Nebulized colistin treatment of multi
Anuncio
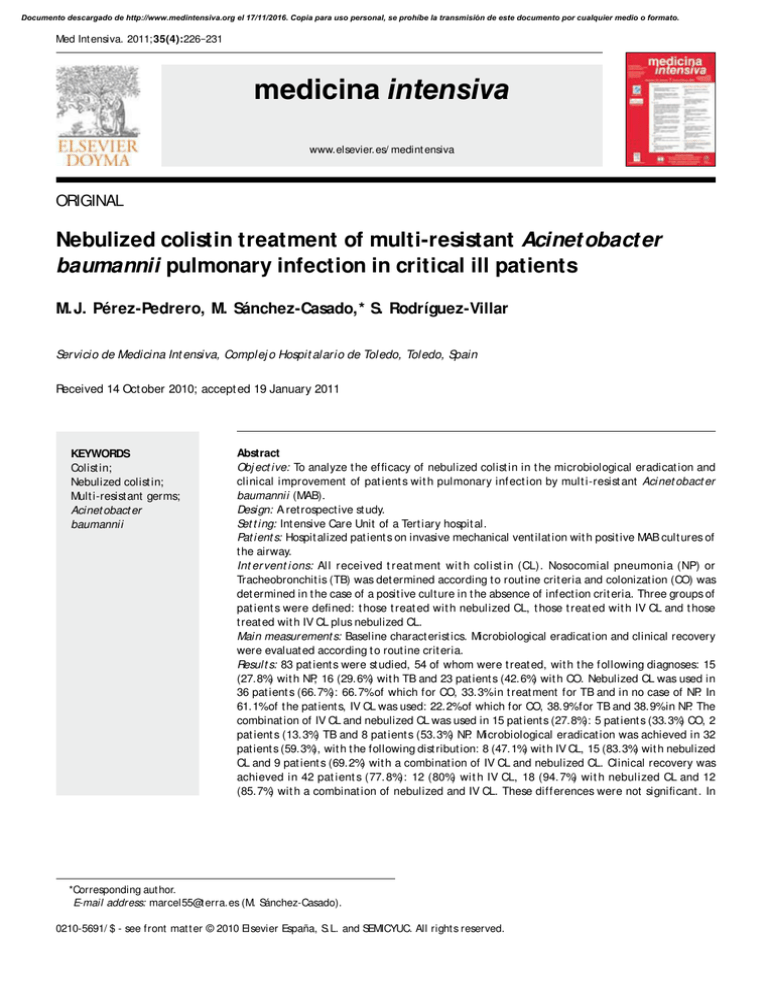
Documento descargado de http://www.medintensiva.org el 17/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. Med Int ensiva. 2011;35(4):226−231 medicina intensiva www.elsevier.es/ medint ensiva ORIGINAL Nebulized colistin treatment of multi-resistant Acinet obact er baumannii pulmonary infection in critical ill patients M.J. Pérez-Pedrero, M. Sánchez-Casado,* S. Rodríguez-Villar Servicio de Medicina Int ensiva, Complej o Hospit alario de Toledo, Toledo, Spain Received 14 Oct ober 2010; accept ed 19 January 2011 KEYWORDS Colist in; Nebulized colist in; Mult i-resist ant germs; Acinet obact er baumannii Abstract Obj ect ive: To analyze t he efficacy of nebulized colist in in t he microbiological eradicat ion and clinical improvement of pat ient s wit h pulmonary inf ect ion by mult i-resist ant Acinet obact er baumannii (MAB). Design: A ret rospect ive st udy. Set t ing: Int ensive Care Unit of a Tert iary hospit al. Pat ient s: Hospit alized pat ient s on invasive mechanical vent ilat ion wit h posit ive MAB cult ures of t he airway. Int er vent i ons: Al l received t reat ment wit h col ist in (CL). Nosocomial pneumonia (NP) or Tracheobronchit is (TB) was det ermined according t o rout ine crit eria and colonizat ion (CO) was det ermined in t he case of a posit ive cult ure in t he absence of infect ion crit eria. Three groups of pat ient s were defined: t hose t reat ed wit h nebulized CL, t hose t reat ed wit h IV CL and t hose t reat ed wit h IV CL plus nebulized CL. Main measurement s: Baseline charact erist ics. Microbiological eradicat ion and clinical recovery were evaluat ed according t o rout ine crit eria. Result s: 83 pat ient s were st udied, 54 of whom were t reat ed, wit h t he following diagnoses: 15 (27.8%) wit h NP, 16 (29.6%) wit h TB and 23 pat ient s (42.6%) wit h CO. Nebulized CL was used in 36 pat ient s (66.7%): 66.7%of which for CO, 33.3%in t reat ment for TB and in no case of NP. In 61.1%of t he pat ient s, IV CL was used: 22.2%of which for CO, 38.9%for TB and 38.9%in NP. The combinat ion of IV CL and nebulized CL was used in 15 pat ient s (27.8%): 5 pat ient s (33.3%) CO, 2 pat ient s (13.3%) TB and 8 pat ient s (53.3%) NP. Microbiological eradicat ion was achieved in 32 pat ient s (59.3%), wit h t he following dist ribut ion: 8 (47.1%) wit h IV CL, 15 (83.3%) wit h nebulized CL and 9 pat ient s (69.2%) wit h a combinat ion of IV CL and nebulized CL. Clinical recovery was achieved in 42 pat ient s (77. 8%): 12 (80%) wit h IV CL, 18 (94. 7%) wit h nebulized CL and 12 (85.7%) wit h a combinat ion of nebulized and IV CL. These differences were not significant . In *Corresponding aut hor. E-mail address: marcel55@t erra.es (M. Sánchez-Casado). 0210-5691/ $ - see front mat t er © 2010 Elsevier España, S.L. and SEMICYUC. All right s reserved. Documento descargado de http://www.medintensiva.org el 17/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. Nebulized colist in t reat ment of mult i-resist ant Acinet obact er baumannii pulmonary infect ion in crit ical ill pat ient s 227 t he group of pat ient s wit h inf ect ion due t o TB and NP (31 pat ient s, 57. 4%), microbiological eradicat ion was achieved in 5 pat ient s (100%) t reat ed wit h nebul ized CL and in 6 of t he 9 pat ient s (42.9%) t reat ed wit h IV CL, t he difference being significant (P < .05). Clinical recovery in t his group was 100%(6 pat ient s) t reat ed wit h nebulized CL and 75%(9 of t he 12 pat ient s) in t he IV CL group. This difference was not significant . Conclusions: Our st udy suggest s t hat t reat ment wit h colist in in pat ient s wit h pulmonary infect ion wi t h mul t i -resi st ant Aci net obact er baumanni i coul d be more ef f i ci ent i f i t were t o be administ rat ed solely nebulized or in combinat ion wit h IV colist in rat her t han administ ered solely int ravenously. © 