- Ninguna Categoria
Cerebral perfusion scintigraphy study as confirmation test of brain
Anuncio
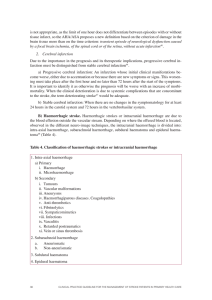
Documento descargado de http://www.elsevier.es el 18/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. Rev Esp Med Nucl Imagen Mol. 2012;31(5):278–285 Special collaboration Cerebral perfusion scintigraphy study as confirmation test of brain death in the process of organ donation for transplant夽 El estudio gammagráfico de perfusión cerebral como prueba de confirmación de muerte encefálica en el proceso de donación de órganos para trasplante J. Banzo a,∗ , P. Razola a , J.J. Araíz b , J. Larraga b , L. Tardín a , A. Andrés a , A. Santapau a , A. Parra a , E. Rambalde a , S. Ayala a , E. Prats a a b Servicio de Medicina Nuclear, Hospital Clínico Universitario Lozano Blesa, Zaragoza, Spain Unidad de Cuidados Intensivos, Coordinación de trasplantes, Hospital Clínico Universitario Lozano Blesa, Zaragoza, Spain “Death is a human cultural event as are the criteria of death. It is man who says what is life and what is death and elaborates definitions which may change with time. Ethicists and physicians may educate society on the scientifically safe and philosophically defendable conceptions of death, but where to draw the line of separation between life and death is a decision which must be made by society as a whole and be regulated by legislation and social principles.” D. Gracia. Vida y muerte: Bioética en el trasplante de órganos. 1995 (Life and death: bioethics of organ transplantation). Introduction Until the introduction of life support measures at the end of the 1950s the close interrelation between encephalic, respiratory and cardiac functions was such that the discontinuation of one of these functions entailed the interruption of the others. The constitution of intensive care units (ICU) demonstrated that the classical criteria defining death as irreversible cardiorespiratory arrest was not adequate in patients with irreversible cerebral and encephalic trunk lesions connected to life support systems. In this new scenario the concept of death had to be redefined, with the Ad Hoc Committee of the Harvard Medical School introducing the term brain death in the medical terminology,1 which has currently been substituted by encephalic death (ED). On the other hand, the technological advances allowing organ transplantation almost simultaneously led to the need for obtaining viable organs from donors who had died without reaching irreversible cardiorespiratory arrest. The legal definition of death had to be modified, elaborating criteria based on “the definitive loss of all the vital neurological signs”: arreactive coma, absence of encephalic trunk reflexes and apnea.2 ED is scientifically recognized as the death of the individual and is accepted as such in the legislations of different countries including Spain. According to data published by the Transplant Working Group of the Spanish Society of Critical Intensive Care Medicine and Coronary Units (SEMICYUC),3 14% of the patients who die in the ICU do so within a setting of ED, rising to 30% if the ICU is a reference 夽 Please cite this article as: Banzo J, et al. El estudio gammagráfico de perfusión cerebral como prueba de confirmación de muerte encefálica en el proceso de donación de órganos para trasplante. Rev Esp Med Nucl Imagen Mol. 2012;31(5):278–85. ∗ Corresponding author. E-mail address: [email protected] (J. Banzo). center for neurosurgery. The most frequent causes leading to ED are hemorrhagic cerebrovascular accidents and cranioencephalic traumatisms.4 Annex I of the Real Decreto (RD) 2070/19995 of December 30 regulates the activities of clinical obtainment and use of human organs and territorial coordination of matters of organ and tissue donation and transplantation and establishes the diagnostic protocols and certification of death for the extraction of organs from dead donors. Cerebral perfusion scintigraphy with lipophilic tracers able to pass through the intact blood–brain barrier is included as the instrumental test of diagnostic support to evaluate cerebral blood flow (CBF) together with cerebral arteriography, cerebral angiography by digital subtraction and transcranial Doppler sonography (TDS). Protocol of cerebral perfusion scintigraphy: technical aspects Patients The clinical diagnosis of ED should be previously established by complete, systematic neurological examination together with atropine and apnea tests. The patients should be hemodynamically stable and not require the interruption of any therapy regimen. During transfer to the Department of Nuclear Medicine (NM) and while planar images are acquired the vital signs must be constantly monitored and mechanical ventilation must be supervised by ICU staff. Prior to initiation of the cerebral perfusion scintigraphy study (CPSS) information should be obtained in all the cases as to the