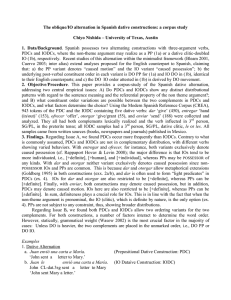
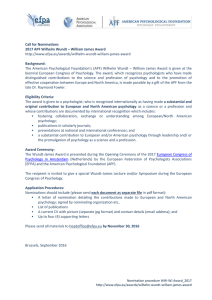
Journal of Consulting and Clinical Psychology 2003, Vol. 71, No. 3, 504 –515 Copyright 2003 by the American Psychological Association, Inc. 0022-006X/03/$12.00 DOI: 10.1037/0022-006X.71.3.504 This document is copyrighted by the American Psychological Association or one of its allied publishers. This article is intended solely for the personal use of the individual user and is not to be disseminated broadly. Treatment of Parental Stress to Enhance Therapeutic Change Among Children Referred for Aggressive and Antisocial Behavior Alan E. Kazdin Moira K. Whitley Yale University School of Medicine Yale University This study evaluated a parent problem-solving (PPS) intervention designed to augment the effects of evidence-based therapy for children referred to treatment for aggressive and antisocial behavior. All children (N ⫽ 127, ages 6 –14 years) and their families received problem-solving skills training (PSST), and parents received parent management training (PMT). Families were randomly assigned to receive or not to receive an additional component (PPS) that addressed parental stress over the course of treatment. Children improved with treatment; the PPS intervention enhanced therapeutic change for children and parents and reduced the barriers that parents experienced during treatment. The implications of the findings for improving evidence-based treatment as well as the limitations of adding components to treatment are detailed. improve and maintain treatment gains over the course of follow-up (e.g., Dadds & McHugh, 1992; Dumas & Wahler, 1983; Kazdin, 1995a; Wahler & Afton, 1980; Webster-Stratton, 1985). Consequently, contextual factors or the processes through which they operate may need to be addressed to optimize the impact of treatment. A dilemma for developing effective treatment is that many of the contextual factors associated with conduct problems come as a “package.” Where ought and can the therapist intervene to attenuate the deleterious impact of these factors on treatment? Stress of the parent may be a reasonable place to begin. Stress has many facets and definitions. In relation to the contextual factors noted previously, it is useful to consider stress as both the events and reactions to them that are disruptive, that alter biological and psychosocial functioning, and that place individuals at risk for untoward mental and physical health outcomes (Miller, 1989). Among families of aggressive and antisocial children, stress of the parent is intertwined with the development and maintenance of aggressive and oppositional child behavior. Stress of the parent influences parent disciplinary practices (e.g., commands to the child, inadvertent or unwitting reinforcement of aversive child behavior, and coercive interchanges) that directly promote and escalate aggressive and oppositional child behavior (e.g., Patterson, Reid, & Dishion, 1992; Sanders, Dadds, & Bor, 1989). More specifically, stress appears to increase parent irritability and attention to deviant behavior and the likelihood that parents initiate or maintain aversive interchanges with their children or counterattack in response to child aggression (e.g., Patterson, 1988; Patterson & Forgatch, 1990; Wahler & Dumas, 1989). On the basis of such findings, including his own set of elegant studies, Patterson (1988) concluded that, “Therapy must help the parents [of aggressive/ antisocial children] cope with their out-of-control children and with their own out-of-control crises at the same time, for crises and antisocial families seem intimately related” (pp. 261–262). The interrelations of stress, discipline practices, and deviant child behavior have yet to be exploited in developing effective treatments. Aggressive and antisocial child behavior includes fighting, theft, vandalism, fire setting, lying, truancy, running away, and other acts that violate social rules and expectations. A persistent pattern of these behaviors, referred to as conduct disorder, is associated with impairment in multiple domains of functioning (e.g., academic performance, sibling and peer relations). The significance of conduct disorder is underscored by its relatively high prevalence rate (e.g., 2%– 6% of the population), the dominance of these behaviors as a basis for clinical referral (33%–50% of the cases of school-age children), and the poor long-term prognosis in relation to mental and physical health outcomes and social adjustment (Kazdin, 1995b; Robins, 1991). This significance is exacerbated by findings that meeting the criteria for a diagnosis of conduct disorder is not a special threshold; children close to but below that cutoff (subsyndromal cases) have poor prognoses and untoward outcomes as well (see Offord et al., 1992). Providing treatment to children and families is a major challenge because aggressive and antisocial child behavior is often embedded in a broader context of parent and family factors that can contribute to and exacerbate deviant child behavior. For example, socioeconomic disadvantage, social isolation, poor living conditions, interpersonal conflict and violence among family members, parent psychopathology, high levels of stress, and lack of social support are often associated with child conduct problems (Maughan, 2001; Stoff, Breiling, & Maser, 1997). These contextual factors influence whether families remain in treatment and, for those who do remain, whether and the extent to which children Alan E. Kazdin, Child Study Center, Yale University School of Medicine; Moira K. Whitley, Child Conduct Clinic, Yale University. Completion of research was facilitated by support from the Leon Lowenstein Foundation, the William T. Grant Foundation Grant 98 –1872–98, and the National Institute of Mental Health Grant MH59029. Correspondence concerning this article should be addressed to Alan E. Kazdin, Child Study Center, Yale University School of Medicine, P.O. Box 207900, New Haven, Connecticut 06520-7900. 504 This document is copyrighted by the American Psychological Association or one of its allied publishers. This article is intended solely for the personal use of the individual user and is not to be disseminated broadly. TREATMENT OF AGGRESSIVE AND ANTISOCIAL CHILDREN The relation of parental stress, parent behavior, and child behavior problems extends well beyond conduct problems of children (Deater-Deckard, 1998). For example, stress and coping of the parents predict subsequent externalizing and internalizing problems among children and adolescents in community samples (Takeuchi, Williams, & Adair, 1991) as well as among special populations, including children with serious medical conditions (e.g., brain injury, diabetes; Holmes, Yu, & Frentz, 1999; Kinsella, Ong, Murtagh, Prior, & Sawyer, 1999) and children who have recently immigrated (e.g., Short & Johnston, 1997). The role of stress in interpersonal interaction also extends beyond the confines of parenting. For example, stress experienced by institutional staff influences staff-client interactions (among clients with developmental disabilities). Greater stress of the staff member is associated with fewer positive staff– client interactions and less caretaking activity (Lawson & O’Brien, 1994; Rose, Jones, & Fletcher, 1998b). Beyond correlational data, researchers have reported that directly intervening to reduce staff stress increases positive staff– client interactions (Rose, Jones, & Fletcher, 1998a). In short, different lines of evidence suggest that stress of a caregiver influences interpersonal interactions in ways that promote deviant behavior. A final reason to consider targeting parental stress might be the role of stress in relation to other contextual factors associated with conduct problems. Stress may be the final common pathway of many contextual influences associated with socioeconomic disadvantage, single-parent family, social isolation, poor living conditions, and conflict with a partner. Also, of the many contextual factors that co-occur among families of aggressive and antisocial children, stress or the perception of stress is malleable, at least in principle. One might be able to provide interventions that alter stress experienced by the parent. Alleviating stress in one’s life or developing coping skills is more feasible within the constraints of providing treatment services than it is in altering socioeconomic disadvantage, poor living conditions, and so on. Although the case can be made for focusing on parental stress as part of the treatment, there are reasons for tempered optimism about the impact such a focus may exert. First, stress is only one of multiple contextual factors that are likely to be present. When evaluated separately, the individual contextual factors often exert a reliable but small role (e.g., effect size) in predicting conduct problems, participation in treatment, or therapeutic change. It is true that the accumulation of the individual factors exerts a much larger influence (Ackerman, Schoff, Levinson, Youngstrom, & Izard, 1999; Deater-Deckard, Dodge, Bates, & Pettit, 1998; Kazdin, 1995a; Kazdin & Wassell, 1999). Yet, this raises the prospect that the focus on any single component such as stress may not necessarily have a palpable influence on treatment. Second, stress as a predictor of either child deviance or therapeutic change may be explained by other influences. For example, socioeconomic status and income often are strongly (and inversely) related to stress experienced by parents (Kazdin, Stolar, & Marciano, 1995; Lindblad-Goldberg, Dukes, & Lasley, 1988; Sanders et al. 1989). If stress is merely a proxy for other variables (e.g., socioeconomic disadvantage), it is unlikely that reducing parental stress would have much impact on treatment outcome. Third, stress experienced by the parent decreases with effective treatment of aggressive and antisocial children, even if parental stress is not focused on directly (Kazdin & Wassell, 2000). That is, 505 as child deviance declines, parent stress decreases. Any further effort to change parental stress beyond the changes that occur anyway might not make a sufficient incremental difference to influence treatment outcome. Stress can be defined and measured in many different ways (e.g., S. Cohen, Kessler, & Gordon, 1997; Miller, 1989). (Indeed, just reading about the options made the authors quite nervous, irritable, pressured, and less able to sleep than usual.) Our work has focused on perceived stress on the part of the parent (i.e., perceptions and the experience that parents report at the outset and over the course of treatment). Perceived stress is readily distinguishable from life events and contributes separately to child outcomes (e.g., Takeuchi et al., 1991). For example, perceived stress at the beginning of treatment influences participation in treatment (e.g., attendance, dropping out prematurely, and child