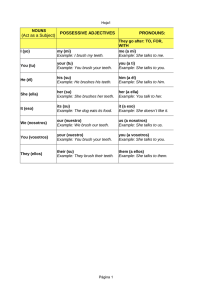
10 Oral Anatomy and Physiology Key learning points A factual knowledge of • the gross anatomy of the tissues and structures of the oral cavity • the microscopic anatomy of teeth and their supporting structures A working knowledge of • the functions of the tissues and structures of the oral cavity • the morphology and functions of teeth • the salivary glands The oral cavity contains many anatomical structures besides the teeth, and to gain a full understanding of the topics of oral health and disease, the dental nurse must have knowledge of all these structures. The bones, muscles, nerves and blood supply to this region are discussed in Chapter 9; this chapter will focus on the following specific anatomical structures and their physiology. • • • • • Oral soft tissues and soft palate. Tongue. Teeth. Supporting structures of the periodontium. Salivary glands. Levison’s Textbook for Dental Nurses, Eleventh Edition. By Carole Hollins. © 2013 John Wiley & Sons, Ltd. Published 2013 by John Wiley & Sons, Ltd. Companion website: www.levisonstextbookfordentalnurses.com Soft tissues of the mouth Epithelial membrane The whole of the mouth is lined with epithelial mucosal tissue as a type of mucous membrane, which is continuous with that lining the digestive tract. Throughout the oral cavity there are three types of this membrane, each with its own particular features. • • • Lining membrane. Masticatory membrane. 249 Specialised membrane. Their details are shown in Table 10.1. The first row identifies the area of the oral cavity where each type of epithelial membrane is normally found, while the second row describes its appearance in each case. The final row explains the function(s) of the membrane in relation to its appearance – so the ridged nature of the masticatory membrane, for example, and its firm underlying attachment are explained by its function of providing a hard-wearing surface that can withstand the regular abrasive contact it has with food. Within the oral cavity, the space between the posterior teeth and the mucous membrane lining the cheeks is called the buccal sulcus whilst that between the anterior teeth and lips is the labial sulcus. The upper lip is attached to the centre of the gingiva above the central incisors by a band of fibrous tissue called a frenum, and when this attachment is thicker than usual, there is often a space created between the two incisor teeth, called a median diastema. Table 10.1 Oral mucous membranes Lining membrane Masticatory membrane Specialised membrane Covers inner surfaces of the cheeks and lips, floor of the mouth, underside of the tongue, soft palate Covers gingivae, topside and edges of the tongue, hard palate Interspersed throughout the masticatory membrane covering of the topside and edges of the tongue Appears as red, smooth and moist membrane, which can be squashed and stretched Contains minor salivary glands Appears as red, moist membrane, often ridged or stippled, firmly attached to underlying structures – forms the mucoperiosteum where it lies over the alveolar processes Appear as discrete papillary structures of the taste buds, in a visible pattern over the tongue Provides a physical barrier between anything entering the mouth and the deep structures of the oral cavity, acts as a cushion, provides lubrication and cleansing Provides a hard-wearing surface that prevents traumatic damage from food, chemicals, oral hygiene products, etc. Provides taste sensation 250 Figure 10.1 Tonsils and oropharynx. Soft palate The soft palate is a flap of soft tissue attached to the back of the hard palate. Its function is to seal off the oral cavity from the nasal cavity during swallowing, in order to prevent food passing up into the nose. The free edge of the soft palate has a central prolongation called the uvula. You can see this for yourself by looking in a mirror with your mouth wide open. To either side of this area at the back of the mouth, called the oropharynx, lie the tonsils which appear as small ball-like structures with a pitted surface (Figure 10.1). They are most noticeable when inflamed during a throat infection, such as tonsillitis. Tongue The floor of the mouth lies within the arch of the mandible and is occupied by the tongue, which is a muscular organ situated in the oral cavity and also the throat. The posterior one-third section, the base of the tongue, lies in the throat and attaches to the floor of the mouth. It is relatively firmly attached and is mainly concerned with swallowing movements. The correct term for swallowing is deglutition. The remaining anterior two-thirds of the tongue, the body, lie within the oral cavity and this section is relatively moveable, being able to perform numerous convoluted movements, as it is composed of many bands of muscle lying in various directions. It is attached to the floor of the mouth by a thin band of fibrous tissue called the lingual frenum. Where excess of this fibrous tissue occurs, the tongue is held more rigidly than normal so that its movements are restricted, and the person affected is often described as ‘short-tongued’ or ‘tongue-tied’, due to the lisp created as they speak. The body of the tongue is concerned with taste, chewing activities and speech. All the muscles of the tongue are innervated by the hypoglossal nerve (12th cranial nerve). The functions of the tongue are as follows. • Speech – by allowing certain sounds to be created by touching the tongue to the upper anterior teeth or the palate (such as ‘s’, ‘t’, ‘n’, ‘the’). • Taste – the tongue is covered by various different types of taste buds (including filiform papillae, fungiform papillae and vallate papillae – Figure 10.2) that allow recognition of the four basic tastes – sweet, sour, salt and bitter. 