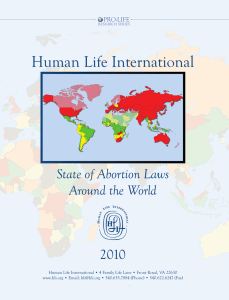
Downloaded from inpractice.bmj.com on September 4, 2014 - Published by group.bmj.com FARM ANIMAL PRACTICE Aborted bovine fetus. Picture, R. D. Murray Bovine abortion: aetiology and investigations EMMA CABELL ABORTION in cattle is a significant cause of reproductive wastage and is of economic importance as a single abortion event in a dairy herd is estimated to cost £630. Some abortions are due to infectious diseases, several of which are zoonotic. Sporadic abortions occur in any herd, but once the incidence exceeds 3 per cent, or several abortions occur in close succession, further investigations must be carried out to try to determine the cause so that control measures can be instigated. This article reviews the common causes of abortion in cattle and outlines an approach to the investigation of an abortion outbreak, describing the tests available for diagnosis. DIAGNOSTIC RATES FOR ABORTIONS The diagnostic rate achieved for abortions is generally low, averaging about 35 per cent of all cases where a fetus and placenta are submitted for an abortion investigation. An important reason for this is that, in cattle, there is frequently a delay between fetal death and expulsion. Autolysis occurs rapidly prior to expulsion, and can have a significant deleterious effect on the sensitivity of diagnostic tests. The causes of abortion can broadly be divided into non-infectious and infectious. In most cases where a diagnosis is reached, the cause is infectious, although non-infectious causes probably account for many un- For the purposes of this article, abortion is defined as the expulsion of a recognisable dead or nonviable fetus prior to the end of the normal gestation period and includes premature and stillborn calves. diagnosed abortions. The relative frequencies of diagnosis of the various infectious causes of abortion are shown in the diagram below. Neospora species 26% Other 30% Emma Cabell graduated from the Royal Veterinary College in 1993. She spent nearly five years in predominantly farm animal practice in north Wales before taking up a residency in ruminant medicine at Liverpool, where she subsequently became a lecturer in the department of livestock health and welfare. Since 2003, she has worked in the Veterinary Laboratories Agency (VLA) Surveillance Centre at Liverpool. She holds the diploma in bovine reproduction from Liverpool, and the RCVS certificate in cattle health and production. Arcanobacter pyogenes 8% Bovine virus diarrhoea 8% Salmonella Dublin 7% Bacillus licheniformis 21% Autolysis of fetal internal organs. Note the large volume of blood-stained fluid within the thoracic and peritoneal cavities. Picture, R. D. Murray In Practice ● SEPTEMBER 20 07 Diagnosis of bovine fetopathy in 2006 as a percentage of all cases of fetopathy where a diagnosis was reached (n=842). From VIDA (2006) 455 In Practice (2007) 29, 455-463 Downloaded from inpractice.bmj.com on September 4, 2014 - Published by group.bmj.com TOXIC Safety precautions Due to the zoonotic potential, care must be taken when handling abortion material to ensure that veterinary surgeons and their employees are not at risk (Health & Safety at Work etc Act 1974). In particular, pregnant women should avoid contact with aborted material. Protective clothing, including waterproof overalls, rubber gloves and Wellington boots, should be worn when handling fetuses and placentas. Cut-proof gloves should be worn if postmortem examination and sample collection is carried out. All instruments, overalls and other equipment should be cleaned and disinfected with an approved disinfectant at the appropriate dilution (see www.defra.gov.uk/animalh/ diseases/control/testing_disinfectants.htm for further information). NON-INFECTIOUS CAUSES PHYSICAL Abortion can be caused by trauma, insemination, hyperthermia and twinning. NUTRITIONAL Iodine deficiency has been associated with stillbirths and weak newborn calves. In affected cases, the fetal thyroid gland is enlarged, usually weighing >30 g. The most common cause of iodine deficiency in farm animals is failure to provide iodine in the diet. Some parts of the UK are iodine deficient, while secondary deficiency has also been associated with high calcium intake, the feeding of Brassica species and the application of human sewage sludge on pasture. Micronutrients are not commonly implicated, but as well as iodine deficiency and toxicity, selenium/vitamin E deficiency has been associated with bovine abortions in the UK (Mee 2004). An increase in the prevalence of abortions has been observed in herds where the diet is deficient in vitamin A or its precursor β-carotene. Several poisonous plants, including hemlock, cypress and juniper, have been associated with abortion in cattle in the UK, although abortion is unlikely to occur in the absence of other