Variables that influence the indication of a second myocardial
Anuncio
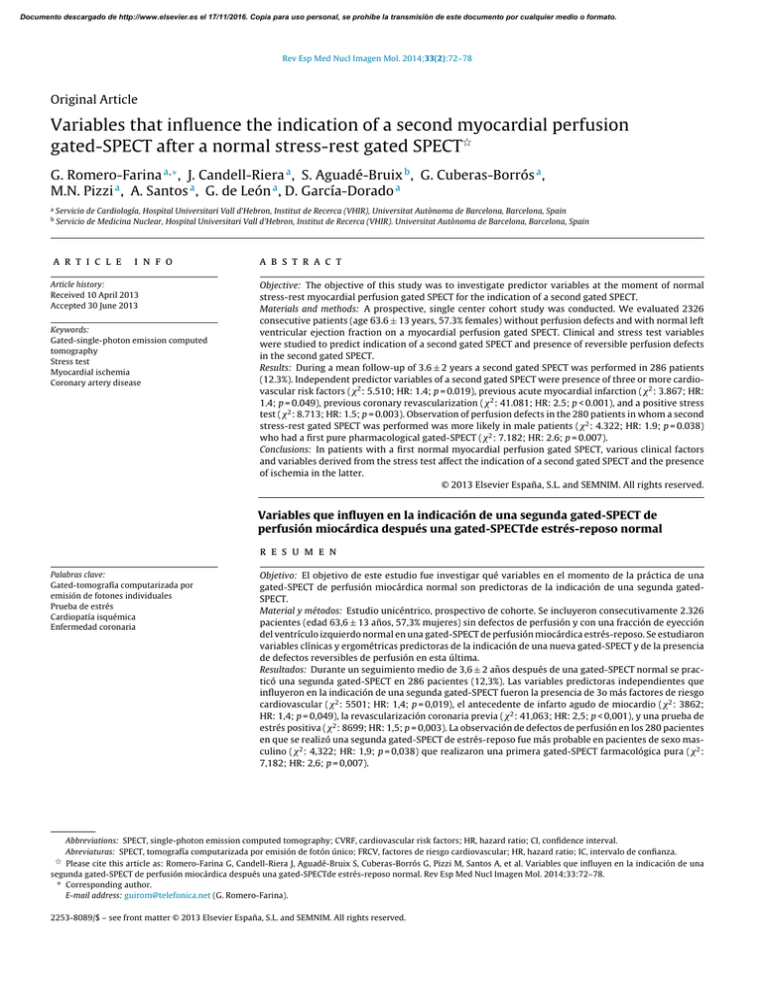
Documento descargado de http://www.elsevier.es el 17/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. Rev Esp Med Nucl Imagen Mol. 2014;33(2):72–78 Original Article Variables that influence the indication of a second myocardial perfusion gated-SPECT after a normal stress-rest gated SPECT夽 G. Romero-Farina a,∗ , J. Candell-Riera a , S. Aguadé-Bruix b , G. Cuberas-Borrós a , M.N. Pizzi a , A. Santos a , G. de León a , D. García-Dorado a a b Servicio de Cardiología, Hospital Universitari Vall d’Hebron, Institut de Recerca (VHIR), Universitat Autònoma de Barcelona, Barcelona, Spain Servicio de Medicina Nuclear, Hospital Universitari Vall d’Hebron, Institut de Recerca (VHIR). Universitat Autònoma de Barcelona, Barcelona, Spain a r t i c l e i n f o Article history: Received 10 April 2013 Accepted 30 June 2013 Keywords: Gated-single-photon emission computed tomography Stress test Myocardial ischemia Coronary artery disease a b s t r a c t Objective: The objective of this study was to investigate predictor variables at the moment of normal stress-rest myocardial perfusion gated SPECT for the indication of a second gated SPECT. Materials and methods: A prospective, single center cohort study was conducted. We evaluated 2326 consecutive patients (age 63.6 ± 13 years, 57.3% females) without perfusion defects and with normal left ventricular ejection fraction on a myocardial perfusion gated SPECT. Clinical and stress test variables were studied to predict indication of a second gated SPECT and presence of reversible perfusion defects in the second gated SPECT. Results: During a mean follow-up of 3.6 ± 2 years a second gated SPECT was performed in 286 patients (12.3%). Independent predictor variables of a second gated SPECT were presence of three or more cardiovascular risk factors (2 : 5.510; HR: 1.4; p = 0.019), previous acute myocardial infarction (2 : 3.867; HR: 1.4; p = 0.049), previous coronary revascularization (2 : 41.081; HR: 2.5; p < 0.001), and a positive stress test (2 : 8.713; HR: 1.5; p = 0.003). Observation of perfusion defects in the 280 patients in whom a second stress-rest gated SPECT was performed was more likely in male patients (2 : 4.322; HR: 1.9; p = 0.038) who had a first pure pharmacological gated-SPECT (2 : 7.182; HR: 2.6; p = 0.007). Conclusions: In patients with a first normal myocardial perfusion gated SPECT, various clinical factors and variables derived from the stress test affect the indication of a second gated SPECT and the presence of ischemia in the latter. © 2013 Elsevier España, S.L. and SEMNIM. All rights reserved. Variables que influyen en la indicación de una segunda gated-SPECT de perfusión miocárdica después una gated-SPECTde estrés-reposo normal r e s u m e n Palabras clave: Gated-tomografía computarizada por emisión de fotones individuales Prueba de estrés Cardiopatía isquémica Enfermedad coronaria Objetivo: El objetivo de este estudio fue investigar qué variables en el momento de la práctica de una gated-SPECT de perfusión miocárdica normal son predictoras de la indicación de una segunda gatedSPECT. Material y métodos: Estudio unicéntrico, prospectivo de cohorte. Se incluyeron consecutivamente 2.326 pacientes (edad 63,6 ± 13 años, 57,3% mujeres) sin defectos de perfusión y con una fracción de eyección del ventrículo izquierdo normal en una gated-SPECT de perfusión miocárdica estrés-reposo. Se estudiaron variables clínicas y ergométricas predictoras de la indicación de una nueva gated-SPECT y de la presencia de defectos reversibles de perfusión en esta última. Resultados: Durante un seguimiento medio de 3,6 ± 2 años después de una gated-SPECT normal se practicó una segunda gated-SPECT en 286 pacientes (12,3%). Las variables predictoras independientes que influyeron en la indicación de una segunda gated-SPECT fueron la presencia de 3o más factores de riesgo cardiovascular (2 : 5501; HR: 1,4; p = 0,019), el antecedente de infarto agudo de miocardio (2 : 3862; HR: 1,4; p = 0,049), la revascularización coronaria previa (2 : 41,063; HR: 2,5; p < 0,001), y una prueba de estrés positiva (2 : 8699; HR: 1,5; p = 0,003). La observación de defectos de perfusión en los 280 pacientes en que se realizó una segunda gated-SPECT de estrés-reposo fue más probable en pacientes de sexo masculino (2 : 4,322; HR: 1,9; p = 0,038) que realizaron una primera gated-SPECT farmacológica pura (2 : 7,182; HR: 2,6; p = 0,007). Abbreviations: SPECT, single-photon emission computed tomography; CVRF, cardiovascular risk factors; HR, hazard ratio; CI, confidence interval. Abreviaturas: SPECT, tomografía computarizada por emisión de fotón único; FRCV, factores de riesgo cardiovascular; HR, hazard ratio; IC, intervalo de confianza. 