251 Figure 10.2 Taste bud. • Aids mastication – by assisting the buccinator muscles to package ingested food into a parcel, or bolus, for easier chewing before swallowing. • • Aids swallowing – by guiding the bolus to the back of the mouth, the oropharynx. Cleansing – by moving around the oral cavity and the smooth surfaces of the teeth to dislodge food particles. The lining epithelium of mucous membrane covering the underside of the tongue is so thin that it allows the very rapid absorption of drugs placed here into the underlying capillaries of the tongue. Patients given glyceryl trinitrate (GTN) tablets or spray for the treatment of angina pectoris use their medications in this way. Swallowing Swallowing is a complex muscular action which aims to direct the food bolus into the oesophagus while also preventing it from entering the nasal cavity or the larynx. The bolus is mixed with saliva to lubricate it, and then propelled by the tongue from the mouth to the oropharynx, and then into the oesophagus. The sequence of events in the swallowing process is as follows (see Figure 5.11). • The lubricated ball of food is propelled backwards to the oropharynx by the actions of the body of the tongue. • The soft palate rises up and seals off the nasopharynx from the oropharynx, to prevent the bolus from passing upwards into the nose. • At the same time, the larynx lifts up and is sealed by the epiglottis to prevent the bolus passing into the trachea and being inhaled into the lungs. • The bolus is propelled downwards from the oropharynx by the base of the tongue, and to the oesophagus by the throat muscles. • Oesophageal muscles then move the bolus downwards by peristalsis into the stomach. Disorders of the tongue Glossitis This is soreness and inflammation of the tongue, and can occur in conditions such as anaemia, vitamin B deficiency and hormonal disturbances (including pregnancy). It is associated with a thin, smooth glazed appearance of the normally thick layer of mucous membrane on its upper surface. Dysphagia 252 This is the condition of having difficulty in swallowing, which occurs relatively frequently and has several causes. • Psychological – an inability to swallow (usually) medication in tablet form, although food and drink can be swallowed normally by the patient. • Xerostomia – dry mouth syndrome, where reduced salivary flow prevents adequate bolus lubrication. • • • Oesophagitis – inflammation of the oesophagus, often due to acid reflux. Other conditions affecting pharyngeal or oesophageal function, including cancers. Central nervous system disorders preventing correct muscle innervation, such as stroke and multiple sclerosis. Teeth The teeth are the anatomical structures within the oral cavity that are of the greatest relevance to the dental team, as their development, health, disease and restoration are the fundamentals of dentistry. The teeth have the following functions. • • • To cut up and masticate food into suitable sized portions before swallowing. • • • • Central and lateral incisors To expose the food surfaces to enzymes and allow digestion to begin. To support the oral soft tissues of the cheeks and tongue, and therefore enable clear speech. Humans have two sets of teeth – the primary (deciduous) teeth of childhood and the secondary (permanent) teeth of adulthood. The number and type of teeth in each set differ, although the shape of the common ones is the same. The detailed anatomical shape of each tooth, and its function, is called tooth morphology. The four types present in the secondary dentition, from the midline of the mouth posteriorly, are as follows. Canine First and second premolars First, second and third molars The primary dentition has just two molars and is made up of just three different types of teeth – there are no premolars present. Cusp s Fissure Crown Enamel Neck Dentine Pulp Root 253 Cementum Apical foramen Figure 10.3 Structure of a tooth. Each tooth of all types, and in both sets, has three sections – the crown, the neck and the root(s). The crown is the section of the tooth visible in the oral cavity, following its eruption from the underlying alveolar bone. The neck is the section where the tooth and the gingival tissues are in contact with each other at the point where the tooth emerges through the gums, and the root is the (usually) non-visible section that holds the tooth in its bony socket. All teeth are composed of the same four tissues. • • Enamel – a highly calcified tissue covering the whole crown of the tooth. • • Cementum – a thin calcified covering of the root dentine only. Dentine – a less calcified tissue than enamel, which forms the inner bulk of the crown and root. Pulp – the inner neurovascular tissue of the tooth, within the central pulp chamber. The structure of a typical tooth is shown in Figure 10.3. Microscopic structure of the teeth The differences in the microscopic structure of the four layers of the teeth are what determine how they function, how they develop disease, how they are treated for that disease, and how they are restored or extracted by the dental team. Enamel This is the highly calcified, protective outer covering of the crown and is the hardest substance in the body. Its properties and microscopic structure are as follows. • It is made up of 96% mineral crystals (inorganic) arranged as prisms in an organic matrix called the interprismatic substance. • • • • • The main mineral crystals are calcium hydroxyapatite. The prisms lie at right angles to the junction with the next tooth layer, the dentine. The junction between these two layers is called the amelodentinal junction (ADJ). Enamel is formed before tooth eruption by the ameloblast cells, which lie at the ADJ. It contains no nerves nor blood vessels and therefore cannot experience any sensation. 254 • It is a non-living tissue which cannot grow and repair itself, so progressive damage caused by injury or tooth decay is permanent. • It can, however, remineralise its surface after an acid attack, by taking in minerals from saliva and from oral health products such as toothpaste and mouthwash. • The crystal structure can also be altered without undergoing acid attack, by the exchange of hydroxyl ions in the hydroxyapatite with fluoride, to form fluorapatite crystals – these make the enamel surface harder and more resistant to acid attack. • The enamel layer is thickest over the biting surface of the tooth (the occlusal surface or the incisal edge) and thinnest at the neck of the tooth (the cervical margin). • It is translucent, so the shade of a tooth is determined by the colour of the underlying dentine. Dentine This tissue forms the main bulk of a tooth and occupies the interior of the crown and root. It is also mineralised, but to a lesser extent than enamel, and is covered by enamel in the crown of the tooth and