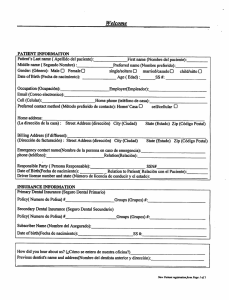
Original Article pISSN 2383-9309❚eISSN 2383-9317 J Dent Anesth Pain Med 2019;19(1):29-36❚https://doi.org/10.17245/jdapm.2019.19.1.29 Comparison of three behavior modification techniques for management of anxious children aged 4-8 years Sreeraksha Radhakrishna, Ila Srinivasan, Jyothsna V Setty, Murali Krishna D R, Anjana Melwani, Kuthpady Manasa Hegde Department of Pediatric and Preventive Dentistry, M.R. Ambedkar Dental College and Hospital, Bengaluru, Karnataka, India Background: An inability to cope with threatening dental stimuli, i.e., sight, sound, and sensation of airotor, manifests as anxiety and behavioral management problems. Behavior modification techniques involving pre-exposure to dental equipment will give children a first-hand experience of their use, sounds, and clinical effects. The aim of this study was to compare the techniques of Tell-Show-Play-doh, a smartphone dentist game, and a conventional Tell-Show-Do method in the behavior modification of anxious children in the dental operatory. Methods: Sixty children in the age group of 4-8 years, with Frankl’s behavior rating score of 2 or 3, requiring Class I and II cavity restorations were divided into three groups. The groups were Group 1: Tell-Show-Play-doh; Group 2: smartphone dentist game; and Group 3: Tell-Show-Do technique and each group comprised of 20 children. Pulse rate, Facial Image Scale (FIS), Frankl’s behavior rating scale, and FLACC (Face, Leg, Activity, Cry, Consolability) behavior scales were used to quantify anxious behavior. Operator compliance was recorded through a validated questionnaire. Results: The results showed lower mean pulse rates, lower FIS and FLACC scores, higher percentage of children with Frankl’s behavior rating score of 4, and better operator compliance in both the Tell-Show-Play-doh and smartphone dentist game groups than in the conventional Tell-Show-Do group. Conclusion: The Tell-Show-Play-doh and smartphone dentist game techniques are effective tools to reduce dental anxiety in pediatric patients. Keywords: Anxiety; Behavior Modification; Game; Pediatric Dentistry; Smartphone. This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. INTRODUCTION ment will dictate the level and amount of information exchange that can take place. Not all children are able to express their fears and anxieties and have relatively The first dental experience is important in molding a limited communication skills at younger ages. It is child's attitude towards dentistry and dental outcomes. difficult for a 5 to 7-year-old child to perceive an idea, Cooperation of a child during dental treatment is vital for which he/she has no conceptual framework and to to render successful and high quality treatment. understand the dentist's frame of reference [1]. Effective communication is important and is a big Child dental anxiety has been a matter of concern for challenge in the dental office. A child's cognitive develop- many years and can be defined as a nonspecific feeling Received: December 14, 2018•Revised: January 18, 2019•Accepted: January 30, 2019 Corresponding Author: Sreeraksha Radhakrishna, Post Graduate Student, Department of Pediatric and Preventive Dentistry, M.R. Ambedkar Dental College and Hospital, Bengaluru, Karnataka, India-560005 Tel: +91-9632522065 E-mail: [email protected] Copyrightⓒ 2019 Journal of Dental Anesthesia and Pain Medicine http://www.jdapm.org 29 Sreeraksha Radhakrishna, et al of apprehension, worry, uneasiness or dread, the source game and conventional Tell-Show-Do techniques in of which may be vague or unknown [2]. The sight, sound, reducing dental anxiety among 4 to 8 -year-old children. and sensation of the airotor is rated as one of the most fear-eliciting stimuli [1]. This inability to cope with MATERIALS AND METHODS threatening dental stimuli often manifests as behavior management problems [1]. Behavior management techniques are a set of proce- This randomized, interventional, clinical study was dures aimed at enhancing a child’s useful coping skills, conducted in the Department of Pediatric and Preventive in order to achieve complete