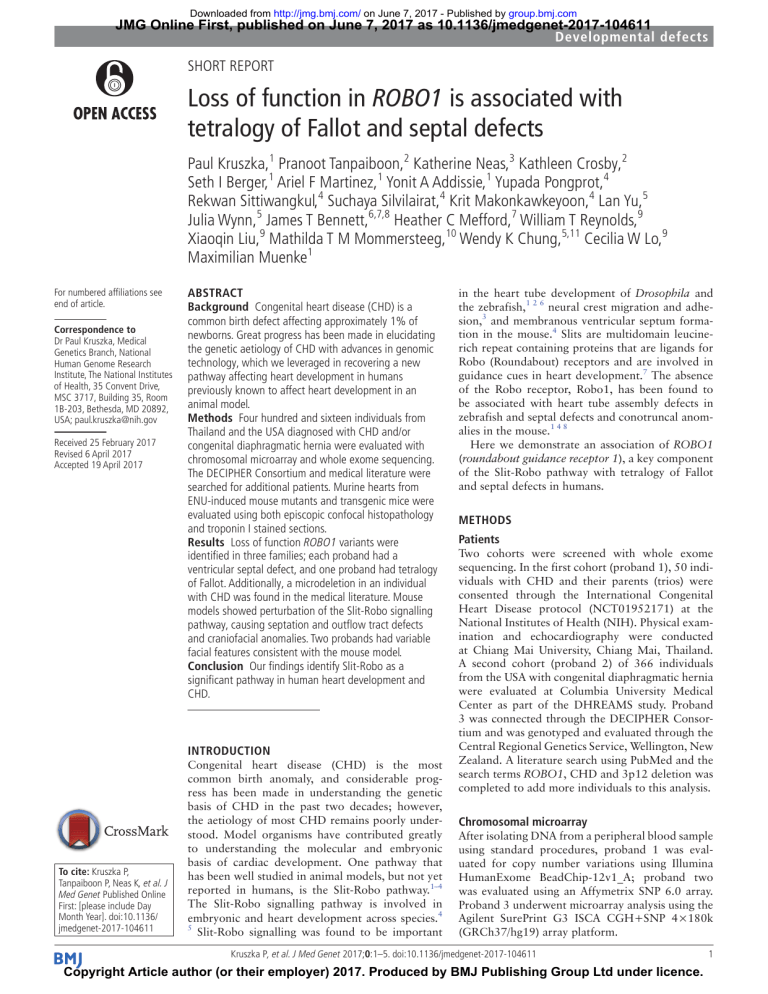
Downloaded from http://jmg.bmj.com/ on June 7, 2017 - Published by group.bmj.com JMG Online First, published on June 7, 2017 as 10.1136/jmedgenet-2017-104611 Developmental defects Short Report Loss of function in ROBO1 is associated with tetralogy of Fallot and septal defects Paul Kruszka,1 Pranoot Tanpaiboon,2 Katherine Neas,3 Kathleen Crosby,2 Seth I Berger,1 Ariel F Martinez,1 Yonit A Addissie,1 Yupada Pongprot,4 Rekwan Sittiwangkul,4 Suchaya Silvilairat,4 Krit Makonkawkeyoon,4 Lan Yu,5 Julia Wynn,5 James T Bennett,6,7,8 Heather C Mefford,7 William T Reynolds,9 Xiaoqin Liu,9 Mathilda T M Mommersteeg,10 Wendy K Chung,5,11 Cecilia W Lo,9 Maximilian Muenke1 For numbered affiliations see end of article. Correspondence to Dr Paul Kruszka, Medical Genetics Branch, National Human Genome Research Institute, The National Institutes of Health, 35 Convent Drive, MSC 3717, Building 35, Room 1B-203, Bethesda, MD 20892, USA; p aul.kruszka@n ih.gov Received 25 February 2017 Revised 6 April 2017 Accepted 19 April 2017 Abstract Background Congenital heart disease (CHD) is a common birth defect affecting approximately 1% of newborns. Great progress has been made in elucidating the genetic aetiology of CHD with advances in genomic technology, which we leveraged in recovering a new pathway affecting heart development in humans previously known to affect heart development in an animal model. Methods Four hundred and sixteen individuals from Thailand and the USA diagnosed with CHD and/or congenital diaphragmatic hernia were evaluated with chromosomal microarray and whole exome sequencing. The DECIPHER Consortium and medical literature were searched for additional patients. Murine hearts from ENU-induced mouse mutants and transgenic mice were evaluated using both episcopic confocal histopathology and troponin I stained sections. Results Loss of function ROBO1 variants were identified in three families; each proband had a ventricular septal defect, and one proband had tetralogy of Fallot. Additionally, a microdeletion in an individual with CHD was found in the medical literature. Mouse models showed perturbation of the Slit-Robo signalling pathway, causing septation and outflow tract defects and craniofacial anomalies. Two probands had variable facial features consistent with the mouse model. Conclusion Our findings identify Slit-Robo as a significant pathway in human heart development and CHD. Introduction To cite: Kruszka P, Tanpaiboon P, Neas K, et al. J Med Genet Published Online First: [please include Day Month Year]. doi:10.1136/ jmedgenet-2017-104611 Congenital heart disease (CHD) is the most common birth anomaly, and considerable progress has been made in understanding the genetic basis of CHD in the past two decades; however, the aetiology of most CHD remains poorly understood. Model organisms have contributed greatly to understanding the molecular and embryonic basis of cardiac development. One pathway that has been well studied in animal models, but not yet reported in humans, is the Slit-Robo pathway.1–4 The Slit-Robo signalling pathway is involved in embryonic and heart development across species.4 5 Slit-Robo signalling was found to be important in the heart tube development of Drosophila and the zebrafish,1 2 6 neural crest migration and adhesion,3 and membranous ventricular septum formation in the mouse.4 Slits are multidomain leucinerich repeat containing proteins that are ligands for Robo (Roundabout) receptors and are involved in guidance cues in