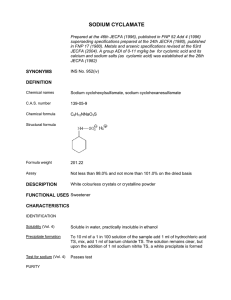
C H A P T ER 10 Ascites Guadalupe Garcia-Tsao Yale University School of Medicine, New Haven, and VA-CT Healthcare System, West Haven, CT, USA Learning points • Ascites is the most common decompensating event in cirrhosis. • Its pathophysiology is mostly explained by splanchnic and peripheral vasodilatation that lead to a decrease in effective blood volume. • The natural history of ascites results from a progressively more deranged circulatory status; with ascites that initially responds to diuretics, then becoming refractory to diuretics, at which time the patient may develop hyponatraemia and, finally, hepatorenal syndrome. • Most patients respond to diuretics. Patients who no longer respond should be treated with repeated largevolume paracenteses. Transjugular intrahepatic portosystemic shunt (TIPS) should be considered in those requiring frequent paracenteses. Fluid restriction is recommended in patients with hyponatraemia. Vasoconstrictors may reverse hepatorenal syndrome and are useful as a bridge to liver transplantation. • Ascites per se is not lethal unless it becomes infected (spontaneous bacterial peritonitis). Infection often precipitates the hepatorenal syndrome leading to death. Antibiotic prophylaxis is indicated for secondary prevention of spontaneous bacterial peritonitis and in highrisk patients. Ascites is free fluid within the peritoneal cavity. It forms because of conditions directly involving the peritoneum (infection, malignancy), or diseases remote from the peritoneum (liver disease, heart failure, hypoproteinaemia). Cirrhosis is the commonest cause of ascites in the Western world (∼75%), followed by peritoneal malignancy (12%), cardiac failure (5%) and peritoneal tuberculosis (2%) [1] (Fig. 10.1). In patients with cirrhosis, the development of ascites marks the transition from compensated to decompensated cirrhosis [2,3]; and is the most frequent first decompensating event, occurring in 48% [4]. The mechanisms of ascites formation in cirrhosis are complex but portal (sinusoidal) hypertension and renal retention of sodium are universal. The natural history of cirrhotic ascites progresses from diuretic-responsive (uncomplicated) ascites to the development of dilutional hyponatraemia, refractory ascites, and finally, hepatorenal syndrome (HRS) (Fig. 10.2). While 1-year survival in patients who develop ascites is 85%, it decreases to 25% once it has progressed to hyponatraemia, refractory ascites or HRS [4]. Treatment of ascites has not resulted in a significant improvement in survival. However, treating ascites is important, not only because it improves quality of life but because spontaneous bacterial peritonitis (SBP), a lethal complication of cirrhosis, does not occur in the absence of ascites. New treatments are being evaluated that modify its pathophysiology, such as the transjugular intrahepatic portosystemic shunt (TIPS) for refractory ascites and vasoconstrictors for HRS. Liver transplantation is the ultimate therapy and should be considered when the patient first presents with ascites. Mechanisms of ascites formation In cirrhosis, the source of ascites is mainly the hepatic sinusoids. Therefore sinusoidal hypertension is the initial mechanism that determines leakage of ascites into the peritoneal space [5,6]. Sinusoidal hypertension results from hepatic venous outflow block secondary to regenerative nodules and fibrosis. The other essential factor in the pathogenesis of cirrhotic ascites is sodium and water retention which allows for the replenishment of the intravascular volume and maintenance of ascites formation [7]. Inappropriate sodium retention is either secondary to vascular changes (underfill and peripheral Sherlock’s Diseases of the Liver and Biliary System, Twelfth Edition. Edited by James S. Dooley, Anna S.F. Lok, Andrew K. Burroughs, E. Jenny Heathcote. © 2011 by Blackwell Publishing Ltd. Published 2011 by Blackwell Publishing Ltd. 210 Ascites 211 Peripheral vasodilatation Diminished effective arterial blood volume Peritoneal malignancy Heart failure Peritoneal tuberculosis Rise in renin, aldosterone, vasopressin Sympathetic system stimulated Sodium and water retention Renal vasoconstriction Plasma volume expansion plus portal hypertension Other Cirrhosis Ascites Fig. 10.1. Causes of ascites. Fig. 10.3. The peripheral arterial vasodilatation hypothesis for ascites formation in cirrhosis [7]. No ascites for their presence [8]; the development of ascites also requires a minimal portal pressure gradient of 12 mmHg [5,6]. A threshold portal pressure gradient of 10 mmHg or more has been defined as ‘clinically significant portal hypertension’ because it best predicts the development of complications of cirrhosis, such as ascites [9,10]. Uncomplicated ascites Ascites + hyponatraemia Sodium retention In patients with cirrhosis and ascites, the normal regulation of sodium balance is lost. Sodium is retained avidly; urinary sodium excretion is often below 5 mmol/day. Inappropriate sodium retention occurs even in the absence of ascites [11]. Refractory ascites Hepatorenal syndrome Vasodilatation theory (Fig. 10.3) Fig. 10.2. Natural history of cirrhotic ascites. Table 10.1. Sequence of events for the hypotheses of ascites formation Primary event Secondary event Underfill/ peripheral arterial vasodilatation theory Overfill theory Vascular Renal Renal Vascular arterial vasodilatation hypotheses) or as a primary event (overfill theory) (Table 10.1). Sinusoidal hypertension Similar to gastro-oesophageal varices, in which a minimal portal pressure gradient of 12 mmHg is needed Arterial vasodilatation, a haemodynamic abnormality typical of the patient with cirrhosis, is the most likely mechanism that explains sodium retention [7]. An increased production of the vasodilator nitric oxide (NO) is considered the main cause of vasodilatation [12]. In experimental models of cirrhosis, inhibition of NO synthase increases systemic blood pressure and renal sodium excretion, resulting in a reduced volume of ascites [13,14]. Other vasodilators implicated in the vasodilatation of cirrhosis include adrenomedullin, carbon monoxide, endocannabinoids, prostacyclin, tumour necrosis factor alpha and urotensin [15]. Arterial vasodilatation results in a reduction in ‘effective’ arterial blood volume and a decrease in systemic arterial pressure, leading to the activation of the renin–angiotensin–aldosterone system (RAAS) and the sympathetic nervous system (through carotid sinus baroreceptors). Renin is produced by the kidney Chapter 10 (juxtaglomerular apparatus) in response to low blood volume and β-adrenergic stimulation. Under the influence of renin, angiotensinogen (produced by the liver) is converted to angiotensin I (a decapeptide), which in turn is converted to angiotensin II (an octapeptide) by angiotensin-converting enzyme (ACE). Angiotensin II is the main stimulant to the synthesis and secretion of aldosterone, a mineralocorticoid, from the glomerular cells of the adrenal cortex. Aldosterone acts on cells in the collecting duct(ule) and, through a cytoplasmic interaction, increases both luminal uptake and basolateral passage of sodium (Fig. 10.3). Natriuresis after spironolactone, an aldosterone antagonist, supports hyperaldosteronism as a major contributor to sodium retention in cirrhosis [16]. In addition to sodium (and water) retention, angiotensin II is a potent vasoconstrictor (both venules and arterioles), a potent stimulant for the non-osmotic release of antidiuretic hormone (ADH) from the posterior pituitary and a potent activator of the adrenergic system (Fig. 10.4). Bacterial translocation to mesenteric lymph nodes with increased endotoxin production and consequent stimulation of cytokine synthesis plays a major role in enhancing vasodilatation in animals with cirrhosis and ascites [17,18]. Further vasodilatation, with further activation of the RAAS, leads to hyponatraemia (through secretion of ADH) [19], and to the HRS (through maximal renal vasoconstriction) [7]. The time course of circulatory, neurohumoral and renal function abnormalities is depicted in Fig. 10.5 [20]. ascites, suggests that in some cases sodium retention occurs unrelated to vasodilatation. An alternative proposal is that, early on in the process, there is a primary renal change—responding to hepatic insufficiency or sinusoidal hypertension—that leads to sodium retention (overfill theory). Several signals have been suggested: reduced hepatic synthesis of a natriuretic agent, reduced hepatic clearance of a sodium-retaining hormone, or a ‘hepatorenal reflex’ of unknown aetiology. This theory is based on findings of sodium Compensated cirrhosis Ascites Degree of splanchnic arterial vasodilatation 212 Time Hyperdynamic circulation Sodium retention Activation SNS and RAAS ADH and hyponatremia Type-2 HRS Type-1 HRS Overfill theory (Fig. 10.6) The presence of normal or low levels of plasma renin activity in about a third of patients with cirrhosis and Decreased cortical perfusion RENIN ANGIOTENSIN II Fig. 10.5. Time course of circulatory, neurohormonal and renal function abnormalities in cirrhosis (in sequence of peripheral arterial vasodilation theory). ADH, antidiuretic hormone; HRS, hepatorenal syndrome; RAAS, renin– angiotensin–aldosterone system; SNS, sympathetic nervous system. (From [20] with permission.) ALDOSTERONE Hepatic signal (baroreceptor, other) Na+ Na+ K+ Na+ K+ * H2O Renal Na+ and H2O retention Plasma volume Cardiac output Systemic vascular resistance Portal hypertension Fig. 10.4. Mechanisms of increased sodium and water reabsorption in cirrhosis. * Increased ADH-stimulated water reabsorption in collecting ducts. Overflow into peritoneal cavity Fig. 10.6. Overfill hypothesis. Ascites 213 handling abnormalities, in the absence of systemic vasodilatation or arterial under-filling, when patients with preascitic cirrhosis are challenged with a sodium load [21]. This hypothesis proposes that primary sodium and water retention lead to expansion of the plasma volume, an increase in cardiac output and a fall in systemic vascular resistance (vasodilatation). Whether vasodilatation is a primary or secondary event, therapy that counteracts the mechanisms that lead to vasodilatation (e.g. NO inhibition) or vasodilation itself (e.g. vasoconstrictors), improves renal haemodynamics and increases sodium excretion [13,22]. Other renal factors Atrial natriuretic peptides (ANP) The plasma concentration of ANP is markedly increased in patients with cirrhosis and ascites, regardless of plasma levels of renin, aldosterone and noradrenaline (norepinephrine). This is a potent natriuretic peptide released from the cardiac atria, probably in response to intravascular volume expansion. In compensated cirrhosis, ANF may maintain sodium homeostasis despite the presence of mild antinatriuretic factors. In later stages, renal resistance to ANF develops, rendering it ineffective [23]. Therefore, sodium retention in cirrhosis cannot be explained on the basis of a deficient synthesis of natriuretic peptides. Prostaglandins Several prostaglandins are synthesized in the kidney and have both vascular and tubular actions. Although they are not primary regulators, they modulate the effects of other factors and hormones locally. Prostaglandin (PG) I2 and E2 are vasodilators, and also increase sodium excretion through vasodilatation and a direct effect on the loop of Henle. They inhibit cyclic adenosine monophosphate (cAMP) synthesis, thereby interfering with the action of vasopressin (ADH). PGI2 is synthesized in the tubules and increases sodium and water excretion. Therefore, prostaglandins have a significant role in sodium and water homeostasis. In conditions where there is a reduced circulating volume, which includes cirrhosis, there is increased prostaglandin synthesis. This counterbalances renal vasoconstriction by antagonizing the local effects of renin, angiotensin II, endothelin 1, vasopressin and catecholamines. The importance of this role is demonstrated clinically by the renal dysfunction precipitated by the administration non-steroidal anti-inflammatory agents to decompensated [24] and compensated [25] patients with cirrhosis. Without the vasodilatory influence of prostaglandins, renal blood flow and glomerular filtration rate fall because of unopposed vasoconstriction due to renin and other factors. Such an imbalance may be a trigger for HRS. Circulation of ascites Once formed, ascitic fluid can exchange with blood through a large capillary bed under the visceral peritoneum. This plays a vital, dynamic role, sometimes actively facilitating transfer of fluid into ascites and sometimes retarding it. Ascitic fluid is continuously circulating, with about half entering and leaving the peritoneal cavity every hour, there being a rapid transit in both directions. The constituents of the fluid are in dynamic equilibrium with those of the plasma. Rate of ascitic fluid reabsorption is limited to 700–900 mL daily. Summary (Fig. 10.5) Ascites in cirrhosis results from sinusoidal hypertension and sodium retention. The most accepted theory for sodium retention is the peripheral arterial