willingness and acceptance Dentistry, M.R Ambedkar Dental College and Hospital of dental care, and ultimately reduce the child’s after obtaining approval from the Institutional Review perception that the dental situation is overwhelming or Board and Ethics Committee (IRB Number: EC-536) and dangerous [3]. written informed consent from the parents and assent The Tell-Show-Do technique is based on the principles from the children, along with a video recording of the of learning theory and is performed by dentists them- same. The study included 60 children, aged 4 to 8 years, selves in the operatory [4,5]. Playing with a dental with equal distribution in both genders. imitation toy and using euphemisms instead of demon- Inclusion criteria: strating on a model or observing one, provides a better 1. Children with Frankl’s behavior rating score of 2 explanatory concept of the dental procedure. or 3 and no prior dental experience With this idea, the Tell-Show-Do technique was 2. Class I or Class II carious lesion on the primary modified into the Tell-Show-Play-doh technique, using molars, limited to enamel and 2/3rd of dentin and the concept of learning by doing, in reducing children's requiring a restoration without local anesthesia fear and anxiety toward dental treatment and promoting Exclusion criteria: adaptive behavior as shown in Fig. 1. Play-doh is a 1. Children with Frankl’s behavior rating score of 1 reusable, flour-based modelling compound used by or 4 children for arts and crafts projects. The Play-Doh Doctor 2. Extensively damaged teeth Drill ’n Fill toy set consists of a plastic human head with 3. Teeth with lesions involving pulp or extending slots into which Play-doh molded teeth can be inserted. below gingiva A battery-operated toy drill is used to drill into and clean 4. Carious teeth with pre-shedding mobility the black, cavitated tooth model and filled with white 5. Medically and developmentally compromising Play-Doh compound to simulate cavity preparation using airotor and restoration using tooth colored cement. conditions 6. Patients with mental / cognitive problems Smartphone dentist games that are available online, Using simple random sampling technique (drawing of approved by a panel of experienced pedodontists for lots), selected children were equally distributed into three clinical usage and demonstrating the use of common groups of 20 each, group 1: Tell-Show-Play-doh, group dental equipment like airotor, ultrasonic scalers, suction 2: smartphone dentist game and group 3: Tell-Show-Do tip, etc. in the form of animated pictures with visual and technique. Samples in each group were treated in a single sound effects were used to give the child a first-hand appointment after using either of the behavior modifi- experience of their usage, sounds produced, and clinical cation techniques. Class I or Class II cavities were prepared effects obtained as shown in Fig. 1. on carious primary molar and restored using Glass Thus, the present study was designed to compare the effectiveness of Tell-Show-Play-doh, smartphone dentist 30 J Dent Anesth Pain Med 2019 February; 19(1): 29-36 ionomer cement. The behavior modification tools used in the study are shown in Fig. 1. Play your worries away! Fig. 1. Play-Doh doctor drill ‘n fill toy set (Group 1) and the smartphone dentist game (Group 2) All children were treated by a single operator in order to avoid bias. Fig. 2. Comparison of mean Facial Image Scale (FIS) scores between three study groups at different time intervals The behavior of the child patient before and after the procedure was assessed using Frankl’s behavior rating scale [6]. The level of dental anxiety of each patient was assessed using a finger pulse oximeter (model number: 6500; Nidek Medical India Pvt. Ltd.) and Facial Image Scale (FIS) [7] at four intervals of the procedure, which were: a) Stage 1: Before the treatment procedure (in waiting/ reception area) b) Stage 2: After using the behavior modification technique, pre-operatively c) Stage 3: During treatment (while using airotor) Fig. 3. Comparison of mean pulse oximeter readings between different time intervals