signs of poisoning. The consumption of needles of the ponderosa pine, found in some parks and experimental forestry plantations in the UK, is a recognised cause of bovine abortion, resulting in a reduction of serum progesterone levels. Ergot alkaloids have a known abortigenic action, although abortion is rare in poisoned animals. Cattle frequently abort following an outbreak of nitrate/nitrite poisoning; this is probably due to methaemoglobinaemia leading to hypoxia in the dam and subsequent fetal hypoxia. Other clinical signs of poisoning such as severe dyspnoea, muscle twitching and brown mucosae and blood are likely to be present. Common sources of nitrate/nitrite on farms are fertilisers and certain plants. GENETIC Genetic abnormalities that result in congenital malformations may cause fetal death and consequent abortion. An example is complex vertebral malformation (CVM), which occurs in purebred Holstein cattle and is caused by a simple recessive genetic defect where both parents are carriers. Affected calves are rarely carried to term. Other defects that may result in the birth of dead calves include dyschondroplasia (bulldog calves) and chromosomal abnormalities. INFECTIOUS CAUSES Infections during the early stage of gestation may result in early embryonic death by directly affecting the embryo. Infections at a later stage may lead to abortion, stillbirths or the birth of weak live calves. Some infections indirectly affect fetal survival by the impairment of uterine function (eg, maternal endotoxaemia due to acute coliform mastitis). Endotoxaemia can evoke prostaglandin synthesis, leading to subsequent abortion, or induce intravascular coagulation, which interferes with placental circulation, resulting in fetal hypoxia. Other infections may (left) Normal thyroid gland and (right) thyroid gland hyperplasia. Pictures, R. D. Murray 456 In Practice ● SEPTEMBER 20 07 Downloaded from inpractice.bmj.com on September 4, 2014 - Published by group.bmj.com directly damage the maternal component of the placenta (eg, Brucella abortus infection). Maternal conditions that lead to fetal hypoxia (eg, severe pneumonia, circulatory failure resulting from traumatic pericarditis, or dehydration and acidosis as a consequence of carbohydrate engorgement) can also lead to fetal death and abortion. Infectious causes can be divided into bacterial, viral, protozoal and fungal agents (see table below), and are discussed in the following sections. BACTERIA Brucella abortus B abortus infection has caused enormous losses to dairy and beef cattle industries worldwide, and eradication schemes exist in many countries. Cattle become infected by ingesting the organism from infected abortion material/genital discharges or contaminated pasture, food or water. It causes endometritis, placentitis and abortion. Retained fetal membranes are a common sequela. COMMON INFECTIOUS CAUSES OF ABORTION IN CATTLE Agent Epidemiology Time of abortion Pathology Fetus Clinical features Abortion rate Notifiable disease. Abortion, birth of weak/ dead calves, retained placenta, infertility Up to 90% in susceptible herds 6+ months Necrosis of cotyledons and leathery, opaque placenta with oedema May be pneumonia, which is only detectable on histopathology Campylobacter fetus fetus Abortion Sporadic 4 to 8 months Mild placentitis Mild fibrinous pleurisy and peritonitis, bronchopneumonia Leptospira hardjo Few cows exhibit signs other than abortion Up to 30% 6+ months Avascular placenta, atonic yellow-brown cotyledons, brown gelatinous oedema between allantois and amnion Fetal death is common Arcanobacter pyogenes Abortion occasionally preceded by systemic illness and mastitis, and/or followed by endometritis Sporadic or multiple 6+ months Suppurative placentitis Often associated with fetal pneumonia (on histopathology) Salmonella species Abortion, frequently without other clinical signs in the dam Sporadic. May be a herd outbreak Any time, 6 to 9 months No specific lesions No specific lesions Listeria monocytogenes Abortion Sporadic. Rare reports of abortion storms Late, towards end of gestation Placentitis, multiple yellow or grey necrotic foci in cotyledons May be multiple yellow or grey necrotic foci in liver Bacillus licheniformis Late abortions or live calves with evidence of placental lesions Sporadic Late, 5+ months Placentitis and dry, leathery, yellow-brown allantochorion. Oedema of allantochorion around cotyledons, giving appearance of vesicles. Haemorrhagic and necrotic cotyledons May be fibrinous pleurisy, pericarditis and peritonitis Depend on the stage of pregnancy at which the cow becomes infected (see table, page 460) Usually low From 2 months No specific gross lesions May be congenital abnormalities of the central nervous system or eyes (eg, cerebellar hypoplasia) Often associated with previous or intercurrent