progress) and child treatment outcome (Kazdin & Mazurick, 1994; Kazdin & Wassell, 1999). This effect cannot be explained by other contextual influences (e.g., socioeconomic factors, living conditions, parent psychopathology) or by life events and specific stressors that occur either prior to or over the course of treatment. Noting that perceived stress (or any other variable) predicts treatment outcome and barriers that families experience during therapy does not necessarily mean that this variable is an appropriate target for intervention (Kraemer, Stice, Kazdin, Offord, & Kupfer, 2001). However, research reviewed earlier indicated that stress plays a pivotal role in the day-to-day parenting and deviance of antisocial children, in the behavioral problems of children without identifiable disorders, and in how institutional staff interact with their clients. These findings are promising in suggesting stress may be an appropriate target for treatment (Deater-Deckard, 1998; Patterson, 1988). A strong test of whether parent stress influences outcome is direct intervention to reduce stress and evaluate the outcomes of interest. This study consisted of a randomized controlled trial to evaluate a component of treatment designed to reduce parent stress. Parental stress is related to multiple facets of treatment (e.g., outcome, participation in treatment). Consequently, we predicted that intervening to alter stress would have broad impact and, specifically, would improve treatment outcomes, reduce the extent to which parents experienced barriers in coming to treatment, and improve treatment attendance. Treatment outcome referred to therapeutic change in three areas: child symptoms and functioning, parent psychopathology and stress, and family relations. Although the priority of child treatment is improvement in the problems for which the child was referred, treatment of the child can have positive outcomes on parent and family functioning as well (Kazdin & Wassell, 2000). We have argued that these concomitant outcomes of child therapy may be important in their own right insofar as the changes (e.g., reduced parent depression and stress, improved family relations) are intertwined with child mental health and family quality of life (e.g., Crowley & Kazdin, 1998). Barriers to treatment refer to perceived demands and problems associated with participating in treatment. Parents who perceive barriers during the course of treatment are more likely to cancel and not show up for sessions; also, their children show less therapeutic change (Kazdin, Holland, & Crowley, 1997; Kazdin, Holland, Crowley, & Breton, 1997). Third, treatment attendance consists of canceling and not showing up for treatment, a significant problem in delivering services to children and families (Ka- KAZDIN AND WHITLEY This document is copyrighted by the American Psychological Association or one of its allied publishers. This article is intended solely for the personal use of the individual user and is not to be disseminated broadly. 506 zdin, 1996a). Attendance is likely to be less consistent among parents who are high in stress. Attendance raises service delivery issues (e.g., cost of unused treatment slots when families fail to attend). Also, at some point, checkered or inconsistent treatment attendance is likely to attenuate the benefits of treatment, hence it is a pertinent domain of interest in relation to therapeutic change. We conducted a treatment trial for children and families referred for outpatient treatment of aggressive and antisocial behavior. All children and families in this study received the same evidencebased treatment, as described later. The families differed on whether they received an additional component of treatment designed to address stress of the parent. Consecutive referrals of children were randomly assigned to receive or not to receive this latter intervention. Method Participants Participation was initiated by families who contacted a triage center at a child psychiatry service that serves a large catchment area or who directly contacted the clinic. Children referred for oppositional, aggressive, antisocial behavior were seen at the Yale Child Conduct Clinic, an outpatient treatment service for children and families. After referral, children and families completed an initial evaluation to assess child, parent, and family functioning and then began treatment. Informed consent was solicited and obtained from all families, including the parent(s) or primary caretaker and all children more than 7 years of age. The sample included consecutive children who completed treatment. The study included 127 children (27 girls and 100 boys) and families. Sample size (⬎ 50 participants per group) was greater than usually used in treatment outcome studies because two active (and effective) interventions were compared. Effect sizes for such comparisons tend to be in the small-to-medium range (e.g., .4 –.5) and are not likely to be detected with sample sizes in the usual range (n ⬍ 20 per group; Kazdin & Bass, 1989; Rossi, 1990). The study included only children who completed treatment, given the focus on pre- and posttreatment. This excluded 34.2% of the children who dropped out before completing treatment. This attrition rate is in keeping with the 40%– 60% for child, adolescent, and adult therapy (Kazdin, 1996a). The drop-out rates for the two treatment groups described later were no different, 2(1, N ⫽ 194) ⫽ 1.13, ns. Dropouts, when compared with completers, were slightly older (10.4 vs. 9.8 years old, t[192] ⫽ 2.50, p ⫽ .01), had lower Wechsler Intelligence Scale for Children—Revised (WISC–R; Wechsler, 1974) intelligence quotient (IQ) scores (94.9 vs. 103.3, t[192] ⫽ 3.44, p ⬍ .001), were from lower socioeconomic status (37.7 vs. 40.8 family Hollingshead score, t[192] ⫽ 2.52, p ⫽ .01), and showed more symptoms of conduct disorder on the diagnostic interview (4.4 vs. 3.0). Dropouts and completers were no different in the number of comorbid diagnoses, number of symptoms across all other diagnoses other than conduct disorder or overall severity of symptoms (Child Behavior Checklist; CBCL; Achenbach, 1991), proportion of boys and girls, or subject and demographic variables, with one exception. More dropouts were from minority (African American, Hispanic American, biracial) families than from European American families, 2(1, N ⫽ 194) ⫽ 8.53, p ⬍ .01. Our prior work has suggested minority group differences are accounted for by the association of ethnic identity in this clinic population with lower socioeconomic status (Kazdin et al., 1995). Overall, the characteristics of dropouts and completers are in keeping with other outcome studies with children referred for aggressive and antisocial behavior (Kazdin, 1996a). In separate reports, we have detailed characteristics of dropouts and therapeutic changes they evince (Kazdin, Mazurick, & Siegel, 1994; Kazdin, Holland, & Crowley, 1997). Children ranged in age from 6 to 14 years (M ⫽ 9.8, SD ⫽ 1.8); 88 (69.3%) of the children were European American, 27 (21.3%) were African American, 6 (4.7%) were Hispanic American, 2 (1.6%) were Asian American, and 4 (3.1%) were biracial, based on parent identification of ethnicity. Diagnoses of the children were obtained from the Research Diagnostic Interview (Kazdin, Siegel, & Bass, 1992), a structured interview of the parents that assessed the presence, absence, and duration of child symptoms, based on the Diagnostic and Statistical Manual of Mental Disorders (3rd ed., rev.; DSM–III–R; American Psychiatric Association, 1987). Reliability of Axis I diagnoses was routinely assessed by independent observers for 10%–15% of randomly selected children over the period in which this project was conducted and yielded high agreement ( ⫽ .95 across all diagnoses). Children were included on the basis of referral for aggressive and antisocial behavior as the primary presenting clinical problem. A psychiatric diagnosis of conduct disorder was not required for inclusion because evidence suggests that impairment, the need for treatment, and long-term deleterious outcomes characterize children who fall below the threshold for meeting criteria for the diagnosis (Offord et al., 1992). Principal Axis I diagnoses were conduct disorder (29.9% of the children), oppositional defiant disorder (40.2%), attention– deficit/hyperactivity disorder (3.1%), major depressive disorder (9.4%), other disorders (12.6%), or no diagnosable Axis I disorder (4.7%). Across primary and secondary diagnoses, the most common diagnosis was conduct disorder (42.5% of the children). Most children (77.2%) met criteria for more than one disorder (M ⫽ 2.4 disorders, SD ⫽ 1.2). The most common comorbid diagnoses were conduct disorder with attention– deficit/hyperactivity disorder and oppositional defiant disorder with attention– deficit/hyperactivity disorder (each for 29.9% of the sample). Full-scale WISC–R IQ scores ranged from 56 to 144 (M ⫽ 103.3, SD ⫽ 15.9); 5 of the cases were below an IQ of 70, one of the DSM–IV (4th ed.; American Psychiatric Association, 1994) criteria for mental retardation. (All cases were retained and the findings did not change with or without these cases.) The primary caretakers of the children included biological (90.6%) or adoptive mothers (7.1%) or other relatives (2.4%), who ranged in age from 24 to 55 years (M ⫽ 36.4, SD ⫽ 6.3); 37.0% of the children came from single-parent families. Family occupational and educational level (Hollingshead, 1975) was distributed from lower to higher sociooccupational classes as follows: Class I ⫽ 5.5%, Class II ⫽ 14.2%, Class III ⫽ 25.2%, Class IV ⫽ 37.8%, and Class V ⫽ 17.3%. Median monthly family income was $2,001 to $2,500 (range: $0 –$500 to ⬎ $5,000); 18.1% of the families received social assistance. Assessment Measures were completed before and after treatment and drew on varied assessment formats (interviews, questionnaires, direct observations) and informants (parents and therapists). The therapist responsible for the case administered pretest measures at intake to obtain pertinent background and diagnostic information. At the end of treatment, research assistants rather than the therapists administered posttreatment outcome measures to the parents to avoid inadvertent influences or expectations that the presence of the therapist might promote. Immediately prior to treatment, parents completed a General Information Form to assess participant, demographic, and family characteristics, in addition to the diagnostic interview, mentioned previously. Additional assessments focused on parent stress and the three domains predicted to reflect intervention effects. Perceived parental stress. At the beginning and end of treatment, parents completed the Parenting Stress Index (PSI; Abidin, 1990; Lloyd & Abidin, 1985). The 120 items, each rated on a 5-point scale, reflect multiple areas of stress related to the parents’ views of their own