vasodilatation hypothesis, which proposes that renal sodium (and water retention) is due to reduced effective blood volume secondary to peripheral arterial vasodilatation (Figs 10.3, 10.4, 10.5). The renal changes are mediated by stimulation of the RAAS, an increase in sympathetic function, and other systemic and local peptide and hormone disturbances. The overfill view suggests that renal retention of sodium is primary with secondary vascular changes and accumulation of ascites and oedema. Depending on the degree of circulatory changes (Table 10.2), these same mechanisms will lead to hyponatraemia and, at the extreme end of severity of renal and vascular changes, HRS develops (Fig. 10.5). Clinical features Symptoms The most frequent symptoms are increased abdominal girth (the patient notices tightness of the belt or garments around the waist) and recent weight gain [26]. As Table 10.2. Circulatory changes in patients with cirrhosis Increased Reduced Plasma/ total blood volume Non-central blood volume Cardiac output Portal pressure and flow Central blood volume Arterial blood pressure Splanchnic vascular resistance Systemic vascular resistance Renal blood flow 214 Chapter 10 fluid continues to accumulate, it leads to elevation of the diaphragm that may cause shortness of breath. Fluid accumulation may also be associated with a feeling of satiety and generalized abdominal pain. The rapid onset of symptoms in a matter of weeks in ascites helps to distinguish it from obesity, which develops over a period of months to years. Examination The presence of ascites in patients with cirrhosis denotes a decompensated, more advanced stage of cirrhosis, therefore stigmata of cirrhosis are usually present (spider angiomata, palmar erythema, muscle wasting). There may also be jaundice and signs of portal hypertension, such as splenomegaly and abdominal wall collaterals. Inferior vena caval collaterals result from a secondary, functional block of the inferior vena cava due to pressure of the peritoneal fluid. They commonly run from the groin to the costal margin or flanks and disappear when the ascites is controlled and intra-abdominal pressure is reduced. Physical examination is relatively insensitive for detecting ascitic fluid, particularly when the amount is small and/or the patient is obese. Patients must have at least 1500 mL of fluid to be detected reliably on physical examination. The clinical diagnosis of ascites will be questionable or incorrect in roughly a third of the cases [27]. When present in small amounts, ascites can be identified by bulging flanks. Flank dullness is very sensitive in detecting ascites [28]. When flank dullness is detected, it is useful to see whether it shifts with rotation of the patient (shifting dullness). This sign is the most sensitive finding (compared to abdominal distension, bulging flanks and fluid wave) [29]. The fluid wave sign has the poorest sensitivity in the diagnosis of peritoneal fluid, even though its specificity is high [26,28,29]. With tense ascites it is difficult to palpate abdominal viscera, but with moderate amounts of fluid the liver or spleen may be ballotted. The presence of a ballotable liver is a good indicator of the presence of ascites [26]. Associated conditions Umbilical hernias. Increased intra-abdominal pressure favours the development of diastasis recti or hernias in the umbilical, femoral or inguinal regions or through old abdominal incisions. Hernias develop in about 20 % of patients with cirrhosis and ascites (whereas only 3% have hernias without ascites), and may increase to up to 70% in patients with long-standing, recurrent, tense ascites [30]. The main risks of these hernias are rupture [31] and incarceration, the latter complication observed mostly in patients in whom ascites has reduced after paracentesis, peritoneovenous shunt or after transjugular intrahepatic portosystemic shunt [32]. Once ascites is optimally Pleural effusion ASCITES Fig. 10.7. A right-sided pleural effusion may accompany ascites and is related to defects in the diaphragm. treated, elective hernia repair with permanent mesh is the best treatment for symptomatic hernias, with far less complications than following emergent repair [33]. Hepatic hydrothorax. Pleural effusion develops in about 5–10% of patients with cirrhosis [34] and although it usually develops in patients with ascites, hepatic hydrothorax may develop in patients without detectable ascites [35]. Pleural effusion is right-sided in 85%, leftsided in 13% and bilateral in 2% of the cases [36]. It is due to defects in the diaphragm allowing ascites to pass into the pleural cavity (Fig. 10.7). Examination of pleural and ascitic fluid may not be reliable to differentiate an effusion due to local pleural disease from that due to hepatic hydrothorax [37].The diagnosis of hepatic hydrothorax can be established by radionuclide scanning of the chest after the intraperitoneal injection of Tc-99m-labelled sulphur colloid or macroaggregated serum albumin [35]. Presence of radiotracer in the pleural space is demonstrated generally within 2 hours following its intraperitoneal injection [38]. Although large amounts of ascites can accumulate in the peritoneal cavity before resulting in significant patient discomfort, the accumulation of smaller amounts of fluid (1–2 litres) in the pleural space results in severe shortness of breath and hypoxaemia. As pleural fluid is in equilibrium with peritoneal fluid, control depends on medical treatment of ascites. Aspiration is followed by rapid filling up of the pleural space by ascitic fluid. TIPS have been successful [39]; pleurodesis following complete drainage is less successful. Peripheral oedema. This usually follows ascites and is related to hypoproteinaemia. A functional inferior vena caval block due to pressure of the abdominal fluid is an additional factor. The presence of oedema without ascites should therefore lead to investigations of causes of fluid retention other than ascites. Ascites 215 Ascitic fluid Diagnostic paracentesis (of about 30 mL) should always be performed in a patient with new-onset ascites, however obvious its cause. In patients with known cirrhotic ascites, diagnostic paracentesis should be performed at every hospital admission and whenever SBP is suspected. Diagnostic paracentesis is a safe procedure with a very low incidence of serious complications, mostly transfusion-requiring haematomas that occur at a rate of 0.2 to 0.9% [40,41]. Fluid appearance is clear, green, straw-coloured or bilestained. The volume is variable and up to 70 litres have been recorded. A blood-stained fluid indicates malignant disease or a recent paracentesis or an invasive investigation, such as liver biopsy or transhepatic cholangiography. Ascites total protein and serum-ascites albumin gradient (SAAG) are two inexpensive tests that, taken together, are most useful in determining the source of ascites (Table 10.3). A high (>2.5 g/dL) ascites total protein occurs with peritoneal involvement (malignancy, tuberculosis) due to leakage of high protein mesenteric lymph from obliterated lymphatics and/or from an inflamed peritoneal surface. A high ascites total protein also occurs in cases of postsinusoidal or posthepatic sinusoidal hypertension when sinusoids are normal and protein-rich lymph leaks into the peritoneal cavity [42]. In cirrhosis, an abnormally low protein content of liver lymph has been demonstrated as a result of deposition of fibrous tissue in the sinusoids (‘capillarization of the sinusoid’), which renders the sinusoid less leaky to macromolecules [43]. On the other hand, the SAAG, which involves subtracting ascites fluid albumin concentration from serum albumin, has been shown to correlate with hepatic sinusoidal pressure [44]. A SAAG more than 1.1 g/dL indicates that there is sinusoidal hypertension and that the source of ascites is the hepatic sinusoid as in the case of cirrhosis, heart failure or Budd–Chiari syndrome [45] (Table 10.3). Ascites polymorphonuclear cells increase with peritoneal infection or with other intra-abdominal inflammatory conditions such as diverticulitis, cholecystitis. The diagnosis of SBP is established with a polymorphonuclear cell count of more than 250/mm3 [46]. In sterile ascites, ascitic fluid white blood cell count is usually less than 100/mm3 with a predominance of mononuclear cells and a low number of polymorphonuclear cells. Ascites bacteriological culture is negative in approximately 40% of patients with clinical manifestations suggestive of SBP and increased ascites polymorphonuclear cells [46]. Nevertheless, aerobic and anaerobic cultures should be performed. The percentage of positive cultures increases when ascitic fluid is inoculated directly into blood culture bottles at the bedside, which is the recommended method of culture [46]. Electrolyte concentrations are those of other extracellular fluids. The rate of accumulation of fluid is variable and depends on the dietary intake of sodium and the ability of the kidneys to excrete it. Ascitic fluid protein and white cell count, but not polymorph concentration, increase during diuresis. Radiological features Plain X-ray of the abdomen shows a diffuse groundglass appearance. Distended loops of bowel simulate intestinal obstruction. Ultrasound and CT scan show a space around the liver and these can be used to demonstrate quite small amounts of fluid (Fig. 10.8). Differential diagnosis Heart failure/ constrictive pericarditis. Diagnostic points include jugular vein distension and, in constrictive pericarditis, the paradoxical pulse and the radiological demonstration of a calcified pericardium [47]. In both cases SAAG will be more than 1.1 mg/dL and ascites protein will be more than 2.5 g/dL [48]. Right and left Table 10.3. Differential diagnosis among the three most common causes of ascites Hepatic vein pressures* Cirrhosis Serum-ascites albumin gradient (cutoff 1.1 g/dL) Ascites protein (cutoff 2.5 g/dL) WHVP FHVP HVPG High Low High Normal High Cardiac ascites High High High High Normal Peritoneal malignancy/ peritoneal TB Low High Normal Normal Normal * Only to be performed in equivocal cases. WHVP, wedged hepatic venous pressure; FHVP, free hepatic venous pressure; HVPG, hepatic venous pressure gradient. 216 Chapter 10 Table 10.4. Spontaneous bacterial peritonitis Suspect grade B and C cirrhosis with ascites Clinical features may be absent and peripheral WBC normal Ascitic protein usually <1 g/dL Usually monomicrobial and Gram-negative Start antibiotics if ascites >250 mm polymorphs Concomitant albumin use if renal dysfunction or jaundice 20% die 69% recur in 1 year non-surgical chylous ascites is cirrhosis [51,52]. Management is of the underlying cause and a low-fat medium chain triglyceride diet for 3 weeks, or if this fails total parenteral nutrition for 4–6 weeks. Fig. 10.8. CT scan showing an irregular cirrhotic small liver, splenomegaly and ascites (arrow). heart catheterization and transjugular liver biopsy with measurements of hepatic venous pressure gradient may be necessary to make the differential between cardiac and cirrhotic ascites [27] (Table 10.3). Malignant ascites. There may be symptoms and localizing signs due to the primary tumour. After paracentesis, the liver may be enlarged and nodular. Fluid cytological exam should be performed, although normal endothelial cells in the peritoneum can resemble malignant cells. Massive hepatic metastasis can lead to the development of ascites but since the mechanism of ascites formation is sinusoidal hypertension, these cases of ‘malignant ascites’ will have the characteristics of cirrhotic ascites [49,50]. Tuberculous ascites. This should be suspected particularly in the severely malnourished alcoholic who may be febrile. Rarely, lumps of matted omentum can be palpated after paracentesis. Ascitic fluid has many lymphocytes. When suspected, ascites should be stained for tubercle bacilli, and suitable cultures set up. Mixed aetiology ascites. In patients with mixed ascites (e.g. cirrhosis with superimposed peritoneal malignancy or tuberculosis), the SAAG is high and the ascites protein is low, that is the findings of ascites due to cirrhosis predominate [48,50]. Chylous ascites. This results from accumulation of fat, predominantly chylomicrons, in the ascitic fluid. Its appearance is milky and diagnosis is confirmed on a triglyceride ascites content more than 200 mg/dL. The most common cause of chylous ascites is postsurgical disruption of lymphatics. The most common cause of Hepatic venous obstruction (Budd–Chiari syndrome). This must be considered, especially if the protein content of the ascitic fluid is high and the SAAG is high. Pancreatic ascites. Ascites is rarely gross. It develops as a complication of acute pancreatitis with pseudocyst rupture, or from pancreatic duct disruption. The amylase content of the ascitic fluid is very high. Ovarian tumour. This is suggested by resonance in the flanks. The maximum bulge is anteroposterior and the maximum girth is below the umbilicus. Spontaneous bacterial peritonitis (Table 10.4) [46] The most common infection in cirrhosis is spontaneous bacterial peritonitis (SBP). It is called spontaneous because it occurs in the absence of a contiguous source of infection (e.g. intestinal perforation, intra-abdominal abscess) and in the absence of an intra-abdominal inflammatory focus (e.g. abscess, acute pancreatitis, cholecystitis). SBP occurs in 9% of hospitalized patients with cirrhosis and accounts for 25% of all infections [53]. It is particularly frequent in severely decompensated cirrhosis. Spontaneous bacterial empyema is an entity akin to SBP in which hepatic hydrothorax becomes infected. Its diagnosis and management are the same as for SBP [54]. SBP is blood-borne and in 90% monomicrobial. Bacteria of gut origin are the most commonly isolated causative organisms. Therefore, migration of enteric bacteria across the intestinal mucosa to extraintestinal sites and the systemic circulation (bacterial translocation) has been implicated in its pathogenesis [55]. In cirrhosis, an overactive sympathetic nervous system slows gut motility and facilitates bacterial stasis and overgrowth, thereby facilitating bacterial translocation. Ascites 217 GI haemorrhage RE function BACTERAEMIA Enteric bacterial translocation Prognosis Invasive procedures, catheters BACTERASCITES Poor SBP Ascitic fluid opsonic activity tion generated by tumour necrosis factor and interleukin 6 [60]. Good Resolution Fig. 10.9. The pathogenesis of spontaneous bacterial peritonitis (SBP) in patients with cirrhosis. GI, gastrointestinal; RE, reticuloendothelial. With SBP, 10–20% of patients will die during that hospital admission. The 1-year probability of SBP recurrence is 69% and median survival of a patient who develops SBP is 9 months [61]. Mortality depends on the development of renal dysfunction [62] and the site of acquisition of the infection, with nosocomial infection being an important predictor of death [63–65]. SBP resolution and immediate survival are 100% in community-acquired SBP that is uncomplicated (i.e. no renal dysfunction, no encephalopathy) whether patients receive oral or intravenous antibiotics [66]. Treatment Persistence of bacteria in extraintestinal sites is favoured by impaired host defences. In cirrhosis, host defences are abnormal because of portosystemic shunting and impaired reticuloendothelial function. Neutrophils are abnormal in the alcoholic. Decreased synthesis of proteins, such as complement and fibronectin, result in diminished adhesiveness and decreased bacterial phagocytosis [56]. Ascitic fluid favours bacterial growth and deficient ascitic opsonins lead to defective coating of bacteria which are indigestible by polymorphs. The opsonic activity of the ascitic fluid is proportional to protein concentration and SBP is more likely if ascitic fluid protein is less than 1 g/dL [57] (Fig. 10.9). Infection with more than one organism or with fungi is likely to be associated with colonic perforation or dilatation, or any intra-abdominal source of infection (i.e. secondary peritonitis). SBP should be suspected when a patient with cirrhosis deteriorates, particularly with encephalopathy and/ or jaundice. Patients with variceal bleeding or with previous SBP are at particular risk. Pyrexia, local abdominal pain and tenderness, and systemic leukocytosis may be noted. These features, however, may be absent and the diagnosis is made following a high index of suspicion with examination of the ascitic fluid. The diagnosis of SBP is established with an ascites polymorophonuclear count more than 250/ mm3 [46]. The infecting organisms are commonly Escherichia coli or group D streptococci [58]. Anaerobic bacteria are rarely found. Blood cultures are positive in 50%. Bacterascites (positive culture, polymorphonuclear cells <250/mm3) may resolve without treatment but can progress to SBP [59]. Patients with SBP are particularly at risk of renal complications, probably related to systemic vascular changes secondary to inflammatory response to infec- Antibiotics should be started empirically in all patients with ascites showing more than 250 polymorphonuclear cells/mm3, except in those in whom a local inflammatory reaction is identified (e.g. diverticulitis, cholecystitis, etc.). Five to seven days of a third-generation cephalosporin such as cefotaxime administered intravenously is usually effective [67,68]. For cefotaxime the optimal cost-effective dosage is 2 g every 12 h. Amoxycillinclavulanic acid is as effective as cefotaxime [69]. The antibiotic choice should be reviewed once results of ascitic culture and sensitivity of the bacterial isolates are known. Because of renal toxicity, aminoglycosides should be avoided. In a randomized study the administration of intravenous albumin to patients with SBP treated with cefotaxime significantly reduced the incidence of renal impairment (10 vs. 33%) and hospital mortality (10 vs. 29%) [62]. Patients that benefit most from the use of albumin are those with renal dysfunction at baseline (creatinine >1.0 mg/dL and/or blood urea nitrogen >30 mg/dL) and serum bilirubin more than 4 mg/dL [62,70,71]. Success rates for cefotaxime and amoxicillin-clavulanic may be as low as 44% in nosocomial SBP because of the presence of multidrug-resistant organisms [72,73]. Extended spectrum antibiotics (e.g. carbapenems, piperacillin/ tazobactam) should be used as initial empirical therapy in patients with hospital-acquired SBP, particularly in those who had been on beta-lactams during admission, had been recently hospitalized or on quinolone prophylaxis [72]. Secondary bacterial peritonitis should be suspected when a suspected SBP fails to respond to antibiotic therapy. Because of reduced survival, SBP is an indication to consider hepatic transplantation, particularly if recurrent. 218 Chapter 10 Prophylaxis Long-term prophylaxis will lead to the emergence of resistant bacteria [53]. Therefore, only patients at the highest risk of developing SBP should receive antibiotic prophylaxis. The risk of SBP is particularly high in patients with cirrhosis with upper gastrointestinal haemorrhage. Oral administration of norfloxacin (400 mg/12 h for a minimum of 7 days) is currently recommended for this group [46]. However, intravenous ceftriaxone should be considered in high quinolone resistance settings or in patients with two or more of the following: malnutrition, ascites, encephalopathy or serum bilirubin more than 3 mg/dL [74]. SBP and other infections should be ruled out by bacterial cultures before starting prophylaxis. In patients with a previous episode of SBP, the risk of recurrence during the subsequent year is 40–70%. Oral administration of norfloxacin (400 mg/day) is recommended in such patients, who should then be evaluated for liver transplantation [46,75]. There is currently insufficient evidence to recommend prophylaxis for patients with a low ascitic fluid protein (<1 g/dL). However, norfloxacin prophylaxis appears justified in patients with advanced liver failure (Child– Pugh score >9 points with serum bilirubin level >3 mg/ dL) or impaired renal function (serum creatinine level >1.2 mg/dL, blood urea nitrogen level >25 mg/dL, or serum sodium level <130 mEq/L). In these patients, the 1-year probability of first SBP is 60% and is significantly reduced with norfloxacin [76] . In patients with a high ascitic fluid protein (>1 g/dL) without a past history of SBP, prophylaxis is not necessary as the 1-year probability of SBP is nil [77]. Treatment of cirrhotic ascites [78,79] Therapy of ascites, whether by diuretics or paracentesis, reduces clinical symptoms and improves quality of life. However, although the initial clinical response may be excellent, if fluid loss is excessive it may lead to hyponatraemia, hyperkalaemia, renal failure or encephalopathy. Treatment must therefore be appropriate to the clinical state and the response properly monitored. The approach must be tailored to the patient. The spectrum of therapeutic intervention ranges from sodium restriction alone (rarely used), to diuretic use, therapeutic paracentesis (Table 10.5), and, for the most severe groups, TIPS and eventually liver transplantation. Indications for treatment include the following: • Symptomatic ascites with abdominal distension sufficient to be obvious and produce physical or emotional distress requires treatment with sodium restriction and diuretics. The presence of subclinical ascites (that seen only on ultrasound without clinical symptoms) may not require active treatment, although to prevent deterioration advice on a reduction in sodium intake is wise. Inappropriate introduction of excessive treatment for ascites may lead to symptomatic hypotension, muscle cramps, dehydration, and renal dysfunction. • Large ascites, causing abdominal discomfort or pain and/or dyspnoea most often demands paracentesis. • Tense ascites with pain may lead to eversion and ulceration of an umbilical hernia, which is near to rupture. This complication has a very high mortality, due to shock, renal failure and sepsis, and urgent paracentesis is indicated. Monitoring during treatment is mandatory. The patient should be weighed daily as it provides a satisfactory guide to progress. Urinary electrolyte (sodium, potassium) determinations are helpful in determining dosage, monitoring the response and assessing compliance. Serum electrolytes and creatinine should be measured two to three times per week while the patient is in hospital. Where liver disease is due to alcohol, the patient should be encouraged to abstain. The mild case is managed as an out-patient by diet and diuretics, but if admitted to hospital, paracentesis is usually a first procedure. In a survey of European hepatologists, 50% used paracentesis initially, followed by diuretics [80]. Fifty per cent regarded complete control of ascites as Table 10.5. General management of ascites Diagnostic paracentesis with first presentation or with any symptom/ sign suggestive of SBP 70–90 mmol sodium diet; weigh daily; check serum creatinine and electrolytes Spironolactone 100 mg daily If tense ascites consider paracentesis (see Table 10.7) After 4 days consider adding frusemide (furosemide) 40 mg daily; check serum creatinine and electrolytes Maximum daily weight loss 0.5 kg/day (1.0 kg/day in those with peripheral oedema) Stop diuretics if precoma (‘flap’), hypokalaemia, azotaemia or alkalosis Continue to monitor weight; increase diuretics as necessary Avoid non-steroidal anti-inflammatory drugs SBP, spontaneous bacterial peritonitis. Ascites 219 desirable, whereas the other half was satisfied with symptomatic relief without removing all the ascites. Thus consensus on standardized treatment regimes is difficult to reach because of the clinical spectrum of ascites, the clinical success of the different regimens and the lack of evidence-based studies comparing individual approaches. Bed rest used to be a feature of initial therapy. Evidence for benefit is sparse but as part of an overall strategy in combination with diuretics it has been found to be beneficial [81]. This may be related to increased renal perfusion and portal venous blood flow during recumbency. Sodium restriction/ diet The patient with cirrhosis who is accumulating ascites on an unrestricted sodium intake excretes less than 10 mmol (approximately 0.2 g) sodium daily in the urine. Extrarenal loss is about 0.5 g. Sodium taken in excess of 0.75 g will result in ascites, with every gram retaining 200 mL of fluid. Historically, such patients were recommended a diet containing 22–40 mmol/day of sodium (approximately 0.5–1.0 g/day). However, such diet is unpalatable and also compromises protein and calorie intake, which in patients with cirrhosis is critical for proper nutrition. Current recommendations are to use a ‘no added salt’ diet (approximately 70–90 mmol or approximately 1.5–2.0 g/day) combined with diuretics to increase urinary sodium excretion (Table 10.6). In this diet, salt should not be used at the table or when cooking. Also, various foods containing sodium should be restricted or avoided (Table 10.6). Many low-sodium foods are now available. A few patients with ascites may respond to this regimen alone, but usually the first line of treatment for ascites includes diuretics. Patients prefer the combination of diuretics and a modest restriction of sodium to severe sodium restriction alone. Very occasionally if there is a good response, diuretics may be withdrawn and the patient maintained on dietary sodium restriction alone. Good responders are liable to be those: • with ascites and oedema presenting for the first time in an otherwise stable patient; • with a normal creatinine clearance (glomerular filtration rate); • with an underlying reversible component of liver disease such as alcoholic hepatitis; • in whom the ascites has developed acutely in response to a treatable complication such as infection or bleeding, or after a non-hepatic operation; • with ascites following excessive sodium intake, such as in sodium-containing antacids or purgatives, or mineral waters with a high sodium content. Diuretics The major reason for sodium retention in cirrhosis is hyperaldosteronism due to increased activity of the renin–angiotensin system. There is avid reabsorption of