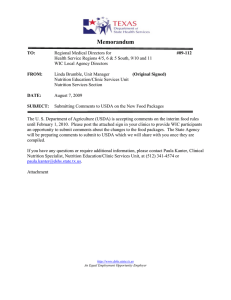
549770 research-article2014 PENXXX10.1177/0148607114549770Journal of Parenteral and Enteral Nutrition X(X)Philipson et al Tutorial Tutorial on Health Economics and Outcomes Research in Nutrition Journal of Parenteral and Enteral Nutrition Volume 38 Supplement 2 November 2014 5S­–16S © 2014 Abbott Nutrition DOI: 10.1177/0148607114549770 jpen.sagepub.com hosted at online.sagepub.com Tomas Philipson, PhD1; Mark T. Linthicum, MPP2; and Julia Thornton Snider, PhD2 Abstract As healthcare costs climb around the world, public and private payers alike are demanding evidence of a treatment’s value to support approval and reimbursement decisions. Health economics and outcomes research, or HEOR, offers tools to answer questions about a treatment’s value, as well as its real-world effects and cost-effectiveness. Given that nutrition interventions have to compete for space in budgets along with biopharmaceutical products and devices, nutrition is now increasingly coming to be evaluated through HEOR. This tutorial introduces the discipline of HEOR and motivates its relevance for nutrition. We first define HEOR and explain its role and relevance in relation to randomized controlled trials. Common HEOR study types—including burden of illness, effectiveness studies, cost-effectiveness analysis, and valuation studies—are presented, with applications to nutrition. Tips for critically reading HEOR studies are provided, along with suggestions on how to use HEOR to improve patient care. Directions for future research are discussed. (JPEN J Parenter Enteral Nutr. 2014;38(suppl 2):5S-16S) Keywords nutrition; health economics; outcomes research; burden of illness; efficacy; effectiveness; cost effectiveness; cost utility analysis; value; oral nutrition supplement; enteral nutrition Clinical Relevancy Statement As nutrition interventions are increasingly coming to be evaluated through health economics and outcomes research (HEOR), clinicians working in the nutrition space can benefit from developing an understanding of HEOR study types and concepts. Such an understanding will enable clinicians to evaluate new evidence generated in nutrition using HEOR methods. Understanding HEOR studies is particularly important given that some outcomes, such as real-world effectiveness and cost impacts of interventions, are difficult or even impossible to study using randomized controlled trials. Understanding a broader array of relevant study types will give clinicians the flexibility to gather and evaluate the most appropriate evidence in their efforts to improve patient care. Introduction Healthcare costs are high and rising, both in the United States and globally. Given the budgetary pressures this cost growth imposes, public and private payers alike have become increasingly focused on value in healthcare. For a product or intervention to represent a good value, it should not only be efficacious but also be worth the scarce resources that were given up to purchase it. But what does it mean for an intervention to be worth its cost, and how is this calculation determined? Answering questions such as these falls within the domain of health economics and outcomes research, or HEOR. HEOR has traditionally been used in the study of medical products (ie, biopharma and devices); however, as cost pressures have extended to all aspects of healthcare, HEOR has become increasingly relevant to nutrition. Over the past century, numerous government bodies across the globe have come to require health technology assessment (HTA) for consideration during their approval and reimbursement decisions. As nutrition products and interventions must compete for space in healthcare budgets along with pharmaceuticals and devices, nutrition is also coming to be evaluated through HEOR. In fact, HEOR may prove to be particularly useful in nutrition, given its low cost relative to its substantial health benefits, making it compare favorably with other interventions in comparative effectiveness From the 1Irving B. Harris School of Public Policy Studies, The University of Chicago, Chicago, Illinois, and 2Precision Health Economics, Los Angeles, California. Financial disclosure: Financial support for the publication of the supplement in which this article appears was provided by Abbott Nutrition. Conflicts of interest: T.P. holds the position of partner at Precision Health Economics. This contribution was prepared by T.P., M.T.L., and J.T.S. at the request of and within the scope of their employment with Precision Health Economics, which received support from Abbott Nutrition to conduct the research appearing in this article, and as such copyright is owned by Abbott Nutrition. Received for publication June 24, 2014; accepted for publication August 8, 2014. Corresponding Author: Julia Thornton Snider, PhD, Precision Health Economics, 11100 Santa Monica Blvd, Suite 500, Los Angeles, CA 90026, USA. Email: [email protected] Downloaded from pen.sagepub.com by guest on March 5, 2015 6S Journal of Parenteral and Enteral Nutrition 38(Suppl 2) Table 1. Comparison of Randomized Controlled Trials (RCTs) and Observational Studies. Characteristic RCT Observational Study Perspective Prospective—the study is designed and the data are then collected to measure the study outcomes Risk of selection bias Low—controlled by restrictive exclusion criteria, more complete data collection and observation, and randomization Usually small due to cost and practical considerations Relatively high Usually finely measured clinical end points such as change in lean body mass or hand grip strength Artificially high Generally short because of cost and difficulty keeping participants in studies long term Limited due to narrow study populations and artificially regulated behaviors Usually retrospective—the study relies on preexisting data sources (such as health insurance claims) to study relationships between treatments and outcomes that have already occurred Moderate—heterogeneous population, with nonrandomized assignment to treatment, but numerous tools exist to control for bias Potentially huge Sample size Research cost Outcomes of interest Adherence Follow-up periods Generalizability research (CER). As such, using HEOR methods may support building an evidence base on the exceptional value of nutrition. HEOR can be based on both trial data and analysis of interventions as they are used by patients in the real world, where patients are more diverse and usually less adherent than in the randomized controlled trial (RCT) setting. It can be used to determine how patients’ everyday decisions reveal the value they place on their health and nutrition status. And it can be used to determine how to allocate a fixed budget on nutrition interventions and other healthcare to maximize patient health and satisfaction. Given the growing importance of HEOR for nutrition interventions, this tutorial has 2 basic objectives: 1. 2. To familiarize the reader with the premise and basic concepts of HEOR To demonstrate the value and usefulness of HEOR for clinicians and researchers working in nutrition To achieve these objectives, the tutorial will proceed as follows. First, it will define HEOR and explain how it adds value in a world where we already have RCTs. Second, it will provide the reader examples of the types of questions HEOR can help us answer. Finally, it will offer practical advice for reading HEOR studies, suggest directions for future research, and present examples of using nutrition HEOR to advance patient care. After reading this tutorial, readers should have a better understanding of the nutrition HEOR literature and HEOR concepts they come across in their daily work, and they should be able to use HEOR to improve their research or practice and, ultimately, patient outcomes. Relatively low Clinical end points, economic outcomes, costs, readmission risk, etc Reflects real-world adherence Potentially long due to nature of data sets (eg, Medicare data includes all claims for a patient over many years) More generalizable because study populations and behavior reflect real-world heterogeneity and decision making What Is HEOR and How Is It Relevant to Nutrition? HEOR Definition HEOR is a discipline used to determine the health effects of interventions, to evaluate those interventions relative to their full cost, and, based on that evaluation, to allocate scarce resources to achieve a particular objective. HEOR serves as a complement to clinical research. While clinical research focuses on issues such as efficacy and safety, HEOR addresses the overall benefits and costs of an intervention, including effectiveness, real-world adherence, complications, and direct and indirect costs. Relation to RCTs While HEOR can be applied to both experimental and observational data, it offers a