夽 Please cite this article as: Romero-Farina G, Candell-Riera J, Aguadé-Bruix S, Cuberas-Borrós G, Pizzi M, Santos A, et al. Variables que influyen en la indicación de una segunda gated-SPECT de perfusión miocárdica después una gated-SPECTde estrés-reposo normal. Rev Esp Med Nucl Imagen Mol. 2014;33:72–78. ∗ Corresponding author. E-mail address: [email protected] (G. Romero-Farina). 2253-8089/$ – see front matter © 2013 Elsevier España, S.L. and SEMNIM. All rights reserved. Documento descargado de http://www.elsevier.es el 17/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. G. Romero-Farina et al. / Rev Esp Med Nucl Imagen Mol. 2014;33(2):72–78 73 Conclusiones: En los pacientes con una gated-SPECT de perfusión miocárdica normal diversos factores clínicos y variables derivadas de la prueba de estrés influyen en la indicación de una segunda gated-SPECT y en la presencia de isquemia en esta última. © 2013 Elsevier España, S.L. y SEMNIM. Todos los derechos reservados. Introduction The role of myocardial perfusion stress SPECT (single photon emission computed tomography) in the prognostic staging of patients with or suspected of having coronary disease is well established.1,2 When the result of this study is normal the possibility of presenting severe complications (death of cardiovascular origin or acute myocardial infarction) during the first years is generally lower than 1%,2–9 although different clinical, ergometric variables derived from the stress test are known to modify this percentage. On the other hand, it is relatively frequent for some patients with a normal SPECT to undergo another SPECT during the clinical outcome of the disease, showing perfusion defects in the second study. Taking into account that no previous study has analyzed the variables which may influence the indication for a second gated-SPECT following a previous normal study, the aim of the present study was to analyze the predictive factors for the indication of a second study when the results of the first are normal and determine which factors may be predictive of the positivity of the second gated-SPECT study. Methods Design In a prospective, single center cohort study we included a total of 2326 consecutive patients (age 63.6 ± 13 years, 57.3% females) referred to our Nuclear Cardiology Unit with known or suspected of coronary artery disease or suspicion of the same from 1998 to 2008 with a normal stress-rest myocardial perfusion gated-SPECT. We excluded patients with valvular disease, non-ischemia myocardiopathy as well as those in whom fixed or reversible perfusion defects were observed. We analyzed clinical, ergometric variables, ventricular volumes and the left ventricular ejection fraction by gated-SPECT in all the patients and reviewed the 286 patients (12.3%) undergoing a second myocardial perfusion gated-SPECT according to the criteria of the cardiologist. The study was approved by the Ethical Committee of our hospital. The procedures used in the patients were performed after obtaining informed consent. a semicircular orbit of 180◦ in a step and shoot mode initiated in the right anterior oblique at 45◦ , with detection every 3◦ (25 s). The detection was synchronized with the R wave of the electrocardiogram and the cardiac cycles were divided into 8 fractions. The reconstruction system used was filtered backprojection (Order 5 Butterworth filter, slice frequency 0.4). Correction of attenuation and dispersion was not applied. Left ventricular ejection fraction and the ventricular volumes were automatically calculated in the rest gated-SPECT using the QGS program (Cedars-Sinai Medical Center, Los Angeles, CA, USA). The interpretation of the images was always made by the consensus of 2 experienced observers (one cardiologist and one nuclear physician). A study was defined as normal when no fixed or reversible perfusion defect was present, and the left ventricular ejection fraction was greater than 50%. Statistical analysis The continuous variables were expressed as mean and standard deviation (±) and the categorical variables as percentages. The continuous variables were compared using the Student’s t test for unpaired samples. Differences between percentages were compared with the Chi-square test, and when the number of values expected was lower than 5 the Fisher exact test was used. The differences with respect to the presence of angina, myocardial infarction and