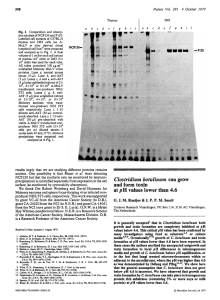
SIMULTANEOUS BOTULISM IN TWO BROTHERS ADDICTED TO
Anuncio

ARCH SOC ESP OFTALMOL 2007; 82: 583-586 SHORT COMMUNICATION SIMULTANEOUS BOTULISM IN TWO BROTHERS ADDICTED TO COCAINE BOTULISMO SIMULTÁNEO EN DOS HERMANOS COCAINÓMANOS AGUIRRE-BALSALOBRE F1, GONZÁLEZ-HERRERA M1, MENGUAL-VERDÚ E2, GARCÍA-CONCA V1, HUESO-ABANCENS JR2 ABSTRACT RESUMEN Introduction: Botulism is currently an uncommon disease in which the botulinum toxin causes a progressive muscular paralysis that can lead to the death due to a failure of respiratory muscles. Clinical case: Two brothers, both addicted to cocaine, came to the casualty department because of a decrease of near visual acuity and bilateral mydriasis. Two days later, they developed eyelid ptosis, asymmetric dysfunction of the extraocular muscles and vomiting. Discussion: The presence of a paralysis of accommodation, with bilateral mydriasis that reacts to pilocarpine, makes it necessary to consider botulism as a possible cause (Arch Soc Esp Oftalmol 2007; 82: 583-586). Introducción: El botulismo es poco frecuente en la actualidad. La toxina botulínica produce una parálisis muscular progresiva que puede producir la muerte del paciente por parada de los músculos respiratorios. Caso clínico: Dos pacientes hermanos, adictos a la cocaína, acudieron al Servicio de Urgencias por disminución de la agudeza visual cercana, con midriasis bilateral. A los dos días presentaban, además, ptosis palpebral, disfunción asimétrica de la motilidad ocular extrínseca, y vómito. Discusión: Ante la presencia de una parálisis de la acomodación con una midriasis bilateral que responde a pilocarpina, se debe considerar el botulismo como una posible etiología. Key words: Botulism, pupil disorders, pupillary reflex, cocaine abuse, mydriasis. Palabras clave: Botulismo, alteraciones pupilares, reflejos pupilares, abuso de cocaína, midriasis. Received: 31/5/06. Accepted: 25/7/07. San Juan de Alicante University Hospital. Alicante. Spain. 1 Graduate in Medicine. 2 Ph.D. in Medicine. Correspondence: Fernando Aguirre Balsalobre Servicio de Oftalmología Hospital Universitario San Juan de Alicante Ctra. Ncnal. 332 Alicante-Valencia, s/n Apartado de correos, 41 03550 San Juan de Alicante (Alicante) Spain E-mail: [email protected] AGUIRRE-BALSALOBRE F, et al. INTRODUCTION Botulism is a neuroparalytic disorder caused by Clostridium botulinum’s exotoxins. It is a rare disease, diagnosing 10 to 50 cases per year in Spain (1). The usual way for contracting this disease in adult patients is through food poisoning, generally caused by the intake of home-made food preserves not previously cooked and manufactured at least eight days before, or else induced by penetrating cutaneous wounds. Depending on the amount present in the body, the first symptoms appear from twelve hours to eight days later. This toxin blocks muscle contractions by blocking the release of preganglionic acetylcholine in the neuromuscular plate, which leads initially to ocular alterations such as non-reactive mydriasis, palpebral pthosis or oculomotor nerve palsy dyplopia. Subsequently, weakness due to muscular palsies expands, leading to respiratory failure and death of the patient (1,2). The diagnosis is made by detecting the toxin in serum or other body fluids. Treatment consists of eliminating the toxin from the digestive tract, administering an antitoxic serum, penicillin G and providing breathing support. Symptoms will revert in the opposite order as they occurred (1,2). CASE REPORT Two brothers, aged 38 and 42, arrived in the emergency room reporting blurry vision for the past 24 hours, and worse near vision. They did cocaine regularly, and linked the current symptoms to it, since they had just changed providers the day before. In both cases, far visual acuity had been preserved (0.8), but near visual acuity stood below 0.4. Their bilateral non-reactive mydriasis (figs. 1 and 2) returned in a few minutes after instilling 1% pilocarpine. Extrinsic ocular movements and convergence, just as the remaining exploration, were normal. They arranged an appointment for check-up and were diagnosed with possible mydriasis due to drug tampering. Two days later, the symptoms included bilateral palpebral pthosis and dyplopia. There was limited abduction of both eyes, while the