variety of tools for analyzing observational data that make it particularly well suited for that purpose. HEOR studies using observational data are useful because RCTs, while deservedly central to modern medicine, have important limitations that observational studies can address. These limitations generally stem from the need to enroll and retain patients in the RCT and manage the costs of doing so. In particular, RCTs generally have small, narrowly selected patient populations; artificially low pricing; artificially high adherence; and short duration of follow-up (see Table 1). RCTs are especially useful for providing fine-tuned and precise estimates of the effect of a given intervention, in a specific setting, with all else being held constant. RCTs are critical to improving practice because they allow us to see the effect of Downloaded from pen.sagepub.com by guest on March 5, 2015 Philipson et al 7S an intervention without the “noise” of the real world. For this reason, RCTs are generally considered the “gold standard” for testing the effects of interventions. Once this effect is understood, however, these findings must inform decisions and treatment in the real world. At this point, other important issues arise, such as the impact on costs in real-world settings, the effect of adherence on the value of the intervention, or the long-term cost reductions from, for example, reduced clinical complications. Because of the need to recruit a relatively homogeneous sample, RCTs tend to provide us evidence of effect on specific subgroups of the population, making it difficult to generalize results to the broader population. This is compounded by the fact that, due to necessary exclusion criteria, difficulty in recruiting to trials, and the high cost of intensive data collection and adherence monitoring, trial sample sizes tend to be small. For example, a recent systematic review of studies examining the use of oral nutrition supplements (ONS) in patients with chronic obstructive pulmonary disease (COPD) included 17 RCTs in its analyses—with a combined total of 632 participants, a sample size much smaller than the thousands or millions of observations often available in observational data.1 In addition, trial researchers follow participants closely, ensuring adherence to treatment in the arm to which they are randomized, but there is considerable evidence that real-world adherence to treatment is far from perfect.2-4 In the field of nutrition, researchers interested in designing and conducting RCTs face unique challenges.5 Compared with a pharmaceutical treatment, adherence may be lower with nutrition interventions, requiring more intensive monitoring by researchers. In addition, sample sizes may need to be larger than in pharmaceutical trials because of concerns about adherence and trial retention. The timeframe for measuring nutrition benefits is also long, raising issues with participant retention over time and increasing costs. Furthermore, findings are affected by the general food consumption of participants, which may increase or decrease the effectiveness of a nutrition intervention. It may be complicated to hold all participants to a uniform diet, and maintaining records of all food consumed may affect study participants’ eating habits, making it difficult to control for diet. For example, 1 randomized study illustrated that the act of recording patients’ nutrition intake in the control arm possibly biased “routine practice” as patients and physicians had a heightened focus of their diets.6 Similarly, the lifestyle and activity level of participants is likely to have a significant impact on outcomes. HEOR can complement RCTs by providing tools with which to study outcomes in observational data, thereby enabling the study of potentially enormous populations, with real-world pricing and adherence, and potentially much longer follow-up than is typical of RCTs. Such studies are generally retrospective and do not allow researchers the ability to randomize patients into treatment and control groups, thereby introducing the risk of selection bias. Specifically, in the real world, whether someone receives a given treatment, as well as his or her response to that treatment, is likely to be influenced by underlying health, economic, social, or demographic factors that may not be observable in the data available to researchers. Because treatment is not random, the effect of treatment may be biased by these factors. HEOR has its roots in economics, a field in which RCT data have generally been unavailable. (For example, it would be impractical and unethical to randomly assign half of the country to experience a recession.) In economics and in the separate but related field of outcomes research, techniques have been developed to analyze observational data to be able to infer cause and effect, even in the absence of randomization. Many have argued that, due to selection bias, observational studies may systematically find larger effects than RCTs, but this criticism has not been borne out by analyses comparing effect sizes.7,8 Another potential limitation of observational studies is the fact that they often take a retrospective perspective, in the sense that they analyze data that already exist at the initiation of the study and were not set up explicitly for the purpose of the study (eg, health insurance claims data). Because the data are preexisting, their collection has not been designed to minimize confounders—hence the need for econometric or statistical techniques to address selection bias. Because both RCTs and observational studies have limitations, they should be viewed as complements rather than substitutes, as each offers a unique and useful vantage point on the advantages and disadvantages of a given treatment. HEOR methods for identifying treatment effects in observational data are discussed in detail below. Questions in Nutrition That HEOR Can Help to Answer Ultimately, HEOR seeks to inform decision making—from the decisions of individual providers to those of hospital administrators, policy makers, and patients. HEOR encompasses a variety of types of studies that can be used to answer questions of relevance to nutrition. For example, what burden does malnutrition impose? Which interventions have been shown effective to alleviate malnutrition in the real-world setting? Which interventions are the most cost-effective? And how do patients reveal their preferences for health and life through their own everyday decisions? The next section presents common types of HEOR studies, with applications to nutrition as available. What Is the Burden on Society From Nutrition Diseases? Diseases cost human life, health, and happiness. Disease not only affects the health of individuals but also has an impact on society. But how does one measure the collective damage imposed by a disease, and could it be compared with the “burden” imposed by other diseases or social ills? How do policy Downloaded from pen.sagepub.com by guest on March 5, 2015 8S Journal of Parenteral and Enteral Nutrition 38(Suppl 2) makers, researchers, or society in general know which diseases to prioritize? How much does malnutrition increase the existing burden of other diseases? These are the types of questions that “burden of illness” studies help to answer. By better understanding the overall economic, or social, burden of a disease, we may better identify important areas for research and investment of resources. The impacts of disease are complex and multifaceted, though, requiring methods for identifying—and differentiating—these components without “double counting.” The greatest costs from illness result from losses in the quantity and quality of life. Through increased morbidity and mortality, disease shortens the life expectancies of many of the ill and decreases the quality of life lived with disease. Disease also causes direct medical costs from treatment. In addition, disease has impacts on employment and productivity, burden on caregivers, and other socioeconomic effects. Clearly, an accurate estimate of all of these societal costs from disease is ambitious at best, but even a partial estimate is often instructive. Malnutrition may be due to socioeconomic forces as well as disease. Historically, applications of burden of illness modeling in the nutrition context have focused on undernutrition in the developing world, especially among children and women of childbearing age.9 For example, the World Health Organization (WHO) conducted a study in 2005 to estimate the burden of malnutrition in children younger than 5 years. The report outlines the WHO estimation process for calculating the economic consequences of malnutrition and provides a numerical example using Nepalese children as a sample population.10 In this case, the burden is