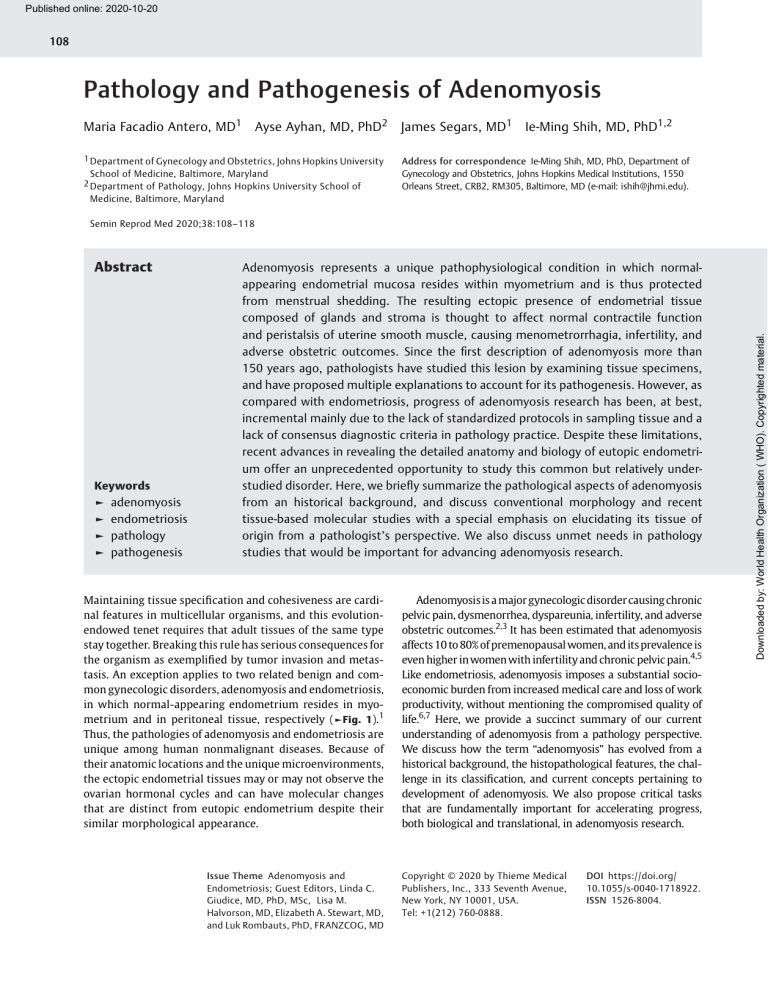
Published online: 2020-10-20 108 Pathology and Pathogenesis of Adenomyosis Maria Facadio Antero, MD1 Ayse Ayhan, MD, PhD2 1 Department of Gynecology and Obstetrics, Johns Hopkins University School of Medicine, Baltimore, Maryland 2 Department of Pathology, Johns Hopkins University School of Medicine, Baltimore, Maryland James Segars, MD1 Ie-Ming Shih, MD, PhD1,2 Address for correspondence Ie-Ming Shih, MD, PhD, Department of Gynecology and Obstetrics, Johns Hopkins Medical Institutions, 1550 Orleans Street, CRB2, RM305, Baltimore, MD (e-mail: [email protected]). Abstract Keywords ► ► ► ► adenomyosis endometriosis pathology pathogenesis Adenomyosis represents a unique pathophysiological condition in which normalappearing endometrial mucosa resides within myometrium and is thus protected from menstrual shedding. The resulting ectopic presence of endometrial tissue composed of glands and stroma is thought to affect normal contractile function and peristalsis of uterine smooth muscle, causing menometrorrhagia, infertility, and adverse obstetric outcomes. Since the first description of adenomyosis more than 150 years ago, pathologists have studied this lesion by examining tissue specimens, and have proposed multiple explanations to account for its pathogenesis. However, as compared with endometriosis, progress of adenomyosis research has been, at best, incremental mainly due to the lack of standardized protocols in sampling tissue and a lack of consensus diagnostic criteria in pathology practice. Despite these limitations, recent advances in revealing the detailed anatomy and biology of eutopic endometrium offer an unprecedented opportunity to study this common but relatively understudied disorder. Here, we briefly summarize the pathological aspects of adenomyosis from an historical background, and discuss conventional morphology and recent tissue-based molecular studies with a special emphasis on elucidating its tissue of origin from a pathologist’s perspective. We also discuss unmet needs in pathology studies that would be important for advancing adenomyosis research. Maintaining tissue specification and cohesiveness are cardinal features in multicellular organisms, and this evolutionendowed tenet requires that adult tissues of the same type stay together. Breaking this rule has serious consequences for the organism as exemplified by tumor invasion and metastasis. An exception applies to two related benign and common gynecologic disorders, adenomyosis and endometriosis, in which normal-appearing endometrium resides in myometrium and in peritoneal tissue, respectively (►Fig. 1).1 Thus, the pathologies of adenomyosis and endometriosis are unique among human nonmalignant diseases. Because of their anatomic locations and the unique microenvironments, the ectopic endometrial tissues may or may not observe the ovarian hormonal cycles and can have molecular changes that are distinct from eutopic endometrium despite their similar morphological appearance. Issue Theme Adenomyosis and Endometriosis; Guest Editors, Linda C. Giudice, MD, PhD, MSc, Lisa M. Halvorson, MD, Elizabeth A. Stewart, MD, and Luk Rombauts, PhD, FRANZCOG, MD Adenomyosis is a major gynecologic disorder causing chronic pelvic pain, dysmenorrhea, dyspareunia, infertility, and adverse obstetric outcomes.2,3 It has been estimated that adenomyosis affects 10 to 80% of premenopausal women, and its prevalence is even higher in women with infertility and chronic pelvic pain.4,5 Like endometriosis, adenomyosis imposes a substantial socioeconomic burden from increased medical care and loss of work productivity, without mentioning the compromised quality of life.6,7 Here, we provide a succinct summary of our current understanding of adenomyosis from a pathology perspective. We discuss how the term “adenomyosis” has evolved from a historical background, the histopathological features, the challenge in its classification, and current concepts pertaining to development of adenomyosis. We also propose critical tasks that are fundamentally important for accelerating progress, both biological and translational, in adenomyosis research. Copyright © 2020 by Thieme Medical Publishers, Inc., 333 Seventh Avenue, New York, NY 10001, USA. Tel: +1(212) 760-0888. DOI https://doi.org/ 10.1055/s-0040-1718922. ISSN 1526-8004. Downloaded by: World Health Organization ( WHO). Copyrighted material. Semin Reprod Med 2020;38:108–118 Antero et al. Fig. 1 The ectopic endometrium and eutopic endometrium. The diseases related to ectopic endometrium include adenomyosis, deep infiltrating endometriosis, peritoneal endometriosis, and ovarian endometriotic cyst (endometrioma). The insets illustrate the similar histology of eutopic endometrium (top) and ectopic lesions (bottom), containing both glandular epithelium and stroma. (Modified from Wang et al1; [© IM Shih, Johns Hopkins University].) A Historical Perspective First, let us wind back the clock to 1860 when Karl von Rokitansky initially described endometrial glands embedded in the uterine myometrium.8 He named this condition “cystosarcoma adenoids uterinum,” reflecting the essence of adenomyosis—glandular and sometimes cystic structures forming tumor-like lesions in uteri. Chiari9 also observed a similar lesion which he called “salpingitis isthmica nodosa (SIN)” around the fallopian tube musculature and believed that it was a variant of adenomyosis. Subsequently, other investigators in the late 19th century attempted to explain the possible mechanisms for the establishment of adenomyosis. Meyer10 was the first to propose the theory of “epithelial heterotopy,” an analogy to wound healing, where epithelial cells would invade inflammatory tissue that was damaged. He developed this theory after finding endometrial glands in the suture lines of a patient who had undergone a prior uterine ventrofixation secondary to pelvic pain. He thought that these glands were derived from either embryonic or “well-differentiated” cells. Cullen, who established gynecologic pathology as a subspecialty of pathology at the Johns Hopkins Hospital, pioneered a systematic and comprehensive description of what we know today as adenomyosis. He suggested a mechanism in which endometrial glands and stroma in endometrium could invade the underlying myometrium, as, in some cases, a direct connection between uterine cavity and the heterotopic glands could be seen.11 Another important contribution by Cullen was that he attributed the pathology of adenomyosis to clinical phenotypes including lengthened menstrual periods and pelvic pain. He further proposed that hysterectomy was the preferred treatment, as unlike a well-circumscribed leiomyoma it was often hard to dissect out adenomyomas because their “growth was so interwoven with the normal muscle.”12 Cullen’s theory of mucosal invasion faced challenges for many years, as other contemporary theories argued that displacement