by cementum in the root of the tooth. Its properties and microscopic structure are as follows. • • It consists of up to 80% inorganic tissue, mainly calcium hydroxyapatite crystals. • In a fully formed tooth, these odontoblast cells lie along the inner edge of the pulp chamber only, but are present throughout life and can lay down more dentine as required. • • In this way, it can repair itself by laying down secondary dentine. • The hollow tubes contain sensory nerve endings called fibrils, which run from the nerve tissue within the pulp chamber. • Dentine is therefore a living tissue and can transmit sensations of pain and thermal changes to the brain. • Its hollow structure allows it a degree of elasticity so that it can absorb normal chewing forces without breaking. • However, it also allows tooth decay (caries) to spread more rapidly through its hollow structure. • Dentine is a yellowish colour, and gives teeth their individual shade. It is composed of hollow tubes which originally surrounded the cells within the dentine structure as it was first being formed. This type of dentine is also formed as part of the natural ageing process, and its formation gradually narrows the pulp chamber. Cementum This is the calcified protective outer covering of the root and is similar in structure to bone. Cementum meets enamel at the neck of the tooth, and normally lies beneath the gingivae. Its properties and microscopic structure are as follows. • • Around 65% mineralised, with calcium hydroxyapatite crystals. • This allows the attachment of the root to the periodontal ligament, and therefore to the walls of the tooth socket. The crystals lie within a matrix of fibrous tissue, with the ends of collagen fibres from the periodontal ligament inserted into the outer layer of the cementum. • The cementum is formed by cells called cementoblasts and they can continue laying down more tissue layers when required. • The thickness of cementum may vary at different parts of the root, and changes throughout life, depending on the forces exerted on individual teeth. • The cementum contains no nerves nor blood vessels itself, so it receives nutrients from the periodontal ligament. Pulp Unlike enamel, dentine and cementum, the pulp contains no mineral crystals and is 255 composed purely of soft tissue. It lies within the very centre of every tooth, from the crown as the coronal pulp and into each root as the radicular pulp. The radicular pulp is often referred to as the ‘root canal’ of the tooth. The properties and microscopic structure of the pulp are as follows. • • The pulp contains sensory nerves and blood vessels. • They allow the tooth to feel hot, cold, touch and pain by the stimulation of its sensory nerve endings which run as fibrils in the hollow dentine tubules. • These pulp tissues enter the tooth through the apical foramen, lying at the root apex of every tooth. • • The pulp chamber itself is lined by the odontoblast cells which form dentine. • It can also become blocked by pulp stones which are formed by lumps of calcium-containing crystals. • The point where the cementum and the root dentine are in contact with each other is called the dentinocemental junction. • Some teeth have additional contact between the pulp and the surrounding periodontal ligament via accessory canals, whose presence can make successful endodontic treatment of the tooth very difficult to achieve. The sensory nerves are end sections of the trigeminal nerve (fifth cranial nerve), either as the inferior dental nerve for the lower teeth or one of the superior dental nerves for the upper teeth. The chamber gradually narrows with age, so that it can become completely obliterated in older patients, making endodontic treatment very difficult. Tooth morphology All people have two sets of teeth: the first or deciduous teeth, and the second or permanent teeth. All have different appearances or morphology, which depends on the set and the individual teeth themselves. Their morphology enables each tooth to be individually identified by any trained member of the dental team, this identification being based on the tooth shape and size, the number of cusps present, and the number of roots present. Curvature of the roots will also help to indicate whether a tooth is from the right or the left side of the dental arch. Deciduous teeth The deciduous teeth are the first set and are also known as milk, temporary or primary teeth (Figure 10.4). • Total set of 20 teeth, 10 in each jaw. • • They begin developing in the jaws of the early embryo, around 6 weeks after conception. They are referred to in dentistry by letter – A, B, C, D and E – starting from the midline of the jaw. A Central incisor Lateral incisor Canine B C 1st molar D 2nd molar E 256 Figure 10.4 Deciduous teeth. Table 10.2 Primary dentition: tooth and root morphology Tooth Letter Number of roots Number of cusps (where applicable) Central incisor A One N/A Lateral incisor B One N/A Canine C One N/A First molar D Three Four Second molar E Three Five Central incisor A One N/A Lateral incisor B One N/A Canine C One N/A First molar D Two Four Second molar E Two Five Uppers Lowers • • They are smaller than permanent teeth, and whiter in colour. • The roots of the deciduous molars are splayed out to accommodate the presence of the underlying permanent premolar teeth, so the roots are described as divergent. • They have a larger pulp chamber than the permanent teeth, with thinner enamel, which makes them more prone to the development of dental caries. • They begin erupting at around 6 months of age, and are usually all present by about 29 months, although individual variation does occur. Their roots are resorbed by the underlying permanent teeth, as the deciduous teeth gradually loosen and fall out – this is called exfoliation. The five deciduous teeth present in each quadrant of the oral cavity are the central and lateral incisors, the canine, and the first and second molars. There are no premolar teeth in the primary dentition. Their tooth and root morphology is summarised in Table 10.2. Table 10.3 Average eruption dates of the deciduous teeth Tooth Letter Uppers in months Lowers in months Central incisor A 10 8 Lateral incisor B 11 13 Canine C 19 20 First molar D 16 16 Second molar E 29 27 257 Figure 10.5 Permanent teeth. The