sodium from the distal tubule and collecting duct (Fig. 10.4). Diuretics can be divided into two main groups (Fig. 10.10) according to their site of action. The first group inhibits Na+–K+–Cl− (NKCC2) cotransporter in the ascending limb of the loop of Henle and includes frusemide (furosemide) and bumetamide. It is not appropriate to use these alone since the sodium remaining in the tubule as a result of diuretic action is reabsorbed in the distal tubule and collecting duct because of hyperaldosteronism. A randomized controlled trial has shown frusemide alone to be less effective than spironolactone [16]. Thiazides inhibit sodium in the distal convoluted tubule, have a longer half-life, may cause hypotension, and should not be used in the treatment of ascites. The second group, spironolactone (an aldosterone antagonist), amiloride and triamterene, (inhibitors of the sodium channel) block sodium reabsorption in the distal tubule and collecting duct. They are the drugs of first choice in the treatment of ascites due to cirrhosis. They are weakly natriuretic but conserve potassium. Potassium supplements are not usually necessary— indeed this type of diuretic sometimes needs to be temporarily stopped because of hyperkalaemia [82]. There are two therapeutic approaches that can be used initially: spironolactone alone, or a combination of spironolactone with frusemide. Both have their advocates and may be chosen depending on the degree of ascites [82,83]. Spironolactone alone. The starting dose is 50–100 mg/day according to the degree of ascites. If there has been insufficient clinical response after 3–4 days (weight loss less than 300 g/day), then the dose is increased by 100 mg/day every 4 days to a maximum of 400 mg/day, unless hyperkalaemia develops. Lack of clinical response indicates the need to check the urinary sodium, because a high value will identify the occasional patient who is exceeding the prescribed low sodium diet. The disadvantage of starting with spironolactone alone is the delay before its clinical effect and associated hyperkalaemia [82]. If there is insufficient clinical response or no response on spironolactone alone (when taking 200 mg/day) or associated hyperkalaemia, a loop diuretic such as frusemide is added at a dose of 20–40 mg/day. Combination therapy. Treatment is started with the combination of spironolactone (100 mg) and frusemide (40 mg) daily. The disadvantage of starting with 220 Chapter 10 Table 10.6. Advice for ‘no added salt diet’ (70–90 mmol/day or 1.5–2.0 g/day) Omit Anything containing baking powder or baking soda (contains sodium bicarbonate): pastry, biscuits, crackers, cakes, self-raising flour and ordinary bread (see restriction below) All commercially prepared foods (unless designated low salt—check packet) Dry breakfast cereals except Shredded Wheat, Puffed Wheat or Sugar Puffs Tinned/ bottled savouries: pickles, olives, chutney, salad cream, bottled sauces Tinned meats/ fish: ham, bacon, corned beef, tongue, oyster, shellfish Meat and fish pastes; meat and yeast extracts Tinned/ bottled vegetables, soups, tomato juice Sausages, kippers Cheese, ice-cream Candy, pastilles, milk chocolate Salted nuts, potato crisps, savoury snacks Drinks: especially Lucozade, soda water, mineral waters according to sodium content (essential to check sodium content of mineral waters, varies from 5 to 1000 mg/L) Restrict Milk (300 mL = half pint/day) Bread (two slices/day) Free use Fresh and home-cooked fruit and vegetables of all kinds Meat/poultry/fish (100 g/day) and one egg; egg may be used to substitute 50 g meat (2 oz) Unsalted butter or margarine, cooking oils, double cream Boiled rice, pasta (without salt), semolina Seasonings help make restricted salt meal more palatable: include lemon juice, onion, garlic, pepper, sage, parsley, thyme, marjoram, bay leaves Fresh fruit juice, coffee, tea Mineral water (check sodium content) Marmalade, jam Dark chocolate, boiled sweets, peppermints, chewing gum Salt substitutes (not potassium chloride) Salt-free bread, crispbread, crackers or matzos combination therapy may be the need for closer laboratory monitoring [83]. Monitoring of daily weight is necessary. The rate of ascitic fluid reabsorption is limited to 700–900 mL/day. If a diuresis of 2–3 litres is induced, much of the fluid must come from non-ascitic, extracellular fluids including oedema fluid and the intravenous compartment. This is safe so long as oedema persists. Indeed diuresis may be rapid (greater than 2 kg daily) until oedema disappears [84]. To avoid the risk of renal dysfunction there should be a maximum daily weight loss of 0.5 kg/ day, with a maximum of 1.0 kg/day in those with oedema. Intravascular volume expansion with intravenous albumin increases natriuresis in response to diuretics, but is expensive and not cost-effective [85]. Long-term spironolactone causes painful gynaecomastia in males and should then be replaced by 10– 15 mg/day of amiloride. However, this is less effective than spironolactone. Before diuretic therapy is deemed to have failed (diuretic-refractory ascites) non-compliance with sodium Ascites 221 night is often helpful to prevent cramps [87], otherwise quinine water can be recommended; weekly intravenous albumin is also effective [87]. Follow-up advice Na+ 1 Na+ Na+ 2 Fig. 10.10. Site of action of diuretics. 1 = loop diuretics: frusemide (furosemide), bumetamide. 2 = distal tubule/ collecting duct: spironolactone, amiloride, triamterene. restriction should be ruled out by measuring 24-h urinary sodium excretion. If this is greater than the ‘prescribed dietary’ sodium intake the patient is not complying with the restriction. Another cause of a lack of response to diuretics are concomitant use of nonsteroidal anti-inflammatory agents, and angiotensin converting enzyme blockers or angiotensin receptor blockers [86]. Failure to respond to diuretics often occurs in those with very poor hepatocellular function who have a poor prognosis without liver transplantation. In such refractory patients, diuretics have eventually to be withdrawn because of intractable uraemia, hypotension or encephalopathy. Complications Rising urea and creatinine reflect contraction of the extracellular fluid volume and reduced renal circulation (prerenal azotaemia). Hepatorenal syndrome may be precipitated. It is necessary to interrupt or reduce diuretic therapy and use plasma expansion with albumin in more severe cases. Encephalopathy may follow any profound diuresis and is usually associated with prerenal azotaemia, hypokalaemia and hypochloraemic acidosis. Hyperkalaemia reflects the effect of spironolactone, which should be reduced or interrupted according to the level of serum potassium. If the level of potassium is not dangerous, frusemide can be added to therapy at this point. Painful gynaecomastia may be caused by spironolactone, which should be reduced or discontinued and substituted by amiloride. Muscle cramps may be a problem. They indicate the need to review the dose of diuretic, but can occur without their use. Quinine sulphate 300 mg given at The out-patient should adhere to the low-sodium diet, and abstain from alcohol where this is the cause of liver disease. Bathroom scales should be used to allow a record of daily weight at the same time of day, nude or with similar clothing. This daily record should be kept and brought to the physician at each visit. The dose of diuretics depends upon the degree of ascites and the severity of the liver disease. A usual regime is 100–200 mg spironolactone (or 10–20 mg amiloride) daily with frusemide 40–80 mg daily for the patient with more marked ascites initially, or with a poor response to spironolactone alone. Serum electrolytes, creatinine, urea and liver function tests are monitored every 4 weeks for the stable out-patient. In the patient who has been treated initially as an in-patient, an earlier check at 1 week after discharge allows an adjustment to the management plan before electrolyte or clinical imbalance has occurred. As liver function improves and the oedema and ascites resolve, it may be possible to stop the frusemide first and then the spironolactone. Symptoms such as postural dizziness and thirst indicate over-enthusiastic treatment. The ‘no added salt’ (70–90 mmol/day or 1.5–2.0 g/day) is maintained in the majority of patients. Therapeutic abdominal paracentesis (Table 10.7) This procedure was abandoned in the 1960s because of the fear of causing acute renal failure. Moreover, the loss of approximately 50 g of protein in a 5-litre paracentesis led to patients becoming severely malnourished. New interest came with the observation that a 5-litre paracentesis was safe in fluid- and salt-restricted patients with ascites and peripheral oedema [88]. This work was extended to daily 4–5-litre paracenteses with 40 g saltpoor albumin infused intravenously over the same period [81]. Finally, a single total paracentesis, about 10 litres in 1 h combined with intravenous albumin (6–8 g/L ascites removed) was shown to be equally effective and safe (Table 10.7) [89,90]. In a controlled trial, serial large-volume paracenteses (LVP) reduced hospital stay compared with standard diuretic treatment [81]. However, readmissions to hospital, survival and causes of death did not differ significantly between the LVP and diuretic groups. Total paracentesis results in hypovolaemia as reflected by a rise in plasma renin levels [88], and can lead to hypotension and renal failure (postparacentesis circulatory syndrome) [88]. 222 Chapter 10 Table 10.7. Therapeutic paracentesis Selection Large or tense ascites Routine No volume limit Table 10.8. Hyponatraemia Serum sodium <130 mEq/L Present in 22% of patients with ascites May contribute to encephalopathy and poor quality of life Water restriction (1–1.5 L/day) ‘Vaptans’ correct sodium but are still under investigation Poor prognostic marker i.v. salt-poor albumin: 6–8 g/L removed No need to perform cell count unless symptoms/ signs suggestive of SBP Advantages Comfort Shortens hospital stay SBP, spontaneous bacterial peritonitis. Albumin replacement is more effective in preventing postparacentesis hypovolaemia and hyponatraemia than less costly plasma expanders such as dextran 70, dextran 40 and polygeline [91]. Major complications, mostly bleeding, have been associated with therapeutic but not diagnostic procedures and tend to be more prevalent in patients with low platelet count (<50 000) and Child–Pugh class C [92]. Major bleeding occurs rarely but may be lethal [93] and is mostly related to puncture of collaterals rather than as a result of coagulopathy. In a series of over 1000 LVPs there was no significant bleeding, even in patients with marked thrombocytopenia or prothrombin time prolongation [94]. Therefore clotting abnormalities should not be considered a contraindication to LVP. Leakage of ascitic fluid is rare and occurs when extraction of ascites is incomplete. Therefore, this complication can be solved by completing the LVP, preferably in a site remote from the leaking puncture site. Similarly, another rare complication of paracentesis is the development of sudden scrotal oedema that results from subcutaneous tracking of peritoneal fluid into the scrotum and which should be treated by elevation of the scrotum [95]. Summary Paracentesis is a safe, cost-effective treatment for cirrhotic ascites. However, approximately 90% of patients with ascites respond to sodium restriction and diuretics, and paracentesis is generally a second-line treatment except for patients with tense and refractory ascites (see below). Despite this, many clinicians opt for early paracentesis rather than waiting for diuretics to be effective [81]. Intravenous salt-poor albumin should be used concomitant to LVP, particularly when more than 5 litres are removed. The paracentesis must be followed by an optimal salt-restricted diet and diuretic regimen. Hyponatraemia [96] (Table 10.8) Hyponatraemia develops in approximately 20–30% of cirrhotic patients with ascites and is defined as a serum sodium concentration less than 130 mEq/L [97,98]. Hyponatraemia in cirrhosis is dilutional. Although hyponatraemia is usually asymptomatic, some patients may complain of anorexia, nausea and vomiting, lethargy and occasionally seizures. Hyponatraemia has been associated with a further reduction in brain organic osmolytes, particularly myoinositol, suggesting that it may play a role in the pathogenesis of hepatic encephalopathy [99]. Serum sodium concentrations of less than 130 mmol/L are treated by fluid restriction, to avoid further reduction in concentrations. Advances in the understanding of the pathogenesis are leading to pharmacological approaches to treatment. Mechanism Eighty per cent of the water in the glomerular filtrate is reabsorbed in the proximal tubule and descending limb of Henle. The ascending limb of Henle and distal tubule are impermeable to water. Control of the volume of water passed in urine is dependent on the amount of water reabsorbed in the collecting tubule and collecting duct. This is under the control of vasopressin, which interacts with V2 receptors on the cells of the renal collecting