2010 Elsevier España, S.L. and SEMICYUC. All right s reserved. PALABRAS CLAVE Colist ina; Colist ina nebulizada; Microorganismos mult irresist ent es; Acinet obact er baumannii Utilización de la colistina nebulizada en la colonización e infección respiratoria por Acinet obact er baumannii en pacientes críticos Resumen Obj et ivo: Evaluar la eficacia de la colist ina nebulizada en la erradicación microbiológica y la mej oría clínica de pacient es con Acinet obact er baumannii en vías respirat orias. Diseño: Est udio ret rospect ivo. Ámbit o: Servicio de medicina int ensiva en hospit al t erciario. Pacient es: Pacient es ingresados en vent ilación mecánica invasiva con cult ivos posit ivos en vía aérea para A. baumannii mult irresist ent e. Int ervenciones: Todos recibieron t rat amient o con colist ina (CL). Se det erminó neumonía nosocomial (NN) o t raqueobronquit is (TB) según crit erios habit uales y colonización (CO) si había cult ivo posit ivo en ausencia de crit erios de infección. Se definieron 3 grupos de pacient es: t rat ados con CL nebulizada, con CL i.v. y con CL i.v. más nebulizada. Variables de int erés: Caract eríst icas basales. Se consideró erradicación microbiológica y curación clínica según crit erios habit uales. Result ados: Se est udió a 83 pacient es; 54 fueron t rat ados, con los diagnóst icos: 15 (27,8%) con NN, 16 (29,6%) con TB y 23 pacient es (42,6%) con CO. La CL nebulizada fue ut ilizada en 36 pacient es (66,7%): en el 66,7%en CO, el 33,3%en t rat amient o de TB y en ningún caso de NN. En el 61,1%de los pacient es se ut ilizó CL i.v.: en la CO en el 22,2%, en la TB en el 38,9%y en las NN en el 38,9%. La combinación de CL i.v. más nebulizada fue ut ilizada en 15 pacient es (27,8%), que se empleó: 5 (33,3%) CO, 2 (13,3%) TB y 8 (53,3%) NN. La erradicación microbiológica se consiguió en 32 pacient es (59,3%), con la dist ribución: 8 (47,1%) con CL i.v., 15 (83,3%) con CL nebulizadas y 9 pacient es (69,2%) con la combinación CL i.v. más nebulizada. La curación clínica se consigue en 42 pacient es (77,8%): 12 (80%) con CL i.v., 18 (94,7%) con CL nebulizada y 12 (85,7%) con la combinación de CL nebulizada e int ravenosa. Est as diferencias no fueron significat ivas. En el grupo de pacient es con infección por TB y NN (31 pacient es, 57,4%) la erradicación microbiológica se consiguió en 5 pacient es (100%) t rat ados con CL nebulizada y en 6 de 14 (42,9%) t rat ados con CL i.v.; est a diferencia fue significat iva (p < 0,05). La curación clínica en est e grupo fue del 100%(6 pacient es) t rat ados con CL nebulizada y del 75%(9 de 12) en el grupo de CL i.v. Est a diferencia no fue significat iva. Concl usiones: Nuest ro est udio señala que el t rat amient o con colist ina en pacient es con infección pulmonar por A. baumannii mult irresist ent e podría ser más eficaz si se administ ra nebulizada o en combinación con colist ina i.v. que si se administ ra de forma int ravenosa solament e.. © 2010 Elsevier España, S.L. y SEMICYUC. Todos los derechos reservados. Introduction Nosocomi al col oni zat i on and i nf ect i on caused by mult iresist ant gramnegat ive bacilli have increased great ly in recent years, and represent one of t he most serious complicat ions in pat ient s admit t ed t o t he Int ensive Care Unit (ICU). Among t he different mult iresist ant gramnegat ive mi cr oor gani sms, Speci al ment i on must be made of Acinet obact er baumannii. 1 The ant ibiot ic colist in was widely used bet ween t he 1960s and 1980s due t o it s pot ent bact ericidal act ion, low incidence of resist ances, and excellent act ivit y against gramnegat ive baci l l i , i ncl udi ng mul t i r esi st ant st r ai ns. However, t he associ at ed t oxi ci t y (nephrot oxi ci t y and neurot oxi ci t y) event ually caused use of t he drug t o be abandoned. 2 In t he 1980s, colist in began t o be used via t he nebulized rout e in pat i ent s wi t h cyst i c f i br osi s chr oni cal l y i nf ect ed wi t h Pseudomonas aeruginosa. 