expressed not in monetary terms but in terms of disability-adjusted life years (DALYs) lost to malnutrition. As discussed below, DALYs—or, alternatively, quality-adjusted life years (QALYs)—are a common measure of disease impact that incorporates both morbidity and mortality. To compare the burden of a disease with the costs of its treatment, however, it is important to understand how society values the losses from disease. Losses due to morbidity and mortality can also be expressed in monetary terms, which allow for an aggregated estimate of burden that also includes direct medical costs, lost productivity, and other impacts of disease. Approaches to understanding how to value losses in quality or quantity of life are discussed in a later section; examples of the application of such valuation are provided here. Inotai et al5 developed such an economic model to estimate the total economic burden of disease-associated malnutrition (DAM) associated with 10 primary diseases in Europe. To do so, the authors broke the economic burden of the diseases into 3 components—acute phase, chronic phase, and premature mortality due to malnutrition—and they included model parameters such as increased length of stay, medical nutrition costs, caregiver burden, and health loss, as well as epidemiological factors such as disease incidence and malnutrition prevalence. The authors estimated the burden of DAM in Europe to be €305 billion annually. In this issue of Journal of Parenteral and Enteral Nutrition, Snider et al11 present a similar analysis of the burden of DAM in the community setting in the United States, using nationally representative data on the prevalence of diagnosed and undiagnosed disease to estimate disease and disease-specific malnutrition incidence using real-world data. The authors find that DAM in the included diseases imposes a burden of $156.7 billion per year in the United States. A common criticism of burden of illness studies is that they invariably find that a given disease imposes a large economic burden on society but that these analyses do not consider the cost of reducing this burden or the effectiveness of available treatments. Both of these dimensions are discussed below. It is worth noting, however, that strong evidence exists to suggest that interventions and treatments for malnutrition can be both low cost and highly effective, making the message of such studies more compelling and more important for motivating public concern about the issue. What Is the Effectiveness of a Nutrition Intervention, and How Does It Compare With Its Efficacy? Knowing that a disease, such as malnutrition, imposes a large burden on society is only useful if there is something that can be done about it. One thing that can be done is to conduct research to discover tools to reduce the burden. Understanding the relative burden from different diseases—and therefore the urgency of treating them—helps to inform the allocation of resources for research and treatment development. Once those tools exist, though, how does one determine whether they successfully treat the targeted disease? In other words, how does one know whether the tools are efficacious (ie, achieving the desired treatment effect in a controlled setting) and effective (ie, achieving the desired treatment effect in a real-world setting)? Efficacy measures the performance of an intervention under ideal and controlled circumstances12; it is determined through RCTs. In RCTs, as discussed above, the decision of whether to treat a particular patient is made through the randomization of patients into treatment and control arms. After randomization, differences in underlying patient health status and other personal characteristics should be small, enabling the identification of the treatment effect. In addition, RCTs eliminate other factors present in real-world settings that could potentially affect the perceived effect of a treatment, including patient access, provider prescribing behaviors, and adherence.12 In contrast, effectiveness measures the performance of an intervention under “real-world” conditions. These studies may be more applicable to predicting expected outcomes for realworld patients. For example, patients may be compared with standard of care rather than a placebo arm, which is a typical approach in RCTs. Limitations of effectiveness studies stem from the fact that the real world is not as controlled or homogeneous as the environment of an RCT. The introduction of Downloaded from pen.sagepub.com by guest on March 5, 2015 Philipson et al 9S endogenous factors in the real world that are not present in RCTs could bias the final effectiveness estimate.12 Numerous trials of efficacy in nutrition have been conducted; however, the nature of nutrition poses some unique challenges for researchers seeking to design and conduct RCTs. Because nutrition is a fundamental requirement of everyday life, the ethics of providing a placebo are not straightforward. Moreover, because nutrition—unlike, say, drugs or devices—is readily available in various forms, adherence can be harder to measure and maintain. Finally, because of the nature of the treatment, nutrition trials are often not blinded. In a recent review of reviews of nutrition efficacy trials, Stratton and Elia13 discussed these issues and commented on the practical difficulties and ethical issues that limit the ability of nutrition trials to score highly on metrics developed to measure RCT quality for pharmaceuticals. Of course, methodological challenges are not limited to efficacy studies. The potential for endogenous factors to bias an analysis of effectiveness in a real-world setting is considerable. Fortunately, the various disciplines that form the basis for HEOR offer a variety of tools for addressing selection bias. With a careful study design, researchers can often control for selection bias and measure effectiveness in the real-world setting. We illustrate these tools using an example in nutrition: a study by Philipson et al14 on the impact of oral nutrition supplements (ONS). Philipson and coauthors14 sought to identify the effect of providing ONS to patients in the hospital. To do this, the authors had to grapple with the issue that, far from being provided at random, ONS was generally given to patients who were considerably older and less healthy than the average hospital patient. That is, the decision of whom to provide ONS was subject to strong selection bias. The authors employed 2 techniques to address this bias. The first technique used by Philipson et al14 was propensity score matching. Propensity score matching addresses the issue of unbalanced covariates across treatment and control groups in observational studies or, in the case of this example, the fact that the ONS users were older and less healthy on observed dimensions. It is particularly useful when the number of influential covariates is great enough that matching on individuals covariates (eg, age and sex) would be impractical.15 If the relevant differences between treated and untreated individuals are observed, propensity score matching can be employed to obtain unbiased estimates of the effect of treatment.16,17 Propensity score matching is most commonly performed by estimating a logistic regression model of the likelihood that a given individual receives the treatment, as a function of observable characteristics. This regression produces an estimated probability that each individual in the sample would be given the treatment. After these estimated probabilities are obtained, each treated individual is matched to one or more untreated individuals who had a similar estimated probability of receiving the treatment. In the Philipson et al14 example, propensity score matching was used to match each episode in which the patient received ONS to an episode in which the patient appeared equally likely to receive ONS (due to similar age, sex, comorbidities, etc) but in fact did not receive ONS. In this way, the treatment and control groups were made more comparable. Another example of propensity score matching can be found in this special issue in the article by Hamdy et al.18 This study examines the effects of providing glycemia-targeted specialized nutrition (GTSN) to patients with diabetes. By using propensity score matching, Hamdy et al were able to restrict the sample of hospitalized patients with diabetes to those who appeared similarly likely to receive GTSN. This process served to render the treatment and control groups more comparable. If propensity score matching is to be used to estimate the causal effect of a treatment, the researchers must be confident that all the relevant difference between treated and controlled individuals can be observed. However, even after matching treatment and control cases to account for observable