of mesonephric elements together with idiopathic stromal hyperplasia were responsible for adenomyosis.13,14 It was not until the 1920s that the endometrial origin of adenomyosis was widely accepted. This acceptance coincided with Sampson’s theory of retrograde menstruation to explain how menstruated endometrial tissue caused endometriosis,15 and helped to clarify that adenomyosis and endometriosis were two different disease entities, although both lesions were thought to originate from uterine endometrium. Finally, the term “adenomyosis uteri” was introduced in 1925 by Frankl,16 who described the mucosal invasion of the myometrium. He explained that the term was chosen so that it remained clear that the condition was not caused by an inflammatory process as had been previously proposed. He also further differentiated adenomyomas from adenomyosis, Seminars in Reproductive Medicine Vol. 38 No. 2-3/2020 109 Downloaded by: World Health Organization ( WHO). Copyrighted material. Pathology and Pathogenesis of Adenomyosis Pathology and Pathogenesis of Adenomyosis Antero et al. stating that the former originated independently within the uterus, and the latter was diffuse with a direct connection with the endometrium. It was only in 1972 that the current histological definition of adenomyosis was put forth by Bird et al17 positing that adenomyosis was characterized by the “… benign invasion of endometrium into myometrium, producing a diffusely enlarged uterus which microscopically exhibits ectopic, nonneoplastic, endometrial glands and stroma surrounded by hypertrophic and hyperplastic myometrium.” The modern histological definition was thus born. Pathology of Adenomyosis and Correlation with Imaging Results Grossly, the uterus may appear slightly enlarged and globular due to myometrial hypertrophy in severe cases of adenomyosis (►Fig. 2a),18–20 but in general, the involved uteri preserve the overall contour, and are rarely bigger than a 12-week size gravid uterus.17,21,22 The cut surface of adenomyotic foci is characterized by hyperfasciculated and trabeculated areas of myometrium, which correspond with myometrial hypertrophy (►Fig. 2b). On gross appearance, adenomyosis, unlike leiomyoma, does not manifest a well-demarcated border (►Fig. 2c, d). The adenomyotic foci may appear grossly indistinct or as a white-gray mass with areas of brown-staining secondary to hemolyzed blood and hemosiderin deposits.23 Blood-filled cysts can also be occasionally observed.24 In some cases, uterine adenomyosis can form localized nodules that grossly mimic leiomyomas. These focal adenomyotic nodules are known as adenomyomas, and are composed of smooth muscle surrounding endometrial glands and stroma. Upon gross examination, adenomyomas, unlike leiomyomas, are unencapsulated, and the hypertrophied myometrium is often mixed with the surrounding normal myometrium (►Fig. 2c, d). Microscopically, adenomyosis consists of irregularly shaped islands of endometrial glands and stroma within the myometrium. They are always multiple, and we believe that the discrete islands, especially those are adjacent to each other on cross tissue sections, are not separated but rather are interconnected, which can be seen if a series of sequential sections are examined or a three-dimensional reconstruction can be generated. Thus, the architecture of adenomyosis is distinct from that of the functional endometrium, in which the glands are solitary, nonbranching, and longitudinally arranged (►Fig. 2e, f ). In fact, the glands and stroma of adenomyotic foci architecturally resemble the basalis layer in eutopic endometrium, where a complex horizontally connected glandular structure is normally formed.25 The gland-to-stroma ratio varies widely among adenomyoma foci, and some may have attenuated or undetectable stromal components,26 which may reflect sampling issue in which the tangential cut surface does not contain the neighboring stroma. The adenomyotic endometrium may retain its proliferative potential, which could contribute to endometrial regrowth and failure after endometrial ablation.27 Glands can vary in shape and size, with 5% of them forming cystic structures filled with cellular debris and hemosiderin-laden macrophages (►Fig. 2g).28 The stromal components of Seminars in Reproductive Medicine Vol. 38 No. 2-3/2020 Fig. 2 Gross and microscopic features of adenomyosis. (a) The involved uterus appears slightly enlarged and globular. (b) A bivalved surface from a hysterectomy specimen shows multiple foci of adenomyosis with petechialike areas (yellow arrows) in myometrium. The smooth muscle appears hypertrophied and disarrayed. (c, d) Comparison of gross appearance of adenomyosis (AD) and leiomyoma (LM). Formalin fixed cross-section in C and hematoxylin and eosin (H&E) stained section in D. (e) Microscopic features showing presence of glandular epithelium and stroma surrounded by hypertrophic smooth muscle cells. (H&E stain 20 magnification). (f) Higher magnification view to show the resemblance of epithelial and stromal components of adenomyosis to eutopic endometrium (H&E stain 40 magnification). (g) Ectopic endometrial tissue showing foci of hemorrhage with histiocytes and hemosiderin-laden macrophages (red arrow) (H&E stain 20 magnification). (h) Marked decidualization with small inactive glands in adenomyosis seen after exogenous progestin therapy. (H&E stain 20 magnification). adenomyosis present a monotonous appearance, and are usually inactive and nonmitotic. Secretory changes, including stromal decidualization, have been observed during gestation and exogenous progestin therapy (►Fig. 2h). Adenomyosis is never found in a leiomyoma. In normal uteri, the junction between endometrium and myometrium is not always well demarcated, and an irregular border with focal extension of endometrial tissue into superficial myometrium is not uncommon. As such, tangential sections can reveal seemingly detached foci of glands and stroma beneath endometrium, and these foci may be mistakenly diagnosed as superficial adenomyosis, further confounding Downloaded by: World Health Organization ( WHO). Copyrighted material. 