respiratory disease in the herd Sporadic, but can be up to 60% 4 months to term No significant gross lesions May be foci of hepatic necrosis Abortion, stillbirths and live births may occur Usually associated with sporadic abortions. Can occasionally cause abortion storms (≥10% of at-risk cows aborting over a six-week period). Repeat abortions from the same cow are common. Prevalence of infection in herds may be high. Congenital transmission is the only known method in cattle 3 to 8 months (mean 5·5 months) No characteristic lesions in placenta Inflammatory lesions widespread in fetus. Non-suppurative encephalitis and myocarditis common with parasite present, identified by immunohistochemistry More prevalent from December to March Sporadic, up to 5 to 10% in some herds 4 to 9 months Diffuse or multifocal thickening, leathery, yellow-brown appearance of cotyledons and intercotyledonary areas May be small, raised, grey-white soft lesions, or diffuse white areas on skin. Resembles ringworm Bacteria Brucella abortus Viruses Bovine virus diarrhoea virus Bovine herpesvirus type 1 Protozoa Neospora caninum Fungi eg, Aspergillus species mycosis Placenta Adapted from Miller (1986) and Radostits and others (2000) 458 In Practice ● SEPTEMBER 20 07 Downloaded from inpractice.bmj.com on September 4, 2014 - Published by group.bmj.com Placental lesions in a case of brucellosis. Picture, VLA Truro sheep may be ‘silent’ carriers and also a potential source of infection. Leptospirosis accounted for less than 2 per cent of total abortion diagnoses from 2003 to 2006 (VIDA 2006) and appears to be declining in importance. This may be a reflection of widespread vaccination. Until recently, the diagnostic method of choice had been the detection of leptospires in fetal kidney using the fluorescent antibody test (FAT), which is relatively insensitive. This has now been replaced by a PCR test for pathogenic leptospires in fetal kidney. Early validation studies for this test report a significantly increased sensitivity and specificity. Culture is considered the gold standard, but is expensive, time consuming and requires expertise, and is therefore not practical for routine diagnostic use. With the more frequent use of PCR testing to investigate suspected cases, a more accurate indication of the true prevalence of abortion due to Leptospira species in the UK should be obtained. Bacillus licheniformis Acid-fast rods typical of Brucella organisms on a vaginal swab smear. Picture, VLA Starcross In non-pregnant animals, the udder and supramammary lymph nodes are colonised and infection of the placenta may occur during the next gestation. Infected cattle often shed the organism in milk, which presents a serious risk to human health. It is a legal requirement for cattle keepers to report every abortion or premature calving to a divisional veterinary manager (DVM) under Article 10 of the Brucellosis (England) Order 2000 and the equivalent legislation in Scotland and Wales. An abortion or premature calving is defined as ‘an abortion or calving that takes place less than 271 days after service, or 265 days after implantation or transfer of an embryo, whether the calf is born dead or alive’. Salmonella species In the UK, Salmonella Dublin is endemic in cattle and is the most common species of Salmonella causing abortion. Many other Salmonella species may be involved in individual cases. Aborting cows are often pyrexic and may be diarrhoeic although some may show no clinical signs other than abortion. All salmonellae, including S Dublin, are zoonotic. S Dublin rarely causes disease in humans but, if it does, infection can be severe. All Salmonella isolates must be reported under zoonoses legislation (The Zoonoses Order 1989) to the appropriate nominated officer – that is, a veterinary investigation officer in regional VLA laboratories in England and Wales, and the DVM of Animal Health (formerly the State Veterinary Service) in Scotland. Bacillus licheniformis is frequently associated with sporadic bovine abortion. During 2006, it accounted for 21 per cent of VLA abortion submissions where a diagnosis was reached (VIDA 2006). Experimental studies have demonstrated a predilection for the placenta, especially the fetal membranes and the fetal side of the placentome (Agerholm and others 1999). The organism is ubiquitous, although silage, run-off water/liquor, foodstuffs and bedding that become contaminated with silage effluent, and wet spoilt hay are the most likely sources of infection. The pathogenesis is not known, but probably involves haematogenous spread to the reproductive tract following ingestion. Listeria species Listeria monocytogenes is ubiquitous in the environment, being present in soil, sewage effluent, bedding and foodstuffs. The organism gains entry by ingestion and has a predilection for the placenta, causing a