Deadly, drug-resistant bug spreading beyond hospitals
Anuncio
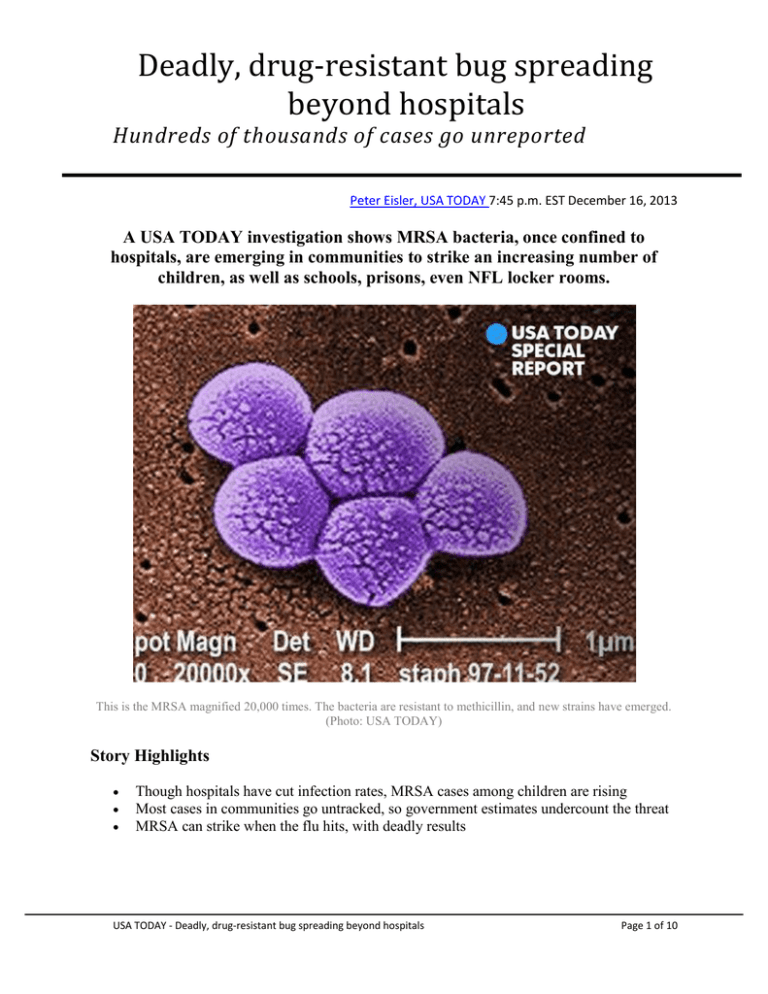
Deadly, drug-resistant bug spreading beyond hospitals Hundreds of thousands of cases go unreported Peter Eisler, USA TODAY 7:45 p.m. EST December 16, 2013 A USA TODAY investigation shows MRSA bacteria, once confined to hospitals, are emerging in communities to strike an increasing number of children, as well as schools, prisons, even NFL locker rooms. This is the MRSA magnified 20,000 times. The bacteria are resistant to methicillin, and new strains have emerged. (Photo: USA TODAY) Story Highlights Though hospitals have cut infection rates, MRSA cases among children are rising Most cases in communities go untracked, so government estimates undercount the threat MRSA can strike when the flu hits, with deadly results USA TODAY - Deadly, drug-resistant bug spreading beyond hospitals Page 1 of 10 Eric Allen went to bed March 1, thinking he had a light flu. By the time he staggered into the hospital in London, Ky., the next day, he was coughing up bits of lung tissue. Within hours, organs failing, he was in a coma. Tests showed that Allen, 39, had a ravaging pneumonia caused by methicillin-resistant Staphylococcus aureus, or MRSA, an antibiotic-resistant bacteria once confined to hospitals and other health care facilities. Allen hadn't been near a doctor or a hospital. Same with the next victim, a 54-year-old man, who came in days later and died within hours. And the victim after that, a 28-year-old woman, dead on arrival. The doctors were alarmed. "What really bothered me was the rapidity of their deterioration, a matter of hours," says Muhammad Iqbal, a pulmonologist who chairs the infection control committee at Saint JosephLondon hospital. "We were worried that something was spreading across the community." Indeed, a deadly form of MRSA had sprung from nowhere, picking off otherwise healthy people. The cases thrust Iqbal and his colleagues to the front lines of modern medicine''s struggle against antibiotic resistant bacteria – perhaps the nation's most daunting public health threat. No drugdefying bug has proved more persistent than MRSA, none has caused more frustration and none has spread more widely. In recent years, new MRSA strains have emerged to strike in community settings, reaching far beyond hospitals to infect schoolchildren, soldiers, prison inmates, even NFL players. A USA TODAY examination finds that MRSA infections, particularly outside of health care facilities, are much more common than government statistics suggest. They sicken hundreds of thousands of Americans each year in various ways, from minor skin boils to deadly pneumonia, claiming upward of 20,000 lives. The inability to detect or track cases is confounding efforts by public health officials to develop prevention strategies and keep the bacteria from threatening vast new swaths of the population. USA TODAY - Deadly, drug-resistant bug spreading beyond hospitals Page 2 of 10 Eric Allen is the only survivor of a deadly MRSA infection that swept through a rural part of Kentucky this year.(Photo: Jack Gruber, USA TODAY) "It's not about winning or losing the battle (against MRSA), it's that the battle is shifting," says Ramanan Laxminarayan, a Princeton University scholar who heads the Center for Disease Dynamics, Economics & Policy. "You're seeing people who are young and healthy getting this (in the community), and it's very serious. ... And it's not picked up in the statistics." To assess the evolving threat, USA TODAY reviewed federal data on hospitalizations and infection rates, academic studies and an array of government reports. Key findings: •Most cases go uncounted: Hundreds of thousands of MRSA cases a year are not included in government incidence estimates, because the Centers for Disease Control and Prevention can track only the sliver of cases that escalate to life-threatening infections. In 2011, the CDC reported 80,500 such cases, but that figure represents less than 20% of the hospitalizations that year in which billing data show an MRSA diagnosis. Countless more cases, typically less-serious skin infections, were treated outside hospitals. USA TODAY - Deadly, drug-resistant bug spreading beyond hospitals Page 3 of 10 This is a cutaneous abscess caused by MRSA on a hand.