three roots of the upper molars are arranged as a tripod, with the developing permanent premolar teeth lying within this area, while the two roots of the lower molars lie one in front of the other in the alveolar bone of the mandible. The average eruption dates of the deciduous teeth, in months, are shown in Table 10.3. The usual eruption pattern of the deciduous dentition is the lower central incisors first, followed by the other incisors, then the first molars followed by the canines, and finally the second molars. The dentition begins changing again at about 6 years of age, when the permanent teeth begin to erupt by resorbing the roots of their deciduous predecessors and causing their exfoliation. Permanent teeth Permanent teeth are the second and final set, and are also called the adult teeth (Figure 10.5). • Total set of 32 teeth, 16 in each jaw. • • They begin developing in the jaws just before birth, and continue for many years afterwards. • They are of very similar morphology to the deciduous teeth, with eight extra teeth called premolars present, two in each quadrant. • They are larger in size and darker in colour than deciduous teeth, with relatively smaller pulp chambers. They are referred to in dentistry by number – 1, 2, 3, 4, 5, 6, 7 and 8 – starting from the midline of the jaw. • The three permanent molar teeth in each quadrant develop behind the deciduous teeth, using the space created as the jaws grow during childhood and the teenage years. Table 10.4 Permanent teeth: tooth and root morphology Tooth Number Number of roots Number of cusps (where applicable) Central incisor 1 One N/A Lateral incisor 2 One N/A Canine 3 One N/A First premolar 4 Two Two Second premolar 5 One Two First molar 6 Three Five Second molar 7 Three Four Third molar 8 Three Four Central incisor 1 One N/A Lateral incisor 2 One N/A Canine 3 One N/A First premolar 4 One Two Second premolar 5 One Two First molar 6 Two Five Second molar 7 Two Four Third molar 8 Two Four Uppers 258 Lowers • • So the deciduous molar teeth are succeeded by the permanent premolar teeth. • They begin erupting at around 6 years of age, and all except the third molars are usually present by the age of 13 years. • The third molars may be congenitally missing, present but unerupted due to lack of jaw space, or they may erupt from the age of 18 years onwards. It is relatively common for some adult teeth to be congenitally missing from the dentition, especially the third molars. The eight permanent teeth present in each quadrant of the oral cavity are the central and lateral incisors, the canine, the first and second premolars, and the first, second and third molars. Their tooth and root morphology is summarised in Table 10.4. Again, the three roots of the upper molars are arranged as a tripod, and the two roots of the lower molars lie one in front of the other in the alveolar bone of the mandible. The two roots of Table 10.5 Average eruption dates of the permanent teeth 259 Tooth Number Uppers in years Lowers in years Central incisor 1 7–8 6–7 Lateral incisor 2 8–9 7–8 Canine 3 10–12 9–10 First premolar 4 9–11 9–11 Second premolar 5 10–11 9–11 First molar 6 6–7 6–7 Second molar 7 12–13 11–12 Third molar 8 18–25 18–25 the upper first premolar teeth lie across the maxillary alveolar bone. The average eruption dates of the permanent teeth, in years, are shown in Table 10.5. Permanent teeth erupt before their roots are fully grown. About two-thirds of their root length has formed when permanent teeth erupt and the apex is still wide open. It takes another 3 years before root growth is complete and the apex closes. The only exceptions are canines and third molars which do not erupt until root growth is complete. Surfaces of the teeth To enable the dental team to describe and discuss individual teeth and the treatment they may require, each surface of every tooth has its own name in relation to the midline of each jaw, and the anatomical structures that they sit against. It is this tooth surface nomenclature that allows the charting of every patient to be recorded accurately – a key task of the dental nurse. Charting is discussed in detail in Chapter 12, as it forms an important part of oral health assessment techniques. The general terminology used for describing the tooth surfaces is summarised below. • Labial – surface adjacent to the lips, applies in both arches and relates to incisor and canine teeth. • Buccal – surface adjacent to the buccinator muscle of the cheeks, applies in both arches and relates to premolars and molars. • Palatal – surface adjacent to the palate, applies to all maxillary teeth. 260 • • Lingual –surface adjacent to the tongue, applies to all mandibular teeth. • Incisal – biting edge of anterior teeth, applies to both arches and relates to incisors (canines have a cusp rather than an edge). • Mesial – interdental surface of all teeth closest to the midline of each arch, so the front interdental surface (Figure 10.6). • Occlusal – biting surface of posterior teeth, applies to both arches and relates to premolars and molars (Figure 10.7). The sharply raised points of these surfaces are called cusps, and the crevices between them are the fissures. Palate 6 Buccal Palatal Occlusal Tongue 6 Lingual Buccal Figure 10.6 Surfaces of the teeth – mesial aspect. Tongue 5 6 Mesial Occlusal Buccal Lingual Distal Contact point Mesial Buccal Occlusal Lingual Distal Figure 10.7 Surfaces of the teeth – occlusal aspect. • • Distal – interdental surface of all teeth furthest from the midline of each arch. • Cervical – the neck region of any tooth, on the buccal, labial, palatal or lingual surface. Contact point – the point where the mesial and distal surfaces of adjacent teeth are in contact with each other. Using these named surfaces, the anatomy of individual teeth can be described in detail. Anatomy of individual teeth A collection of extracted teeth in good condition is a great help in learning dental anatomy and tooth morphology, but they are more difficult to acquire nowadays due to infection control issues. The secondary dentition is shown diagrammatically for clarity in Figure 10.8, and various extracted teeth are shown in Figure 10.9. In the primary dentition there are five teeth in each quadrant of the mouth: central and lateral incisors, a canine, and first and