functioning. The measure was selected because it assesses perceived sources of stress, delineates perceived stress from life events, and distinguishes sources of stress from the child (e.g., subscales such as Adaptability, Demandingness, and Child Mood) and sources of stress related to the parent functioning (e.g., subscales such as Restrictions of Role, Social This document is copyrighted by the American Psychological Association or one of its allied publishers. This article is intended solely for the personal use of the individual user and is not to be disseminated broadly. TREATMENT OF AGGRESSIVE AND ANTISOCIAL CHILDREN Isolation, and Relations With Others). The focus of our intervention was primarily on parents’ views of how stress related to their own functioning. However, sources of perceived stress are related. Hence, child, parent, and total perceived stress scores were used in this study. Diverse types of reliability (internal consistency, test–retest) and validity (concurrent, predictive) for the PSI have been reported in the measure references. Treatment outcome. To evaluate treatment outcome, we administered measures before and after treatment. Three outcome domains of interest were changes in the children, parents, and family, each assessed with multiple measures. The measures to represent these domains were based on prior work attesting to their validity, lack of redundancy within a domain, and ability to discriminate among treatments (Kazdin & Wassell, 1999, 2000). Therapeutic changes of the children were evaluated with three measures that focused on child symptoms and dysfunction. First, parents completed the Interview for Antisocial Behavior (IAB; Kazdin & EsveldtDawson, 1986; Kazdin et al., 1992), a semistructured interview that measures multiple overt (e.g., fighting) and covert (e.g., lying) antisocial behaviors of the child. This measure reflects primary symptoms for which children are referred to the clinic. Each of the 30 items is rated on a 5-point scale for severity of dysfunction (1 ⫽ not a problem at all, 5 ⫽ very much a problem) and a 3-point scale for duration (1 ⫽ recent or new problem [ 6 months], 3 ⫽ always). Total antisocial behavior is obtained by summing severity and duration scores, in keeping with scoring of the IAB in studies of the validity of the scale. Internal consistency and construct validity have been supported in studies noted previously. Second, at the beginning of treatment, parents were interviewed to identify oppositional, aggressive, and antisocial child behaviors that occurred at home in the past week. The interview included a list of 23 behaviors that served as a pretreatment index of problems for the Parent Daily Report (PDR; Chamberlain & Reid, 1987). At the end of treatment, parents observed behavior at home for 10 days within a 2–3 week period to assess the daily occurrence of each of the 23 behaviors (i.e., whether each occurred within the past 24 hr). The mean daily total number of behaviors observed by the parent served as the measure of child problems in the home. The PDR shows adequate internal consistency, test–retest reliability, and interrater agreement, and correlates with overt behavior recorded by observers in the home (Foster & Robin, 1997). Finally, to assess a broad range of symptoms, parents completed the CBCL. This measure includes 118 items (each rated on a 0- to 2-point scale) that comprise multiple behavior problems. The total problem score was evaluated to assess severity of dysfunction across a broad range of symptom domains. The measure is especially relevant to the present sample because of the high rates of comorbid disorders and symptoms spanning multiple diagnoses. Various forms of reliability and validity of the CBCL have been studied extensively in clinic and nonclinic samples. Therapeutic changes of the parent were assessed by three measures that focused on parent psychopathology and perceived stress. First, parents completed the Beck Depression Inventory (BDI; Beck, Steer, & Garbin, 1988). For each of 21 items, the parent selected one of three statements that differed in the presence or severity of the symptom. Second, to sample a broader range of symptoms, parents completed the Hopkins Symptom Checklist (SCL-90; Derogatis & Cleary, 1977). The scale included 90 items, rated on a 5-point scale, to reflect the degree of discomfort across several symptom areas. The total score was used as an overall index of psychiatric dysfunction of the parent. The psychometric properties of the BDI and SCL-90 have been studied extensively. Third, parent perceptions of stress were assessed by the PSI. We used the total score from the PSI. (In some analyses, stress on the PSI is evaluated separately from therapeutic change to evaluate whether stress was influenced specifically by the intervention designed to reduce stress.) Therapeutic changes in the family were assessed with three measures that focused on relationships and resources within the family. Two measures were drawn from the Family Environment Scale (FES; Moos & Moos, 1981) completed by the parents. The FES includes 90 items (true– 507 false) that assess quality of interpersonal relationships, support, structure, and functioning of the family. Two second-order factors were used from the scale to assess quality of family relationships (cohesion, expressiveness, conflict) and system maintenance (organization and functioning of the family as a system). The FES has been studied extensively, and diverse types of reliability and validity have been demonstrated. The third measure, completed by the parents, was the Sense of Support Scale (SSS; Aneshensel & Stone, 1982), and it assessed perceived social support. Parents reported how often within the past 2 months they received support in their daily lives (e.g., someone was thoughtful when they were tired, provided emotional support, or helped with problems). Seven items or opportunities to receive support were rated on a 5-point scale (1 ⫽ all of the time, 5 ⫽ never). Total perceived support is based on the sum of all items. The psychometric properties of the SSS have not been extensively evaluated. The scale was selected because it has reflected changes in parents over treatment in our prior research and because of the brevity of the scale in the context of a large assessment battery. Barriers to participation in treatment. Parents often experience barriers that are directly related to participation in treatment and these barriers influence therapeutic change of the child. Parents completed the Barriers to Treatment Participation Scale (BTPS; Kazdin, Holland, & Crowley, 1997; Kazdin, Holland, Crowley, & Breton, 1997).1 The BTPS is an interview that consists of 44 items rated on a 5-point scale (1 ⫽ never a problem, 5 ⫽ very often a problem). The items compose four themes: (a) stressors and obstacles that interfere with participating in and coming to treatment (e.g., conflict with a significant other about treatment, problems with other children that interfered with treatment), (b) treatment demands and issues (e.g., concerns the treatment and the extent to which treatment was confusing, difficult, or demanding), (c) perceived relevance of treatment (e.g., whether treatment was seen as relevant to the child’s problems and met with parent expectations), and (d) relationship with the therapist (e.g., parent’s alliance and bonding with the therapist). Data on the internal consistency, interrater agreement, subscales, and convergent and discriminant validity have been provided in the previously cited references. At the end of treatment, parents and therapists independently completed the BTPS to provide separate sources and perspectives about barriers experienced by the parent. Treatment attendance. Two measures of participation in treatment consisted of canceling sessions and not showing up for treatment. Canceling sessions referred to occurrences when the parents or family member called the clinic in advance of a session to say that they could not attend. An answering machine was always available for those times in which the clinic was closed (after hours, weekends) so that calls could be received at any time. Missed treatments referred to participants not appearing for a session without calling in advance. Canceling and not showing up were coded routinely on a master schedule each day by someone unaware of the study or hypotheses. The number of cancellations and no-shows for a given family are partially confounded by how long a person is in treatment (i.e., greater time in treatment could lead to more missed appointments). Consequently, cancellations and no-shows were divided by the number of weeks in treatment to provide cancel and no-show rates per week. Cancellations and no-shows relate to perceived barriers (i.e., greater barriers are associated with poorer treatment attendance; Kazdin, Holland, Crowley, & Breton, 1997). Treatment Treatment provided to all families. After intake assessment, children and families began treatment. All families received an evidence-based treatment that consisted of the combination of cognitive problem-solving skills training (PSST) provided to the child and parent management train- 1 A copy of the Barriers to Treatment Participation Scale can be obtained from Alan E. Kazdin. This document is copyrighted by the American Psychological Association or one of its allied publishers. This article is intended solely for the personal use of the individual user and is not to be disseminated broadly. 