placentitis. A substantial number of outbreaks have occurred following the start of silage feeding. Other manifestations of listeriosis, including encephalitis and eye infections, are rarely seen in conjunction with abortion. The disease accounted for 3 to 4 per cent of abortion diagnoses from 2003 to 2006 (VIDA 2006). Other Listeria species, such as Listeria ivanovii and Listeria innocua, also occasionally cause abortion. Arcanobacter pyogenes Arcanobacter pyogenes is sporadically isolated from aborted calves and accounted for 8 per cent of abortion Leptospira species Leptospira interrogans serovar hardjo causes abortion in cattle four to 12 weeks after infection, with or without additional clinical signs of illness in the dam. The pathogen is transmitted venereally and via urine and abortion material, and is a potential zoonosis. Watercourses can become contaminated and be a source of infection, while In Practice ● SEPTEMBER 20 07 Placentitis due to Bacillus licheniformis (arrow). Haematoxylin & eosin, magnification x200. Picture, M. Wessels 459 Downloaded from inpractice.bmj.com on September 4, 2014 - Published by group.bmj.com diagnoses during 2006 (VIDA 2006). Experimental evidence suggests that it is a primary pathogen, directly capable of causing abortion. Campylobacter species Two species of Campylobacter affect the reproductive tract of cattle. Campylobacter fetus venerealis is commonly associated with infectious infertility and early embryonic loss, while Campylobacter fetus fetus, a commensal organism of the intestinal tract, causes sporadic abortions. Mycoplasma and Ureaplasma species Mycoplasma species are occasionally isolated from aborted fetuses. Mycoplasma bovis causes mastitis and polyarthritis in cattle and, in some cases, extensive lesions in the uterus. Ureaplasma infections are also occasionally implicated in bovine abortion, with the main route of transmission thought to be venereal. Mycoplasma and Ureaplasma species are not considered to be major infectious causes of abortion and routine testing is not undertaken. Other bacterial infections Other bacteria that are rarely isolated from bovine fetuses include Chlamydophila abortus and Coxiella burnetii (Q fever), both of which have zoonotic potential. VIRAL DISEASE Bovine virus diarrhoea Bovine virus diarrhoea (BVD) virus is widespread in the UK, with approximately 95 per cent of herds having serological evidence of BVD infection (Paton and others 1998). Reproductive losses may be the most economically important clinical consequences associated with BVD. The potential reproductive outcomes following infection of a naive cow with BVD virus are listed in the table below. BVD infection is maintained in a cattle population by the development of persistently infected (PI) animals. These act as a potent source of infection for naive animals and are estimated to make up between 1 and 2 per cent of the national herd, and potentially a much higher proportion within an infected individual herd. Conversely, some herds (eg, those in the Premium Cattle Health Scheme) are free from infection. It is generally POTENTIAL REPRODUCTIVE OUTCOMES FOLLOWING INFECTION WITH BOVINE VIRUS DIARRHOEA (BVD) VIRUS AT DIFFERENT STAGES OF GESTATION Potential manifestations of infection in naive dams Period of gestation when these are most likely to occur Decreased conception rates, early embryonic death 0 to 45 days Abortions Fetal death following BVD virus infection can occur at any time during gestation, but is most common during the first trimester. Fetal reabsorption, mummification or expulsion can occur Immunotolerance Fetuses that survive infection with non-cytopathic BVD virus at between 80 and 125 days’ gestation invariably develop immunotolerance to the virus and subsequently become persistently infected Congenital defects Fetal infection at between 100 and 150 days’ gestation often results in the development of congenital defects Fetal immune response to BVD virus and virus cleared Late gestation (125 to 285 days) when immunocompetence and organogenesis are usually complete From Grooms (2004) 460 Cerebellar hypoplasia caused by mid-gestational bovine virus diarrhoea virus infection. Picture, R. D. Murray considered that fetal infection prior to the development of immunocompetence (at days 90 to 120) results in either fetal death or the development of a lifelong persistent infection. By day 125, the immune system is becoming fully functional and infection after this time usually results in a competent immune response and subsequent elimination of the virus, so that at birth the calf is BVD antibody positive but antigen (virus) negative. With the recent development of a real-time reverse transcriptase (RT) PCR test for BVD RNA, it was anticipated that the detection rate for the virus in aborted fetuses would increase. In fact, fewer