second molars. In the secondary dentition there are eight teeth in each quadrant: central and lateral incisors, a canine, first and second premolars, first, second and third molars. The morphology and function of the similar teeth in each dentition are the same. Uppers Longest root Largest molar 261 Largest incisor 8 7 6 5 Three roots Lowers 8 7 4 3 2 1 Two roots 6 5 4 3 Two roots 2 1 Smallest incisors Figure 10.8 Tooth anatomy. Central incisor • • • • • • Chisel-shaped crown with an incisal biting edge. Single root. Palatal or lingual surface has a raised area called the cingulum. Upper permanent central incisor is the largest of all incisors. Lower central incisor is the smallest tooth. Functions are to: ○ cut into food and separate bite-size chunks from the food product ○ assist tongue in making certain speech sounds (‘th’) ○ assist lips in making certain speech sounds (‘f’). Lateral incisor • • Narrow, chisel-shaped crown with an incisal biting edge. • Palatal or lingual surface has a cingulum. Single root. • Lower lateral incisor sometimes has a second (lingual) root canal, especially if the root has split into two. • Function is to bite in a scissor action with the upper incisors, and break off separate bite-size portions. • Uppers can be congenitally absent or develop as abnormally small teeth – often called peg laterals. (a) (b) (c) (d) (e ) (f ) 262 (g) (h ) (i ) (j) (n ) (k ) (l) (m) (o ) (p) Figure 10.9 Features of individual teeth. (a) Upper right lateral incisor. (b) Upper right central incisor. (c) Lower left central incisor. (d) Lower left lateral incisor. (e) Upper right canine. (f) Lower left canine. (g) Upper right second premolar. (h) Upper right first premolar. (i) Lower left second premolar. (j) Lower left first premolar. (k) Upper right third molar. (l) Upper right second molar. (m) Upper right first molar. (n) Lower right first molar. (o) Lower left second molar. (p) Lower left third molar. Canine • • • • • Robust tooth forming the ‘corner’ of each dental quadrant. • Functions are to: ○ pierce food and tear into it ○ support the oral soft tissues at the ‘corners’ of the oral cavity Incisal edge is sloped to a sharp cusp tip that lies more mesially than distally. Single root and the longest of all teeth. Root apex sometimes curves distally slightly. Upper and lower canines have a cingulum, the upper is joined to the cusp tip by a palatal ridge. ○ provide ‘guidance’ for normal occlusion, especially when the mandible is moved sideways. First premolar • • • Not present in primary dentition. • • • • • Cusps are of equal height in uppers, but lingual is always smaller in lowers. • • Lower first premolar has one root. • Usual tooth to be extracted for orthodontic reasons, as it lies midway along the dental arch and can therefore relieve either anterior or posterior crowding. Are the permanent successors to the deciduous first molars. Has occlusal surface arranged as two cusps lying bucally and palatally, or buccally and lingually (upper or lower). Mesial and distal edges of all are raised into marginal ridges. 263 Upper has two roots lying in the same orientation as the cusps. Root apices sometimes curve distally. Concavity between the roots mesially is called the canine fossa, and can be a harbour for micro-organisms and calculus in patients with periodontal disease. Functions are to: ○ assist canine to pierce and tear food (cusps) ○ assist molars to grind food (occlusal surface) ○ help maintain the shape of the mouth. Second premolar • • • • • • • • • • • • Not present in primary dentition. Is the permanent successor to the deciduous second molar. Has occlusal surface arranged as two cusps, like the first premolars. Cusps are of equal height in all. Mesial and distal edges are raised as marginal ridges. Upper is usually slightly smaller than the first premolar. Lower is usually slightly larger than the first premolar. Single root, apex sometimes curves distally. Root apex of uppers can lie very close to the floor of the maxillary antrum. Functions as for first premolars. Lowers are sometimes congenitally absent. Can become impacted in either arch, following the early loss of deciduous predecessor and the eruption of the permanent first molars, so that the arch space for the second premolars is lost. First molar • Primary first molars are succeeded by the first premolars, and are the smaller of the deciduous molars. 264 • Widely divergent roots present in deciduous molars, with the crown of the developing first premolar lying contained by them. • • • • • • Permanent first molars are the largest of all teeth. • • Lowers have two roots arranged as mesial and distal, apices are sometimes curved distally. • • Function is to grind and masticate food chunks so that they can be swallowed. Upper has occlusal surface arranged as four cusps – two buccally and two palatally. Fifth palatal cusp of uppers may develop as the cusp of Carabelli. Lower has five cusps – three buccal and two lingual. Mesial and distal edges are raised as marginal ridges. Uppers have three roots arranged as a tripod – large palatal, shorter mesiobuccal and distobuccal – apices of latter two are sometimes curved distally. Junction of the roots beneath the crown is called the furcation area and can be a harbour for micro-organisms when periodontal disease is present. Root apices of uppers can lie close to, or even penetrate, the floor of the maxillary antrum. Second molar • Primary second molars are succeeded by the second premolars, and are the larger of the deciduous molars. • Widely divergent roots present in deciduous molars, with the crown of the developing second premolar lying contained by them. • • • • • • • • Crown of both upper and lower is smaller than that of the first molar. Has occlusal surface arranged as four cusps. Mesial and distal edges are raised as marginal ridges. Uppers have three roots, arranged as for the first molar and sometimes curved distally. Lower has two roots, arranged as for the first molar and sometimes curved distally. Furcation area present in both. Function as for the first molar. Root apices of the upper can also lie in close proximity to the floor of the maxillary antrum. Third molar • • • • • • • • • • Not present in the primary dentition. Not always present in the secondary dentition. Referred to as wisdom