heart development.7 The absence of the Robo receptor, Robo1, has been found to be associated with heart tube assembly defects in zebrafish and septal defects and conotruncal anomalies in the mouse.1 4 8 Here we demonstrate an association of ROBO1 (roundabout guidance receptor 1), a key component of the Slit-Robo pathway with tetralogy of Fallot and septal defects in humans. Methods Patients Two cohorts were screened with whole exome sequencing. In the first cohort (proband 1), 50 individuals with CHD and their parents (trios) were consented through the International Congenital Heart Disease protocol (NCT01952171) at the National Institutes of Health (NIH). Physical examination and echocardiography were conducted at Chiang Mai University, Chiang Mai, Thailand. A second cohort (proband 2) of 366 individuals from the USA with congenital diaphragmatic hernia were evaluated at Columbia University Medical Center as part of the DHREAMS study. Proband 3 was connected through the DECIPHER Consortium and was genotyped and evaluated through the Central Regional Genetics Service, Wellington, New Zealand. A literature search using PubMed and the search terms ROBO1, CHD and 3p12 deletion was completed to add more individuals to this analysis. Chromosomal microarray After isolating DNA from a peripheral blood sample using standard procedures, proband 1 was evaluated for copy number variations using Illumina HumanExome BeadChip-12v1_A; proband two was evaluated using an Affymetrix SNP 6.0 array. Proband 3 underwent microarray analysis using the Agilent SurePrint G3 ISCA CGH+SNP 4×180k (GRCh37/hg19) array platform. Kruszka P, et al. J Med Genet 2017;0:1–5. doi:10.1136/jmedgenet-2017-104611 Copyright Article author (or their employer) 2017. Produced by BMJ Publishing Group Ltd under licence. 1 Downloaded from http://jmg.bmj.com/ on June 7, 2017 - Published by group.bmj.com Developmental defects Sequencing Whole exome sequencing was performed on the Thailand cohort (proband 1) at the NIH Intramural Sequencing Center as previously described.9 Exome findings were confirmed with Sanger sequencing. For the US cohort (proband 2), targeted sequencing on an Illumina HiSeq2500 of all of the coding exons of ROBO1 was performed on 366 subjects with congenital diaphragmatic hernia after library preparation using molecular inversion probes (MIPS).10 Variants were aligned, and rare variants with an allele frequency of <1% were annotated with Annovar. Mouse model Two previously reported mouse models with Robo1 variants associated with CHD are described in this report.3 8 In the first model, mice with ENU-induced mutation were isolated in a screen as previously described.8 The molecular lesion (c.T809T>C, NM_019413) is predicted to convert an isoleucine residue to a threonine at position 270 of the encoded protein (p.I270T). In the second model, transgenic Robo1−/− mice were created using previously described procedures.3 Immunohistochemistry for cardiac troponin I (DAPI) was applied to both Robo1+/+and Robo1−/− mice at E18.5. In situ hybridisation for cardiac troponin I was completed on Robo1−/− mice at E18.5.3 All experimental procedures were performed in accordance with the UK Animals (Scientific Procedures) Act 1986 and institutional guidelines. Results Case descriptions The proband in family 1 is the second male child of unrelated parents of Thai ancestry. There is no family history of CHD or genetic syndromes. He presented with cyanosis and tachypnoea at 1 year of age. Referred to cardiology at 14 months old, physical