in each study group d) Stage 4: After treatment (completion of treatment) The patient was asked to select the image from the readings between the three study groups at different time FIS that he/she can closely associate with at that moment intervals. A repeated measures ANOVA followed by and the patient’s pulse rate was noted. The operator Bonferroni's post-hoc analysis was used to compare the graded the child’s behavior during the procedure using mean FIS scores and pulse oximeter readings between the FLACC (Face, Leg, Activity, Cry, Consolability) different time intervals in each study group. The chi- behavioral pain assessment scale [8]. The ease of square test was used to compare the distributions of the handling the patient (pre-operatively and during the FLACC scale scores, Frankl’s scale scores, ease of procedure) and the ease of carrying out the procedure by handling patients, and ease of carrying out the procedure the pediatric dentist after using the three behavior at different time intervals between the three study groups. modification techniques was assessed using a validated The level of significance (P-value) was set at P < 0.05. questionnaire on a 5-point Likert scale (1 = Very good, 2 = Good, 3 = Average, 4 = Not bad, 5 = Bad). RESULTS The data collected was tabulated and subjected to the following statistical analyses performed using SPSS statistical software package Version 22.0. A one-way A statistically significant difference between the mean ANOVA followed by Tukey's HSD post-hoc analysis was FIS scores was obtained at Stages 2 and 4 of the dental used to compare the mean FIS scores and pulse oximeter procedure in Group 1 (P = 0.005) and Group 2 (P = 0.01), http://www.jdapm.org 31 Sreeraksha Radhakrishna, et al Fig. 4. Comparison of distributions of Faces Leg Activity Cry Consolabilty (FLACC) scale scores between three study groups Fig. 5. Comparison of distributions of responses on Frankl's behavior rating scale at different time intervals between three study groups Table 1. Comparison of distributions of responses for pediatric dentist questionnaire at different time intervals between three study groups Variables Ease of handling patient during treatment Ease of carrying out treatment Scores Bad Not bad Average Good Very good Bad Not bad Average Good Very good Tell Show Do n % 0 0% 4 20% 1 5% 11 55% 4 20% 0 0% 4 20% 1 5% 11 55% 4 20% n 0 0 0 7 13 0 0 0 6 14 Play doh % 0% 0% 0% 35% 65% 0% 0% 0% 30% 70% App n 0 0 0 9 11 0 0 0 8 12 2 % 0% 0% 0% 45% 55% 0% 0% 0% 40% 60% χ Value P-Value 15.675 0.02* 17.120 0.009* * Statistically Significant indicating a greater reduction of dental anxiety in these the greatest reduction in dental anxiety amongst all the two groups when compared to Group 3. A statistically groups as shown in Fig. 3. significant difference was obtained between Stages 3 and The FLACC scores showed that more patients were 4 of the dental procedure in the Tell-Show-Play-doh group relaxed in the smartphone dentist game and the (P = 0.005), indicating the greatest reduction in dental Tell-Show-Play-doh groups as compared to the Tell- anxiety amongst all the groups as shown in Fig. 2. Show-Do group that was statistically significant (P = There was a significant reduction in mean pulse rate, 0.03), as shown in Fig. 4. after treatment, for both Group 1 (P = 0.002) and Group The Frankl’s scale scores after the dental procedure 2 (P = 0.007) indicating low anxiety levels in these two showed that a greater percentage (85%) of patients groups when compared to Group 3. A statistically exhibited definitely positive behavior (Frankl’s behavior significant difference was obtained between Stages 2 and rating 4) in Groups 1 and 2 when compared to Group 4 of the dental procedure in Group 1 (P < 0.001) and 3 (55%). More patients in the Tell-Show-Play-doh and Group 2 (P < 0.001), indicating a better reduction of smartphone dentist game groups exhibited definitely dental anxiety in these two groups when compared to positive behavior, whereas there were more patients Group 3. A statistically significant difference was (20%) exhibiting negative behavior (Frankl’s behavior obtained between Stages 3 and 4 of the dental procedure rating 2) in the Tell-Show-Do group (P = 0.04), which in the Tell-Show-Play-doh group (P = 0.04), indicating was statistically significant as shown in Fig. 5. 