differences, crucial unobservable differences may remain, with the potential to confound the analysis.19 Returning to the Philipson et al14 ONS example, imagine 2 patients who are identical along observable dimensions—same age, race, comorbidities, history of prior hospitalization, and so on. A clinician who walks into these patients’ rooms to evaluate and plan their respective courses of treatment is likely to perceive 2 very different patients, despite their similarity in the data. It is reasonable to expect that the clinician’s decision of whether to provide ONS would be related to the patients’ individual needs, and therefore, the patients’ clinical outcomes would result from both their underlying health status and whether they received ONS. How, then, can we separate these underlying variables from the effect of treatment to determine treatment effectiveness? HEOR offers several techniques to address bias from unobserved factors. We discuss here a technique called instrumental variables (IV) analysis, which was employed in the Philipson et al14 study. Other common techniques include difference-indifference and regression discontinuity design; sources on these methods are provided in the Further Reading section at the end of this tutorial. IV analysis essentially serves as a quasi-randomization device to sort individuals into treatment and controls groups with similar observed and unobserved characteristics. It is useful when unobserved characteristics are influential in the treatment decision, and significant heterogeneity in unobserved characteristics is present even among those who are similar on observed dimensions. Returning to the Philipson et al14 ONS example, consider 2 patients who are both 71-year-old women with comorbid chronic obstructive pulmonary disease (COPD), one with a body mass index (BMI) of 24 and the other with a BMI of 16. If we observed only their age, sex, and comorbid COPD, we would not know the reason why one received ONS and the other did not (due to unobserved underweight). If we were to estimate the effects of the intervention without taking Downloaded from pen.sagepub.com by guest on March 5, 2015 10S Journal of Parenteral and Enteral Nutrition 38(Suppl 2) Table 2. Types of Cost Analyses. Study Type Definition Cost-effectiveness analysis (CEA) An economic analysis that compares the costs and outcomes of 2 alternative interventions. Cost-benefit analysis (CBA) An economic analysis that compares the costs of an intervention with its benefits, both expressed in monetary terms. CBA can also be used to compare 2 alternative interventions. Approach to Benefits Example Benefits of intervention could be infections averted, qualityadjusted life years (QALYs) gained, and life years saved. Benefits converted to monetary values. The result of a nutrition screening program, in terms of its cost and life years saved, is compared with the standard of care. The result of a nutrition screening program is quantified in terms of monetized benefits and costs, as well as compared with the monetized benefits and costs of the standard of care. this unobserved heterogeneity (the difference in BMI) into account, we may even come to the erroneous conclusion that providing ONS caused poorer health outcomes, when in fact the intervention was given to the woman who faced a worse prognosis (due to her low BMI) in the first place. Indeed, naive regression analysis on this sample suggested that ONS was causing patients to have longer hospital stays, more expensive episodes, and a higher risk of being readmitted. To remove confounding in such a situation, an instrument must be found that predicts treatment but otherwise does not affect outcomes except through its influence on the treatment. In this case, the authors used hospitals’ propensity to provide ONS as an instrument. Because some hospitals were more likely to offer ONS to any given patient, regardless of the patient’s characteristics, while others were less likely, this variable essentially simulates a randomization into ONS and non-ONS treatment groups. To check the validity of the approach, the authors tested the 2 requirements of a valid instrument: that it predicts the treatment but otherwise does not influence outcomes except through its influence on the treatment. Specifically, they confirmed that (1) hospital-level ONS usage rates were a strong predictor of the individual patient’s ONS use, and (2) hospitals with high ONS rates did not have (observably) healthier patients or better technology than did hospitals with low ONS rates. Numerous other researchers have used the IV approach to measure the effects of interventions. In this issue, Lakdawalla et al20 employ a similar approach to evaluate the effectiveness of ONS in pediatric patients. Outside of the nutrition space, IV has been successfully employed to create natural experiments in a wide range of contexts, including the estimation of supply and demand,21 determining the effect of police force size on crime,22 and calculating the effect of veteran status in the Vietnam era on mortality.23 How Should Resources Be Directed to Optimally Reduce Burden of Illness by Improving Nutrition? The previous subsection discussed how to gauge whether a given intervention works, whether in the highly controlled environment of an RCT (“efficacy”) or in the real world (“effectiveness”). From a patient’s perspective, this may be all the information needed to make treatment decisions—if a more effective treatment exists, that is the treatment a patient would be expected to want. However, from the broader perspective of society or health systems, decision makers must determine how to allocate limited resources to do the most good with a given budget. To do this, some measure of the “good” an intervention produces must be weighed against its cost. This is the domain of cost-effectiveness analysis (CEA) and its closely related cousin, cost-benefit analysis (CBA). Both of these study types are economic analyses that facilitate an assessment of the result of an intervention compared with an alternative intervention. The types differ in terms of how the results of the intervention are measured, as shown in Table 2. Both types of studies take into account the costs of an intervention; however, they differ in how they measure the benefits. Costs should be equal to the value of the opportunity cost had the resources been used elsewhere.24 For example, when an individual visits the doctor’s office, the full cost of the treatment includes not only the cost paid for the visit (both by any insurance and out-of-pocket), but also the cost of transportation from the individual’s home or workplace to the doctor’s office, as well as the missed wages or home production that individual did not earn because of the visit to the doctor’s office. An intervention that improves an individual’s health may not only reduce doctor’s visits and other healthcare utilization but also improve the individual’s productivity and reduce caregiver burden. In practice, however, such “indirect” costs of illness—those apart from the “direct” healthcare costs—are difficult to measure and are therefore often left out of CEA studies. In CEA, benefits are measured in terms of health outcomes, such as life years, QALYs, or DALYs saved, or cases of disease averted.25 In contrast, in CBA, both benefits and costs are expressed in monetary terms, which makes it possible to incorporate diverse types of costs and benefits into a single calculation of net benefit.26 Both CBA and CEA can be used to facilitate policy making,27 whether in the public or the private sector. For health-related questions, CEA is often preferred to Downloaded from pen.sagepub.com by guest on March 5, 2015 Philipson et al 11S CBA because in CEA, the outcome of the intervention (eg, QALYs saved or cases of disease averted) is transparent and can be easily compared across studies.25,26,28 Unlike other types of health interventions, however, nutrition affects every organ of the body. Therefore, measuring the benefits of nutrition along a single dimension can be difficult. For this reason, CBA is often a more appropriate approach. This difficulty is compounded by the fact that, relative to the potential benefits, the cost of nutrition interventions, especially in the clinical context, tends to be low. As a result, traditional CEA is difficult to conduct, leading to CEA studies that focus on cost savings, rather than cost per change in health outcomes. (Typically, CEA studies report the cost required to attain a given incremental change in a health outcome [eg, $57,600 per life year]. Nutrition interventions often reduce costs while improving health outcomes. In CEA, such interventions are called cost saving, and a cost per unit of incremental change in health is not reported.) Below, we