ducts (Fig. 10.4). Vasopressin receptor activation stimulates the translocation of the water channel aquaporin 2 from a cytoplasmic vesicular compartment to the apical membrane. This mechanism may be affected by prostaglandins which inhibit vasopressin-stimulated water reabsorption. Vasopressin is produced in the hypothalamus. Production is controlled in two ways: by osmoreceptors in the anterior hypothalamus under the influence of plasma osmolarity, and by parasympathetic stimulation as a result of activation of baroreceptors in the atria, ventricles, aortic arch and carotid sinus. Water retention in patients with cirrhosis and ascites is due to excess vasopressin as a result of baroreceptor stimulation. This Ascites 223 is thought to be related to the reduced effective circulating volume as a result of splanchnic and systemic vasodilatation—the same circulatory abnormality which leads to activation of the renin–angiotensin–aldosterone axis and the sympathetic nervous system and sodium retention. However, alterations in sodium and water handling are not synchronous, sodium abnormalities occurring first (Fig. 10.5). Vasopressin concentrations are not grossly elevated in cirrhosis. However, the normal inhibition of vasopressin by a water load is blunted or absent. Although there is reduced hepatic metabolism of vasopressin in patients with cirrhosis, related to the severity of disease, this is not thought to be the primary reason for water retention. Treatment Hyponatraemia reflects reduced free water clearance. In the patient with severe hepatocellular dysfunction it may also indicate the passage of sodium into the cells. If the serum sodium falls below 130 mmol/L, fluid intake should be restricted to 1–1.5 litres per day [19]. Intravenous albumin is beneficial but its effect is transient [100]. Several approaches are being studied to increase free water clearance. Drugs such as kappa-opioid receptor agonists, which inhibit vasopressin release, and demeclocycline, which interferes with generation and action of cAMP in collecting ducts, have been reported to be effective but their use has been abandoned due to important side effects [101,102]. V2 receptor antagonists (‘vaptans’) have been the most investigated aquaretic agents. The short-term (7–14 days) use of lixivaptan [103,104] or satavaptan [105] was effective in increasing serum sodium. However, their use was associated with severe sideeffects, dehydration and Q–T prolongation, respectively, and has led to their withdrawal. In a large multicenter randomized trial, tolvaptan used for 30 days in patients with euvolaemic or hypervolaemic hyponatraemia (of whom 63 had cirrhosis), was associated with a rapid improvement in serum sodium and significant weight loss compared to placebo, without significant side effects [106]. Longer-term trials targeting patients with cirrhosis are awaited. nized that hyponatraemia is a predictor of reduced survival in cirrhotic patients with ascites [107,108] and is a risk factor for encephalopathy and the HRS syndrome [96,98]. Liver transplantation should be considered providing serum sodium can be increased to 125 mmol/L or more. Refractory ascites [109,110] (Table 10.9) This is defined as ascites that cannot be mobilized or prevented from recurring by medical therapy. It is divided into diuretic-resistant (ascites is not mobilized despite maximal diuretic dosage) and diuretic-intractable ascites (development of diuretic-induced complications that preclude the use of an effective diuretic dosage) [109]. Dietary history, use of NSAID or angiotension converting enzyme or angiotensin II receptor blockers [86], and patient compliance with the treatment regimen must be reviewed before confirming the diagnosis. Treatment The therapeutic options for patients with refractory ascites include repeated LVPs, TIPS, peritoneovenous (Le Veen) shunting and liver transplantation. Therapeutic paracentesis This has been discussed above as initial treatment for the patient with tense severe ascites. For refractory ascites repeated LVP plus albumin is the most accepted initial therapy. It is easy to perform and relatively inexpensive compared to other therapies such as the peritoneovenous shunt. In this group of patients recurrence of ascites is the rule because paracentesis is symptomatic therapy that does not act on the mechanisms responsible for ascites formation. Patients generally require paracentesis every 2 to 4 weeks. Reintroduction of diuretic treatment after paracentesis lengthens time to recurrence [111] in patients with a urinary sodium greater Table 10.9. Refractory ascites First line: Second line: Summary Although advances are being made in pharmacological approaches to correct water retention and the associated hyponatraemia, these are not yet clinically applicable. The mainstay of treatment is fluid restriction. Intravenous albumin infusion may be effective in the short term [100]. Whichever approach is used, it should be recog- Third line: Serial therapeutic paracenteses Relapse is the rule TIPS When paracenteses >1–2/month MELD <15 ?Survival benefit Peritoneovenous shunt Non-LVP, non-TIPS candidates TIPS, transjugular intrahepatic portosystemic shunt; MELD, Model for End Stage Liver Disease; LVP, largevolume paracenteses. 224 Chapter 10 and have reasonable hepatic reserve with normal or minimal renal dysfunction. Peritoneovenous (Le Veen) shunt Fig. 10.11. The transjugular intrahepatic portosystemic shunt (TIPS) decompresses hepatic sinusoids. than 30 mEq/L. In others, diuretics should be discontinued, particularly if associated with complications [110]. Transjugular intrahepatic portosystemic shunt (TIPS) Side-to-side portacaval shunts, unlike end-to-side shunts, decompress the hepatic sinusoids (Fig. 10.11) and had been shown to be effective in the treatment of ascites. However, they have been abandoned because of the associated morbidity and mortality of major surgery and the advent of TIPS, which is a less invasive procedure that achieves the same decompression of the sinusoid [112]. Early experience with TIPS showed a reduction in diuretic requirements, and a fall in plasma renin and aldosterone activities. However, TIPS may precipitate hepatic encephalopathy and/or liver failure. Not surprisingly, since TIPS acts on the pathophysiological mechanisms responsible for ascites TIPS is more effective than LVP in preventing recurrence of ascites in randomized comparative trials [113,114], but had a higher risk for severe encephalopathy, without differences in mortality. A meta-analysis of individual patient data in randomized studies showed that mortality was significantly lower in patients treated with TIPS and identified a Model for End Stage Liver Disease (MELD) score above 15 as having a high risk of death [115]. In trials performed to date, uncovered TIPS stents were used. Uncovered stents frequently obstruct (18 to 78%) [116] and have been largely substituted by polytetrafluoroethylene-covered stents which are associated with a significantly lower obstruction rate. [117]. Until results of ongoing trials using covered stents are available, TIPS should be considered second-line treatment for refractory ascites, and reserved for patients who require frequent paracentesis This consists of a plastic tube with multiple holes that is placed in the peritoneal cavity and is connected to a unidirectional pressure-sensitive valve lying extraperitoneally, from which a silicone rubber tube passes subcutaneously to the neck and thence to the internal jugular vein and superior vena cava (SVC). When the diaphragm descends during inspiration, the intraperitoneal fluid pressure rises while that in the intrathoracic SVC falls. This allows ascitic fluid to pass from the peritoneal cavity into the general circulation. It is generally inserted under general anaesthesia. Flow of ascites along the shunt depends upon this pressure gradient between peritoneal cavity and SVC. The peritoneovenous shunt may control ascites over many months. It produces sustained expansion of the circulating blood volume and a fall in plasma levels of renin–angiotensin, noradrenaline and antidiuretic hormone. Renal function and nutrition improve. In uncontrolled studies, peritoneovenous shunts resulted in frequent blockage, severe complications (disseminated intravascular coagulation, pulmonary oedema, variceal haemorrhage) and high perioperative mortality. However, randomized trials comparing peritoneovenous shunt with LVP and albumin replacement resulted in similar efficacy, with similar complication rates and survival [89,118]. Since paracentesis with albumin replacement is simpler and can be done on an out-patient basis, it is the preferred procedure. Additionally, peritoneovenous shunt may hinder future placement of TIPS and may complicate liver transplant surgery due to peritoneal adhesions. Therefore, it is mostly indicated in patients who require LVP frequently and who are not candidates for TIPS [119]. Hepatorenal syndrome [120] Hepatorenal syndrome (HRS) is the development of renal failure in patients with severe liver disease in the absence of any identifiable renal pathology. It is a functional rather than structural disturbance in renal function. The histology of the kidney is virtually normal. Such kidneys have been successfully transplanted, following which they functioned normally. After liver transplantation, kidney function also usually returns to normal. The mechanism is not fully understood, but the renal disturbance is thought to represent the severest form of vascular and neurohumoral changes associated with severe liver disease, which in a less severe form results in ascites (Figs 10.5, 10.12) [7]. Ascites 225 • Worsening liver function • Precipitants* Peripheral vasodilatation Further vasodilatation Diminished effective arterial blood volume Further decrease in effective arterial blood volume Rise in renin, aldosterone, vasopressin Sympathetic stimulated Further rise in vasoactive systems Sodium and water retention Renal vasoconstriction Intense renal vasoconstriction Plasma volume expansion plus portal hypertension Decreased renal perfusion Ascites Hepatorenal syndrome Decreased cardiac output Fig. 10.12. Mechanism for hepatorenal syndrome. *Precipitants include bacterial infections (particularly spontaneous bacterial peritonitis), hypovolaemia (gastrointestinal haemorrhage, over-diuresis, diarrhoea), vasodilators. Table 10.10. Criteria for diagnosis of hepatorenal syndrome [122] 1 Cirrhosis with ascites 2 Serum creatinine >1.5 mg/dL (>133 μmol/L) 3 No improvement in serum creatinine (decrease to 1.5 mg/dL or less) after at least 2 days of diuretic withdrawal and expansion of plasma volume with albumin (1 g/kg of body weight/day up to a maximum of 100 g/day) 4 Absence of shock 5 No current or recent treatment with nephrotoxic drugs or vasodilators 6 Absence of parenchymal kidney disease as indicated by proteinuria >500 mg/day, microhaematuria (>50 red blood cells per high power field), and/or abnormal renal ultrasonography HRS is a rare but severe complication in patients with cirrhosis and ascites. From first presentation with ascites, the 5-year probability of developing HRS is 11% [97], with increasing probability in patients who develop hyponatraemia or refractory ascites. Without liver transplantation and prior to the recent studies of treatment using vasocontrictors, recovery of renal function was unusual (<5% of patients) and prognosis was poor with a median survival of 2 weeks [121]. Diagnostic criteria (Table 10.10) These are based largely on abnormal creatinine, the absence of other causes of renal failure and the absence of sustained improvement in renal function after diuretic withdrawal and plasma volume expansion [122]. The occurrence of shock before deterioration of renal function precludes a diagnosis of HRS and is more indicative of acute tubular necrosis (ATN) [120]. Additional criteria describe the characteristics of urine volume and content, but since these may be present with other types of renal failure, for example ATN, they are not considered essential for the diagnosis of HRS [120]. Classification HRS syndrome may be classified into two types: Type 1. Patients have a rapidly progressive (less than 2 weeks) reduction of renal function with doubling of the initial serum creatinine to greater than 2.5 mg/dL (220 μmol/L) [122]. However, as recently proposed [120], a diagnosis of HRS (type 1) should be considered whenever there are criteria for acute kidney injury, namely an abrupt increase in serum creatinine ≥0.3 mg/ dL (≥26.4 μmol/L) or an increase ≥150% (1.5-fold) from baseline [123]. This ensures that treatment is not unnecessarily delayed as baseline creatinine is a predictor of HRS reversal with vasoconstrictors [124]. Type 2. Patients satisfy the criteria for the diagnosis of HRS but the renal failure does not progress rapidly [122]. These patients usually have relatively preserved 226 Chapter 10 hepatic function with refractory ascites. Survival is reduced compared with patients with cirrhosis and ascites and normal renal function. Mechanism The peripheral arterial vasodilatation theory for the