coronary revascularization between the first and second SPECT were analyzed with the McNemar test. Different Cox multiple regression models were used for the analysis of the variables predictive of a second gated-SPECT and of myocardial ischemia in the second study. The hazard ratios (HR) with their respective confidence intervals (CI) were evaluated using the stepwise forward (LR) method with a probability of entry and removal of 0.05 and 0.10, respectively. For choosing the final model and calculation of the predictive value the sensitivity, specificity, correct classifications and C statistics of each model were evaluated. The proportionality assumption and the log-linear relationship of each model were compared. The accumulated incidence of a second gated-SPECT was shown in Kaplan–Meier curves. Differences were considered significant with a p < 0.05. All the data were analyzed using the SPSS program for Windows, version 15.0 (SPSS Inc, Chicago, IL, USA) and MedCal® . Stress-rest myocardial perfusion gated-SPECT Results A single day protocol was used for the first and second gatedSPECTs (first the stress and then rest) with technetium compounds (99m Tc-methoxy-isobutyl-isonitryl or 99m Tc-tetrofosmin). In the first gated-SPECT 68.7% of the patients underwent a stress test limited by symptoms, 16.8% did a submaximum + dipyridamole stress test and 13.5% only underwent a pharmacologic test (dipyridamole: 217 patients; dobutamine: 92 patients). In the 286 patients in whom a second SPECT was indicated, 6 were of rest and 280 stress-rest. In these patients 46.6% performed an stress test limited by symptoms, 11.9% a submaximum stress test + dipyridamole, and 11.4% only a pharmacologic test (dipyridamole: 14 patients; dobutamine: 18 patients).10 The first dose of the technetium compound was administered 30–60 s prior to the end of the stress test and was of 8 mCi, and the second dose (rest) was of 24 mCi, with an interval greater than 45 min between each. The equipment used was a Siemens dual head E.CAM gamma camera in a 90◦ configuration with high resolution collimator with Table 1 shows the clinical characteristics of the patients at the time of the first gated-SPECT in the 2326 patients (age 63.6 ± 13 years, 57.3% females) included in the study. During the mean inter SPECT follow-up of 3.6 ± 2 years a second gated-SPECT was performed in 280 (12%) of the patients (mean age 63.3 ± 10 years, 49% females). In the patients undergoing the second gated-SPECT the prevalence of previous myocardial infarction (16.15 vs. 9.4%; p < 0.001) and coronary revascularization (25.9 vs. 10%; p < 0.001) was significantly greater than in those in whom a second gatedSPECT was not indicated. The mean time to perform a second gated-SPECT in the patients with known coronary artery disease was slightly, albeit not significantly, lower than in the patients without previous coronary artery disease (1.9 vs. 2.2 years; p = 0.114). All the patients in whom a second gated-SPECT was performed were symptomatic with chest pain; 7.5% of these patients presented acute myocardial infarction and 14.6% underwent Documento descargado de http://www.elsevier.es el 17/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. 74 G. Romero-Farina et al. / Rev Esp Med Nucl Imagen Mol. 2014;33(2):72–78 Table 1 Characteristics of the patients at the time of the first normal gated-SPECT. Global 2326 1 SPECT n = 2040 2 SPECTs n = 286 p Age (years) BMI Males (%) Diabetes mellitus (%) Arterial hypertension (%) Hypercholesterolemia (%) Smoking (%) 1 CVRF (%) 2 CVRF (%) CVRF ≥3 63.5 ± 13 28.2 ± 16 993 (42.7) 419 (18) 1371 (58.9) 1121 (48.2) 753 (32.4) 709 (30.5) 821 (35.3) 423 (18.2) 63.6 ± 13 28.1 ± 14 847 (41.5) 354 (17.4) 1195 (58.6) 960 (47.1) 649 (31.8) 630 (30.9) 725 (35.5) 347 (17) 63.3 ± 10 29.8 ± 15 146 (51) 65 (22.7) 176 (61.5) 161 (56.3) 104 (36.4) 79 (27.6) 96 (33.6) 76 (26.6) 0.731 0.243 0.002 0.027 0.341 0.003 0.124 0.262 0.513 <0.001 Clinical history Previous AMI (%) Previous CR (%) Angina (%) Chest pain (%) 237 (10.2) 279 (12) 246 (10.6) 2080 (89.4) 191 (9.4) 205 (10) 207 (10.1) 1833 (89.9) 46 (16.15) 74 (25.9) 39 (13.6) 247 (86.4) <0.001 <0.001 0.072 0.072 ECG LBBB (%) PM (%) 78 (3.4) 21 (0.9) 63 (3.1) 19 (0.9) 15 (5.2) 2 (0.7) Type of stress ST (%) ST + PHARM (%) PHARM (%) Positive ST (%) 1640 (70.5) 377 (16.2) 309 (13.3) 422 (18.1) 1421 (69.7) 343 (16.8) 276 (13.5) 347 (17) 219 (76.6) 34 (11.9) 33 (11.5) 75 (26.2) Gated-SPECT LVEF (%) TDV (ml) TSV (ml) 65 ± 151 76.7 ± 40.3 31.3 ± 22.2 64.9 ± 15.4 76.9 (25) 31.6 (20) 66.3 ± 13 74.8 (27) 28.6 (15) 0.058 0.698 0.016 0.034 0.353 < 0.001 0.103 0.399 0.115 1 SPECT: patients only undergoing the first normal SPECT. 