abortions than expected have been attributed to BVD infection despite the increased sensitivity of the RT-PCR test, which suggests that, at present, there is still no evidence that BVD is a major cause of abortion. Vaccination against BVD is likely to have influenced this as it reduces the occurrence of fetal infection. Even if BVD antigen is detected in a fetus, which is a significant finding, it is still entirely possible that BVD was not the cause of abortion, as many PI animals are born and live for some time, with most succumbing to mucosal disease at between six and 24 months of age. Some PI animals live long enough to join the adult herd and produce PI calves, so it is advisable to test the dam of a fetus found to be positive for BVD virus to determine if she is a PI animal. The indirect fluorescent antibody test (IFAT) for the detection of BVD antibody can be used in fetuses of 125 days’ gestation or greater to indicate BVD challenge in utero. Both type 1 and type 2 BVD virus are present in the UK, with type 1 being the most widespread. RT-PCR is able to differentiate between the two. Immunohistochemistry on fixed brain tissue is a useful aid to diagnosis in fetuses in the first trimester of gestation prior to the development of immunocompetence. Infectious bovine rhinotracheitis Infectious bovine rhinotracheitis (IBR) is caused by bovine herpesvirus type 1 (BHV-1). It usually results in respiratory disease, but abortion may be seen in cows up to 100 days after infection. Abortion generally occurs in mid- to late pregnancy and aborting cows may or may not have shown respiratory signs previously. Where systemic and respiratory disease results in pyrexia, which is often very marked, this can cause abortion. The diagnosis of IBR-related abortions is difficult due to the rapidly developing necrotising placentitis and expulsion of the fetus before it is infected (reported experimentally). Currently, a FAT is used to detect IBR antigen, but, in common with other FAT tests and virus isolation, this test is much less sensitive in autolysed tissue. In Practice ● SEPTEMBER 20 07 Downloaded from inpractice.bmj.com on September 4, 2014 - Published by group.bmj.com Immunohistochemistry on internal organs can be useful where lesions of multifocal necrosis are observed on postmortem examination. PROTOZOAL DISEASE Cluster of Neospora caninum tachyzoites in a cardiac myofibre. Peroxidase–antiperoxidase immunostaining with N caninum-specific polyclonal antibody, magnification x100. Picture, E. H. Gibney Neosporosis Neospora caninum was first recognised as a cause of abortion in cattle in 1989 and is now the most commonly diagnosed infectious cause. Oocysts are excreted by dogs and ingested by intermediate hosts, including cattle, sheep, goats and horses. Tissue cysts and tachyzoites are the stages of the life cycle found in cattle. Tachyzoites develop in a wide range of tissues, including placenta and amniotic fluids, while tissue cysts (containing bradyzoites) are found only within the central nervous system. The vertical route is the major mode of transmission in cattle, with infection of calves in utero occurring due to recrudescence of disease in chronically infected cows. Horizontal cow-to-cow transmission does not occur. 4 µm Cows of any age may abort from three months’ gestation to term, although most neosporosis-induced abortions occur at six to seven months’ gestation. Fetuses may die in utero, be resorbed, mummified, autolysed, stillborn or born alive with clinical (neurological) signs, or born clinically normal, but chronically infected; however, congenitally infected calves are generally clinical- Postmortem examination of a fetus and placenta When it is not possible to submit a fetus and placenta to a laboratory, the practitioner can perform a useful postmortem examination and collect appropriate samples either on the farm or back at the practice. Technique ■ Examine the skin of the fetus and placenta for lesions. Gross lesions are seen relatively infrequently and are usually associated with mycotic and B licheniformis infections. Where the fetus is full term and stillborn, look for signs of dystocia (eg, oedema of the head, neck and tongue, widespread petechial haemorrhages and rib fractures) ■ If possible, measure the crown-to-rump length (CRL). Calculate the gestation length in days (Y) using the formula: Y = 2·5 x (21 + CRL) ■ Place the fetus on its back and incise into the axillae. Reflect the scapulae and disarticulate the hip joints to stabilise the carcase ■ Open the abdomen by incising along the midline and the edges of the ribs ■ Open the thorax by incising along the costochondral junction on each side ■ Record any gross pathology Gross pathological findings in the aborted fetus are frequently unremarkable, but can include purulent or fibrinous inflammation, which