508 KAZDIN AND WHITLEY ing (PMT) provided to the parents (Kazdin, 1996b). Prior research has indicated that PSST and PMT, alone or combined, lead to change and are more effective than waiting-list, no-treatment, and minimal-treatment control conditions and other interventions such as relationship therapy (Brestan & Eyberg, 1998; Kazdin, 2000b; Sheldrick, Kendall, & Heimberg, 2001).2 Although each of these treatments separately produces therapeutic change and qualifies as an evidence-based treatment, the combination tends to be more effective (Kazdin, 1996b; Webster-Stratton & Hammond, 1997). In PSST, children were seen individually for approximately 20 –25 sessions and learned problem-solving skills (e.g., generating alternative solutions, means– ends thinking) to manage interpersonal situations (e.g., with parents, teachers, siblings, and peers). Within the sessions, problemsolving skills were developed through practice, modeling, role-playing, corrective feedback, and social and token reinforcement. Outside of the sessions, the children applied problem-solving steps to interpersonal situations in everyday life. In PMT, parents saw therapists individually for approximately 16 sessions to develop adaptive parenting practices and child–parent interaction patterns and to alter child behavior at home and at school. Practice, feedback, and shaping were used to develop parental skills in the sessions and specific behavior-change programs for use outside of the sessions. Child functioning at school was incorporated into treatment through contact with the teacher and home-based reinforcement programs. Each treatment included a core set of sessions to convey content, themes, and skills. Within the core sessions, child domains of dysfunction at home and at school and special family circumstances (e.g., living conditions, job schedules, custody issues, use of extended family members) were individualized. Occasionally, additional sessions were provided to address specific problems or a theme that was not sufficiently well conveyed in the core session. For each treatment, parents were brought into the child sessions and/or the child was brought into the parent session. The goals of these sessions were to review that part of treatment that was carried out at home and to role-play and practice under supervision (feedback, shaping, praise) of the therapist. Treatment provided to some families. Families were randomly assigned at intake to receive an additional component of treatment referred to as parent problem solving (PPS). Although assignment to conditions was random, a slightly greater percentage of cases was allocated in advance to be assigned to PPS rather than the no-PPS condition (55% vs. 45%). Our pilot work suggested potential gains for the families that received PPS, hence we provided this to slightly more than half of the families, as determined on an a priori basis. Although statistical power is maximized when group size is equal, the small difference in sample sizes for the two groups provided a potentially helpful procedure (PPS) to more families without any palpable loss of power. PPS consisted of five sessions interspersed over the course of treatment, approximately every 2 to 4 weeks. In the initial session, the therapist explained the nature of treatment and conducted an interview about stressors in the parent’s life. These stressors asked the parent to comment on problems at work, finances, marriage and relationships, involvement with social agencies (e.g., family services), extended family, medical issues and conditions, and other areas the parent identified. Also, the interview ended with a focus on what might make life more enjoyable (e.g., more time with a partner, time for oneself). During these sessions the therapist and parent met to develop problem-solving skills in the parent and to focus on using these skills to address stressors of the parent in everyday life. The focus of PPS is on one parent (usually the mother) in two-parent families or the person who has primary care responsibilities for the child.3 (PMT is provided to both parents, as available; PPS is reserved for only one parent.) The rationale for this focus was drawn from prior research on the role stress, isolation, and insularity of the mother or primary caretaker plays in relation to child deviance and untoward parent– child interaction (Patterson, 1988; Wahler, 1980). During the PPS sessions the parent was trained to identify alternative solutions to stressful problems and to select and attempt concrete solutions as part of treatment. For many stressors (e.g., living with HIV, deplorable living conditions, loss of a partner), there may not be “solutions,” hence the focus was on helping the parent develop coping strategies and use resources (e.g., friends, work, activities) to participate in life in ways that the person would see as helping. Each PPS session focused on a single area or theme (e.g., relationship with one’s partner). The themes were devised by reviewing with the parent in the initial session potential sources of stress and having him or her rate severity in a semistructured interview that part of this initial session. Each session, approximately 50 min, comprised three phases. The first phase was information gathering, in which the therapist queried to identify the situation, context, circumstances, and details about the source of stress. The second phase focused on cognitions (attributions, beliefs about the problem) and affect (feelings about different facets of the problem). The goal was to identify the impact of the situation on the parent’s thoughts and feelings. In the third phase, problem solving was approached more concretely either to alter aspects of the situation or to develop coping methods. The parent was encouraged to discuss different solutions or alternatives (problem solve) to address a facet of the problem. Concrete ideas (alternative solutions) were carefully weighed and evaluated (solutions and consequences). Plans (means– ends thinking) were spelled out in very specific terms and structured in a manageable stepwise fashion. During this phase, the therapist used prompts (e.g., modeling, instructions), shaping, and social reinforcement to foster use of a problemsolving approach and to generate concrete, realistic solutions that could be tried. Typically, one to three solutions were selected as a homework assignment and mutually agreed to by the therapist and parent. The parent played the more central role in selecting the solutions to ensure the solutions addressed critical facets about the situation, pertained to how the parent felt and thought about the situation, and were feasible to carry out in light of practical considerations (e.g., demands of parenting or work). Some of the homework assignments required special behaviors or behaviors that the parent may have considered difficult (e.g., asking a partner to care for the children one night, speaking to a relative, or talking to a coworker). Role-play, modeling, and practice were used to help the parent, as needed. The therapist and parent alternated roles in practicing what to say and what reactions might be evident in the other person. Role-playing, shaping, feedback, praise, and practice, central to PMT, were used in the role-play to develop parent behavior as needed in PPS. Execution of the homework assignment was evaluated by phone contacts during the week and reviewed at the beginning of the next session. Themes addressed in PPS were stressors the parent identified as part of assessment at the beginning of treatment. The most common themes were having more time with one’s partner, having more time for oneself, job-related stress, and finances. Major psychopathology (e.g., bipolar disorder, substance abuse) and stressful problems such as marital discord in which marital and legal counseling were required were not treated. The parent was referred for treatment, as was true of all clients at the clinic whether or not they were involved in PPS. Although five PPS sessions were planned, occasionally optional sessions were provided if a homework assignment could not be carried out or if the theme required further immediate attention after a PPS session. 2 Comparison of the different treatments is beyond the scope of this study and has been addressed elsewhere (see Kazdin, 1996b). 3 PPS was piloted for a period of 18 months. As part of this, we attempted to administer the intervention to both parents together. This did not prove to be feasible or productive primarily because venting of marital issues, blaming of child deviance, and comments of one parent often dominated the session. This document is copyrighted by the American Psychological Association or one of its allied publishers. This article is intended solely for the personal use of the individual user and is not to be disseminated broadly. TREATMENT OF AGGRESSIVE AND ANTISOCIAL CHILDREN Therapists and treatment administration. Fifteen clinicians (3 men and 12 women, ages 23–56, all European American) served as therapists. Therapists had a master’s degree (n ⫽ 13) or doctoral degree (n ⫽ 2) from programs in clinical psychology, social work, or another mental healthrelated field. The therapists participated in a 6 –12 month training program to learn the treatments. Training involved extensive role-playing and modeling to master treatment. After initial training, training cases were assigned. These cases were closely supervised using direct observation, review of tapes, and discussion of the case on a session-by-session basis. Throughout the study, treatment sessions continued to be taped for supervision and review. Treatment integrity. To maintain integrity of treatment, we used the following steps: (a) therapists followed a treatment manual that delineated the content and focus of each session; (b) materials were provided to foster correct execution of the treatment, including checklists that prescribed the necessary materials (e.g., charts, games for each session, the specific themes and tasks to be covered) and notes and outlines for use within the sessions; (c) documentation of the session summarized what transpired and how the child or parent progressed; (d) ongoing clinical supervision was provided through direct observation of live treatment sessions with television monitors connected to cameras in the treatment rooms; (e) all treatment sessions were videotaped, and some of them were reviewed weekly to provide feedback to the therapists; and (f) all cases were reviewed weekly to identify the current status of treatment, including what transpired in the previous session, what was planned in the upcoming session, and whether there were any special issues that would influence treatment delivery. These procedures were designed to maintain treatment integrity. No quantitative measure of treatment integrity was obtained in this study. In our program, we have assessed treatment integrity by randomly audiotaping sessions and having naive raters score the extent to which treatmentspecific activities for the sessions were engaged in or completed, including review of the programs or child activity (e.g., for PMT and PSST) in the home, presentation of the new material for that session, practice and role-play of activities, therapist use of praise, and other tasks. The only “lapses” of treatment integrity are not completing all of the tasks because of time constraints (e.g., parent has come in late and the session cannot be 509 completed; review and repair of the program required the entire sessions). These are not lapses, but they serve as a basis for providing optional sessions if a session has not been completed. Results Preliminary Analyses Changes from pre- to posttreatment. The study tested whether PPS influenced therapeutic change, perceived barriers to treatment participation, and treatment attendance. Among these three domains, only therapeutic change included pre- and posttreatment assessment. Preliminary analyses were completed to identify whether children, parents, and families improved over the course of treatment. The means for pre- and posttreatment performance on the child, parent, and family outcome measures are presented in Table 1 for both groups combined. Within-group t tests indicated that children improved over the course of treatment, as reflected by reductions in total antisocial