ORIGINALES Practice Of Central Nervous System
Anuncio

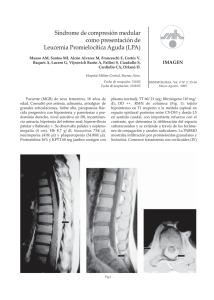
Documento descargado de http://www.elsevier.es el 21/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. ORIGINALES Practice of central nervous system prophylaxis and treatment in acute leukemias in Spain. Prospective registry study 210.658 Juan-Manuel Sanchoa, Mireia Morgadesa, Reyes Arranzb, Pascual Fernández-Abellánc, Guillermo Debend, Natalia Alonsoe, Margarita Blanesf, María José Rodríguezg, Concepción Nicolásh, Eva Sánchezi, Alberto Fernández de Sevillaj, Eulogio Condek and Josep-Maria Riberaa, on behalf of investigators of QUIT Study (PETHEMA, GELTAMO and GOTEL Groups) a Servicio de Hematología Clínica. ICO-Hospital Germans Trias i Pujol. Badalona. Universitat Autònoma de Barcelona. Barcelona. Servicio de Hematología. Hospital Universitario de la Princesa. Madrid. c Servicio de Hematología. Hospital General Universitario de Alicante. Alicante. d Servicio de Hematología. Hospital Juan Canalejo. La Coruña. e Servicio de Hematología. Complejo Hospitalario Universitario de Santiago. Santiago de Compostela. La Coruña. f Servicio de Hematología. Hospital La Fe. Valencia. g Servicio de Hematología. Hospital Universitario de Canarias. Santa Cruz de Tenerife. h Servicio de Hematología. Hospital Universitario Central de Asturias. Oviedo. Asturias. i Servicio de Hematología. Hospital Vall d’Hebron. Barcelona. j Servicio de Hematología. ICO-Hospital Duran i Reynals. L’Hospitalet de Llobregat. Barcelona. k Servicio de Hematología. Hospital Marqués de Valdecilla. Santander. Cantabria. España. b BACKGROUND AND OBJECTIVE: Central nervous system (CNS) involvement in patients diagnosed with acute leukemias (AL) is an uncommon complication with poor prognosis. The indication and the schedules of prophylaxis and treatment of CNS involvement in AL are not homogenous among countries and within the same country. The aim of this prospective longitudinal study was to analyze and report the practice of CNS prophylaxis and treatment in patients with AL in Spain. PATIENTS AND METHOD: Prospective study conducted from June 2005 to June 2006. Adult patients (ⱖ 18 yr.) diagnosed with AL who received CNS prophylaxis or treatment were consecutively included through online registration. RESULTS: 265 patients from 32 hospitals were included. Mean (standard deviation) age was 44 (16) yr. and 133 (50%) were males. For acute lymphoblastic leukemia patients (n = 158), CNS therapy was given to 12 cases (10 at diagnosis and 2 at relapse) and consisted of triple intrathecal therapy (TIT, methotrexate, cytarabine and hydrocortisone) in 11 and liposomal depot cytarabine in one. CNS prophylaxis (n = 146) consisted of TIT in 135 cases, intrathecal methotrexate in 7, intrathecal cytarabine in 2 and intrathecal liposomal depot cytarabine in 2. No cranial irradiation either for prophylaxis or therapy was given in any case. In acute myeloblastic leukemia patients (n = 107), CNS therapy was administered to 17 cases (9 at diagnosis and 8 at relapse). Intrathecal therapy consisted of TIT in 11, intrathecal liposomal depot cytarabine in 5 and intrathecal cytarabine in one. One patient also received craniospinal irradiation. CNS prophylaxis (n = 90) consisted of TIT in 68 cases and intrathecal methotrexate in 22. CONCLUSIONS: In Spain, the patterns of CNS prophylaxis and therapy for AL are homogeneous. TIT was the most frequent schedule for CNS prophylaxis and therapy. The lack of use of cranial or craniospinal irradiation and the administration of new drugs (i.e.: liposomal depot cytarabine) for CNS therapy and prophylaxis is of note. Key words: Acute leukemia. Central nervous system involvement. Intrathecal. Liposomal depot cyitarabine. Práctica habitual de profilaxis y tratamiento de la infiltración neuromeníngea en pacientes con leucemia aguda en España. Estudio de registro prospectivo FUNDAMENTO Y OBJETIVO: La infiltración del sistema nervioso central (SNC) en pacientes diagnosticados de leucemia aguda (LA) es una complicación infrecuente que comporta un mal pronóstico. La indicación y las pautas de profilaxis y tratamiento de la infiltración neuromeníngea en la LA no son homogéneas en los diferentes países, y tampoco en los diferentes centros de un mismo país. El objetivo de este estudio longitudinal y prospectivo ha sido describir la práctica real de profilaxis y tratamiento de la infiltración neuromeníngea en pacientes con LA en España. PACIENTES Y MÉTODO: Se trata de un estudio prospectivo llevado a cabo desde junio de 2005 a junio de 2006. Se incluyó, mediante registro electrónico, a los pacientes adultos (edad ⱖ 18 años) diagnosticados de LA que recibieron profilaxis o tratamiento de la infiltración del SNC. RESULTADOS: Se incluyó a un total de 265 pacientes procedentes de 32 hospitales. La media (desviación estándar) de edad fue de 44 (16) años y 133 (50%) eran varones. Entre los 158 pacientes con leucemia linfoblástica aguda, 12 (10 en el momento del diagnóstico y 2 en recaída) recibieron tratamiento del SNC por infiltración neuromeníngea, que consistió en tratamiento intratecal triple (TIT: metotrexato, citarabina e hidrocortisona) en 11 casos y citarabina liposómica de liberación lenta por vía intratecal en uno. La profilaxis del SNC administrada en los 146 pacientes restantes incluyó TIT en 135 casos, metotrexato intratecal en 7, citarabina intratecal en 2 y citarabina liposómica de liberación lenta por vía intratecal en 2. No se administró radioterapia