examination revealed a weight of 9.08 kg (20th centile), height of 82 cm (95th centile), head circumference of 46 cm (40th centile), pulse oximetry of 80% and an echocardiogram showed tetralogy of Fallot. At age 3 years, a cardiac catheterisation showed severe valvular and subvalvular pulmonic stenosis and a left superior vena cava. Surgical correction at 3 years of age, which included ventricular septal Table 1 defect (VSD) closure, infundibulectomy, pulmonary vavulotomy, transanular patch and closure of a secundum atrial septal defect (ASD), resolved the patient’s clinical cyanosis. At age 14 years, he had normal cognition and growth parameters were: weight of 35 kg (less than fifth centile) and a height of 156 cm (15th centile). Exam revealed dolichocephaly, micrognathia, prominent nasal root, normal ear position and rotation, high arched palate and crowded teeth. Proband 2 is an 8-year-old female of Chinese ethnicity conceived via in vitro fertilisation. She was diagnosed with a congenital diaphragmatic hernia and VSD immediately after birth. On the second day of life, the patient had a congenital diaphragmatic hernia repair with a patch. She has had normal development with a full-scale IQ of 107 at age 5 years and no other congenital anomalies or health problems. Proband 3 was ascertained through the DECIPHER Consortium where we found two deletions only encompassing ROBO1; the other deletion was only 80 kb and thought to be benign as it was an intronic deletion. Proband 3 is a 4-month-old male of mixed Greek and Japanese ethnicity, conceived via in vitro fertilisation. A large membranous VSD was diagnosed during newborn period. A microarray demonstrated a 417.75 kb deletion on chromosome 3 spanning 78653579–79071345 (hg19) that encompassed ROBO1. Parental microarray analysis has identified that the deletion is inherited from his normal mother. He had a large membranous VSD (repaired) and has left vocal cord paralysis with mild subglottic stenosis and mild right bronchomalacia. He has subtle ear anomalies, with crumpled helices and uplifted lobes. His development to date (current age 6 months) is normal. In the medical literature, Petek et al reported a male of Bosnian descent with a 15 Mb deletion of six genes (PROK2, GPR27, RYBP, PPP4R2, ROBO1 and GBE1).11 Since publication of this study, eight additional genes have been found to be in this interval (EIF4E3, SHQ1, GXYLT2, EBLN2, PDZRN, CNTN3, ROBO2 and IGSF4D3).12 This individual had a secundum ASD, developmental delay and multiple other congenital anomalies (table 1). Sequencing results In 50 trios with CHD from Thailand and 366 trios from the USA, two were found to have a pathogenic variant in ROBO1 Genotype and phenotype of probands with ROBO1 loss of function variants Patient characteristics Proband 1 Proband 2 Proband 3 Petek et al11 ROBO1 variant c.355C>T, p.(R119*) (NM_002941.3) c.928C>T, p.(R310*) (NM_002941.3) Chr3:78653579–79071345 deletion; 417.75 kb 15 Mb deletion between marker D3S3551 and the centromere; 46,XY,del(3)(p13p11) Inheritance De novo De novo Maternally inherited De novo Allele frequency in ExAC 0 0 41 ASDII CADD score 36 Cardiac phenotype ToF VSD VSD Current age 14 years 8 years 4 months Gender Male Female Male Male Ethnicity Thai Chinese Japanese/Greek Bosnian Cognitive impairment None None Unknown Delayed Non-cardiac phenotype Dolichocephaly, micrognathia, Congenital diaphramatic prominent nasal root, high hernia arch palate, crowding teeth Left vocal cord paresis, minimal Cleft lip, downslanting palpebral fissures, square facial dysmorphism fancies with wide forehead, hypoplastic supraorbital ridges, arched eyebrows, short nose, low-set posteriorly angulated ears, short neck, narrow shoulders, mild pectus carinatum,mild rhizomelia and hypospadias ASDII, secundum atrial septal defect; CADD, combined annotation dependent depletion; ExAC, exome aggregation consortium; ToF, tetralogy of Fallot; VSD, ventricular septal defect. 