3 On t he ot her hand, t he emergence of inf ect ions due t o A. baumanni i in crit ical pat ient s has ret urned t his ant ibiot ic t o t he front line in clinical pract ice. There is evidence t hat nebulized colist in in conj unct ion wit h t he int ravenous rout e could be useful for t he t reat ment Documento descargado de http://www.medintensiva.org el 17/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. 228 of A. baumannii and P. aeruginosa infect ions. 4 The present st udy describes our experience wit h t he use of nebulized colist in f or t he t reat ment of respirat ory colonizat ion and inf ect ion caused by A. baumannii in crit ical pat ient s. The aim is t o evaluat e t he ef f icacy of nebulized colist in in t he clinical eradicat ion and/ or clinical improvement (in t he cont ext of t racheobronchit is and/ or nosocomial pneumonia) of pat i ent s wi t h A. baumanni i i sol at ed f r om ai r way cult ures. M.J. Pérez-Pedrero et al The pat i ent s w er e eval uat ed f or mi cr obi ol ogi cal eradicat ion and clinical recovery. The lat t er was defined by disappearance of t he fever, normalizat ion of t he leukocyt e count s, disappearance or signif icant improvement of t he r adi ol ogi cal i nf i l t r at es i n t he case of pneumoni a, and disappearance or significant improvement of t he bronchial secret ions in t he case of t racheobronchit is. Microbiological eradicat ion in t urn was def ined by negat ive conversion of t he respirat ory sample cult ure in at least t wo consecut ive cult ures. Vigilance cult ures were conduct ed on a weekly basis. Material and method A r et r ospect i ve st udy was made i n t he Depar t ment of Int ensive Care Medicine of Virgen de la Salud Hospit al in Toledo (Spain). We included all pat ient s wit h A. baumannii posit ive airway sample cult ures (t racheobronchial aspirat e) at any t ime during admission, and who received t reat ment wit h colist in. All pat ient s were subj ect ed t o mechanical vent ilat ion, t hough at t he t ime of t he diagnosis some of t hem had al r eady been weaned f r om t he vent i l at or (11 pat ient s; 20.4%) – wit h t racheot omy in all cases. Col i st i n was admi ni st ered vi a t he i nt ravenous rout e, nebulized, or via bot h rout es simult aneously (mixed). The int ravenous dose was adj ust ed according t o renal funct ion. The clinician in t urn decided t he dose of nebulized colist in, using t hree regimens: 106 IU/ 8 h, 5 x 105 IU/ 6 h and 106 IU/ 12 h. The pat i ent s were di vi ded i nt o t hree cl i ni cal groups: – Nosocomial pneumonia (NP): diagnosis 48 hours af t er admi ssi on, based on t he f ol l ow i ng cr i t er i a: new radiological infilt rat es or progression of already exist ing inf il t rat es, f ever > 38ºC wit hout any ot her expl aining cause, l eukocyt osi s ( ≥ 12, 000/ μl ) or l eukopeni a (< 4000/ μl ), purul ent sput um or i ncreased bronchi al secret ion. Microbiological conf irmat ion of t he diagnosis was made based on posit ive respirat ory sample cult ures (bronchial aspirat e) wit h a signif icant bact erial count (≥ 100,000 cfu/ ml). – Tracheobronchit is (TB): f ever > 38ºC wit hout any ot her explaining cause, leukocyt osis (≥ 12,000/ μl) or leukopenia (< 4000/ μl) and purulent sput um or increased bronchial secret ion wit hout radiol ogical inf il t rat es indicat ive of pneumonia. Microbiological confirmat ion of t he diagnosis was made based on posit ive respirat ory sample cult ures (bronchial aspirat e)(≥ 100,000 cfu/ ml). – Colonizat ion: posit ive cult ure in t he absence of crit eria of infect ion. Colonized pat ient s are not usually t reat ed wit h ant ibiot ics. The i ncl uded col oni zed i ndi vi dual s were of t wo ki nds: pat i ent s di agnosed wi t h i nf ect i on (and t he deci si on t o provide t reat ment t herefore had been t aken), and pat ient s who upon review were regarded as being only colonized, since t hey did not meet t he diagnost ic crit eria for pneumonia or t racheobronchit is. On t he ot her hand, we included some colonized pat ient s t reat ed according t o t he crit erion of t he supervising physician, on t he grounds t hat t he t reat ment of colonizat ion by mult iresist ant microorganisms is warrant ed i n cert ai n ci rcumst ances (e. g. , i n pat i ent s wi t h cyst i c fibrosis colonized by Pseudomonas). 