craneal ni craneoespinal a ningún paciente. Entre los 107 pacientes con leucemia mieloblástica aguda, 17 tenían infiltración del SNC (9 en el momento del diagnóstico y 8 en la recaída). El tratamiento intratecal consistió en TIT en 11 casos, citarabina liposómica de liberación lenta en 5 y citarabina intratecal en uno. Un paciente recibió además radioterapia craneoespinal. La profilaxis del SNC en los 90 pacientes restantes incluyó TIT en 68 casos y metotrexato intratecal en 22. CONCLUSIONES: En España las pautas de profilaxis y tratamiento de la infiltración neuromeníngea en pacientes con LA son homogéneas. El TIT fue el esquema usado con mayor frecuencia tanto para la profilaxis como para el tratamiento del SNC. Llama la atención la escasa utilización de la radioterapia holocraneal o craneoespinal, así como la administración de nuevos fármacos, como la citarabina liposómica de liberación lenta, en el tratamiento y la profilaxis de la meningosis leucémica. Palabras clave: Leucemia aguda. Infiltración del sistema nervioso central. Intratecal. Citarabina liposómica de liberación lenta. Meningeal involvement in patients diagnosed with acute leukemia (AL) is associated with poor prognosis. In patients diagnosed with acute lymphoblastic leukemia (ALL), this is a well-recognized complication that appears in about 5% of the patients at the time of the diagnosis, and in 3-8% of patients at relapse, despite central nervous system (CNS) prophylaxis1-3. In patients with acute myeloid leukemia (AML), CNS involvement is a more infrequent event. Risk factors for leukemic meningeosis in both AML and, specially, ALL patients have been identified, which has led to the development of prophylaxis schedules based on the administration of CNS-directed therapies such as cranial irradiation, intrathecal drugs and systemic therapy with drugs able to cross the blood-brain barrier4-7. However, the schedules of prophylaxis and treatment of CNS involvement in AL are not homogeneous in different countries and even within the same country. The QUIT (Registro Español de Pacientes que Reciben Quimioterapia Intratecal) registry was an initiative of the PETHEMA (Programa para el Estudio y Tratamiento de las Hemopatías Malignas, Asociación Española de Hematología y Hemotera- Study supported in part by grant P-EF/06 from the José Carreras International Leukemia Foundation. The study was also partially supported by an unrestricted grant from Mundipharma Pharmaceuticals SL, and RD06/0020/1056 from RETICS. Correspondence: Dr. J.M. Ribera. Servicio de Hematología Clínica. Institut Català d’Oncologia-Hospital Germans Trias i Pujol. Ctra. Canyet, s/n. 08916 Badalona. Barcelona. España. E-mail: [email protected] Recibido el 29-5-2007; aceptado para su publicación 5-6-2007. Med Clin (Barc). 2008;131(11):401-5 401 Documento descargado de http://www.elsevier.es el 21/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. SANCHO JM ET AL. PRACTICE OF CENTRAL NERVOUS SYSTEM PROPHYLAXIS AND TREATMENT IN ACUTE LEUKEMIAS IN SPAIN. PROSPECTIVE REGISTRY STUDY pia), GEL/TAMO (Grupo Español de Linfomas/Trasplante Autólogo de Médula Ósea) and GOTEL (Grupo Oncológico para el Tratamiento y Estudio de los Linfomas) groups designed to prospectively know the current practice of CNS prophylaxis and therapy in patients diagnosed with hematological malignancies (AL and lymphoproliferative disorders) in Spain. The objective of this study was to report the practice of CNS prophylaxis and treatment in patients with AL. Patients and method This prospective study was conducted from June 2005 to June 2006 in 32 Spanish hospitals. Adult patients (ⱖ 18 yr.) diagnosed with AL who received CNS prophylaxis or CNS treatment were consecutively included through online registration. Each patient was included only once. The questionnaire included sociodemographic variables (age, sex, hospital), AL subtype (ALL, AML, and risk group in ALL patients) and date of diagnosis, presence or absence of meningeal involvement at diagnosis, timing of the CNS involvement (at diagnosis or at relapse), date of diagnosis of leukemic meningeosis, neurological symptoms at the time of CNS involvement, and the method used for diagnosis of CNS involvement (detection of blast cells in a sample of cerebrospinal fluid [CSF] by cytology or by flow cytometry, computed tomography [CT] scan or magnetic resonance imaging [MRI]). The following data of CNS therapy were recorded: reason of CNS-directed therapy (prophylaxis or treatment, and in case of prophylaxis, the reason: protocol requirement, hyperleukocytosis, conditioning regimen for stem cell transplantation [SCT] and others), date of the start of intrathecal drugs administered (methotrexate, cytarabine, and triple intrathecal therapy [TIT], including methotrexate, cytarabine and hydrocortisone), route (intrathecal through lumbar puncture or intraventricular) and schedule of administration, as well as other CNS-directed therapies such as cranial irradiation or the use of new drugs. An intermediate analysis after 6 months of start of registry was performed and their results were reported at meetings of PETHEMA, GEL/TAMO and GOTEL groups. Results were expressed as crude frequencies and percentages, and were analyzed separately for ALL and AML. Results A total of 265 patients diagnosed with AL from 32 hospitals were included. The mean (standard deviation) age was 44 (16) yr. (range: 18-78) and 133 (50%) were males. Distribution according to AL subtype was: ALL in 158 cases (59.6%) and AML in 107 (40.4%). Regarding ALL patients (table 1), intrathecal therapy was administered for leukemic meningeosis in 12 cases and as CNS prophylaxis in 146. Ten out of 12 patients with CNS involvement had blast cells at CSF at the time of the diagnosis, and 2 showed first CNS relapse. Diagnosis of CNS involvement was established by the observation of blast cells in CSF in 9 cases, flow cytometry in 8, and MRI or CT scan in 4. Neurological symptoms included: mental status impairment in 4 cases, cranial nerve palsy in 5, muscle weakness in 5, headache in 5, diplopy in 3, sensorial neuropathy in 2, impairment in march in 2 402 Med Clin (Barc). 