are suggestive of an infectious insult. Sample collection FOR CULTURE ■ Fetal stomach contents collected aseptically into a Vacutainer, or using a 5 ml syringe and 16 gauge needle for ‘thick’ contents ■ Liver or lung (4 cm cube approximately) ■ Placenta with several cotyledons In Practice ● SEPTEMBER 20 07 Kit for sample collection ■ Rubber and cut-proof gloves ■ Postmortem knife ■ Side-cutting pliers ■ Hacksaw ■ Scissors ■ Rat-tooth forceps ■ Number 22 scalpel blade and handle ■ Vacutainer and needle ■ 5 ml syringe and 16 gauge needle ■ Disposable pipette for obtaining fetal fluid ■ Bijou vial x 2 ■ Sterile sample pots x 5 FOR NEOSPORA IFAT (AND BVD IFAT, IF REQUIRED) ■ 2 ml fetal fluid from thoracic, pericardial or abdominal cavities using a pipette and bijou vial FOR BVD RT-PCR ■ Thymus (1 cm cube in bijou vial) FOR PATHOGENIC LEPTOSPIRES PCR ■ Kidney (1 cm cube in bijou vial) FOR HISTOPATHOLOGY ■ If possible, fix the following tissues in 10 per cent formalin: – 1 to 2 cm cube of heart – Caruncle/cotyledon with intercotyledonary membrane – Liver, lung and kidney – Whole brain. Unless the fetus is nearly full term, the bones of the skull are soft and not completely fused and it is easy to remove them using scissors or side-cutting pliers. In stillborn animals, the skull will need to be sawed. First reflect the skin from the head, and make the first cut caudal to the lateral canthus of the eye and at 90° to the midline. Two cuts should then be made approximately 2·5 cm either side of the midline through the nuchal eminence, and extending cranially through the frontal bones and crossing the first cut. Caudally, they extend towards the occipital condyles. A bone chisel can be used as a lever to remove the frontal bones. The dura mater is incised and reflected, taking care also to cut the tentorium cerebelli, a crescentic fold that occupies the fissure between the cerebellum and cerebral hemispheres. The brain can be removed by tilting the head and severing the olfactory, optic and remaining cranial nerves. STILLBORN CALVES ■ Remove the entire thyroid gland, which consists of two lobes connected by a band adherent to the thyroid cartilage. If possible, weigh the gland, then fix half in formalin and submit the fresh half for tissue biochemistry, specifically iodine analysis. FOR MATERNAL SEROLOGY ■ Dam serum or clotted blood Further information Fetuses and placentas should be disposed of in accordance with the Animal By-Products Regulations 2005. For further information in each of the devolved countries, see: ■ ENGLAND. www.defra.gov.uk/animalh/ by-prods/default.htm ■ WALES. new.wales.gov.uk/topics/ environmentcountryside/ahw/animal_ byproducts_waste/?lang=en ■ SCOTLAND. www.scotland.gov.uk/ Topics/Agriculture/animal-welfare/ policies/PolicyInfo/AnimalByProducts/ Introduction 461 Downloaded from inpractice.bmj.com on September 4, 2014 - Published by group.bmj.com Placenta showing typical lesions of mycotic abortion. Picture, W. R. Ward Mycotic lesions on the skin of an aborted fetus. Picture, A. P. Foster ly normal (Dubey 2005). Cows that are seropositive to N caninum are 3·5 times more likely to abort than seronegative cows (Davison and others 1999). Congenitally infected retained/replacement heifer calves may themselves infect future offspring or abort. Replacement stock should therefore not be bred from known positive cows. The mechanisms by which Neospora infection of the dam results in abortion are not understood, but appear to involve recrudescence of infection possibly associated with changes in local uterine immune status during pregnancy. Diagnosis of Neospora-induced abortion relies on the demonstration of antibodies to N caninum in fetal fluid by IFAT or in maternal serum by ELISA; this must be supported by histopathology of fetal tissues (particularly the brain and heart) to show multifocal encephalitis and myocarditis, which are consistent with neosporosis. Immunohistochemistry is required to demonstrate the organism in tissues and distinguish it from other protozoa. Other protozoal infections Outbreaks of abortion involving other protozoa, such as Sarcocystis species, are occasionally reported. FUNGAL DISEASE Abortion can be caused by fungal invasion of the placenta and fetus. In the UK, mycotic abortion is much more prevalent from December to March than the rest of the year, suggesting an association with housing and feeding of preserved fodder. Mouldy hay, straw, silage and brewer’s grains are important sources of infection. The fungi most frequently isolated are Aspergillus fumigatus and Absidia, Rhizopus and Mucor species. The lesions on the placenta and calf are fairly characteristic of mycotic infection, but need to be differentiated from those caused by B licheniformis and, to some extent, C abortus – hence the need for laboratory testing. It is possible for infected live calves to be born. The dam does not usually show any other clinical signs associated with fungal abortion. Fungal hyphae can be demonstrated in smears of fetal stomach contents and deep placental cotyledon scrapes, and are cultured using selective media (Sabouraud’s dextrose agar). Detection in placenta alone requires histopathological demonstration of characteristic necrotising placentitis and the presence of fungal hyphae using special stains (periodic acid–Schiff [PAS] reaction or a silver stain such as Grocott’s). 