discuss the use of CEA and CBA in nutrition, highlighting a number of examples from the nutrition literature. Cost-effectiveness analysis in nutrition. As discussed above, many of the CEA studies in nutrition focus on cost savings rather than health outcomes. For example, Doig et al29 present a cost impact comparison of early (within 24 hours of admission to the intensive care unit [ICU]) administration of enteral nutrition (EN) with the provision of EN at any point after 24 hours. The authors use a computer simulation, built based on evidence from the literature, to model the effects of early vs later EN, using various measures of resource consumption (ICU length of stay, duration of intubation, and hospital length of stay) as an estimate of costs. The study found that early EN resulted in $14,462 in cost savings per patient (95% confidence interval [CI], US$5464–$23,669). Modified CEA studies have also focused on oral nutrition supplementation. One such analysis was performed on a patient population in the Netherlands undergoing abdominal surgery. The study demonstrated that ONS resulted in a 7.6% cost savings per patient. The 0.72-day reduction in length of stay was a driver of the cost savings (8.3% cost savings per patient) and was sufficient to cancel out the added costs of the ONS therapy. Therefore, they were able to conclude that ONS is indeed a cost-effective (indeed, cost-saving) treatment as opposed to standard care without the nutrition supplement.30 In another case, a budget impact analysis was conducted on an elderly patient population in the Netherlands to assess whether adding the expense of ONS to the nation’s healthcare budget was costeffective. The study affirmed that the use of ONS to treat disease-related malnutrition (DRM) leads to cost-savings, resulting in €13 million in savings per year (a 4.7% reduction). The additional costs were offset by the reduction in readmission.31 Standardized and consistent reporting across CEA studies is essential if CEAs are to be used to inform decision making.32 This is a major motivation for the development of cost utility analysis (CUA), a type of CEA in which the outcome of an intervention is measured in terms of years of life lived in perfect health (QALYs).33,34 QALYs weight life years by the health-related quality of life experienced, which can be determined using any of several validated methods of health state measurement.24,33 This standardized use of QALYs has the effect of making studies more comparable.24 Studies can also be more easily compared when they take a common perspective (eg, societal) and a common definition of costs (eg, only “direct” costs).24 For example, a cost-utility analysis was performed to compare enteral tube feeding (ETF) in patients with cerebrovascular accident (CVA) in 2 separate locations (home vs nursing home). Using patient data from insurance charges and adopting a payer perspective, the study demonstrated that the cost-effectiveness ratio (cost/QALY) of patients receiving long-term ETF in their own home (£12,817 per QALY) compares favorably with other interventions.35 Cost-benefit analysis in nutrition. Although CEA and CUA are often preferred for comparison of health interventions, CBA is also a valuable tool. CBA assigns a monetary value to all costs and benefits—a difficult and often contentious process. However, stating all costs and benefits in monetary terms allows decision makers to compare interventions or policies that have multiple costs and benefits. Approaches for assigning value to nonmonetary costs and benefits are discussed in the next subsection. CBA is particularly useful in circumstances where the benefits of an intervention are not easily measured along a single dimension—in a program that not only affects the health of individuals but also has economic benefits for a neighborhood, for example, or where improved health outcomes themselves lead to further reductions in medical costs or increased economic productivity. Given the array of potential benefits from improved nutrition, use of CBA in nutrition is often a natural fit. CBA may better convey the full value of nutrition interventions, as well, because it strives to capture all costs and benefits. In fact, the Copenhagen Consensus has repeatedly considered programs designed to reduce hunger and malnutrition to be among the most promising in terms of the ratio of benefits to costs.9,36-38 For example, a CBA of the Expanded Food and Nutrition Education Program in Virginia compared the costs of the program with the benefit of prevented or delayed costs from chronic diseases. Benefits and costs accrue over time; a delay of disease onset for 10 years leads to 10 years of benefits, discounted over time. Comparing total benefits with total costs, the authors found a benefit/cost ratio of $10.64/$1.00.39 Facilitating decision making: the incremental cost effectiveness ratio, or ICER. To decide whether a new intervention is worth initiating in the place of an old one, CEA can be used to produce a valuable tool, the incremental cost-effectiveness Downloaded from pen.sagepub.com by guest on March 5, 2015 12S Journal of Parenteral and Enteral Nutrition 38(Suppl 2) A new nutrional regimen (regimen “A”) is introduced, which has been shown to improve survival in a nutrionally at-risk populaon, relave to the standard of care (regimen “B”). Cost: $10,000 Cost: $20,000 Life expectancy: 1.5 years Cost: $10,000 Life expectancy: 0.5 years 1.5 years year Life expectancy: 1.0 years $10,000 0.5 years per life year Is $20,000 per life year “worth it”? Figure 1. Hypothetical example of an incremental cost-effectiveness ratio (ICER) calculation. ratio (ICER). An ICER is used to compare the cost to attain a fixed amount of health benefits under one intervention, relative to another intervention.24 The formula, illustrated in Figure 1, is as follows: ICER = Cost A − Cost B . Effect A − Effect B Policy makers and other decision makers often compare the performance of interventions in relation to a given ICER threshold. Internationally, use of a threshold of €50,000/QALY is widely accepted as standard practice in CEA. For example, a health economic analysis of a population of 114 malnourished patients showed that a 3-month nutrition intervention with ONS was cost-effective when its results were compared with the international ICER benchmark of €50,000/QALY. Two different pricing scenarios for ONS—a minimum and maximum— were used and the study confirmed that intervention with ONS increases the quality of life in malnourished patients.40 Limitations of cost-effectiveness analysis. While CEA is a useful tool for healthcare decision making, it does have limitations.25 For example, indirect costs, such as foregone wages and caregiver burden, can be substantial, but they are difficult to measure and hence frequently excluded from CEA. Disagreement exists over the proper way to measure health outcomes; for example, there is not yet a consensus on whether to age-adjust QALYs to account for different utilities experienced across stages of life. Moreover, even if indirect costs are obtained and agreement is reached on how to measure health outcomes, there remains the question of how much a given health outcome is “worth.” For example, if a given intervention costs $10,000 to extend life by 1 QALY, relative to the standard of care, is this a good value? What if it costs $100,000? Or $1,000,000? Does using an ICER threshold of €50,000/QALY accurately capture the priorities or values of society? While different individuals— and nations—would answer these questions differently, health economists have developed some techniques for producing “objective” answers. How the value of health is determined is the subject of the next section. Is a Given Intervention “Worth It”? How to Determine Value Cost-effectiveness analysis tells us how much it costs to use a particular intervention to extend life by a given amount, but it Downloaded from pen.sagepub.com by guest on March 5, 2015 Philipson et al 13S does not tell us whether it is worth it to pay for the intervention. While there is no one definitive answer on which technologies are worth their cost, HEOR does offer methods that stakeholders can use to make these challenging but important decisions. The value of life extension, or of increasing an individual’s quality of life, depends on one’s perspective. On the individual level, the value of a year of life would seem to be priceless— imagine being told you would lose 1 year of your life unless you paid for the 1 treatment that would preserve it. Without limits on budget, you would likely pay any price. The same holds true for extending life for family, friends, or patients. In reality, however, we do face budget constraints. In addition, society faces decisions about trade-offs