2008;131(11):401-5 and loss of vision in one. As shown in table 1, TIT was the most common CNS-directed therapy administered, followed by depot liposomal cytarabine (as compassionate use). Lumbar puncture was the preferred route for intrathecal administration (11 out of the 12 patients), whereas in the remaining patient an intraventricular administration through an Ommaya reservoir was used. Cranial irradiation was not used in any case. With respect to CNS prophylaxis (n = 146), TIT was also the most frequent schedule (table 1), but the use of intrathecal depot liposomal cytarabine in 2 patients is of note. The reasons reported by the investigators for the compassionate use of this drug were the development of arachnoiditis due to intrathecal methotrexate in one case, and a high white blood cell count in the remaining patient. As occurred in patients with CNS involvement, lumbar puncture was the most frequent route for intrathecal administration (144 cases; 98.6%), whereas an Ommaya reservoir was used in only 2 patients (1.4%). Cranial or craniospinal radiotherapy was not administered as CNS prophylaxis in any case. Patients with AML (table 2) received intrathecal therapy for leukemic meningeosis in 17 cases and as CNS prophylaxis in the remaining 90. Nine out of these 17 patients showed CNS leukemia at the TABLE 1 Main characteristics of the acute lymphoblastic leukemia patients (n = 158) included in the QUIT Registry Variable Age (yr)* 40 (16) Gender (M/F) 82/76 Subtype ALL High-risk non-Ph ALL Intermediate-risk ALL Mature B ALL (Burkitt’s leukemia) Ph ALL Not specified 90 22 15 27 4 Therapy for CNS involvement (n = 12) TIT Methotrexate Cytarabine Depot liposomal cytarabine Cranial or craniospinal irradiation 11 0 0 1 0 Therapy for CNS prophylaxis (n = 146) TIT Methotrexate Cytarabine Depot liposomal cytarabine Cranial or craniospinal irradiation 135 7 2 2 0 Reason for CNS prophylaxis (n = 146) Protocol requirement Relapse Conditioning regimen for SCT 136 5 5 *Mean (standard deviation). ALL: acute lymphoblastic leuke- mia; CNS: central nervous system; F: female; M: male; Ph ALL: Philadelphia chromosome-positive acute lymphoblastic leukemia; QUIT Registry: Registro Español de Pacientes que Reciben Quimioterapia Intratecal; SCT: stem cell transplantation; TIT: triple intrathecal therapy (including methotrexate, cytarabine and hydrocortisone). time of diagnosis and 8 as relapse. Diagnosis of CNS involvement was established by: cytology (n = 10), flow cytometry (n = 6), and CT scan or MRI (n = 8). Neurological symptoms included: headache in 9 patients, vomiting in 7, impairment in march in 6, muscle weakness in 4, sensorial neuropathy in 4, cranial nerve palsy in 3, mental status impairment in 2, diplopy in 2 and loss of vision in 1. TIT was the most frequent CNS-directed therapy, but 5 patients received intrathecal depot liposomal cytarabine (as compassionate use). Only 2 patients received intrathecal therapy through an Ommaya reservoir. Craniospinal irradiation was given to one patient. The remaining 90 patients with AML received intrathecal therapy as prophylaxis (in all cases by lumbar puncture), with TIT again being the most frequent schedule reported (table 2). Similar to ALL patients, radiotherapy was not administered in any case. Tables 1 and 2 show that protocol requirement was the most frequent reason for CNS prophylaxis, followed by the administration of intrathecal therapy as part of the conditioning regimen for SCT. Discussion This is the first study that prospectively describes the current practice of prophylaxis and therapy for leukemic meningeosis in Spain. This study demonstrates that, in the Spanish population with AL, CNS prophylaxis and therapy schedules are homogeneous, with TIT through lumbar puncture being the most frequent therapy for CNS involvement or CNS prophylaxis. Two additional features are of note: the lack of use of cranial or craniospinal irradiation for prophylaxis or therapy of leukemic meningeosis, and the compassionate use of new formulations of drugs, such as liposomal depot cytarabine, in CNS involvement and even for CNS prophylaxis. Most of the information on CNS prophylaxis or therapy in patients diagnosed with hematological malignancies is provided by the analysis of patients treated according to local or multicenter protocols, but systematic reviews on the current practice of CNS chemoprophylaxis have only been reported in non-Hodgkin’s lymphoma patients8,9, but not in patients with AL. The uniform results of CNS prophylaxis in ALL are due to the wide use of the riskadapted protocols from the PETHEMA group in Spain10-16, which only included TIT as CNS prophylaxis and limited the use of CNS irradiation for selected cases of T-cell ALL in children with hyperleukocytosis in the early studies. With respect to the type of intrathecal therapy, two