behavior (IAB), specific problem behaviors observed at home (PDR), and total symptoms (CBCL total Behavioral Problems score). Parent and family functioning also improved over the course of treatment as reflected in reductions in parental depression (BDI), a broader range of symptoms (SCL–90), improved relationships and system organization (FES), and social support in the home (SSS). Overall, within-group improvements were evident for both groups in each domain; this is in keeping with prior work on children and families that receive PSST and PMT. Changes in stress. The PPS intervention was intended to reduce parental stress, hence one would expect greater reductions in parenting stress as a function of treatment condition. To evaluate stress, we evaluated measures of the PSI (as noted in Table 1) with a multivariate analysis of variance involving Condition (two dif- Table 1 Measures of Treatment Outcome: Means, Standard Deviations, and Within-Group Changes (t tests) for Treatment Groups Combined Pretreatment Measure Parenting Stress Index (PSI) PSI Parenting subscale PSI Child subscale PSI total Child outcome measures Interview Antisocial Behavior Parent Daily Report CBCL total behavior problems Parent outcome measures Beck Depression Inventory Symptom Checklist-90 Family outcome measures Family Relationships Family System Social Support Posttreatment M SD M SD t(125) 130.17 133.21 263.42 30.46 21.12 45.82 115.19 111.71 227.13 29.87 27.07 52.29 6.60*** 10.72*** 9.69*** 96.25 15.17 68.57 24.82 4.26 9.06 79.68 3.13 60.90 27.28 3.27 9.94 8.36*** 28.53*** 9.89*** 8.18 50.22 6.99 44.70 5.71 34.11 7.15 38.35 5.55*** 6.28*** 6.73 .35 16.89 5.12 2.49 5.80 9.32 1.09 17.83 4.80 2.33 5.45 7.07*** 3.38*** 1.99* Note. Improvements in child and parent measures are based on reduction of scores (e.g., lower symptoms) whereas improvements on family measures reflect an increase in scores (e.g., improved relationships, support). The signs of the t tests for the family measures were reversed so that all tests in the table reflect improvement. CBCL ⫽ Child Behavior Checklist. * p ⱕ .05. *** p ⱕ .001. KAZDIN AND WHITLEY This document is copyrighted by the American Psychological Association or one of its allied publishers. This article is intended solely for the personal use of the individual user and is not to be disseminated broadly. 510 ferent treatments) ⫻ Time (pretreatment, posttreatment). The multivariate effect of primary interest from the analyses is the Condition ⫻ Time interaction that conveys whether groups differed at posttreatment. The results indicated that this effect was not statistically significant, F(3, 123) ⫽ 1.76, ns, Wilks’s ⫽ .96. There was a significant time effect, F(3, 123) ⫽ 39.57, p ⬍ .001, Wilks’s ⫽ .51, and no condition effect, F(3, 123) ⬍ 1.0. The effect of time is in keeping with our prior work, which shows that parent stress decreases over the course of child treatment as the child improves regardless of whether the special parenting stress intervention (PPS) was provided. The focus of the PPS intervention was on parenting stress. If one examines the Parenting subscale of the PSI that more specifically addresses the focus of treatment, the PPS and no-PPS intervention groups differ as predicted. Specifically, the PPS group showed a significantly greater reduction in parenting stress than did the non-PPS group, t(125) ⫽ 2.08, p ⬍ .05. Overall, our primary conclusion from the analyses is that stress changes over the course of treatment. This is the most marked effect in this study and in our prior work. One could argue whether the PPS intervention was shown to lead to greater reduction in stress than the no-PPS condition. Our one t test on a subscale of parenting stress is not persuasive in this regard. Moreover, one wonders whether an interaction effect (Condition ⫻ Time) can be easily shown because of the statistically robust effect due to time. Further analyses of the role of stress and therapeutic change are presented later. Magnitude of therapeutic changes. We were interested in a summary score for child, parent, and family outcomes to provide an overall index of change, to estimate the magnitude of improvements in each domain, to examine the relations of changes across domains, and to test the effects of PPS. A therapeutic index of change was calculated separately for child, parent, and family outcome measures on the basis of combining measures within each domain. For each child, a z change score was derived for each measure (IAB, PDR, CBCL) by subtracting the posttreatment from the pretreatment raw score and dividing by the pretreatment standard deviation. This yielded a z score that reflected how much change was made relative to the pretreatment distribution of scores. This z score placed each outcome measure on the same metric. The mean of these three scores provided an overall z score and a summary index of improvement for the children. A mean z score was also computed for the parent measures and family measures from pre- to posttreatment in the same way. The indices of change for children, parents, and families, as expressed as z scores, are equivalent to effect size (i.e., pre ⫺ posttreatment/standard deviation unit). Small, medium, and large effect size estimates, calculated as .20, .50, and .80 (J. Cohen, 1988), can be used as reference points to evaluate the impact of treatment. For both treatment conditions combined (PPS and no PPS), child, parent, and family mean z scores were 1.36 (95% confidence interval [CI] ⫽ 1.23, 1.49), 0.38 (95% CI ⫽ 0.29, 0.48), and 0.28 (95% CI ⫽ 0.17, 0.38), respectively. The child therapeutic changes correspond to a large effect size; parent and family changes correspond to small-to-medium effect sizes. Impact of PPS The central question guiding the study was whether focusing on PPS and stress would have beneficial effects on three domains: treatment outcome, barriers parents experienced over the course of treatment, and treatment attendance. To compare the two treatment conditions, we completed multivariate analyses (Hotelling’s T2) separately for each domain. Therapeutic outcome for children, parents, and families. A multivariate analysis of child, parent, and family indices of therapeutic change indicated a significant overall effect, T2(3, 122) ⫽ 4.54, p ⬍ .01. Therapeutic change was significantly greater among families that received PPS. In addition to the overall domain, we were interested separately in the child, parent, and family outcomes. Table 2 presents the mean z scores separately for the two treatment groups. For the group that received PPS, child, parent, and family mean z scores were 1.50 (95% CI ⫽ 1.33, 1.68), 0.50 (95% CI ⫽ 0.36, 0.64), and 0.28 (95% CI ⫽ 0.13, 0.44), respectively. For the group that did not receive PPS, child, parent, and family mean z scores were 1.19 (95% CI ⫽ 1.01, 1.37), 0.25 (95% CI ⫽ 0.13, 0.36), and 0.27 (95% CI ⫽ 0.11, 0.42). We were interested in indexes of change for child, parent, and family domains. To evaluate whether treatment conditions differed Table 2 Comparison of Treatments With and Without Parent Problem Solving (PPS) PPS Domain/measures Therapeutic change Child Change Index Parent Change Index Family Change Index Barriers to treatment BTPS (Parent report) BTPS (Therapist report) Treatment attendance Cancelling Not showing up No PPS M SD M SD t(125) Effect size d 1.50 0.50 0.28 0.71 0.56 0.63 1.19 0.25 0.27 0.69 0.43 0.58 2.49*** 2.79*** ⬍1 .45 .50 .02 59.79 61.46 9.44 10.55 63.38 67.62 10.97 13.69 1.94* 2.80** .35 .50 0.24 0.04 0.16 0.01 0.22 0.09 0.21 0.47 ⬍1 ⬍1 .09 .13 Note. BTPS ⫽ Barriers to Treatment Participation Scale. * p ⱕ .05. ** p ⱕ .01. *** p ⱕ .001. This document is copyrighted by the American Psychological Association or one of its allied publishers. This article is intended solely for the personal use of the individual user and is not to be disseminated broadly. TREATMENT OF AGGRESSIVE AND ANTISOCIAL CHILDREN in outcome effects, we conducted multivariate analyses (Condition ⫻ Time) separately for child, parent, and family domains, as these domains and constituent measures are noted in Table 1. The multivariate effect of interest from the analyses is the Condition ⫻ Time interaction, which conveys whether groups differed at posttreatment. Results of the multivariate analyses indicated that at posttreatment, the PPS intervention group showed greater change in child outcome measures, F(3, 114) ⫽ 4.38, p ⬍ .001, Wilks’s ⫽ .91, and parent outcome measures, F(3, 114) ⫽ 3.82, p ⬍ .01, Wilks’s ⫽ .93, but no differences in family outcome measures, F(3, 121) ⫽ 1.26, ns, Wilks’s ⫽ .97. Thus, children whose parents received PPS, compared with those who did not, showed less severe antisocial behavior, fewer problem behaviors at home, and fewer overall symptoms. Similarly, parent outcome of treatment was better for parents who received PPS, as reflected in a greater reduction in parent depression, overall symptoms, and stress. The two treatment conditions indicated no differences on the family outcome domain (t ⬍ 1.0). Other effects from the multivariate analyses indicated no group differences at pretreatment (group effect) and overall changes from pretreatment (time effect) in keeping with other analyses. The analyses of treatment outcome provide partial support for the hypothesis. Children, parents, and families improved over the course of treatment. The gains in child and parent outcome measures were significantly greater among families that received PPS. Overall, the prediction that targeting parental stress with an added treatment component would improve therapeutic change was supported. Supplementary analyses indicated that the effects of PPS did not vary as a function of child age, gender, ethnicity, therapist, or child diagnosis alone or in combination (interaction) with PPS. Also, initial level of parent stress did not influence (moderate) treatment. That is, the effects of PPS were equal among families that varied in initial levels of stress. Barriers to participation in treatment. Parents and therapists independently completed the BTPS to measure barriers to participation in treatment. A multivariate analyses of two measures as a function of treatment condition yielded a significant effect, T2 (2, 117) ⫽ 4.59, p ⬍ .01. Overall, parents who received PPS experienced fewer barriers to participation in treatment than parents who did not receive PPS. The t tests in Table 2 convey that barriers were significantly lower on both the parent-completed and therapist-completed measures. Effect sizes were in the small-tomedium range (d ⫽ .35 and .50, respectively). Treatment attendance. A multivariate analyses of two measures of treatment attendance (rates of cancelled and no-show sessions) as a function of treatment condition yielded no significant overall effect, T2(2, 124) ⬍ 1, ns. We peeked at the univariate tests (but only for a second), which indicated group means for either measure were