3 Statistical analysis Qual i t at i ve vari abl es are present ed as absol ut e val ues (percent ages), while quant it at ive variables are report ed as t he mean ± st andard deviat ion (SD). The comparison of cat egorical variables was based on t he chi-squared t est , wit h t he Fisher exact t est in 2 x 2 groups. The comparison of quant it at ive variables in t urn was carried out wit h t he MannWhit ney U-t est . St at ist ical significance was considered for p<0.05. The SPSS version 15.0 st at ist ical package was used t hroughout (SPSS Inc., Chicago, IL, USA). Results We reviewed a t ot al of 83 pat ient s wit h posit ive cult ures for col ist in-sensit ive A. baumanni i in bronchial secret ions. Pat ient s considered by t he clinician t o be colonized and who t herefore received no ant ibiot ic t reat ment were excluded. A t ot al of 54 subj ect s were t reat ed wit h colist in and included in t he st udy. Their baseline charact erist ics, including t he severit y and mult iorgan dysf unct ion scores at t he t ime of t he diagnosis of colonizat ion or inf ect ion, are report ed in Tabl e 1. The most f requent causes of admi ssi on were: polyt raumat ism, 17 pat ient s (31. 5%); st roke, 10 pat ient s (18.6%); sept ic shock, 10 pat ient s (18.5%) and pneumonia, 8 pat ient s (14.9%). A t ot al of 42. 6% of t he pat ient s were col onized by A. baumanni i ; 29. 6% present ed t racheobronchit is and 27. 8% pneumonia at t ribut able t o t his organism. In 35. 2% of t he cases A. baumanni i was t he only microorganism isolat ed from t he respirat ory t ract . The most frequent ly associat ed microorganisms were: Klebsiella (2), E. coli (1), E. f aecium (1) and Pseudomonas [1]. In 46.3%of t he cases colist in was admi ni st er ed as onl y ant i bi ot i c – t he most f r equent l y associat ed ant ibiot ic drugs being meropenem (7 cases), aminoglycosides (6 cases), linezolid (4 cases), cefot axime / cef t r i axone (3 cases), and pi per aci l l i n / t azobact am (3 cases). The nebulized colist in dose was 106 IU/ 8 h in 33.3%of t he cases, 5 x 105 IU/ 6 h in 14.8%, and 106 IU/ 12 h in 14.8%. No pat i ent devel oped er yt hema. In 14. 8% of t he pat i ent s cort icost eroid premedicat ion was provided, and in no case did bronchospasm occur when colist in was used in nebulized f or m. Four pat i ent s ( 7%) devel oped nephr ot oxi ci t y at t ribut able t o colist in. Table 1 also report s t he dif f erent variables according t o t he t ype of colist in administ ered t o t he pat ient . Microbiological eradicat ion was achieved in 32 pat ient s (59.3%). Specifically, eradicat ion was achieved in 47%of t he Documento descargado de http://www.medintensiva.org el 17/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. Nebulized colist in t reat ment of mult i-resist ant Acinet obact er baumannii pulmonary infect ion in crit ical ill pat ient s 229 Table 1 General charact erist ics of t he pat ient s and dist ribut ion of t he variables according t o t he t ype of colist in administ ered Tot al (n = 54) Int ravenous colist in (n = 18) Nebulized colist in (n = 21) Mixed colist in (n = 15) Males Age (years) APACHE II SOFA Mechanical vent ilat ion 43 (79.6%) 57.1 ± 17.6 12.6 ± 5.3 4.4 ± 2.2 43 (79.6%) 15 (83.3%) 60.1 ± 17.4 12.8 ± 5.7 4.6 ± 2 15 (83.3%) 16 (76.2%) 55.5 ± 19.8 11.2 ± 4.3 3.7 ± 2 14 (66.7%) 12 (80%) 55.6 ± 14.8 14.1 ± 5.7 4.9 ± 2.4 14 (93.3%) Clinical diagnosisa,b Colonizat ion Tracheobronchit is NP 23 (42.6%) 