cause of the coma, the situation of the cardiorespiratory function parameters, the presence or not of soft tissue head lesions secondary to traumatism or recent surgery, the situation of the catheter to measure intracranial pressure, when present, and identification, with aid from ICU nursing personnel, of the most adequate venous via for administration of the tracer. Image acquisition Injection of the tracer Both 99m Tc-HMPAO (hexamethyl propylene amine oxime) and (ethyl cysteinate dimer) are accepted as biomarkers of cerebral perfusion6,7 and may be used in the diagnosis of confirmation of ED, although there is greater experience with the former. While the American Academy of Neurology (AAN) only 99m Tc-ECD 2253-8089/$ – see front matter © 2012 Elsevier España, S.L. and SEMNIM. All rights reserved. Documento descargado de http://www.elsevier.es el 18/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. J. Banzo et al. / Rev Esp Med Nucl Imagen Mol. 2012;31(5):278–285 recommends the use of 99m Tc-HMPAO, the American College of Radiology (ACR) and the Society of Nuclear Medicine (SNM) recommend both of the biomarkers of cerebral perfusion indistinctly.8 In the above-mentioned RD it is specified that the scintigraphic examination must be performed with “radiotracers able to pass the blood–brain barrier”. The use of unspecific tracers such as 99m Tc-DTPA (diehyilenetriaminopentaacetic acid) or 99m TcGH (glucoheptonate) is not currently justified. Quality control is mandatory and must determine the efficacy of the labeling by chromatography and should also take into account the stability of the radiotracer preparation. In the particular case of 99m Tc-HMPAO the labeled preparation is eliminated with a lipophilic fraction less than 85%. In our department we use a fixed dose of nonstabilized (925 MBq) 99m Tc-HMPAO in adults which is prepared immediately before administration. The dose in children is calculated following the recommendations of the European Association of Nuclear Medicine.9 Injection of the tracer is performed in a bolus through a central vein immediately followed by a 10 cc injection of physiological saline. Cerebral angioscintigraphy and planar images The dynamic cerebral study is acquired in anterior projection centering the head of the patient slightly flexed on the axial plane of the collimator so that the plane passes through the external angles of the orbits and both external auditory tubes are perpendicular to the plane of the detector. The field of examination should include the head, the neck and the upper third of the thorax. The duration of the dynamic study is 60 s (1 image/s in a matrix 64 × 64) from the instant that the tracer reaches the aortic arch. Immediately after completing the dynamic study the planar images are obtained in anterior, right lateral and left lateral projections with an acquisition time of less than 120 s/image in a matrix of 256 × 256. To acquire the images in lateral projection the head of the patient is turned from the anterior position to situate the sagittal plane of the head parallel to the plane of the collimator continuously controlling the situation of the endotracheal tube. If the external ear makes interpretation of some of the lateral images difficult, they may be repeated by folding the ear forward. We do not recommend systematic SPECT. Evolutive scintigraphic studies In patients in which the CPSS shows persistence of CBF and therefore does not confirm the clinical diagnosis of ED a second CPSS may be carried out after 15 h. Prior to administration of the tracer it is advisable to acquire at least one planar image to know the intensity of the residual hemispheric and/or cerebellous activity resulting from the previous CPSS. When the interval between the first and second CPSS is 15 and 24 h, the dose of the tracer should be increased 20% with respect to the standard dose. Decision making In cases in which the clinical diagnosis of ED is confirmed by CPSS, the NM specialist responsible for the study certifies the death of the patient together with the neurologist or neurosurgeon and the intensive care specialist. If the patient is an organ donor the transplant coordinator activates the donation procedure while the life support measures are withdrawn in cases which are not donors. When the CPSS does not confirm the diagnosis of ED the support measures remain unvariable in the ICU. Table 1 shows the procedure followed in the clinical diagnosis of irreversible coma in a possible organ transplant donor. 