2 Kruszka P, et al. J Med Genet 2017;0:1–5. doi:10.1136/jmedgenet-2017-104611 Downloaded from http://jmg.bmj.com/ on June 7, 2017 - Published by group.bmj.com Developmental defects (proband 1 and proband 2). Proband 1 has a de novo variant in ROBO1, c.355C>T, p.(R119*) (NM_002941.3), identified using whole exome sequencing. An additional de novo missense variant was found in KLHL38 (c.356T>C, p.L119P), a gene not associated with cardiac development or human disease. There were no rare variants in genes previously known to be associated with CHD. Proband 2 has a de novo variant in ROBO1 (c.928C>T, p.(R310*) (NM_002941.3) identified by targeted sequencing of ROBO1. Chromosomal microarrays were normal in both probands 1 and 2, and next-generation sequencing findings were confirmed with Sanger sequencing. In proband 3, a 418 kb deletion (Chr3:78653579–79071345; hg19) on 3p12.2 encompassing exons 4–29 (total of 31 exons; NM_002941). Parental analysis identified this to be inherited from his unaffected mother. Mouse model Mice harbouring an ENU-induced mutation in Robo1 showed both craniofacial and cardiac anomalies (figure 1). The newborn Robo1I270T mutant exhibited shortened snout (figure 1B) with micrognathia (figure 1B) and cleft palate (figure 1D), as compared with that of a normal newborn mouse (figure 1A,C). Heart malformations in the newborn Robo1I270T mutant included double outlet right ventricle (DORV) with perimembranous VSD (figure 1E and see online supplementary video 1), atrioventricular septal defect (figure 1F), muscular VSD (figure 1G),and secundum ASD (figure 1H). The DORV is better visualised in the 3D reconstruction of the heart, showing connection of both the aorta and pulmonary artery to the right ventricle (see online supplementary video 1). In the transgenic Robo1−/− mice (figure 1I–L), perimembranous VSDs can be seen at embryonic day (E)18.5 just before birth.3 Discussion We report three unrelated patients with ROBO1 loss of function variants and cardiac septation and conotruncal defects and review a previously reported case with a 15 Mb deletion that comprised 14 genes including ROBO1. These 14 genes have not been previously associated with CHD, and only ROBO1 has been associated with CHD in the animal model. Interestingly, ROBO2 was included in this deletion and has been found to be expressed in the developing mouse heart; however, Mommersteng et al demonstrated that ROBO2 mutants lack heart defects.3 The two patients with non-sense variants have normal development but several other anomalies including minor facial anomalies in proband one and a congenital diaphragmatic hernia in proband 2. These are the first reported patients in the medical literature with ROBO1 loss of function variants except for large microdeletions encompassing multiple contiguous genes.11 Although the most consistent finding among patients with ROBO1 variants is CHD, proband 1 (table 1) and the patient reported by Petek et al11 (table 1) have craniofacial findings consistent with the ENU-induced Robo1I270T mouse (figure 1B,D). The finding of diaphragmatic hernias in