16 (29.6%) 15 (27.8%) 4 (22.2%) 7 (38.9%) 7 (38.9%) 14 (66.7%) 7 (33.3%) 0 5 (33.3%) 2 (13.3%) 8 (53.3%) St ay in ICU (days) Hospit al st ay (days) Nephrot oxicit y Microbiological eradicat ion Clinical recovery Deat h 46.8 ± 34.3 66.1 ± 54.1 4 (7.4%) 32 (59.3%) 42 (77.8%) 12 (22.2%) 45.5 ± 36.5 64.1 ± 63 2 (11.1%) 8 (47.1%) 12 (66.6%) 5 (27.8%) 49 ± 40.2 70.9 ± 59 1 (4.8%) 15 (83.3%) 18 (85.7%) 4 (19%) 45.3 ± 22.7 61.9 ± 35 1 (6.7%) 9 (69.2%) 12 (80%) 2 (20%) NP: nosocomial pneumonia. a In relat ion t o A. Baumannii. b p < 0.05 among t he t hree colist in administ rat ion groups. pat ient s t reat ed wit h int ravenous colist in and in 83. 3% of t hose t reat ed wit h nebulized colist in only. The dif f erence bet ween t hese t wo groups was signif icant (p < 0. 05). On analyzing the colonization group (23 patients), microbiological eradicat ion was achieved in 76.9% of t he pat ient s t reat ed wit h nebulized colist in, in 75%of t hose administ ered mixed colist in, and in 66.7%of t he pat ient s t reat ed wit h int ravenous colist in – t he differences in t his case being nonsignificant . In t he pat i ent s wi t h t r acheobr onchi t i s and pneumoni a (31 pat ient s), microbiological eradicat ion was achieved in 100%of t he pat ient s administ ered nebulized colist in, in 66.7% of t hose administ ered mixed colist in, and in 42. 9% of t he pat ient s t reat ed wit h int ravenous colist in. In t his case t he difference bet ween nebulized and int ravenous colist in proved significant (p < 0.05) (Fig. 1). Clinical recovery was evident ly analyzed only in t he group w i t h r espi r at or y i nf ect i on ( t r acheobr onchi t i s and pneumonia), and occurred in 24 pat ient s (85.7%of t he t ot al pat ient s st udied). Clinical recovery occurred in 100%of t he 6 pat ient s t reat ed wit h nebulized colist in only (all diagnosed wit h t racheobronchit is), in 90%of t hose t reat ed wit h mixed colist in, and in 75%of t hose t reat ed wit h int ravenous colist in – no st at ist ical l y signif icant dif f erences being observed among t hese groups. growing emergence of mult iresist ant microorganisms such as A. baumannii and P. aeruginosa complicat es t he t reat ment of pat i ent s wi t h i nf ect i ons associ at ed t o mechani cal vent ilat ion (pneumonia and t racheobronchit is), and has led t o a change in t he approach t o t reat ment and t he ut ilizat ion of ant ibiot ics such as colist in. The guides of t he American Thoracic Societ y (ATS) indicat e t hat ant ibiot ics in aerosol can be used f or t he t reat ment of i nf ect i ons caused by m i c r oor gani sm s w i t h a h i gh m i n i m u m i n h i b i t or y concent rat ion (MIC) and which are resist ant t o syst emic t reat ment s. 5 100% 100% 100 90 76.9% 76,9% 80 70 66,7% 66.7% 66.7% 66,7% 66.7% 66,7% 60 50 42.9% 42,9% 40 COLISTINA Intravenous Intravenosa Nebulizada Nebulized Mixta Mixed 30 20 10 Discussion Of t he different nosocomial infect ions seen in t he Int ensive Care Unit , special ment ion must be made of respirat ory infect ions in pat ient s subj ect ed t o mechanical vent ilat ion, in view of t heir import ant frequency and repercussions. The 0 COLONIZATION COLONIZACIÓN (ENS) (ENS) INFECTION INFECCIÓN (p<0.05) (P < 0,05) Fi gur e 1 Mi cr obi ol ogi cal er adi cat i on. Per cent age of eradications in colonized and infected patients (tracheobronchitis and nosocomial pneumonia). Documento descargado de http://www.medintensiva.org el 17/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. 230 Colist in (polymyxin B) is an ant ibiot ic of great bact ericidal capaci t y w i t h concent r at i on- dependent act i vi t y i n applicat ion t o gramnegat ive bacilli, including mult iresist ant st rains. Following it s discovery in t he 1940s, colist in use peaked i n t he 1960s, f ol l owed by abandonment of i t s administ rat ion due t o t he associat ed neurot oxicit y and nephrot oxicit y. In t he 1980s t he drug was reint roduced in nebulized f orm f or t he t reat ment of pat ient s wit h cyst ic f ibrosis col onized by P. aer ugi nosa, in view of t he good result s obt ained in t hese cases. 