279 Legal aspects The diagnosis and certification of ED is of great clinical relevance in the modern health care system in both the cases of organ donation and those not involving donation. The first case allows the availability of viable organs for transplantation, and the second facilitates the withdrawal of all life support measures thereby shortening the time of familial uncertainty and suffering as well as avoiding the sensation of useless effort and pressure on the health care personnel. The Candanchú Report,10 endorsed by the Spanish Society of Neurology, on the neurological diagnosis of brain death states that “suppression of all artificial maintenance of functions is justified after the signing of the death certificate”. The patient does not die as a consequence of the withdrawal of reanimation, and health care is interrupted because the patient is dead. There are not, therefore, two different criteria of the diagnosis of death, one for the organ donor and another for the non-donor; the same criterion is used for two different actions. The promotion of the RD 2070/19995 represented a notable legislative advance compared with the previous RD 426/1980,11 with incorporation, among other things, of the latest scientific advances in the diagnosis of ED. This facilitated the clinical work of the Departments of NM which, as in our case, had been applying scintigraphic techniques in the diagnosis of ED for many years. Escudero et al.4 compared the content of the two RD and noted the contributions of the RD 2070/19995 : 1. Define death following cardiorespiratory and neurological criteria so that the diagnosis and certification of death is based on the confirmation of irreversible cessation of both cardiorespiratory (death by cardiorespiratory arrest) and encephalic (ED) function; 2. Indicate when the hour of death should be registered; 3. Specify the primarily infratentorial disease; 4. Incorporate updated diagnostic protocols; 5. Allow the diagnosis of ED without instrumental tests; and 6. Include specific criteria for the pediatric population. Instrumental tests of diagnostic support are not always obligatory provided that the cause of the coma is known, there is no intolerance to the apnea test, all situations which may hinder or impede examination of encephalic trunk reflexes are excluded such as severe destruction of the facial structure, hypothermia less than 32 ◦ C and intoxication or previous treatment with high doses of central nervous system depressants. However, when these circumstances are present, there is no demonstrated destructive cerebral lesion, the cause of coma is primarily infratentorial or there is intolerance to the apnea test, it is obligatory to at least perform one instrumental diagnostic support test. With respect to the observation period which is different for adults and children and variable according to the etiology of the coma, this period may be shortened by the performance of an instrumental test with conclusive results (Table 2). The possibility of reducing the observation period avoids prolonged hemodynamic maintenance which may lead to functional deterioration or the loss of organs for transplantation. The results of a multicenter study undertaken by Escalante et al.3 showed that 6% of potential organs donors presented cardiac arrest during the obligatory observation period. Along the same line, Lustbader et al.12 recently reported that during the 6-h interval between the first and second neurological examination performed to certify ED following the recommendations of the clinical guidelines elaborated by the New York State Department of Health, 12% of organ donors were lost due to the increase in rejection to organ donation by the relatives or to the presentation of irreversible cardiac arrest. The instrumental diagnostic support tests included in the current legislation evaluate neuronal function (electroencephalogram and evoked potentials) and CBF. CPSS is among the latter group, together with four-vessel cerebral arteriography, cerebral angio- Documento descargado de http://www.elsevier.es el 18/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. 280 J. Banzo et al. / Rev Esp Med Nucl Imagen Mol. 2012;31(5):278–285 Table 1 Cerebral blood flow tests in the process of organ transplant donation. Intensive Care (Clinical diagnosis) - Neurological study - Atropin test - Apnea test - Echo-Doppler Nuclear Medicine (Confirmation) Cerebral perfusion Confirmation Encephalic death Diagnosis of Encephalic death graphy by digital subtraction and TDS. Different authors have defined the qualities to be fulfilled by an ideal instrumental diagnostic support test: availability, rapid, safe, non-invasive, portable, without false positive results or influenced by internal or external factors and inexpensive. Both the technical aspects and the criteria of interpretation should be standardized. In addition, as indicated by Zuckier and Kolano,13 the procedure should be sufficiently robust in itself to confirm or not the clinical diagnosis. Cerebral perfusion scintigraphic study Interpretation criteria Edema and necrosis of the cerebral parenchyma induced by catastrophic lesion of the central nervous system are the cause of the increase in intracranial pressure and the progressive diminishment of perfusion