2 SPECTs: patients undergoing the second SPECT, LBBB: left bundle branch block, PHARM: pharmacologic test, LVEF: left ventricular ejection fraction, CVRF: cardiovascular risk factors; AMI: acute myocardial infarction, BMI: body mass index, PM: pacemaker, ST: stress test, CR: coronary revascularization, TDV: telediastolic volume, TSV: telesystolic volume. coronary revascularization gated-SPECT study. between the first and second Predictors of a second gated-SPECT In the univariate analysis the percentages of males, patients with diabetes mellitus, hypercholesterolemia, ≥3 cardiovascular risk factors (CVRF), a history of previous myocardial infarction, previous coronary revascularization who did exercise and those with a positive clinical stress and/or electrocardiogram for myocardial ischemia were significantly higher in the patients in whom a second gated-SPECT was indicated (Table 1). In the Cox multivariate analysis (constituted by the 12 variables in Table 2) the predictive variables (C statistics: 0.61 [CI 95%: 0.58–0.62] p < 0.001; sensitivity: 72% [CI 95%: 66–76.8]; specificity: 50% [CI 95%: 45.9–50.3] for a second gated-SPECT (−2 Log likelihood, 4094.6; 2 : 85,494; p < 0.001) were (Table 2) ≥3 CVRF (HR: 1.4; p = 0.019), a history of myocardial infarction (HR: 1.4; p = 0.049), previous coronary revascularization (HR: 2.5; p < 0.001) and a positive stress test (HR: 1.5; p = 0.003). Fig. 1 shows the Kaplan–Meier curves of these predictors during the follow-up after the first normal gated-SPECT. With respect to the reference category (without predictors of a second SPECT), the HR for one predictor was 2.1 (CI 95%: 1.6–2.8; 2 : 25,926; p < 0.001), being 2.6 (CI 95%: 1.9–3.6; : 31,166; p < 0.001) for 2 predictors and 3.4 (CI 95%: 2.2–5.3; 2 : 30,391; p < 0.001) (−2 Log likelihood, 4,097,472; 2 : 68,521; p > 0.001) for ≥3 predictors. The probability of indicating a second SPECT during the follow-up rose with the number of predictor variables found (log rank test for trend, 2 : 616,410; p < 0.001). Predictors of myocardial ischemia in the second gated-SPECT Reversible perfusion defects were detected in 58 of the 280 (20.7%) patients undergoing a second stress-rest SPECT: mild (sum of differential score between 2 and 3) in 43 patients (74.1%) and moderate (sum of differential score between 4 and 6) in 15 patients (25.9%). In 26 patients the defects were of anterior, septal and/or apical localization, being inferolateral in 32 patients. Table 3 shows the characteristics of the first SPECT in the patients with and without reversible defects in the second SPECT. The only significant variable was having performed a purely pharmacologically stimulated ischemia test in the first SPECT (207 vs. 9%; p = 0.013). Table 4 describes the HR of the significant variables in the univariate analysis and those included by clinical consensus for multivariate analysis. The independent predictor variables of myocardial ischemia in the second SPECT were: male (HR: 1.9; CI 95%: 1.1–3.7; p = 0.038) and the performance of a purely pharmacological test (HR: 2.6; CI 95%: 1.3–5.3; p = 0.007) during the first SPECT (Fig. 2A and B). Fig. 3 provides an example of a normal first SPECT and a second SPECT with a reversible perfusion defect. With respect to the category of reference (without predictors of myocardial ischemia in the second SPECT), the HR for one predictor was 1.4 (CI 95%: 0.7–2.5; 2 : 0.963; p = 0.326) and 2.3 (CI 95%: 1.1–5.4; : 3948; p = 0.047) (−2 Log likelihood, 536,509; 2 : 14,501 p = 0.025) for 2 predictors. The probability of myocardial ischemia in the second SPECT rose significantly on summing these predictors (log rank test for trend, 2 : 39,624; p = 0.0465). Discussion In the database of our Nuclear Cardiology Unit the prevalence of a normal stress-rest myocardial perfusion gated-SPECT was of 34% (2326/6811), and in 12% of these patients (286/2326) a second gated SPECT was indicated for health care reasons. Our results demonstrate that several clinical factors and those achieved from the stress test performed influence the indication for a new myocardial perfusion gated-SPECT study despite the first being normal. Documento descargado de http://www.elsevier.es el 17/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. G. Romero-Farina et al. / Rev Esp Med Nucl Imagen Mol. 2014;33(2):72–78 75 Table 2 Variables at the time of the first gated-SPECT which were predictive of the need for a second gated-SPECT. Variables Univariate Age Males Diabetes Hypercholesterolemia ≥3 CVRF Previous angina LBBB