not different and would not even allow us to use the inappropriate term “approached significance” (please see Table 2). Supplementary Analyses This study was not designed to identify the mechanisms through which the intervention achieved change, a topic to which we return in the Discussion. Even so, further analyses can shed light on possible explanations of the findings. First, the superior effects of PPS might be due to a relatively straightforward interpretation 511 related to the dose of treatment. Families that received PPS received approximately five more sessions of treatment. Perhaps duration of treatment and additional therapy time with families would explain why PPS families fared better in treatment. Extra sessions might provide benefits because of more social support provided by the therapist or by spreading PMT out over a longer period. However, amount of time in treatment was not consistently related to therapeutic change among children, parents, and families, as reflected in correlations of .20 ( p ⬍ .05), .04 (ns), and .01 (ns), respectively. In short, more treatment is not a highly plausible explanation of the present results. Second, parent stress served as the guiding construct and focus of PPS. Is change in stress on the part of the parent a plausible explanation for the benefits of that intervention? (Actually, we were hoping the reader would not ask this.) Testing this requires assessment of processes and proposed mediators during the course of treatment, which was not part of the design of this study (Kazdin, 2003). Also, our prior work has shown that parental stress decreases markedly as the child improves in treatment, even without focusing on parent stress during treatment. With such a strong effect, an additional effort to demonstrate changes in stress specific to the PPS group and changes in stress in relation to outcome domains would have methodological (assessment, power) constraints. Mentioned previously was the finding that the PPS group showed significantly greater reductions in parenting stress (PSI subscale) over the course of treatment than the no-PPS group. The correlations between reductions in parenting stress and improvements in treatment for child, parent, and family (n ⫽ 69) indices of change were .12 (ns), .31 ( p ⬍ .01), and .32 ( p ⬍ .01), respectively. A more direct test of the possibility that stress reduction accounts for the changes can be achieved with procedures described by Holmbeck (2002). The procedures allow for post hoc probing of significant mediational effects, including direct and indirect effects and whether the mediator effect meets criterion for statistical significance. Using these techniques, we did not show that parenting stress met criteria for a mediational effect in relation to child, parent, or family therapeutic change. The results do not support stress as a mediator of the benefits of the PPS treatment. Discussion In this study, all children received PSST and all parents received PMT. Improvements were evident among children, parents, and families whether or not they received the added component of PPS. For families who also received PPS, there were greater therapeutic changes and reduced barriers to participation in treatment. The incremental benefits of PPS are noteworthy because the core treatment (PSST ⫹ PMT) produces relatively potent changes (Sheldrick et al., 2001). The addition of an intervention that focused on the parents made a difference nonetheless. Given that this study was a randomized controlled trial, it is parsimonious and plausible to conclude that the intervention was responsible for the differences between groups (i.e., that there was a causal relation between the intervention and the outcomes of interest). A randomized controlled trial is not a final step in the process of understanding change and, indeed, in the case of the present research is actually an early step. The reason pertains to the notion of construct validity (Cook & Campbell, 1979). Specifi- This document is copyrighted by the American Psychological Association or one of its allied publishers. This article is intended solely for the personal use of the individual user and is not to be disseminated broadly. 512 KAZDIN AND WHITLEY cally, although it is reasonable to attribute the effects to “the intervention,” that facet of the intervention or why the intervention led to the differences is not clear. Effective treatments— even very well investigated treatments— often are shown and known to produce change without evidence that the putative processes involved account for the change. An excellent example is cognitive therapy for depression, in which the proposed reasons for the effectiveness of treatment (e.g., changes in specific cognitions) have not been established as mediators of outcome (Burns & Spangler, 2001; Hollon & Beck, 1994; Kazdin, 2003). In a parallel way, this study conveys that the intervention is likely to be responsible for change, but without a demonstration of why or through what processes. As noted previously, stress is one of many factors that often co-occur among families of children with conduct problems and that influence treatment outcome. The usual research strategy by which this influence is established is measurement of multiple risk factors and statistical evaluation of their separate, combined, and incremental contributions to a particular outcome (e.g., onset of disorder, relapse, therapeutic change). We have taken this strategy in some of our prior work (Kazdin, 1995a; Kazdin et al., 1995). In this report, we elected a complementary strategy, namely, to select a construct (parental stress) that (a) has been implicated in prior research as pivotal to the clinical problem (e.g., the interrelation of parent stress, disciplinary practices, and deviant child behavior), (b) has been shown to relate to child treatment outcome, and (c) is malleable (i.e., it can change and be changed within the confines of an intervention study). These criteria helped us to sift through many variables (e.g., socioeconomic status, life events, living conditions, poor neighborhoods, parent history of antisocial behavior) relevant to treatment outcome and led us to parental stress. Also, we have seen parental stress change in response to treatment of aggressive and antisocial children (Kazdin & Wassell, 2000). Thus, stress is likely to be reciprocally related to child deviance (i.e., it contributes to but also is influenced by deviant child behavior). Although the study indicated that PPS led to significant changes, many constructs other than stress might be proposed to explain the findings. Indeed, it is incumbent on us to look elsewhere because mediational tests did not suggest stress was the critical influence. Changes in parent depression, self-esteem, and empowerment and improved marital relations sometimes are concomitant effects of effectively treating children with externalizing problems (e.g., Scovern et al., 1980; Taub, Tighe, & Burchard, 2001). Moreover, parental stress is intertwined with depression and absence of social support in families of children with conduct problems (Patterson & Forgatch, 1990; Wahler & Dumas, 1989). Perhaps our PPS intervention achieved change by altering one of these other facets, and stress played an indirect role. As an alternative interpretation, perhaps PPS exerted its effect by improving patient adherence to the core treatments. PSST and PMT make demands on families (e.g., setting up reinforcement programs in the home, engaging in problem-solving skills homework assignments included as part of the child’s treatment). PPS may serve a motivational function by improving how well parents carry out the procedures. In support of this, attention to parental concerns and family issues in the context of treating disruptive children improves parent attendance and retention in treatment (Prinz & Miller, 1994; Santisteban et al., 1996). It is only a small leap to propose that other facets of complying with treatment (e.g., executing behavior-change programs at home) are enhanced by PPS and account for the present results. Indeed, many families of aggressive and antisocial children are quite stressed, and reduction of stress may be essential to execution of any treatment procedure. The present study was not designed to elaborate the mechanism of change. Rather, our first goal was to evaluate whether an added intervention to an evidence-based treatment could lead to reliable changes and to do so across multiple domains. The next priorities would be to replicate the effect and test alternative interpretations to explain any changes PPS produces. Parent training, a core part of our intervention, is the most well-investigated treatment for oppositional, aggressive, and antisocial children (Brestan & Eyberg, 1998; Kazdin, 2000a). In the context of treatment and prevention, several studies have supplemented parent training with problem-solving interventions directed toward the children (e.g., Kazdin, 1996b; Webster-Stratton, 1996) and social support and problem solving of the parent (e.g., Dadds & McHugh, 1992; Pfiffner, Jouriles, Brown, Etscheidt, & Kelly, 1990; Sanders, Markie-Dadds, Tully, & Bor, 2000). The results indicate that treatment effects can be enhanced with additional interventions. Our results are in keeping with these other studies. Clearly, the upcoming tasks are better triage, that is, matching children and families to identify who requires or profits from such treatments and of course the mechanisms through which adjunctive interventions effect change. Several limitations of this study deserve mention. First, this study focused on children clinically referred for aggressive and antisocial behavior. Parent stress may well play a role in diverse clinical problems for which children are referred. However, there is reason to be cautious about generalization of the present findings to other clinical populations, given the special role that stress has been shown to play in disciplinary practices, child deviance, and treatment outcome among children referred for aggressive and antisocial behavior. That research served as a critical impetus for our focus on parental stress. Second, perception of parent stress was assessed with a single measure. There is a danger in generalizing beyond any one measure of a construct, even one as well investigated as the PSI. Replication of the present study with different ways to operationalize perception of stress would be quite valuable. Our study was restricted to one measure to capture the facet of perceived stress that has emerged as critical to treatment in our prior research. Yet, there is such a broad range of measures of stress and hassles and the perception and experience of each of these as to provide many research leads for further study. Third, and related, the measures were restricted to parent report as the source of information regarding therapeutic change. Different