features should be pointed out. First, Documento descargado de http://www.elsevier.es el 21/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. SANCHO JM ET AL. PRACTICE OF CENTRAL NERVOUS SYSTEM PROPHYLAXIS AND TREATMENT IN ACUTE LEUKEMIAS IN SPAIN. PROSPECTIVE REGISTRY STUDY TABLE 2 Main characteristics of the acute myeloid leukemia patients (n = 107) included in the QUIT Registry Variable Age (yr)a 49 (14) Gender (M/F) 51/57 AML subtype AML Relapse of AML APL Relapse of APL 96 4 4 3 Therapy for CNS involvement (n = 17) TIT Methotrexate Cytarabine Depot liposomal cytarabine Cranial or craniospinal irradiation 11 0 1 5 1 Therapy for CNS prophylaxis (n = 90) TIT Methotrexate Cytarabine Depot liposomal cytarabine Cranial or craniospinal irradiation 68 22 0 0 0 Reason for CNS prophylaxis (n = 90) AML subtypeb and/or protocol requirement Conditioning regimen for SCT High WBC count Extramedullary involvement 69 14 6 1 a Mean (standard deviation); bmyelomonocytic or monocytic subtypes. AML: acute myeloid leukemia; APL: acute promyelocytic leukemia; CNS: central nervous system; F: female; M: male; QUIT Registry: Registro Español de Pacientes que Reciben Quimioterapia Intratecal; SCT: stem cell transplantation; TIT: triple intrathecal therapy (including methotrexate, cytarabine and hydrocortisone); WBC: white blood cells. the use of hydrocortisone instead of the more common dexamethasone, prednisone or prednisolone described in other studies3,17. This was due to the fact that in Spain the protocols for adult ALL patients were developed from ongoing pediatric trials in which hydrocortisone was the steroid drug used in TIT11,14,16. On the other hand, the use of combined intrathecal therapy instead of monotherapy with intrathecal methotrexate or intrathecal cytarabine reported in other studies is of note2,18. Despite these two differences, the frequency of CNS relapse in Spain using TIT as CNS prophylaxis1 was not different from that reported in other studies. Another remarkable point in this study is the scarce use reported of intrathecal prophylaxis in the conditioning regimen for SCT. The reason could be that this is not an uniformly admitted practice in SCT units. Thus, a recent survey carried out among EBMT (European Group for Bone Marrow Transplantation) centers showed that 47% of them never used pre-transplant intrathecal prophylaxis as part of the conditioning regimen for allogeneic SCT, whereas only 32% gave prophylactic intrathecal therapy after SCT19. In this study, the low frequency of cranial or craniospinal irradiation as CNS prophylaxis or treatment schedules in both ALL and AML is of note. In fact, recent studies performed in childhood ALL20-23 have described low rates of CNS relapse in patients in which CNS prophylaxis consisted of intrathecal therapy and systemic chemotherapy with drugs able to pass the blood-brain barrier, without concomitant radiotherapy. In these studies radiotherapy was eliminated to avoid its long-term effects on cognitive and endocrine function. Several studies have demonstrated similar results in adults. In a previous study from the PETHEMA group1, the frequency of CNS recurrence was only 5.8%, similar to that described in other studies in which CNS radiotherapy was omitted, provided that intrathecal therapy was used together with highdose systemic therapy2,18,24. In addition, in the present study radiotherapy was not used as CNS therapy in cases of initial involvement or CNS relapse in both ALL and AML (except in one patient), in spite of the poor prognosis associated with these events. This was probably because intrathecal and high-dose systemic therapy can adequately control CNS disease, and the cause of this poor prognosis is in fact systemic relapse, often present at the time of CNS relapse. In this situation, the best approach is systemic and CNS-directed therapy followed by SCT25-27. The compassionate use of new formulations of intrathecal drugs such as depot liposomal cytarabine is of note in this study, provided that there is no accepted indication by the regulatory agencies outside of neoplastic28-30 and lymphomatous31 meningeosis. Intrathecal depot liposomal cytarabine is a sustained-released formulation of cytarabine that maintains cytotoxic concentrations of the drug in the CSF during more than 2 weeks, thereby allowing fewer intrathecal administrations32,33. Despite the demonstrated efficacy in CNS involvement from solid tumors and lymphomas, there is scarce information on its use in AL, mostly reported as individual cases or small series34-36. The largest reports are focused on its use in meningeosis from ALL37,38 and describe response rates of about 80%. In a previous report from our group36, 3 out of 4 patients with CNS involvement in AL treated with intrathecal depot liposomal cytarabine (in 2 cases as the only drug and in the remaining as adjuvant therapy to other CNS-directed therapies) achieved blast cell clearance in CSF, whereas the remaining patient showed partial response. In an update of a European collaborative study with 19 patients recruited, the response rate was 83% in ALL patients and 43% in patients with Burkitt’s lymphoma or B-ALL (N. Gökbuget, personnel communication). Reports on the effectiveness of intrathecal depot liposomal cytarabine in AML are extremely infrequent, but in another study by our group39, 5 out of 6 AML patients receiving this drug alone achieved cytologic response, although all responders also received systemic therapy with