LVEF Previous AMI Previous CR ET Positive ST 2 HR (CI 95%) 1.591 8.644 1.121 12.044 12.652 1.914 1.276 5.429 12.316 60.856 3.334 11.529 1.1 (0.9–1.1) 1.4 (1.1–1.8) 1.2 (0.9–1.5) 1.5 (1.2–1.9) 1.6 (1.2–2.1) 1.3 (0.9–1.8) 1.4 (0.8–2.3) 0.9 (0.9–0.99) 1.8 (1.3–2.4) 2.9 (2.2–3.7) 1.3 (0.9–1.7) 1.6 (1.2–2.1) Multivariate p 0.442 0.003 0.29 0.001 <0.001 0.167 0.259 0.02 <0.001 <0.001 0.068 0.001 2 HR (CI 95%) 5.501 1.4 (1.05–1.8) 0.019 3.862 41.063 1.4 (1.1–1.8) 2.5 (1.9–3.3) 0.049 <0.001 8.699 1.5 (1.1–1.9) 0.003 p LBBB: left bundle branch block, HR: hazard ratio, CI: confidence interval, LVEF: left ventricular ejection fraction, CVRF: cardiovascular risk factors, AMI: acute myocardial infarction, ET: effort test, ST: stress test; CR: coronary revascularization. Although the literature has important information related to the favorable prognosis in patients with a normal myocardial perfusion SPECT,2–9 the variables influencing the indication for a second SPECT during follow-up and the presence of patterns of reversibility (ischemia) in the second remain unknown. and coronary revascularization prior to the first gated-SPECT and a positive stress test at the time of the first study. It is known that patients with the greatest number of CVRF have a worse prognosis11 and that in clinical practice the proportion of diagnostic tests indicated in these patients is greater. On the other hand, it has been observed that in patients without known coronary artery disease and with a normal stress SPECT study, the long-term follow-up is significantly affected by the burden of the CVRF.12 In a population of 2597 patients with no history of coronary disease and with a normal stress SPECT followed over a mean of 6.8 years, Supariwala et al.13 observed that the total annual mortality was of Predictive variables for a second gated-SPECT In the present study we observed that the principal variables influencing the indication for a second gated-SPECT were the presence of 3 or more CVRF, a history of acute myocardial infarction 100 A Probability in a 2nd SPECT (%) Probability in a 2nd SPECT (%) 100 80 60 40 ≥ 3 CVRF < 3 CVRF Chi-square: 12.8889 p<0.001 20 0 B 80 60 40 With previous AMI Without previous AMI Chi-square: 12.6453 p<0.001 20 0 0 2 1 3 4 5 6 0 1 Number of patients at risk <3 CVRF 1902 1551 ≥3 CVRF 423 363 1248 996 768 574 402 295 245 168 115 65 Number of patients at risk Without previous AMI 2088 1710 With previous AMI 237 204 100 C 80 60 40 With previous CR Without previous CR Chi-square: 66.7071 p<0.001 20 4 5 6 Follow-up (years) Probability in a 2nd SPECT (%) Probability in a 2nd SPECT (%) 100 3 2 Follow-up (years) 1384 1119 857 629 432 159 122 79 60 35 3 4 5 6 D 80 60 40 st Positive ST in the 1 SPECT st Negative ST in the 1 SPECT Chi-square: 11.7347 p<0.0 01 20 0 0 0 1 2 4 5 6 Follow-up (years) Number of patients at risk Without previous CR 2046 With previous CR 279 3 0 1 2 Follow-up (years) Number of patients at risk st 1685 1377 1105 847 628 427 Negative ST in the 1 SPECT 1903 1570 1254 1009 755 566 391 289 232 181 123 76 st 229 166 136 89 61 40 Positive ST in the 1 SPECT 422 344 Fig. 1. Kaplan–Meier analysis of the accumulated incidence of a second SPECT in relation to its predictive variables. (A) Cardiovascular risk factors (CVRF). (B) Acute myocardial infarction (AMI) prior to the first SPECT. (C) Coronary revascularization (CR) prior to the first SPECT. (D) Positive stress test (ST) in the first SPECT. Documento descargado de http://www.elsevier.es el 17/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. 76 G. Romero-Farina et al. / Rev Esp Med Nucl Imagen Mol. 2014;33(2):72–78 Table 3 Characteristics of the patients at the time of the first gated-SPECT in relation to the presence of ischemia in the second gated-SPECT. Global 2 SPECT No ischemia n = 222 Ischemia n = 58 p Age (years) BMI Males (%) Diabetes mellitus (%) Arterial hypertension (%) Hypercholesterolemia (%) Smoking (%) 1 CVRF (%) 2 CVRF (%) ≥3 CVRF 63.5 ± 10.7 29.9 ± 16 143 (51.1) 64 (22.9) 174 (62.1) 158 (56.4) 101 (36.1) 77 (27.5) 94 (33.6) 75 (26.8) 63.1 ± 10.8 30.6 ± 19 110 (49.5) 53 (23.9) 143 (64.4) 126 (56.8) 76 (34.2) 126 (56.8) 71 (32) 62 (27.9) 65.1 ± 10.5 27.7 ± 5 33 (56.9) 11 (19) 31 (53.4) 32 (55.2) 25 (43.1) 32 (55.2) 23 (39.7) 13 (22.4) 0.731 0.559 0.396 0.428 0.125 0.828 0.210 0.828 0.271 0.398 Clinical history Previous AMI (%) Previous CR (%) Angina (%) Chest pain (%) 45 (16.1) 73 (26.1) 38 (13.6) 242 (86.4) 37 (16.7) 56 (25.2) 34 (15.3%) 188 (84.7%) 8 (13.8) 17 (29.3) 4 (6.9%) 54 (93.1) 0.596 0.528 0.096 0.096 ECG LBBB (%) PM (%) 15 (5.4) 2 (0.7) 13 (5.9) 2 (0.9) 2 (3.4) 