pressure which perpetuate edema and necrosis. Circulatory arrest at the base of the cranium is, therefore, the essential trait of ED and the techniques evaluating CBF are the best candidates for consideration as the reference standard.14 The technical conditions and the interpretation criteria of cerebral study with 99m Tc-HMPAO applied in the diagnosis of ED in both adults and children were defined during the second half of the 1980s and the first years of the following decade,15–19 Posteriorly the procedure was endorsed in different clinical guidelines elabora- Table 2 Observational period (whenever the diagnosis of EDa is only clinical). • Adults - Known destructive lesion: 6 h - Anoxic encephalopathy: 24 h - Intoxication or treatment with CNS depressants: >drug half life Transplant Coordinator (Process of donation) • Children - Preterm neonates: 48 h - Neonates up to 2 months: 48 h - Children from 2 months to 1 year: 24 h -Children from 2 months to 1 year: 24 h -Children from 1 to 2 years: •Anoxic cause: 24 h • Destructive cause: 12 h The observation period may be shortened according to medical criteria, if a diagnostic support test with conclusive results is performed. a ED: encephalic death. Donation? Yes No Transplant Procedure Withdrawal of life support measures ted by recognized, prestigious professional scientific societies.8,20 Studies with 99m Tc-HMPAO progressively replaced cerebral angioscintigraphy with non-diffusible tracers (99m Tc-DTPA or 99m Tc-GH), providing simultaneous reporting of CBF, cerebral perfusion and functional neuronal viability. Although significant differences have been demonstrated in the regional distribution of 99m Tc-HMPAO and 99m Tc-ECD, it is widely recognized that CPSS with one radiotracer or another is a safe, reliable and specific study which does not require any type of patient preparation or have any contraindications, and is also easy to perform, interpret and understand by non-medical personnel (patient relatives and judges) provided that the procedure applied fulfills the optimum standards of quality,13,14,21–24 The use of CPSS allows evaluation of CBF of all the regions of the encephalus and differentiates the situation of low versus absent cerebral blood flow. Moreover, the results are not influenced by the conditions which hinder and limit the clinical diagnosis of ED. Studies with diffusible tracers provide information on functional neuronal viability. Cerebral uptake depends on the transformation of lipophilic molecules to a hydrophilic form which is only possible if neuronal metabolism is preserved.23 In the case of ED, angioscintigraphy demonstrates circulatory arrest at the base of the cranium deriving the blood flow exclusively through the external carotid arteries. The planar images show complete absence of uptake in the cerebral hemispheres, basal ganglia and cerebellum. Dynamic study and the planar images should be evaluated together by a specialist in NM with wide experience in interpreting CPSS following the strict criteria recommended by the NM group of the Hospital Reina Sofía of Córdoba, Spain15,16 any intracranial parenchymatous uptake or image of unclarified doubtful interpretation rules out scintigraphic diagnosis of ED. The use of SPECT is controversial. Authors such as Munari et al.25 reported that cerebral perfusion SPECT should be considered the reference standard in the diagnosis of ED while Al Shammri and Al Feeeli26 described similar results between the planar images and SPECT in a series of 28 patients with clinical diagnosis of ED and did not recommend routine use. It could be argued that SPECT would facilitate the interpretation of doubtful planar images, which are mostly related to increased uptake in soft tissue or with anatomical variants which modify the usual pattern of tracer biodistribution. In clinical practice it is not difficult to identify as such any extracerebral uptake without the need to perform SPECT (Fig. 1 of Annex 1) and, additionally, it is questionable whether SPECT allows evaluation of encephalic trunk perfusion.8 The length of time a patient remains Documento descargado de http://www.elsevier.es el 18/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. J. Banzo et al. / Rev Esp Med Nucl Imagen Mol. 2012;31(5):278–285 Table 3 Patients and etiology of the coma (period January 2000–August 2011). • Patients: 305 - Women: 108 - Men: 197 - Excluded: 3a • Age - 1 day–86 years • Donors: 202 • Etiology of the coma - Cerebrovascular accident: 174 • Hemorrhagic: 145 • Ischemic: 29 - Cranioencephalic traumatism: 95 - Anoxic encephalopathy: 9 - Cerebral tumor surgery: 6 - Others: 16 - No clinical history: 2 281 Table 4 Recommendations for performing and interpreting a CPSS. • Perform the procedure following the standard optimum quality (radiotracer preparation and image acquisition). • Interpret the vascular phase (dynamic study) and parenchymatous images (planar images) together. • Carefully evaluate the posterior fossa in the lateral projections. • Identify any extracerebral activity. • Interpret according to strict criteria: any intracranial parenchymatous uptake rules out the diagnosis of encephalic death. a CPSS: Cerebral perfusion scintigraphic study. One patient had a cardiac arrest few seconds after administration of the tracer. a In 2 patients the clinical record was not available. in the Department of NM should be as short as possible and if SPECT is performed, acquisition of planar images should be avoided.27 Experience of the Department of Nuclear Medicine, HCU Lozano Blesa Table 3 shows the etiology of coma in 302 patients with clinical diagnosis of ED in whom CPSS was performed during the period from January 2000 to August 2011. Hemorrhagic cerebrovascular accidents and cranioencephalic traumatisms predominated. The etiology of the coma was not determined in only two patients. The patterns of cerebral perfusion found were: - I: absence of CBF in the dynamic study and supra- and infratentorial uptake in the planar images in 270 patients (Figs. 1–3 of Annex 1). - II: CBF was not detected in the dynamic study with limited uptake in the infratentorial compartment in the planar images in 10 patients (Figs. 2 and 3B of Annex 1). - III: detection of CBF in the dynamic study with uptake exclusively localized in the cerebral hemispheres of 7 patients (Figs. 4 and 5 of Annex 1). - IV: detection of CBF with supra- and infratentorial uptake in 15 patients (Fig. 4 of Annex 1). In most of the patients with types III and IV perfusion patterns more or less extensive uptake defects were observed in the planar images related to destructive lesions identified in the CT. The clinical diagnosis of ED was confirmed and certification was firstly initiated in the 270 patients presenting the type I pattern, while the diagnosis of ED was not confirmed in the remaining 32 patients (10.59%) with type II, III or IV perfusion patterns. In 23 of these 32 patients a second CPSS (Fig. 6 of Annex 1) was performed. In 21 patients the perfusion pattern was modified to a type I pattern (Fig. 7 of Annex 1) while no changes were observed in the other 2 patients. One of these patients with persistence of CBF died in the ICU several days later and the other, a full term neonate, was discharged with the diagnosis of severe anoxic encephalopathy. Of the 9 patients in whom a second CPSS was not performed, 7 died in the ICU and 2 were discharged, one in a persistent vegetative state and the other, diagnosed with intracranial hemorrhage after extirpation of a suprasellar meningioma, presented severe neurological sequelae (Fig. 8 of Annex 1). When the interval between the first and second CPSS was 15–24 h after the previous procedure, the residual cerebellous and/or hemispheric activity did not make interpretation of either the dynamic study or the planar images difficult in any case. Of the 291 patients in whom the first or the second CPSS con- firmed the diagnosis of ED 202 were organ donors, representing 69.4%. The results obtained show that CPSS is more sensitive than neurological examination and that the planar images are, in turn, more sensitive than cerebral angioscintigraphy. We found discrepancies between the neurological examination and the CPSS results in 10.59% of the patients (Fig. 6 of Annex 1). The group from the Newark University Hospital reported similar results.17 On ruling out situations which make neurological diagnosis difficult, it would have to be assumed that CPSS allows identification of areas of the cerebral parenchyma without necrosis in patients with a clinical diagnosis of ED. These discrepancies are more often seen when the CPSS is obtained immediately after making the clinical diagnosis. In most of the patients with persistence of CBF who have undergone a second CPSS, complete absence of CBF was observed at 24–48 h. The lack of concordance between the neurological and the CPSS has also been reported in pediatric patients and neonates.28 The greater sensitivity of the planar images over angioscintigraphy, in particular, to demonstrate persistence of CBF in the posterior fossa questions the need for a dynamic study. We did not find any patient with persistence of CBF in the angioscintigraphy presenting complete absence of uptake in the planar images. However, in addition to not consuming extra time the dynamic study allows confirmation that the injection of the tracer is correct. The results published based on clinical cases, series of patients, reviews and clinical guidelines do not provide exact knowledge of the sensitivity of CPSS, due to the inclusion of patients with factors which hinder or make clinical diagnosis impossible. With respect to the specificity, the study would have to be performed in patients with destructive cerebral lesions without a clinical diagnosis of ED. In our institution CPSS is indicated to confirm the diagnosis of ED in the following circumstances: 1. Lack of any previous requisite. 