high-dose cytarabine. Regarding the use of intrathecal depot liposomal cytarabine as CNS prophylaxis, there are 2 studies in which the feasibility of the administration of this drug has been demonstrated40,41. In this sense, the recently published study by Jabbour et al41 points out that 5 out of 31 patients (16%) developed neurotoxicity, almost always related to the concomitant administration of systemic high-dose methotrexate and cytarabine (in this study high-dose cytarabine was 3 g/m2 administered every 12 h for 2 days). These adverse events have not been described in other series. The promising results with intrathecal depot liposomal cytarabine justify the development of clinical trials to establish the role of this new formulation in the therapy and the prophylaxis of leukemic meningeosis. The lack of the systematic inclusion of all the cases in which CNS-directed therapy was administered in Spain constitutes the main limitation of the present study. However, this is probably a representative sample since the results of the present study are very similar to those obtained from the analysis of the frequency and patterns of CNS relapse in patients with ALL in the PETHEMA studies1. There are no similar published studies in AML, and consequently the magnitude of the possible biases of the present study cannot be demonstrated. A report on the use of CNS-directed therapy in cases of AML with CNS involvement carried out in Italy42 showed the preferential use of intrathecal therapy, although the combination of intrathecal therapy, CNS irradiation and high-dose systemic therapy yielded promising results. The results of the QUIT Registry demonstrated the preferential use of intrathecal therapy by lumbar route for prophylaxis and therapy of AL meningeosis in Spain, with the main reason for use being in the setting of protocols for therapy of AML and ALL. The lack of use of cranial irradiation is in concordance with modern protocols in which irradiation tends to be omitted due to excess toxicity when combined with chemotherapy. Finally, the anticipated phenomenon of compassionate use of new formulations of drugs (such as depot liposomal cytarabine) for which a formal indication is still not established has to be emphasized. Acknowledgements The following institutions and clinicians participated in the study: Hospital Universitari Germans Trias i Pujol, Badalona (J.M. Ribera, J.M. Med Clin (Barc). 2008;131(11):401-5 403 Documento descargado de http://www.elsevier.es el 21/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. SANCHO JM ET AL. PRACTICE OF CENTRAL NERVOUS SYSTEM PROPHYLAXIS AND TREATMENT IN ACUTE LEUKEMIAS IN SPAIN. PROSPECTIVE REGISTRY STUDY Sancho, M. Morgades); Hospital Universitario de la Princesa, Madrid (R. Arranz); Hospital General Universitario de Alicante, Alicante (P. Fernández-Abellán); Hospital Juan Canalejo, A Coruña (G. Deben); Complejo Hospitalario Universitario de Santiago, Santiago de Compostela (N. Alonso); Hospital Universitario La Fe, Valencia (M. Blanes); Hospital Universitario de Canarias, Santa Cruz de Tenerife (M.J. Rodríguez); Hospital Universitario Central de Asturias, Oviedo (C. Nicolás); Hospital Vall d’Hebron, Barcelona (E. Sánchez); Hospital Duran i Reynals, L’Hospitalet de Llobregat (A. Fernández de Sevilla); Hospital Marqués de Valdecilla, Santander (E. Conde); Hospital Josep Trueta, Girona (M. Hermosilla); Hospital Xeral, Lugo (J. Arias); Hospital Universitario de Getafe, Madrid (J.A. García); Hospital Universitario Virgen de la Arrixaca, Murcia (P. Rosique); Hospital del Mar, Barcelona (E. Abella); Hospital de Basurto, Bilbao (J.A. Márquez); Hospital Universitario Príncipe de Asturias, Madrid (J. García); Hospital Universitario de Salamanca, Salamanca (L. Vázquez); Hospital Universitario Miguel Servet, Zaragoza (A. Rubio); Complexo Hospitalario Universitario de Vigo, Pontevedra (C. Albo); Hospital Clínico de Zaragoza, Zaragoza (L. Palomera); Hospital Virgen del Camino, Pamplona (M.C. Mateos); Hospital General Universitario Gregorio Marañón, Madrid (M. Mayayo); Hospital Universitario La Paz, Madrid (M.A. Canales); Hospital de Fuenlabrada, Madrid (J.A. Hernández); Complejo Hospitalario de Jaén, Jaén (J.A. López); Hospital Clínico Universitario de Valladolid, Valladolid (F.J. Fernández); Hospital de Móstoles, Madrid (M.A. Andreu); Hospital Universitario Central de Asturias, Asturias (P. Chamorro); Hospital 12 de Octubre, Madrid (R. Toscano); Hospital de Sant Pau, Barcelona (S. Brunet). REFERENCES 1. Sancho JM, Ribera JM, Oriol A, Hernández-Rivas JM, Rivas C, Bethencourt C, et al. Central nervous system relapse in adult patients with acute lymphoblastic leukemia: frequency and prognosis in 467 patients without cranial irradiation for prophylaxis. Cancer. 2006;106:2540-6. 2. Linker C, Damon L, Ries C, Navarro W. Intensified and shortened cyclical chemotherapy for adult acute lymphoblastic leukemia. J Clin Oncol. 2002;20:2464-71. 3. Annino L, Vegna ML, Camera A, Specchia G, Visani G, Fioritoni G, et al for the GIMEMA Group. Treatment of adult acute lymphoblastic leukemia (ALL): long-term follow-up of the GIMEMA ALL 0288 randomized study. Blood. 2002;99:863-71. 4. Pinkel D, Woo S. Prevention and treatment of meningeal leukemia in children. Blood. 1994;84: 355-66. 5. Gokbuget N, Hoelzer D. Meningeosis leukaemica in adult acute lymphoblastic leukaemia. J Neurooncol. 1998;38:167-80. 6. Cortes J. Central nervous system involvement in adult acute lymphocytic leukemia. Hematol Oncol Clin North Am. 2001;15:145-62. 