teeth. Morphology varies widely. Smaller crown size than the second molar usually. Has occlusal surface arranged as three or four cusps, with marginal ridges present. Uppers usually have three roots, but not always. Lowers usually have two roots, but not always. Furcation area present unless the roots are fused together. Function as for the first and second molars. • Often extracted if involved with recurrent bouts of disease, or if impacted and associated with pericoronitis. Occlusion of the teeth When the upper and lower teeth are closed together, they are said to be in occlusion. The arch of the upper teeth is larger than the lower so upper teeth overlap the lower on the buccal side. Lower buccal cusps accordingly bite into the fissure between upper buccal and palatal cusps (Figure 10.10). The mesial edges of upper and lower central incisors form one straight vertical line. This is called the midline. As lower central incisors are much narrower than uppers, all the remaining lower teeth occlude with two upper teeth – their corresponding upper tooth and the one in front. From this explanation of normal occlusion it is clear that: • the mesial cusp of the upper first molar bites into the fissure between the mesial and distal cusps of the lower first molar • • the lower canine bites in front of the upper canine the mesial edges of the upper and lower central incisors form one straight vertical midline. Palate Tongue 1 2 2 1 3 1 3 1 1 2 6 5 4 4 2 1 5 6 7 7 Figure 10.10 Normal occlusion. Supporting structures of the periodontium The supporting structures are collectively referred to as the periodontium, and are those lying around the roots of the teeth which hold them in their sockets (Figure 10.11). Their hold on the teeth is not a rigid one; rather, it allows the teeth to ‘bounce’ in their sockets so that there is some shock absorption effect when the teeth are used for chewing. This prevents fracture of the tooth under normal occlusal forces. The four supporting structures are as follows. 266 • Alveolar bone– specialised ridge of bone over the bony arch of each jaw, where the teeth sit in their sockets. • Gingiva – specialised soft tissue covering of the alveolar processes, that are also in attachment with the teeth at their necks. • Periodontal ligament – connective tissue attachment between the tooth and the alveolar bone. • Cementum – hard tissue covering of the root that anchors the periodontal ligament to the tooth (discussed previously). 265 Alveolar bone The maxilla and the mandible both contain a horseshoe-shaped ridge of bone called the alveolar process. It is here that the teeth form during the growth of the fetus and then the Figure 10.11 Supporting structures of a tooth. child, and from where they erupt into the mouth at various ages. The properties of the alveolar bone are as follows. • It is a specialised bone found only in the jaws. • Its outer layer is made of hard, compact bone the outer surface of which is called the lamina dura. • The inner layer is called cancellous bone and is sponge-like in appearance, to allow the passage of the various nerves and blood vessels that supply the jaws, teeth and surrounding oral soft tissues. • The sole purpose of the alveolar bone is to support the teeth, and it is gradually lost when a tooth is extracted as the bone slowly resorbs away. • The teeth lie within individual sockets in the alveolar bone, each one being lined by lamina dura which shows on dental radiographs as a continuous white line – its absence indicates the presence of dental disease. • The outer surface of the alveolar bone is covered in specialised alveolar mucosa, which forms the gingivae (gums) around the necks of the teeth. • Destruction of the alveolar bone occurs in periodontal disease. Gingiva This is the correct anatomical term for the gums (plural – gingivae). It is a continuous layer of specialised epithelium found only in the oral cavity, which is firmly attached to the underlying alveolar bone as a mucoperiosteal layer of tissue. This layer is raised as a flap during oral surgical procedures, to expose the bone below. There are three distinct areas of gingival coverage (Figure 10.12). Gingival crevice (sulcus) Enamel of tooth Sulcular epithelium 267 Marginal epithelium Epithelial attachment of the junctional epithelium • Attached gingiva – that covering the majority of the alveolar process, which is firmly attached to the underlying bone as the mucoperiosteum. • Marginal gingiva – that forming the gingival margin of the teeth, which is free from the underlying bone and follows the shape of each tooth in the arch, as well as extending between the teeth in the contact areas. The level at which these two areas meet is called the free gingival groove. • Junctional tissues – the specialised gingival tissue lying within the gingival crevice and forming the anatomical junction between the teeth and the oral epithelium – this point is called the junctional attachment, and the tissues are called the junctional epithelium. Free gingival groove Attac hed gingi va Figure 10.12 The three gingival areas. The junctional attachment is the point where the integrity of the periodontium has to be maintained in order to avoid the devastation of periodontal disease, and the resultant tooth loss that can occur. It provides a mechanical barrier between the oral cavity and the deeper periodontal tissues, preventing micro-organisms from gaining entry and causing disease. The main method of maintaining the health and functionality of the whole gingival area is to carry out good levels of oral hygiene on a daily basis. During a periodontal examination, the gingival crevice should be less than 3 mm deep when probed, with the periodontal probe contacting the junctional attachment at its deepest point. The properties of the gingiva are as follows. • The gingivae fit around 268 the neck of every tooth like a tight cuff, when healthy. • The gingival crevice exists as a shallow space of less than 3 mm between the tooth surface and the gingival margin, and contains the junctional epithelium. • A natural mound of gingival tissue occurs between each tooth and is called the interdental papilla. • • In health, the gingivae are pink in colour with a stippled surface, like orange peel. • Gingivitis appears as red and shiny gingivae that