110 clinicopathological studies of adenomyosis. Tissue biomarkers that help distinguish true adenomyosis from endometrial extensions from the irregular border would be useful. Along this line, upregulation of the biomarker STING (stimulator of interferon gene) has recently been reported to distinguish epithelial cells of adenomyosis from eutopic endometrium.29 The endometrial–myometrial junctional zone located between the endometrium and the inner myometrium has received much attention in adenomyosis research because this zone is often thickened and exhibits architectural changes that may lead to abnormal uterine peristalsis.30,31 Architectural changes include loss of nerve fibers and smooth muscle hypertrophy.32 At the ultrastructural level, these myocytes associated with adenomyosis show abnormal nuclear and mitochondrial shapes, abundant myelin bodies and intermediate filament aggregates, extensive endoplasmic reticulum, and increased expression of oxytocin receptors.33,34 Although these findings and their biological significance requires validation, the morphological abnormalities in the junctional zone in adenomyosis may play a role in hyperperistalsis. It is not certain whether hyper- or dysperistalsis facilitates invasion of endometrial glands into the myometrium,35 or whether the presence of abundant ectopic endometrial tissues in myometrium interferes with or triggers peristalsis. Adenomyotic lesions also have a higher angiogenic potential, as evidenced by an increased level of vascular endothelial growth factor (VEGF) and hypoxia-inducible factor-1α (HIF-1α) compared with paired eutopic endometrium and with endometrium from disease-free women.36 Furthermore, although verification will be required, it appears that ectopic endometrium contains a greater density of Antero et al. microvessels than adjacent normal endometrium or eutopic endometrium of disease-free women.37 The aforementioned pathologic features of adenomyosis can explain many of the commonly observed findings reported in ultrasound or MRI studies. Subendometrial echogenic linear striations, nodules, and/or asymmetrical myometrial bulkiness may be related to muscular hypertrophy in different regions in reaction to the presence of ectopic endometrium. Moreover, hyperechoic islands and subendometrial cysts can be a result of focal cystic dilatation of the fluid-filled glands in adenomyosis. Thus, the irregular endometrial–myometrial junction may reflect the complex and convoluted connection between endometrium and the underlying adenomyosis. In color Doppler sonography, a general increase in vascularity and in numbers of tortuous vessels penetrating myometrium is likely associated with enhanced angiogenesis. Thickening of the junctional zone, visualized as a hypoechoic halo beneath the endometrial layer (usually greater than 12 mm), is suggestive of an adenomyosis. However, it is challenging to correlate such thickening with adenomyosis-associated histopathological findings. Unusual Pathology and Related Gynecologic Conditions Hyperplastic changes with or without atypia are not unusual in adenomyosis, and can often be detected in the corresponding eutopic endometrium. However, malignant transformation of adenomyosis is a rare event occurring mostly in postmenopausal women (►Fig. 3).38,39 Fig. 3 Atypical hyperplasia and low-grade endometrioid carcinoma arising from adenomyosis. (a) Foci of atypical hyperplasia within a preexisting adenomyosis lesion. (b) An incipient low-grade endometrioid carcinoma arising from adenomyosis with cancerous tissue coexisting with ectopic benign glandular tissue (hematoxylin and eosin stain 20 magnification). Seminars in Reproductive Medicine Vol. 38 No. 2-3/2020 111 Downloaded by: World Health Organization ( WHO). Copyrighted material. Pathology and Pathogenesis of Adenomyosis Pathology and Pathogenesis of Adenomyosis Antero et al. Endometrioid carcinoma is the most common histological type of malignant transformation of adenomyosis, but serous carcinoma, clear cell carcinoma, and poorly differentiated carcinoma may also be seen.40 Pathologic findings that suggest malignant transformation of adenomyosis include the presence of cancerous tissue and ectopic endometrial tissue in the same lesion, diagnosis of adenomyosis, transformation evidence between benign and malignant gland structures, and exclusion of other sources of tumor invasion or metastasis.41 In addition to epithelial cells, stromal cells in adenomyosis can also undergo neoplastic transformation to form intramural adenosarcoma, but this is exceedingly rare. Other unusual subtypes of adenomyosis have been described. As mentioned earlier, adenomyomas are a nodular form of adenomyosis involving myometrium focally, which distinguishes it from the diffuse appearance of conventional adenomyosis. Both adenomyomas and diffuse types of adenomyosis may be present in the same specimen. One lesion related to adenomyoma is “polypoid adenomyoma” which is a benign tumor commonly arising from the lower uterine segment forming either a single polypoid lesion or multiple polyps.42 Histologically, endometrial glands are embedded in a fibromuscular or muscular stroma. The glands are usually lined with endometrioid cells and embedded by smooth muscle fascicles.42,43 The endometrial stromal cells are not always present, arguing that atypical polypoid adenomyoma is related to conventional adenomyosis. SIN, once considered to be a variant of adenomyosis, is now mostly seen as an acquired fallopian tube lesion analogous to adenomyosis of the uterus. Grossly, SIN appears as a nodular protrusion on the tubal serosa and is most often localized to the isthmic portion of the tube. SIN can cause either infertility due to luminal obstruction or tubal pregnancy due to the irregular and convoluted lumen of the fallopian tubes. Adenomyosis and SIN may share pathogenic mechanisms, as they have similar glandular proliferation with an associated muscular hypertrophy phenotype. Pathology-Based Classification Several classification systems based on histological features of adenomyosis have been proposed: (1) depth of myometrium involvement, (2) location of adenomyotic lesions, and (3) whether the myometrial involvement is diffuse or localized. However, a standard and well-accepted system for histological classification has not yet been established, in part because studies attempting to correlate pathological features with clinical presentations have not shown significant or reproducible results. We believe that this is related to how specimens are processed and examined. For example, there is a direct correlation between the number of histologic sections examined and the prevalence of adenomyosis. In a study by Bird et al,17 the prevalence of adenomyosis increased from 31 to 61.5% when additional histologic uterine sections were obtained and examined. Despite this fact, Seminars in Reproductive Medicine Vol. 38 No. 2-3/2020 there is no consensus among pathologists regarding sampling hysterectomy specimens. Moreover, not all adenomyotic lesions are created equal. It is plausible that other than conventional histopathology, adenomyosis can be classified according to developmental patterns or the molecular alterations. Molecular classification would be welcome but appear to be out of reach until we better understand the pathogenesis of adenomyosis, and can correlate molecular changes and clinical phenotypes. Nevertheless, it is worth briefly reviewing classifications that have been proposed in the past so that investigators can design better studies for future classification of adenomyosis. Since the depth of myometrial involvement is the most obvious histopathological feature of adenomyosis, many investigators