0 0.468 1 Type of stress ST (%) ST + PHARM (%) PHARM (%) Positive ST (%) 214 (76.4) 34 (12.1) 32 (11.4) 74 (26.4) 171 (77) 31 (14) 20 (9) 57 (25.7) 43 (74.1) 3 (5.2) 12 (20.7) 17 (29.3) 0.644 0.068 0.013 0.576 Gated-SPECT LVEF (%) TDV (ml) TSV (ml) 66.4 ± 13 74.9 ± 30 28.6 ± 19 66.6 ± 13 75.6 ± 10 29.5 ± 3 65.6 ± 12.1 72.2 ± 16 26.6 ± 10 0.618 0.558 0.521 LBBB: left bundle branch block, PHARM: pharmacologic test, LVEF: left ventricular ejection fraction, CVRF: cardiovascular risk factors; AMI: acute myocardial infarction, BMI: body mass index, PM: pacemaker, ST: stress test, CR: coronary revascularization, TDV: telediastolic volume, TSV: telesystolic volume. Table 4 Variables at the time of the first gated-SPECT which were predictive of myocardial ischemia in the second gated-SPECT. Variables Multivariatea Univariate 2 First gated-SPECT Male Angina Previous AMI Previous CR Pharmacologic test Positive ST 2 HR (CI 95%) p HR (CI 95%) p 2.813 3.320 0.020 1.039 6.501 1.077 1.6 (0.93–2.7) 0.4 (0.1–1.1) 0.9 (0.4–2) 1.3 (0.7–2.4) 2.3 (1.2–4.4) 1.4 (0.8–2.3) 0.094 0.068 0.888 0.308 0.011 0.299 4.322 1.9 (1.1–3.7) 0.038 7.182 2.6 (1.3–5.3) 0.007 HR: hazard ratio, CI: confidence interval, AMI: acute myocardial infarction, ST: stress test, CR: coronary revascularization. a Adjusted for age, diabetes, ≥3 cardiovascular risk factors and left ventricular ejection fraction. 100 A Probability of ischemia in the 2nd SPECT (%) Probability of ischemia in the 2nd SPECT (%) 100 80 60 40 Male Female Chi-square: 4.322 p=0.038 20 0 B 80 st 60 With PHARM test in the 1 SPECT st Without PHARM test in the 1 SPECT Chi-square: 6.8899 p<0.038 40 20 0 0 1 2 3 4 5 6 Follow-up (years) Number of patients at risk Female 97 137 Male 104 143 0 1 2 3 4 5 6 68 42 18 9 8 6 0 0 Follow-up (years) 57 41 27 12 7 50 35 21 6 2 Number of patients at risk st Without PHARM test in the 1 SPECT 248 179 97 st With PHARM test in the 1 SPECT 32 22 10 Fig. 2. Kaplan–Meier analysis of the accumulated incidence of the presence of myocardial ischemia in the second SPECT in relation to its predictive variables. (A) Genre; (B) pure pharmacological (PHARM) test in the first SPECT. Documento descargado de http://www.elsevier.es el 17/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. G. Romero-Farina et al. / Rev Esp Med Nucl Imagen Mol. 2014;33(2):72–78 1 EC ELH ELV E R 2 EC ELH ELV E R Fig. 3. Example of a normal first myocardial perfusion maximum stress-rest SPECT (1) in a patient with atypical pain after the implantation of a stent in the right coronary artery and of a second SPECT (2) performed 2 years later in which a moderate reversible apical defect may be observed. E: stress, EC: short axis, ELH: long horizontal axis, ELV: long vertical axis, R: rest. 1.8% in the patients with 3 risk factors (hypertension, diabetes and smoking), being of only 0.2% in patients with no risk factor. The presence of known coronary artery disease was at a higher prognostic value compared to a normal SPECT result since this indicates a population of patients with an elevated risk of new cardiac complications.14 From a clinical point of view it is logical for a history of acute myocardial infarction and/or coronary revascularization to carry a strict patient follow-up and thus, a greater probability of indication for tests to rule out residual ischemia, particularly in symptomatic patients. Carryer et al., 7 observed that a second routine SPECT following a first normal SPECT was indicated in 13% of 2354 patients with no history of coronary disease while this percentage was of 26% in the 656 patients with already diagnosed coronary disease. In our series of patients in whom a second gated-SPECT was performed the prevalence of a previous acute myocardial infarction (16.15 vs. 9.4%; p < 0.001) and previous coronary revascularization (25.9 vs. 10%; p < 0.001) was also significantly greater than in those in whom a second SPECT was not indicated, although no significant differences were found in the intervals of time between the first and the second study in the patients with and without known coronary artery disease (1.9 vs. 2.2 years; p = 0.114). Schinkel et al.14 published a series of 147 consecutive patients with a history of infarction and/or revascularization with a normal stress SPECT or with dobutamine followed over a mean of 6.5 years. They observed that the annual cardiac mortality was 0.5% during the first 3 years and 1.3% during the following 3 years. The independent predictive factors of this mortality were male genre and the cardiac frequency by both resting and effort blood pressure. These authors concluded that