(Photo: Gregory Moran via cdc.gov) •Successes are masking new threats: The medical establishment has made substantial headway reducing MRSA linked to health care facilities, cutting the worst of those infections 30% or more since 2005. That widely touted progress obscures the fact that there's been little or no decline in cases from community-based strains. •Infections in kids are climbing: MRSA cases in children continue to rise, jumping 10% a year among youths ages 3 months to 17 years. A much larger share of the infections hitting children have been linked to community strains that can pass from kid to kid by, say, brushing against a victim at school or handling a contaminated object, such as a locker room towel. •Officials have a patchwork control plan: Health officials have made little progress developing strategies to reduce severe infections from the community strains that have grown increasingly prevalent. That's partly because most states, like the federal government, collect virtually no data on where and when most community-based cases occur. "The challenge now is in the community," says Robert Daum, an infectious disease physician and founder of the University of Chicago's MRSA Research Center. "With all due respect to our public health authorities, they made the transition in their minds very slowly that the epidemiology of MRSA had shifted. … So we are left with a community problem that has been largely unaddressed." NEW STRAINS: MRSA's favorite targets OLD BUG, NEW THREATS Staphylococcus aureus bacteria have been around for ages, but today's staph infections aren't what they used to be. USA TODAY - Deadly, drug-resistant bug spreading beyond hospitals Page 4 of 10 Staph occurs naturally and often exists without consequence on people's skin. It most often creates problems when it gets into cuts, causing skin infections – from small pimples to painful boils – that usually can be treated easily by doctors. In some cases, the infections advance, destroying tissue and causing large abscesses that can require hospitalization. When staph enters the bloodstream or attacks the lungs as bacterial pneumonia, it becomes especially dangerous — often fatal. In the 1940s, penicillin proved effective in treating staph infections, but the bacteria quickly grew resistant, so doctors switched to methicillin. By the 1960s, staph had beaten that, too. Methicillin-resistant Staphylococcus aureus – MRSA – had arrived. For the next 30 years, MRSA struck mainly in hospitals, creeping into patients via surgical sites, catheters and other paths. Then, in the '90s, new "community-associated" strains began showing up in people who'd had no contact with the medical system – and the MRSA problem got far more complicated. "We don't really understand the origin of these strains," says Costi Sifri, an infectious-disease physician at the University of Virginia Health System. "And we don't really know how to contain them." Today, community MRSA strains cause more than half of all the skin and soft tissue infections that send people to the hospital, various studies show. The good news is that there still are a few antibiotics that work against them – most of the time. The bad news is that there are other, more dangerous strains that pose especially grave threats. Perhaps most worrisome, some community strains carry a toxin linked to a lung-ravaging "necrotizing" pneumonia that tends to strike people with the flu or other underlying illnesses. When that pneumonia takes hold, victims often die in as little as 72 hours. Researchers at Texas A&M University's Health Science Center noted the toxin's ties to pneumonia in a 2007 study that raised alarms about its risks, especially if community MRSA infiltrates hospitals. Co-author M. Gabriela Bowden warned in a related article about "the aggressiveness of these (community MRSA) strains and the urgent need to develop new strategies to battle these infections." A BACTERIAL NIGHTMARE With two patients dead and Eric Allen fighting for his life, Iqbal and the infection control staff at Saint Joseph swung into emergency mode. USA TODAY - Deadly, drug-resistant bug spreading beyond hospitals Page 5 of 10 Muhammad Iqbal is a pulmonologist at Saint Joseph-London Hospital and chairman of the hospital's Infection Control Committee.(Photo: Jack Gruber, USA TODAY) They directed that any patient or new arrival with symptoms of respiratory illness be isolated and tested for MRSA. They notified the state Health Department, which alerted other hospitals in the region to watch for – and report – any patients with similar ailments. The department's regional epidemiologist, already on scene, was joined by a CDC counterpart assigned to the state Health Department. "Our first priority was to determine whether there was any ongoing, acute threat to public health," says Matthew Groenewold, the CDC epidemiologist. "We were looking for a common source of infection or transmission." USA TODAY - Deadly, drug-resistant bug spreading beyond hospitals Page 6 of 10 Matthew Groenewold, a CDC epidemiologist assigned to the Kentucky Department for Public Health, investigated a cluster of MRSA cases in the Cumberland Valley region.