462 Mycotic placentitis. Fungal hyphae (arrows) are clearly visible. Periodic acid–Schiff reaction, magnification x200. Picture, M. Wessels APPROACH TO THE INVESTIGATION OF ABORTION IN CATTLE Investigating every abortion may be considered uneconomical. Caldow and Gray (2004) suggest an interference level of 3 per cent for abortions that occur after pregnancy is confirmed at around six weeks, based on reports that quote unavoidable fetal losses at around 1·7 to 2 per cent. Each abortion should be considered in the light of other clinical findings, such as whether there has been a cluster of abortions or if the aborting cow(s) is/are ill. It must be remembered that many abortifacient agents are potential zoonoses and, under the Control of Substances Hazardous to Health (COSHH) regulations, a farmer has a legal responsibility to protect staff from avoidable health hazards. DIAGNOSIS For a detailed examination to be undertaken, the entire fetus and placenta should be submitted to the laboratory for an abortion investigation. Appropriate tests will be authorised at the discretion of the veterinary investigation officer carrying out the investigation. Placenta (or placentome) is often not submitted, but is frequently very useful in establishing a diagnosis, particularly for fungal, B licheniformis and Chlamydophila infections. The following information is also helpful in assessing the extent of the problem and providing clues about possible pathogens: ■ Age of the dam (heifer/cow); ■ Approximate stage of gestation; ■ Approximate date of first abortion; ■ Number of abortions occurred so far; ■ Number of normal calvings; In Practice ● SEPTEMBER 20 07 Downloaded from inpractice.bmj.com on September 4, 2014 - Published by group.bmj.com LABORATORY TESTS AVAILABLE FOR USE ON FETAL AND PLACENTAL SAMPLES Test Samples required Significance of result Bacteria and fungi (eg, Salmonella Dublin, Arcanobacter pyogenes, Bacillus licheniformis, Aspergillus fumigatus, Brucella abortus, Campylobacter species) Bacterial and fungal culture (all samples). Stained smears for Brucella and Chlamydophila abortus and Coxiella burnetii, and wet preparations for fungal hyphae (fetal stomach contents and deep cotyledonary scrapes) Fetal stomach contents (5 ml), placenta/placentome, liver or lung Culture from fetal viscera is usually significant. Culture only from placenta requires histopathological evidence of placentitis with demonstration of the organism in lesions Bovine virus diarrhoea (BVD) antibody IFAT Fetal fluid (1 ml) A positive result after immunocompetency has been gained indicates fetal exposure. The significance is questionable as late pregnancy challenge is not often fetopathic Bovine virus diarrhoea antigen RT-PCR Immunohistochemistry Lymphoid tissue (eg, thymus) or other viscera (eg, liver) A positive result indicates that the fetus has been infected in utero and, hence, BVD virus may be the cause of the abortion Bovine herpesvirus type 1 antigen FAT Immunohistochemistry Fetal liver A positive result is significant, but the sensitivity of FAT is low. Immunohistochemistry tends to be performed only when suggestive inflammatory lesions are identified in fetal viscera by histopathology Neospora caninum antibody IFAT Fetal fluid (1 ml) A positive result indicates fetal infection in utero (histopathology is required to demonstrate lesions to indicate if it is the cause of abortion) Leptospira hardjo PCR Fetal kidney PCR recently developed and sensitivity is much greater than previously used FAT Iodine deficiency (stillbirths only) Thyroid weight Thyroid iodine concentration Histopathology of thyroid gland Fetal thyroid gland Half thyroid gland (fresh) Half thyroid gland (fixed) Thyroid gland weight >30 g may be significant, but must be supported by iodine concentration <1000 ppm or characteristic hyperplasia FAT Fluorescent antibody test, IFAT Indirect fluorescent antibody test, RT-PCR Real-time reverse transcriptase PCR ■ Any illness in dams or other disease problems; ■ Whether animals are housed or at grass; ■ Diet; ■ Recent purchases, stock movements or feed changes; ■ Herd serological status (from bulk milk or individual cow tests); ■ Vaccination status; ■ History of previous disease/infections in the herd. The table above lists the laboratory tests available for the investigation