7. Pui CH. Towards optimal central nervous systemdirected treatment in childhood acute lymphoblastic leukemia. J Clin Oncol. 2003;21:179-81. 8. Cheung CW, Burton C, Smith P, Linch DC, Hoskin PJ, Ardeshna KM. Central nervous system chemoprophylaxis in non-Hodgkin lymphoma: current practice in the UK. Br J Haematol. 2005;131:193-200. 9. Buckstein R, Lim W, Franssen E, Imrie KL. CNS prophylaxis and treatment in non-Hodgkin’s lymphoma: variation in practice and lessons from the literature. Leuk Lymphoma. 2003; 44:955-62. 404 Med Clin (Barc). 2008;131(11):401-5 10. Ribera JM, Ortega JJ, Oriol A, Fontanillas M, Hernández-Rivas JM, Brunet S, et al, and members of PETHEMA Cooperative Group, Spanish Society of Haematology. Late intensification chemotherapy has not improved the results of intensive chemotherapy in adult acute lymphoblastic leukaemia. Results of a prospective multicenter randomized trial (PETHEMA ALL-89). Haematologica. 1998;83:222-30. 11. Ortega JJ, Ribera JM, Oriol A, Bastida P, González ME, Calvo C, et al, on belhalf of PETHEMA Group, Spanish Society of Haematology. Early and delayed consolidation chemotherapy significantly improves the outcome of children with intermediate risk acute lymphoblastic leukemia. Final results of the prospective randomized PETHEMA ALL-89 TRIAL. Haematologica. 2001;86: 586-95. 12. Ribera JM, Oriol A, Sanz MA, Abella E, Tormo M, Del Potro E, et al. Results of PETHEMA ALL96 protocol for standard risk adult ALL patients. Hematology J. 2004;5 Suppl 2:134. 13. Ribera JM, Oriol A, Bethencourt C, Parody R, Hernández-Rivas JM, Moreno MJ, et al. Comparison of intensive chemotherapy, allogeneic or autologous stem cell transplantation as post-remission treatment for adult patients with highrisk acute lymphoblastic leukemia. Results of the PETHEMA ALL-93 trial. Haematologica. 2005;90:1346-56. 14. Ribera JM, Ortega JJ, Oriol A, Bastida P, Calvo C, Pérez-Hurtado JM, et al. Comparison of intensive chemotherapy, allogeneic, or autologous item-cell transplantation as postremission treatment for children with very high risk acute lymphoblastic leukemia: PETHEMA ALL-93 Trial. J Clin Oncol. 2007;25:16-24. 15. Oriol A, Ribera JM, Esteve J, Sanz MA, Brunet S, García-Boyero R, et al. Lack of influence of human immunodeficiency virus infection status in the response to therapy and survival of adult patients with mature B-cell lymphoma or leukemia. Results of the PETHEMA-LAL3/97 study. Haematologica. 2003;88:445-53. 16. Sancho JM, Ribera JM, Xicoy B, Morgades M, Oriol A, Tormo M, et al. Results of the PETHEMA ALL-96 trial in elderly patients with Philadelphia chromosome-negative acute lymphoblastic leukemia. Eur J Haematol. 2007;78:102-10. 17. Bassan R, Intermesoli T, Di Bona E, Pogliani EM, Rossi G, Fabris P, et al. Central nervous system involvement in adult acute lymphoblastic leukaemia: retrospective analysis from Northern Italy Leukaemia Group (NILG) on 687 total patients (1979-2004). Haematologica. 2005;90:167. 18. Kantarjian H, Thomas D, O’Brien S, Cortes J, Giles F, Jeha S, et al. Long-term follow-up results of hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone (hyperCVAD), a dose-intensive regimen, in adult acute lymphocytic leukemia. Cancer. 2004; 101: 2788-801. 19. Ruutu T, Corradini P, Gratwohl A, Holler E, Apperley J, Dini G, et al. Use of intrathecal prophylaxis in allogeneic haemopoietic stem cell transplantation for malignant blood diseases: a survey of the European Group for Blood and Marrow Transplantation (EBMT). Bone Marrow Transplant. 2005;35:121-4. 20. Pui CH, Mahmoud H, Rivera GK, Hancock ML, Sandlund JT, Behm FG, et al. Early intensification of intrathecal chemotherapy virtually eliminates central nervous system relapse in children with acute lymphoblastic leukemia. Blood. 1998;92:411-5. 21. Hill FG, Richards S, Gibson B, Hann I, Lilleyman J, Kinsey S, et al. Successful treatment without cranial radiotherapy of children receiving intensified chemotherapy for acute lymphoblastic leukaemia: results of the risk stratified randomized central nervous system treatment trial MRC UKALL XI (ISRC TN 16757172). Br J Haematol. 2004;124:33-46. 22. Vilmer E, Suciu S, Fester A, Bertrand Y, Cave H, Thyss A, et al. Long-term results of three randomized trials (58831, 58832, 58881) in childhood acute lymphoblastic leukemia: a CLCGEORTC report. Leukemia. 2000;14:2257-66. 23. Manera R, Ramírez I, Mullins J, Pinkel D. Pilot studies of species-specific chemotherapy of childhood acute lymphoblastic leukemia using genotype and immunophenotype. Leukemia. 2000; 14:1354-61. 24. Surapanemi UR, Cortes JE, Thomas D, O’Brien S, Giles FJ, Koller C, et al. Central nervous system relapse in adults with acute lymphoblastic leukemia. Cancer. 2002;94:773-9. 25. Lazarus HM, Richards SM, Chopra R, Litzow MR, Burnett AK, Wiernik PH, et al. Adult patients with acute lymphoblastic leukemia (ALL) and central nervous system (CNS) leukemia at diagnosis may attain durable complete remissions (CR). Results from the international ALL trial (MRC UKALL-XII/ECOG E2993). Blood. 2004; 104:204b. 26. Nagatoshi Y, Kawano Y, Nagayama J, Okamura J. Treatment of isolated central nervous system relapse in high-risk lymphoid malignancy with allogeneic bone marrow transplantation and extended intrathecal therapy. Br J Haematol. 2004;125:766-8. 27. Messina C, Valsecchi MG, Aricò M, Locatelli F, Rosetti F, Rondelli R, et al, on belhaf of the AIEOP/FONOP-TMO group. Autologous bone marrow trasplantation for treatment of isolated central nervous system relapse of childhood acute lymphoblastic leukemia. Bone Marrow Transplant. 