2. Incomplete neurological examination. 3. Intolerance to the apnea test. 4. Shortening of the observation period and 5. Judicial patient. Table 4 shows the recommendations we follow and interpretation of the study. Strengths and limitations CPSS is a very reliable study which provides information on the state of encephalic perfusion in terms of neuronal viability. Performance and interpretation of the study is simple, the results are not influenced by factors which limit, hinder or make clinical diagnosis difficult and the images obtained remain registered in a graphic document which is easily comprehensible for non-medical persons. The reviews published in the last years by groups of experts coincide in pointing out that CPSS is a first line examination and is considered the reference standard,28–33 The limitations were classically related to the need for a Department of NM with a Radiopharmacy Unit, displacement of the patient outside the ICU and the limited timetable availability in Documento descargado de http://www.elsevier.es el 18/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. 282 J. Banzo et al. / Rev Esp Med Nucl Imagen Mol. 2012;31(5):278–285 Table 5 Circumstances invalidating or making neurological examination impossible. Circumstances invalidating or making neurological examination impossible A) B) C) D) Severe destruction of the facial structure Intolerance to the apnea test Hypothermia < 32 ºC Intoxication or previous treatment with drugs or CNS depressants E) Destructive infratentorial lesion YES EEG (B and C) Blood flow test* (A,C and D) NO Neurological examination Blood flow test** *Scintigraphic study **To shorten the observation period the Departments of NM. Most of the hospitals with an organ transplant program have a Department of NM and the performance of CPSS does not require specialized or sophisticated detection equipment. The only methodological limitation is the need to transfer the patient outside the ICU, otherwise common to the radiological techniques evaluating cerebral perfusion. If a portable gamma camera or a mini gamma camera used in radioguided surgery is available, it is possible to evaluate the CBF without the need to displace the patient.34 Although the Departments of NM do not do in-hospital extra-timetable duties, in the last decade there has been a trend to increasing the timetable availability of these departments, particularly in the afternoon. In our department, most of the CPSS were performed from 8 and 19 h, that is, within the work day timetable. In regard to examinations requested outside this schedule, weekends and holidays, an agreement may be reached with the hospital management. Other procedures The lack of opacity in the internal carotid arteries above the carotid siphon, of the vertebral arteries from their penetration in the dura mater and the lack of filling of the internal cerebral vein are the cardinal signs to establish the diagnosis of ED by 4-vessel cerebral arteriography. Nonetheless, despite being classically considered as the reference standard, the relative complexity of the procedure, the possible false positive results when the intracranial pressure is not elevated above the perfusion pressure and the potential toxicity of the contrast medium to transplantable organs such as the kidney are factors which advise against their systematic use.30 At present, angio-CT may be an alternative to arteriography since it is less invasive and is widely usable, with scarce dependence of the operator and is rapid to perform. The lack of opacity of the cortical segments of the middle cerebral arteries and the internal cerebral veins are reliable signs to establish the diagnosis of ED.35 False negative results have been reported in patients with anoxic encephalopathy and decompressive craniectomy.36 Despite the recognized advantages of TDS, most authors and institutions which have performed a critical analysis of the different instrumental tests do not recommend this as a procedure of confirmation of ED; the results largely depend on the experience of the operator, with false positive and negative results having been published in 10–15% of the patients, there are limitations in the studies of children and an optimum acoustic window is not found in 20% of the cases,30–33 Nonetheless, despite these limitations and whenever possible we have performed TDS prior to CPSS thereby allowing determination of the most adequate time to carry out the scintigraphic study. Left lateral Anterior. Fig. 1. Extensive subgaleal hematoma in a patient with clinical diagnosis of encephalic death secondary to cranioencephalic traumatism. Recognition of the soft tissue lesions facilitates the interpretation of the dynamic study and the planar images. SPECT is not required to identify the extracerebral uptake (arrows). Documento descargado de http://www.elsevier.es el 18/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. 