32 J Dent Anesth Pain Med 2019 February; 19(1): 29-36 Play your worries away! It was appreciably easier to handle the patient during in various studies [9,10]. In the present study, the mean treatment and carry out the dental procedure in the FIS scores were lower in both the Tell-Show-Play-doh Tell-Show-Play-doh and smartphone dentist game groups and smartphone dentist game groups indicating low when compared to Tell-Show-Do group with P = 0.02 anxiety levels in these groups when compared to the and P = 0.009 respectively, which was statistically Tell-Show-Do group. significant as shown in Table 1. The FLACC scale is a measurement used to assess pain and behavior in children between the ages of 2 months DISCUSSION and 7 years or in individuals who are unable to communicate their pain. Recent studies have also used the FLACC scale to rate behavior in children during The management of children’s behavior is an integral dental treatment [11-14]. In the present study, a majority component of pediatric dental practice. Behavior modifi- of children in the Tell-Show-Play-doh and smartphone cation techniques are employed by dental practitioners to dentist game groups were relaxed indicating better establish communication, alleviate fear and anxiety, behavior during cavity preparation and restoration, facilitate delivery of quality dental care, build a trusting whereas a majority of children showed moderate pain in relationship between dentist, child, and parent, and the Tell-Show-Do group. promote the child’s positive attitude towards oral The Frankl behavior rating scale is commonly used by healthcare, thus helping them to cope and show researchers to study the child’s behavior toward different willingness to undertake dental treatment procedures [3]. variables [15,16]. In the present study, 85% of children The dentist must have a basic understanding of the in the Tell-Show-Play-doh and smartphone dentist game cognitive development of the child. Based on Piaget’s groups exhibited definitely positive behavior after dental classification, children aged 4-7 years are in the treatment when compared with the Tell-Show-Do group preoperational phase. The development in vocabulary, (55%). attention, and concentration abilities in this period is a In this study it was found that it was notably easier sign of their readiness for social communication. Hence, to carry out the procedure using the Tell-Show-Play-doh this age group is ideal for testing behavior modification and smartphone dentist game techniques than the techniques [1] and the positive impact that it can bring Tell-Show-Do technique. Effective handling of patients about in children. pre-operatively and during the procedure was observed Pulse rate is a direct measure of physiological arousal in the Tell-Show-Play-doh and smartphone dentist game and its increase is attributed to stress during dental techniques when compared with the Tell-Show-Do procedures. In the first dental visit of children, the most technique. The two aforementioned parameters (ease of likely responses to dental stimuli reported would be either carrying out the procedure and ease of handling patients) fear or anxiety. Thus, measuring pulse rate using a finger were previously not found to be noted in literature and pulse oximeter is an objective measure for anxiety levels therefore, were included in the present study. in children. In the present study, there was a reduction This study showed a lower significance of gender on in mean pulse rate, after treatment, for both the behavioral changes, which is in accordance with previous Tell-Show-Play-doh and smartphone dentist game groups studies [17-20]. indicating low anxiety levels in these groups when compared to the Tell-Show-Do group. The Tell-Show-Do technique remains the most commonly used technique in pediatric dentistry and is still The FIS is repeatable, easy to use, quick, reliable and considered the technique