measures were used including observations of concrete behaviors parents observed in the home (PDR). Even so, this too can be conceived as parent report. The perspectives of others pertinent to therapeutic change (children, teachers, clinicians) and different assessment modalities (e.g., records of fights, school detentions) were not included. The generality of results across informants and modalities of assessments remains to be shown. Fourth, our PPS intervention was provided in the context of an effective, evidence-based treatment. We cannot state and do not even propose that PPS would be effective on its own (without the other treatments) or as an adjunct to another treatment. PPS was developed after years of work with highly stressed families of This document is copyrighted by the American Psychological Association or one of its allied publishers. This article is intended solely for the personal use of the individual user and is not to be disseminated broadly. TREATMENT OF AGGRESSIVE AND ANTISOCIAL CHILDREN referred aggressive and antisocial children. PPS addresses one facet of a larger child–parent–family-context gestalt specific to conduct problems (Kazdin, 1995b). Fifth, we did not quantify treatment integrity. The supervision procedures in place are no substitute for quantifying execution of treatment. Assessment of treatment integrity would permit analyses more specifically of constructs of interest such as whether stress influences or is influenced by integrity or execution of treatment by the therapist. Finally, we did not examine long-term effects of treatment. Our prior work has shown that treatment outcomes with PSST and PMT are maintained up to a year or 2 later at the level achieved at posttreatment. However, the long-term effects of PPS were not studied here, and one must be commensurately cautious about the impact. It might well be that the PPS exerts short-term impact and we provided no evidence to suggest otherwise. There are issues that are pertinent to this study but have broader implications. First, the present study portrays stress as a villain. The deleterious effects of stress on mental and physical health outcomes are well established. Yet, it is likely that stress of the type we studied or some levels of that stress do not invariably disrupt child-rearing practices among parents of conduct problem children. Indeed, there might even be beneficial effects. Alternatively, a moderator we have yet to study might negate deleterious effects of stress. This study did not analyze stress in a way to reveal these relations, and we are wary of implying uniform, linear, and simplistic effects of parental stress or its amelioration. Second, there is a strategic issue about treatment research that this study raises. We began with an evidence-based treatment and added a component to enhance treatment outcome. This is a useful strategy because evidence-based treatments are not effective for everyone and not sufficiently effective for many children. Efforts to supplement and augment treatments are important, and there are very few such efforts in the child treatment literature (Kazdin, 2000a). Consequently, adding a component to enhance treatment impact seems reasonable and perhaps even wise. Yet there are serious limitations of this approach. One cannot keep adding components to a treatment that might enhance or indeed actually does enhance therapeutic change. From a methodological standpoint, demonstrating that any new component will make a difference can be quite difficult because of limitations in assessment (e.g., ceiling effects) and research design (e.g., sample sizes needed to show small increments in effects). The methodological and design constraints limit how much one can add to an evidence-based treatment and expect to show an effect, even if there is one. From a more clinical and service delivery standpoint, the strategy of adding components to treatment has further limitations. Patient attrition, already high in child, adolescent, and adult therapy (40%– 60%) is a partial function of the demands made of the client (Kazdin, Holland, & Crowley, 1997) and the duration of treatment (Phillips, 1985). Adding a component to treatment that increases either one of these is quite likely to cause greater attrition so that fewer patients will complete treatment. Also, of course, there is the monetary cost. Improving treatment by adding components may add to the number of sessions and raise reimbursement issues and questions about incremental costs in relation to incremental benefits. Two other strategies than ours can be used to enhance treatment effects. First, for evidence-based treatments, it is important to 513 identify who is not likely to respond to treatment or who has not in fact responded during the course of treatment. These individuals may warrant a targeted extra or “new and improved” treatment (i.e., a stepped-care model; Haaga, 2000). Providing an added component of treatment to everyone, as in the present study, may not be optimal or necessary; many of the children and families may respond well or well enough to the treatment in its less intensive, less costly, and more abbreviated form. In the present study, PPS was given to everyone assigned to that condition. The approach of this study may not be the best for improving therapy, especially for improving outcomes for those who need something new or different. That is, raising the mean level for the entire group (that received the extra treatment) may not be as important as targeting those who do not respond and raising just their mean. Second, understanding the mechanisms through which treatment leads to change is another strategy for enhancing treatment effects. It is still the case that we know very little about why treatments lead to change, even among the evidence-based treatments (Kazdin, 2000a). This means that the treatments we are using, without any added components, may not be optimal. It may be premature to add further components to treatment without understanding how to optimize change of the treatment to which the components are added. Moreover, these components, even if they enhance outcome, further raise the importance of understanding mechanisms (i.e., it will be essential to understand why any new component improves outcome). The present study focused on stress of the parent over the course of treatment and the effects of this focus on several outcomes. As predicted, addressing parent stress during treatment improved treatment outcome for children and parents and reduced the burden of treatment that parents experience while attending therapy. The next steps are those we have outlined in our comments about alternative strategies to improve treatment effects. Specifically, it will be important to identify youths who respond well with the core or minimal treatment, to provide additional or new interventions to only those who require them, and to understand for responders and nonresponders the mechanisms through which change occurs. Understanding the mechanisms of change will be critical. Indeed, if the mechanisms of core treatments were better understood, it might be possible to enhance treatment effects markedly without new components such as the one evaluated in this study. References Abidin, R. R. (1990). Parenting Stress Index clinical manual. Charlottesville, VA: Pediatric Psychology Press. Achenbach, T. M. (1991). Manual for the Child Behavior Checklist/4 –18 and 1991 Profile. Burlington: University of Vermont, Department of Psychiatry. Ackerman, B. P., Schoff, K., Levinson, K., Youngstrom, E., & Izard, C. D. (1999). The relations between cluster indexes of risk and promotion and the problem behaviors of 6- and 7-year-old children from economically disadvantaged families. Developmental Psychology, 35, 1355–1366. American Psychiatric Association. (1987). Diagnostic and statistical manual of mental disorders (3rd ed., rev.). Washington, DC: Author. American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author. Aneshensel, C. S., & Stone, J. D. (1982). Stress and depression: A test of the buffering model of social support. Archives of General Psychiatry, 39, 1392–1396. This document is copyrighted by the American Psychological Association or one of its allied publishers. This article is intended solely for the personal use of the individual user and is not to be disseminated broadly. 514 KAZDIN AND WHITLEY Beck, A. T., Steer, R. A., & Garbin, M. G. (1988). Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review, 8, 77–100. Brestan, E. V., & Eyberg, S. M. (1998). Effective psychosocial treatment of conduct-disordered children and adolescents: 29 years, 82 studies, 5,275 children. Journal of Clinical Child Psychology, 27, 180 –189. Burns, D. D., & Spangler, D. L. (2001). Do changes in dysfunctional attitudes mediate changes in depression and anxiety in cognitive– behavioral therapy. Behavior Therapy, 32, 337–369. Chamberlain, P., & Reid, J. B. (1987). Parent observation and report of child symptoms. Behavioral Assessment, 9, 97–109. Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Erlbaum. Cohen, S., Kessler, R. C., & Gordon, L. U. (Eds.). (1997) Measuring stress: A guide for health and social scientists. New York: Oxford University Press. Cook, T. D., & Campbell, D. T. (1979). Quasi-experimentation: Design and analysis issues for field settings. Chicago: Rand McNally. Crowley, M. J., & Kazdin, A. E. (1998). Child psychosocial functioning and parent quality of life among clinically referred children. Journal of Child and Family Studies, 7, 233–251. Dadds, M. R., & McHugh, T. A. (1992). Social support and treatment outcome in behavioral family therapy for child conduct problems. Journal of Consulting and Clinical Psychology, 60, 252–259. Deater-Deckard, K. (1998). Parenting stress and child adjustment: Some old hypotheses and new questions. Clinical Psychology: Science and Practice, 5, 314 –332. Deater-Deckard, K., Dodge, K. A., Bates, J. E., & Pettit, G. S. (1998). Multiple risk factors in the development of externalizing behavior problems: Group and individual differences. Development and Psychopathology, 10, 469 – 493. Derogatis, L. R., & Cleary, P. A. (1977). Confirmation of the dimensional structure of the SCL–90: A study in construct validation. Journal of Clinical Psychology, 33, 981–989. Dumas, J. E., & Wahler, R. G. (1983). Predictors of treatment outcome in parent training: Mother insularity and socioeconomic disadvantage. Behavioral Assessment, 5, 301–313. Foster, S. L., & Robin, A. L. (1997). Family conflict and communication in adolescence. In E. J. Mash & L. G. Terdal (Eds.), Assessment of childhood disorders (3rd ed., pp. 627– 682). New York: Guilford Press. Haaga, D. A. F. (2000). Introduction to the special section on stepped-care models in psychotherapy. Journal of Consulting and Clinical Psychology, 68, 547–548. Hollingshead, A. B. (1975). Four-Factor Index of Social Status. New