between life extension and cost for many millions of individuals; although we wish to preserve the lives of all in society, we must make difficult decisions in allocating resources. For this reason, economists have developed the concept of the value of a statistical life year, or the amount society appears to be willing to spend to extend life by 1 year for an individual whose identity is unknown. After adjusting for health-related quality of life, this concept then provides us with an estimate of the value of a QALY, which can then be used in CEA or burden of illness models. But how should we determine what the value of a QALY should be? Health economists use several approaches to determine the value an individual places on health and survival. The simplest approach is known as the human capital approach. This approach calculates expected lifetime earnings after adjustments based on one’s health status. While this approach captures the effects of disease on productivity, it misses important nuances of valuing one’s remaining life years.41 For example, this suggests that younger people’s lives may be more valuable, because they are expected to live longer, but other valuation methods indicate that older people may value remaining life more.42 Furthermore, many believe that an individual’s value to society is not adequately represented by the amount that he or she earns. Many believe that a better measure of how society values health and life is seen through the trade-offs people are willing to make. Studies of revealed preference use observed behavior to estimate the willingness to assume risk, for example, through the increased pay required for someone to accept a job with greater risk of injury or death. Alternatively, researchers may present subjects with tradeoff decisions that reveal their value of time alive or quality of life. Such survey-based methods are the domain of contingent valuation and conjoint analysis. Researchers ask respondents about their willingness to give up one thing for another (contingent valuation) or rank their preferences for a range of options (conjoint analysis) and then use regression analysis to learn about respondents’ valuations of intangible items such as health and the environment.43 Techniques have been developed to improve accuracy when eliciting such valuations.44 These methods are particularly useful in questions related to health. For example, in studies of time trade-off and standard gambles, researchers ask the subject to sacrifice time or risk of death, respectively, in exchange for perfect health relative to his or her current health state. In addition, this approach is extremely valuable in determining the relative importance of healthrelated quality of life, which is necessary to accurately estimate QALYs and perform cost-utility analysis. How to Use This Tutorial As we approach the end of this tutorial, we would like to offer some guidance on how to use the content presented here. We see 3 potential uses, depending on the aims of the reader. First, for those interested in understanding the existing nutrition HEOR evidence base, we offer tips for reading HEOR studies. Second, for those looking to include HEOR concepts in nutrition research, we identify gaps in the literature and suggest directions for future research. Third, for those making decisions about nutrition care, we provide examples to illustrate how clinicians, providers, and payers can use HEOR in nutrition to improve patient outcomes. Tips for Reading HEOR Studies When reading an HEOR study, the key questions to ask are the following: 1. Are there important differences between treated and untreated individuals? Or in other words, is the decision to treat some individuals and not others subject to selection bias? Given that HEOR usually relies on observational data, the answer to question 1 will usually be yes. In this case, the reader should proceed to question 2. 2. If so, how has the selection bias been addressed? There are numerous techniques for addressing selection bias in HEOR studies, as discussed above. Regardless of the technique, assessing the validity of the study essentially comes down to carefully considering whether the analyzed treatment and control groups are really comparable. For example, if the treatment is providing ONS, one might ask whether the researchers accounted for the fact that individuals receiving ONS may be older and have more comorbidities than those not receiving ONS. Suppose that the answer is yes, and those differences were controlled for. In that case, the reader might ask whether more subtle differences such as different BMI or laboratory values (indicating malnutrition) were controlled for. Suppose the answer is no. In this case, the study approach may still be valid if an appropriate technique was performed to account for unobserved differences. In that case, not only should an appropriate technique be used (eg, instrumental variables, regression discontinuity design, difference-in-difference), but the authors should also make a reasonable case for its validity. Downloaded from pen.sagepub.com by guest on March 5, 2015 14S Journal of Parenteral and Enteral Nutrition 38(Suppl 2) In practice, many poorly designed observational studies suffer from insufficiently comparable treatment and control groups. Therefore, in asking the above 2 questions, the reader can go a long way toward gauging the quality of the work. Additional reading on specific methods, techniques, and concepts are provided below in a list of suggested further reading. without needing the approval of a physician. The rule is expected to reduce healthcare costs and improve patient outcomes.55 In general, HEOR can be used to complement RCTs to determine the most effective and cost-effective interventions in the real-world setting. As the available evidence base continues to grow, the tools to improve patient care will continue to become more powerful. Directions for Future Research Conclusion As this tutorial has shown, HEOR studies in nutrition have demonstrated the burden of malnutrition, shown the effectiveness and cost-effectiveness of various interventions to improve nutrition status, and offered tools to gauge whether a given intervention is “worth it.” At the same time, gaps exist that future research can help to fill. For example, although numerous studies have measured the effects of nutrition interventions in the acute care setting,14,30,35,40,45-53 analyses focused on the effects of interventions in the community setting are less common. While many studies have shown the health benefits and cost-effectiveness of nutrition support (whether through ONS, EN, or other means), questions remain about which type of nutrition and what timing of nutrition would be best suited to an individual patient’s circumstances. Research is needed to refine measures of the benefits from better nutrition, both to individuals and to society. In addition, an opportunity exists to apply the valuation methods described above—particularly contingent valuation and conjoint analysis—to better understand the impacts of malnutrition on quality of life and how much patients value healthy nutrition status. Finally, due to financial and practical considerations noted above, RCTs in nutrition have often featured small and narrowly selected patient populations, leaving room for well-designed HEOR studies to investigate how the effects found in RCTs may generalize to a larger, more diverse, and likely less adherent real-world patient population. HEOR can help measure the burden of malnutrition, identify the most effective interventions for malnourished or nutritionally atrisk patients, facilitate the comparison of the outcomes achieved through various interventions relative to their costs, and provide a framework for deciding whether a given intervention is “worth it.” Such studies may be particularly useful in nutrition, given that nutrition interventions often come at a modest cost relative to their health benefits. In a world where private and public payers alike increasingly demand evidence to justify a therapy’s effectiveness and value, HEOR provides a tool for demonstrating the value of nutrition as a fundamental pillar of health. Using HEOR to Improve Patient Outcomes HEOR is not solely a tool for researchers; it can also be used to allocate resources to achieve the best health outcomes on a fixed budget, direct patients to the most appropriate treatments given real-world safety and effectiveness, and improve patient quality of life. For example, in the United Kingdom, the National Institute for Health and Clinical Excellence (NICE) surveyed the available evidence to find ONS valuable for malnourished patients. Consequently, NICE issued guidelines recommending the use of ONS by clinicians.54 In the United States, after surveying the evidence, the Centers for Medicare & Medicaid Services (CMS) recently issued a new rule that registered dietitian nutritionists be provided more independence in the hospital. Under this rule, registered dietitian nutritionists will be able to manage patients’ diets and order nutrition-related laboratory tests Acknowledgments The authors thank Nick Summers for research support. Further Reading General Russell CA. The impact of malnutrition on healthcare costs and economic considerations for the use of oral nutritional supplements. Clin Nutr Suppl. 