3,4 The aerosol administ rat ion of ant ibiot ics is now being seen as a benef icial f orm of t reat ment in pat ient s wit h respirat ory inf ect ion. 6 This is mainly due t o t he high drug concent rat ions reached in t he respirat ory t ract . In effect , t he administ rat ion of t wo million nebulized unit s reaches peak sput um concent rat ion wit hin one hour – t his being over 10 t imes higher t han t he MIC of P. aer ugi nosa and A. baumanni i . Post er i or l y, t he concent rat ion decreases, but maint ains an average of 4 μg/ ml 12 hour s af t er admi ni st r at i on, wi t h l ow syst emi c concent r at i ons. 3 In t hi s w ay, nebul i zed or aer osol administ rat ion would allow a reduct ion of t he drug doses used in int ravenous ant ibiot herapy, by deposit ing t he drug direct ly in t he sit e of infect ion. The blood concent rat ions in t urn would be reduced, t oget her wit h t he t oxic side effect s of colist in. 7 At present , when using t he nebulized rout e, t he r ecommended dose i s 500, 000 uni t s/ 12 h f or pat i ent s weighing under 40 kg, and one million unit s/ 8-12 h for t hose weighing over 80 kg. In t he case of recurrent infect ions, t he recommendat ion would be t wo million unit s every 8 hours. 8,9 The main inconvenience of t he aerosol f ormulat ion is t he p ot ent i al i nd uct i on of l ocal si d e ef f ect s such as bronchoconst rict ion. 6 In Oct ober 2009, Qin Lu et al. published an experiment al st udy in pigs involving t he induct ion of vent ilat or-associat ed pneumoni a due t o P. aer ugi nosa wi t h a MIC f or col i st i n < 2 μg/ ml. 10 The animals were t reat ed wit h nebulized or int ravenous colist in, and were sacrificed 48 hours aft er t he t reat ment . In t he aerosol group t he mean peak concent rat ion i n l ung t i ssue was 2. 8 μg/ g. In t he pi gs t r eat ed wi t h int ravenous col ist in, t he col ist in concent rat ions in l ung t i ssue were undet ect abl e. The aut hors concl uded t hat nebulized colist in of f ers rapid and ef f ect ive bact ericidal act ion, and proposed t he conduct ion of st udies warrant ing it s use in pat ient s wit h pneumonia, as well as it s combinat ion wit h t he int ravenous rout e in pat ient s wit h bact eremic pneumonia. These dat a had been correlat ed t o clinical dat a from previous years. In t hi s cont ext , i n 2005, Kw a et al . publ i shed a ret rospect ive st udy involving 21 pat ient s wit h pneumonia due t o A. baumannii and P. aeruginosa. They reviewed t he pat ient s t reat ed wit h nebul ized col ist in and recorded a microbiol ogical eradicat ion rat e of 85. 7% and a cl inical r ecover y r at e of 57. 1%. 11 In 2007, Per ei r a et al . used inhalat ory colist in in 14 pat ient s wit h pneumonia in which previous t reat ment wit h int ravenous colist in had failed, and in anot her 5 pat ient s diagnosed wit h t racheobronchit is12 – all of t hem wit h colist in-sensit ive gramnegat ive bacilli. The pat i ent s wi t h pneumoni a wer e j oi nt l y t r eat ed wi t h int ravenous and nebulized colist in, while t he pat ient s wit h t racheobronchit is received only nebulized colist in; 93% of t he pneumonias met crit eria of clinical recovery at t he end of t reat ment , and 100% of t he cases of t racheobronchit is M.J. Pérez-Pedrero et al were healed. In 2008, Michalopoulos et al. used nebulized col i st i n t o t r eat 60 cr i t i cal pat i ent s di agnosed wi t h pneumoni a caused by A. baumanni i , P. aer ugi nosa and Kl ebsi el l a pneumoni ae; 57 of t he pat ient s also received syst emic t reat ment . 