283 J. Banzo et al. / Rev Esp Med Nucl Imagen Mol. 2012;31(5):278–285 Cerebral angioscintigraphy Cerebral angioscintigraphy No cerebral flow (n=280) Cerebral flow (n=22) Planar images No supra-or infra-tentorial uptake (n=270) Planar images Infra-‐tentorial uptake (n=10) Supra-tentorial uptake (n=7) Type II pattern Type I pattern Supra-and infra-tentorial uptake (n=15) Type III pattern Fig. 2. Types I and II perfusion patterns observed. Type IV pattern Fig. 4. Types III and IV cerebral perfusion patterns observed. Conclusions Cerebral perfusion scintigraphic study may be the diagnostic support test of reference for the diagnosis of confirmation of ED in potential organ transplant donors. Although it does not replace the clinical diagnosis it may be performed when neurological examination or the apnea test cannot be completed or to shorten the observation period (Table 5). Acknowledgments Conflict of interests Annex 1. To Isabel De Haro, Eva María Domingo, Antonio Lastres, María del Mar Muñoz, Ana Sebastián, Patricia Tolosana and Sonia Vicente, Technical Specialists in Nuclear Medicine for their excellent work in performing the cerebral perfusion scintigraphic studies. Figs. 1–8. The authors declare no conflict of interests. A Anterior Left lateral B Right lateral Anterior Left lateral Fig. 3. (A) Gemistocytic grade II astrocytoma. Postsurgical coma. Type I perfusion pattern. Absence of supra- and infra-tentorial uptake. (B) Severe cranioencephalic traumatism due to traffic accident. Type II perfusion pattern. Exclusively cerebellous uptake. The importance of acquiring planar images in lateral projections is of note. Documento descargado de http://www.elsevier.es el 18/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. 284 J. Banzo et al. / Rev Esp Med Nucl Imagen Mol. 2012;31(5):278–285 Right lateral Fig. 5. Cerebellous hemorrhage. Type III perfusion pattern: Persistence of blood flow in both cerebral hemispheres and absence of infratentorial uptake (arrows). Supra-and infratentorial uptake (n=15) Supra-tentorial uptake (n=7) Scintigraphic control (n=23) Death (n=21) Flow (n=2) Death (n=1) Infra-tentorial uptake (n=10) No scintigraphic control (n=9) Death (n=7) Severe anoxic encephalopathy (n=1) ICU discharge (n=1) Persistent vegetative state (n=1) 4 days 35 days Fig. 6. Patients evolution (n = 32) in whom the clinical diagnosis of encephalic death was not initially confirmed by CPSS. B Right lateral Anterior Fig. 8. Postsurgical bleeding in patients operated for suprasellar meningioma. Persistence of supra- and infra-tentorial blood flow. Right fronto-basal perfusion defect in relation to the intraparenchymatous hemorrhage detected in the CT scan. A References 25 hours C Fig. 7. Cranioencephalic traumatism secondary to traffic accident. (A) Type II perfusion pattern: Persistence of blood flow in the infratentorial compartment. (B) The residual cerebellous activity does not impede the interpretation of the CPSS performed 25 h later. (C) Absence of cerebral and cerebellous uptake. 1. A definition of irreversible coma. Report of the Ad Hoc Committee of the Harvard Medical School to examine the definition of brain death. JAMA. 1968;205:337–40. 2. Ara JR. Diagnóstico neurológico de la muerte. Rev Esp Med Nucl. 2001;20:79–81. 3. Escalante JL, Escudero MD, Nolla M, Navarro A. Grupo de Trabajo de Trasplantes de la SEMICYU.C. Muerte encefálica en UCI: epidemiología y métodos diagnósticos. Libro de ponencias XXXI Congreso Nacional de la SEMIUC Castellón. 1996:631–40. 4. Escudero D, Otero J. Avances clínicos y legales en el diagnóstico de muerte encefálica durante la década de los trasplantes en España. Nefrología. 2001;21 Suppl. 4:30–40. 5. Real Decreto 2070/1999 de 30 de diciembre por el que se regulan las actividades de obtención y utilización clínica de órganos humanos y la coordinación territorial en materia de donación y trasplante de órganos y tejidos. BOE. 2000;3:179–90. 6. Arbizu J, Domínguez PD, Díez-Valle R, Vígil C, García-Eulate R, Zubieta JL, et al. Neuroimagen de los tumores cerebrales. Rev Esp Med Nucl. 2011;30:47–65. 7. Martí-Climent JM, Prieto E, López Lapuente J, Arbizu J. Neuroimagen: Fundamentos técnicos y prácticos. Rev Esp Med Nucl. 2010;29:189–210. Documento descargado de http://www.elsevier.es el 18/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. J. Banzo et al. / Rev Esp Med Nucl Imagen Mol. 2012;31(5):278–285 8. Sinha P, Conrad GR. Scintigraphic confirmation of brain death. Semin Nucl Med. 2012;42:27–32. 9. Kapucu OL, Nobili F, Varrone A, Booij J, Borght TV, Nägren K, et al. EANM procedure guideline for brain perfusion SPECT using 99m Tc-labelled radiopharmaceuticals. Eur J Nucl Med Mol Imaging. 2009;36:2093–102. 10. Dictamen de Candanchú 1993 de la Sociedad Española de Neurología. Quadern CAPS. 1994;20:45–6. 