Haven, CT: Yale University. Hollon, S. D., & Beck, A. T. (1994). Cognitive and cognitive behavioral therapies. In A. E. Bergin & S. L. Garfield (Eds.), Handbook of psychotherapy and behavior change (4th ed., pp. 428 – 466). New York: Wiley. Holmbeck, G. N. (2002). Post hoc probing of significant moderational and mediational effects in studies of pediatric populations. Journal of Pediatric Psychology, 27, 87–96. Holmes, C. S., Yu, Z., & Frentz, J. (1999). Chronic and discrete stress as predictors of children’s adjustment. Journal of Consulting and Clinical Psychology, 37, 411– 419. Kazdin, A. E. (1995a). Child, parent, and family dysfunction as predictors of outcome in cognitive– behavioral treatment of antisocial children. Behaviour Research and Therapy, 33, 271–281. Kazdin, A. E. (1995b). Conduct disorder in childhood and adolescence (2nd ed.). Newbury Park, CA: Sage. Kazdin, A. E. (1996a). Dropping out of child psychotherapy: Issues for research and implications for practice. Clinical Child Psychology and Psychiatry, 1, 133–156. Kazdin, A. E. (1996b). Problem solving and parent management in treating aggressive and antisocial behavior. In E. D. Hibbs & P. S. Jensen (Eds.), Psychosocial treatments for child and adolescent disorders: Empirically based strategies for clinical practice (pp. 377– 408). Washington, DC: American Psychological Association. Kazdin, A. E. (2000a). Psychotherapy for children and adolescents: Directions for research and practice. New York: Oxford University Press. Kazdin, A. E. (2000b). Treatments for aggressive and antisocial children. In D. O. Lewis & C. A. Yeager (Eds.), Child and Adolescent Psychiatric Clinics of North America, 9, 841– 858. Kazdin, A. E. (2003). Research design in clinical psychology (4th ed.). Needham Heights, MA: Allyn & Bacon. Kazdin, A. E., & Bass, D. (1989). Power to detect differences between alternative treatments in comparative psychotherapy outcome research. Journal of Consulting and Clinical Psychology, 57, 138 –147. Kazdin, A. E., & Esveldt-Dawson, K. (1986). The Interview for Antisocial Behavior: Psychometric characteristics and concurrent validity with child psychiatric inpatients. Journal of Psychopathology and Behavioral Assessment, 8, 289 –303. Kazdin, A. E., Holland, L., & Crowley, M. (1997). Family experience of barriers to treatment and premature termination from child therapy. Journal of Consulting and Clinical Psychology, 65, 453– 463. Kazdin, A. E., Holland, L., Crowley, M., & Breton, S. (1997). Barriers to Participation in Treatment Scale: Evaluation and validation in the context of child outpatient treatment. Journal of Child Psychology and Psychiatry, 38, 1051–1062. Kazdin, A. E., & Mazurick, J. L. (1994). Dropping out of child psychotherapy: Distinguishing early and late dropouts over the course of treatment. Journal of Consulting and Clinical Psychology, 62, 1069 – 1074. Kazdin, A. E., Mazurick, J. L., & Siegel, T. C. (1994). Treatment outcome among children with externalizing disorder who terminate prematurely versus those who complete psychotherapy. Journal of the American Academy of Child and Adolescent Psychiatry, 33, 549 –557. Kazdin, A. E., Siegel, T., & Bass, D. (1992). Cognitive problem-solving skills training and parent management training in the treatment of antisocial behavior in children. Journal of Consulting and Clinical Psychology, 60, 733–747. Kazdin, A. E., Stolar, M. J., & Marciano, P. L. (1995). Risk factors for dropping out of treatment among White and Black families. Journal of Family Psychology, 9, 402– 417. Kazdin, A. E., & Wassell, G. (1999). Barriers to treatment participation and therapeutic change among children referred for conduct disorder. Journal of Clinical Child Psychology, 28, 160 –172. Kazdin, A. E., & Wassell, G. (2000). Therapeutic changes in children, parents, and families resulting from treatment of children with conduct problems. Journal of the American Academy of Child and Adolescent Psychiatry, 39, 414 – 420. Kinsella, G., Ong, B., Murtagh, D., Prior, M., & Sawyer, M. (1999). The role of the family for behavioral outcome in children and adolescents following traumatic brain injury. Journal of Consulting and Clinical Psychology, 67, 116 –123. Kraemer, H. C., Stice, E., Kazdin, A. E., Offord, D. R., & Kupfer, D. J. (2001). How do risk factors work together? Mediators, moderators, independent, overlapping, and proxy-risk factors. American Journal of Psychiatry, 158, 848 – 856. Lawson, D. A., & O’Brien, R. M. (1994). Behavioral and self-report measures of burnout in developmental disabilities. Journal of Organizational Behavior Management, 14, 37–54. Lindblad-Goldberg, M., Dukes, J. L., & Lasley, J. H. (1988). Stress in Black, low-income single-parent families: Normative and dysfunctional patterns. American Journal of Orthopsychiatry, 58, 104 –120. Lloyd, B. H., & Abidin, R. R. (1985). Revision of the Parenting Stress Index. Journal of Pediatric Psychology, 10, 169 –177. Maughan, B. (2001). Conduct disorder in context. In J. Hill & B. Maughan This document is copyrighted by the American Psychological Association or one of its allied publishers. This article is intended solely for the personal use of the individual user and is not to be disseminated broadly. TREATMENT OF AGGRESSIVE AND ANTISOCIAL CHILDREN (Eds.), Conduct disorders in childhood and adolescence (pp. 169 –201). Cambridge, England: Cambridge University Press. Miller, T. W. (Ed). (1989). Stressful life events. Madison, CT: International Universities Press. Moos, R. H., & Moos, B. S. (1981). Family Environment Scale manual. Palo Alto, CA: Consulting Psychologists Press. Offord, D., Boyle, M. H., Racine, Y. A., Fleming, J. E., Cadman, D. T., Blum, H. M., et al. (1992). Outcome, prognosis, and risk in a longitudinal follow-up study. Journal of the American Academy of Child and Adolescent Psychiatry, 31, 916 –923. Patterson, G. R. (1988). Stress: A change agent for family process. In N. Garmezy & M. Rutter (Eds.), Stress, coping, and development in children (pp. 235–264). Baltimore: Johns Hopkins University Press. Patterson, G. R., & Forgatch, M. S. (1990). Initiation and maintenance of process disrupting single-mother families. In G. R. Patterson (Ed.), Depression and aggression in family interaction (pp. 209 –245). Hillsdale, NJ: Erlbaum. Patterson, G. R., Reid, J. B., & Dishion, T. J. (1992). Antisocial boys. Eugene, OR: Castalia. Pfiffner, L. G., Jouriles, E. N., Brown, M. M., Etscheidt, M. A., & Kelly, J. A. (1990). Effects of problem-solving therapy on outcomes of parent training for single-parent families. Child and Family Behavior Therapy, 12, 1–11. Phillips, E. L. (1985). Psychotherapy revised: New frontiers in research and practice. Hillsdale, NJ: Erlbaum. Prinz, R. J., & Miller, G. E. (1994). Family-based treatment for childhood antisocial behavior: Experimental influences on dropout and engagement. Journal of Consulting and Clinical Psychology, 62, 645– 650. Robins, L. N. (1991). Conduct disorder. Journal of Child Psychology and Psychiatry, 32, 193–212. Rose, J., Jones, F., & Fletcher, C. B. (1998a). The impact of a stress management program on staff well-being and performance at work. Work and Stress, 12, 112–124. Rose, J., Jones, F., & Fletcher, C. B. (1998b). Investigating the relationship between stress and worker behavior. Journal of Intellectual Disability Research, 42, 163–172. Rossi, J. S. (1990). Statistical power of psychological research: What have we gained in 20 years? Journal of Consulting and Clinical Psychology, 58, 646 – 656. Sanders, M. R., Dadds, M. R., & Bor, W. (1989). Contextual analysis of child oppositional and maternal aversive behaviors in families of conduct-disordered and nonproblem children. Journal of Clinical Child Psychology, 18, 72– 83. Sanders, M. R., Markie-Dadds, C., Tully, L. A., & Bor, W. (2000). The Triple P-Positive Parenting Program: A comparison of enhanced, standard, and self-directed behavioral family intervention for parents of children with early onset conduct problems. Journal of Consulting and Clinical Psychology, 68, 624 – 640. Santisteban, D. A., Szapocznik, J., Perez-Vidal, A., Kurtines, W. H., Murray, E. J., & LaPerriere, A. (1996). Efficacy of intervention for 515 engaging youth and families into treatment and some variables that may contribute to differential effectiveness. Journal of Family Psychology, 10, 35– 44. Scovern, A. W., Bukstel, L. H., Kilmann, P. R., Laval, R. A., Busemeyer, J., & Smith, V. (1980). Effects of parent counseling on the family system. Journal of Counseling Psychology, 27, 268 –275. Sheldrick, R. C., Kendall, P. C., & Heimberg, R. G. (2001). Assessing clinical significance: A comparison of three treatments for conduct disordered children. Clinical Psychology: Science and Practice, 8, 418 – 430. Short, K. H., & Johnston, C. (1997). Stress, maternal distress, and children’s adjustment following immigration: The buffering role of social support. Journal of Consulting and Clinical Psychology, 65, 494 –503. Stoff, D. M., Breiling, J., & Maser, J. D. (Eds.). (1997). Handbook of antisocial behavior. New York: Wiley. Takeuchi, D. T., Williams, D. R., & Adair, R. K. (1991). Economic stress in the family and children’s emotional and behavioral problems. Journal of Marriage and the Family, 53, 1031–1041. Taub, J., Tighe, T. A., & Burchard, J. (2001). The effects of parent empowerment on adjustment for children receiving comprehensive mental health services. Children’s Services: Social Policy, Research, and Practice, 4, 103–122. Wahler, R. G. (1980). The insular mother: Her problems in parent– child treatment. Journal of Applied Behavior Analysis, 13, 207–219. Wahler, R. G., & Afton, A. D. (1980). Attentional processes in insular and noninsular mothers: Some differences in their summary reports about child problem behaviors. Child Behavior Therapy, 2, 25– 41. Wahler, R. G., & Dumas, J. E. (1989). Attentional problems in dysfunctional mother– child interactions: An interbehavioral model. Psychological Bulletin, 105, 116 –130. Webster-Stratton, C. (1985). Predictors of treatment outcome in parent training for conduct disordered children. Behavior Therapy, 16, 223– 243. Webster-Stratton, C. (1996). Early intervention with videotape modeling: Programs for families of children with oppositional defiant disorder or conduct disorder. In E. D. Hibbs & P. Jensen (Eds.), Psychosocial treatment research of child and adolescent disorders. Empirically based strategies for clinical practice (pp. 435– 474). Washington, DC: American Psychological Association. Webster-Stratton, C., & Hammond, M. (1997). Treating children with early-onset conduct problems: A comparison of child and parent training interventions. Journal of Consulting and Clinical Psychology, 65, 93– 109. Wechsler, D. (1974). Manual for the Wechsler Intelligence Scale for Children—Revised. New York: Psychological Corporation. Received October 8, 2001 Revision received March 19, 2002 Accepted May 13, 2002 䡲