proband 3 suggesting a role for Slit-Robo pathway in development of the diaphragm is supported by the finding of congenital diaphragmatic hernias in mice deficient for Slit3, a ligand of Robo1.13 14 Recovery of more patients with ROBO1 variants are needed to confirm if these patients have syndromic versus isolated CHD. ROBO1, a transmembrane receptor, along with its Slit ligands is part of the Slit-Robo pathway involved in cardiac development. Morpholino (MO) knockdown of robo1 in Kruszka P, et al. J Med Genet 2017;0:1–5. doi:10.1136/jmedgenet-2017-104611 the zebrafish is associated with inhibition of endocardial and myocardial migration resulting in unfused heart fields in early embryogenesis.1 Interestingly, Fish et al found that subphenotypic doses of robo1 and vegfa MOs together in the zebrafish (low doses that cause only subtle effects when injected alone) resulted in delayed heart field fusion, suggesting an in vivo interaction between robo1 and vegfa.1 In both the Robo1 knockout and ENU mutant mouse, membranous ventricular septum and overriding aorta were observed.4 All probands in this study had septal defects, but interestingly, the mouse model exhibited double outlet right ventricle/overriding aorta, phenotypes that are similar to tetralogy of Fallot reported in proband 1.3 Additionally, Robo1 was found to be expressed in Isl1 mouse model second heart field, which is significant, as both second heart field and neural crest defects can cause outflow alignment problems and septal defects.4 Whereas Fish et al reported robo1 was associated with vascular endothelial growth factor (VEGF) signalling pathway, Mommersteeg et al showed a connection of Robo1 with the Notch signalling pathway, with loss of Robo1 associated with decreased expression of Notch1, Notch2 and Hey1.3 Both of these pathways have been associated with CHD. VEFG is known to be important for heart development, and VEGF variants have been associated with tetralogy of Fallot15 and VSD.16 Notch signalling and both NOTCH1 and NOTCH2 have been associated with ToF.17 Heart formation requires the function of multiple pathways including cross-talk between Notch and VEGF,18 and ROBO1 has been shown to be related to both signalling pathways. Like many CHD genes, there may be other factors such as gene–gene and gene–environment factors that affect phenotype, which is seen in the variable presentation in both humans and the two different mouse models described above. ROBO1 loss of function mutations were found in 2 of 416 trios screened in this study compared with 25 loss of function variants found in the ExAC database (approximate 60 000 exomes of presumably healthy individuals).19 Although this is a significant difference in the ratio of loss of function variants in our study compared the ExAC database (p<0.05; Fisher’s exact test), other factors such as genetic modifiers may be involved in the clinical phenotype of CHD. Additionally, although the ExAC cohort is presumed to be relatively healthy, the possibility exists that some of the individuals with loss of function variants had septal defects that were repaired or that closed spontaneously without intervention. In conclusion, we show that variants in ROBO1 are associated with CHD involving septal defects and tetralogy of Fallot. Author affiliations 1 Medical Genetics Branch, National Human Genome Research Institute, The National Institutes of Health, Bethesda, Maryland, USA 2 Division of Genetics and Metabolism, Children’s National Health System, Washington, DC, USA 3 Genetic