have proposed classification systems based on the depth of glands within the myometrium. This is analogous to endometrial carcinoma in which the depth of myometrial invasion by the cancer cells determines the FIGO stage, which is highly associated with clinical outcome.44,45 For example, one study46 proposed that superficial adenomyosis could be characterized as glands within 40% of the myometrial thickness, intermediate adenomyosis when glands were present in 40 to 80% of myometrial thickness, and deep adenomyosis when glands were seen beyond 80% of the myometrial thickness. Another study applied onethird and two-third as the cut-off.47 Unfortunately, those proposed cut-offs are arbitrary, lacking biological or clinical grounds. In general, significant conflicts are seen among results of studies aimed at correlating disease symptoms with depth of glands within the myometrium. In some studies, the two most common symptoms of pain (dysmenorrhea, chronic pelvic pain, or dyspareunia) and abnormal uterine bleeding (AUB, or menorrhagia) were assessed.23 Some studies found a positive correlation between depth of adenomyosis involvement and dysmenorrhea,17,46,48 whereas others found no correlation at all.49 Dysmenorrhea has been reported to correlate with the number of glandular tissue foci seen within the myometrium.46,48,49 Dyspareunia is also associated with the number of lesion foci but not with depth of the lesion.49 Diffuse adenomyosis has been associated with worse dysmenorrhea than focal disease, while the later has been associated with infertility especially when located in the outer myometrium.50,51 Conflicting data have been reported concerning the relationship of AUB and histologic features such as depth and glandular density. Most studies have shown that there is no relationship between AUB and glandular depth, but the numbers of adenomyotic foci per slide show a strong correlation with the reported bleeding volume. In one report, menorrhagia was found to be more prevalent in women with deep adenomyosis than in those with intermediate disease.46 Another study used the gross appearance of uterus and tissue consistency at the time of surgery was used to classify adenomyosis as either diffuse type or as sclerotic type in which densely packed collagen fibers surrounded the adenomyotic foci.28 Menorrhagia was found to be more frequently present in the diffuse type than in other types. Downloaded by: World Health Organization ( WHO). Copyrighted material. 112 Pathogenesis of Adenomyosis The pathogenesis of adenomyosis, especially the steps through which normal-appearing endometrial tissue is displaced to myometrium, and the mechanisms by which adenomyotic foci cause symptoms, remain largely unclear. Current evidence from histopathological observations and recent molecular genetic studies indicates that adenomyosis is derived from invagination from the basal layer of endometrium into adjacent myometrium, a modern view resonant with what Cullen proposed almost one century ago. Tissue sections of adenomyotic lesions that are prepared for pathology diagnosis almost always show multiple irregularly shaped seemingly interconnected endometrial glands embedded in stroma. This is one of the salient morphological features of adenomyosis, and suggests that the glands within adenomyosis are highly convoluted, forming a labyrinth network, and do not display a simple arrangement (►Fig. 4a). This architecture of adenomyosis resembles that in the basal layer of endometrium. Comparison of eutopic endometrium between uteri with and without adenomyosis may offer some clues. In hysterectomy specimens showing adenomyosis, it is not uncommon to observe a more irregular endo-myometrial border with endometrial glands and stroma “attempting” to extend from basalis into Antero et al. superficial myometrium (►Fig. 4b). Several studies argue that this involves a true invasion process. If this is the case, it would be different from that seen in carcinoma. If this were a bone fide invasion, both glandular epithelium and stroma would have to acquire a constellation of complex molecular and cellular changes including expression of proteases that degrade the extracellular matrix, enhanced motility, and the ability to comigrate and dissect into remarkably cohesive smooth muscle layers. These features are highly unusual for any adult normalappearing tissues. Moreover, adenomyosis does not exhibit a classical stromal reaction (desmoplasia), which is one of the hallmarks of tumor invasion under microscopic examination. Rather, we propose that the genesis of adenomyosis derives from an embryonic or an early postnatal invagination of the basal endometrium followed by extension deep into myometrium, likely associated with a physiological or pathological defect of the endometrial–myometrial junction. This is supported by reported cases of fetal and prepubescent adenomyosis and endometriosis.52–54 It is also possible that the basal endometrium can acquire access to myometrium in a gestational uterus where the myometrium is relatively loosened due to interstitial edema and focal disarray of the muscular layer. Nevertheless, the eutopic endometrium of adenomyosis patients may possess certain characteristics that differ from Fig. 4 Adenomyosis originating from the basal layer of endometrium. (a) A schematic representation of the development of adenomyosis with the focal extension of a single clonally distinct endometrial gland from the endometrial basalis into the myometrium. In the myometrium, the incipient adenomyosis continues to clonally expand to form intricate and interconnected glandular foci which are similar to the endometrial basalis layer. Together with the “invading” gland, stromal cells also migrate and clonally expand. Different color lines (glands) and dots (stroma) represent clonally distinct subpopulations. (b) Immunostaining of cytokeratin suggesting the process of early adenomyosis development. The adenomyotic tissue appears to descend from the basal endometrium through the endometrial myometrial interface (dashed red line) with the vertical “invasion” of ectopic glandular and stromal tissue into myometrium. (20 magnification). Seminars in Reproductive Medicine Vol. 38 No. 2-3/2020 113 Downloaded by: World Health Organization ( WHO). Copyrighted material. Pathology and Pathogenesis of Adenomyosis Pathology and Pathogenesis of Adenomyosis Antero et al. tissue of disease-free controls. Indeed, eutopic endometrium in adenomyosis shows molecular changes which favor a phenotype including increased angiogenesis and proliferation, decreased apoptosis, impaired immune function, and altered hormone levels (increased estrogen production and progesterone resistance).36,55–63 As a result, the basal layer of eutopic endometrium has a propensity to migrate into myometrium. If more comprehensive molecular studies are able to confirm these findings, it may help explain the origins and