remaining gaze cardinal positions were only partially restricted. Furthermore, both patients suffered from nauseas, vomits, dysphagia and micturition difficulties. Deepening the anamnesis, the patients reported they had eaten home-made cardoon preserves two days before the onset of symptoms. The likelihood of poisoning caused by Clostridium botulinum was suggested. The cranial image testing performed (computed axial tomography) was normal. However, the electromyograms revealed blocking at the level of the muscular motor plate, prompting the administration of botulinum antitoxin. The youngest brother required in-hospital care during eighteen days, twenty-nine days for the eldest, who required mechanical ventilation. Toxin detection in the faeces was negative in both patients. Ocular pathologies remitted completely and in the reverse order. Mydriasis did not fully disappear forty days after the onset (figs. 1 and 2), and improvement Fig. 1: Bilateral mydriasis in the eldest brother, in worse condition, three weeks after the onset of symptoms. 584 ARCH SOC ESP OFTALMOL 2007; 82: 583-586 Botulism in cocaine addicts Fig. 2: Mydriasis in the younger brother three weeks after the onset of symptoms. occurred earlier than in the youngest brother, who suffered the less acute condition (figs. 3 y 4). DISCUSSION Faced with a fixed pupilary mydriasis without prior trauma, we must first discard as the most frequent cause pupilary dilation by means of eye drops or vegetal products, whether by accident or willingly. It is also important to assess extrinsic and palpebral ocular movements in case the cause was palsy of the II cranial nerve. If the biomicroscopy reveals an irregular pupil in the context of a mydriasis slowly reactive to light, the most probable diagnosis would be Adie’s pupil (3). The instillation of topical pilocarpine facilitates diagnosis. Any pupil subjected to the instillation of a parasympathetic agent may react or react slightly to 1% pilocarpine. Adie’s pupil contracts at low doses of 0.125% pilocarpine, whereas the III nerve palsy tends to react to higher doses. The two last pathologies are more frequently unilateral than pharmacological mydriasis (3). Accommodation should be taken into consideration. A bilateral mydriasis cannot be attributed to cocaine (sympathetic stimulation) when there is an accommodation disorder because of parasympathetic blockers (4,5). Even though botulism is extremely rare, when faced with a bilateral mydriasis that reacts to pilocarpine one should question the patient regarding any potential relevant food-related history. Whenever in doubt, the patient should be immediately referred for electromyographic examination. The botulum antitoxin should be administered early on, Fig. 3: Palpebral pthosis and weak ocular movements in the eldest brother three weeks after the onset of symptoms. ARCH SOC ESP OFTALMOL 2007; 82: 583-586 585 AGUIRRE-BALSALOBRE F, et al. Fig. 4: Lesser degree pthosis and lower limitation of ocular movements in the youngest brother three weeks after the onset of symptoms. even if the presence of toxins in the body or food has not been confirmed, which sometimes may be the case. In other words, early diagnosis of this pathology is crucial for the vital prognosis of patients, thus the significance of taking it into account in the differential diagnosis of bilateral mydriasis. 2. 3. 4. REFERENCES 1. Torrabadella de Reynoso P, Piédrola Angulo G, Prat Aymerich C, Vallés Casanova X. Infecciones causadas por 586 5. bacterias anaerobias esporuladas. In: Farreras, Rozman. Medicina Interna. 14th Ed. Madrid: Harcourt; 2000; II: 2632-2640. Caya JG. Clostridium botulinum and the ophthalmologist: a review of botulism, including biological warfare ramifications of botulinum toxin. Surv Ophthalmol 2001; 46: 25-34. Savino PJ, Sergott RC. Neurooftalmología. In: Rhee, Pyfer. Manual de Urgencias Oftalmológicas. 3rd Ed. Philadelphia: Mc Graw-Hill Interamericana; 2001; 301-364. Penas SC, Faria OM, Serrao R, Capao-Filipe JA, MotaMiranda A, Falcao-Reis F. Ophthalmic Manifestations in 18 patients with botulism diagnosed in Porto, Portugal between 1998 and 2003. J Neuroophthalmol 2005; 25: 262-267. Simcock PR, Kelleher S, Dunne JA. Neuro-ophthalmic findings in botulism type B. Eye 1994; 8: 646-648. ARCH SOC ESP OFTALMOL 2007; 82: 583-586