formation of ascites proposes initial splanchnic and systemic arterial dilatation with consequent stimulation of the sympathetic nervous system (raised noradrenaline) and the renin–angiotensin system. This is the result of activation of volume receptors responding to vascular under-filling. Initially, despite changes in vasoconstrictors and vasodilators, renal function is preserved. HRS occurs with extreme vasodilatation, decrease in cardiac output [125] and an imbalance between systemic and intrarenal vasodilator and vasoconstrictor mechanisms, with increases in vasoconstrictors such as thromboxane A2 and endothelin [126] and decreases in vasodilators such as prostaglandin E2 and nitric oxide [127]. Table 10.11. Iatrogenic causes of acute kidney injury in cirrhosis Drugs Treatment Diuretics Lactulose NSAID (prostaglandin inhibition) Aminoglycosides Volume expansion Volume expansion Stop drug Diagnose urine β2-microglobulins Haemofiltration Ciclosporin NSAID, non-steroidal anti-inflammatory drug. usually in the alcoholic. Hepatitis B and C are associated with immune-related glomerulonephritis. These lesions are diagnosed by finding proteinuria with microscopic haematuria and casts. The main differential diagnosis and the most difficult to make is ATN. A history of shock, increased urine sodium and granular casts indicate ATN, however all these findings can also be present in HRS. Clinical features Many features are associated with an increased risk for HRS including marked sodium (<5 mmol/L) and water retention (hyponatraemia), low mean arterial blood pressure (<80 mmHg) and marked elevation of the RAAS [121], all indicative of a worsening haemodynamic status. A lower cardiac output (<6 L/min) (in the setting of severe arterial vasodilatation) has also been identified as an independent predictor of HRS [125]. Patients with HRS characteristically have advanced liver disease (median Child–Pugh score 11.2), difficult to control ascites, a low mean arterial pressure and hyponatraemia [120]. Hyperkalaemia is unusual. Death is due to liver failure; survival depends on the reversibility of the liver disease. Prevention The risk of HRS syndrome is reduced by careful use and monitoring of diuretic therapy, and the early recognition of any complication such as electrolyte imbalance, haemorrhage or infection. Nephrotoxic drugs should be avoided. The risk of renal deterioration after large volume paracentesis is reduced by the administration of salt-poor albumin. The risk of further worsening renal failure in patients with SBP is prevented by intravenous albumin and concomitant antibiotics [62]. The risk of SBP and HRS in high-risk patients without a prior episode of SBP is reduced by prophylactic antibiotics [76]. Treatment Differential diagnosis Prerenal azotaemia (or volume-responsive acute kidney injury). In a patient with cirrhosis this must be differentiated from HRS as the management and prognosis are different (Table 10.11). Causes include over-diuresis and severe diarrhoea, for example due to lactulose. Bacterial infection, particularly SBP, may present with reversible impairment of renal function. Non-steroidal antiinflammatory drugs reduce renal prostaglandin production, thereby reducing the glomerular filtration rate and free water clearance. Intrinsic renal failure. Nephrotoxic drugs should be identified, including aminoglycosides and X-ray contrast media. Glomerular mesangial IgA deposits, accompanied by complement deposition, complicate cirrhosis, General measures Since renal dysfunction may be related to hypovolaemia and since assessment of volume status may be uncertain, diuretics are stopped and intravascular volume is assessed by measuring central venous pressure (CVP). A normal or increased CVP indicates that the cause of renal failure is not volume-related, but this must be interpreted in relation to diaphragmatic pressure secondary to ascites. Intravascular volume should be expanded with intravenous albumin at a dose of 1 g/kg body weight up to a maximum of 100 g [122]. This dose can be repeated in 12 hours if the serum creatinine has not normalized, provided that the CVP is less than 10 mmHg. A reduction in serum creatinine indicates that acute kidney injury is due to prerenal azotaemia. Ascites 227 Intravenous albumin is preferred over saline solution as a volume expander. Potentially nephrotoxic drugs, diuretics and vasodilators are stopped. A search for sepsis is made. Ascites is tapped for white cell count, Gram stain and culture. Blood, urine and cannula tips are cultured. A broadspectrum antibiotic is started if infection is suspected. Renal replacement therapy (mainly continuous arteriovenous and venovenous haemofiltration) should be started if there is severe volume overload, acidosis or hyperkalaemia. However, it does not lead to renal recovery, unless liver transplantation occurs. Complications occur, including arterial hypotension, coagulopathy, sepsis and gastrointestinal haemorrhage, and many patients die during this treatment. Suitability for liver transplantation needs to be rapidly evaluated as this is the only curative therapy for HRS. New therapeutic pharmacological approaches may act as a bridge to liver transplantation by lengthening survival time. Liver transplantation Liver transplantation is the only definitive therapy for HRS, and the only therapy that results in improved survival. However, it is important to try to reverse HRS prior to transplantation because lower pretransplantation serum creatinine is associated with improved posttransplantation outcomes [128,129]. Patients with HRS have longer stays in intensive care units (21 vs. 4.5 days) and haemodialysis is required more often post-transplant (35 vs. 5%). Since calcineurin inhibitors may con- tribute to renal deterioration, it has been suggested that azathioprine and steroids or interleukin 2 receptor blockers, be given until a diuresis has started—usually by 48–72 hours [130]. In patients with type 2 HRS, liver transplantation results in return of acceptable renal function in 90%, and the overall survival rates are similar to those without HRS [130]. Pharmacological treatment [120] Vasodilators. These have been used in an attempt to reverse renal vasoconstriction. Dopamine at renal support doses has a renal vasodilatory effect, however it has no effect in HRS [131]. Prostaglandin administration is not associated with significant improvement in renal function. Vasoconstrictors (Table 10.12). The rationale for use of these agents is to reverse the intense splanchnic and systemic vasodilatation. Administration of vasoconstrictors (ornipressin, terlipressin, octreotide with midodrine, noradrenaline) for periods greater than 3 days is associated with significant increases in mean arterial pressure, decreased serum creatinine and plasma renin activity as well as an increase in serum sodium [131–134]. The best evidence supports the use of terlipressin, a synthetic analogue of vasopressin. It has intrinsic vasoconstrictor effects and in vivo slow conversion to vasopressin, with a longer biological half-life. It has fewer side effects than ornipressin. Terlipressin is more effective than control therapy in randomized controlled trials Table 10.12. Vasoconstrictors in HRS: doses used and adverse events Drug Dose range Observed adverse events Terlipressin 0.5–2.0 mg i.v. every 4–6 h Cardiac: arrhythmia, angina, myocardial infarction GI: abdominal cramps, diarrhoea, nausea, vomiting, intestinal ischaemia Peripheral: livedo reticularis, finger ischaemia, cutaneous necrosis at the infusion site, scrotal necrosis Others: arterial hypertension, dyspnoea, bronchospasm, respiratory acidosis Vasopressin 0.01–0.8 U/min (continuous intravenous infusion) None reported although expectedly same as for terlipressin Noradrenaline 0.5–3.0 mg/h (continuous i.v. infusion) Chest pain with or without ventricular hypokinesia Octreotide + midodrine 100–200 μg subcutaneously three times a day 7.5–12.5 mg orally three times a day Diarrhoea Tingling Goosebumps 25 μg → 25 μg/h (continuous intravenous infusion) 2.5 mg/day orally i.v., intravenous; GI, gastrointestinal. 228 Chapter 10 [135–138], the largest being a double-blind, placebocontrolled trial [138]. Meta-analysis of these studies shows that vasoconstrictors are associated with significantly higher HRS-1 reversal rates compared to controls (46% vs. 11%) and a decreased risk of death, although mortality is still very high in patients treated with vasoconstrictors (58 vs. 74% in controls)[139]. Survival is significantly better in terlipressin ‘responders’. Terlipressin should be started at a dose 0.5–1 mg i.v. every 4–6 hours. If there is no early response (>25% decrease in creatinine levels) after 2 days of therapy, the dose can be doubled every 2 days up to a maximum of 12 mg/day (i.e. 2 mg i.v. every 4 hours). Treatment can be stopped if serum creatinine does not decrease by at least 50% after 7 days at the highest dose, or if there is no reduction in creatinine after the first 3–4 days. In patients with early response, treatment should be extended until reversal of HRS (decrease in creatinine below 1.5 mg/dL or 130 μmol/L) or for a maximum of 14 days [122]. The dose of vasoconstrictors can be adjusted by monitoring mean arterial blood pressure (an indirect indicator of vasodilatation). Alternative pharmacological approaches have used intravenous noradrenaline infusion [134] with one small randomized trial showing it to be equivalent to terlipressin [140], vasopressin infusion [141] or long-term midrodine (an α-adrenergic agonist) combined with octreotide (an inhibitor of the release of glucagon) and intravenous albumin [142]. Randomized trials for the latter are lacking. Transjugular intrahepatic portosystemic shunt (TIPS) Uncontrolled studies have shown that TIPS may improve renal perfusion and reduce the activity of the RAAS. In a prospective study of 31 non-transplantable patients, approximately 75% had improvement in renal function after TIPS [143]. The 1-year survival was significantly better in type 2 than type 1 patients (70 vs. 20%). This study excluded patients with a Child score above 12, serum bilirubin above 15 mg/dL (250 μmol/L) and severe spontaneous encephalopathy. Sequential treatment with vasoconstrictors and albumin followed by TIPS also resulted long-term success in some patients [144]. TIPS can be considered if HRS recurs after discontinuation of successful vasoconstrictor therapy, with creatinine returning to near normal values, particularly if transplantation is not likely in the near future and the patient has refractory ascites [120]. Extracorporeal albumin dialysis A small randomized trial of the molecular absorbent recirculating system, has shown benefit for patients with type 1 HRS syndrome [145]. This modified dialysis method uses an albumin-containing dialysate. Studies are ongoing to establish whether it has a role in such patients as a bridge to transplantation. Summary New approaches offer hope that HRS syndrome, which previously had a dismal outlook, may be improved or reversed. Once the diagnosis of HRS is suspected, specific treatment with vasoconstrictors and intravenous albumin should be initiated. The best evidence supports the use of terlipressin, which should be started at a dose of 0.5 mg i.v. every 6 hours. Prognosis The prognosis is poor when ascites develops in a patient with cirrhosis. While median survival in patients with compensated cirrhosis is around 9 years [146], once decompensation occurs, median survival decreases to 1.6–1.8 years [146,147]; with ascites, mortality is about 20% per year [148,149]. An analysis of over 200 patients with cirrhosis admitted to hospital for the treatment of ascites showed four variables with independent prognostic value. These were renal water excretion (diuresis after water load), mean arterial pressure, Child–Pugh class and serum creatinine [150]. Except for the Child– Pugh score, which is indicative of a poor liver function, all other parameters indicate a worsened haemodynamic status (that is, a more vasodilated state) and are consistent with other studies that have shown that hyponatraemia and renal dysfunction are predictors of a poor survival in cirrhosis [97,151,152]. Because of the poor prognosis, liver transplantation should be considered in all patients with ascites. Early assessment is needed and a decision taken before the clinical decline associated with refractory ascites or hepatorenal syndrome. References 1 Runyon BA. Ascites. In: Schiff L, Schiff ER, eds. Diseases of the Liver. Philadelphia: Lippincott Company, 1993; pp. 990–1015. 2 Gines P, Quintero E, Arroyo V et al. Compensated cirrhosis: natural history and prognostic factors. Hepatology 1987; 7: 122–128. 3 D’Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis. A systematic review of 118 studies. J. Hepatol. 2006; 44: 217–231. 4 Planas R, Balleste B, Alvarez MA et al. Natural history of decompensated hepatitis C virus-related cirrhosis. A study of 200 patients. J. Hepatol. 2004; 40: 823–830. 5 Morali GA, Sniderman KW, Deitel KM et al. Is sinusoidal portal hypertension a necessary factor for the development of hepatic ascites? J. Hepatol. 