13 The aut hors observed clinical recovery and microbiological eradicat ion in 83.3%of t he cases, and concluded t hat nebulized colist in can be regarded as an adj uvant t o i nt ravenous admi ni st rat i on i n pneumoni as caused by col i st i n-sensi t i ve mi croorgani sms i n cri t i cal pat ient s. Likewise in 2008, Fagalas et al. published a series of 5 pat i ent s w i t h nosocomi al pneumoni a due t o A. baumannii and P. aeruginosa t reat ed only wit h nebulized colist in and wit hout adj unct ive int ravenous t herapy. Four of t he 5 pat ient s (80%) recovered and survived. 14 The aut hors concluded t hat t reat ment wit h nebulized colist in alone in applicat ion t o pneumonias caused by microorganisms t hat are sensit ive t o t his drug deserves t o be st udied more in dept h. In 2009, Korbila et al. published a ret rospect ive st udy of 78 pat ient s wit h vent ilat or-associat ed pneumonia t reat ed wit h int ravenous plus nebulized colist in, versus 43 pat ient s t reat ed wit h t he int ravenous f ormulat ion only. 15 Clinical recovery was recorded in 79.5%of t he pat ient s in t he first group and in 60.5%of t he pat ient s t reat ed wit h int ravenous colist in only – t he dif f erence being st at ist ically signif icant (p < 0.025). Our study shows colistin in mixed administration (nebulized and intravenous) to be superior for the treatment of respiratory infect ion due t o A. baumannii t han int ravenous t reat ment only. The use of nebulized colist in, alone or in combinat ion, improved t he result s in t erms of microbiological eradicat ion and clinical recovery in all the treatment groups. Our st udy has clear limit at ions, including it s ret rospect ive nat ure and t he limit ed number of pat ient s in each group. Anot her limit at ion is t he use of different dosing regimens. The regimen was decided by t he physician t reat ing t he pat ient , and was independent of t he nosologic charact erist ics of t he case (colonizat ion, t racheobronchit is or pneumonia). The exist ing lit erat ure describes different dosing regimens, t hough none have been shown t o be superior t o t he rest . Nevert heless, we feel t he regimen used t o be represent at ive of our cl inical experience in t he dail y use of nebul ized colist in in pat ient s of t his kind. 16 Special ment ion should be made of t he group of pat ient s wit h t racheobronchit is t reat ed wit h nebulized colist in only. The 5 pat ient s recovered, and microbiological eradicat ion was achieved in all of t hem, while in cont rast in t he group of subj ect s t reat ed via t he int ravenous rout e, only t hree out of 5 r ecover ed (60%). These dat a ar e not st at i st i cal l y signif icant , due t o t he small number of pat ient s involved, t hough despit e t he l imit at ions of our st udy, t he resul t s suggest t hat nebulized colist in alone should be viewed as an alt ernat ive for t he t reat ment of t hese pat ient s. In our series, t he pat ient s t reat ed wit h nebulized colist in achieved a significant ly higher microbiological eradicat ion rat e t han t he group subj ect ed t o int ravenous t reat ment . The cases diagnosed wit h pneumonia also achieved bet t er result s wit h combinat ion t reat ment t han wit h int ravenous dosing alone. The infect ed pat ient s who all recovered (100%) wit h nebulized colist in all present ed t racheobronchit is; no pat i ent di agnosed wi t h pneumoni a was t r eat ed wi t h nebul i zed col i st i n onl y. On j oi nt l y consi der i ng al l t he pat i ent s wi t h i nf ect i on, i . e. , t r acheobr onchi t i s and Documento descargado de http://www.medintensiva.org el 17/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. Nebulized colist in t reat ment of mult i-resist ant Acinet obact er baumannii pulmonary infect ion in crit ical ill pat ient s pneumoni a, t he mi cr obi ol ogi cal er adi cat i on r at e was likewise significant ly favorable t o t he group wit h nebulized colist in versus t hose administ ered int ravenous colist in only. In conclusion, our dat a coincide wit h t hose f ound in t