(Photo: Jack Gruber, USA TODAY) Searching for clues, the epidemiologists interviewed victims' families, the coroner and staff from hospitals and county health departments across the region. The key question proved hardest to answer: Were the London cases an anomaly, or were similar illnesses cropping up elsewhere? In Kentucky, as in most states, hospitals are not required to report individual MRSA cases. So there was no way to tell what they were dealing with. "It was hard to make statistical conclusions about the true fatality rate in the population," Groenewold says. More refined lab tests brought bad news about the MRSA strain seen in London: It carried the toxin that attacks victims' lungs. INFECTION DETECTIVES IN DARK Figuring out where and how often MRSA strikes is a huge challenge because nobody tracks all the cases. "We have more data on how many cows are in each county than we do on how many MRSA cases there are," says Kevin Kavanagh, a physician who chairs Health Watch USA, a patient advocacy group. "It's very hard to come up with (prevention strategies) if you don't have solid data." The CDC tracks only "invasive" MRSA infections – cases where the bacteria have reached the bloodstream or invaded internal organs. The CDC's estimate of 80,500 invasive MRSA cases in 2011, the most recent year of data, was celebrated as a significant decline from previous years. But that same year, there were nearly 460,000 hospitalizations involving an MRSA diagnosis, according to hospital billing data collected by the U.S. Agency for Healthcare Research and Quality. The data suggest those hospitalizations resulted in nearly 23,000 deaths. That means the CDC's figures on invasive MRSA cases excluded more than 375,000 MRSA infections that still were severe enough to involve hospital care. The agency also doesn't count lesser cases that were resolved on their own or with outpatient treatment and are never reported — a group some researchers put in the millions. What's more, most of the decline in severe MRSA infections has been in cases linked to health care, which fell 30% to 50%, reflecting better hygiene practices and new hospital protocols for maintaining catheters and other devices that can let bacteria into the body. The news for MRSA cases originating in the community is less encouraging: just a 5% decline. Among children, the outlook is especially bad. USA TODAY - Deadly, drug-resistant bug spreading beyond hospitals Page 7 of 10 Though no major outbreaks have been documented in schools, they report individual MRSA cases routinely, usually involving minor skin infections. Around Detroit, several schools have seen multiple cases this year; in Prince William County, Va., the school system issues monthly MRSA incident reports (one case in November; two in October). In a CDC-led report out this year, researchers found that MRSA is making its biggest gains among children. Not only did the study document a 10%-a-year rise in MRSA in kids from 2005-2010, it also found that the proportion of those cases involving community-associated MRSA jumped 55%. "With community strains getting more prevalent among children, that's going in a direction we don't want to see," says Scott Fridkin, an infectious disease physician who oversees the CDC's surveillance of antibiotic resistant illnesses in health care. KENTUCKY DOCTORS ZERO IN As the epidemiologists in Kentucky pressed ahead with their investigation, they began finding evidence of similar cases around the region. One was a 9-year-old boy who died in a neighboring county days before Eric Allen fell ill. The boy had the same rapid decline, and tests later showed that he had the same MRSA strain. But all the cases were isolated: one here, another there – nothing widespread, nothing to suggest a true outbreak. There were no known links between victims. "We could not identify any common risk factor," recalls Marion Pennington, the regional epidemiologist who helped lead the investigation. Marion Pennington, regional epidemiologist for the Kentucky Department of Health, played a lead role in investigating a deadly cluster of MRSA cases in 2013.