Health Service New Zealand (Central Hub), Wellington, New Zealand 4 Division of Pediatric Cardiology, Department of Pediatrics, Chiangmai University, Chiang Mai, Thailand 5 Department of Pediatrics, Columbia University Medical Center, New York, New York, USA 6 Center for Integrative Brain Research, Seattle Children’s Research Institute, Seattle, Washington, USA 7 Division of Genetic Medicine, Department of Pediatrics, University of Washington, Seattle, Washington, USA 8 Division of Genetic Medicine, Seattle Children's Hospital, Seattle, Washington, USA 9 Department of Developmental Biology, University of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania, USA 10 Department of Physiology, Anatomy and Genetics, University of Oxford, Oxford, UK 11 Department of Medicine, Columbia University Medical Center, New York, New York, USA 3 Downloaded from http://jmg.bmj.com/ on June 7, 2017 - Published by group.bmj.com Developmental defects Figure 1 Craniofacial (A–D) and cardiac (E–H) defect phenotypes shown with episcopic confocal histopathology in Robo1I270T mutant mouse; (A and C) normal newborn mouse; (B) newborn Robo1I270T mutant exhibited shortened snout (delineated by black line) with micrognathia (see arrowheads). (D) Newborn Robo1I270T mutant with cleft palate; (E) double outlet right ventricle with perimembranous ventricular septal defect; (F) atrioventricular septal defect; (G) a muscular VSD (arrowhead); and (H) secundum atrial septal defect (arrowhead). (I–L) Troponin I stained sections of transgenic murine heart at E18.5. (I) Wildtype. Arrow shows ventricular septum; asterisk at entrance to aorta; plus sign at pulmonary vein; (J) Robo−/− with arrowhead shows ventricular septal defect; and (K and L) Robo−/− with arrowhead shows ventricular septal defect. Ao, aorta; AVSD, atrioventricular septal defect; CP, cleft palate; DORV, double outlet right ventricle; LA, left atrium; Pa, pulmonary artery; RA, right atrium; VSD, ventricular septal defect. Contributors PK, PT and WKC designed the study. PT, KN, KC, YP, RW, SS, KM and JW collected data. SIB, YAA, LY, HCM, JTB, PK and WKC performed next-generation sequencing. AFM and LY performed Sanger sequencing. MTMM, WTR and CWL conducted animal studies. PK, PT, WKC and MM drafted the manuscript. All authors revised the manuscript. Funding This work was supported by the intramural programme of the National Human Genome Research Institute, National Institutes of Health, the Wellcome Trust 4 and the British Heart Foundation (PG/15/50/31594), the Burroughs Wellcome Fund Career Award for Medical Scientists (JTB), the National Institute of Health grant (HD057036) and by Columbia University's Clinical and Translational Science Award (CTSA), grant (UL1 RR024156) from National Center for Advancing Translational Sciences/National Institutes of Health (NCATS-NCRR/NIH), a grant from CHERUBS, a grant from the National Greek Orthodox Ladies Philoptochos Society, Inc. and generous donations from The Wheeler Foundation, Vanech Family Foundation, Larsen family, Kruszka P, et al. J Med Genet 2017;0:1–5. doi:10.1136/jmedgenet-2017-104611 Downloaded from http://jmg.bmj.com/ on June 7, 2017 - Published by group.bmj.com Developmental defects Wilke family and many other families. Funding was also provided to CWL by the National Institutes of Health (HL098180 and HL132024). This study makes use of data generated by the DECIPHER community. A full list of centres who contributed to the generation of the data is available from and via email from d