in patients with this history and with a normal SPECT it is not necessary to repeat the study 77 prior to 3 years except on the development of symptoms during the follow-up. In our population and excluding the patients with left bundle branch block we also observed that the indication for a second gated-SPECT was more often requested (26.2 vs. 17%; p < 0.001) in patients in whom the stress test had been positive for ischemia showing ST segment depression and/or angina in the first normal gated-SPECT. In previous studies it has been observed that a significant ST segment depression, especially in males, even in the presence of a normal SPECT may be highly indicative of multivessel disease and/or of the common trunk.15 In this clinical context, and despite a negative first study, it is logical to think that the clinician may request a second SPECT. Predictive variables of myocardial ischemia in the second gated-SPECT In the multivariate analysis of our series the principal predictive variables for an ischemic pattern in the second SPECT were male genre and the performance of a purely pharmacological test during the first gated-SPECT. These findings are not surprising taking into account that, on one hand, the prevalence of coronary artery disease is greater in men than in women of a similar age and the fact that not being able to do physical exercise and having to do a pharmacological test to stimulate ischemia both carry a worse prognosis.16 The mortality is inversely related to the duration of the exercise and is only of 0.1%/year in patients able to achieve 10 MET in the stress test.17 It is therefore logical that the cardiologists have a greater tendency to request a new study after a purely pharmacological first SPECT, despite being normal, than in cases in which the normal SPECT was obtained after a sufficient stress test, particularly if this was clinically and electrocardiographically negative. In previous series18–21 the long-term mortality was reportedly longer after a normal SPECT with a purely pharmacological test compared with a SPECT performed with a stress test. In a metaanalysis of 14,918 patients from 24 studies, Navare et al.22 observed that the percentage of complications after a SPECT was significantly higher if a pharmacological test had been performed compared to a stress test regardless of whether the result had been normal (1.78 vs. 0.65%; p < 0.001) or not (9.98 vs. 4.3%; p < 0.001). Despite patients evaluated with pharmacological tests generally presenting an older age, diabetes, arterial hypertension, and atrial fibrillation, in a series of 6069 patients followed over a mean of 10 years Rozanski et al.23 observed that the annual mortality of the patients who had received adenosine as the stimulation test was 2-fold greater than that of those who had performed a stress test (3.9 vs. 1.6%; p < 0.001). In these cases the mortality was inversely related to the duration of the exercise, being comparable to that of adenosine in those who did not surpass 3 min in the stress test. Limitations This was a single center study and may have a possible bias in that cohort studies do not allow a clear cause–effect relationship to be established. It is true that after a normal gated-SPECT new symptoms may appear which, according to the criteria of the attending physician, carry an indication for a second study. Indeed, this was the main reason for indicating a second gated-SPECT. However, the objective of this study was to analyze the characteristics of the patients in the first study which influence the indication for a second study despite the first being normal, independently of the symptomatology prior to the second gated-SPECT which, in general, was chest pain in our series. Documento descargado de http://www.elsevier.es el 17/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. 78 G. Romero-Farina et al. / Rev Esp Med Nucl Imagen Mol. 2014;33(2):72–78 Conclusions In patients with a normal myocardial perfusion SPECT different clinical factors (≥3 CVRF, previous acute myocardial infarction and coronary revascularization) and factors derived from the stress test (angina and/or ST segment depression) influence the indication for a second gated-SPECT during follow-up. The observation of perfusion defects in the second SPECT is more probable in males and in patients doing a purely pharmacological first gated-SPECT. Conflict of interests 10. 11. 12. 13. 14. The authors declare no conflict of interests. References 1. Shaw LJ, Iskandrian AE. Prognostic value of gated myocardial perfusion SPECT. J Nucl Cardiol. 2004;11:171–85. 