he lit erat ure: t reat ment wit h inhalat ory colist in improves t he result s in pat ient s wit h respirat ory infect ions produced by A. baumannii. Despit e t he limit at ions of our st udy, we feel t hat inhalat ory colist in should be regarded as an adj unct t o int ravenous dosing of t he drug in pat ient s wit h nosocomial pneumonia due t o A. baumannii. Colist in administ rat ion in nebulized form only, wit hout associat ed int ravenous t herapy, could be an alt ernat ive in pat ient s wit h t racheobronchit is, or might possibly be t he t reat ment of choice f or securing microbiological eradicat ion in colonized pat ient s. Conflict of interest 6. 7. 8. 9. 10. 11. The aut hors declare no conflict of int erest . 12. References 1. Gar nacho- Mont er o J, Amaya- Vi l l ar R. Mul t i r esi st ant Aci net obact er baumanni i i nf ect i ons: epi demi ol ogy and management . Curr Opin Infect Dis. 2010;23:332-9. 2. Michal opoul os AS, Karat za DC. Mul t idrug-resist ant Gramnegat ive infect ions: t he use of colist in. Expert Rev Ant i Infect Ther. 2010;8:1009-17. 3. Rat j en F, Riet schel E, Kasel D, Kasel D, Schwiert z R, St arke K, et al. Pharmacokinet ics of inhaled colist in in pat ient s wit h cyst ic fibrosis. J Ant imicrob Chemot her. 2006;57:306-11. 4. Michalopoulos A, Kasiakou SK, Mast ora Z, Rellos K, Kapaskelis AM, Falagas ME. Aerosolized colist in f or t he t reat ment of nosocomi al pneumonia due t o mul t idrug-resist ant gramnegat ive bact eria in pat ient s wit hout cyst ic fibrosis. Crit Care. 2005;9:R53-59. 5. American Thoracic Societ y/ Inf ect ious Disease Societ y of America. Guidel ines f or t he management of adul t s wit h 13. 14. 15. 16. 231 hospit al -acquired, vent il at or-associat ed, and heal t hcareassociat ed pneumonia. Am J Respir Crit Care Med. 2005;171: 388-416. Dhand R. The role of aerosolized ant imicrobials in t he t reat ment of vent ilat or-associat ed pneumonia. Respir Care. 2007; 52: 866-84. Michalopoulos A, Papadakis E. Inhaled ant i-inf ect ive agent s: emphasis on colist in. Infect ion. 2010;38:81-8. Palmer LB. Aerosolized ant ibiot ics in crit ically ill vent ilat ed pat ient s. Curr Opin Crit Care. 2009;15:413-8. Linden PK, Pat erson DL. Parent eral and inhaled colist in f or t reat ment of vent ilat or-associat ed pneumonia. Clin Infect Dis. 2006;43:S89-94. Lu Q, Girardi C, Zhang M, Bouhemad B, Louchahi K, Pet it ij ean O, et al. Nebulized and int ravenous colist in in expeimenal neumonia caused by Pseudomonas aeruginosa. Int ensive Care Med. 2010;36:1147-55. Kwa AL, Loh C, Low JG, Kurup A, Tam VH. Nebulized colist in in t he t r eat ment of neumoni a due t o mul t i dr ug-r esi st ant Acinet obact er baumannii and seudomonas aeruginosa. Clin Infect Dis. 2005;41:754-7. Perei ra GH, Mul l er PR, Levi n AS. Sal vage t reat ment of pneumonia and init ial t reat ment of t racheobronchit is caused by mul t idrug-resist ant gram-negat ive bacil l i wit h inhal ed polymyxin B. Diagn Microbiol Infect Dis. 2007;58:235-40. Michalopoulos A, Fot akis D, Virt zili S, Vlet sas C, Raft opoulou S, Mast ora Z, et al. Aerosolized colist in as adj unct ive t reat ment of vent ilat or-associat ed pneumonia due t o mult idrug-resist ant Gram-negat ive bact eria: A prospect ive st udy. Resp Med. 2008;102:407-12. Falagas ME, Siempos II, Raf ailidis PI, Korbila IP, Ioannidou E, Michalopoulos A. Inhaled colist in as monot herapy for mult idrugresist ant gram (–) nosocomial pneumonia: A case series. Respirat ory Medicine. 2009;10:1-7. Korbila IP, Michalopoulos A, Rafailidis PI, Nikit a D, Samonis G, Fal agas ME. Inhal ed col i st i n as adj unct i ve t her apy t o int ravenous colist in f or t he t reat ment of microbiologically document ed vent ilat or-associat ed pneumonia: a comparat ive cohort st udy. Clin Microbiol Infect . 2010;16:1230-6. Ol aechea P. Epi demi ol ogía e i mpact o de l as i nf ecci ones nosocomiales. Med Int ensiva. 2010;34:256.