2007;2(1):25-32. Burden of Illness Rice DP. Estimating the cost of illness. Am J Public Health Nations Health. 1967;57(3):424-440. Zhao F-L, Gao L, Li S-C. Burden of disease studies in the Asia-Pacific region: are there enough being performed to provide information for evidencebased health policy? Value Health Region Issues. 2013;2(1):152-159. Efficacy vs Effectiveness Gartlehner G, Hansen RA, Nissman D, Lohr KN, Carey TS. Criteria for Distinguishing Effectiveness From Efficacy Trials in Systematic Reviews. Rockville, MD: Agency for Healthcare Research and Quality; April 2006. Technical Review 12 (AHRQ Publication No. 06-0046). Regression Analysis Overview Wooldridge J.Introductory Econometrics: A Modern Approach. 4th ed. Mason, OH: South-Western Cengage Learning; 2009. Zöphel M, Egger C, Riedi H. A Short Critical, Non-Technical, Non-Mathematical Paper About Regression Analysis. Munich, Germany: GRIN Publishing GmbH; 2008: http://www.grin.com/en/e-book/171083/a-short-criticalnon-technical-non-mathematical-paper-about-regression Instrumental Variables Brookhart MA, Rassen JA, Schneeweiss S. Instrumental variable methods in comparative safety and effectiveness research. Pharmacoepidemiol Drug Saf. 2010;19(6):537-554. Cawley J, Meyerhoefer C. The medical care costs of obesity: an instrumental variables approach. J Health Econ. 2012;31(1):219-230. Martens EP, Pestman WR, de Boer A, Belitser SV, Klungel OH. Instru­mental variables: application and limitations. Epidemiology. 2006;17(3):260-267. Difference-in-Difference Donald SG, Lang K. Inference with difference-in-differences and other panel data. Rev Econ Stat. 2007;89(2):221-233. Downloaded from pen.sagepub.com by guest on March 5, 2015 Philipson et al 15S Grafova IB, Freedman VA, Lurie N, Kumar R, Rogowski J. The difference-indifference method: assessing the selection bias in the effects of neighborhood environment on health. Econ Hum Biol. 2014;13:20-33. Gruber J, Poterba J. Tax incentives and the decision to purchase health insurance: evidence from the self-employed. Q J Econ. 1994;109(3): 701-733. Regression Discontinuity Design Imbens GW, Lemieux T. Regression discontinuity designs: a guide to practice. J Econometrics. 2008;142(2):615-635. Linden A, Adams JL, Roberts N. Evaluating disease management programme effectiveness: an introduction to the regression discontinuity design. J Eval Clin Pract. 2006;12(2):124-131. Thistlethwaite DL, Campbell DT. Regression-discontinuity analysis: an alternative to the ex post facto experiment. J Educ Psychol. 1960;51(6):309. Valuing Life Extensions Hirth RA, Chernew ME, Miller E, Fendrick AM, Weissert WG. Willingness to pay for a quality-adjusted life year: in search of a standard. Med Decis Making. 2000;20(3):332-342. Rosen S. The value of changes in life expectancy. J Risk Uncertainty. 1988;1(3):285-304. Ubel PA, Hirth RA, Chernew ME, Fendrick AM. What is the price of life and why doesn’t it increase at the rate of inflation? Arch Intern Med. 2003;163(14):1637-1641. Glossary Burden of illness study—designed to quantify the overall burden faced by patients diagnosed with a particular disease, often aggregated to a societal level and presented in monetary values. Comprehensive estimates consider both direct costs (eg, cost of treatment, morbidity, mortality) as well as indirect costs (eg, caregiver burden, productivity effects, quality of life). Cost-benefit analysis—economic analysis technique used to compare the costs and benefits of an intervention, where both values are expressed in monetary terms. Cost-effectiveness analysis—economic analysis technique used to compare the relative costs and outcomes of 2 or more alternative interventions. Difference-in-differences—statistical analysis technique used to imitate an experimental design with observational data by calculating a change over time for a given outcome within a treatment group and comparing it with a change over time for the same outcome within a control group. Discounting—financial analysis technique used to adjust monetary estimates to account for the fact that individuals consider $1 in the present time to be more valuable than $1 received in the future. Discounting can also be applied to health outcomes (eg, life years). For example, it would commonly be considered more valuable to save a year of life now rather than to save a year of life 100 years in the future. Effectiveness—measure of how well an intervention performs in a realworld setting. Efficacy—measure of how well an intervention performs in a controlled setting (ie, clinical trial or laboratory setting). Endogenous—economic term used to describe variables included in a statistical model that are correlated with error term. Explanatory variables may be endogenous if they not only affect but are also affected by the outcome (ie, if causality runs in both directions). In health studies, treatment may be endogenous due to selection bias. For example, a nutrition intervention may increase BMI, but it may be given to individuals with low BMI—meaning that causality runs in both directions. If appropriate steps are not taken to address the endogeneity, estimating a model with endogenous explanatory variables will lead to biased estimates of the treatment effect. Exogenous—economic term used to describe variables determined outside of a statistical model. Exogenous variables may influence the outcome of a statistical model, but they are not influenced by it. For example, sunshine is exogenous to crop growth. Sunshine influences crop growth, but crop growth does not influence sunshine. Instrumental variables analysis—statistical analysis technique used to imitate an experimental design with observational data by including an instrumental variable in the model that is correlated with the treatment but does not otherwise influence the study outcome except through its influence on the treatment. Observational study—designed to estimate treatment effects in a real-world setting using data on observed behaviors (eg, insurance claims, hospital records, etc) where the assignment of the intervention is not conducted by the study investigator. There are multiple observational study designs such as cross-sectional studies, longitudinal studies, and case-control studies, among others. Propensity score matching—statistical matching technique used to mitigate the possible bias of real-world treatment selection by identifying a control sample that has similar observed demographics and health characteristics to the treatment sample. Randomized controlled trial (RCT)—designed to estimate treatment efficacy in a controlled setting where the assignment of the intervention and control arms is decided randomly by the study investigator. Regression analysis—statistical analysis technique used to assess the relationship among variables by predicting the effect that changing a given variable has on an outcome of interest, all else equal. Regression discontinuity design—an observational study design that mimics a randomized controlled trial by comparing an outcome of interest among individuals just above and just below a given arbitrary threshold that is used in policy. For example, suppose a hospital provides nutrition support to all individuals with BMI below 18.5. One could study the effect of nutrition support on outcomes by comparing outcomes among individuals with BMI just below and just above the cutoff. References 1. Ferreira IM, Brooks D, White J, Goldstein R. Nutritional supplementation for stable chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2012;12:CD000998. 2. Dunbar-Jacob J, Mortimer-Stephens MK. Treatment adherence in chronic disease. J Clin Epidemiol. 2001;54(suppl 1):S57-S60. 3. Kothawala P, Badamgarav E, Ryu S, Miller RM, Halbert RJ. Systematic review and meta-analysis of real-world adherence to drug therapy for osteoporosis. Mayo Clin Proc. 2007;82(12):1493-1501. 4. Sajatovic M, Valenstein M, Blow FC, Ganoczy D, Ignacio RV. Treatment adherence with antipsychotic medications in bipolar disorder. Bipolar Disord. 2006;8(3):232-241. 5. Inotai A, Nuijten M, Roth E, Hegazi R, Kaló Z. Modelling the burden of disease associated malnutrition. ESPEN J. 2012;7(5):e196-e204. 