are swollen due to their inflammation, and they bleed easily on touching – either during tooth brushing or during dental exami nation. • The swollen appearance of the inflamed gingivae presents as ‘false pockets’ when probed, giving the impression that the gingival crevice is deeper than 3 mm – in fact, the junctional attachment is still present and the underlying periodontal tissues are unaffected by the inflamed condition of the gingivae. • The gingiva can also be stimulated to overgrow and become hyperplastic as a side-effect of various drugs being taken by the patient, including some antihypertensives (such as nifedipine) and some drugs used to control epilepsy (such as phenytoin). Inflammation of the gingivae is called gingivitis; it affects the marginal gingivae and occurs in the presence of dental plaque due to poor oral hygiene control. Oral diseases, including gingivitis and periodontitis, are discussed in detail in Chapter 11. Periodontal ligament The periodontal ligament is a specialised fibrous tissue which attaches the teeth to the alveolar bone and the surrounding gingivae. It acts as a shock absorber to the teeth during chewing, and its main fibres run between the alveolar bone and the cementum covering the root of the tooth. Other fibres run between the necks of the teeth, and from the cementum into the surrounding gingivae. The various periodontal ligament fibre groups and their functions are summarised below, and illustrated in Figure 10.13. • Alveolar crest fibres – run from the alveolar bone crest to the cementum at the neck of the tooth; prevent tooth movements in (intrusion) and out (extrusion) of the socket, as well as resisting tilting and rotation. • Horizontal fibres – run horizontally from the alveolar bone to the cementum, just below the crest fibres; resist tilting and rotation of the tooth. • Oblique fibres – run at an angle from the alveolar bone down to the cementum; prevent intrusion and rotation of the tooth. • Apical fibres – occur at the root apex and run between the bone and cementum; prevent extrusion and rotation of the tooth. Transeptal fibres Free gingival fibres 269 Alveolar crest fibres Horizontal fibres Oblique fibres Apical fibres Figure 10.13 Fibre groups of the periodontal ligament. • Transeptal fibres – run between the cementum of adjacent teeth through the interdental region; maintain the gingival attachments between the teeth and therefore their positions in the dental arch. • Free gingival fibres – run from the cervical cementum into the gingival papillae; maintain the gingival cuff around each tooth. The properties of the periodontal ligament are as follows. • Its fibres are made up of a protein called collagen. • They run in various directions, the end result being that the teeth are held in their sockets but can ‘bounce’ under normal chewing forces. • • This prevents tooth fracture and pain during normal occlusal loading and chewing actions. • The ligament has a sensory nerve supply which transmits pressure, pain, touch and temperature changes; the ability of the tooth to detect and transmit these sensations is called proprioception. • Inflammation of the ligament is called periodontitis and occurs during periodontal disease. When excessive occlusal forces are applied, the resultant pain experienced by the patient tends to stop further overuse from occurring. Salivary glands The salivary glands are present in the oral cavity as either numerous minor glands dotted throughout the lining membrane of the oral mucosa, or as one of the three pairs of major salivary glands (Figure 10.14). • Parotid salivary glands – located between the ramus of the mandible and the ear, and deep to the muscles in that area. • Submandibular salivary glands – located in the posterior area of the floor of the mouth, beneath the mylohyoid muscle. • Sublingual salivary glands – located in the anterior area of the floor of the mouth, above the mylohyoid muscle. 270 of mouth Figure 10.14 Floor of the mouth (cross-section). The function of all the salivary glands is to produce the secretion saliva, which is deposited from the glands into the oral cavity only – it occurs nowhere else in the body. The saliva is transported to the oral cavity through tube-like structures called ducts, so the salivary glands are classed as exocrine glands. Other structures elsewhere in the body are classed as endocrine glands – their secretions pass directly into the adjacent blood vessels (without travelling through ducts) and are transported by the circulatory system to their area of action. Examples are certain glands within the pancreas, the stomach, the liver and the adrenal glands that lie over the kidneys. Both types of glands have their secretions controlled by the effects of motor nerve transmission, via the autonomic nervous system. Parotid gland The parotid gland lies partly over the outside and partly behind the ramus of the mandible, in front of the ear. It is the largest of the three major salivary glands, and the only one to be affected by the viral infection mumps, which is caused by a paramyxovirus. The tube connecting the gland to the oral cavity, the Stenson duct, passes forwards across the surface of the masseter muscle and then inwards through the cheek to open into the buccal sulcus opposite the upper second molar. The parotid gland is innervated by the glossopharyngeal nerve (ninth cranial nerve) and is the salivary gland most commonly associated with both benign and malignant tumours. Submandibular gland The submandibular gland lies in the posterior region of the floor of the mouth below the mylohyoid line, against the inner and lower surface of the body of the mandible and near the angle. The submandibular duct (Wharton duct) passes forward in the floor of the mouth to open at the midline, beside the lingual frenum. It is the longest of the salivary ducts, and the most likely to become blocked by salivary stones (calculi). The submandibular gland is innervated by the facial nerve (seventh cranial nerve). Sublingual gland The sublingual gland also lies in the floor of the mouth, but above the mylohyoid line and much further forward than the submandibular gland. There are several sublingual ducts, and these open into the floor of the mouth just behind the orifice of the submandibular duct (Figure 