ecipher@sanger.ac.uk. Competing interests None declared. Patient consent Obtained. Ethics approval National Human Genome Research Institute IRB. Provenance and peer review Not commissioned; externally peer reviewed. Data sharing statement We deposit phenotypic and genomic data including medically significant findings in public databases, ClinVar or dbGAP, consistent with NHGRI datasharing policy. Consent forms for this protocol inform participants of the data sharing plan. © Article author(s) (or their employer(s) unless otherwise stated in the text of the article) 2017. All rights reserved. No commercial use is permitted unless otherwise expressly granted. References 1. Fish JE, Wythe JD, Xiao T, Bruneau BG, Stainier DY, Srivastava D, Woo S. A Slit/ miR-218/Robo regulatory loop is required during heart tube formation in zebrafish. Development 2011;138:1409–19. 2. Medioni C, Astier M, Zmojdzian M, Jagla K, Sémériva M. Genetic control of cell morphogenesis during Drosophila melanogaster cardiac tube formation. J Cell Biol 2008;182:249–61. 3. Mommersteeg MT, Andrews WD, Ypsilanti AR, Zelina P, Yeh ML, Norden J, Kispert A, Chédotal A, Christoffels VM, Parnavelas JG. Slit-roundabout signaling regulates the development of the cardiac systemic venous return and pericardium. Circ Res 2013;112:465–75. 4. Mommersteeg MT, Yeh ML, Parnavelas JG, Andrews WD. Disrupted Slit-Robo signalling results in membranous ventricular septum defects and bicuspid aortic valves. Cardiovasc Res 2015;106:55–66. 5. Qian L, Liu J, Bodmer R. Slit and Robo control cardiac cell polarity and morphogenesis. Curr Biol 2005;15:2271–8. 6. Santiago-Martínez E, Soplop NH, Patel R, Kramer SG. Repulsion by Slit and Roundabout prevents Shotgun/E-cadherin-mediated cell adhesion during Drosophila heart tube lumen formation. J Cell Biol 2008;182:241–8. 7. Morlot C, Thielens NM, Ravelli RB, Hemrika W, Romijn RA, Gros P, Cusack S, McCarthy AA. Structural insights into the Slit-Robo complex. Proc Natl Acad Sci U S A 2007;104:14923–8. 8. Li Y, Klena NT, Gabriel GC, Liu X, Kim AJ, Lemke K, Chen Y, Chatterjee B, Devine W, Damerla RR, Chang C, Yagi H, San Agustin JT, Thahir M, Anderton S, Lawhead C, Vescovi A, Pratt H, Morgan J, Haynes L, Smith CL, Eppig JT, Reinholdt L, Francis R, Leatherbury L, Ganapathiraju MK, Tobita K, Pazour GJ, Lo CW. Global genetic analysis in mice unveils central role for cilia in congenital heart disease. Nature 2015;521:520–4. Kruszka P, et al. J Med Genet 2017;0:1–5. doi:10.1136/jmedgenet-2017-104611 9. Kruszka P, Uwineza A, Mutesa L, Martinez AF, Abe Y, Zackai EH, Ganetzky R, Chung B, Stevenson RE, Adelstein RS, Ma X, Mullikin JC, Hong SK, Muenke M. Limb body wall complex, amniotic band sequence, or new syndrome caused by mutation in IQ Motif containing K (IQCK)? Mol Genet Genomic Med 2015;3:424–32. 10. Boyle EA, O'Roak BJ, Martin BK, Kumar A, Shendure J. MIPgen: optimized modeling and design of molecular inversion probes for targeted resequencing. Bioinformatics 2014;30:2670–2. 11.Petek E, Windpassinger C, Simma B, Mueller T, Wagner K, Kroisel PM. Molecular characterisation of a 15 Mb constitutional de novo interstitial deletion of chromosome 3p in a boy with developmental delay and congenital anomalies. J Hum Genet 2003;48:283–7. 12. UCSC Genome Browser. http://genome.ucsc.edu/ (accessed apr 2017). 13. Liu J, Zhang L, Wang D, Shen H, Jiang M, Mei P, Hayden PS, JSedor JR, Hu H. Congenital diaphragmatic hernia, kidney agenesis and cardiac defects associated with Slit3-deficiency in mice. Mech Dev 2003;120:1059–70. 