pathogenesis of adenomyosis. Despite the histopathological evidence, the tissue origin of adenomyosis from eutopic endometrium has only recently received molecular validation; the identification of somatic mutations using next-generation sequencing has provided unequivocal evidence that adenomyosis develops from eutopic endometrium.64 In many cases, the same somatic mutations, including mutations in KRAS, could be detected in both adenomyosis and corresponding eutopic endometrium, suggesting that both ectopic and eutopic endometrium are clonally related. In further separating glandular epithelium from stroma of adenomyotic lesions using laser capture microdissection, mutations were found to occur only in the epithelial component of adenomyosis,64 a result similar to a previous report showing that mutations in endometriosis are detected only in epithelium and not in stroma.65 Since adenomyosis may select cancer driver mutations like KRAS, which is known to promote cell survival and growth, thus confounding the clonality studies, we analyzed selection-neutral mutations (synonymous and passenger gene mutations) that do not confer any selection advantage to cells in adenomyosis and matched basal layer samples of eutopic endometrium. We found truncal mutations shared by ectopic and eutopic endometrium, confirming that both adenomyosis and associated eutopic endometrium are progeny of the same endometrial epithelial progenitor cells (Lihong Li, MD; unpublished data October 1, 2020). However, the adenomyosis and eutopic endometrium also harbor distinct mutations. It is thus possible that after leaving the endometrium, these progenitor cells develop into adenomyosis in myometrium through the acquisition of private mutations. An interesting result from this recent study is that the KRAS mutations identified in adenomyosis were associated with increased risk of cooccurring endometriosis, and that KRAS mutations were often shared between the two coexisting pathologies.64 Whether this is coincidental or biologically meaningful is uncertain. Among different types of endometriotic lesions, ovarian endometriotic cysts (69%) were more likely to cooccur in KRAS-mutated adenomyotic lesions than in deeply infiltrating endometriosis (46%), or peritoneal endometriosis (11.6%). The study also showed that KRAS mutations were often shared by cooccurring adenomyosis and endometriotic lesions. This finding appears consistent with other studies that have shown that deeply infiltrating endometriosis and ovarian endometriomas harbor a variety of somatic cancer driver mutations in PIK3CA, ARID1A, PPP2R1A, and/or KRAS.66,67 Since the number of cases that have been subjected to mutational Seminars in Reproductive Medicine Vol. 38 No. 2-3/2020 analysis is limited, it remains to be confirmed if KRAS mutations are important in the pathogenesis of adenomyosis and endometriosis, or if the mutations merely represent clonal markers without biological consequences. Endometriosis is a common finding in patients with adenomyosis and vice versa; both diseases cooccur in up to 80% of patients.35,68–70 Among different types of endometriosis (►Fig. 1), deeply infiltrative endometriosis is more commonly seen in women who have focal adenomyosis of the outer myometrium.69 Like adenomyosis, deeply infiltrative endometriosis is characterized by the ectopic presence of normal-appearing endometrial glands and stroma in the smooth muscle layers of peritoneal organs such as urinary bladder and bowel wall. Imaging studies have also shown an increased incidence of deeply infiltrative endometriosis and ovarian endometriomas in women with adenomyosis, specifically in adenomyosis involving the outer portion of the myometrium.71–73 This suggests that adenomyosis and certain types of endometriosis may be biologically related. Inoue et al. looked at the genetic landscape of the eutopic endometrium in disease-free women and those with adenomyosis.64 As noted in other studies,74,75 the eutopic endometria of disease-free women were found to have somatic cancer driving mutations in genes such as KRAS and PIK3CA at much higher variant allele frequencies. Whether the single cancer driver mutation, as occurs in ectopic endometrium, is sufficient to drive the disease phenotypes remains to be determined. It is still not known if these somatic mutations are present at birth or acquired later in life, and whether there is a genetic basis for the development of adenomyosis. A recent study reports the mutational landscape of the normal endometrium, showing that while age positively correlates with the mutational burden in the endometrium, some KRAS and PIK3CA mutations arise as early as the first decade of life.75 The fact that adenomyosis develops later in life, usually in the fourth or fifth decade, would seem to favor the theory that the mutations are acquired, and that the disease is not genetically predetermined. However, there have been reports of adenomyosis developing in adolescents,24,76 and a case report of familial adenomyosis suggests that the disease may have a genetic predisposition.77 Furthermore, relatively late diagnosis of adenomyosis as compared with endometriosis may be due to the diagnosis at hysterectomy, which is uncommonly performed in young women. Therefore, this interesting observation awaits confirmation in future studies. Recently, differentially expressed genes were identified in the eutopic endometrium of patients with adenomyosis.78 Using RNA sequencing followed by quantitative real-time PCR and immunohistochemistry to validate findings, they were able to identify 373 differentially expressed genes in both ectopic and eutopic endometrium of adenomyosis patients irrespective of menstrual cycle phases. Pathway analysis of these differentially expressed genes identified pathways responsible for regulating cellular proliferation and growth, tissue morphology, and angiogenesis. Among the identified differentially expressed genes was C/EBPβ, a core node in the network analysis. The protein encoded by C/ Downloaded by: World Health Organization ( WHO). Copyrighted material. 