with which dentists and parents valid. It has been used to quantify anxiety in children are comfortable and justifies being the method of choice http://www.jdapm.org 33 Sreeraksha Radhakrishna, et al as the backbone of child education and behavior guidance managing the child effectively during dental treatment. during the first dental visit [1,21-23]. They are novel, simple, and effective tools that can result The modification of the Tell-Show-Do to Tell-Show- in improved outcomes related to dental fear and anxiety. Play-doh technique is considerably effective in reducing the pulse rate and improving behavior than the con- AUTHOR ORCIDs ventional Tell-Show-Do technique. The children were Sreeraksha Radhakrishna: introduced to a Play-doh dental model and allowed to https://orcid.org/0000-0002-2385-408X Ila Srinivasan: https://orcid.org/0000-0001-9584-6954 Jyothsna V Setty: https://orcid.org/0000-0001-7346-7849 play with a battery-operated toy drill. They were shown how the suction, airotor, and air‑water syringe felt and worked in a playful way. This served to familiarize them with the dental setup, helped reduce anxiety, built a Murali Krishna D R: https://orcid.org/0000-0002-8189-6667 Anjana Melwani: https://orcid.org/0000-0001-5457-9095 Kuthpady Manasa Hegde: https://orcid.org/0000-0001-7801-1760 bridge for future communication, and helped them prepare for further treatment sessions. Smartphone dentist games educating child patients ACKNOWLEDGEMENTS: The authors would like to thank about the use of common dental equipment like the and acknowledge Dr. Santhosh for helping us with airotor, ultrasonic scalers, suction tip, etc. will help reduce statistical analyses. dental fear or apprehension and give children a first-hand DECLARATION OF INTERESTS: The authors declare no experience of their usage, sounds produced, and clinical financial or competing interests. effects obtained. FUNDING: The authors declare no funding/financial This study was designed to compare the efficiency of support the Tell-Show-Play-doh, smartphone dentist game, and PREVIOUS PRESENTATION IN CONFERENCES: 40th ISPPD the Tell-Show-Do techniques in reducing child anxiety National Conference on 24th October 2018 in Nagpur, during dental treatment. The results of this study showed India that the Tell-Show-Play-doh and smartphone dentist game techniques were more effective than the Tell-Show-Do REFERENCES technique on child anxiety levels and increased cooperative behavior during dental treatment among 4– 8‑year‑old children, which is consistent with previous studies [1,2,16,24,25]. 1. Vishwakarma AP, Bondarde PA, Patil SB, Dodamani AS, Vishwakarma PY, Mujawar SA. Effectiveness of two The advantages of using the Play-Doh dental toy and different behavioral modification techniques among 5– smartphone dentist game are that they are convenient to 7-year-old children: A randomized controlled trial. J Indian use, easily available, child-friendly, playful, and require Soc Pedod Prev Dent 2017; 35: 143-9. no additional virtual reality headgears. 2. Shah HA, Nanjunda Swamy KV, Kulkarni S, Choubey In conclusion, it is the responsibility of pedodontists S. Evaluation of dental anxiety and hemodynamic changes to make dentistry as child-friendly and pain-free as (Sympatho-Adrenal Response) during various dental possible to bring about positive changes in the behavior procedures using smartphone applications v/s traditional of children during dental treatment. behaviour management techniques in pediatric patients. The Play-Doh Doctor Drill ’n Fill toy set and “Dentist Int J Appl Res 2017; 3: 429-33. games for kids” smartphone game simulate various dental 3. Kawia HM, Mbawalla HS, Kahabuka FK. Application of procedures to the child patient and are far superior than behavior management techniques for paediatric dental the Tell-Show-Do technique in reducing anxiety and in patients by Tanzanian dental practitioners. Open Dent J 34 J Dent Anesth Pain Med 2019 February; 19(1): 29-36 Play your worries away! 2015; 9: 455-61. Piana G. Effects of audiovisual distraction in children 4. Wright GZ, Stigers JI. Non-pharmacologic management with special healthcare needs during dental restorations: of children’s behaviors. In: Dentistry for the Child and a randomized crossover clinical trial. Int J Paediatr Dent Adolescent. 