14. Yuan W, Rao Y, Babiuk RP, Greer JJ, Wu JY, Ornitz DM. A genetic model for a central (septum transversum) congenital diaphragmatic hernia in mice lacking Slit3. Proc Natl Acad Sci U S A 2003;100:5217–22. 15. Lambrechts D, Devriendt K, Driscoll DA, Goldmuntz E, Gewillig M, Vlietinck R, Collen D, Carmeliet P. Low expression VEGF haplotype increases the risk for tetralogy of Fallot: a family based association study. J Med Genet 2005;42:519–22. 16. Xie J, Yi L, Xu ZF, Mo XM, Hu YL, Wang DJ, Ren HZ, Han B, Wang Y, Yang C, Zhao YL, Shi DQ, Jiang YZ, Shen L, Qiao D, Chen SL, Yu BJ, Zf X, Xm M, Yl H, Bj Y. VEGF C-634G polymorphism is associated with protection from isolated ventricular septal defect: case-control and TDT studies. Eur J Hum Genet 2007;15:1246–51. 17.Pierpont ME, Basson CT, Benson DW, Gelb BD, Giglia TM, Goldmuntz E, McGee G, Sable CA, Srivastava D, Webb CL. Genetic basis for congenital heart defects: current knowledge: a scientific statement from the American Heart Association Congenital Cardiac Defects Committee, Council on Cardiovascular Disease in the Young: endorsed by the American Academy of Pediatrics. Circulation 2007;115:3015–38. 18.Holderfield MT, Hughes CC. Crosstalk between vascular endothelial growth factor, notch, and transforming growth factor-beta in vascular morphogenesis. Circ Res 2008;102:637–52. 19. Lek M, Karczewski KJ, Minikel EV, Samocha KE, Banks E, Fennell T, O'Donnell-Luria AH, Ware JS, Hill AJ, Cummings BB, Tukiainen T, Birnbaum DP, Kosmicki JA, Duncan LE, Estrada K, Zhao F, Zou J, Pierce-Hoffman E, Berghout J, Cooper DN, Deflaux N, DePristo M, Do R, Flannick J, Fromer M, Gauthier L, Goldstein J, Gupta N, Howrigan D, Kiezun A, Kurki MI, Moonshine AL, Natarajan P, Orozco L, Peloso GM, Poplin R, Rivas MA, Ruano-Rubio V, Rose SA, Ruderfer DM, Shakir K, Stenson PD, Stevens C, Thomas BP, Tiao G, Tusie-Luna MT, Weisburd B, Won HH, Yu D, Altshuler DM, Ardissino D, Boehnke M, Danesh J, Donnelly S, Elosua R, Florez JC, Gabriel SB, Getz G, Glatt SJ, Hultman CM, Kathiresan S, Laakso M, McCarroll S, McCarthy MI, McGovern D, McPherson R, Neale BM, Palotie A, Purcell SM, Saleheen D, Scharf JM, Sklar P, Sullivan PF, Tuomilehto J, Tsuang MT, Watkins HC, Wilson JG, Daly MJ, MacArthur DG. Analysis of protein-coding genetic variation in 60,706 humans. Nature 2016;536:285–91. 5 Downloaded from http://jmg.bmj.com/ on June 7, 2017 - Published by group.bmj.com Loss of function in ROBO1 is associated with tetralogy of Fallot and septal defects Paul Kruszka, Pranoot Tanpaiboon, Katherine Neas, Kathleen Crosby, Seth I Berger, Ariel F Martinez, Yonit A Addissie, Yupada Pongprot, Rekwan Sittiwangkul, Suchaya Silvilairat, Krit Makonkawkeyoon, Lan Yu, Julia Wynn, James T Bennett, Heather C Mefford, William T Reynolds, Xiaoqin Liu, Mathilda T M Mommersteeg, Wendy K Chung, Cecilia W Lo and Maximilian Muenke J Med Genet published online June 7, 2017 Updated information and services can be found at: http://jmg.bmj.com/content/early/2017/06/07/jmedgenet-2017-104611 These include: References This article cites 18 articles, 11 of which you can access for free at: http://jmg.bmj.com/content/early/2017/06/07/jmedgenet-2017-104611 #BIBL Email alerting service Receive free email alerts when new articles cite this article. Sign up in the box at the top right corner of the online article. Notes To request permissions go to: http://group.bmj.com/group/rights-licensing/permissions To order reprints go to: http://journals.bmj.com/cgi/reprintform To subscribe to BMJ go to: http://group.bmj.com/subscribe/