114 Pathology and Pathogenesis of Adenomyosis Conclusions Adenomyosis is a benign gynecological disorder which consists of endometrial glands and stroma in the myometrium. Although adenomyosis is related to endometriosis, both lesions are thought to develop through different mechanisms. Results of recent molecular genetic studies imply that adenomyosis is clonally derived from the basal endometrium, a result in resonance to the original Cullen’s hypothesis that adenomyosis is the “invasion” of endometrial tissue into myometrium. Despite this fact, adenomyosis develops its own progeny during development, and can be molecularly distinguished from proximal eutopic endome- 115 trium. Several studies have also suggested that the eutopic endometrium is inherently different in women with versus without adenomyosis. However, the data on this are not conclusive, and more rigorous research employing new technologies with a larger case cohort will be needed to validate these conclusions. Future Directions Despite new progress in our understanding of the pathology and pathogenesis of adenomyosis, several fundamental questions remain unanswered. Future pathology research is needed to classify adenomyosis, and there is a pressing need to understand the molecular and genetic underpinnings of this disease to facilitate new diagnostic and therapeutic paradigms. Classification. Foremost is that a standardized classification system is developed in pathology to accurately document and report the disease and for a consistency in designing basic and clinical studies for meaningful interpretation in future adenomyosis research. With the advent of molecular technologies, we believe that a model integrating clinical–pathological findings and molecular data such as somatic mutation load, cancer driver mutation landscape, and methylation profiles can be developed to correlate with clinical phenotypes. This knowledge will be essential for a better understanding of the pathogenesis of the disease. Diagnosis. Development of practical diagnostic tools with high accuracy is desirable to guide diagnosis and clinical management. While MRI and ultrasound in the past two decades have provided a noninvasive diagnostic tool for adenomyosis, correlation of these with pathological findings is warranting. As molecular signatures may likely differ in eutopic endometrium of women with versus without adenomyosis, it is envisioned that adenomyosis could be reliably predicted based on an endometrial molecular “adenomyosis signature,” ideally including imaging results in a risk-predicting algorithm. Equally important is to develop blood-based biomarkers that can help diagnose a woman with adenomyosis with high sensitivity and specificity. This will be made possible after a better understanding of the aberrant adenomyosisspecific secretome including exosome, miRNA species, and unique protein biomarkers and their combinations. Disease mechanisms. It is important for future directions in studying the pathology of adenomyosis to focus on understanding molecular and genetic changes present in both eutopic and ectopic lesions to determine their roles in the development of adenomyosis and how they relate to specific disease phenotypes. More studies are needed to determine phylogenetic trajectories in the development of adenomyosis from eutopic endometrium. Future studies also need to integrate the somatic mutation data to the theory of endometrial progenitor (stem cell-like) cells. While truncal mutations are shared by progenitor cells and their progeny, indicating a clonal derivation of the latter from the former, it remains unclear where those progenitor cells are physically located and how many they are in eutopic and ectopic endometrium. Seminars in Reproductive Medicine Vol. 38 No. 2-3/2020 Downloaded by: World Health Organization ( WHO). Copyrighted material. EBPβ acts as a transcription factor regulating expression of genes that control cellular proliferation, differentiation, and metabolism. C/EBPβ is also a key regulator of human endometrial stromal proliferation and differentiation.79,80 Other pathways noted to be upregulated were IL-6, which has been shown to be increased in adenomyotic stromal cells cocultured with macrophages,59 and ERK/MAPK, which has been associated with uterine smooth muscle proliferation in women with adenomyosis.81 The aforementioned evidence supports that invagination of the endometrial basalis into the myometrium is the favored model for the genesis of adenomyosis, as both epithelial and stromal progenitor cells residing in basalis are responsible not only for regenerating the entire functional layer after menstruation but can also promote adenomyosis development in the opposite direction. However, the data should not be construed as supporting only this model of the pathogenesis of adenomyosis. For example, it has also been proposed that metaplasia of displaced embryonic pluripotent Müllerian remnants or differentiation of adult endometrial progenitor cells can also be the origin of adenomyosis and its related lesion, endometriosis. Over the last few years, it has been shown that stem cells present in the endometrium basalis have the capacity to regenerate and replace endometrium.82 This discovery has led to the postulation that individual stem cells may disseminate locally or spread through the circulation to cause adenomyosis if deposited in the myometrium and/or to cause endometriosis if deposited outside the uterus. Why are stem cells present in the myometrium? A possible explanation is that stem cells may be activated by tissue injury which favors migration to the myometrium rather than the endometrium.83,84 However, this stem cell hypothesis faces a major challenge, that is, how does an individual stem cell simultaneously could differentiate into both epithelium and stroma which are present in all adenomyosis and endometriosis lesions. If it does, both lesions should harbor the same founder mutations, and future studies need to provide such new evidence. From the standpoint of histopathology, it is more likely that endometrial epithelial progenitor cells reside in basal glands which may extend into the myometrium, where the progenitor cells and their glands accompanied by presumed stromal progenitor cells codevelop into adenomyosis. Antero et al. Pathology and Pathogenesis of Adenomyosis Antero et al. Moreover, experimental designs of molecular studies warrant revisiting. Historically bulk tissue analyses of the lesions as a whole (combining epithelium and stroma) or only on epithelium were conducted. Given the critical roles of the stromal components in codeveloping adenomyosis with glandular epithelium, it will be necessary to study stroma alongside glandular epithelium by careful separation of glands and stroma using laser-capture microdissection before sequencing analysis and genome-wide profiling. Finally, recent technological developments have greatly helped advance our understanding of many human diseases, especially in the fields of cancer and immunology. Tools such as multiplexed imaging analysis, single cell profiling, and epigenetic and epigenomic methods all offer unprecedented opportunities to accelerate discovery of altered genetic and molecular pathways in adenomyosis and associated eutopic endometrium. The new knowledge will, in turn, inform clinical studies for the development of improved diagnosis and treatments, which may be more patient centered, potentially curative, and fertility sparing. This task is long overdue. Funding This study is supported by an NIH grant RO1HD096147 and by the Richard W. TeLinde Endowment, Department of Gynecology and Obstetrics, Johns Hopkins University. Conflict of Interest None declared. 