 884. Ludwig H, Durie BG, McCarthy P, et al, and the International Myeloma Working Group. IMWG consensus on maintenance therapy in multiple myeloma. Blood 2012; 119: 3003–15. Morgan GJ, Gregory WM, Davies FE, et al, and the National Cancer Research Institute Haematological Oncology Clinical Studies Group. The role of maintenance thalidomide therapy in multiple myeloma: MRC Myeloma IX results and meta-analysis. Blood 2012; 119: 7–15. Palumbo A, Bringhen S, Caravita T, et al, and the Italian Multiple Myeloma Network, GIMEMA. Oral melphalan and prednisone chemotherapy plus thalidomide compared with melphalan and prednisone alone in elderly patients with multiple myeloma: randomised controlled trial. Lancet 2006; 367: 825–31. Wijermans P, Schaafsma M, Termorshuizen F, et al, and the Dutch-Belgium Cooperative Group HOVON. Phase III study of the value of thalidomide added to melphalan plus prednisone in elderly patients with newly diagnosed multiple myeloma: the HOVON 49 Study. J Clin Oncol 2010; 28: 3160–66. Waage A, Gimsing P, Fayers P, et al, and the Nordic Myeloma Study Group. Melphalan and prednisone plus thalidomide or placebo in elderly patients with multiple myeloma. Blood 2010; 116: 1405–12. Beksac M, Haznedar R, Firatli-Tuglular T, et al. Addition of thalidomide to oral melphalan/prednisone in patients with multiple myeloma not eligible for transplantation: results of a randomized trial from the Turkish Myeloma Study Group. Eur J Haematol 2011; 86: 16–22. McCarthy PL, Owzar K, Hofmeister CC, et al. Lenalidomide after stem-cell transplantation for multiple myeloma. N Engl J Med 2012; 366: 1770–81. Mellqvist UH, Gimsing P, Hjertner O, et al, and the Nordic Myeloma Study Group. Bortezomib consolidation after autologous stem cell transplantation in multiple myeloma: a Nordic Myeloma Study Group randomized phase 3 trial. Blood 2013; 121: 4647–54. San Miguel J, Weisel K, Moreau P, et al. Pomalidomide plus low-dose dexamethasone versus high-dose dexamethasone alone for patients with relapsed and refractory multiple myeloma (MM-003): a randomised, open-label, phase 3 trial. Lancet Oncol 2013; 14: 1055–66. 94 95 96 97 98 99 100 101 102 103 104 105 106 107 108 109 Siegel DS, Martin T, Wang M, et al. A phase 2 study of single-agent carfilzomib (PX-171-003-A1) in patients with relapsed and refractory multiple myeloma. Blood 2012; 120: 2817–25. Vij R, Siegel DS, Jagannath S, et al. An open-label, single-arm, phase 2 study of single-agent carfilzomib in patients with relapsed and/or refractory multiple myeloma who have been previously treated with bortezomib. Br J Haematol 2012; 158: 739–48. Rajkumar SV. Multiple myeloma: 2011 update on diagnosis, risk-stratification, and management. Am J Hematol 2011; 86: 57–65. Dimopoulos MA, Petrucci MT, Foa R, et al. Analysis of second-Line lenalidomide following initial relapse in the MM-015 trial. ASH Annu Meet Abstr 2012; 120: 944. Alvares CL, Davies FE, Horton C, Patel G, Powles R, Morgan GJ. The role of second autografts in the management of myeloma at first relapse. Haematologica 2006; 91: 141–42. Neben K, Sellner L, Heiss C, et al. Autologous Re-transplantation for patients with relapsed multiple myeloma: a single center experience with 200 patients. ASH Annu Meet Abstr 2012; 120: 3086. Fermand JP, Ravaud P, Chevret S, et al. High-dose therapy and autologous peripheral blood stem cell transplantation in multiple myeloma: up-front or rescue treatment? Results of a multicenter sequential randomized clinical trial. Blood 1998; 92: 3131–36. Vesole DH, Crowley JJ, Catchatourian R, et al. High-dose melphalan with autotransplantation for refractory multiple myeloma: results of a Southwest Oncology Group phase II trial. J Clin Oncol 1999; 17: 2173–79. Kumar S, Zhang MJ, Li P, et al. Trends in allogeneic stem cell transplantation for multiple myeloma: a CIBMTR analysis. Blood 2011; 118: 1979–88. Mhaskar R, Redzepovic J, Wheatley K, et al. Bisphosphonates in multiple myeloma: a network meta-analysis. Cochrane Database Syst Rev 2012; 5: CD003188. Terpos E, Morgan G, Dimopoulos MA, et al. International myeloma working group recommendations for the treatment of multiple myeloma-related bone disease. J Clin Oncol 2013; 31: 2347–57. Lacy MQ, Dispenzieri A, Gertz MA, et al. Mayo clinic consensus statement for the use of bisphosphonates in multiple myeloma. Mayo Clin Proc 2006; 81: 1047–53. Dickinson M, Prince HM, Kirsa S, et al. Osteonecrosis of the jaw complicating bisphosphonate treatment for bone disease in multiple myeloma: an overview with recommendations for prevention and treatment. Intern Med J 2009; 39: 304–16. Kristinsson SY, Landgren O, Dickman PW, Derolf AR, Björkholm M. Patterns of survival in multiple myeloma: a population-based study of patients diagnosed in Sweden from 1973 to 2003. J Clin Oncol 2007; 25: 1993–99. Kumar SK, Rajkumar SV, Dispenzieri A, et al. Improved survival in multiple myeloma and the impact of novel therapies. Blood 2008; 111: 2516–20. Kumar SK, Dispenzieri A, Gertz MA, et al. Continued Improvement in Survival in Multiple Myeloma and the Impact of Novel Agents. ASH Annu Meet Abstr 2012; 120: 3972. www.thelancet.com Vol 385 May 30, 2015