9th ed. Edited by Dean JA, Avery DR, 2018; 28: 111-20. McDonald RE. St. Louis, CV Mosby Co. 2011, p 30. 15. Riba H. A review of behavior evaluation scales in pediatric 5. Townsend JA. Behaviour guidance of the paediatric dental dentistry and suggested modification to the Frankl scale. patient. In: Paediatric Dentistry- Infancy through Adole- EC Dental Science 2017; 16: 269-75. scence. 5th ed. Edited by Casa Massimo PS, Fields HW, 16. Patil VH, Vaid K, Gokhale NS, Shah P, Mundada M, McTigue DJ, Nowak AJ. Philadelphia, Elsevier Saunders. Hugar SM. Evaluation of effectiveness of dental apps in 2013, p 358. management of child behaviour: A pilot study. Int J Pedod 6. Frankl SN, Shire FR, Fogels HR. Should the parent remain with the child in the dental operatory? J Dent Child 1962; 29: 150-62. 7. Buchanan H, Niven N. Validation of a Facial Image Scale to assess child dental anxiety. Int J Paediatr Dent 2002; 12: 47-52. 8. Merkel SI, Voepel-Lewis T, Shayevitz JR, Malviya S. The FLACC: a behavioral scale for scoring postoperative pain in young children. Pediatr Nurs 1997; 23: 293-7. 9. Rank RC, Rank MS, Vilela JE, Ogawa WN, Correa MS. Dental anxiety and behavior in young children undergoing different distraction techniques. Pesq Bras Odontoped Clin Integr 2017; 17: 1-11. 10. Abanto J, Vidigal EA, Carvalho TS, Bönecker M. Factors for determining dental anxiety in preschool children with Rehabil 2017; 2: 14-8. 17. Wogelius P, Poulsen S, Toft Sørensen H. Prevalence of dental anxiety and behavior management problems among six to eight years old Danish children. Acta Odontol Scand 2003; 61: 178-83. 18. Hoist A, Crossner CG, Hoist A. Direct ratings of acceptance of dental treatment in Swedish children. Community Dent Oral Epidemiol 1987; 15: 258-63. 19. Corkey B, Freeman R. Predictors of dental anxiety in six-year old children: findings from a pilot study. ASDC J Dent Child 1994; 61: 267-71. 20. Cuthbert MI, Melamed BG. A screening device: children at risk for dental fears and management problems. ASDC J Dent Child 1982; 49: 432-6. 21. Adair SM, Waller JL, Schafer TE, Rockman RA. A survey severe dental caries. Braz Oral Res 2017; 31: e13. of members of the American Academy of Pediatric 11. Melwani AM, Srinivasan I, Setty JV, Pamnani SS, Lalitya Dentistry on their use of behavior management techniques. D. A clinical comparative study between conventional and Pediatr Dent 2004; 26: 159-66. camouflaged syringes to evaluate behavior and anxiety in 22. Sharath A, Rekka P, Muthu MS, Rathna Prabhu V, 6–11-year-old children during local anesthesia administ- Sivakumar N. Children’s behavior pattern and behavior ration- a novel approach. J Dent Anesth Pain Med 2018; management techniques used in a structured postgraduate 18: 35-40. dental program. J Indian Soc Pedod Prev Dent 2009; 27: 12. Geetha Priya PR, Asokan S, John JB, Punithavathy R, 22-6. Karthick K. Comparison of behavioral response to caries 23. Grewal N. Implementation of behavior management removal methods: A randomised controlled cross over trial. techniques: how well accepted they are today. J Indian J Indian Soc Pedod Prev Dent 2014; 32: 48-52. Soc Pedod Prev Dent 2003; 21: 70-4. 13. Mitrakul K, Asvanund Y, Arunakul M, Paka-Akekaphat 24. Meshki R, Alidadi F, Behboudi A, Oliadarani FK. Effects S. Effect of audiovisual eyeglasses during dental treatment of pre-treatment exposure to dental practice using a smart- in 5-8 year-old children. Eur Arch Paediatr Dent 2015; phone dental simulation game on children’s pain and 16: 239-45. anxiety: a preliminary double-blind randomized clinical trial. 14. Bagattoni S, D'alessandro G, Sadotti A, Alkhamis N, J Dent 2018; 15: 250-8. http://www.jdapm.org 35 Sreeraksha Radhakrishna, et al 25. Lee JH, Jung HK, Lee GG, Kim HY, Park SG, Woo SC. Effect of behavioral intervention using smartphone 36 J Dent Anesth Pain Med 2019 February; 19(1): 29-36 application for preoperative anxiety in pediatric patients. Korean J Anesthesiol 2013; 65: 508-18.