11. Real Decreto 426/1980 de 22 de febrero que desarrolla la ley 30/1079 de 27 de octubre sobre Extracción y Trasplante de órganos. BOE. 1980;63:5705–7. 12. Lustbader D, O’Hara D, Wijdicks EFM, MacLean L, Tajik W, Ying A, et al. Second brain death examination may negatively affect organ donation. Neurology. 2011;76:119–24. 13. Zuckier LS, Kolano J. Radionuclide studies in the determination of brain death: criteria, concepts, and controversies. Semin Nucl Med. 2008;38: 262–73. 14. Conrad GR, Sinha P. Scintigraphy as a confirmatory test of brain death. Semin Nucl Med. 2003;33:312–23. 15. de la Riva A, González FM, Llamas-Elvira JM, Latre JM, Jiménez-Hefferman A, Vidal E, et al. Diagnosis of brain death: superiority of perfusion studies with 99m Tc-HMPAO over convencional radionuclide cerebral angiography. Brit J Radiol. 1992;62:289–94. 16. González García FM, de la Riva Aguilar A, Vallejo Casas JA, Robles Arista JC, Infante de la Torre JR, Delgado Acosta F, et al. Medicina Nuclear y diagnóstico de muerte encefálica: angiogammagrafía cerebral con Tc99m-HMPAO Sensibilidad y especificidad diagnóstica. Medicina Intensiva. 2000;24:143–50. 17. Laurin NR, Driedger AA, Hurwitz GA, Mattar AG, Powe JE, Chamberlain MJ, et al. Cerebral perfusion imaging with technetium-99m HM-PAO in brain death and severe central nervous system injury. J Nucl Med. 1989;30: 1627–35. 18. Reid RH, Gulenchyn KY, Ballinger JR. Clinical use of technetium-99m HM-PAO for determination of brain death. J Nucl Med. 1989;30:1621–6. 19. Costa DC, Motteux IMJ, McCready AC. Diagnosis of brain death with technetium 99m hexamethypropylene amino oxime. Eur J Nucl Med. 1991;18:503–6. 20. Donohoe KJ, Frey KA, Gerbaudo VH, Mariani G, Nagel JS, Shulkin B. Procedure guideline for brain death scintigraphy. J Nucl Med. 2003;44:846–51. 21. Asenbaum S, Brücke T, Pirker W, Pietrzyk U, Podreka I. Imagen of cerebral blood flow with technetium-99m-HMPAO and technetium-99m-ECD: a comparison. J Nucl Med. 1998;39:613–8. 285 22. Guerrero Ortiz M, Manrique Legaz A. Papel de la medicina nuclear en el diagnóstico de muerte cerebral. Rev Esp Med Nucl. 2001;20:123–7. 23. Weckesser M, Schober O. Brain death revisited: utility confirmed for nuclear medicine. Eur J Nucl Med. 1999;26:1387–91. 24. de Haro Del Moral FJ, Sánchez Lajusticia A, González García B, Sánchez García M, Chamorro Jambrina C, Suárez Orozco RP, et al. Evaluation of brain scintigraphy with Tc-99m ECD in brain death. Rev Esp Med Nucl. 2008;27:372–3. 25. Munari M, Zucchetta P, Carollo C, Gallo F, De Nardin M, Marzola MC, et al. Confirmatory tests in the diagnosis of brain death: comparison between SPECT and contrast angiography. Crit Care Med. 2005;33:2068–73. 26. Al Shammri S, Al Feeeli M. Confirmation of brain death using brain radionuclide perfusion imaging technique. Med Princ Pract. 2004;13:267–72. 27. Bertagna F, Barozzi O, Puta E, Lucchini S, Paghera B, Savelli G, et al. Residual brain viability, evaluated by (99m)Tc-ECD SPECT, in patients with suspected brain death and with confounding clinical factors. Nucl Med Commun. 2009;30:815–21. 28. Nakagawa TA, Ashwal S, Mathur M, Mysore M. Clinical Report. Guidelines for the determination of brain death in infants and children: an update of the 1987 Task Force recommendations. Pediatrics. 2011;128:e720–40. 29. Joffe AR, Lequier L, Cave D. Specificity of radionuclide brain blood flow testing in brain death: case report and review. J Intensive Care Med. 2010;25:53–64. 30. Heran MKS, Heran NS, Shemie SD. A review of ancillary test in evaluating brain death. Can J Neurol Sci. 2008;35:409–19. 31. Shemie SD, Lee D, Sharpe M, Tampieri D, Young B. Brain blood flow in the neurological determination of death: Canadian expert report. Can J Neurol Sci. 2008;35:140–5. 32. Young GB, Lee D. A critique of ancillary test for brain death. Neurocritical Care. 2004;1:499–508. 33. Scripto PD, Greer DM. An update on brain death criteria. A simple algorithm with complex questions. The Neurologist. 2011;17:237–40. 34. Calvo Morón C, de la Riva Pérez PA, Cambil Molina T, Álvarez Márquez E, Castro Montaño J. Imagen de perfusión cerebral con minigammacámara portátil (Sentinella® ) en muerte cerebral. Rev Esp Med Nucl. 2009;28:83–4. 35. Frampas E, Videcoq M, de Kerviler E, Ricolfi F, Kuoch V, Mourey F, et al. CT angiography for brain death diagnosis. Am J Neuroradiol. 2009;30:1566–70. 36. Escudero D, Otero J, Marqués L, Parra D, Gonzalo JA, Albaiceta GM, et al. Diagnosing brain death by CT perfusion and multislice CT angiography. Neurocrit Care. 2009;11:261–71.
Anuncio
Documentos relacionados
Descargar
Anuncio
Añadir este documento a la recogida (s)
Puede agregar este documento a su colección de estudio (s)
Iniciar sesión Disponible sólo para usuarios autorizadosAñadir a este documento guardado
Puede agregar este documento a su lista guardada
Iniciar sesión Disponible sólo para usuarios autorizados