1998;21:9-14. 28. Glantz MJ, Jaeckle KA, Chamberlain MC, Phuphanich S, Recht L, Swinnen LJ, et al. A randomized controlled trial comparing intrathecal sustained-release cytarabine (DepoCyt) to intrathecal methotrexate in patients with neoplastic meningitis from solid tumors. Clin Cancer Res. 1999;5: 3394-402. 29. Jaeckle KA, Phuphanich S, Van den Bent MJ, Aiken R, Batchelor T, Campbell T, et al. Intrathecal treatment of neoplastic meningitis due to breast cancer with a slow-release formulation of cytarabine. Br J Cancer. 2001;84:157-63. 30. Jaeckle KA, Batchelor T, O’Day SJ, Phuphanich S, New P, Lesser G, et al. An open label trial of sustained-release cytarabine (DepoCytTM) for the intrathecal treatment of solid tumor neoplastic meningitis. J Neurooncol. 2002;57:231-9. 31. Glantz MJ, LaFollette S, Jaeckle KA, Shapiro W, Swinnen L, Rozental JR, et al. Randomized trial of a slow-release versus a standard formulation of cytarabine for the intrathecal treatment of lymphomatous meningitis. J Clin Oncol. 1999;17: 3110-6. 32. Kim S, Chatelut C, Kim JC, Howell SB, Cates C, Kormanik PA, et al. Extended CSF cytarabine exposure following intrathecal administration of DTC 101. J Clin Oncol. 1993;11:2186-93. 33. Chamberlain MC, Kormanik P, Howell SB, Kim S. Pharmacokinetics of intralumbar DTC 101 for the treatment of leptomeningeal metastases. Arch Neurol. 1995;52:912-7. 34. Sommerfeld SA, Radford JA, Dennis MW. Administration of sustained release intrathecal cytarabine for neoplastic meningitis – a single centre experience. Haematologica. 2005;90:297. 35. Giménez E, Bustelos R, De la Serna J, Grande C. Intrathecal liposomal cytarabine (DepoCyte®) as treatment for CNS infiltration in an adult woman with acute myeloid leukaemia. Bone Marrow Transplant. 2005;35 Suppl 2:378. 36. Sancho JM, Ribera JM, Romero MJ, Martín-Reina V, Giraldo P, Ruiz E. Compassionate use of intrathecal depot liposomal cytarabine as treatment of central nervous system involvement in acute leukaemia: report of 6 cases. E-case Haematologica. 2006;91:(ECR)02. Available in: http:// www.haematologica.org/online/2006/ECR02/index.html 37. Bomgaars L, Geyer JR, Franklin J, Dahl G, Park J, Winick NJ, et al. Phase I trial of intrathecal liposomal cytarabine in children with neoplastic meningitis. J Clin Oncol. 2004;22:3916-21. 38. Goekbuget N, Bassan R, Hug S, Jentsch-Ullrich K, Rutjes J, Matthias S, et al. First promising results from an European trial with liposomal cytarabine (DepoCyte®) for intrathecal (i.th.) application in CNS relapse of acute lymphoblastic leukemia (ALL) or very aggressive lymphoma (vaNHL). Ge- Documento descargado de http://www.elsevier.es el 21/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. SANCHO JM ET AL. PRACTICE OF CENTRAL NERVOUS SYSTEM PROPHYLAXIS AND TREATMENT IN ACUTE LEUKEMIAS IN SPAIN. PROSPECTIVE REGISTRY STUDY meinsame Jahrestagung der [abstract 789]. Proceedings of Deutschen Österreichischen und Schweizerischen Gesellschaften für Hämatologie und Onkologie; 2005, Oktober 1-5; Hannover. 39. Sancho JM, Deben G, Parker A, Piñana JL, Bolam S, Sánchez-García E, et al. Results of compassionate therapy with intrathecal depot liposomal cytarabine in acute myeloid leukemia meningeosis. Int J Hematol. 2007;86:33-6. 40. McClune B, Buadi F, Aslam N, Przepiorka D. Intrathecal liposomal cytarabine (Depocyt) is safe and effective for prevention of meningeal disease in patients with acute lymphoblastic leukemia and high-grade lymphoma treated with the HyperCVAD regimen. Blood. 2005;106: 227b-8b. 41. Jabbour E, O’Brien S, Kantarjian H, García-Manero G, Ferrajoli A, Ravandi F, et al. Neurologi- 260.433 CRÍTICA DE LIBROS Manual básico de cirugía bariátrica para internistas clínicas médicas de Norteamérica Editado por Nilesh A. Patel, Lisa S. Koche. Barcelona: Elsevier; 2007. 215 páginas. Los primeros tres capítulos del libro son básicos para un internista: «Conocer el impacto económico de la obesidad», «La evaluación preoperatoria o la asistencia perioperatoria del paciente intervenido» y el manual básico para el internista de las distintas técnicas en cirugía bariátrica. Sólo con este conocimiento, podrá colaborar con cualquier unidad dedicada a esta enfermedad. El cuarto capítulo es interesante, pues se adentra en el paciente que ya ha sufrido infinidad de tratamientos médicos y sus fracasos y exige ser intervenido. Los autores también encuadran su proyecto en la mujer fértil intervenida de su obesidad, que puede presentar problemas en el seguimiento a largo plazo, bien sea por la hipoabsorción de anticonceptivos, bien por carencias de vitamina B (para ella o el feto) o de ácido fólico, con posibles lesiones neuronales. ¿Y por qué no conocer los aspectos metabólicos que tan bien conocen hoy día los cirujanos que se dedican a este tema? ¿Quién iba a decir que el mejor tratamiento de la diabetes del adulto es la cirugía metabólica o que la hipoglucemia hiperinsulinémica endógena, es decir la neuroglucopenia, es una consecuencia de una hipersecreción de GLP-1? Una revuelta a la normalidad en un metabolismo mal encaminado en el obeso. El impacto de la cirugía en el paciente obeso con trastorno cardiovascular es tremendo. En este siglo, un cardiólogo debe conocer qué son las adipocinas (leptina y adiponectina) si no quiere perder el concepto de la nueva fisiopatología cardiovascular de sus pacientes. La obesidad, además de un problema de peso, es una enfermedad de inflamación sistémica. El obeso presenta cambios moleculares y anatómicos con sus consecuencias: asma, apnea obstructiva del sueño, síndrome de hipoventilación e hipertensión pulmonar. Esta es la ganancia final pero, para que toda vaya bien, hay que reconocer que el obeso es un enfermo que precisa una evaluación cuidadosa, multidisciplinaria, antes y después de la cirugía bariátrica. La conclusión final es simple y cal complications associated with intrathecal liposomal cytarabine given prophylactically in combination with high dose methotrexate and cytarabine to patients with acute lymphocytic leukemia. Blood. 