1992; 16: 249–250. Ascites 229 6 Casado M, Bosch J, Garcia-Pagan JC et al. Clinical events after transjugular intrahepatic portosystemic shunt: correlation with hemodynamic findings. Gastroenterology 1998; 114: 1296–1303. 7 Schrier RW, Arroyo V, Bernardi M et al. Peripheral arterial vasodilation hypothesis—A proposal for the initiation of renal sodium and water retention in cirrhosis. Hepatology 1988; 8: 1151–1157. 8 Garcia-Tsao G, Groszmann RJ, Fisher RL et al. Portal pressure, presence of gastroesophageal varices and variceal bleeding. Hepatology 1985; 5: 419–424. 9 D’Amico G, Garcia-Tsao G, Cales P et al. Diagnosis of portal hypertension: how and when. In: DeFranchis R, ed. Portal Hypertension III. Proceedings of the Third Baveno International Consensus Workshop on Definitions, Methodology and Therapeutic Strategies. Oxford: Blackwell Science, 2001, p. 36–64. 10 Ripoll C, Groszmann R, Garcia-Tsao G et al. Hepatic venous pressure gradient predicts clinical decompensation in patients with compensated cirrhosis. Gastroenterology 2007; 133: 481–488. 11 Wong F, Liu P, Blendis L. Sodium homeostasis with chronic sodium loading in preascitic cirrhosis. Gut 2001; 49: 847–851. 12 Wiest R, Groszmann RJ. The paradox of nitric oxide in cirrhosis and portal hypertension: Too much, not enough. Hepatology 2002; 35: 478–491. 13 Martin PY, Ohara M, Gines P et al. Nitric oxide synthase (NOS) inhibition for one week improves renal sodium and water excretion in cirrhotic rats with ascites. J. Clin. Invest. 1998; 101: 235–242. 14 Lee FY, Colombato LA, Albillos A et al. N-ω-nitro-Larginine administration corrects peripheral vasodilation and systemic capillary hypotension, and ameliorates plasma volume expansion and sodium retention in portal hypertensive rats. Hepatology 1993; 17: 84–90. 15 Iwakiri Y, Groszmann RJ. The hyperdynamic circulation of chronic liver diseases: from the patient to the molecule. Hepatology 2006; 43: S121–S131. 16 Perez-Ayuso RM, Arroyo V, Planas R et al. Randomized comparative study of efficacy of furosemide versus spironolactone in nonazotemic cirrhosis with ascites. Relationship between the diuretic response and the activity of the renin-aldosterone system. Gastroenterology 1983; 84: 961–968. 17 Wiest R, Das S, Cadelina G et al. Bacterial translocation to lymph nodes of cirrhotic rats stimulates eNOS-derived NO production and impairs mesenteric vascular contractility. J. Clin. Invest. 1999; 104: 1223–1233. 18 Wiest R, Cadelina G, Milstien S et al. Bacterial translocation up-regulates GTP-cyclohydrolase I in mesenteric vasculature of cirrhotic rats. Hepatology 2003; 38: 1508–1515. 19 Gines P, Berl T, Bernardi M et al. Hyponatremia in cirrhosis: from pathogenesis to treatment. Hepatology 1998; 28: 851–863. 20 Arroyo V, Jimenez W. Complications of cirrhosis. II. Renal and circulatory dysfunction. Lights and shadows in an important clinical problem. J. Hepatol. 2000; 32: 157–170. 21 Girgrah N, Liu P, Collier J et al. Haemodynamic, renal sodium handling, and neurohormonal effects of acute administration of low dose losartan, an angiotensin II receptor antagonist, in preascitic cirrhosis. Gut 2000; 46: 114–120. 22 Krag A, Moller S, Henriksen JH et al. Terlipressin improves renal function in patients with cirrhosis and ascites without hepatorenal syndrome. Hepatology 2007; 46: 1863–1871. 23 Gerbes AL, Wernze H, Arendt RM et al. Atrial natriuretic factor and renin-aldosterone in volume regulation of patients with cirrhosis. Hepatology 1989; 9: 417–422. 24 Boyer TD, Zia P, Reynolds TB. Effect of indomethacin and prostaglandin A1 on renal function and plasma renin activity in alcoholic liver disease. Gastroenterology 1979; 77: 215–222. 25 Wong F, Massie D, Hsu P et al. Indomethacin-induced renal dysfunction in patients with well-compensated cirrhosis. Gastroenterology 1993; 104: 869–876. 26 Simel DL, Halvorsen RA Jr, Feussner JR. Quantitating bedside diagnosis: clinical evaluation of ascites. J. Gen. Intern. Med. 1988; 3: 423–428. 27 Khalid SK, Garcia-Tsao G. Ascites: Clinical features, diagnosis and natural history. In: Sanyal AJ, Shah V, ed. Portal Hypertension. Pathobiology, Evaluation and Treatment. Totowa: Humana Press, 2005, p. 285–299. 28 Cattau EL Jr, Benjamin SB, Knuff TE et al. The accuracy of the physical examination in the diagnosis of suspected ascites. JAMA 1982; 247: 1164–1166. 29 Cummings S, Papadakis M, Melnick J et al. The predictive value of physical examinations for ascites. West. J. Med. 1985; 142: 633–636. 30 Belghiti J, Durand F. Abdominal wall hernias in the setting of cirrhosis. Semin. Liver Dis. 1997; 17: 219–226. 31 Kirkpatrick S, Schubert T. Umbilical hernia rupture in cirrhotics with ascites. Dig. Dis. Sci. 1988; 33: 762–765. 32 Trotter JF, Suhocki PV. Incarceration of umbilical hernia following transjugular intrahepatic portosystemic shunt for the treatment of ascites. Liver Transpl. Surg. 1999; 5: 209–210. 33 Trianto CK, Kehagias I, Nikolopoulou V, et al. Surgical repair of umbilical hernias. Am. J. Med. Sci. 2010 doi 10.1097/MAJ.0b013e3181f31982. 34 Lieberman FL, Hidemura R, Peters RL et al. Pathogenesis and treatment of hydrothorax complicating cirrhosis with ascites. Ann. Intern. Med. 1966; 64: 341–351. 35 Rubinstein D, McInnes IE, Dudley FJ. Hepatic hydrothorax in the absence of clinical ascites: diagnosis and management. Gastroenterology 1985; 88: 188–191. 36 Strauss RM, Boyer TD. Hepatic hydrothorax. Sem. Liver Dis. 1997; 17: 227–232. 37 Ackerman Z, Reynolds TB. Evaluation of pleural fluid in patients with cirrhosis. J. Clin. Gastroenterol. 1997; 25: 619–622. 38 Bhattacharya A, Mittal BR, Biswas T et al. Radioisotope scintigraphy in the diagnosis of hepatic hydrothorax. J. Gastroenterol. Hepatol. 2001; 16: 317–321. 39 Strauss RM, Martin LG, Kaufman SL et al. Transjugular intrahepatic portal systemic shunt for the management of symptomatic cirrhotic hydrothorax. Am. J. Gastroenterol. 1994; 89: 1522. 40 Runyon BA. Management of adult patients with ascites caused by cirrhosis. Hepatology 1998; 27: 264–272. 41 McVay PA, Toy PT. Lack of increased bleeding after paracentesis and thoracentesis in patients with mild coagulation abnormalities. Transfusion 1991; 31: 164–171. 42 Witte CL, Witte MH. The congested liver. In: Lautt WW, ed. Hepatic Circulation in Health and Disease. New York: Raven Press, 1981, p. 307–323. 230 Chapter 10 43 Henriksen JH, Horn T, Christoffersen P. The blood-lymph barrier in the liver. A review based on morphological and functional concepts of normal and cirrhotic liver. Liver 1984; 4: 221–232. 44 Hoefs JC. Serum protein concentration and portal pressure determine the ascitic fluid protein concentration in patients with chronic liver disease. J. Lab. Clin. Med. 1983; 102: 260–273. 45 Pare P, Talbot J, Hoefs JC. Serum-ascites albumin concentration gradient: a physiologic approach to the differential diagnosis of ascites. Gastroenterology 1983; 85: 240–244. 46 Rimola A, Garcia-Tsao G, Navasa M et al. Diagnosis, treatment and prophylaxis of spontaneous bacterial peritonitis: a consensus document. J. Hepatol. 2000; 32: 142–153. 47 Van der MS, Dens J, Daenen W et al. Pericardial disease is often not recognised as a cause of chronic severe ascites. J. Hepatol. 2000; 32: 164–169. 48 Runyon BA, Montano AA, Akriviadis EA et al. The serumascites albumin gradient is superior to the exudatetransudate concept in the differential diagnosis of ascites. Ann. Intern. Med. 1992; 117: 215–220. 49 Runyon BA, Hoefs JC, Morgan TR. Ascitic fluid analysis in malignancy-related ascites. Hepatology 1988; 8: 1104–1109. 50 Albillos A, Cuervas-Mons V, Millan I et al. Ascitic fluid polymorphonuclear cell count and serum to ascites albumin gradient in the diagnosis of bacterial peritonitis. Gastroenterology 1990; 98: 134–140. 51 Runyon BA, Akriviadis EA, Keyser AJ. The opacity of portal hypertension-related ascites correlates with the fluid’s triglyceride concentration. Am. J. Clin. Pathol. 1991; 96: 142–143. 52 Rector WG Jr. Spontaneous chylous ascites of cirrhosis. J. Clin. Gastroenterol. 1984; 6: 369–372. 53 Fernandez J, Navasa M, Gomez J et al. Bacterial infections in cirrhosis: epidemiological changes with invasive procedures and norfloxacin prophylaxis. Hepatology 2002; 35: 140–148. 54 Xiol X, Castellvi JM, Guardiola J et al. Spontaneous bacterial empyema in cirrhotic patients: a prospective study. Hepatology 1996; 23: 719–723. 55 Garcia-Tsao G, Lee FY, Barden GE et al. Bacterial translocation to mesenteric lymph nodes is increased in cirrhotic rats with ascites. Gastroenterology 1995; 108: 1835–1841. 56 Homann C, Varming K, Hogasen K et al. Acquired C3 deficiency in patients with alcoholic cirrhosis predisposes to infection and increased mortality. Gut 1997; 40: 544–549. 57 Runyon BA. Patients with deficient ascitic fluid opsonic activity are predisposed to spontaneous bacterial peritonitis. Hepatology 1988; 8: 632–635. 58 Garcia-Tsao G. Spontaneous bacterial peritonitis. Gastro. Clin. North Am. 1992; 21: 257–275. 59 Runyon BA. Monomicrobial nonneutrocytic bacterascites: a variant of spontaneous bacterial peritonitis. Hepatology 1990; 12: 710–715. 60 Navasa M, Follo A, Filella X et al. Tumor necrosis factor and interleukin-6 in spontaneous bacterial peritonitis in cirrhosis: relationship with the development of renal impairment and mortality. Hepatology 1998; 27: 1227–1232. 61 Tito L, Rimola A, Gines P et al. Recurrence of spontaneous bacterial peritonitis in cirrhosis: frequency and predictive factors. Hepatology 1988; 8: 27–31. 62 Sort P, Navasa M, Arroyo V et al. Effect of intravenous albumin on renal impairment and mortality in patients with cirrhosis and spontaneous bacterial peritonitis. N. Engl. J. Med. 1999; 341: 403–409. 63 Toledo C, Salmeron JM, Rimola A et al. Spontaneous bacterial peritonitis in cirrhosis: predictive factors of infection resolution and survival in patients treated with cefotaxime. Hepatology 1993; 17: 251–257. 64 Bert F, Panhard X, Johnson J et al. Genetic background of Escherichia coli isolates from patients with spontaneous bacterial peritonitis: relationship with host factors and prognosis. Clin. Microbiol. Infect. 2008; 14: 1034–1040. 65 Cheong HS, Kang CI, Lee JA et al. Clinical significance and outcome of nosocomial acquisition of spontaneous bacterial peritonitis in patients with liver cirrhosis. Clin. Infect. Dis. 2009; 48: 1230–1236. 66 Navasa M, Follo A, Llovet JM et al. Randomized, comparative study of oral ofloxacin versus intravenous cefotaxime in spontaneous bacterial peritonitis. Gastroenterology 1996; 111: 1011–1017. 67 Rimola A, Salmeron JM, Clemente G et al. Two different dosages of cefotaxime in the treatment of spontaneous bacterial peritonitis in cirrhosis: results of a prospective, randomized, multicenter study. Hepatology 1995; 21: 674–679. 68 Runyon BA, McHutchison JG, Antillon MR et al. Shortcourse versus long-course antibiotic treatment of spontaneous bacterial peritonitis. Gastroenterology 1991; 100: 1737–1742. 69 Ricart E, Soriano G, Novella M et al. Amoxicillin-clavulanic acid versus cefotaxime in the therapy of bacterial infections in cirrhotic patients. J. Hepatol. 2000; 32: 596–602. 70 Sigal SH, Stanca CM, Fernandez J et al. Restricted use of albumin for spontaneous bacterial peritonitis. Gut 2007; 56: 597–599. 71 Terg R, Gadano A, Cartier M et al. Serum creatinine and bilirubin predict renal failure and mortality in patients with spontaneous bacterial peritonitis: a retrospective study. Liver Int. 2009; 29: 415–419. 72 Acevedo J, Fernandez J, Castro M et al. Current efficacy of recommended empirical antibiotic therapy in patients with cirrhosis and bacterial infection. J. Hepatol. 2009; 50 (Suppl. 1): S5 (abstract). 73 Umgelter A, Reindl W, Miedaner M et al. Failure of current antibiotic first-line regimens and mortality in hospitalized patients with spontaneous bacterial peritonitis. Infection 2009; 37: 2–8. 74 Fernandez J, Ruiz DA, Gomez C et al. Norfloxacin vs ceftriaxone in the prophylaxis of infections in patients with advanced cirrhosis and hemorrhage. Gastroenterology 2006; 131: 1049–1056. 75 Gines P, Rimola A, Planas R et al. Norfloxacin prevents spontaneous bacterial peritonitis recurrence in cirrhosis: results of a double-blind, placebo-controlled trial. Hepatology 1990; 12: 716–724. 76 Fernandez J, Navasa M, Planas R et al. Primary prophylaxis of spontaneous bacterial peritonitis delays hepatorenal syndrome and improves survival in cirrhosis. Gastroenterology 2007; 133: 818–824. Ascites 231 77 Llach J, Rimola A, Navasa M et al. Incidence and predictive factors of first episode of spontaneous bacterial peritonitis in cirrhosis with ascites: relevance of ascitic fluid protein concentration. Hepatology 1992; 16: 724–727. 78 Runyon BA. Management of adult patients with ascites due to cirrhosis: an update. Hepatology 2009; 49: 2087–2107. 79 Garcia-Tsao G, Lim JK. Management and treatment of patients with cirrhosis and portal hypertension: recommendations from the Department of Veterans Affairs Hepatitis C Resource Center Program and the National Hepatitis C Program. Am. J. Gastroenterol. 2009; 104: 1802–1829. 80 Arroyo V, Gines A, Salo J. A European survey on the treatment of ascites in cirrhosis. J. Hepatol. 