(Photo: Jack Gruber, USA TODAY) USA TODAY - Deadly, drug-resistant bug spreading beyond hospitals Page 8 of 10 Ultimately, the investigators focused on six cases. Community-associated MRSA was confirmed in four. In two, the strain was suspected but not confirmed because the patients hadn't been tested. The epidemiologists developed a hypothesis. All six victims were infected after catching a late-season flu. Perhaps the MRSA was there all along, the investigators reasoned, and the flu simply weakened the patients' immune systems enough for it to take over. Groenewold says the theory rests partly on indications that the region has high MRSA "carriage rates" – a high percentage of people who carry the bacteria on their skin. The MRSA goes unnoticed until a bad flu sweeps in and then serious infections crop up sporadically. "We concluded that this wasn't something that was common, but probably wasn't rare either," Groenewold says. Because there's no systematic tracking of cases, he says, "we just don't know how often this is happening." MRSA CARRIERS CAN BE ISOLATED, TREATED Though upward of 30% of the public have garden-variety staph on their bodies, the CDC estimates that just 2% or so carry MRSA. Rodney Rohde, associate dean for research at Texas State University's College of Health Professions, says he thinks there's more. "We underestimate how much MRSA is out there in the general public," Rohde says. In studies, he's found MRSA in the nostrils of 4%-5% of prisoners and up to 8% of students in a single college dorm. He suspects the percentage in the general public could be twice the CDC's estimate. Those colonized with the bacteria are far more likely to get infections, so hospitals are eager to identify them quickly – and stop them from getting sick or spreading MRSA to other patients. Since 2007, the Veterans Health Administration – the nation's largest health care system – has screened all hospital patients for MRSA. Carriers are isolated and treated with special precautions. Hospital Corp. of America — the nation's largest health care provider — embraces a different approach. High-risk patients, usually in intensive care, are "decolonized" by wiping them down with antiseptic solution and antibiotic ointment. Both strategies, along with better hand washing and other infection controls, have been shown to reduce infections significantly. Many hospitals and other health care facilities where MRSA is common, such as nursing homes, have been slow to adopt such tactics. USA TODAY - Deadly, drug-resistant bug spreading beyond hospitals Page 9 of 10 "We need all the components for reducing infections at every health care facility – screening, hand hygiene, environmental hygiene, better management of antibiotics," says Jeanine Thomas, founder of the MRSA Survivors Network, a patient advocacy group. "That's just not happening." The challenges of reducing community-associated MRSA are even more daunting. Unlike the structured environment of a hospital, it's much harder to control behavior in a community. The CDC has issued guidelines encouraging better hygiene – bathing and hand washing – and warning people not to share personal items, such as sports equipment, towels or razors. Fact sheets tell administrators at schools, prisons and athletic facilities how to improve cleaning and disinfection practices. There's no knowing if the measures are adopted. "While there are general strategies to prevent people from developing skin infections ... it's not obvious what the most effective strategies are to prevent the more severe infections," says Fridkin, the CDC official. "Getting a handle on that is going to be very challenging." Many MRSA researchers say the best way to tackle community MRSA is to develop a vaccine for staph. Although there has been promising research, a marketable vaccine remains years away. BACTERIA MIGHT RETURN Victims such as Eric Allen are left wondering just what happened to them. "They don't even know for certain how I got this," says Allen, who was in a coma for about three weeks. When he awoke, he was the only survivor among the six suspected victims in Kentucky. "Nobody knows how any of these people got this, and a little boy died from it," Allen says. "It really took a toll." Although the infections in Allen's community vanished as quickly as they arrived, nobody knows if the bacteria are gone for good or simply waiting for another opportunity to strike again. "Some of these bugs tend to come and go over decades, and the question now is what will happen with community-associated MRSA," says Bob Weinstein, an infectious disease physician who chairs the Department of Medicine for the Cook County Health and Hospitals System. "How long will it be here before it wanes – or will it wane? We don't know." USA TODAY - Deadly, drug-resistant bug spreading beyond hospitals 10 Page 10 of