6. Ha L, Hauge T, Spenning AB, Iversen PO. Individual, nutritional support prevents undernutrition, increases muscle strength and improves QoL among elderly at nutritional risk hospitalized for acute stroke: a randomized, controlled trial. Clin Nutr. 2010;29(5):567-573. 7. Benson K, Hartz AJ. A comparison of observational studies and randomized, controlled trials. N Engl J Med. 2000;342(25):1878-1886. 8. Concato J, Shah N, Horwitz RI. Randomized, controlled trials, observational studies, and the hierarchy of research designs. N Engl J Med. 2000;342(25):1887-1892. 9. Horton S, Alderman H, Rivera JA. The Challenge of Hunger and Malnutrition. Copenhagen Consensus Center 2008 Challenge Paper. 2008. http://www.copenhagenconsensus.com/sites/default/files/cp_hungerandmalnutritioncc08vol2.pdf. Accessed June 18, 2014. 10. Snider J, Linthicum M, Wu Y, et al. Economic burden of communitybased disease-associated malnutrition in the United States. JPEN J Parenter Enteral Nutr. 2014;38(supp 2):77S-85S. 11. Blössner M, de Onís M. Malnutrition: Quantifying the Health Impact at National and Local Levels. Geneva, Switzerland: World Health Organization; 2005. Downloaded from pen.sagepub.com by guest on March 5, 2015 16S Journal of Parenteral and Enteral Nutrition 38(Suppl 2) 12. Singal AG, Higgins PD, Waljee AK. A primer on effectiveness and efficacy trials. Clin Transl Gastroenterol. 2014;5:e45. 13. Stratton RJ, Elia M. A review of reviews: a new look at the evidence for oral nutritional supplements in clinical practice. Clin Nutr Supp. 2007;2(1):5-23. 14. Philipson TJ, Snider JT, Lakdawalla DN, Stryckman B, Goldman DP. Impact of oral nutritional supplementation on hospital outcomes. Am J Manag Care. 2013;19(2):121-128. 15. Dehejia RH, Wahba S. Propensity score–matching methods for nonexperimental causal studies. Rev Econ Stat. 2002;84(1):151-161. 16. Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70(1):41-55. 17. Perkins SM, Tu W, Underhill MG, Zhou XH, Murray MD. The use of propensity scores in pharmacoepidemiologic research. Pharmacoepidemiol Drug Saf. 2000;9(2):93-101. 18. Hamdy O, Ernst FR, Baumer D, Mustad V, Partridge J, Hegazi R. Differences in resource utilization between patients with diabetes receiving glycemia-targeted specialized nutrition vs standard nutrition formulas in US hospitals. JPEN J Parenter Enteral Nutr. 2014;38(supp 2):86S-91S. 19. Caliendo M, Kopeinig S. Some practical guidance for the implementation of propensity score matching. J Econ Surv. 2008;22(1):31-72. 20. Lakdawalla DN, Mascarenhas M, Jena AB, et al. Impact of oral nutrition supplements on hospital outcomes in pediatric patients. JPEN J Parenter Enteral Nutr. 2014;38(supp 2):42S-49S. 21. Wright PG. The Tariff on Animal and Vegetable Oils (Appendix B). New York: Macmillan; 1928. 22. Levitt SD. Using electoral cycles in police hiring to estimate the effect of police on crime. Am Econ Rev. 1997;87(3):270-290. 23. Angrist JD, Imbens GW, Rubin DB. Identification of causal effects using instrumental variables. J Am Stat Assoc. 1996;91(434):444-455. 24. Weinstein MC, Siegel JE, Gold MR, Kamlet MS, Russell LB. Recommendations of the panel on cost-effectiveness in health and medicine. JAMA. 1996;276(15):1253-1258. 25. Garber AM, Phelps CE. Economic foundations of cost-effectiveness analysis. J Health Econ. 1997;16(1):1-31. 26. Weinstein MC, Stason WB. Foundations of cost-effectiveness analysis for health and medical practices. N Engl J Med. 1977;296(13):716-721. 27. Hodgson TA, Meiners MR. Cost-of-illness methodology: a guide to current practices and procedures. Milbank Mem Fund Q Health Soc. 1982;60(3):429-462. 28. Russell LB, Gold MR, Siegel JE, Daniels N, Weinstein MC. The role of cost-effectiveness analysis in health and medicine. JAMA. 1996;276(14):1172-1177. 29. Doig GS, Chevrou-Severac H, Simpson F. Early enteral nutrition in critical illness: a full economic analysis using US costs. Clinicoecon Outcomes Res. 2013;5:429-436. 30. Freijer K, Nuijten MJ. Analysis of the health economic impact of medical nutrition in the Netherlands. Eur J Clin Nutr. 2010;64(10):1229-1234. 31. Freijer K, Nuijten MJ, Schols JM. The budget impact of oral nutritional supplements for disease related malnutrition in elderly in the community setting. Front Pharmacol. 2012;3:78. 32. Siegel JE, Weinstein MC, Russell LB, Gold MR. Recommendations for reporting cost-effectiveness analyses. JAMA. 1996;276(16):1339-1341. 33. Gold MR, Stevenson D, Fryback DG. HALYS and QALYS and DALYS, oh my: similarities and differences in summary measures of population Health. Annu Rev Publ Health. 2002;23:115-134. 34. Dolan P, Gudex C, Kind P, Williams A. Valuing health states: a comparison of methods. J Health Econ. 1996;15(2):209-231. 35. Reddy P, Malone M. Cost and outcome analysis of home parenteral and enteral nutrition. JPEN J Parenter Enteral Nutr. 1998;22(5):302-310. 36. Behrman JR, Alderman H, Hoddinott J. The Challenge of Hunger and Malnutrition. Copenhagen Consensus Center 2004 Challenges and 37. 38. 39. 40. 41. 42. 43. 44. 45. 46. 47. 48. 49. 50. 51. 52. 53. 54. 55. Opportunities. 2004. http://www.copenhagenconsensus.com/sites/default/ files/CP%2B-%2BHunger%2BFINISHED.pdf. Accessed June 18, 2014. Bhagwati J, Bourguignon F, Kydland FE, et al. Copenhagen Consensus 2008—Results. Copenhagen Consensus Center 2008 Results. 2008. http:// www.copenhagenconsensus.com/sites/default/files/cc08_results_final_0. pdf. Accessed June 18, 2014. Bhagwati J, Fogel R, Frey B, et al. Copenhagen Consensus 2004: The Results. Copenhagen Consensus Center 2004 Results. 2004. http://www. hetn.org/pdf/CC_2004.pdf. Accessed June 18, 2014. Rajgopal R, Cox RH, Lambur M, Lewis EC. Cost-benefit analysis indicates the positive economic benefits of the expanded food and nutrition education program related to chronic disease prevention. J Nutr Educ Behav. 2002;34(1):26-37. Norman K, Pirlich M, Smoliner C, et al. Cost-effectiveness of a 3-month intervention with oral nutritional supplements in disease-related malnutrition: a randomised controlled pilot study. Eur J Clin Nutr. 2011;65(6):735-742. Hodgson TA, Meiners MR. Cost-of-illness methodology: a guide to current practices and procedures. Milbank Mem Fund Q Health Soc. 1982;60(3):429-462. Philipson TJ, Becker G, Goldman D, Murphy KM. Terminal care and the value of life near its end. Cambridge, MA: National Bureau of Economic Research; 2010. NBER Working Paper Series No. 15649. Stevens TH, Belkner R, Dennis D, Kittredge D, Willis C. Comparison of contingent valuation and conjoint analysis in ecosystem management. Ecol Econ. 2000;32(1):63-74. Arrow KJ, Solow R, Portney PR, Leamer E, Radner R, Schuman H. Report of the NOAA Panel on Contingent Valuation. Washington, DC: National Oceanic and Atmospheric Administration; 1993. de Lucas C, Moreno M, Lopez-Herce J, Ruiz F, Perez-Palencia M, Carrillo A. Transpyloric enteral nutrition reduces the complication rate and cost in the critically ill child. J Pediatr Gastr Nutr. 2000;30(2):175-180. Doig GS, Chevrou-Severac H, Simpson F. Early enteral nutrition in critical illness: a full economic analysis using US costs. Clinicoecon Outcomes Res. 2013;5:429-436. Elia M, Stratton RJ. A cost-utility analysis in patients receiving enteral tube feeding at home and in nursing homes. Clin Nutr. 2008;27(3):416-423. Amaral TF, Matos LC, Tavares MM, et al. The economic impact of disease-related malnutrition at hospital admission. Clin Nutr. 2007;26(6):778-784. Braunschweig C, Gomez S, Sheean PM. Impact of declines in nutritional status on outcomes in adult patients hospitalized for more than 7 days. J Am Diet Assoc. 2000;100(11):1316-1322. Chima CS, Barco K, Dewitt ML, Maeda M, Teran JC, Mullen KD. Relationship of nutritional status to length of stay, hospital costs, and discharge status of patients hospitalized in the medicine service. J Am Diet Assoc. 1997;97(9):975-980. Correia MI, Waitzberg DL. The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin Nutr. 2003;22(3):235-239. Efthimiou J, Fleming J, Gomes C, Spiro SG. The effect of supplementary oral nutrition in poorly nourished patients with chronic obstructive pulmonary disease. Am Rev Respir Dis. 1988;137(5):1075-1082. Kruizenga HM, Van Tulder MW, Seidell JC, Thijs A, Ader HJ, Van Bokhorst-de van der Schueren MA. Effectiveness and cost-effectiveness of early screening and treatment of malnourished patients. Am J Clin Nutr. 2005;82(5):1082-1089. National Collaborating Centre for Acute Care. Nutrition Support for Adults: Oral Nutrition Support, Enteral Tube Feeding and Parenteral Nutrition. London, UK: National Collaborating Centre for Acute Care; 2006. Centers for Medicare & Medicaid Services (HHS). Medicare and Medicaid programs; regulatory provisions to promote program efficiency, transparency, and burden reduction; part II; final rule. Fed Regist. 2014;91: 27106-27157. Downloaded from pen.sagepub.com by guest on March 5, 2015