1994; 21: 667–672. 81 Gines P, Arroyo V, Quintero E et al. Comparison of paracentesis and diuretics in the treatment of cirrhotics with tense ascites: Results of a randomized study. Gastroenterology 1987; 93: 234–241. 82 Angeli P, Fasolato S, Mazza E et al. Combined versus sequential diuretic treatment of ascites in nonazotemic patients with cirrhosis: results of an open randomized clinical trial. Gut 2010; 59: 98–104 83 Santos J, Planas R, Pardo A et al. Spironolactone alone or in combination with furosemide in the treatment of moderate ascites in nonazotemic cirrhosis. A randomized comparative study of efficacy and safety. J. Hepatol. 2003; 39: 187–192. 84 Pockros PJ, Reynolds TB. Rapid diuresis in patients with ascites from chronic liver disease: the importance of peripheral edema. Gastroenterology 1986; 90: 1827–1833. 85 Gentilini P, Casini-Raggi V, Di Fiore G et al. Albumin improves the response to diuretics in patients with cirrhosis and ascites: results of a randomized, controlled trial. J. Hepatol. 1999; 30: 639–645. 86 Vlachogiannakos J, Tang AKW, Patch D et al. Angiotensin converting enzyme inhibitors and angiotensin II antagonists as therapy in chronic liver disease. Gut 2001; 49: 303–308 87 Corbani A, Manousou P, Calvaruso V et al. Muscle cramps in cirrhosis. The therapeutic value of quinine. Is it underused? Dig. Liver Dis. 2008; 40: 794–799 88 Kao HW, Rakov NE, Savage E et al. The effect of large volume paracentesis on plasma volume—a cause of hypovolemia? Hepatology 1985; 5: 403–407. 89 Tito L, Gines P, Arroyo V et al. Total paracentesis associated with intravenous albumin management of patients with cirrhosis and ascites. Gastroenterology 1990; 98: 146–151. 90 Gines P, Arroyo V, Vargas V et al. Paracentesis with intravenous infusion of albumin as compared with peritoneovenous shunting in cirrhosis with refractory ascites. N. Engl. J. Med. 1991; 325: 829–835. 91 Gines A, Fernandez-Esparrach G, Monescillo A et al. Randomized trial comparing albumin, dextran-70 and polygeline in cirrhotic patients with ascites treated by paracentesis. Gastroenterology 1996; 111: 1002–1010. 92 De Gottardi A, Thevenot T, Spahr L et al. Risk of complications after abdominal paracentesis in cirrhotic patients: a prospective study. Clin. Gastroenterol. Hepatol. 2009; 7: 906–909. 93 Arnold C, Haag K, Blum HE et al. Acute hemoperitoneum after large-volume paracentesis. Gastroenterology 1997; 113: 978–982. 94 Grabau CM, Crago SF, Hoff LK et al. Performance standards for therapeutic abdominal paracentesis. Hepatology 2004; 40: 484–488. 95 Conn HO. Sudden scrotal edema in cirrhosis: a postparacentesis syndrome. Ann. Intern. Med. 1971; 74: 943–945. 96 Gines P, Guevara M. Hyponatremia in cirrhosis: pathogenesis, clinical significance, and management. Hepatology 2008; 48: 1002–1010. 97 Angeli P, Wong F, Watson H et al. Hyponatremia in cirrhosis: Results of a patient population survey. Hepatology 2006; 44: 1535–1542. 98 Planas R, Montoliu S, Balleste B et al. Natural history of patients hospitalized for management of cirrhotic ascites. Clin. Gastroenterol. Hepatol. 2006; 4: 1385–1394. 99 Restuccia T, Gomez-Anson B, Guevara M et al. Effects of dilutional hyponatremia on brain organic osmolytes and water content in patients with cirrhosis. Hepatology 2004; 39: 1613–1622. 100 McCormick PA, Mistry P, Kaye G et al. Intravenous albumin infusion is an effective therapy for hyponatraemia in cirrhotic patients with ascites. Gut 1990; 31: 204–207. 101 Carrilho F, Bosch J, Arroyo V et al. Renal failure associated with demeclocycline in cirrhosis. Ann. Intern. Med. 1977; 87: 195–197. 102 Gadano A, Moreau R, Pessione F et al. Aquaretic effects of niravoline, a kappa-opioid agonist, in patients with cirrhosis. J. Hepatol. 2000; 32: 38–42. 103 Wong F, Blei AT, Blendis LM et al. A vasopressin receptor antagonist (VPA-985) improves serum sodium concentration in patients with hyponatremia: a multicenter, randomized, placebo-controlled trial. Hepatology 2003; 37: 182–191. 104 Gerbes AL, Gulberg V, Gines P et al. Therapy of hyponatremia in cirrhosis with a vasopressin receptor antagonist: a randomized double-blind multicenter trial. Gastroenterology 2003; 124: 933–939. 105 Gines P, Wong F, Watson H et al. Effects of satavaptan, a selective vasopressin V(2) receptor antagonist, on ascites and serum sodium in cirrhosis with hyponatremia: a randomized trial. Hepatology 2008; 48: 204–213. 106 Schrier RW, Gross P, Gheorghiade M et al. Tolvaptan, a selective oral vasopressin V2-receptor antagonist, for hyponatremia. N. Engl. J. Med. 2006; 355: 2099–2112. 107 Heuman DM, Abou-Assi SG, Habib A et al. Persistent ascites and low serum sodium identify patients with cirrhosis and low MELD scores who are at high risk for early death. Hepatology 2004; 40: 802–810. 108 Kim WR, Biggins SW, Kremers WK et al. Hyponatremia and mortality among patients on the liver-transplant waiting list. N. Engl. J. Med. 2008; 359: 1018–1026. 109 Arroyo V, Gines P, Gerbes AL et al. Definition and diagnostic criteria of refractory ascites and hepatorenal syndrome in cirrhosis. Hepatology 1996; 23: 164–176. 110 Moore KP, Wong F, Gines P et al. The management of ascites in cirrhosis: report on the consensus conference of the International Ascites Club. Hepatology 2003; 38: 258–266. 111 Fernandez-Esparrach G, Guevara M, Sort P et al. Diuretic requirements after therapeutic paracentesis in nonazotemic patients with cirrhosis. A randomized doubleblind trial of spironolactone versus placebo. J. Hepatol. 1997; 26: 614–620. 232 Chapter 10 112 Ferral H, Bjarnason H, Wegryn SA et al. Refractory ascites: early experience in treatment with transjugular intrahepatic portosystemic shunt. Radiology 1993; 189: 795–801. 113 D’Amico G, Luca A, Morabito A et al. Uncovered transjugular intrahepatic portosystemic shunt for refractory ascites: a meta-analysis. Gastroenterology 2005; 129: 1282–1293. 114 Albillos A, Banares R, Gonzalez M et al. A meta-analysis of transjugular intrahepatic portosystemic shunt versus paracentesis for refractory ascites. J. Hepatol. 2005; 43: 990–996. 115 Salerno F, Camma C, Enea M et al. Transjugular intrahepatic portosystemic shunt for refractory ascites: a metaanalysis of individual patient data. Gastroenterology 2007; 133: 825–834. 116 Boyer TD, Haskal ZJ. The role of transjugular intrahepatic portosystemic shunt in the management of portal hypertension. Hepatology 2005; 41: 386–400. 117 Bureau C, Garcia-Pagan JC, Otal P et al. Improved clinical outcome using polytetrafluoroethylene-coated stents for TIPS: results of a randomized study. Gastroenterology 2004; 126: 469–475. 118 Gines A, Planas R, Angeli P et al. Treatment of patients with cirrhosis and refractory ascites by LeVeen shunt with titanium tip. Comparison with therapeutic paracentesis. Hepatology 1995; 22: 124–131. 119 Dumortier J, Pianta E, Le Derf Y et al. Peritoneovenous shunt as a bridge to liver transplantation. Am. J. Transplant. 2005; 5: 1886–1892. 120 Garcia-Tsao G, Parikh CR, Viola A. Acute kidney injury in cirrhosis. Hepatology 2008; 48: 2064–2077. 121 Gines A, Escorsell A, Gines P et al. Incidence, predictive factors, and prognosis of the hepatorenal syndrome in cirrhosis with ascites. Gastroenterology 1993; 105: 229–236. 122 Salerno F, Gerbes A, Gines P et al. Diagnosis, prevention and treatment of the hepatorenal syndrome in cirrhosis. A consensus workshop of the international ascites club. Gut 2007; 56: 1310–1318. 123 Mehta RL, Kellum JA, Shah SV et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit. Care 2007; 11: R31. 124 Sanyal AJ, Boyer TD, Garcia-Tsao G et al. A randomized prospective, double-blind, placebo-controlled trial of terlipressin for type 1 hepatorenal syndrome. Gastroenterology 2008; 134: 1360–68 125 Ruiz-del-Arbol L, Monescillo A, Arocena C et al. Circulatory function and hepatorenal syndrome in cirrhosis. Hepatology 2005; 42: 439–447. 126 Moore K, Wendon J, Frazer M et al. Plasma endothelin immunoreactivity in liver disease and the hepatorenal syndrome. N. Engl. J. Med. 1992; 327: 1774–1778. 127 Martin PY, Gines P, Schrier RW. Nitric oxide as a mediator of hemodynamic abnormalities and sodium and water retention in cirrhosis. N. Engl. J. Med. 1998; 339: 533–541. 128 Gonwa TA, McBride MA, Anderson K et al. Continued influence of preoperative renal function on outcome of orthotopic liver transplant (OLTX) in the US: where will MELD lead us? Am. J. Transplant. 2006; 6: 2651–2659. 129 Weismuller TJ, Prokein J, Becker T et al. Prediction of survival after liver transplantation by pre-transplant parameters. Scand. J. Gastroenterol. 2008; 43: 736–746. 130 Gonwa TA, Morris CA, Goldstein RM et al. Long-term survival and renal function following liver transplantation in patients with and without hepatorenal syndrome— experience in 300 patients. Transplantation 1991; 51: 428–430. 131 Angeli P, Volpin R, Piovan D et al. Acute effects of the oral administration of midodrine, an α-adrenergic agonist, on renal hemodynamics and renal function in cirrhotic patients with ascites. Hepatology 1998; 28: 937–943. 132 Lenz K, Hortnagel H, Druml W et al. Ornipressin in the treatment of functional renal failure in decompensated liver cirrhosis. Effects on renal haemodynamics and atrial natriuretic factor. Gastroenterology 1991; 101: 1060–1067. 133 Uriz J, Gines P, Cardenas A et al. Terlipressin plus albumin infusion: an effective and safe therapy of hepatorenal syndrome. J. Hepatol. 2001; 33: 43–48. 134 Duvoux C, Zanditenas D, Hezode C et al. Effects of noradrenalin and albumin in patients with type I hepatorenal syndrome: A pilot study. Hepatology 2002; 36: 374–380. 135 Solanki P, Chawla A, Garg R et al. Beneficial effects of terlipressin in hepatorenal syndrome: a prospective, randomized placebo-controlled clinical trial. J. Gastroenterol. Hepatol. 2003; 18: 152–156. 136 Neri S, Pulvirenti D, Malaguarnera M et al. Terlipressin and albumin in patients with cirrhosis and type I hepatorenal syndrome. Dig. Dis. Sci. 2008; 53: 830–835. 137 Martin-Llahi M, Pepin MN, Guevara M et al. Terlipressin and albumin vs albumin in patients with cirrhosis and hepatorenal syndrome: a randomized study. Gastroenterology 2008; 134: 1352–1359. 138 Sanyal AJ, Boyer T, Garcia-Tsao G et al. A randomized, prospective, double-blind, placebo-controlled trial of terlipressin for type 1 hepatorenal syndrome. Gastroenterology 2008; 134: 1360–1368. 139 Gluud LL, Christensen K, Christensen E et al. Systematic review of randomized trials on vasoconstrictor drugs for hepatorenal syndrome. Hepatology 2009; 50: 1–9 140 Sharma P, Kumar A, Shrama BC et al. An open label, pilot, randomized controlled trial of noradrenaline versus terlipressin in the treatment of type 1 hepatorenal syndrome and predictors of response. Am. J. Gastroenterol. 2008; 103: 1689–1697 141 Kiser TH, Fish DN, Obritsch MD et al. Vasopressin, not octreotide, may be beneficial in the treatment of hepatorenal syndrome: a retrospective study. Nephrol. Dial. Transplant. 2005; 20: 1813–1820. 142 Angeli P, Volpin R, Gerunda G et al. Reversal of type 1 hepatorenal syndrome with the administration of midodrine and octreotide. Hepatology 1999; 29: 1690–1697. 143 Brensing KA, Textor J, Perz J et al. Long-term outcome after transjugular intrahepatic portosystemic stent-shunt in non-transplant cirrhotics with hepatorenal syndrome: a phase II study. Gut 2000; 47: 288–295. 144 Wong F, Pantea L, Sniderman K. Midodrine, octreotide, albumin, and TIPS in selected patients with cirrhosis and type 1 hepatorenal syndrome. Hepatology 2004; 40: 55–64. 145 Mitzner SR, Stange J, Klammt S et al. Improvement of hepatorenal syndrome with extracorporeal albumin dialysis MARS: results of a prospective randomized, controlled clinical trial. Liver Transpl. 2000; 6: 277–286. 146 Gines P, Quintero E, Arroyo V. Compensated cirrhosis: natural history and prognosis. Hepatology 1987; 7: 122–128. Ascites 233 147 D’Amico G, Morabito A, Pagliaro L et al. Survival and prognostic indicators in compensated and decompensated cirrhosis. Dig. Dis. Sci. 1986; 31: 468–475. 148 Salerno F, Borroni G, Moser P et al. Survival and prognostic factors of cirrhotic patients with ascites: a study of 134 outpatients. Am. J. Gastroenterol. 1993; 88: 514–519. 149 D’Amico G. Natural history of compensated cirrhosis and varices. In: Boyer TD, Groszmann RJ. Complications of Cirrhosis: Pathogenesis, Consequences and Therapy. American Association for the Study of Liver Diseases, 2001, p. 118–123. 150 Fernandez-Esparrach G, Sanchez-Fueyo A, Gines P et al. A prognostic model for predicting survival in cirrhosis with ascites. J. Hepatol. 2001; 34: 46–52. 151 Arroyo V, Rodes J, Gutierrez Lizarraga MA et al. Prognostic value of spontaneous hyponatremia in cirrhosis with ascites. Am. J. Dig. Dis. 1976; 21: 249–256. 152 Llach J, Gines P, Arroyo V et al. Prognostic value of arterial pressure, endogenous vasoactive systems, and renal function in cirrhotic patients admitted to the hospital for the treatment of ascites. Gastroenterology 1988; 94: 482–487.
![phillip-s-ge-treatment-of-patients-with-cirrhosis-2016[1]](http://s2.studylib.es/store/data/009477725_1-9ab59afcf7a46383597afd8f78b6747f-300x300.png)