11 Kelly HA, Cullen TS. Myomata of the Uterus. Saunders; 1909 12 Cullen T. Adenomyoma of the Uterus. Philadelphia, PA: W. B. Saunders Company; 1908 13 Von Recklinghausen F. Die Adenomyome und Cystadenome der 14 15 16 17 18 19 20 21 22 23 24 25 26 References 1 Wang Y, Nicholes K, Shih IM. The origin and pathogenesis of endometriosis. Annu Rev Pathol 2020;15:71–95 27 2 Bruun MR, Arendt LH, Forman A, Ramlau-Hansen CH. Endome- 3 4 5 6 7 8 9 10 triosis and adenomyosis are associated with increased risk of preterm delivery and a small-for-gestational-age child: a systematic review and meta-analysis. Acta Obstet Gynecol Scand 2018; 97(09):1073–1090 Harada T, Taniguchi F, Amano HJapan Environment and Children’s Study Group. , et al; . Adverse obstetrical outcomes for women with endometriosis and adenomyosis: a large cohort of the Japan Environment and Children’s Study. PLoS One 2019;14(08):e0220256 Orazov M, Nosenko EN, Radzinsky VE, Khamoshina MB, Lebedeva MG, Sounov MA. Proangiogenic features in chronic pelvic pain caused by adenomyosis. Gynecol Endocrinol 2016;32 (Suppl 2):7–10 Seidman JD, Kjerulff KH. Pathologic findings from the Maryland Women’s Health Study: practice patterns in the diagnosis of adenomyosis. Int J Gynecol Pathol 1996;15(03):217–221 Nnoaham KE, Hummelshoj L, Webster PWorld Endometriosis Research Foundation Global Study of Women’s Health Consortium. , et al; . Impact of endometriosis on quality of life and work productivity: a multicenter study across ten countries. Fertil Steril 2011;96(02):366–373.e8 Struble J, Reid S, Bedaiwy MA. Adenomyosis: a clinical review of a challenging gynecologic condition. J Minim Invasive Gynecol 2016;23(02):164–185 Rokitansky C. Ueber Uterusdrusen-neubildung in Uterus and Ovariul Sarcomen. Z Gesellschaft Aerzte Wien 1860;16:577 Chiari H. Zur pathologischen anatomie des eileitercatarrhs. Z Heilkunde 1887;8:457–464 Meyer R. Uber eine adenomatose Wucherung der Serosa in einer Bauchnarbe. Z Geburtshilfe Gynakol 1903;49:32–41 Seminars in Reproductive Medicine Vol. 38 No. 2-3/2020 28 29 30 31 32 33 34 35 36 Uterus-und Tubenwandung: ihre Abkunft von Resten des Wolff’schen Körpers. Hirschwald1896 Diesterweg A. Ein Fall von Cystofibroma uteri verum. Z. Geburtshilfe 1883;9:191–195 Sampson JA. Peritoneal endometriosis due to the menstrual dissemination of endometrial tissue into the peritoneal cavity. Am J Obstet Gynecol 1927;14(04):422–469 Frankl O. Adenomyosis uteri. Am J Obstet Gynecol 1925;10(05): 680–684 Bird CC, McElin TW, Manalo-Estrella P. The elusive adenomyosis of the uterus. Am J Obstet Gynaecol 1972;112:583–593 Shutter J. Uterus-like ovarian mass presenting near menarche. Int J Gynecol Pathol 2005;24(04):382–384 Bell CD, Ostrezega E. The significance of secretory features and coincident hyperplastic changes in endometrial biopsy specimens. Hum Pathol 1987;18(08):830–838 Ferenczy A. Pathophysiology of adenomyosis. Hum Reprod Update 1998;4(04):312–322 Molitor JJ. Adenomyosis: a clinical and pathological appraisal. Am J Obstet Gynecol 1971;110(02):275–284 Langlois PL. The size of the normal uterus. J Reprod Med 1970;4 (06):220–228 Azziz R. Adenomyosis: current perspectives. Obstet Gynecol Clin North Am 1989;16(01):221–235 Brosens I, Gordts S, Habiba M, Benagiano G. Uterine cystic adenomyosis: a disease of younger women. J Pediatr Adolesc Gynecol 2015;28(06):420–426 Tempest N, Jansen M, Baker AM, et al. Histological 3D reconstruction and in vivo lineage tracing of the human endometrium. J Pathol 2020;251(04):440–451 Goldblum JR, Clement PB, Hart WR. Adenomyosis with sparse glands. A potential mimic of low-grade endometrial stromal sarcoma. Am J Clin Pathol 1995;103(02):218–223 Haber G, Ferenczy A. Electrosurgical solutions to gynecological problems. Contemp Obstet Gynecol 1993;1:25–36 Pistofidis G, Makrakis E, Koukoura O, Bardis N, Balinakos P, Anaf V. Distinct types of uterine adenomyosis based on laparoscopic and histopathologic criteria. Clin Exp Obstet Gynecol 2014;41(02): 113–118 Qu H, Li L, Wang TL, Seckin T, Segars J, Shih IM. Epithelial cells in endometriosis and adenomyosis upregulate STING expression. Reprod Sci 2020;27(06):1276–1284 Birnholz JC. Ultrasonic visualization of endometrial movements. Fertil Steril 1984;41(01):157–158 Exacoustos C, Brienza L, Di Giovanni A, et al. Adenomyosis: threedimensional sonographic findings of the junctional zone and correlation with histology. Ultrasound Obstet Gynecol 2011;37 (04):471–479 Quinn M. Uterine innervation in adenomyosis. J Obstet Gynaecol 2007;27(03):287–291 Mehasseb MK, Bell SC, Pringle JH, Habiba MA. Uterine adenomyosis is associated with ultrastructural features of altered contractility in the inner myometrium. Fertil Steril 2010;93(07):2130–2136 Guo S-W, Mao X, Ma Q, Liu X. Dysmenorrhea and its severity are associated with increased uterine contractility and overexpression of oxytocin receptor (OTR) in women with symptomatic adenomyosis. Fertil Steril 2013;99(01):231–240 Leyendecker G, Bilgicyildirim A, Inacker M, et al. Adenomyosis and endometriosis. Re-visiting their association and further insights into the mechanisms of auto-traumatisation. An MRI study. Arch Gynecol Obstet 2015;291(04):917–932 Goteri G, Lucarini G, Montik N, et al. Expression of vascular endothelial growth factor (VEGF), hypoxia inducible factor-1α (HIF-1α), and microvessel density in endometrial tissue in Downloaded by: World Health Organization ( WHO). Copyrighted material. 116 Pathology and Pathogenesis of Adenomyosis 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 117 59 Yang JH, Wu MY, Chang DY, Chang CH, Yang YS, Ho HN. Increased 60 61 62 63 64 65 66 67 68 69 70 71 72 73 74 75 76 77 78 79 interleukin-6 messenger RNA expression in macrophage-cocultured endometrial stromal cells in adenomyosis. Am J Reprod Immunol 2006;55(03):181–187 Yang J-H, Chen MJ, Chen HF, Lee TH, Ho HN, Yang YS. Decreased expression of killer cell inhibitory receptors on natural killer cells in eutopic endometrium in women with adenomyosis. Hum Reprod 2004;19(09):1974–1978 Sotnikova N, Antsiferova I, Malyshkina A. Cytokine network of eutopic and ectopic endometrium in women with adenomyosis. Am J Reprod Immunol 2002;47(04):251–255 Mehasseb MK, Panchal R, Taylor AH, Brown L, Bell SC, Habiba M. Estrogen and progesterone receptor isoform distribution through the menstrual cycle in uteri with and without adenomyosis. Fertil Steril 2011;95(07):2228–2235, 2235.e1 Nie J, Lu Y, Liu X, Guo SW. Immunoreactivity of progesterone receptor isoform B, nuclear factor kappaB, and IkappaBalpha in adenomyosis. Fertil Steril 2009;92(03):886–889 Inoue S, Hirota Y, Ueno T, et al. Uterine adenomyosis is an oligoclonal disorder associated with KRAS mutations. Nat Commun 2019;10(01):5785 Noë M, Ayhan A, Wang TL, Shih IM. Independent development of endometrial epithelium and stroma within the same endometriosis. J Pathol 2018;245(03):265–269 Suda K, Nakaoka H, Yoshihara K, et al. Clonal expansion and diversification of cancer-associated mutations in