2. Shaw LJ, Hage FG, Berman DS, Hachamovitch R, Iskandrian A. Prognosis in the era of comparative effectiveness research: where is nuclear cardiology now and where should it be. J Nucl Cardiol. 2012;19:1026–43. 3. Elhendy A, Schinkel A, Bax JJ, van Domburg RT, Poldermans D. Long-term prognosis after a normal exercise stress Tc-99m sestamibi SPECT study. J Nucl Cardiol. 2003;10:261–6. 4. Shaw LJ, Hendel R, Borges-Neto S, Lauer MS, Alazraki N, Burnette J, et al. Myoview Multicenter Registry. Prognostic value of normal exercise and adenosine (99m)Tc-tetrofosmin SPECT imaging: results from the multicenter registry of 4.728 patients. J Nucl Med. 2003;44:648. 5. Metz LD, Beattie M, Hom R, Redberg RF, Grady D, Fleischmann KE. The prognostic value of normal exercise myocardial perfusion imaging and exercise echocardiography: a meta-analysis. J Am Coll Cardiol. 2007;49:227–37. 6. Miller TD, Hodge DO, Milavetz JJ, Gibbons RJ. A normal stress SPECT scan is an effective gatekeeper for coronary angiography. J Nucl Cardiol. 2007;14:187–93. 7. Carryer DJ, Askew JW, Hodge DO, Miller TD, Gibbons RJ. The timing and impact of follow-up studies after normal stress single-photon emission computed tomography sestamibi studies. Circ Cardiovasc Imaging. 2010;3:520–6. 8. Hachamovitch R, Hayes S, Friedman JD, Cohen I, Shaw LJ, Germano G, et al. Determinants of risk and its temporal variation in patients with normal stress myocardial perfusion scans: what is the warranty period of a normal scan. J Am Coll Cardiol. 2003;41:1329–40. 9. Schinkel AF, Boiten HJ, van der Sijde JN, Ruitinga PR, Sijbrands EJ, Valkema R, et al. 15-Year outcome after normal exercise (99m)Tc-sestamibi myocardial 15. 16. 17. 18. 19. 20. 21. 22. 23. perfusion imaging: what is the duration of low risk after a normal scan. J Nucl Cardiol. 2012;5:901–6. Zoghbi GJ, Iskandrian AE. Pharmacological stress testing. In: Iskandrian AE, García EV, editors. Nuclear cardiac imaging. Principles and applications. Oxford: Oxford University Press; 2008. p. 293–315. Marrugat J, Solanas P, D’Agostino R, Sullivan L, Ordovas J, Cordón F, et al. Estimación del riesgo coronario en España mediante la ecuación de Framingham calibrada. Rev Esp Cardiol. 2003;56:253–61. Lloyd-Jones DM, Leip EP, Larson MG, D’Agostino RB, Beiser A, Wilson PW, et al. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006;113:791–8. Supariwala A, Uretsky S, Singh P, Memon S, Khokhar SS, Wever-Pinzon O, et al. Synergistic effect of coronary artery disease risk factors on long-term survival in patients with normal exercise SPECT studies. J Nucl Cardiol. 2011;18:207–14. Schinkel AF, Elhendy A, Bax JJ, van Domburg RT, Huurman A, Valkema R, et al. Prognostic implications of a normal stress technetium-99m-tetrofosmin myocardial perfusion study in patients with a healed myocardial infarct and/or previous coronary revascularization. Am J Cardiol. 2006;97:1–6. Candell-Riera J, Fernández C, Escudero F, de León G, Aguadé-Bruix S, CastellConesa J. Prevalencia y significado angiográfico de la SPECT de perfusión miocárdica normal con electrocardiograma de esfuerzo positivo. Rev Esp Cardiol. 2004;57:894–7. Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002;346:793–801. Bourke JM, Charlton GT, Holland BH, Belyea CM, Watson DD, Beller GA. Prognosis in patients achieving >= 10 METs on exercise stress testing: was SPECT imaging useful. J Nucl Cardiol. 2011;18:230–7. Abbott BG, Afshar M, Berger AK, Wackers FJ. Prognostic significance of ischemic electrocardiographic changes during adenosine infusion in patients with normal myocardial perfusion imaging. J Nucl Cardiol. 2003;10:9–16. Klodas E, Miller TD, Christian TF, Hodge DO, Gibbons RJ. Prognostic significance of ischemic electrocardiographic changes during vasodilator stress testing in patients with normal SPECT images. J Nucl Cardiol. 2003;10:4–8. Sharma J, Roncari C, Giedd KN, Fox JT, Kanei Y. Patients with adenosine-induced ST-segment depressions and normal myocardial perfusion imaging: cardiac outcomes at 24 months. J Nucl Cardiol. 2010;17:874–80. Johnson NP, Schimmel Jr DR, Dyer SP, Leonard SM, Holly TA. Survival by stress modality in patients with a normal myocardial perfusion study. Am J Cardiol. 2011;107:986–9. Navare SM, Mather JF, Shaw LJ, Fowler MS, Heller GV. Comparison of risk stratification with pharmacologic and exercise stress myocardial perfusion imaging: a meta-analysis. J Nucl Cardiol. 2004;11:551–61. Rozanski A, Gransar H, Hayes SW, Friedman JD, Hachamovitch R, Berman DS. Comparison of long-term mortality risk following normal exercise vs adenosine myocardial perfusion SPECT. J Nucl Cardiol. 2010;17:999–1008.