10.15). The sublingual gland is also innervated by the facial nerve. Functions of saliva Although saliva appears as a watery fluid in the mouth, it contains many different components which differ between each salivary gland, depending on the main type of secretory cell present. The two types of cell found in the glands are as follows. • Mucous secretory cells – produce a thick, mucus-like secretion which aids lubrication in the oral cavity, and contains minerals and enzymes. • Serous secretory cells – produce a thin, serum-like secretion containing antibodies and electrolytes. The different components present in the secretion are related to the various functions and roles of saliva, as shown in Table 10.6. The seven components of saliva are individually identified in the Hyoglossus Figure 10.15 Salivary glands. Table 10.6 Components of saliva and their functions Component Function or role Minerals – sodium, calcium, potassium, and their electrolytes – such as phosphates Neutralise dietary acids Buffering to maintain stable pH in the oral cavity Also allow mineralisation of plaque to form supragingival calculus Salivary amylase Digestive enzyme that begins starch digestion, before food is swallowed. Also called ptyalin Antibodies Immunoglobulins (especially IgA) present to fight infections, such as periodontal disease Promote wound healing IgA is the most common antibody of the immune system 272 Leucocytes White blood cells, as a defence mechanism against oral infection and disease Mucus From the mucous secretory cells, to aid lubrication and allow speech and swallowing to occur Other enzymes Antibacterial enzymes, to aid in the defence of the oral cavity against disease Promote wound healing Water Carrying agent for other components Aids with lubrication for speech and swallowing Dissolves food particles to allow taste sensation Cleansing action by dislodging food particles from around the teeth first column, while their function(s) are explained in the second column. So, for example, the enzyme salivary amylase is present to allow carbohydrate digestion to begin in the oral cavity, and acts on the food bolus as it is chewed and broken into smaller pieces before being swallowed. Patients with low mineral content, mainly watery saliva tend to develop little calculus but have a higher caries incidence than patients with high mineral content saliva. Those with a high mineral content tend to have thick, stringy saliva and develop calculus more readily, in the absence of adequate oral hygiene. They also tend to have a lower incidence of caries, often despite i nadequate dietary sugar control. The position of the salivary ducts against the upper molars and the lower incisors allows dental calculus to build up easily in these areas, and it can be seen as particularly heavy deposits when patients attend for scaling treatment. Saliva is slightly alkaline, due to its electrolyte components, but maintains the oral cavity at a neutral pH of 7 between meals. When the pH falls below 7 following the intake of food, the mineral content of saliva acts to neutralise the acidic environment produced and raise the pH again. If the pH of the oral cavity falls to the critical level of 5.5, enamel demineralisation will occur. The role of saliva in oral health is discussed in detail in Chapter 11. Disorders of the salivary glands Xerostomia This is the uncomfortable condition of having a constantly dry mouth due to the decreased production of saliva. It is relatively common, and has several causes. • Irradiation – of the head and neck area, usually as radiotherapy treatment for cancer in this area. • Medications – any that affect the nerve supply to the salivary glands to reduce their salivary flow, or that act as a diuretic and stimulate fluid loss, as well as certain drugs such as tricyclic antidepressants which cause dry mouth as a side-effect. • Sjögren’s syndrome – a syndrome that occurs in conjunction with an autoimmune disorder, such as rheumatoid arthritis, where the body’s defence system attacks itself and destroys its own glandular tissues, including the salivary glands and the lacrimal glands in the eye. As all dental professionals know, saliva has many functions in the oral cavity and any reduction in its production will have serious oral consequences. • Increased incidence of dental caries, as the self-cleansing ability is lost. • • • • Increased risk of oral infections, as the defence capability is reduced. Increased risk of oral soft tissue trauma, as the protective mechanism is reduced. Problems with speech, swallowing and chewing, as the lubrication effect is reduced. Poor taste sensation and lack of food enjoyment, as the taste buds cannot function correctly in a dry field. Other than to change the patient’s drug regime where possible, there is little else that can be done to ease this condition. The use of salivary stimulants and artificial saliva sprays may help in some cases, and research is currently ongoing into salivary gland 273 tissue transplant. Dental patients suffering from xerostomia should be advised by the dental team as follows. • • • Frequent recall attendance to monitor for the onset of caries and other oral problems. • • Dietary advice to avoid cariogenic products. Use of artificial saliva sprays or constant sipping of plain water. High standard of oral hygiene, and especially the use of topical fluoride products to strengthen teeth against caries. Avoidance of oral health products containing alcohol, as these tend to worsen the drying effect. Ptyalism Excessive salivation, or ptyalism, is a symptom associated with an underlying disease rather than a disorder in its own right. It can occur due to any of the following disorders. • • • • Periodontal disease. Oral soft tissue injury or trauma, including that caused by sharp-edged dental appliances. Oesophagitis and other conditions causing acid reflux. Disorders affecting the nervous system, including Parkinson’s disease and mercury poisoning. Treatment is focused on the causative disease and the relief of its symptoms, although some drugs may be used to directly reduce the salivary gland secretions. In particular, the drug atropine may be used during oral and maxillofacial surgery to significantly reduce saliva flow and provide a clear, dry operating field for the surgeons.