endometriosis and normal endometrium. Cell Rep 2018;24(07):1777–1789 Anglesio MS, Papadopoulos N, Ayhan A, et al. Cancer-associated mutations in endometriosis without cancer. N Engl J Med 2017; 376(19):1835–1848 Di Donato N, Montanari G, Benfenati A, et al. Prevalence of adenomyosis in women undergoing surgery for endometriosis. Eur J Obstet Gynecol Reprod Biol 2014;181:289–293 Chapron C, Tosti C, Marcellin L, et al. Relationship between the magnetic resonance imaging appearance of adenomyosis and endometriosis phenotypes. Hum Reprod 2017;32(07):1393– 1401 Eisenberg VH, Arbib N, Schiff E, Goldenberg M, Seidman DS, Soriano D. Sonographic signs of adenomyosis are prevalent in women undergoing surgery for endometriosis and may suggest a higher risk of infertility. Biomed Res Int 2017:8967803 Donnez J, Dolmans M-M, Fellah L. What if deep endometriotic nodules and uterine adenomyosis were actually two forms of the same disease? Fertil Steril 2019;111(03):454–456 Khan KN, Fujishita A, Koshiba A, et al. Biological differences between intrinsic and extrinsic adenomyosis with coexisting deep infiltrating endometriosis. Reprod Biomed Online 2019;39 (02):343–353 Dior UP, Nisbet D, Fung JN, et al. The association of sonographic evidence of adenomyosis with severe endometriosis and gene expression in eutopic endometrium. J Minim Invasive Gynecol 2019;26(05):941–948 Suda K, Nakaoka H, Yoshihara K, et al. Different mutation profiles between epithelium and stroma in endometriosis and normal endometrium. Hum Reprod 2019;34(10):1899–1905 Moore L, Leongamornlert D, Coorens THH, et al. The mutational landscape of normal human endometrial epithelium. Nature 2020;580(7805):640–646 Zannoni L, Del Forno S, Raimondo D, et al. Adenomyosis and endometriosis in adolescents and young women with pelvic pain: prevalence and risk factors. Minerva Pediatr 2020 Arnold LL, Ascher SM, Simon JA. Familial adenomyosis: a case report. Fertil Steril 1994;61(06):1165–1167 Xiang Y, Sun Y, Yang B, et al. Transcriptome sequencing of adenomyosis eutopic endometrium: A new insight into its pathophysiology. J Cell Mol Med 2019;23(12):8381–8391 Wang W, Taylor RN, Bagchi IC, Bagchi MK. Regulation of human endometrial stromal proliferation and differentiation by C/EBPβ Seminars in Reproductive Medicine Vol. 38 No. 2-3/2020 Downloaded by: World Health Organization ( WHO). Copyrighted material. 37 women with adenomyosis. Int J Gynecol Pathol 2009;28(02): 157–163 Schindl M, Birner P, Obermair A, Kiesel L, Wenzl R. Increased microvessel density in adenomyosis uteri. Fertil Steril 2001;75 (01):131–135 Mori M, Furusawa A, Kino N, Uno M, Ozaki Y, Yasugi T. Rare case of endometrioid adenocarcinoma arising from cystic adenomyosis. J Obstet Gynaecol Res 2015;41(02):324–328 Kazandi M, Zeybek B, Terek MC, Zekioglu O, Ozdemir N, Oztekin K. Grade 2 endometrioid adenocarcinoma arising from adenomyosis of the uterus: report of a case. Eur J Gynaecol Oncol 2010;31(06):719–721 Baba A, Yamazoe S, Dogru M, Ogawa M, Takamatsu K, Miyauchi J. Clear cell adenocarcinoma arising from adenomyotic cyst: a case report and literature review. J Obstet Gynaecol Res 2016;42(02): 217–223 Koike N, Tsunemi T, Uekuri C, et al. Pathogenesis and malignant transformation of adenomyosis (review). Oncol Rep 2013;29(03): 861–867 Longacre TA, Chung MH, Rouse RV, Hendrickson MR. Atypical polypoid adenomyofibromas (atypical polypoid adenomyomas) of the uterus. A clinicopathologic study of 55 cases. Am J Surg Pathol 1996;20(01):1–20 Young RH, Treger T, Scully RE. Atypical polypoid adenomyoma of the uterus. A report of 27 cases. Am J Clin Pathol 1986;86(02):139–145 Singh N, Hirschowitz L, Zaino R, et al. Pathologic prognostic factors in endometrial carcinoma (other than tumor type and grade). Int J Gynecol Pathol 2019;38(Suppl 1):S93–s113 FIGO Committee on Gynecologic Oncology. FIGO staging for carcinoma of the vulva, cervix, and corpus uteri. Int J Gynaecol Obstet 2014;125(02):97–98 Levgur M, Abadi MA, Tucker A. Adenomyosis: symptoms, histology, and pregnancy terminations. Obstet Gynecol 2000;95(05): 688–691 Hulka CA, Hall DA, McCarthy K, Simeone J. Sonographic findings in patients with adenomyosis: can sonography assist in predicting extent of disease? AJR Am J Roentgenol 2002;179(02): 379–383 Nishida M. Relationship between the onset of dysmenorrhea and histologic findings in adenomyosis. Am J Obstet Gynecol 1991; 165(01):229–231 Sammour A, Pirwany I, Usubutun A, Arseneau J, Tulandi T. Correlations between extent and spread of adenomyosis and clinical symptoms. Gynecol Obstet Invest 2002;54(04):213–216 Grimbizis GF, Mikos T, Tarlatzis B. Uterus-sparing operative treatment for adenomyosis. Fertil Steril 2014;101(02):472–487 Exacoustos C, Morosetti G, Conway F, et al. New sonographic classification of adenomyosis: Do type and degree of adenomyosis correlate to severity of symptoms? J Minim Invasive Gynecol 2020;27(06):1308–1315 Signorile PG, Baldi F, Bussani R, et al. Embryologic origin of endometriosis: analysis of 101 human female fetuses. J Cell Physiol 2012;227(04):1653–1656 Signorile PG, Baldi A. Endometriosis: new concepts in the pathogenesis. Int J Biochem Cell Biol 2010;42(06):778–780 Benagiano G, Brosens I, Habiba M. Adenomyosis: a life-cycle approach. Reprod Biomed Online 2015;30(03):220–232 Yang J-H, Wu MY, Chen CD, Chen MJ, Yang YS, Ho HN. Altered apoptosis and proliferation in endometrial stromal cells of women with adenomyosis. Hum Reprod 2007;22(04):945–952 Jones RK, Searle RF, Bulmer JN. Apoptosis and bcl-2 expression in normal human endometrium, endometriosis and adenomyosis. Hum Reprod 1998;13(12):3496–3502 Wang F, Li H, Yang Z, Du X, Cui M, Wen Z. Expression of interleukin-10 in patients with adenomyosis. Fertil Steril 2009; 91(05):1681–1685 Wang F, Wen Z, Li H, Yang Z, Zhao X, Yao X. Human leukocyte antigen-G is expressed by the eutopic and ectopic endometrium of adenomyosis. Fertil Steril 2008;90(05):1599–1604 Antero et al. Pathology and Pathogenesis of Adenomyosis Antero et al. involves cyclin E-cdk2 and STAT3. Mol Endocrinol 2012;26(12): 2016–2030 80 Zahnow CA. CCAAT/enhancer-binding protein β: its role in breast cancer and associations with receptor tyrosine kinases. Expert Rev Mol Med 2009;11:e12 81 Streuli I, Santulli P, Chouzenoux S, Chapron C, Batteux F. Activation of the MAPK/ERK cell-signaling pathway in uterine smooth muscle cells of women with adenomyosis. Reprod Sci 2015;22 (12):1549–1560 82 Hufnagel D, Li F, Cosar E, Krikun G, Taylor HS. The role of stem cells in the etiology and pathophysiology of endometriosis. Semi Reprod Med 2015;33(05):333–340 83 Vannuccini S, Tosti C, Carmona F, et al. Pathogenesis of adenomyosis: an update on molecular mechanisms. Reprod Biomed Online 2017;35(05):592–601 84 Gargett CE. Uterine stem cells: What is the evidence? Hum Reprod Update 2007;13(01):87–101 Downloaded by: World Health Organization ( WHO). Copyrighted material. 118 Seminars in Reproductive Medicine Vol. 38 No. 2-3/2020