2007;109:3214-8. 42. Castagnola C, Nozza A, Corso A, Bernasconi C. The value of combination therapy in adult acute myeloid leukemia with central nervous system involvement. Haematologica. 1997;82:577-80. demoledora: la cirugía para perder peso parece ser inestimable en el tratamiento de la disfunción pulmonar relacionada con la obesidad. Al médico de atención primaria le acudirán pacientes intervenidos en quienes las consecuencias de la técnica y el diseño le incomodarán. La esteatohepatitis no alcohólica, la incidencia de litiasis postoperatorias, reflujo gatroesofágico si el paciente lleva una banda gástrica, son ejemplos de lo que se avecina. Muchos trastornos nuevos como la oclusión, la hernia interna o la invaginación, los aporta la propia técnica y por el sólo hecho de haber sido intervenidos. Es necesario e imprescindible el papel de un psicólogo en la valoración preoperatoria y todavía lo es más en el control postoperatorio de algunos pacientes. Las consecuencias de la intervención son impredecibles y particulares y, por consiguiente, es necesario tener la posibilidad de dirigir a quien lo precise, y pueden ser muchos, a un profesional que conozca el tema. La experiencia de los autores de este capítulo, en la que expresan su valoración de 2.500 pacientes candidatos a este tipo de cirugía, merece ser leída y tenida en cuenta. Muchas de las complicaciones de las 250.000 intervenciones que posiblemente se realizarán en Estados Unidos en el próximo año presentarán complicaciones. El médico que ha derivado a un determinado paciente a un centro de excelencia en este tipo de técnicas deberá cargar luego con el control ambulatorio de ese paciente. Ése va a ser el pacto. La incidencia, la presentación clínica y el tratamiento de las complicaciones frecuentes deberán ser tenidas en cuenta y, sobre todo, conocidas por los médicos responsables. ¿Cómo resolverá un médico de asistencia primaria una ictericia obstructiva si al paciente no se le puede realizar una colangiografia retrógrada endoscópica? ¿Cómo tratará una esofagitis por candidas o una discinesia biliar? Y, sobre todo, ¿qué hará cuando el paciente presente una gastroenteritis grave en un intestino corto o, simplemente, como suele pasar, recupere parte del peso perdido con el tiempo y le pregunte por qué? En cuanto al capítulo de las complicaciones de la banda gástrica, aunque el autor lo defina como un tratamiento nuevo y prometedor, lo cierto es que ya se conocen sus efectos y su consecuencias, no muy buenas. Ajuste y reversibilidad son dos premisas que venden el proceso, pero lo cierto es que es mejor remitirlos de nuevo a su cirujano, pues un médico de asistencia primaria sólo puede hacer eso. Su cirujano, si se ha complicado el proceso, debe retirar la banda. Otra cosa es si en el año 2008 hay alguna indicación para colocar una banda gástrica. La obesidad es una forma de desnutrición. La desnutrición es una consecuencia en muchos pacientes de las técnicas hipoabsortivas, cada vez más agresivas, que se realizan. Vitaminas y minerales de por vida. En este penúltimo capítulo del libro, los autores a quienes corresponde esta tarea se adentran en reconocer la desnutrición provocada y por ello es importante un estricto seguimiento por el equipo multidiciplinario y dietético, pues todos sabemos que más del 50% de los pacientes presentarán algún grado de mala nutrición. Y saben una cosa: muchos pacientes dejan de acudir al seguimiento programado. Y finalmente, el último capítulo, donde los autores afirman que existe una incidencia relativamente baja de complicaciones relacionadas con el embarazo en pacientes que han sido intervenidas. Macrosomía, hipertensión inducida por el embarazo, preeclampsia y diabetes gestacional, frecuentes en una madre obesa, son inferiores si el peso se normaliza y similares a las mujeres no obesas de la población general. Aun así, se recomienda retrasar cualquier embarazo 2 años, aunque puede ser difícil pues no existe consenso en cómo conseguirlo. Naturalmente, otro efecto beneficioso se verifica en las pacientes con ovarios poliquísticos o con esterilidad. Ambas afecciones mejoran con una normalización del peso. Aunque estas beneficiosas consecuencias no deben ser consideradas como una indicación de la cirugía, sí que pueden valorarse como ganancia secundaria significativa para pacientes prospectivas. En fin, hay que ver lo que están dando de sí la obesidad y la cirugía. Los internistas, a quienes va dirigido este libro, deben leerlo con atención, pues muchos de los pacientes intervenidos serán los suyos. Solamente una última observación. Aconsejaría a los autores añadir junto al concepto de bariátrica, la denominación de metabólica. Antoni Alastrué Vidal Unidad Hepatobiliopancreática, Metabólica-Obesidad, Endocrino. Hospital Germans Trias i Pujol. Badalona. Barcelona. España. Med Clin (Barc). 2008;131(11):401-5 405