of an abortion at the regional laboratories of the VLA and Scottish Agricultural College. SEROLOGICAL TESTS Bulk milk serology for BVD, IBR and leptospirosis Bulk milk serology provides an indication of exposure to the pathogens responsible for BVD, IBR and leptospirosis at herd level for minimal cost. The results are of most value if they are used to monitor the antibody status of a herd on a regular basis. This is particularly important for naive herds where the appearance of antibodies would be significant. In herds where seroconversion rates are high, the results are most useful in determining the risk of infection in non-immune animals entering the herd. Vaccination will influence the results obtained. Individual maternal serology for BVD, IBR, neosporosis and leptospirosis Single or paired serology is of little use in the diagnosis of abortion and, at best, can only provide supportive evidence. Rising titres to BVD virus are rarely demonstrated in cases of abortion because of the delay between infection and abortion. High titres can be maintained for many years after infection and, therefore, are not necessarily an indication of recent infection. Serology could be considered to rule out BVD virus infection – if the aborted cow is seronegative (and antigen negative), it is unlikely BVD was involved. In Practice ● SEPTEMBER 20 07 Rising titres to BHV-1 may be detected in paired serology, but it is not possible to differentiate a naive IBR infection from recrudescence in a latently infected animal. Positive N caninum serology confirms that the dam is infected, indicating an increased likelihood of abortion occurring. It is useful to support fetal histopathological examination, and for deciding on the future breeding of the animal (as mentioned earlier). Serology for Leptospira species is usually unhelpful in individual aborting animals, as antibody titres are falling or absent at the time of abortion. Further investigation of herd seroprevalence may be warranted (in unvaccinated herds) to determine if a significant level of infection is present and, bearing in mind the risk of zoonotic disease, to decide whether to vaccinate. Use and misuse of serology Serology provides an indication of exposure to a particular pathogen. It cannot confirm the causal agent of an abortion, but can sometimes provide supportive evidence. Serology is generally unhelpful where stock are vaccinated. Acknowledgement The author would like to thank Dr Arthur Otter for his helpful comments on this article. References and further reading AGERHOLM, J. S., JENSEN, N. E., DANTZER, V., JENSEN, H. E. & AARESTRUP, F. M. (1999) Experimental infection of pregnant cows with Bacillus licheniformis bacteria. Veterinary Pathology 36, 191-201 CALDOW, G. & GRAY, D. (2004) Fetal loss. In Bovine Medicine, 2nd edn. Ed A. H. Andrews. Oxford, Blackwell Science. pp 577-593 DAVISON, H. C., OTTER, A. & TREES, A. J. (1999) Significance of Neospora caninum in British dairy cattle determined by estimation of seroprevalence in normally calving cattle and aborting cattle. International Journal of Parasitology 29, 1189-1194 DUBEY, J. P. (2005) Neosporosis in cattle. Veterinary Clinics of North America: Food Animal Practice 21, 473-483 ESSLEMONT, D. E. (2005) The cost of abortion in dairy cattle. UK Vet 10, 49-56 GROOMS, D. L. (2004) Reproductive consequences of infection with bovine diarrhoea virus. Veterinary Clinics of North America: Food Animal Practice 20, 5-19 MEE, J. F. (2004) The role of micronutrients in bovine periparturient problems. Cattle Practice 12, 95-108 MILLER, R. B. (1986) Bovine abortion. In Current Therapy in Theriogenology 2. Ed D. A. Morrow. Philadelphia, W. B. Saunders. pp 291-300 PATON, D. J., CHRISTIANSEN, K. H., ALENIUS, S., CRANWELL, M. P., PRITCHARD, G. C. & DREW, T. W. (1998) Prevalence of antibodies to bovine virus diarrhoea virus and other viruses in bulk tank milk in England and Wales. Veterinary Record 142, 385-391 RADOSTITS, O. M., GAY, G. C., BLOOD, D. C. & HINCHCLIFF, K. W. (2000) Veterinary Medicine. London, W. B. Saunders VIDA (2006) Veterinary Investigation Diagnosis Analysis. Addlestone, UK, Veterinary Laboratories Agency 463 Downloaded from inpractice.bmj.com on September 4, 2014 - Published by group.bmj.com Bovine abortion: aetiology and investigations Emma Cabell In Practice 2007 29: 455-463 doi: 10.1136/inpract.29.8.455 Updated information and services can be found at: http://inpractice.bmj.com/content/29/8/455 These include: Email alerting service Receive free email alerts when new articles cite this article. Sign up in the box at the top right corner of the online article. Notes To request permissions go to: http://group.bmj.com/group/rights-licensing/permissions To order reprints go to: http://journals.bmj.com/cgi/reprintform To subscribe to BMJ go to: http://group.bmj.com/subscribe/